Return to flip book view
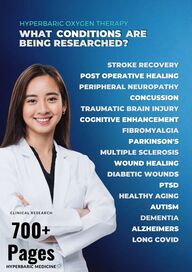
HYPERBARIC OXYGEN THERAPY WHAT CONDITIONS ARE BEING RESEARCHED STROKE RECOVERY POST OPERATIVE HEALING PERIPHERAL NEUROPATHY CONCUSSION TRAUMATIC BRAIN INJURY COGNITIVE ENHANCEMENT FIBROMYALGIA PARKINSON S MULTIPLE SCLEROSIS WOUND HEALING DIABETIC WOUNDS PTSD HEALTHY AGING CLINICAL RESEARCH 700 Pages HYPERBARIC MEDICINE AUTISM DEMENTIA ALZHEIMERS LONG COVID
About Hyperbarics 3 / 9 / 99 / 109 / 122 / 203Alzheimer's 425 / 473 / 642Aging 545 / 547
Brain Injury133 / 233 / 140 / 259 / 267 / 279 305 / 351 / 371 / 383 / 569Cerebal Palsy
401 / 413
Cognitive Issues
282 / 323 / 233 / 579
Concussion215 / 237 / 285Coronary Disease79 / 87
Covid199 / 211 / 645
Diabetes141 / 465Erectile Dysfunction27 / 31Middle Aged Athletes 751
Osteonecrosis724
Post Menopause
757
Parkinsons586 / 591 / 613 / 623Pancreatic Issues93
Skin Rejuvenation531 / 533SPECT Imaging41 / 61 / 65
Stroke441 / 501 / 507 / 627 / 652 / 687 / 691
Telomere Length
437 / 545
Research Papers on Hyperbaric Oxygen Therapy
1642 THE NEW ENGLAND JOURNAL OF MEDICINE June 20 1996 REVIEW ARTICLES MEDICAL PROGRESS HYPERBARIC OXYGEN THERAPY AND PATRICK M TIBBLES M D JOHN S EDELSBERG M D M P H H YPERBARIC oxygen 100 percent oxygen at two to three times the atmospheric pressure at sea level can result in arterial oxygen tension in excess of 2000 mm Hg1 and oxygen tension in tissue of almost 400 mm Hg 2 3 Such doses of oxygen have a number of bene cial biochemical cellular and physiologic effects and today there are 259 hyperbaric facilities in the United States with 344 single occupant monoplace hyperbaric oxygen chambers 4 In this article we review the mechanisms of action evidence of clinical ef cacy and risks of therapy with hyperbaric oxygen PHYSIOLOGIC EFFECTS For hyperbaric oxygen pressure is expressed in multiples of the atmospheric pressure at sea level which is 1 atmosphere 1 atmosphere 14 7 psi 1 kg per square centimeter 101 3 kPa 760 torr or 760 mm Hg At sea level the blood plasma oxygen concentration is 0 3 ml per deciliter 1 5 Tissues at rest extract 5 to 6 ml of oxygen per deciliter of blood assuming normal perfusion 1 6 Administering 100 percent oxygen at ambient normobaric pressure increases the amount of oxygen dissolved in the blood vefold to 1 5 ml per deciliter and at 3 atmospheres the dissolved oxygen content is approximately 6 ml per deciliter 1 more than enough to meet resting cellular requirements without any contribution from oxygen bound to hemoglobin The sudden formation of inert gas bubbles in blood vessels and tissues causes decompression sickness and air embolism Boyle s law which states that the volume of gas in an enclosed space is inversely proportional to the pressure exerted on it governs this process and explains some of the bene cial effects of hyperbaric oxygen in conditions caused by the formation of gas bubbles At 2 8 atmospheres bubble volume is reduced by almost two thirds In addition hyperbaric oxygen hastens the dissolution of the inert gas bubble by replacing the inert gas in the bubble with oxygen which is then rapidly metabolized by the tissues The use of hyperbaric oxygen also prevents the formation of new bubbles BIOCHEMICAL AND CELLULAR EFFECTS Local hypoxia predisposes wounds to infection because the neutrophil mediated killing of bacteria by From the Department of Emergency Medicine University of Massachusetts Medical Center 55 Lake Ave N Worcester MA 01655 where reprint requests should be addressed to Dr Tibbles 1996 Massachusetts Medical Society free radicals is decreased 7 8 Hyperbaric oxygen restores this defense against infection and increases the rate of killing of some common bacteria by phagocytes 2 In addition hyperbaric oxygen alone is bactericidal for certain anaerobes including Clostridium perfringens 9 and bacteriostatic for certain species of escherichia10 11 and pseudomonas 12 It also suppresses clostridial production of alpha toxin 13 14 Local hypoxia leads to poor wound healing Adequate oxygen tension is a prerequisite for the formation of collagen matrix which is essential for angiogenesis 7 15 16 In irradiated tissue hyperbaric oxygen is more effective than normobaric oxygen in increasing the partial pressure of oxygen to a level that promotes the formation of collagen matrix and angiogenesis 17 Whether hyperbaric oxygen is superior to 40 to 100 percent normobaric oxygen in improving wound healing in nonirradiated tissue is not clear 16 18 20 Reperfusion injury can worsen crush injuries and compartment syndromes and cause skin aps and reattachment procedures to fail Neutrophils have been implicated as the prime endogenous culprit in reperfusion injury 21 Adhering to the walls of ischemic vessels they release proteases and produce free radicals leading to pathologic vasoconstriction and extensive tissue destruction 22 Hyperbaric oxygen inhibits neutrophil adherence and postischemic vasoconstriction in ischemic rat tissue 21 23 Since the pioneering work of Bernard in the 1850s the toxic effects of carbon monoxide have been attributed primarily to its indirect inhibition of cellular respiration by its reversible binding to hemoglobin 24 Hyperbaric oxygen at 2 5 atmospheres reduces the half life of carboxyhemoglobin from 4 to 5 hours in subjects breathing room air to 20 minutes or less 25 Two additional bene cial effects of hyperbaric oxygen in carbon monoxide poisoning have been established In vitro carbon monoxide binds to a component of the electron transport chain cytochrome c oxidase leading to cellular asphyxiation The dissociation of carbon monoxide from this enzyme by hyperbaric oxygen is postulated to account for some of the ef cacy of this therapy 26 27 In rats with carbon monoxide mediated brain injury neutrophils appeared to trigger an enzymatic process leading to the formation of oxygen radicals and neuronal death from lipid peroxidation 28 29 The timely administration of hyperbaric oxygen to these animals prevented neuronal injury in a dose dependent fashion by an unknown mechanism 30 31 ADMINISTRATION To be effective hyperbaric oxygen must be inhaled in the atmosphere or through an endotracheal tube in a monoplace chamber Fig 1 or through masks tight tting hoods or endotracheal tubes in a larger multi occupant chamber The duration of single treatments varies from 45 minutes for carbon monoxide poisoning to almost 5 hours for some severe decompression disorders For treatment of wounds that do not respond to d bride Downloaded from www nejm org by ROBERT WARRINER on July 31 2004 Copyright 1996 Massachusetts Medical Society All rights reserved
Vol 334 No 25 MEDICAL PROGRESS ment or antibiotics that is problem wounds most protocols average 90 minutes for each of 20 to 30 treatments Critical care monitoring and treatment including mechanical ventilation should be readily available Their portability minimal personnel requirements and relatively low cost have made monoplace chambers the most common type of chamber worldwide 32 THERAPEUTIC USES OF HYPERBARIC OXYGEN Carbon Monoxide Poisoning Carbon monoxide poisoning primarily from smoke inhalation and suicide attempts is the most common cause of death by poisoning in the United States 33 34 Although there is no universally accepted scheme for grading the severity of carbon monoxide poisoning severe poisoning is indicated by loss of consciousness syncope seizures and coma neurologic de cits pulmonary edema myocardial ischemia and severe metabolic acidosis Less severely poisoned patients may have headache nausea and other constitutional symptoms In addition to the acute toxic effects all victims of carbon monoxide poisoning are at risk for delayed neuropsychological sequelae Carboxyhemoglobin levels do not correlate well with the clinical severity of carbon monoxide poisoning Numerous nonrandomized studies have found that hyperbaric oxygen reverses both the acute and the delayed effects of carbon monoxide poisoning 35 However two trials comparing hyperbaric oxygen with normobaric oxygen delivered outside a hyperbaric chamber in patients with no loss of consciousness had con icting results36 37 in a third trial in which 17 of 26 patients had transient loss of consciousness hyperbaric oxygen was bene cial Table 1 38 An early analysis of data on 50 patients with acute carbon monoxide poisoning who were enrolled in a trial of hyperbaric oxygen as compared with normobaric oxygen delivered in a hyperbaric chamber a true sham control revealed no difference in persistent or delayed neuropsychological sequelae between the treatment groups Table 1 39 Because hyperbaric oxygen is the fastest method of reversing the potentially life threatening effects of acute carbon monoxide poisoning we think that patients with severe carbon monoxide poisoning should receive at least one treatment with hyperbaric oxygen at 2 5 to 3 0 atmospheres additional treatments may produce greater improvement in neuropsychological de cits For patients with lesser degrees of poisoning we advise consultation with a toxicologist to determine whether the administration of 100 percent normobaric oxygen for four to six hours or until symptoms abate would be adequate therapy Decompression Sickness When recreational divers breathing compressed air return to the water surface too rapidly the partial pressure of nitrogen dissolved in their tissues and blood may exceed the ambient pressure Gas bubbles then form in the tissues and blood causing a disease called decompression sickness Affected divers may have a spectrum of symptoms ranging from self limited rash to paralysis seizures and even death as a result of the 1643 blocking of lymphatics veins and arteries by the gas bubbles Each year in the United States approximately 500 recreational divers using self contained underwater breathing apparatus scuba have decompression sickness 47 Although it is largely a disease of divers persons ascending above 5500 m can also have decompression sickness altitude decompression sickness 48 Reduction in bubble size and correction of hypoxia have been considered the primary mechanisms by which hyperbaric oxygen bene ts patients with decompression sickness In this disorder biochemical actions at the blood gas interface lead to alterations in hemostasis endothelial damage and activation of leukocytes 49 The bene cial effect of hyperbaric oxygen on these pathologic mechanisms may play a more important part in clinical improvement than the reduction in the size of bubbles and the correction of hypoxia Thousands of favorable responses to early therapy with hyperbaric oxygen during the past 50 years have established it as the primary treatment for decompression sickness although no randomized trials have compared hyperbaric with normobaric oxygen Patients who have decompression sickness should receive hyperbaric oxygen at 2 5 to 3 0 atmospheres for two to four hours with repeated or longer treatment as necessary until they are symptom free or there is no further clinical improvement The outcome is more likely to be successful if therapy is begun within six hours after the onset of symptoms 50 Arterial Gas Embolism Arterial gas embolism can arise from pulmonary overin ation during a dive often as a consequence of uncontrolled ascent to the surface or during mechanical ventilation This disorder can also result from the placement of a central venous catheter cardiothoracic surgery hemodialysis and oral vaginal sex during pregnancy 51 53 Immediate therapy with hyperbaric oxygen typically at 2 5 to 3 0 atmospheres for two to four hours is the treatment of choice given the well established pathophysiology of arterial gas embolism and numerous reports of improvement immediately after hyperbaric treatment 50 Such treatment improves outcome in these patients by the mechanisms described for decompression sickness Radiation Induced Tissue Injury Irradiated tissues lose the capacity for restorative cellular proliferation leading to decreased vascularity local hypoxia and eventually necrosis 17 54 This loss manifests itself clinically as edema ulceration bone necrosis increased risk of infection and poor wound healing processes that can persist for years 55 One hundred percent oxygen at 1 atmosphere produces insuf cient tissue oxygen gradients for wound healing in irradiated tissue but higher arterial partial pressures of oxygen result in new blood vessel growth and partial healing 56 Before hyperbaric oxygen therapy was available reconstruction of previously irradiated mandibular tissue in patients with oropharyngeal and other head and neck tumors was often unsuccessful with complications including osteonecrosis soft tissue radio Downloaded from www nejm org by ROBERT WARRINER on July 31 2004 Copyright 1996 Massachusetts Medical Society All rights reserved
1644 THE NEW ENGLAND JOURNAL OF MEDICINE June 20 1996 1200 cases of clostridial myonecrosis treated with hyperbaric oxygen have been reported 61 The available clinical and experimental evidence suggests that multiple early treatment sessions with hyperbaric oxygen at 3 atmospheres for 90 minutes when administered in conjunction with antibiotics and surgery confer the following bene ts the border between devitalized and healthy tissue is more clearly demarcated permitting surgeons to be more conservative in their excisions the extent of amputation required in clostridial myonecrosis involving the extremities is decreased and systemically ill patients often improve substantially after one or two treatments Necrotizing Fasciitis Figure 1 Monoplace Hyperbaric Chamber Photograph courtesy of Massachusetts Eye and Ear In rmary Boston necrosis mucositis dermatitis and laryngeal radionecrosis developing in 50 to 60 percent of patients With hyperbaric oxygen success rates of up to 93 percent have been reported among selected patients 41 57 59 In an unblinded controlled trial 30 hyperbaric oxygen treatments were more effective in preventing the development of mandibular osteoradionecrosis than penicillin in 37 previously irradiated patients Table 1 40 In a preliminary analysis of 160 irradiated patients undergoing soft tissue ap surgery preoperative therapy with hyperbaric oxygen was superior to routine care in reducing wound dehiscence infections and delayed wound healing 41 Current protocols for the prevention and treatment of osteoradionecrosis involve 30 preoperative hyperbaric oxygen sessions at 2 4 atmospheres for 90 minutes each followed by 10 treatments after surgery Clostridial Myonecrosis Although clostridia commonly contaminate traumatic wounds clostridial myonecrosis a rapidly progressive life threatening infection is rare In this disease clostridial production of toxins especially alpha toxin leads to extensive tissue destruction and shock Although classically associated with traumatic wounds in war clostridial myonecrosis occurs almost as often after abdominal surgery as it does after traumatic wounds and cases have been reported after bee stings and venipuncture The patients present with pain out of proportion to the apparent severity of their wounds and often have evidence of tissue gas gas gangrene The mainstay of treatment of clostridial myonecrosis has always been immediate surgical decompression and excision of all necrotic tissue Penicillin remains the most effective antimicrobial drug In a study comparing treatment of clostridial myonecrosis in dogs with and without hyperbaric oxygen in combination with surgery and antibiotics the respective survival rates were 95 percent and 70 percent P 0 05 60 More than Rapidly progressive infections of the skin and underlying tissue without muscle involvement are most commonly referred to as necrotizing fasciitis Mortality is high Because these infections have similarities to clostridial myonecrosis hyperbaric oxygen in conjunction with surgery and antibiotic therapy has been used to treat them although fewer patients have been treated with hyperbaric oxygen for necrotizing fasciitis than for clostridial myonecrosis Hyperbaric oxygen was effective in two of four small observational studies in humans some with historical controls 62 65 Refractory Osteomyelitis Hyperbaric oxygen has proved effective in the treatment of experimental osteomyelitis in rabbits66 and has greatly improved the outcome in patients with chronic osteomyelitis that is unresponsive to standard surgical and antibiotic therapy 67 In a study comparing hyperbaric oxygen therapy with no additional therapy beyond surgical d bridement and antibiotics in 28 patients with chronic refractory osteomyelitis there was no difference between the groups in length of hospitalization mean 54 days or clinical outcome 68 However because more than 90 percent of the patients in the group that did not receive hyperbaric oxygen were cured the de nition of refractory osteomyelitis in this study is suspect Hyperbaric oxygen at 2 0 to 2 5 atmospheres for 90 to 120 minutes after d bridement in combination with antibiotic therapy can improve healing Acute Traumatic Ischemic Injury Crush injury and other severe trauma to the extremities can result in tears of the major vessels and damage to the microcirculation with resultant ischemia edema compartment syndromes and tissue necrosis Surgery remains the cornerstone of therapy for these injuries Reduction of edema protection from reperfusion injury and enhanced wound healing are postulated bene ts of adjunctive therapy with hyperbaric oxygen Downloaded from www nejm org by ROBERT WARRINER on July 31 2004 Copyright 1996 Massachusetts Medical Society All rights reserved
Vol 334 No 25 MEDICAL PROGRESS 1645 Table 1 Summary of Randomized Controlled Trials of Hyperbaric Oxygen for Current Therapeutic Uses TRIAL NO OF PATIENTS INDICATIONS TYPE OF ANALYSIS CONTROL THERAPY RESULTS P VALUE VALUE IN OUTCOME MEASURES Raphael et al 36 343 Carbon monoxide poisoning without loss of consciousness 100 normobaric oxygen Thom et al 37 65 Carbon monoxide poisoning without loss of consciousness 100 normobaric oxygen Ducasse et al 38 26 Carbon monoxide poisoning in 100 normobaric patients with transient loss oxygen of consciousness mild neurologic de cits or constitutional symptoms Weaver et al 39 Marx et al 40 Marx41 Perrins42 Hart et al 43 Brannen et al 44 50 Carbon monoxide poisoning with and without loss of consciousness 74 Dental extraction after mandibular irradiation 160 Major soft tissue surgery including ap placement after irradiation 48 Every patient presenting for split skin grafting 16 Thermal burns over 10 50 of the body 125 Acute thermal burns Surgery and routine wound care Usual burn care at the time and 21 oxygen at 1 3 atmospheres in hyperbaric chamber Usual burn care Hammarlund and Sundberg45 16 Leg ulcers in nondiabetic patients with no large vessel disease Air at 2 5 atmospheres Doctor et al 46 30 Chronic diabetic foot lesions Surgery antibiotics local wound care VALUE IN OXYGEN CONTROL GROUP GROUP Not blinded Symptoms of carbon monoxide poi34 32 NS soning or neurologic de cits assessed by physical examination and questionnaire Not blinded Acute neuropsychological symptoms Multiple comparisons NS of symptoms and neuropsychological test scores Delayed neuropsychological 0 23 0 05 sequelae Open and Symptoms and abnormal physical 0 38 0 05 blinded examination at 12 hr Class II EEG at 24 hr 31 62 NS Class II EEG at 21 days 0 60 0 02 Degree of cerebral vessel 45 33 Signi cant reactivity Blinded Persistent and delayed neuro16 8 NS psychological sequelae 100 oxygen at 1 0 atmosphere in hyperbaric chamber Penicillin for 10 days Not blinded Osteoradionecrosis at 6 mo Reparative surgery HYPERBARIC Unknown Wound dehiscence Infection Wound healing delay Not blinded Mean percentage of permanent graft survival Blinded Mean healing time Fluid requirement in 24 hr Unknown Length of hospital stay Extent of autografting Mortality Blinded Reduction in wound area at 2 wk 4 wk 6 wk Not blinded Bacterial growth Major amputation Length of hospital stay 5 30 0 005 11 6 11 84 48 24 55 62 0 001 0 005 0 005 0 01 20 days 44 days 35 reduc tion 0 005 Unknown 21 days 21 days 1352 cm2 1379 cm2 11 11 NS NS NS 6 3 22 4 36 3 3 patients 12 patients 2 patients 7 patients 41 days 47 days NS 0 05 0 001 0 05 0 05 NS NS denotes reported as not statistically signi cant P value not given and EEG electroencephalogram Blinded interim analysis with treatment groups unknown at this time Hyperbaric oxygen was more effective than no treatment in animals with experimentally induced ischemia and compartment syndromes 20 69 71 Although many case reports and case series suggest a bene t of hyperbaric oxygen 72 it has not been compared with normobaric oxygen in patients or animals with acute traumatic ischemic injury Perioperative protocols involve treatment at pressures ranging from 2 0 to 2 8 atmospheres for up to two hours Compromised Skin Grafts and Flaps Skin grafts and reconstructive aps may fail because of inadequate perfusion and hypoxia Graft or ap failure is less frequent in animals receiving hyperbaric oxygen than in those receiving no treatment 23 73 74 In a series of 105 patients hyperbaric oxygen reversed distal ap ischemia and increased the rate of successful grafting in poorly vascularized tissue 75 In a group of 48 patients receiving split thickness skin grafts the graft survival rates were higher in the patients treated with hyperbaric oxygen Table 1 42 Hyperbaric oxygen treatments at 2 0 to 2 5 atmospheres for 90 to 120 minutes each should be considered when a graft or ap must be placed over a capillary bed with poor circulation especially if previous reconstruction in the same area was unsuccessful Anemia Due to Exceptional Blood Loss Under hyperbaric conditions the amount of oxygen dissolved in the blood can be suf cient to meet cellular metabolic demands without any contribution from oxygen transported by hemoglobin Hyperbaric oxygen has been used successfully to treat hemorrhagic shock in patients for whom suitable blood was not available or who refused transfusion for religious reasons 76 Thermal Burns The postulated mechanisms of a bene cial effect of hyperbaric oxygen on burn wounds are decreased edema due to hyperoxic vasoconstriction 43 77 78 increased Downloaded from www nejm org by ROBERT WARRINER on July 31 2004 Copyright 1996 Massachusetts Medical Society All rights reserved
1646 THE NEW ENGLAND JOURNAL OF MEDICINE collagen formation and improved phagocytic killing of bacteria In a trial comparing burn treatment with and without hyperbaric oxygen in 16 patients the mean healing time was signi cantly shorter in the group receiving hyperbaric oxygen Table 1 43 Among 266 patients with burns who were treated with hyperbaric oxygen and 609 who were not there were no signi cant differences in mortality and length of hospital stay 79 The preliminary results of a randomized controlled trial of hyperbaric oxygen at a burn center in Augusta Georgia were reported recently among 125 patients randomly assigned to usual burn care or usual burn care plus hyperbaric oxygen the outcomes were virtually identical Table 1 44 During the past two decades there have been many advances in burn therapy including improved respiratory care better use of topical and parenteral antibiotics early d bridement and parenteral nutrition At this time it is not clear that hyperbaric oxygen confers any bene ts when added to the usual care provided to patients in burn centers Problem Wounds In this country hyperbaric oxygen is used for problem wounds especially diabetic foot infections and leg ulcers caused by arterial insuf ciency more than for any other indication In a study comparing 62 diabetic patients with foot ulcers who were treated with hyperbaric oxygen an average of 72 treatments per patient 18 similar patients unable or unwilling to undergo therapy with hyperbaric oxygen and 49 patients treated before the availability of hyperbaric oxygen at the same institution Oriani et al found amputation rates of 4 49 and 39 percent respectively 80 In a prospective double blind study of 16 nonsmokers with chronic leg ulcers but with no largevessel disease or major chronic illnesses who received 30 treatments with either hyperbaric oxygen or hyperbaric air the wound area had decreased more at four and six weeks in the patients treated with hyperbaric oxygen Table 1 45 It is not clear that these results can be generalized to the majority of patients with problem wounds many of whom are smokers and have chronic illnesses such as vascular disease and diabetes In a study of 30 diabetic patients with foot lesions treated with routine care or with routine care plus four 45minute hyperbaric oxygen treatments fewer patients in the group receiving hyperbaric oxygen required abovethe ankle amputation Table 1 46 It is not clear why improvement occurred with so few treatments when in other studies a minimum of 30 treatments was necessary to improve healing Measurements of the transcutaneous oxygen tension are useful for evaluating the severity of peripheral vascular disease and the healing potential of lower extremity wounds 81 83 A trial of adjunctive therapy with hyperbaric oxygen at 2 0 to 2 5 atmospheres for 90 to 120 minutes may be reasonable in patients with problem wounds if arterial insuf ciency has been appropriately treated maximal antibiotic therapy has been given and June 20 1996 Table 2 Diseases for Which Hyperbaric Oxygen Is Currently Used Diseases for which the weight of scienti c evidence supports hyperbaric oxygen as effective therapy Primary therapy Arterial gas embolism Decompression sickness Exceptional blood loss anemia Severe carbon monoxide poisoning Adjunctive therapy Clostridial myonecrosis Compromised skin grafts and aps Osteoradionecrosis prevention Diseases for which the weight of scienti c evidence suggests hyperbaric oxygen may be helpful Primary therapy Less severe carbon monoxide poisoning Adjunctive therapy Acute traumatic ischemic injury Osteoradionecrosis Refractory osteomyelitis Selected problem wounds Radiation induced soft tissue injury Diseases for which the weight of scienti c evidence does not support the use of hyperbaric oxygen but for which it may be helpful Adjunctive therapy Necrotizing fasciitis Thermal burns the transcutaneous oxygen tension around the wound increases during exposure to hyperbaric oxygen 84 ADVERSE EFFECTS When used according to standard protocols with oxygen pressures not exceeding 3 atmospheres and treatment sessions limited to a maximum of 120 minutes hyperbaric therapy is safe However some adverse effects may occur Reversible myopia a consequence of the direct toxic effect of oxygen on the lens is the most common side effect Cataract formation however has not been seen in patients treated according to standard protocols 85 A few patients may experience mild tosevere pain from rupture of the middle ear the cranial sinuses and in rare cases the teeth or lungs as a result of rapid pressure changes that is barotrauma Inhalation of high concentrations of oxygen under pressure may precipitate generalized seizures but these are rare and self limited and cause no permanent damage 86 With repeated exposure to hyperbaric oxygen some patients have reversible tracheobronchial symptoms chest tightness a substernal burning sensation and cough with concomitant reversible decrements in pulmonary function Critically ill patients who have required high concentrations of normobaric oxygen for a prolonged period and then undergo repeated exposure to hyperbaric oxygen are at greater risk for toxic pulmonary effects Claustrophobia can be a problem in monoplace chambers No evidence of a tumorigenic effect of hyperbaric oxygen has been found to date 87 COST An average 90 minute hyperbaric oxygen treatment in the United States costs between 300 and 400 The cost of 30 to 40 sessions for the treatment of radione Downloaded from www nejm org by ROBERT WARRINER on July 31 2004 Copyright 1996 Massachusetts Medical Society All rights reserved
Vol 334 No 25 MEDICAL PROGRESS crosis or problem wounds can therefore range from 9 000 to 16 000 A simple economic analysis of hyperbaric oxygen therapy and surgery in patients with osteoradionecrosis however reported a savings of 96 000 as compared with in hospital nonhyperbaric oxygen therapy 41 CONCLUSIONS Hyperbaric oxygen has been described as a therapy in search of diseases 88 Many of its past uses had little or no scienti c support The discovery of bene cial cellular and biochemical effects has strengthened the rationale for administering hyperbaric oxygen as primary therapy in patients with severe carbon monoxide poisoning decompression sickness and arterial gas embolism and as adjunctive therapy for the prevention and treatment of osteoradionecrosis clostridial myonecrosis and compromised skin grafts and aps The physiologic effects of hyperbaric oxygen on plasma oxygen content make this therapy the treatment of choice in severe anemia when transfusion is not an option There is less scienti c support for the other uses of hyperbaric oxygen although reports of favorable effects support many of them In Table 2 we have attempted to aid clinicians in their decision making by categorizing the indications for hyperbaric oxygen therapy proposed by the Undersea and Hyperbaric Medical Society 89 The paucity of randomized controlled trials makes it dif cult to assess the ef cacy of hyperbaric oxygen in most diseases In diseases for which the use of hyperbaric oxygen is not well supported the potential bene ts must be carefully weighed against the risks of transferring the patient if necessary and the cost We are indebted to Dr Paul Weathersby Dr Paul Marik Dr Robert Stine and Mr Dick Clarke for their comments on the manuscript and to Ms Christine Haig for secretarial assistance REFERENCES 1 Lambertsen CJ Kough RH Cooper DY Emmel GL Loeschcke HH Schmidt CF Oxygen toxicity effects in man of oxygen inhalation at 1 and 3 5 atmospheres upon blood gas transport cerebral circulation and cerebral metabolism J Appl Physiol 1953 5 471 86 2 Mader JT Brown GL Guckian JC Wells CH Reinarz JA A mechanism for the amelioration by hyperbaric oxygen of experimental staphylococcal osteomyelitis in rabbits J Infect Dis 1980 142 915 22 3 Marx RE Johnson RP Problem wounds in oral and maxillofacial surgery the role of hyperbaric oxygen In Davis JC Hunt TK eds Problem wounds the role of oxygen New York Elsevier 1988 65 123 4 Directory of hyperbaric chambers United States and Canada Bethesda Md Undersea and Hyperbaric Medical Society 1996 5 Boerema I Meyne NG Brummelkamp WK et al Life without blood a study of the in uence of high atmospheric pressure and hypothermia on dilution of the blood J Cardiovasc Surg 1960 1 133 46 6 Kety SS Schmidt CF The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood ow and cerebral oxygen consumption of normal young men J Clin Invest 1948 27 484 92 7 Hunt TK The physiology of wound healing Ann Emerg Med 1988 17 1265 73 8 Knighton DR Halliday B Hunt TK Oxygen as an antibiotic a comparison of the effects of inspired oxygen concentration and antibiotic administration on in vivo bacterial clearance Arch Surg 1986 121 191 5 9 Hill GB Osterhout S Experimental effects of hyperbaric oxygen on selected clostridial species I In vitro studies J Infect Dis 1972 125 17 25 10 Boehm DE Vincent K Brown OR Oxygen and toxicity inhibition of amino acid biosynthesis Nature 1976 262 418 20 11 Brown OR Reversible inhibition of respiration of Escherichia coli by hyperoxia Microbios 1972 5 7 16 1647 12 Park MK Muhvich KH Myers RAM Marzella L Hyperoxia prolongs the aminoglycoside induced postantibiotic effect in Pseudomonas aeruginosa Antimicrob Agents Chemother 1991 35 691 5 13 van Unnik AJM Inhibition of toxin production in Clostridium perfringens in vitro by hyperbaric oxygen Antonie Van Leeuwenhoek 1965 31 181 6 14 Kaye D Effect of hyperbaric oxygen on Clostridia in vitro and in vivo Proc Soc Exp Biol Med 1967 124 360 6 15 Prockop DJ Kivirikko KI Tuderman L Guzman NA The biosynthesis of collagen and its disorders N Engl J Med 1979 301 13 23 77 85 16 Hunt TK Pai MP The effect of varying ambient oxygen tensions on wound metabolism and collagen synthesis Surg Gynecol Obstet 1972 135 561 7 17 Marx RE Ehler WJ Tayapongsak P Pierce LW Relationship of oxygen dose to angiogenesis induction in irradiated tissue Am J Surg 1990 160 519 24 18 Knighton DR Silver IA Hunt TK Regulation of wound healing angiogenesis effect of oxygen gradients and inspired oxygen concentration Surgery 1981 90 262 70 19 Kulonen E Niinikoski J Effect of hyperbaric oxygenation on wound healing and experimental granuloma Acta Physiol Scand 1968 73 383 4 20 Uhl E Sirsjo A Haapaniemi T Nilsson G Nylander G Hyperbaric oxygen improves wound healing in normal and ischemic skin tissue Plast Reconstr Surg 1994 93 835 41 21 Zamboni WA Roth AC Russell RC Graham B Suchy H Kucan JO Morphologic analysis of the microcirculation during reperfusion of ischemic skeletal muscle and the effect of hyperbaric oxygen Plast Reconstr Surg 1993 91 1110 23 22 Weiss SJ Tissue destruction by neutrophils N Engl J Med 1989 320 36576 23 Zamboni WA Roth AC Russell RC Nemiroff PM Casas L Smoot EC The effect of acute hyperbaric oxygen therapy on axial pattern skin ap survival when administered during and after total ischemia J Reconstr Microsurg 1989 5 343 7 24 Bernard C Le ons sur les effets des substances toxiques et m dicamenteuses Paris J B Bailli re et Fils 1857 25 Pace N Strajman E Walker EL Acceleration of carbon monoxide elimination in man by high pressure oxygen Science 1950 111 652 4 26 Brown SD Piantadosi CA In vivo binding of carbon monoxide to cytochrome c oxidase in rat brain J Appl Physiol 1990 68 604 10 27 Goldbaum LR Ramirez RG Absalon KB What is the mechanism of carbon monoxide toxicity Aviat Space Environ Med 1975 46 1289 91 28 Thom SR Dehydrogenase conversion to oxidase and lipid peroxidation in brain after carbon monoxide poisoning J Appl Physiol 1992 73 1584 9 29 Idem Leukocytes in carbon monoxide mediated brain oxidative injury Toxicol Appl Pharmacol 1993 123 234 47 30 Idem Functional inhibition of leukocyte B2 integrins by hyperbaric oxygen in carbon monoxide mediated brain injury in rats Toxicol Appl Pharmacol 1993 123 248 56 31 Thom SR Ohnishi ST Ischiropoulos H Nitric oxide released by platelets inhibits neutrophil B2 integrin function following acute carbon monoxide poisoning Toxicol Appl Pharmacol 1994 128 105 10 32 Hart GB The monoplace chamber In Kindwall EP ed Hyperbaric medicine practice Flagstaff Ariz Best 1994 57 82 33 Cobb N Etzel RA Unintentional carbon monoxide related deaths in the United States 1979 through 1988 JAMA 1991 266 659 63 34 National Center for Health Statistics Vital statistics of the United States 1990 Vol II Mortality Part A Washington D C Government Printing Of ce 1994 DHHS publication no PHS 95 1101 35 Tibbles PM Perrotta PL Treatment of carbon monoxide poisoning a critical review of human outcome studies comparing normobaric oxygen with hyperbaric oxygen Ann Emerg Med 1994 24 269 76 36 Raphael J C Elkharrat D Jars Guincestre MC et al Trial of normobaric and hyperbaric oxygen for acute carbon monoxide intoxication Lancet 1989 2 414 9 37 Thom SR Taber RL Mendiguren II Clark JM Hardy KR Fisher AB Delayed neuropsychologic sequelae after carbon monoxide poisoning prevention by treatment with hyperbaric oxygen Ann Emerg Med 1995 25 47480 38 Ducasse JL Celsis P Marc Vergnes JP Non comatose patients with acute carbon monoxide poisoning hyperbaric or normobaric oxygenation Undersea Hyperb Med 1995 22 9 15 39 Weaver LK Hopkins RO Larson Lohr V Howe S Haberstock D Doubleblind controlled prospective randomized clinical trial RCT in patients with acute carbon monoxide CO poisoning outcome of patients treated with normobaric oxygen or hyperbaric oxygen HBO2 an interim report Undersea Hyperb Med 1995 22 Suppl 14 abstract 40 Marx RE Johnson RP Kline SN Prevention of osteoradionecrosis a randomized prospective clinical trial of hyperbaric oxygen versus penicillin J Am Dent Assoc 1985 111 49 54 41 Marx RE Radiation injury to tissue In Kindwall EP ed Hyperbaric medicine practice Flagstaff Ariz Best 1994 447 503 42 Perrins DJD In uence of hyperbaric oxygen on the survival of split skin grafts Lancet 1967 1 868 71 Downloaded from www nejm org by ROBERT WARRINER on July 31 2004 Copyright 1996 Massachusetts Medical Society All rights reserved
1648 THE NEW ENGLAND JOURNAL OF MEDICINE 43 Hart GB O Reilly RR Broussard ND Cave RH Goodman DB Yanda RL Treatment of burns with hyperbaric oxygen Surg Gynecol Obstet 1974 139 693 6 44 Brannen AL Still J Haynes MS et al A randomized prospective trial of hyperbaric oxygen in a referral burn center population Undersea Hyperb Med 1995 22 Suppl 11 abstract 45 Hammarlund C Sundberg T Hyperbaric oxygen reduced size of chronic leg ulcers a randomized double blind study Plast Reconstr Surg 1994 93 829 33 46 Doctor N Pandya S Supe A Hyperbaric oxygen therapy in diabetic foot J Postgrad Med 1992 38 112 4 47 Divers Alert Network report on 1993 diving accidents and fatalities Durham N C Duke University Medical Center 1995 48 Blumen IJ Abernethy MK Dunne MJ Flight physiology clinical considerations Crit Care Clin 1992 8 597 618 49 Francis TJR Gorman DF Pathogenesis of the decompression disorders In Bennett PB Elliott DH eds The physiology and medicine of diving 4th ed Philadelphia W B Saunders 1993 454 80 50 Moon RE Gorman DF Treatment of the decompression disorders In Bennett PB Elliott DH eds The physiology and medicine of diving 4th ed Philadelphia W B Saunders 1993 506 41 51 Murphy BP Harford FJ Cramer FS Cerebral air embolism resulting from invasive medical procedures treatment with hyperbaric oxygen Ann Surg 1985 201 242 5 52 Baskin SE Wozniak RF Hyperbaric oxygenation in the treatment of hemodialysis associated air embolism N Engl J Med 1975 293 184 5 53 Fyke FE III Kazmier FJ Harms RW Venous air embolism life threatening complication of orogenital sex during pregnancy Am J Med 1985 78 333 6 54 Mustoe TA Porras Reyes BH Modulation of wound healing response in chronic irradiated tissues Clin Plast Surg 1993 20 465 72 55 Ewing J Radiation osteitis Acta Radiol 1926 6 399 413 56 Marx RE Johnson RP Studies in the radiobiology of osteoradionecrosis and their clinical signi cance Oral Surg Oral Med Oral Pathol 1987 64 379 90 57 Marx RE Ames JR The use of hyperbaric oxygen therapy in bony reconstruction of the irradiated and tissue de cient patient J Oral Maxillofac Surg 1982 40 412 20 58 Mainous EG Boyne PJ Hyperbaric oxygen in total rehabilitation of patients with mandibular osteoradionecrosis Int J Oral Surg 1974 3 297 301 59 Hart GB Mainous EG The treatment of radiation necrosis with hyperbaric oxygen OHP Cancer 1976 37 2580 5 60 Demello FJ Haglin JJ Hitchcock CR Comparative study of experimental Clostridium perfringens infection in dogs treated with antibiotics surgery and hyperbaric oxygen Surgery 1973 73 936 41 61 Heimbach RD Gas gangrene In Kindwall EP ed Hyperbaric medicine practice Flagstaff Ariz Best 1994 373 94 62 Gozal D Ziser A Shupak A Ariel A Melamed Y Necrotizing fasciitis Arch Surg 1986 121 233 5 63 Riseman JA Zamboni WA Curtis A Graham DR Konrad HR Ross DS Hyperbaric oxygen therapy for necrotizing fasciitis reduces mortality and the need for debridements Surgery 1990 108 847 50 64 Tehrani MA Ledingham IM Necrotizing fasciitis Postgrad Med J 1977 53 237 42 65 Brown DR Davis NL Lepawsky M Cunningham J Kortbeek J A multicenter review of the treatment of major truncal necrotizing infections with and without hyperbaric oxygen therapy Am J Surg 1994 167 485 9 66 Mader JT Guckian JC Glass DL Reinarz JA Therapy with hyperbaric oxygen for experimental osteomyelitis due to Staphylococcus aureus in rabbits J Infect Dis 1978 138 312 8 June 20 1996 67 Davis JC Heckman JD DeLee JC Buckwold FJ Chronic non hematogenous osteomyelitis treated with adjuvant hyperbaric oxygen J Bone Joint Surg Am 1986 68 1210 7 68 Esterhai JL Jr Pisarello J Brighton CT Heppenstall RB Gellman H Goldstein G Adjunctive hyperbaric oxygen therapy in the treatment of chronic refractory osteomyelitis J Trauma 1987 27 763 8 69 Strauss MB Hargens AR Gershuni DH et al Reduction of skeletal muscle necrosis using intermittent hyperbaric oxygen in a model compartment syndrome J Bone Joint Surg Am 1983 65 656 62 70 Skyhar MJ Hargens AR Strauss MB Gershuni DH Hart GB Akeson WH Hyperbaric oxygen reduces edema and necrosis of skeletal muscle in compartment syndromes associated with hemorrhagic hypotension J Bone Joint Surg Am 1986 68 1218 24 71 Haapaniemi T Nylander G Sirsjo A Larsson J Hyperbaric oxygen reduces ischemia induced skeletal muscle injury Plast Reconstr Surg 1996 97 6027 72 Strauss MB Crush injury and other acute traumatic peripheral ischemias In Kindwall EP ed Hyperbaric medicine practice Flagstaff Ariz Best 1994 525 49 73 Shulman AG Krohn HL In uence of hyperbaric oxygen and multiple skin allografts on the healing of skin wounds Surgery 1967 62 1051 8 74 Jurell G Kaijser L The in uence of varying pressure and duration of treatment with hyperbaric oxygen on the survival of skin aps an experimental study Scand J Plast Reconstr Surg 1973 7 25 8 75 Bowersox JC Strauss MB Hart GB Clinical experience with hyperbaric oxygen therapy in the salvage of ischemic skin aps and grafts J Hyperb Med 1986 1 141 9 76 Hart GB HBO and exceptional blood loss anemia In Kindwall EP ed Hyperbaric medicine practice Flagstaff Ariz Best 1994 517 24 77 Cianci P Lueders H Lee H et al Adjunctive hyperbaric oxygen reduces the need for surgery in 40 80 burns J Hyperb Med 1988 3 97 101 78 Nylander G Nordstrom H Eriksson E Effects of hyperbaric oxygen on oedema formation after a scald burn Burns 1984 10 193 6 79 Niu AKC Yang C Lee HC Chen SH Chang LP Burns treated with adjunctive hyperbaric oxygen therapy a comparative study in humans J Hyperb Med 1987 2 75 85 80 Oriani G Meazza D Favales F Pizzi GL Aldeghi A Faglia E Hyperbaric oxygen therapy in diabetic gangrene J Hyperb Med 1990 5 171 5 81 Harward TRS Volny J Golbranson F Bernstein EF Fronek A Oxygen inhalation induced transcutaneous PO2 changes as a predictor of amputation level J Vasc Surg 1985 2 220 7 82 Pecoraro RE Ahroni JH Boyko EJ Stensel VL Chronology and determinants of tissue repair in diabetic lower extremity ulcers Diabetes 1991 40 1305 13 83 Wattel F Mathieu D Coget J M Billard V Hyperbaric oxygen therapy in chronic vascular wound management Angiology 1990 41 59 65 84 Roth RN Weiss LD Hyperbaric oxygen and wound healing Clin Dermatol 1994 12 141 56 85 Palmquist B M Philipson B Barr P O Nuclear cataract and myopia during hyperbaric oxygen therapy Br J Ophthalmol 1984 68 113 7 86 Clark JM Lambertsen CJ Pulmonary oxygen toxicity a review Pharmacol Rev 1971 23 37 133 87 Kindwall EP Hyperbaric oxygen s effect on radiation necrosis Clin Plast Surg 1993 20 473 83 88 Gabb G Robin ED Hyperbaric oxygen a therapy in search of diseases Chest 1987 92 1074 82 89 Hyperbaric oxygen therapy a committee report Rev ed Bethesda Md Undersea and Hyperbaric Medical Society 1992 Downloaded from www nejm org by ROBERT WARRINER on July 31 2004 Copyright 1996 Massachusetts Medical Society All rights reserved
biomolecules Review The Hyperoxic Hypoxic Paradox Amir Hadanny 1 2 3 and Shai Efrati 1 2 4 1 2 3 4 The Sagol Center for Hyperbaric Medicine and Research Shamir Assaf Harofeh Medical Center Zerifin 70300 Israel efratishai outlook com Sackler School of Medicine Tel Aviv University Tel Aviv 6997801 Israel The Mina and Everard Goodman Faculty of Life Sciences Bar Ilan University Ramat Gan 5290002 Israel The Sagol School of Neuroscience Tel Aviv University Tel Aviv 6997801 Israel Correspondence amir had gmail com Tel 972 544707381 Fax 972 8 9779748 Received 27 May 2020 Accepted 22 June 2020 Published 25 June 2020 Abstract Effective metabolism is highly dependent on a narrow therapeutic range of oxygen Accordingly low levels of oxygen or hypoxia are one of the most powerful inducers of gene expression metabolic changes and regenerative processes including angiogenesis and stimulation of stem cell proliferation migration and differentiation The sensing of decreased oxygen levels hypoxia or increased oxygen levels hyperoxia occurs through specialized chemoreceptor cells and metabolic changes at the cellular level which regulate the response Interestingly fluctuations in the free oxygen concentration rather than the absolute level of oxygen can be interpreted at the cellular level as a lack of oxygen Thus repeated intermittent hyperoxia can induce many of the mediators and cellular mechanisms that are usually induced during hypoxia This is called the hyperoxic hypoxic paradox HHP This article reviews oxygen physiology the main cellular processes triggered by hypoxia and the cascade of events triggered by the HHP Keywords hyperoxia hypoxia hyperbaric oxygen biogenesis hyperoxic hypoxic paradox hypoxia inducible factor HIF 1 Introduction Oxygen is the third most abundant element in the universe after hydrogen and helium and it is the most dominant effector of most living creatures on earth About 300 million years ago during the Carboniferous period atmospheric oxygen levels reached a maximum of 35 which may have contributed to the large size of animals and insects at this time 1 2 Today oxygen constitutes 20 8 of the earth s atmosphere and any slight change in its concertation will have a dramatic impact on all levels of mammalian physiology The ability to maintain oxygen homeostasis is essential for survival and all mammalian physiological systems evolved to ensure the optimal level of oxygen supplied to all cells in each organism This has transpired through the evolution of a complex physiological infrastructure for oxygen delivery the lungs oxygen transport carriers erythrocytes and plasma oxygen transport pathways vascular system and the pump heart Both the development and regulation of these systems in organisms provide the basis for oxygen homeostasis Effective metabolism is highly dependent on a narrow therapeutic range of oxygen Accordingly low levels of oxygen or hypoxia are one of the most powerful inducers of gene expression metabolic changes and regenerative processes including angiogenesis and stimulation of stem cell proliferation migration and differentiation The sensing of decreased oxygen hypoxia levels or increased hyperoxia oxygen levels occurs through specialized chemoreceptor cells and metabolic changes at the cellular level which regulate the response Interestingly in the cellular milieu fluctuations in free oxygen concentrations rather than the absolute level of oxygen can be interpreted as a lack of oxygen Thus intermittent increases in oxygen concentration can induce many of the mediators and cellular Biomolecules 2020 10 958 doi 10 3390 biom10060958 www mdpi com journal biomolecules
Biomolecules 2020 10 958 2 of 17 Biomolecules 2020 10 x 2 of 17 mechanisms that are usually induced during hypoxia This is the so called hyperoxic hypoxic paradox of the mediators and cellular mechanisms that are usually induced during hypoxia This is the so HHP called hyperoxic hypoxic paradox HHP In this article we review oxygen physiology the main cellular processes triggered by hypoxia In this article we review oxygen physiology the main cellular processes triggered by hypoxia and the cascade of events triggered by the HHP and the cascade of events triggered by the HHP 2 Oxygen Homeostasis 2 Oxygen Homeostasis All of our body s tissues rely on a continuous oxygen supply at a rate that matches the changing All of our body s tissues rely on a continuous oxygen supply at a rate that matches the changing metabolic Theoxygen oxygendelivery deliverychain chain begins lungs with destination being metabolic demands demands The begins at at thethe lungs with thethe destination being the the mitochondria Oxygenisisdelivered deliveredbybyconvection convection airways blood vessels It then mitochondria Figure Figure 1 1 Oxygen inin thethe airways andand blood vessels It then diffuses across the alveolar capillary membrane and through the capillary wall to the interstitium diffuses across the alveolar capillary membrane and through the capillary wall to the interstitium and destination the themitochondria mitochondria In the blood oxygen is carried two forms a andto to its its destination In the blood oxygen is carried in two in forms a fraction fraction that that is bound to hemoglobin a free fraction dissolved in theThe plasma The dissolved is bound to hemoglobin and a and free fraction dissolved in the plasma amount of amount dissolvedofoxygen oxygen is proportional to thepartial oxygen partial at pressure at temperature a specific temperature according to Henry s is proportional to the oxygen pressure a specific according to Henry s law 3 law 3 At physiologic normoxic conditions i e atcontent normalofcontent ofoxygen inspired oxygen 20 8 At physiologic normoxic conditions i e at normal inspired 20 8 most up tomost 99 of theofoxygen is carried by hemoglobin and the quantity of oxygen is small 4 4 up to 99 the oxygen is carried by hemoglobin anddissolved the dissolved quantity of oxygen is small Therefore the the amount amount of affect thethe total capacity of oxygen delivery Therefore of red redblood bloodcells cellswill willdominantly dominantly affect total capacity of oxygen delivery However at at an an elevated elevated partial asas breathing pure oxygen andand during a a However partial pressure pressureofofoxygen oxygen such such breathing pure oxygen during hyperbaric exposure the dissolved amount can become significant In all cases the diffusion hyperbaric exposure the dissolved amount can become significant In all cases the diffusion gradients gradients aredriving oxygen s driving from the plasma to the mitochondria Thus the free dissolved are oxygen s force from force the plasma to the mitochondria Thus the free dissolved fraction has a fraction has a dominant effect on the mitochondria It is assumed that oxygen freely diffuses across dominant effect on the mitochondria It is assumed that oxygen freely diffuses across cell membranes cell membranes However recent data indicate that water channels such as aquaporin 1 AQP 1 However recent data indicate that water channels such as aquaporin 1 AQP 1 also work as oxygen also work as oxygen transporters 5 transporters 5 Figure 1 Oxygen delivery chain Figure 1 Oxygen delivery chain At the normal steady state oxygen homeostasis is a dynamically regulated process The physiological cellular demand for oxygen can vary depending on tissue requirements at a
Biomolecules 2020 10 958 3 of 17 given moment For example an exercising muscle has significantly higher oxygen demand than a relaxed muscle Consequently the oxygen delivery rate to tissues is continuously adjusted Several mechanisms enable the human body to maintain an adequate oxygen supply 6 The systemic sensing and response to hypoxia include a carotid body glomus a chemosensor in the arterial circulation that can increase the ventilation rate b and the neuroepithelial bodies NEBs which are clusters of cells exposed to the airway lumen at branching points innervated by the Vagus nerve which dilate the pulmonary arteries to optimize the ventilation perfusion exchange The adrenergic system is activated during hypoxia increasing cardiac output and selective blood perfusion to the more crucial organs At the organ level arteries dilate in response to hypoxia to increase oxygen delivery Oxygenation levels are also sensed by the kidneys which regulate erythropoietin production to adjust the number of red blood cells RBC and oxygen carrying capacity In addition to the dynamic respiratory and metabolic systems allowing increased oxygen delivery as outlined above it is necessary to have regulating mechanisms at the cellular level These are essential for survival at extreme environmental conditions and pathological disease states where systemic regulation is insufficient At the cellular level 80 of the available oxygen is used by the mitochondria while only 20 is used by other organelles Being the major oxygen consumer and metabolizer the partial pressure in the mitochondria is very low only 1 3 mmHg Figure 1 Mitochondria are therefore the key oxygen sensor as well as important signaling organelles 7 Most evidence so far points to the following theory mitochondria signal the onset of hypoxia by generating reactive oxygen species ROS signals by the electron transport chain When ROS are released to the intermembrane space they interplay with the activation of enzymes transcription factors and post translation responses 8 In addition several cells can adapt to reduced oxygen levels by unique mechanisms 6 For example the hemoglobin in red blood cells can change its form and affinity under hypoxic conditions 4 Cytochrome P 450 monooxygenases CYP include a vast number of homologous oxygen sensitive proteins that oxidize a wide range of compounds Numerous reports have suggested that CYP metabolites contribute to the hypoxia response in the systemic microvasculature and endothelium and may contribute to hypoxic pulmonary vasoconstriction 6 9 10 3 Hypoxia Induced Cellular Cascade As detailed above effective metabolism is highly dependent on a narrow therapeutic window of oxygen However while the arterial oxygen partial pressure in adult mammals is 100 mmHg in the mammalian fetus it is around 40 mmHg Thus hypoxia is a relative term and is most usefully defined as a condition in which failure of either delivery or utilization of oxygen limits normal function 3 1 Hypoxic Inducible Factor A low level of oxygen is signaled by all living cells which starts with a class of enzymes called prolyl hydroxylase domain PHD proteins 11 12 Figure 2 Under normal oxygen concentrations these PHD enzymes include oxygen sensing hydroxylases which hydroxylate specific proline and asparagine residues on the subunit of the transcription factor hypoxia inducible factor HIF Following hydroxylation the HIF 1 subunit is targeted by the E3 ubiquitin ligase also known as the von Hippel Lindau protein VHLp which induces HIF 1 ubiquitination and degradation Factor inhibiting HIF FIH is an additional hydroxylase which hydroxylates an asparagine residue on the subunit of HIF deactivating the HIF transcription factor HIF is a heterodimer composed of HIF 1 HIF 2 or HIF 3 subunits which dimerize with HIF 1 HIF 2 and HIF 3 subunits respectfully forming HIF 1 HIF 2 and HIF 3 factors HIF 1 is produced in all cell types while the HIF 2 subunit is found in specific cells including myeloid cells liver parenchyma vascular endothelia type II pneumocytes and renal interstitium While HIF 1 and HIF 2 function as lead regulators of the transcriptional response to hypoxia the HIF 3 function is yet to be known Although the HIF1A gene
Biomolecules 2020 10 958 4 of 17 is constitutively expressed at low levels under normoxic conditions it is significantly upregulated in response to hypoxia 13 HIF 1 when stabilized by hypoxic conditions without hydroxylases repression Figure 2 serves as a transcription factor that regulates over 100 genes essential for survival in oxygen deprived conditions 14 These include glycolysis enzymes which allow adenosine triphosphate ATP synthesis in an oxygen independent manner enzymes decreasing the basal respiratory rate and upregulating the vascular endothelial growth factor VEGF to induce angiogenesis which improves tissue perfusion Unlike HIF 1 HIF 2 regulates iNOS inducible NO synthase and other factors that support increases in tissue oxygenation in adults such as erythropoietin production 15 In addition to modulating cellular metabolism needs for survival in a hypoxic environment HIF 1 can either turn on or off key mammalian regeneration processes 16 18 In controlled mammalian models it was demonstrated that continuous downregulation of HIF 1 results in a scarring response and loss of tissue 16 HIF 1 also has an important role in the regeneration and maintenance of essential organ functions that are highly oxygen dependent such as the brain and the heart Research conducted on mice demonstrated that increased HIF expression is neuroprotective and enhances regenerative effects that can enhance hippocampal memory and induce better neuroregeneration in post stroke and spinal cord injuries 17 19 20 With regard to the heart increased HIF expression initiates the metabolic processes needed to regenerate the damaged myocardium and improve cardiac functions after various types of injuries 18 21 Biomolecules 2020 10 x 5 of 17 Figure 2 The intracellular cascade HIF 1 alpha Legend is composed a heterodimer composed of Figure 2 The intracellular of cascade of HIF 1 alpha Legend HIF 1 is aHIF 1 heterodimer of cytoplasmatic HIF 1 and the nuclear HIF 1 subunits a Under normal oxygen environments the cytoplasmatic HIF 1 and the nuclear HIF 1 subunits a Under normal oxygen environments ratio of ROS scavenger is high and the free ROS molecules initiate HIF 1 hydroxylation HIF 1 subunits become a target for VHLp von Hippel Lindau protein protein which facilitates HIF 1 the ratio of ROS scavenger is high and the free ROS molecules initiate HIF 1 hydroxylation HIF 1 subunits ubiquitination and degradation b Under hypoxic conditions less oxygen and ROS
Biomolecules 2020 10 958 5 of 17 subunits become a target for VHLp von Hippel Lindau protein protein which facilitates HIF 1 subunits ubiquitination and degradation b Under hypoxic conditions less oxygen and ROS molecules are available HIF 1 subunits are not hydrolyzed and more HIF 1 subunits penetrate the nucleus to conjugate with HIF 1 subunits and generate the active HIF transcription factor c At the hyperoxic environment more ROS and oxygen are available thus more HIF 1 subunits are hydrolyzed and degraded d The adaptive response to repeated hyperoxia includes increases in the production of scavengers that adjust to the increased ROS generation Thus the ROS scavenger ratio gradually becomes similar to the ratio under normal oxygen environment prior to initiating repeated hyperoxic exposures e Upon return to normoxia following repeated hyperoxic exposures the ratio of ROS scavenger is low due to the fact scavengers elimination half life T1 2 is significantly longer than the T1 2 of ROS Accordingly less HIF 1 subunits are hydroxylated and more of them penetrate the nucleus conjugate with HIF 1 to generate the active HIF similar to the hypoxic state 3 2 Vascular Endothelial Growth Factor VEGF The VEGF family comprises five members VEGF A placenta growth factor PGF VEGF B VEGF C and VEGF D VEGF A is the most known factor out of the VEGF family All VEGF factors induce different cellular responses by binding to their respective tyrosine kinase receptors located on the cell surface inducing the receptors dimerization phosphorylation and activation 22 VEGF A production is induced by HIF 1 which in turn activates vascular cells to initiate angiogenesis the budding of new capillaries from existing vessels and arteriogenesis the remodeling of collateral blood vessels to handle the increased flow bypassing stenotic regions of the original conduit arteries 11 23 In addition the VEGF A factor induces vasodilatation activity as well as microvascular permeability increase needed for immediate improvement of tissue ischemia 11 VEGF A also stimulates the mobilization of bone marrow derived angiogenic cells BMDACs which in turn migrate to ischemic tissues and participate in angiogenesis and arteriogenesis 11 3 3 Sirtuin Sirtuins are a family of signaling proteins involved in metabolic regulation Sirtuins activities include mono adenosine diphosphate ADP ribosyltransferase or deacylase 24 25 In mammals seven sirtuins SIRT 1 7 have been discovered in different subcellular compartments SIRT1 SIRT6 and SIRT7 located in the nucleus SIRT2 in the cytoplasm and SIRT3 SIRT4 and SIRT5 in the mitochondria 24 25 SIRT1 is involved in various mechanisms regulating apoptosis inflammation and senescence which are associated with aging related diseases 14 26 29 Reductions in the nuclear energy state and nicotinamide adenine dinucleotide NAD levels decrease the SIRT1 activity which results in diminished pVHL levels and the stabilization of HIF 1 Conversely overexpression of SIRT1 promotes mitochondrial biogenesis by deacetylation resulting in the activation of HIF 1 30 The decreased level of SIRT1 in both transcriptional and posttranscriptional stages during aging is considered to be a major metabolic pathway that attenuates mitochondrial biogenesis and causes aging related diseases 14 In mice models overexpression of SIRT1 results in delayed aging phenotypes and lifespan extension whereas inhibition of SIRT1 annuls the lifespan extension 31 Overexpression of SIRT1 or SIRT6 is protective in many murine disease models including cancer type 2 diabetes and cardiovascular disease 26 28 32 35 The crosstalk between oxygen and redox responsive signal transducers occurs through the SIRT1 HIF interaction 36 37 During hypoxia the reduced NADH consumption in mitochondria and increased NADH production from glycolysis causes a reduction of the NAD NADH ratio downregulating SIRT1 transcription Reduced SIRT1 allows the acetylation of HIF 1 and its activation and provides a positive feedback loop that maintains high levels of HIF 1 activity during hypoxia Due to the metabolic crisis in hypoxia HIF 1 blocks mitochondrial energy metabolism by 1 inducing PDK 1 which inhibits the conversion of pyruvate to acetyl CoA by 2 inhibiting mitochondrial biogenesis via c Myc repression and by 3 reducing mitochondrial transcription factor A TFAM required for replication transcription and maintenance of mitochondrial biogenesis 38 39
Biomolecules 2020 10 958 6 of 17 3 4 Mitochondria Biogenesis Maintaining an adequate mitochondrial population during one s lifetime is crucial Mitochondrial quality control occurs via the process of mitophagy degradation of damaged mitochondria and generation of newly functioning mitochondria by mitochondrial biogenesis a process in which new mitochondria are formed by growth and division of preexisting mitochondria Mitochondrial biogenesis is crucial for preserving most human cell integrity and in recent years there is growing evidence about their important role in preserving brain functionality and in neurodegenerative diseases 40 Mitochondrial biogenesis is a complex process requiring coordinated bi genomic cellular and mitochondrial DNAs regulation to execute several distinct processes including 1 inner and outer mitochondrial membrane synthesis 2 synthesis of mitochondrial encoded proteins 3 synthesis and import of nuclear encoded mitochondrial proteins and 4 replication of mitochondrial DNA mtDNA Several cell signaling pathways tightly regulate mitochondrial biogenesis The AMP activated kinase AMPK PGC 1a axis and Sirtuin 1 SIRT1 PGC 1a are two major pathways that regulate mitochondrial biogenesis AMPK can be activated by physiological stimuli such as exercise starvation and transient hypoxia 41 44 There is considerable overlap between the AMPK and HIF signaling pathways as both are involved in energetic stresses though the relationship is complex with both opposing and cooperative outcomes depending on the context 45 As mentioned AMPK is a potent stimulator of mitochondrial biogenesis which in normoxic conditions acts to restore ATP homeostasis However as detailed above once AMPK activation occurs under hypoxic conditions i e energetic stress additional mitochondrial biogenesis and oxygen consumption would further decrease oxygen availability and worsen the stress Therefore HIF signaling under prolonged hypoxia generally acts to decrease mitochondrial biogenesis and mass 45 3 5 Stem Cells Stem cells SC are undifferentiated or partially differentiated cells that can differentiate into various types of cells and divide indefinitely to produce more of the same stem cell In mammals the major groups of stem cells include hematopoietic stem cells HSC which replenish blood and immune cells basal cells which maintain the skin epithelium and mesenchymal stem cells MSC which maintain bone cartilage muscle and fat cells There are also more targeted subgroups of SCs that include neuronal stem cells NSC that persist in restricted regions in the adult brain and continue to produce neurons throughout the person s life NSCs can generate nerve cells and their supporting cells oligodendrocytes and astrocytes 46 In addition to their differentiation capacity SCs have multipotent properties that include anti inflammatory effects that make them potential therapeutic candidates for a variety of disorders 47 During normal conditions SCs are at a reversible state of quiescence i e at a temporary cell cycle arrest 48 While being quiescent they exhibit improved stress resistance and enhanced survival ability Oxygen has an important role in the regulation of stem cell proliferation and differentiation 48 50 Short term hypoxia can induce SC proliferation migration and differentiation capacity 48 50 In addition hypoxia also modulates the paracrine activity of MSCs causing upregulation of various secreted factors such as VEGF and exosomes that also have important angiogenesis and anti inflammatory effects 50 52 The mechanisms by which hypoxia exerts its effect on cells is mainly regulated by HIF 1 and related down cascade protein expression 48 50 4 The Hyperoxic Hypoxic Paradox As detailed above hypoxia is the natural trigger for mitochondria metabolic changes via elevated levels of HIF VEGF Sirtuin mitochondria metabolic changes and SC proliferation and migration However the understanding that at the cellular level oxygen level fluctuations can trigger a cellular cascade that is usually triggered by hypoxia allows the use of intermittent hyperoxia to stimulate
Biomolecules 2020 10 958 Biomolecules 2020 10 x 7 of 17 8 of 17 tissue regeneration without thewithout hazardous of hypoxia Thisofis hypoxia termed the hyperoxic hypoxic stimulate tissue regeneration theeffects hazardous effects This is termed the paradox Figure 3 hyperoxic hypoxic paradox Figure 3 clinicalpractice practice intermittent intermittenthyperoxia hyperoxiacan canbe begenerated generatedusing usinghyperbaric hyperbaricoxygen oxygentherapy therapy InInclinical HBOT HBOT includes inhaling 100 oxygen at pressures exceeding 1 atmosphere absolute ATA HBOT HBOT includes inhaling 100 oxygen at pressures exceeding 1 atmosphere absolute ATA to enhance the amount of oxygen dissolved in the body tissues During HBOT the arterial O2 to enhance the amount of oxygen dissolved in the body tissues During HBOT the arterial O2 tension tension typically exceeds 1500and mmHg levels of 200 400 mmHg occurIn inatissues a normal typically exceeds 1500 mmHg levelsand of 200 400 mmHg occur in tissues normal In individual individual at a normal environment 20 8 oxygen at 1ATA the hemoglobin is almost entirely at a normal environment 20 8 oxygen at 1ATA the hemoglobin is almost entirely saturated 94 saturated 94 99 when Accordingly when inenvironment a hyperbaric environment the in effect only in the dissolved 99 Accordingly in a hyperbaric the effect is only the is dissolved oxygen As oxygen As mentioned above the dissolved oxygen is the fraction responsible for the diffusion gradient mentioned above the dissolved oxygen is the fraction responsible for the diffusion gradient from the from the capillaries to the mitochondria In the following of the we will thecascade cellular capillaries to the mitochondria In the following part of thepart article wearticle will review thereview cellular cascade following induced following hyperoxia induced repeated repeated transient transient hyperoxia Figure 3 The major cellular response cascade initiated by hypoxia and by intermittent hyperoxia Legends HIF Hypoxic induce factor VEGF Vascular endothelial growth factor SIRT Sirtuin Figure 3 The major cellular response cascade initiated by hypoxia and by intermittent hyperoxia HIF Hypoxic induce factor VEGF Vascular endothelial growth factor SIRT Sirtuin 4 1 Legends Hypoxia Inducible Factor It has been proposed 4 1 Hypoxia Inducible Factorthat the relative changes in oxygen availability rather than constant hypoxia or hyperoxia have a more dominant effect on HIF expression 53 55 According to this hypothesis It hasinterpret been proposed that the normoxia relative changes in oxygen availability rather than following constant the cells the change from to hypoxia or the change back to normoxia hypoxia or hyperoxia have a more dominant effect on HIF expression 53 55 According this a hyperoxic exposure as an oxygen shortage and induce HIF 1 regulated gene synthesis to 53 55 hypothesis thethere cellsisinterpret theunderstanding change from normoxia to hypoxia orresponsible the change for back to normoxia Even though a growing of the cellular cascade HIF expression following a hyperoxic exposure as an oxygen shortage and induce HIF 1 regulated gene as detailed below the precise level of inspired oxygen and the exact timeframe for itssynthesis iterative 53 55 Even though there is known a growing administrations are not fully yet understanding of the cellular cascade responsible for HIF expression as detailed below the level of availability inspired oxygen and theafter exacthyperoxic timeframe for its The proposed mechanisms forprecise increased HIF at normoxia exposure iterative administrations are not fully known yet relates to ROS availability and scavengers such as the glutathione synthase and superoxide dismutase Theenzymes proposed 53 55 mechanisms for increased availability at normoxia after hyperoxic exposure SOD As detailed above HIF Figure 2 at normoxic conditions when oxygen and relates to ROS availability and scavengers such as the glutathione synthase and superoxide its ROS derivates are available at higher ratios compared to their scavengers most of the HIF 1 dismutase SOD enzymes 53 55 AsThis detailed above Figure 2 at normoxic conditions oxygen subunits are hydroxylated by PHD results in their ubiquitination by VHLp andwhen consequently and its ROS derivates are available at higher ratios compared to their scavengers most of the HIF 1 subunits are hydroxylated by PHD This results in their ubiquitination by VHLp and consequently degradation of HIF 1 in the proteasome In hypoxia oxygen and its ROS derivates are less available
Biomolecules 2020 10 958 8 of 17 degradation of HIF 1 in the proteasome In hypoxia oxygen and its ROS derivates are less available the HIF 1 is not hydroxylated and ubiquitinated by VHLp and more HIF 1 is available to enter the nucleus and is dimerized with HIF 1 to form the active HIF promotor During hyperoxia increased levels of oxygen availability will enhance the production ROS and the production of ROS scavengers including glutathione peroxidase SOD as well as other ROS scavengers 56 60 Based on the above cumulative data our perspective is that this scavenger level increase is limited and gradual following a single hyperoxic exposure and repeated exposures are required in order to obtain significant scavenging activity Figure 2 After returning to normoxia from a single hyperoxic exposure the ROS scavenging capacity ratio will be high leading to ubiquitination of all HIF molecules Upon return to normoxia following repeated hyperoxic exposures the level of scavengers is increased along with their inherent elimination half life T1 2 which is significantly longer than ROS T1 2 Thus the ratio of ROS scavenging capacity will be low similar to the hypoxic state With enhanced scavenging capacity less ROS is available to bind PHD less degradation of HIF subunits which in turn will enter the nucleus to bind to HIF 1 and generate the active HIF gene promotor Meaning intermittent hyperoxia generates a hypoxia mimicking state without hypoxia by decreasing the ratio of ROS scavenging capacity The effect of repeated intermittent hyperoxia by HBOT on HIF expression was demonstrated in different types of organs and cells 57 58 61 62 For example HBOT can induce HIF expression and its related regenerative cascade in the injured brain 58 63 gastrointestinal tract 57 and liver 61 62 In addition HBOT induces the expression of different types of HIF and in different types of stem cells 59 64 The dose response curve related to the applied pressure time and number of HBOT exposures and its relation to HIF expression is still not fully understood and further studies are needed to find the optimal HBOT protocols It should be noted that when HBOT is administrated to an ischemic tissue which overexpresses HIF tissue hypoxia is being reversed and corrected accordingly the overexpressed HIF is reduced towards the normalized baseline 65 70 Moreover when HBOT is being used as preconditioning therapy for hypoxia by HIF induction the tissue will tolerate the ischemic insult better less ischemic injury induced and the overall post insult HIF expression will be lower than expected for the same insult 71 72 4 2 VEGF and Angiogenesis VEGF production is induced by HIF 1 and then goes on to stimulate the cellular processes needed for both angiogenesis and arteriogenesis as detailed above VEGF is significantly increased following intermittent hyperoxic exposures utilizing the HHP There is growing evidence from preclinical as well as from clinical studies demonstrating that repeated HBOT sessions induce the crucial elements for angiogenesis VEGF expression and endothelial progenitor cells EPCs 61 73 75 Unlike VEGF induced under ischemic conditions VEGF induction under hyperoxic stimuli can facilitate angiogenesis in tissues that are hypoxic ischemic while breathing normal air Clinical studies have confirmed that repeated daily HBOT sessions augment the circulating levels of VEGF EPCs and improve the blood flow in ischemic areas of patients with chronic peripheral arterial occlusive diseases with or without non healing wounds 73 76 The use of hyperoxic stimuli to induce angiogenesis is crucial for organs that are oxygen deprived even at normal conditions such as the human brain 77 78 Therefore to enable brain angiogenesis and regenerative processes it is essential to increase oxygen delivery in addition to VEGF induction which is achieved by cyclic hyperoxic exposure HBOT can initiate the cellular and vascular repair mechanisms to induce brain angiogenesis and improve cerebral blood flow in damaged brain regions 79 81 4 3 Sirtuin SIRT1 acts as a metabolic sensor by its ability to deacetylate the mitochondrial biogenesis factor PGC 1 During hyperoxia the NAD NADH ratio is increased through the Krebs cycle and mitochondrial metabolism triggering SIRT1 82 83 SIRT1 is known to deacetylate FOXO3a which
Biomolecules 2020 10 958 9 of 17 induces antioxidant responses via modulating SOD2 and CAT FOXO3a has further been shown to regulate mitochondrial gene expression resulting in modulated ROS levels 82 SIRT1 regulates the acetylation of PGC 1 a master regulator of mitochondrial biogenesis 83 SIRT1 along with other sirtulins appears to be an integral part of an important cellular defense mechanism against oxidative stress and ROS formation Intermittent hyperoxic exposures can produce ROS molecules that increase the activity of SIRT 1 inside cells through the activation of mitogen activated protein kinase MAPK 84 The effect of intermittent hyperoxic exposure was evaluated in several animal models Yan et al evaluated the effect of HBOT on SIRT1 in a model of focal cerebral ischemia induced by middle cerebral artery occlusion and also on primary cultured cortical neurons subjected to oxygen glucose deprivation injury 84 85 Their findings indicate that HBOT s neuroprotective effect is mediated by increased SIRT1 mRNA and protein expression HBOT s neuroprotection was attenuated by a SIRT1 inhibitor and also in SIRT1 knockdown rats 84 In another study done in hyperglycemic rats after middle cerebral artery occlusion HBOT induced activation of ATP NAD and SIRT1 and SIRT2 pathways resulting in attenuation of hemorrhagic transformation brain infarction as well as neurological function improvement 86 Similar results indicating that the neuroprotective effects of HBOT are mediated by SIRT1 were demonstrated in middle aged mice with postoperative cognitive dysfunction 87 4 4 Mitochondria Any change in the free dissolved oxygen generates a diffusion gradient that directly affects the oxygen delivered and sensed by the mitochondria through the production of ROS signaling molecules Therefore intermittent increases in dissolved oxygen generated by HBOT can be compared to intense interval training with an expected cumulative effect along with repeated exposures In a well designed mice model study it was demonstrated that adding intermittent hyperbaric exposure to exercise training further improves endurance performance by facilitating oxidative and glycolytic capacities and by increasing the expression of proteins involved in mitochondrial biogenesis in striated muscles 88 In humans combining HBOT to an exercise training regimen induces better cardiorespiratory fitness compared to exercise training alone 89 Regarding the brain ROS are considered to have significant metabolic effects and the main source of ROS in the brain is the mitochondria 90 Normally 1 2 of the oxygen consumed by the mitochondria is converted to O2 1 and related ROS metabolites such as hydrogen peroxide H2 O2 and peroxynitrite ONOO 91 O2 1 and related ROS formations increase in proportion to the partial pressure of oxygen and in high pressure multiplied by the exposure duration Exposure may induce high neurological activity presented in the form of epileptic seizures 90 In a study done by Gutsaeva et al it was demonstrated that pre convulsive dosages of HBOT induce significant mitochondrial biogenesis in the hippocampus 91 The cellular response in the hippocampus was mediated by increased NRF 2 gene expression TFAM gene expression and mitochondrial gene transcription 91 In recent years there is growing evidence about the possibility and the importance of mitochondrial transfer between astrocytes and neurons for proper maintenance of neuronal function and as cell cell signaling 92 93 Neurons can release and transfer damaged mitochondria to astrocytes for disposal and recycling 92 and astrocytes can release functional mitochondria that enter into neurons 93 In a study done by Borlongan and Lippert it was demonstrated that HBOT could facilitate the transfer of resilient mitochondria from astrocytes to neuronal cells that are more susceptible to inflammation 94 The mitochondrial transfer from astrocytes to neurons makes the neurons more resilient to inflammatory insults These findings suggest a new mitochondrial mechanism of neuroglial crosstalk that may contribute to endogenous neuro protective and neuro recovery mechanisms induced by HBOT 4 5 Stem Cells Both hypoxia and intermittent hyperoxia increase HIF and its downstream gene expression including stem cell factors SCFs 95 Growing data from preclinical and clinical studies demonstrate
Biomolecules 2020 10 958 10 of 17 the cumulative effect of repeated intermittent hyperoxia by HBOT on proliferation and mobilization of stem cells 59 96 112 Clinical studies on patients suffering from diabetic wounds and post traumatic brain injury have demonstrated that repeated HBOT sessions increase circulating mobilization stem cells in correlation with the clinical improvements 96 98 With regard to subtypes of stem cells it was demonstrated that HBOT promotes neuronal stem cell proliferation 99 105 stimulates vasculogenic stem cell growth and differentiation 59 106 stimulates colonic stem cells and induces mucosal healing 107 improves the osteogenic properties of mesenchymal stem cells 108 109 and increases the myoblast growth rate and enhances muscle regeneration 110 112 The main advantage of stimulating stem cells by intermittent hyperoxia instead of hypoxia is that stem cell proliferation and differentiation similar to any other regenerative process is energy dependent and cannot be accomplished in a hypoxic environment The fact that oxygen is crucial for stem cells related to regenerative effects has been validated in different studies that compared the results of stem cell injections along with or without HBOT The potential added value of using HBOT in addition to stem cell injections was seen in a variety of tissues including brain 113 114 spinal cord and peripheral nerves 115 116 myocardium 117 118 and diabetic wounds 119 In all those studies adding HBOT to stem cell injections had synergistic beneficial effects 4 6 Oxygen Toxicity Although oxygen therapy is considered to be safe like other active ingredients or drugs at high dosage it can be harmful and result in oxygen toxicity Prolonged exposure to high oxygen pressure with a prolonged imbalance between ROS to scavengers can lead to membrane lipid peroxidation and enzyme inhibition and modulations most commonly seen in the central nervous system CNS that lead to alterations in neuronal metabolism and its related electrical activity 120 As was first suggested in 1878 breathing hyperbaric oxygen can culminate in grand mal seizures 121 Another organ that is relatively sensitive to oxygen toxicity is the lung Pulmonary oxygen toxicity can be manifested by chest tightness cough and a reversible decline of pulmonary function 122 Both CNS and pulmonary toxicity depend upon the partial pressure of oxygen and the duration of exposure 123 Accordingly the new HBOT protocol used today includes repeated daily sessions limited to 60 90 min with oxygen partial pressure not exceeding 2 4 ATA as well as air brakes every 20 30 min Using those new protocols HBOT is considered to be safe while both pulmonary and oxygen toxicity are very rare 124 126 In a recent analysis of 62 614 hyperbaric sessions the overall incidence of seizures during hyperbaric sessions was 0 011 1 8 945 sessions 124 125 In addition in patients without chronic lung diseases the currently used HBOT protocols do not cause any pulmonary toxicity or changes in pulmonary functions following 60 repeated exposures 126 5 Summary As in Albert Einstein s theory of relativity that explains the basic physical aspects of our cosmos relatively can also be found in the micro cosmos i e the microenvironmental interpretation at the cellular level As summarized in Figure 3 most of the cellular cascades initiated by hypoxia can be induced by intermittent hyperoxia the so called hyperoxic hypoxic paradox HIF VEGF SIRT mitochondrial biogenesis and stem cell proliferation and migration could all be induced by biological fooling the cells with certain protocols of repeated intermittent hyperoxia Even though the exact dose response curve has yet to be discovered in clinical practice certain HBOT protocols have already demonstrated induction of damaged tissue regeneration Funding The study was funded by a research grant from the Research fund of the Shamir medical center Acknowledgments We would like to thank Mechael Kanovsky for his editing of this manuscript Conflicts of Interest AH works for AVIV Scientific LTD ES is a shareholder in AVIV Scientific LTD Aviv Scientific LTD had no role in the design execution interpretation or writing of the study
Biomolecules 2020 10 958 11 of 17 References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Berner R A Atmospheric oxygen over Phanerozoic time Proc Natl Acad Sci USA 1999 96 10955 10957 CrossRef PubMed Butterfield N J Oxygen animals and oceanic ventilation An alternative view Geobiology 2009 7 1 7 CrossRef PubMed Trayhurn P Oxygen A Critical but Overlooked Nutrient Front Nutr 2019 6 10 CrossRef PubMed Collins J A Rudenski A Gibson J Howard L O Driscoll R Relating oxygen partial pressure saturation and content The haemoglobin oxygen dissociation curve Breathe Sheff 2015 11 194 201 CrossRef Echevarria M Munoz Cabello A M Sanchez Silva R Toledo Aral J J Lopez Barneo J Development of cytosolic hypoxia and hypoxia inducible factor stabilization are facilitated by aquaporin 1 expression J Biol Chem 2007 282 30207 30215 CrossRef Ward J P Oxygen sensors in context Biochim Biophys Acta 2008 1777 1 14 CrossRef Palmeira C M Teodoro J S Amorim J A Steegborn C Sinclair D A Rolo A P Mitohormesis and metabolic health The interplay between ROS cAMP and sirtuins Free Radic Biol Med 2019 141 483 491 CrossRef Waypa G B Smith K A Schumacker P T O2 sensing mitochondria and ROS signaling The fog is lifting Mol Asp Med 2016 47 48 76 89 CrossRef Roman R J P 450 metabolites of arachidonic acid in the control of cardiovascular function Physiol Rev 2002 82 131 185 CrossRef Michaelis U R Fisslthaler B Barbosa Sicard E Falck J R Fleming I Busse R Cytochrome P450 epoxygenases 2C8 and 2C9 are implicated in hypoxia induced endothelial cell migration and angiogenesis J Cell Sci 2005 118 5489 5498 CrossRef Semenza G L Oxygen sensing homeostasis and disease N Engl J Med 2011 365 537 547 CrossRef PubMed Choudhury R Hypoxia and hyperbaric oxygen therapy A review Int J Gen Med 2018 11 431 442 CrossRef PubMed Minet E Ernest I Michel G Roland I Remacle J Raes M Michiels C HIF1A gene transcription is dependent on a core promoter sequence encompassing activating and inhibiting sequences located upstream from the transcription initiation site and cis elements located within the 5 UTR BioChem Biophys Res Commun 1999 261 534 540 CrossRef PubMed Yeo E J Hypoxia and aging Exp Mol Med 2019 51 1 15 CrossRef PubMed Haase V H Hypoxic regulation of erythropoiesis and iron metabolism Am J Physiol Ren Physiol 2010 299 F1 F13 CrossRef Zhang Y Strehin I Bedelbaeva K Gourevitch D Clark L Leferovich J Messersmith P B Heber Katz E Drug induced regeneration in adult mice Sci Transl Med 2015 7 290ra92 CrossRef Adamcio B Sperling S Hagemeyer N Walkinshaw G Ehrenreich H Hypoxia inducible factor stabilization leads to lasting improvement of hippocampal memory in healthy mice Behav Brain Res 2010 208 80 84 CrossRef Schreiber T Salhofer L Quinting T Fandrey J Things get broken The hypoxia inducible factor prolyl hydroxylases in ischemic heart disease Basic Res Cardiol 2019 114 16 CrossRef Xing J Lu J HIF 1alpha Activation Attenuates IL 6 and TNF alpha Pathways in Hippocampus of Rats Following Transient Global Ischemia Cell Physiol BioChem 2016 39 511 520 CrossRef Chen H Li J Liang S Lin B Peng Q Zhao P Cui J Rao Y Effect of hypoxia inducible factor 1 vascular endothelial growth factor signaling pathway on spinal cord injury in rats Exp Ther Med 2017 13 861 866 CrossRef Kido M Du L Sullivan C C Li X Deutsch R Jamieson S W Thistlethwaite P A Hypoxia inducible factor 1 alpha reduces infarction and attenuates progression of cardiac dysfunction after myocardial infarction in the mouse J Am Coll Cardiol 2005 46 2116 2124 CrossRef PubMed Karkkainen M J Petrova T V Vascular endothelial growth factor receptors in the regulation of angiogenesis and lymphangiogenesis Oncogene 2000 19 5598 5605 CrossRef PubMed
Biomolecules 2020 10 958 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 12 of 17 van Weel V van Tongeren R B van Hinsbergh V W van Bockel J H Quax P H Vascular growth in ischemic limbs A review of mechanisms and possible therapeutic stimulation Ann Vasc Surg 2008 22 582 597 CrossRef PubMed Dai H Sinclair D A Ellis J L Steegborn C Sirtuin activators and inhibitors Promises achievements and challenges Pharmacol Ther 2018 188 140 154 CrossRef PubMed Ye X Li M Hou T Gao T Zhu W G Yang Y Sirtuins in glucose and lipid metabolism Oncotarget 2017 8 1845 1859 CrossRef PubMed Poulose N Raju R Sirtuin regulation in aging and injury Biochim Biophys Acta 2015 1852 2442 2455 CrossRef Bai X Yao L Ma X Xu X Small Molecules as SIRT Modulators Mini Rev Med Chem 2018 18 1151 1157 CrossRef Matsushima S Sadoshima J The role of sirtuins in cardiac disease Am J Physiol Heart Circ Physiol 2015 309 H1375 H1389 CrossRef Zhang H N Dai Y Zhang C H Omondi A M Ghosh A Khanra I Chakraborty M Yu X B Liang J Sirtuins family as a target in endothelial cell dysfunction Implications for vascular ageing Biogerontology 2020 CrossRef Gomes A P Price N L Ling A J Moslehi J J Montgomery M K Rajman L White J P Teodoro J S Wrann C D Hubbard B P et al Declining NAD induces a pseudohypoxic state disrupting nuclear mitochondrial communication during aging Cell 2013 155 1624 1638 CrossRef Satoh A Brace C S Rensing N Cliften P Wozniak D F Herzog E D Yamada K A Imai S Sirt1 extends life span and delays aging in mice through the regulation of Nk2 homeobox 1 in the DMH and LH Cell Metab 2013 18 416 430 CrossRef Banks A S Kon N Knight C Matsumoto M Gutierrez Juarez R Rossetti L Gu W Accili D SirT1 gain of function increases energy efficiency and prevents diabetes in mice Cell Metab 2008 8 333 341 CrossRef PubMed Firestein R Blander G Michan S Oberdoerffer P Ogino S Campbell J Bhimavarapu A Luikenhuis S de Cabo R Fuchs C et al The SIRT1 deacetylase suppresses intestinal tumorigenesis and colon cancer growth PLoS ONE 2008 3 e2020 CrossRef PubMed Yamamoto T Sadoshima J Protection of the heart against ischemia reperfusion by silent information regulator 1 Trends Cardiovasc Med 2011 21 27 32 CrossRef PubMed Pfluger P T Herranz D Velasco Miguel S Serrano M Tschop M H Sirt1 protects against high fat diet induced metabolic damage Proc Natl Acad Sci USA 2008 105 9793 9798 CrossRef PubMed Lim J H Lee Y M Chun Y S Chen J Kim J E Park J W Sirtuin 1 modulates cellular responses to hypoxia by deacetylating hypoxia inducible factor 1alpha Mol Cell 2010 38 864 878 CrossRef Chen R Dioum E M Hogg R T Gerard R D Garcia J A Hypoxia increases sirtuin 1 expression in a hypoxia inducible factor dependent manner J Biol Chem 2011 286 13869 13878 CrossRef Kim J W Tchernyshyov I Semenza G L Dang C V HIF 1 mediated expression of pyruvate dehydrogenase kinase A metabolic switch required for cellular adaptation to hypoxia Cell Metab 2006 3 177 185 CrossRef Zhang H Gao P Fukuda R Kumar G Krishnamachary B Zeller K I Dang C V Semenza G L HIF 1 inhibits mitochondrial biogenesis and cellular respiration in VHL deficient renal cell carcinoma by repression of C MYC activity Cancer Cell 2007 11 407 420 CrossRef Uittenbogaard M Chiaramello A Mitochondrial biogenesis A therapeutic target for neurodevelopmental disorders and neurodegenerative diseases Curr Pharm Des 2014 20 5574 5593 CrossRef Zhang H Liu B Li T Zhu Y Luo G Jiang Y Tang F Jian Z Xiao Y AMPK activation serves a critical role in mitochondria quality control via modulating mitophagy in the heart under chronic hypoxia Int J Mol Med 2018 41 69 76 CrossRef PubMed Li P A Hou X Hao S Mitochondrial biogenesis in neurodegeneration J Neurosci Res 2017 95 2025 2029 CrossRef PubMed Yin W Signore A P Iwai M Cao G Gao Y Chen J Rapidly increased neuronal mitochondrial biogenesis after hypoxic ischemic brain injury Stroke 2008 39 3057 3063 CrossRef PubMed Marsin A S Bertrand L Rider M H Deprez J Beauloye C Vincent M F Van den Berghe G Carling D Hue L Phosphorylation and activation of heart PFK 2 by AMPK has a role in the stimulation of glycolysis during ischaemia Curr Biol 2000 10 1247 1255 CrossRef
Biomolecules 2020 10 958 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 13 of 17 Thomas L W Ashcroft M Exploring the molecular interface between hypoxia inducible factor signalling and mitochondria Cell Mol Life Sci 2019 76 1759 1777 CrossRef PubMed De Gioia R Biella F Citterio G Rizzo F Abati E Nizzardo M Bresolin N Comi G P Corti S Neural Stem Cell Transplantation for Neurodegenerative Diseases Int J Mol Sci 2020 21 3103 CrossRef Pittenger M F Discher D E Peault B M Phinney D G Hare J M Caplan A I Mesenchymal stem cell perspective Cell biology to clinical progress NPJ Regen Med 2019 4 22 CrossRef Mohammad K Dakik P Medkour Y Mitrofanova D Titorenko V I Quiescence Entry Maintenance and Exit in Adult Stem Cells Int J Mol Sci 2019 20 2158 CrossRef Alijani N Johari B Moradi M Kadivar M A review on transcriptional regulation responses to hypoxia in mesenchymal stem cells Cell Biol Int 2019 44 14 26 CrossRef Das R Jahr H van Osch G J Farrell E The role of hypoxia in bone marrow derived mesenchymal stem cells Considerations for regenerative medicine approaches Tissue Eng Part B Rev 2010 16 159 168 CrossRef Han Y Ren J Bai Y Pei X Han Y Exosomes from hypoxia treated human adipose derived mesenchymal stem cells enhance angiogenesis through VEGF VEGF R Int J Biochem Cell Biol 2019 109 59 68 CrossRef PubMed Cui G H Wu J Mou F F Xie W H Wang F B Wang Q L Fang J Xu Y W Dong Y R Liu J R et al Exosomes derived from hypoxia preconditioned mesenchymal stromal cells ameliorate cognitive decline by rescuing synaptic dysfunction and regulating inflammatory responses in APP PS1 mice FASEB J 2018 32 654 668 CrossRef PubMed Rocco M D Itri L De Bels D Corazza F Balestra C The normobaric oxygen paradox A new tool for the anesthetist Minerva Anestesiol 2014 80 366 372 PubMed Cimino F Balestra C Germonpre P De Bels D Tillmans F Saija A Speciale A Virgili F Pulsed high oxygen induces a hypoxic like response in human umbilical endothelial cells and in humans J Appl Physiol 2012 113 1684 1689 CrossRef PubMed Balestra C Germonpre P Hypoxia a multifaceted phenomenon The example of the normobaric oxygen paradox Eur J Appl Physiol 2012 112 4173 4175 CrossRef Haddad J J Antioxidant and prooxidant mechanisms in the regulation of redox y sensitive transcription factors Cell Signal 2002 14 879 897 CrossRef Novak S Drenjancevic I Vukovic R Kellermayer Z Cosic A Tolusic Levak M Balogh P Culo F Mihalj M Anti Inflammatory Effects of Hyperbaric Oxygenation during DSS Induced Colitis in BALB c Mice Include Changes in Gene Expression of HIF 1alpha Proinflammatory Cytokines and Antioxidative Enzymes Mediat Inflamm 2016 2016 7141430 CrossRef Hu Q Liang X Chen D Chen Y Doycheva D Tang J Tang J Zhang J H Delayed hyperbaric oxygen therapy promotes neurogenesis through reactive oxygen species hypoxia inducible factor 1alpha beta catenin pathway in middle cerebral artery occlusion rats Stroke 2014 45 1807 1814 CrossRef Milovanova T N Bhopale V M Sorokina E M Moore J S Hunt T K Hauer Jensen M Velazquez O C Thom S R Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo J Appl Physiol 2009 106 711 728 CrossRef Yu Q H Zhang P X Liu Y Liu W Yin N Hyperbaric oxygen preconditioning protects the lung against acute pancreatitis induced injury via attenuating inflammation and oxidative stress in a nitric oxide dependent manner BioChem Biophys Res Commun 2016 478 93 100 CrossRef Ren P Kang Z Gu G Liu Y Xu W Tao H Zhang J H Sun X Ji H Hyperbaric oxygen preconditioning promotes angiogenesis in rat liver after partial hepatectomy Life Sci 2008 83 236 241 CrossRef PubMed Salhanick S D Belikoff B Orlow D Holt D Reenstra W Buras J A Hyperbaric oxygen reduces acetaminophen toxicity and increases HIF 1alpha expression Acad Emerg Med 2006 13 707 714 CrossRef PubMed Peng Z Ren P Kang Z Du J Lian Q Liu Y Zhang J H Sun X Up regulated HIF 1alpha is involved in the hypoxic tolerance induced by hyperbaric oxygen preconditioning Brain Res 2008 1212 71 78 CrossRef PubMed Milosevic J Adler I Manaenko A Schwarz S C Walkinshaw G Arend M Flippin L A Storch A Schwarz J Non hypoxic stabilization of hypoxia inducible factor alpha HIF alpha Relevance in neural progenitor stem cells Neurotox Res 2009 15 367 380 CrossRef PubMed
Biomolecules 2020 10 958 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 14 of 17 Calvert J W Cahill J Yamaguchi Okada M Zhang J H Oxygen treatment after experimental hypoxia ischemia in neonatal rats alters the expression of HIF 1alpha and its downstream target genes J Appl Physiol 2006 101 853 865 CrossRef Bai X Sun B Pan S Jiang H Wang F Krissansen G W Sun X Down regulation of hypoxia inducible factor 1alpha by hyperbaric oxygen attenuates the severity of acute pancreatitis in rats Pancreas 2009 38 515 522 CrossRef Li Z Li M Li X Zhang M Zhao Y Ren W Cheng J Wang X Hyperbaric oxygen inhibits venous neointimal hyperplasia following arteriovenous fistulization Int J Mol Med 2017 39 1299 1306 CrossRef Zhang Q Chang Q Cox R A Gong X Gould L J Hyperbaric oxygen attenuates apoptosis and decreases inflammation in an ischemic wound model J Investig Dermatol 2008 128 2102 2112 CrossRef Sun L Marti H H Veltkamp R Hyperbaric oxygen reduces tissue hypoxia and hypoxia inducible factor 1 alpha expression in focal cerebral ischemia Stroke 2008 39 1000 1006 CrossRef Li Y Zhou C Calvert J W Colohan A R Zhang J H Multiple effects of hyperbaric oxygen on the expression of HIF 1 alpha and apoptotic genes in a global ischemia hypotension rat model Exp Neurol 2005 191 198 210 CrossRef Duan S Shao G Yu L Ren C Angiogenesis contributes to the neuroprotection induced by hyperbaric oxygen preconditioning against focal cerebral ischemia in rats Int J Neurosci 2015 125 625 634 CrossRef PubMed Gu G J Li Y P Peng Z Y Xu J J Kang Z M Xu W G Tao H Y Ostrowski R P Zhang J H Sun X J Mechanism of ischemic tolerance induced by hyperbaric oxygen preconditioning involves upregulation of hypoxia inducible factor 1alpha and erythropoietin in rats J Appl Physiol 2008 104 1185 1191 CrossRef PubMed Lin P Y Sung P H Chung S Y Hsu S L Chung W J Sheu J J Hsueh S K Chen K H Wu R W Yip H K Hyperbaric Oxygen Therapy Enhanced Circulating Levels of Endothelial Progenitor Cells and Angiogenesis Biomarkers Blood Flow in Ischemic Areas in Patients with Peripheral Arterial Occlusive Disease J Clin Med 2018 7 548 CrossRef PubMed Anguiano Hernandez Y M Contreras Mendez L de Los Angeles Hernandez Cueto M Muand Oz Medina J E Santillan Verde M A Barbosa Cabrera R E Delgado Quintana C A Trejo Rosas S Santacruz Tinoco C E Gonzalez Ibarra J et al Modification of HIF 1alpha NF akappaB IGFBP 3 VEGF and adiponectin in diabetic foot ulcers treated with hyperbaric oxygen Undersea Hyperb Med 2019 46 35 44 Hsu S L Yin T C Shao P L Chen K H Wu R W Chen C C Lin P Y Chung S Y Sheu J J Sung P H et al Hyperbaric oxygen facilitates the effect of endothelial progenitor cell therapy on improving outcome of rat critical limb ischemia Am J Transl Res 2019 11 1948 1964 Sureda A Batle J M Martorell M Capo X Tejada S Tur J A Pons A Antioxidant Response of Chronic Wounds to Hyperbaric Oxygen Therapy PLoS ONE 2016 11 e0163371 CrossRef Hadanny A Efrati S Oxygen A limiting factor for brain recovery Crit Care 2015 19 307 CrossRef Vadas D Kalichman L Hadanny A Efrati S Hyperbaric Oxygen Environment Can Enhance Brain Activity and Multitasking Performance Front Integr Neurosci 2017 11 25 CrossRef Efrati S Ben Jacob E Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Rev Neurother 2014 14 233 236 CrossRef Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E Efrati S Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 2015 33 943 951 CrossRef Tal S Hadanny A Sasson E Suzin G Efrati S Hyperbaric Oxygen Therapy Can Induce Angiogenesis and Regeneration of Nerve Fibers in Traumatic Brain Injury Patients Front Hum Neurosci 2017 11 508 CrossRef PubMed Yao H Chung S Hwang J W Rajendrasozhan S Sundar I K Dean D A McBurney M W Guarente L Gu W Ronty M et al SIRT1 protects against emphysema via FOXO3 mediated reduction of premature senescence in mice J Clin Investig 2012 122 2032 2045 CrossRef PubMed Nemoto S Fergusson M M Finkel T SIRT1 functionally interacts with the metabolic regulator and transcriptional coactivator PGC 1 alpha J Biol Chem 2005 280 16456 16460 CrossRef PubMed
Biomolecules 2020 10 958 84 15 of 17 Yan W Fang Z Yang Q Dong H Lu Y Lei C Xiong L SirT1 mediates hyperbaric oxygen preconditioning induced ischemic tolerance in rat brain J Cereb Blood Flow Metab 2013 33 396 406 CrossRef PubMed 85 Xue F Huang J W Ding P Y Zang H G Kou Z J Li T Fan J Peng Z W Yan W J Nrf2 antioxidant defense pathway is involved in the neuroprotective effects of Sirt1 against focal cerebral ischemia in rats after hyperbaric oxygen preconditioning Behav Brain Res 2016 309 1 8 CrossRef PubMed 86 Hu Q Manaenko A Bian H Guo Z Huang J L Guo Z N Yang P Tang J Zhang J H Hyperbaric Oxygen Reduces Infarction Volume and Hemorrhagic Transformation Through ATP NAD Sirt1 Pathway in Hyperglycemic Middle Cerebral Artery Occlusion Rats Stroke 2017 48 1655 1664 CrossRef 87 Hong Qiang H Mang Qiao S Fen X Shan Shan L Hui Juan C Wu Gang H Wen Jun Y Zheng Wu P Sirt1 mediates improvement of isoflurane induced memory impairment following hyperbaric oxygen preconditioning in middle aged mice Physiol Behav 2018 195 1 8 CrossRef 88 Suzuki J Endurance performance is enhanced by intermittent hyperbaric exposure via up regulation of proteins involved in mitochondrial biogenesis in mice Physiol Rep 2017 5 e13349 CrossRef 89 DeCato T W Bradley S M Wilson E L Harlan N P Villela M A Weaver L K Hegewald M J Effects of sprInt interval training on cardiorespiratory fitness while in a hyperbaric oxygen environment Undersea Hyperb Med 2019 46 117 124 90 Chavko M Harabin A L Regional lipid peroxidation and protein oxidation in rat brain after hyperbaric oxygen exposure Free Radic Biol Med 1996 20 973 978 CrossRef 91 Gutsaeva D R Suliman H B Carraway M S Demchenko I T Piantadosi C A Oxygen induced mitochondrial biogenesis in the rat hippocampus Neuroscience 2006 137 493 504 CrossRef PubMed 92 Davis C H Kim K Y Bushong E A Mills E A Boassa D Shih T Kinebuchi M Phan S Zhou Y Bihlmeyer N A et al Transcellular degradation of axonal mitochondria Proc Natl Acad Sci USA 2014 111 9633 9638 CrossRef PubMed 93 Hayakawa K Esposito E Wang X Terasaki Y Liu Y Xing C Ji X Lo E H Transfer of mitochondria from astrocytes to neurons after stroke Nature 2016 535 551 555 CrossRef 94 Lippert T Borlongan C V Prophylactic treatment of hyperbaric oxygen treatment mitigates inflammatory response via mitochondria transfer CNS Neurosci Ther 2019 25 815 823 CrossRef PubMed 95 Han Z B Ren H Zhao H Chi Y Chen K Zhou B Liu Y J Zhang L Xu B Liu B et al Hypoxia inducible factor HIF 1 alpha directly enhances the transcriptional activity of stem cell factor SCF in response to hypoxia and epidermal growth factor EGF Carcinogenesis 2008 29 1853 1861 CrossRef 96 Shandley S Wolf E G Schubert Kappan C M Baugh L M Richards M F Prye J Arizpe H M Kalns J Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy Undersea Hyperb Med 2017 44 257 269 CrossRef 97 Heyboer M 3rd Milovanova T N Wojcik S Grant W Chin M Hardy K R Lambert D S Logue C Thom S R CD34 CD45 dim stem cell mobilization by hyperbaric oxygen Changes with oxygen dosage Stem Cell Res 2014 12 638 645 CrossRef 98 Thom S R Bhopale V M Velazquez O C Goldstein L J Thom L H Buerk D G Stem cell mobilization by hyperbaric oxygen Am J Physiol Heart Circ Physiol 2006 290 H1378 H1386 CrossRef 99 Wang X L Yang Y J Xie M Yu X H Liu C T Wang X Proliferation of neural stem cells correlates with Wnt 3 protein in hypoxic ischemic neonate rats after hyperbaric oxygen therapy Neuroreport 2007 18 1753 1756 CrossRef 100 Feng Z Liu J Ju R Hyperbaric oxygen treatment promotes neural stem cell proliferation in the subventricular zone of neonatal rats with hypoxic ischemic brain damage Neural Regen Res 2013 8 1220 1227 101 Yang Y Wei H Zhou X Zhang F Wang C Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor extracellular signal regulated kinase signaling after traumatic brain injury Neuroreport 2017 28 1232 1238 CrossRef PubMed 102 Zhang T Yang Q W Wang S N Wang J Z Wang Q Wang Y Luo Y J Hyperbaric oxygen therapy improves neurogenesis and brain blood supply in piriform cortex in rats with vascular dementia Brain Inj 2010 24 1350 1357 CrossRef PubMed
Biomolecules 2020 10 958 16 of 17 103 Yang Y J Wang X L Yu X H Wang X Xie M Liu C T Hyperbaric oxygen induces endogenous neural stem cells to proliferate and differentiate in hypoxic ischemic brain damage in neonatal rats Undersea Hyperb Med 2008 35 113 129 PubMed 104 Lee Y S Chio C C Chang C P Wang L C Chiang P M Niu K C Tsai K J Long course hyperbaric oxygen stimulates neurogenesis and attenuates inflammation after ischemic stroke Mediat Inflamm 2013 2013 512978 CrossRef 105 Wei L Wang J Cao Y Ren Q Zhao L Li X Wang J Hyperbaric oxygenation promotes neural stem cell proliferation and protects the learning and memory ability in neonatal hypoxic ischemic brain damage Int J Clin Exp Pathol 2015 8 1752 1759 106 Thom S R Milovanova T N Yang M Bhopale V M Sorokina E M Uzun G Malay D S Troiano M A Hardy K R Lambert D S et al Vasculogenic stem cell mobilization and wound recruitment in diabetic patients Increased cell number and intracellular regulatory protein content associated with hyperbaric oxygen therapy Wound Repair Regen 2011 19 149 161 CrossRef 107 Bekheit M Baddour N Katri K Taher Y El Tobgy K Mousa E Hyperbaric oxygen therapy stimulates colonic stem cells and induces mucosal healing in patients with refractory ulcerative colitis A prospective case series BMJ Open Gastroenterol 2016 3 e000082 CrossRef 108 Gardin C Bosco G Ferroni L Quartesan S Rizzato A Tatullo M Zavan B Hyperbaric Oxygen Therapy Improves the Osteogenic and Vasculogenic Properties of Mesenchymal Stem Cells in the Presence of Inflammation In Vitro Int J Mol Sci 2020 21 1452 CrossRef 109 Lin S S Ueng S W Niu C C Yuan L J Yang C Y Chen W J Lee M S Chen J K Effects of hyperbaric oxygen on the osteogenic differentiation of mesenchymal stem cells BMC Musculoskelet Disord 2014 15 56 CrossRef 110 Chiu C H Chang S S Chang G J Chen A C Cheng C Y Chen S C Chan Y S The Effect of Hyperbaric Oxygen Treatment on Myoblasts and Muscles After Contusion Injury J Orthop Res 2020 38 329 335 CrossRef 111 Chaillou T Lanner J T Regulation of myogenesis and skeletal muscle regeneration Effects of oxygen levels on satellite cell activity FASEB J 2016 30 3929 3941 CrossRef PubMed 112 Horie M Enomoto M Shimoda M Okawa A Miyakawa S Yagishita K Enhancement of satellite cell differentiation and functional recovery in injured skeletal muscle by hyperbaric oxygen treatment J Appl Physiol 2014 116 149 155 CrossRef PubMed 113 Zadori A Agoston V A Demeter K Hadinger N Varady L Kohidi T Gobl A Nagy Z Madarasz E Survival and differentiation of neuroectodermal cells with stem cell properties at different oxygen levels Exp Neurol 2011 227 136 148 CrossRef PubMed 114 Zhou H X Liu Z G Liu X J Chen Q X Umbilical cord derived mesenchymal stem cell transplantation combined with hyperbaric oxygen treatment for repair of traumatic brain injury Neural Regen Res 2016 11 107 113 CrossRef PubMed 115 Geng C K Cao H H Ying X Yu H L Effect of mesenchymal stem cells transplantation combining with hyperbaric oxygen therapy on rehabilitation of rat spinal cord injury Asian Pac J Trop Med 2015 8 468 473 CrossRef 116 Pan H C Chin C S Yang D Y Ho S P Chen C J Hwang S M Chang M H Cheng F C Human amniotic fluid mesenchymal stem cells in combination with hyperbaric oxygen augment peripheral nerve regeneration Neurochem Res 2009 34 1304 1316 CrossRef PubMed 117 Khan M Meduru S Pandian R P Rivera B K Kuppusamy P Effect of oxygenation on stem cell therapy for myocardial infarction Adv Exp Med Biol 2011 701 175 181 118 Khan M Meduru S Mohan I K Kuppusamy M L Wisel S Kulkarni A Rivera B K Hamlin R L Kuppusamy P Hyperbaric oxygenation enhances transplanted cell graft and functional recovery in the infarct heart J Mol Cell Cardiol 2009 47 275 287 CrossRef 119 Pena Villalobos I Casanova Maldonado I Lois P Prieto C Pizarro C Lattus J Osorio G Palma V Hyperbaric Oxygen Increases Stem Cell Proliferation Angiogenesis and Wound Healing Ability of WJ MSCs in Diabetic Mice Front Physiol 2018 9 995 CrossRef 120 Torbati D Church D F Keller J M Pryor W A Free radical generation in the brain precedes hyperbaric oxygen induced convulsions Free Radic Biol Med 1992 13 101 106 CrossRef
Biomolecules 2020 10 958 17 of 17 121 Kellogg R H La Pression barometrique Paul Bert s hypoxia theory and its critics Respir Physiol 1978 34 1 28 CrossRef 122 Leach R M Rees P J Wilmshurst P Hyperbaric oxygen therapy BMJ 1998 317 1140 1143 CrossRef PubMed 123 Jain K K Torbati D Tao H Y Ni G T Oxygen Toxicity In Textbook of Hyperbaric Medicine 4th ed Best Publishing Company North Palm Beach FL USA 1999 pp 47 59 124 Hadanny A Meir O Bechor Y Fishlev G Bergan J Efrati S The safety of hyperbaric oxygen treatment retrospective analysis in 2334 patients Undersea Hyperb Med 2016 43 113 122 PubMed 125 Hadanny A Meir O Bechor Y Fishlev G Bergan J Efrati S Seizures during hyperbaric oxygen therapy Retrospective analysis of 62 614 treatment sessions Undersea Hyperb Med 2016 43 21 28 PubMed 126 Hadanny A Zubari T Tamir Adler L Bechor Y Fishlev G Lang E Polak N Bergan J Friedman M Efrati S Hyperbaric oxygen therapy effects on pulmonary functions A prospective cohort study BMC Pulm Med 2019 19 148 CrossRef PubMed 2020 by the authors Licensee MDPI Basel Switzerland This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution CC BY license http creativecommons org licenses by 4 0
The Aging Male ISSN 1368 5538 Print 1473 0790 Online Journal homepage https www tandfonline com loi itam20 The impact of hyperbaric oxygen therapy on erectile functions and serum testosterone levels in patients with erectile dysfunction Volkan Sen Mehmet Oguz Sahin Bora Irer Evin Koc Guner Yildiz To cite this article Volkan Sen Mehmet Oguz Sahin Bora Irer Evin Koc Guner Yildiz 2020 The impact of hyperbaric oxygen therapy on erectile functions and serum testosterone levels in patients with erectile dysfunction The Aging Male 23 1 66 70 DOI 10 1080 13685538 2019 1578740 To link to this article https doi org 10 1080 13685538 2019 1578740 Published online 23 Mar 2019 Submit your article to this journal Article views 793 View related articles View Crossmark data Citing articles 2 View citing articles Full Terms Conditions of access and use can be found at https www tandfonline com action journalInformation journalCode itam20
THE AGING MALE 2020 VOL 23 NO 1 66 70 https doi org 10 1080 13685538 2019 1578740 ORIGINAL ARTICLE The impact of hyperbaric oxygen therapy on erectile functions and serum testosterone levels in patients with erectile dysfunction Volkan Sena Mehmet Oguz Sahina Bora Irerb Evin Kocc and Guner Yildizd a Department of Urology Manisa State Hospital Manisa Turkey bDepartment of Urology Izmir Metropolitan Municipality Esrefpasa Hospital Izmir Turkey cDepartment of Underwater and Hyperbaric Medicine Neoks Hyperbaric Oxygen Therapy Center Izmir Turkey dDepartment of Urology Dr Suat Seren Chest Diseases and Surgery Training and Research Hospital Izmir Turkey ABSTRACT ARTICLE HISTORY Objective To evaluate the effects of hyperbaric oxygen therapy HBOT on erectile functions and serum testosterone levels in patients with erectile dysfunction ED Methods The patients treated by HBOT for several diseases between July 2017 May 2018 and had erectile dysfunction were included in the study All patients filled the International Index of Erectile Function IIEF questionnaire form serum total testosterone TT and free testosterone FT levels were examined before the first day and after the last day of HBOT The effects of demographic characteristics of patients on erectile functions were evaluated Patients were categorized according to the risk factors The IIEF scores TT and FT levels of patients in first day and after last day of HBOT were compared Results Totally 43 patients were included in the study The mean post HBOT IIEF EF score was significantly higher than the mean pre HBOT IIEF EF score of patients 25 4 5 3 vs 20 6 5 1 p 001 There was no statistical difference between the pre HBOT and post HBOT serum TT and FT levels of patients 4 0 2 3 ng ml vs 4 1 2 0 ng ml p 797 8 6 3 8 pg ml vs 8 9 3 5 pg ml p 658 Conclusions HBOT improved the erectile functions in ED patients however we cannot detect any effect on testosterone levels in our study Received 17 January 2019 Accepted 30 January 2019 Published online 22 February 2019 Introduction Erectile dysfunction ED is defined as the persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance 1 ED is a worldwide health problem increasing with aging and has negative impacts on men s quality of life 2 The prevalence of ED in 40 70 years old men was detected between 25 52 in previous reports 3 6 Several treatment modalities can be used in ED first line treatment of ED includes oral pharmacotherapy with phosphodiesterase type 5 PDE 5 inhibitors Intracavernous injections constitute second line treatment and surgical treatment penile prostheses may be offered to patients as a third line therapy for ED However new treatment modalities have become popular in recent years including low intensity extracorporeal shock wave therapy ESWT and hyperbaric oxygen therapy HBOT as an alternative treatment 7 9 HBOT is a kind of therapy in which the patients breathe 100 oxygen at pressures greater than CONTACT Volkan Sen sen_volkan yahoo com Erection erectile dysfunction hyperbaric oxygen therapy International Index of Erectile Function IIEF testosterone normal atmospheric sea level pressure 1 atm HBOT increases oxygen tensions and oxygen delivery to tissues by extra dissolved content of oxygen in the blood 10 HBOT had been used in the treatment of several medical conditions during the past 50 years including urological diseases such as interstitial cystitis radiation induced hemorrhagic cystitis and Fournier s gangrene FG 10 13 The first reports about the effect of HBOT on erectile functions were published ller et al and Yuan et al 8 11 Both of these by Mu studies showed that HBOT improved erectile functions in rat cavernous injury model 8 and in patients with posterior urethral reconstruction 14 Recent clinical studies showed that HBOT improved the erectile functions in non surgical patients and this effect was linked to induction of angiogenesis 15 16 We hypothesized that the improvement in erectile functions may be associated with increasing serum testosterone levels Passavanti et al showed that HBOT increased the serum total testosterone levels in both non ED patients and healthy men 17 However there Department of Urology Manisa State Hospital Manisa Turkey 2019 Informa UK Limited trading as Taylor Francis Group KEYWORDS
THE AGING MALE is no clinical study that investigates the effects of HBOT on serum total testosterone TT and free testosterone FT levels in patients with ED yet In this study we aimed to evaluate the effects of HBOT on erectile functions serum TT and FT levels in patients with ED 67 presented as mean standard derivation numbers n and percent Student Paired T test was used for comparison of variables before and after HBOT Statistical significance was set at a p values of
68 V SEN ET AL Table 2 Comparison of pre HBOT and post HBOT IIEF domain scores serum total testosterone and free testosterone levels Erectile function EF Intercourse satisfaction Orgasmic function Sexual desire Overall satisfaction Total testosterone ng ml Free testosterone pg ml Pre HBOT mean SD Post HBOT mean SD pa 20 6 5 1 10 7 3 0 9 0 1 5 7 0 2 0 7 4 2 3 4 0 2 3 8 6 3 8 25 4 5 3 12 3 2 6 9 3 1 4 8 0 1 6 8 4 1 9 4 1 2 0 8 9 3 5
THE AGING MALE 69 Table 3 The association between HBOT and the demographic characteristics erectile dysfunction risk factors and testosterone levels Covariate Age Category
IJIR Your Sexual Medicine Journal 2018 30 292 299 https doi org 10 1038 s41443 018 0023 9 ARTICLE Corrected Correction Hyperbaric oxygen can induce angiogenesis and recover erectile function Amir Hadanny MD1 2 3 Erez Lang MD1 2 4 Laurian Copel MD2 5 Oshra Meir MD1 Yair Bechor MD1 Gregory Fishlev MD1 2 Jacob Bergan MD1 2 Mony Friedman MD1 Amnon Zisman MD2 4 Shai Efrati MD1 2 6 7 1234567890 1234567890 Received 21 September 2016 Revised 29 January 2018 Accepted 7 April 2018 Published online 18 May 2018 The Author s 2018 This article is published with open access Abstract Erectile dysfunction ED is caused by microvascular or macrovascular insuf ciency in the majority of patients Recent studies have shown that hyperbaric oxygen therapy HBOT can induce angiogenesis in different body organs The effect of HBOT on the non surgery related ED has not been investigated yet The aim of the current study was to evaluate the effects of HBOT on sexual function and penile vascular bed in non surgical ED patients A prospective analysis of patients suffering from chronic ED treated with 40 daily HBOT sessions Clinical ef cacy was assessed using the International Index of Erectile Function questionnaire IIEF and a global ef cacy question GEQ The effect on the penile vascular bed was evaluated by perfusion MRI Thirty men mean age of 59 2 1 4 suffering from ED for 4 2 0 6 years completed the protocol HBOT signi cantly improved all IIEF domains by 15 88 p 0 01 Erectile function improved by 88 p 0 0001 and 80 of the patients reported positive outcome according to the GEQ Angiogenesis was indicated by perfusion MRI that showed a signi cant increase by 153 3 43 2 of K trans values in the corpous cavernous p 0 0001 HBOT can induce penile angiogenesis and improve erectile function in men suffering from EcD HBOT reverses the basic common pathophysiology atherosclerosis and decreased penile perfusion responsible for most cases of ED Introduction The normal erection is a complex event resulting from the coordinated function of psychological neurological hormonal and vascular systems 1 Penile blood ow disruption due to inadequate vascular perfusion is present in at least 60 of the erectile dysfunction ED patients 2 The Amir Hadanny MD Amir had gmail com 1 Sagol Center for Hyperbaric Medicine and Research Assaf Harofeh Medical Center Zeri n Israel 2 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 3 Bar Ilan University Ramat Gan Israel 4 Urology Department Asaf Harofeh Medical Center Zeri n Israel 5 Radiology Department Asaf Harofeh Medical Center Zeri n Israel 6 Research and Development Unit Assaf Harofeh Medical Center Zeri n Israel 7 Sagol School of Neuroscience Tel Aviv University TelAviv Israel rst line therapy used for ED relies on the vasodilatation effect of phosphodiesterase 5 inhibitors PDE5Is 3 However since the vasodilatation effect of PDE5Is is transient and dependent on the presence of adequate blood vessels within the corpora cavernosa CC there is a need for a treatment modality that intervenes with the baseline pathology and induces generation of new blood vessels angiogenesis Hyperbaric oxygen therapy HBOT has been shown to induce angiogenesis in different tissues experiencing compromised blood perfusion such as the brain and non healing wounds 4 5 The effect of HBOT on penile angiogenesis has not been investigated yet HBOT incorporates the inhalation of 100 oxygen at pressures exceeding 1 atmosphere absolute ATA thus increasing the amount of oxygen dissolved in the body tissues 6 One of the most interesting mechanisms induced by HBOT is angiogenesis mediated by release of omnipotent stem cells capable of differentiating into endothelial cells 7 9 HBOT also boosts the release of vascular endothelial growth factor VEGF and hypoxia inducible factor 1alpha HIF 1alpha crucial mediators for the angiogenesis process 9 In addition the improved oxygenation by HBOT creates the necessary environment
Hyperbaric oxygen can induce angiogenesis and recover erectile function needed for stem cells proliferation Pre clinical and clinical studies have demonstrated that HBOT can induce angiogenesis even in tissues with low regenerative potential such as the brain 10 12 Two studies on both humans and animals suggested a possible therapeutic effect of HBOT on ED related to surgical injuries 13 14 In the clinical study which included a cohort of 12 men suffering from ED after posterior urethral reconstruction surgery HBOT signi cantly improved erectile function 14 Aims The aim of the current study was to evaluate the effects of HBOT on sexual function and penile microvasculature in non surgical ED patients 293 dysfunction Each item is rated on a ve point ordinal scale Zero is scored when responders did not attempt intercourse Primary outcome was measured by questions 3 and 4 Question 3 asks Over the past four weeks when you have attempted sexual intercourse how often were you able to penetrate enter your partner Question 4 asks Over the past four weeks during sexual intercourse how often were you able to maintain your erection after you have penetrated your partner Ef cacy was also assessed on the basis of the scores for the ve separate domains of male sexual function of the IIEF 15 The domain scores were computed by adding the scores for the individual questions in each domain In addition ef cacy was also assessed using the global ef cacy question GEQ Did the treatment improve your erections with a yes or no response Perfusion MRI protocol Materials and methods A prospective analysis of men age 18 years or older with a clinical diagnosis of erectile dysfunction of more than six months duration The study was approved by the institutional review board and all participants gave written informed consent prior to their inclusion The study was registered in the US National Institute of Health Clinical Trails registry NCT02619383 Exclusion criteria included penile anatomical defects any active or history of malignancy including prostate cancer spinal cord injury any major psychiatric disorder uncontrolled with treatment claustrophobia chronic lung disease or chronic middle ear or sinus diseases Participants were allowed to continue with PDE5I medication if it was chronically used for more than 6 months prior to their inclusion Perfusion imaging technique called dynamic contrastenhanced MRI DCE MRI was used to evaluate the change in capillary leakage ow as indicated by K trans parameter values serving as indicator of angiogenesis 16 Seven patients underwent two MRI scans baseline and after HBOT Imaging was conducted using a 3 Tesla system MAGNETOM Skyra Siemens Germany The MRI protocol included anatomic T1 and T2 sequences and DCE detailed in supplementary section S1 K trans calculations were performed in four speci c axial sections located in the CC at the level of the penis base for better localization and reduced variability Fig 1a Another control K trans measurement was performed at the psoas muscle as it passes through the groin The relative change in penile K trans values in was calculated as post pre HBOT values pre HBOT value 100 Hyperbaric oxygen therapy Statistical analysis The treatment comprised 40 daily hyperbaric sessions 5 days a week in a multiplace hyperbaric chamber HAUXLife Support GmbH Germany Each session consisted of 90 min of exposure to 100 oxygen at 2 ATA with 5 min air breaks every 30 min The mean frequency of responses to questions 3 and 4 of the IIEF was calculated An analysis of covariance ANCOVA model was tted for each question which included maineffect terms for base line score patient age smoking diabetes mellitus hypertension ischemic heart disease use of PDE5Is and duration as covariates Mean domain scores from the IIEF were calculated and the treatment effect was analyzed by the described ANCOVA model The answers to the GEQ question yes or no were analyzed with the use of logistic regression analysis accounting for the same covariates as those listed for the ANCOVA models Using IIEF and erectile function domain scores means and standard deviations pairwise analysis was performed to calculate the sample size In order to detect a two sided change of one Sexual function assessment Ef cacy of the treatment was assessed at baseline 2 weeks after signing informed consent and in 2 weeks post their last HBOT session using the International Index of Erectile Function IIEF questionnaire 15 The IIEF is a validated multidimensional self administered questionnaire consisting of 15 items used for the clinical assessment of erectile
294 A Hadanny et al Fig 2 Flowchart of the patients included in the study using the Kolmogorov Smirnov test The alpha level was set to 0 05 Data were statistically analyzed using SPSS software version 22 0 Results Patients Fig 1 DCE MRI was performed using injection of contrast media Gd DTPA and aquring serial images in order to measure blood perfusion DCE MRI Ktrans map is calculated from the serial images see S 1 for further details a Penile MRI coordinates of measurement T2 MRI sequence demonstrates the 4 locations in each CC which were used to extract K trans values The base of the penis area was chosen for better localization in each patient and variability reduction b Average MRI dynamic contrast enhancement DCE maps pre and post HBOT Black to blue and green in this order re ect low K trans values low perfusion in the corporoa cavernousa Yellow and red in this order re ect high K trans values increased perfusion in the corpora cavernousa Top row K trans values at baseline Middle row K trans values after HBOT Bottom row delta map showing increase in K trans after HBOT Between June 2013 to May 2015 42 men suffering from ED were screened Two did not ful ll inclusion criteria and 3 were excluded due to contraindications 2 middle ear diseases 1 active malignancy HBOT was applied for 37 patients Seven patients did not complete 40 hyperbaric sessions 6 due to barotrauma 1 claustrophobia Accordingly 30 men completed the study and were included in the nal analysis Fig 2 The mean age was 59 2 1 4 years and the mean duration of symptoms prior to inclusion was 4 2 0 6 years All 30 patients reported having previous experience with PDE5Is 46 7 continued using PDE5Is while in the study Baseline characteristics are summarized in Table 1 Ef cacy standard deviation in Q3 Q4 and erectile function domain the calculated sample size was 20 23 Two sided paired t test was performed to compare K trans values before and after HBOT Continuous data were expressed as means standard errors The normal distribution for all variables was tested HBOT improved the mean scores of IIEF questions assessing the frequency of penetration 3 0 0 2 post HBOT vs 1 9 0 2 pre HBOT p 0 001 and maintenance of erections after penetration 3 4 0 2 post HBOT vs 1 7 0 2 pre HBOT p 0 001 The percent increase from base line
Hyperbaric oxygen can induce angiogenesis and recover erectile function Table 1 Patients baseline characteristics Age 59 2 1 4 Duration of symptoms years 4 2 0 6 Concurrent PDE5I No 16 53 3 Yes 14 46 7 Testosterone level ng dl 11 8 1 3 BMI Kg m2 27 8 0 6 History of smoking No 20 66 7 Yes 10 33 3 No 15 50 Yes 15 50 295 did not affect any of the above mentioned outcome measures p 0 1 Penile perfusion A signi cant increase in the renal blood ow was indicated in the seven participants who agreed to undergo penile perfusion MRI pre and post HBOT After HBOT the relative change in K trans values increased by 153 3 43 3 in the CC p 0 0001 The average K trans values are depicted in Fig 1b Comorbidities Diabetes Mellitus II HBA1c in Diabetics 7 8 0 3 Hypertension No 13 56 7 Yes 17 43 3 Dyslipidemia No 10 33 3 Yes 20 66 7 Ischemic Heart Disease No 22 73 3 Yes 8 26 7 No 9 30 Yes 21 70 No 26 86 7 Yes 4 13 3 Adverse events Six from the 37 patients who included in the study discontinued the treatment due to barotrauma 16 and one due to claustrophobia Barotraumas were mild and fully recovered in all patients after 3 days Five out of 30 men who completed the study protocol reported minor pain in the ear during recompression recovered completely and resumed HBOT sessions without any need for additional treatment Medications Beta blockers SSRI SNRI PDE5I phosphodiesterase 5 inhibtors BMI body mass index SSRI selective serotonin reuptake inhibitor SNRI serotonin norepinephrine reuptake inhibitor was 58 for question 3 and 100 for question 4 Table 2 Fig 3 Penetration and maintenance of erections improved to a response level of 4 or 5 success most times in 50 of men who were at level 0 or 1 no attempts or almost never successful before treatment and in 50 and 70 of men who were at level 2 and 3 success at half or less than half the times respectively prior to the treatment HBOT increased the mean scores for the erectilefunction domain by 10 4 1 2 90 p 0 001 Table 2 After HBOT 63 of the men had none to mild erectile dysfunction total of questions 1 2 3 4 5 and 15 was within 19 30 Fig 4 The mean scores for the orgasmic function intercourse satisfaction and overallsatisfaction domains were signi cantly improved by 29 59 after HBOT p 0 001 Table 2 Fig 3 After HBOT 24 of the 30 men 80 reported improved erections global ef cacy question Age duration of symptoms BMI the presence of diabetes mellitus hypertension dyslipidemia ischemic heart disease history of smoking and concurrent use of PDE5Is Discussion The present study shows for the rst time that penile angiogenesis and improved erectile function can be induced by HBOT in men suffering from chronic non surgical ED The improvement in sexual performance was signi cant in all IIEF domains and was most noticeable in both erectile function and the global ef cacy question responses Penile angiogenesis was demonstrated by perfusion MRI analysis Vascular integrity including appropriate vascular dilatation and increased blood ow to the cavernous sinusoidal system is a key component of the physiology of penile erections 17 18 Endothelial dysfunction atherosclerosis and microvascular diseases disrupt the penile blood ow and accordingly vascular etiology is the leading cause of ED 2 Because of the small diameter of penile arteries 1 2 mm compared with other arteries such as coronary arteries the same level of endothelial dysfunction and atherosclerosis may lead to a clinically more signi cant reduction of blood ow to the penis culminating in ED 19 Consequently ED can be the earliest symptom of cardiovascular disease Angiogenesis is the sprouting of new blood vessels using vasculogenic stem cells which differentiate into endothelial cells as well as other supporting structures The use of stem cells and or angiogenic growth factors for erectile dysfunction has been suggested previously Several pre clinical studies have shown bene cial effects using intracavernosal injections of bone marrow stem cells as well as VEGF in
296 Table 2 IIEF questionnaire Q3 Q4 and domains at baseline and after hyperbaric oxygen therapy HBOT A Hadanny et al Baseline Post HBOT Mean Change Percent change from baseline Sig Q3 1 9 0 2 3 0 0 2 1 1 0 2 58 10 p 0 0001 Q4 1 7 0 2 3 4 0 2 1 7 0 2 100 11 p 0 0001 IIEF Total 35 3 2 5 50 4 2 2 15 1 2 2 43 6 p 0 0001 Erectile function 11 4 1 1 21 9 1 2 10 4 1 2 91 10 p 0 0001 Orgasmic function 6 6 0 6 8 6 0 4 1 9 0 5 29 7 p 0 001 Sexual desire 6 3 0 4 7 2 0 3 0 9 0 3 14 5 p 0 009 Intercourse 6 2 0 6 9 2 0 6 3 0 0 6 48 10 p 0 0001 Overall satisfaction 4 8 0 4 7 0 0 4 2 2 0 5 46 10 p 0 0001 satisfaction Data are expressed as means standard errors Q3 question 3 item Q4 question 4 item IIEF international index of erectile function HBOT hyperbaric oxygen therapy Fig 3 Erectile dysfunction measures before and after hyperbaric oxygen therapy HBOT a Penetration erections Erections maintenance intercourse satisfaction and overall satisfaction scores signi cantly increased after HBOT b Erectile function and IIEF total score improved signi cantly after HBOT b IIEF total and erectile function scores signi cantly improved after HBOT
Hyperbaric oxygen can induce angiogenesis and recover erectile function 297 Fig 4 Erectile function severity at baseline and after hyperbaric oxygen therapy HBOT After HBOT 63 of the men had none to mild erectile dysfunction Erectile function is calculated as the total of questions 1 2 3 4 5 and 15 Erectile dysfunction severity is graded as 0 6 severe dysfunction 7 12 moderate dysfunction 13 18 mild to moderate dysfunction 19 24 mild dysfunction 25 30 normal function Fig 5 Case 1 DCE MRI After HBOT there was a signi cant increase in K trans values in both the right and left corpus cavernosum K trans values map was overlaid on the T2 sequence Black to blue and green in this order re ect low K trans values low perfusion in the corporoa cavernousa Yellow and red in this order re ect high Ktrans values increased perfusion in the corpora cavernousa different rat models 20 21 Both mobilization of vasculogenic stem cells and induction of angiogenic factors release such as VEGF and HIF 1alpha can be induced by repetitive HBOT sessions 5 9 Recent studies in patients suffering chronic neurological impairments stemming from stroke traumatic brain injury and anoxic brain injury have shown that HBOT neuro therapeutic effects are mediated by brain angiogenesis 22 24 One of the known differentiation characteristics of newly formed blood vessels is their relatively high leakage compared to normal blood vessels 25 The high leakage of these newly formed blood vessels has been exploited to demonstrate angiogenesis using DCE MRI 25 In the present study by use of DCE MRI and demonstration of higher K trans values after HBOT it was clearly demonstrated that angiogenesis was induced in the penis CC The demonstrated penile angiogenesis may be one of the underlying physiological mechanisms responsible for the bene cial clinical effect of HBOT on erectile and sexual functions When compared to PDE5I or other ED treatments HBOT holds the promise of unique new intervention modality with several advantages and disadvantages Starting with the advantages the induction of angiogenesis by HBOT is aiming for resolution of the basic vascular pathology instead of short term symptomatic relief PDE5I or other penile injections interventions require pre planning and preparation prior to sexual intercourse When compared to PDE5I HBOT enables regaining the ability to have spontaneous or unplanned intercourse Second diabetic patients had similar ef cacy with HBOT unlike the lower ef cacy seen with PDE5I 26 The third and most important advantage relates to the high potency of HBOT even in men in whom PDE5Is have no bene cial effect compared to at least 30 of patients who do not regain erectile function using PDE5Is 27 In the current study population ED persisted 4 2 0 6 years prior to inclusion and all men used PDE5Is prior to inclusion without gaining satisfactory erectile function HBOT carries two main disadvantages First while PDE5Is or intracavernosal injections have immediate effect in
298 HBOT as in other regenerative therapies the bene cial effect can be recognized only after a series of sessions Second HBOT sessions require considerable time and dedication 40 daily treatments 90 min each HBOT is considered to be a safe method of treatment in general 28 in other vascular related pathologies 29 30 and was found to be safe also for ED patients In general the main adverse effects include middle ear or sinus barotraumas which are usually mild and temporary with complete resolution after several days 28 In the current study the six patients who stopped HBOT due to barotrauma could have continued the treatment with no additional risk if they so wanted Our study has several limitations The rst is related to the relatively small number of patients However the clear statistical signi cant effect a two way pairwise method analysis has considerable power 100 even in a small group of patients Second our study lacks an appropriate control placebo group Nevertheless one should not expect any signi cant improvement in IIEF questionnaires within 3 months in men suffering from ED for several years In addition the improvement in penile perfusion was clearly noticeable in objective analysis of perfusion MRI The correlation between the clinical and the objective penile perfusion MRI ndings give further strength to study results Third HBOT is a rather costly therapy compared to the accepted medications This is the rst study evaluating the effect of HBOT on this population suffering from chronic non surgical ED Additional studies are necessary in order to evaluate which subgroups of patients can bene t the most from this treatment and the optimal HBOT protocol needed for those patients HBOT can induce penile angiogenesis and improve erectile function in men suffering from ED HBOT reverses the basic common pathophysiology atherosclerosis and decreased penile perfusion responsible for most of ED cases The treatment can be considered even years after the onset of erectile dysfunction and in men with unsatisfactory response to PDE5Is Further studies are needed to evaluate the subgroups of men who can bene t the most from this treatment Appendix The following is a case example including the clinical data and the MR imaging results A 52 year old male with history of hypertension dyslipidemia and ischemic heart disease who suffered from erectile dysfunction during the last 4 years prior to his inclusion During the rst year experienced partial improvement using PDE5I but the effect waned off After 40 sessions of HBOT erectile function improved from 9 to 19 penetration erections Q3 increased from 1 to 3 and A Hadanny et al maintenance of erections Q4 increased from 1 to 3 Intercourse satisfaction and overall satisfaction improved from 8 to 11 K trans increased by 225 in the right CC and by 61 in the left CC Fig 5 Acknowledgements The authors thank Ms Michal Ben Jacob and Mr Raz Tuval for reviewing and proo ng the manuscript Compliance with ethical standards Con ict of interest The authors declare that they have no con ict of interest Open Access This article is licensed under a Creative Commons Attribution 4 0 International License which permits use sharing adaptation distribution and reproduction in any medium or format as long as you give appropriate credit to the original author s and the source provide a link to the Creative Commons license and indicate if changes were made The images or other third party material in this article are included in the article s Creative Commons license unless indicated otherwise in a credit line to the material If material is not included in the article s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use you will need to obtain permission directly from the copyright holder To view a copy of this license visit http creativecommons org licenses by 4 0 References 1 Burls A Gold L Clark W Systematic review of randomised controlled trials of sildena l Viagra in the treatment of male erectile dysfunction Br J Gen Pract 2001 51 1004 12 2 Virag R Bouilly P Frydman D Is impotence an arterial disorder A study of arterial risk factors in 440 impotent men Lancet 1985 1 181 4 3 Bella AJ Lee JC Carrier S Benard F Brock GB 2015 CUA Practice guidelines for erectile dysfunction Can Urol Assoc J 2015 9 23 9 4 Duan S Shao G Yu L Ren C Angiogenesis contributes to the neuroprotection induced by hyperbaric oxygen preconditioning against focal cerebral ischemia in rats Int J Neurosci 2015 125 625 34 5 Lin KC Niu KC Tsai KJ Kuo JR Wang LC et al Attenuating in ammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury J Trauma Acute Care Surg 2012 72 650 9 6 Fosen KM Thom SR Hyperbaric oxygen vasculogenic stem cells and wound healing Antioxid Redox Signal 2014 21 1634 47 7 Thom SR Bhopale VM Velazquez OC Goldstein LJ Thom LH et al Stem cell mobilization by hyperbaric oxygen Am J Physiol Heart Circ Physiol 2006 290 H1378 86 8 Hopf HW Gibson JJ Angeles AP Constant JS Feng JJ et al Hyperoxia and angiogenesis Wound Repair Regen 2005 13 558 64 9 Peng ZR Yang AL Yang QD The effect of hyperbaric oxygen on intracephalic angiogenesis in rats with intracerebral hemorrhage J Neurol Sci 2014 342 114 23 10 Chen J Zhang ZG Li Y Wang L Xu YX et al Intravenous administration of human bone marrow stromal cells induces angiogenesis in the ischemic boundary zone after stroke in rats Circ Res 2003 92 692 9
Hyperbaric oxygen can induce angiogenesis and recover erectile function 11 Jiang Q Zhang ZG Ding GL Zhang L Ewing JR et al Investigation of neural progenitor cell induced angiogenesis after embolic stroke in rat using MRI Neuroimage 2005 28 698 707 12 Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E et al Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 2015 33 943 51 13 Muller A Tal R Donohue JF Akin Olugbade Y Kobylarz K et al The effect of hyperbaric oxygen therapy on erectile function recovery in a rat cavernous nerve injury model J Sex Med 2008 5 562 70 14 Yuan JB Yang LY Wang YH Ding T Chen TD et al Hyperbaric oxygen therapy for recovery of erectile function after posterior urethral reconstruction Int Urol Nephrol 2011 43 755 61 15 Rosen RC Riley A Wagner G Osterloh IH Kirkpatrick J et al The international index of erectile function IIEF a multidimensional scale for assessment of erectile dysfunction Urology 1997 49 822 30 16 Li L Wang K Sun X Wang K Sun Y et al Parameters of dynamic contrast enhanced MRI as imaging markers for angiogenesis and proliferation in human breast cancer Med Sci Monit 2015 21 376 82 17 Fournier GR Jr Juenemann KP Lue TF Tanagho EA Mechanisms of venous occlusion during canine penile erection an anatomic demonstration J Urol 1987 137 163 7 18 Costa C Virag R The endothelial erectile dysfunction connection an essential update J Sex Med 2009 6 2390 404 19 Montorsi P Ravagnani PM Galli S Rotatori F Veglia F et al Association between erectile dysfunction and coronary artery disease Role of coronary clinical presentation and extent of coronary vessels involvement the COBRA trial Eur Heart J 2006 27 2632 9 20 Qiu X Lin H Wang Y Yu W Chen Y et al Intracavernous transplantation of bone marrow derived mesenchymal stem cells 299 21 22 23 24 25 26 27 28 29 30 restores erectile function of streptozocin induced diabetic rats J Sex Med 2011 8 427 36 Qiu X Sun C Yu W Lin H Sun Z et al Combined strategy of mesenchymal stem cell injection with vascular endothelial growth factor gene therapy for the treatment of diabetes associated erectile dysfunction J Androl 2012 33 37 44 Boussi Gross R Golan H Fishlev G Bechor Y Volkov O et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 2013 8 e79995 Boussi Gross R Golan H Volkov O Bechor Y Hoo en D et al Improvement of memory impairments in poststroke patients by hyperbaric oxygen therapy Neuropsychology 2015 29 610 21 Hadanny A Golan H Fishlev G Bechor Y Volkov O et al Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restor Neurol Neurosci 2015 33 471 86 Nagy JA Benjamin L Zeng H Dvorak AM Dvorak HF Vascular permeability vascular hyperpermeability and angiogenesis Angiogenesis 2008 11 109 19 Salonia A Rigatti P Montorsi F Sildena l in erectile dysfunction a critical review Curr Med Res Opin 2003 19 241 62 McMahon CN Smith CJ Shabsigh R Treating erectile dysfunction when PDE5 inhibitors fail BMJ 2006 332 589 92 hadanny A Meir O Bechor Y Fishlev G Bergan J et al The safety of hyperbaric oxygen treatment retrospective analysis in 2 334 patients Undersea Hyperb Med 2016 43 113 22 Kalani M Jorneskog G Naderi N Lind F Brismar K Hyperbaric oxygen HBO therapy in treatment of diabetic foot ulcers Longterm follow up J Diabetes Complicat 2002 16 153 8 Mathews R Rajan N Josefson L Camporesi E Makhuli Z Hyperbaric oxygen therapy for radiation induced hemorrhagic cystitis J Urol 1999 161 435 7
70 V SEN ET AL References 1 2 3 4 5 6 7 8 9 10 11 12 13 Hatzimouratidis K Giuliano F Moncada I et al Guideline Associates Parnham A Serefoglu EC EAU Guidelines on Erectile Dysfunction Premature Ejaculation Penile Curvature and Priapism Edn presented at the EAU Annual Congress London 2017 Arnhem The Netherlands EAU Guidelines Office Fisher WA Eardley I McCabe M et al Erectile dysfunction ED is a shared sexual concern of couples I couple conceptions of ED J Sex Med 2009 6 2746 2760 Zhang X Yang B Li N et al Prevalence and risk factors for erectile dysfunction in Chinese adult males J Sex Med 2017 14 1201 1208 Braun M Wassmer G Klotz T et al Epidemiology of erectile dysfunction results of the Cologne Male Survey Int J Impot Res 2000 12 305 311 Quilter M Hodges L von Hurst P et al male sexual function in New Zealand a population based crosssectional survey of the prevalence of erectile dysfunction in men aged 40 70 years J Sex Med 2017 14 928 936 Nguyen HMT Gabrielson AT Hellstrom WJG Erectile dysfunction in young men a review of the prevalence and risk factors Sex Med Rev 2017 5 508 520 Kalyvianakis D Hatzichristou D Low intensity shockwave therapy improves hemodynamic parameters in patients with vasculogenic erectile dysfunction a triplex ultrasonography based sham controlled trial J Sex Med 2017 14 891 897 ller A Tal R Donohue JF et al The effect of hyperMu baric oxygen therapy on erectile function recovery in a rat cavernous nerve injury model J Sex Med 2008 5 562 570 Cormier J Theriot M Patient diagnosed with chronic erectile dysfunction refractory to PDE 5 Inhibitor therapy reports improvement in function after hyperbaric oxygen therapy Undersea Hyperb Med 2016 43 463 465 Tang H Sun Y Xu C et al Effects of hyperbaric oxygen therapy on tumor growth in murine model of PC 3 prostate cancer cell line Urology 2009 73 205 208 Ribeiro de Oliveira TM Carmelo Rom ao AJ Gamito Guerreiro FM et al Hyperbaric oxygen therapy for refractory radiation induced hemorrhagic cystitis Int J Urol 2015 22 962 966 Mindrup SR Kealey GP Fallon B Hyperbaric oxygen for the treatment of Fournier s gangrene J Urol 2005 173 1975 1977 Tanaka T Nitta Y Morimoto K et al Hyperbaric oxygen therapy for painful bladder syndrome interstitial cystitis resistant to conventional treatments long 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 term results of a case series in Japan BMC Urol 2011 11 11 Yuan JB Yang LY Wang YH et al Hyperbaric oxygen therapy for recovery of erectile function after posterior urethral reconstruction Int Urol Nephrol 2011 43 755 761 Sahin MO Sen V Eser E et al The effect of hyperbaric oxygen therapy on erectile functions a prospective clinical study Urol Int 2018 101 206 211 Hadanny A Lang E Copel L et al Hyperbaric oxygen can induce angiogenesis and recover erectile function Int J Impot Res 2018 30 292 299 Passavanti G Tanasi P Brauzzi M et al Can hyperbaric oxygenation therapy HOT modify the blood testosterone concentration Urologia 2010 77 52 56 Cimsit M editor The history of hyperbaric treatment In Hyperbaric Medicine ed 1 Ankara Eflatun Publishing House Place published 2009 p 1 12 Churchill Davidson I Sanger C Thomlinson RH Highpressure oxygen and radiotherapy Lancet 1955 268 1091 1095 Degener S Pohle A Strelow H et al Long term experience of hyperbaric oxygen therapy for refractory radio or chemotherapy induced haemorrhagic cystitis BMC Urol 2015 15 38 Nakada T Nakada H Yoshida Y et al Hyperbaric oxygen therapy for radiation cystitis in patients with prostate cancer a long term follow up study Urol Int 2012 89 208 214 Rosa I Guerreiro F Hyperbaric oxygen therapy for the treatment of Fournier s gangrene a review of 34 cases Acta Med Port 2015 28 619 623 Mehl AA Nogueira Filho DC Mantovani LM et al Management of Fournier s gangrene experience of a university hospital of Curitiba Rev Col Bras Cir 2010 37 435 441 Li C Zhou X Liu LF et al Hyperbaric oxygen therapy as an adjuvant therapy for comprehensive treatment of Fournier s gangrene Urol Int 2015 94 453 458 Shupak A Shoshani O Goldenberg I et al Necrotizing fasciitis an indication for hyperbaric oxygenation therapy Surgery 1995 118 873 878 Chiles KA Staff I Johnson Arbor K et al A doubleblind randomized trial on the efficacy and safety of hyperbaric oxygenation therapy in the preservation of erectile function after radical protastectomy J Urol 2018 199 805 811 Gilliver SC Ashcroft GS Sex steroids and cutaneous wound healing the contrasting influences of estrogens and androgens Climateric 2007 10 276 288 Nakada T Saito H Ota K et al Serum testosterone testicular connective tissue protein and testicular histology in rats treated with hyperbaric oxygen Int Urol Nephrol 1986 18 439 447
Dr Paul Harch President 504 348 1660 www hyperbarics org Ken Locklear Executive Director 561 640 4546 www hbomedtoday com dbsearch html LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Presentation prepared by Anita Poole CPS CAP Hyperbaric Oxygen Therapy and SPECT Brain Imaging in the Treatment of Chronic Brain Injury Paul G Harch M D Clinical Assistant Professor L S U School of Medicine Refined low pressure Hyperbaric Oxygen Therapy HBOT protocols for neurological injuries Presentation includes selective sampling of nearly 400 chronic brain injuries over the past 12 years Original case was demented diver with residual brain decompression sickness 7 months after injury Diver achieved clinical psychometric functional brain imaging improvement Discovery then generalized to patients with Chronic traumatic brain injury Cerebral palsy Chronic carbon monoxide poisoning Toxic brain injury Chronic stroke Alzheimer s Disease Autism Substance abuse 30 other neurological conditions After demonstrating effectiveness in humans a 1996 and 2001 animal study demonstrated the first ever improvement in chronic brain injury Treatment protocol developed by Dr Harch now being used in research clinical practices by multiple centers throughout the United States and internationally World wide experience has demonstrated the generic rehabilitative potential of low LHE May 02 2002 pressure HBOT in chronic brain and neurological injury Copyright Retained Paul G Harch M D 2002 1
Case Presentation Triple head SPECT Scan of Normal Brain SPECT is a tool to directly measure brain blood flow and indirectly measure metabolism 26 year old female left scan 34 year old male right scan No alcohol or substance abuse No brain traumas No diseases to affect brain blood flow or metabolism Notice smooth appearance LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Triple head SPECT Scan of Normal Brain female male LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 2
Case Presentation Acute Chronic Treatment of Traumatic Brain Injury and Coma 19 year old male college freshman Ejected from motor vehicle at 65 mph in 1991 1st HBOT began 19 hours post accident Impacted left frontal parietal skull region Within hour Glascow coma scale was 6 7 ventilator dependent CT revealed diffuse edema midline shift petechial hemorrhages subarachnoid hemorrhage small subdural hematoma basilar skull fracture 1st scan SPECT image 1 month after accident shows significant injury to left frontal area and contra coup injury to right parietal occipital with luxury perfusion Scan shows very large defects in brain flood flow After initial treatments patient became conversant independently ambulatory with slight spasticity Within 8 weeks of accident patient went from ventilator to walking and talking LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Acute Chronic Treatment of Traumatic Brain Injury and Coma continued 2nd scan 1 year later after 188 HBOT treatments Improved perfusion in ischemic penumbral areas of right sided lesions Noticeable improvement in cognition 40 gain written computation math Patient verbalized insight to condition and that he could no longer aspire to be a surgeon Balance and gait improvement from 3 wheel trike to 2 wheel bike Treatments discontinued when patient enrolled in remedial college courses Patient referred to as Lazarus by his doctor In Jan 2001 12 years post injury patient called physician to tell him of 2nd promotion at the bank Patient active functional and employed Current cost of 188 HBOT treatments at 150 200 each 28 200 37 600 Note treatment during immediate acute phase of injury could cost more LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 3
Case Presentation Acute Chronic Treatment of Traumatic Brain Injury and Coma 19 y male Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 See previous page for case history on this patient LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 4
Case Presentation Traumatic Brain Injury and Substance Abuse 23 year old male Navy Medical Corpsman graduated second in class 5 TBIs 4 w loss of consciousness the 3rd resulted in largest loss of memory and started migraines Complaints of migraines short long term memory loss speech problems serious alcohol abuse Treated at Bethesda and Walter Reed Brain Injury Center Discharged from Navy with 60 VA disability Unable to remember anatomy and physiology during rehab training 14 jobs in 2 years 1st scan Extensive frontal lobe injury top scan shows extensive tissue damage Jan 2001 40 HBOT treatments over 4 weeks 2nd scan Extensive improvement in blood flow to frontal parietal lobes Dramatic cessation of migraine headaches Cessation of marijuana use dramatic reduction in alcohol use 1 month after treatments Return of memory tremendous improvement in speech cognition math skills and energy levels 8 months after treatment Married remains functional to date patient to return for additional HBOTs LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Traumatic Brain Injury and Substance Abuse 23 y male Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 5
Case Presentation Traumatic Brain Injury 23 year old female 5 years post motor vehicle accident major TBI ventilation for 3 weeks Complaints of aphasia left body weakness with spasticity cognitive problems w generalized decrease in intellectual capacity emotional instability mood swings temper tantrums post injury Prior to HBOT Innumerable therapies with no resolution of problems 1st scan Marked reduction in flow to right temporal lobe Marked decrease in parasagittal regions of brain Surface texture very coarse heterogeneous blood flow 80 HBOT treatments 2nd scan Shows greatly improved brain blood flow Improvement in left body paresis imbalance Temper tantrums mood swings noticeably decreased Ability to read write substantially improved Marked improvement in physical endurance LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Traumatic Brain Injury 23 y female Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 6
Case Presentation Alzheimer s Disease 58 year old male Accomplished architect with decline in work memory 8 years ago Alzheimer s diagnosis 5 years ago started on Aricept Continued to decline over next 3 years Started CPAP for sleep apnea 9 98 without effect 3 years prior to HBOT treatments Switched to Neotrophin for 9 months limited improvement 9 2000 began Exelon dose increased to maximum level 6 weeks before HBOT Wife notes improvement in cognition behavior 89 HBOT treatments During treatment progressive slow improvement in cognition behavior Generalized non significant improvement in scores Some new learning ability Symptomatically patient better Patient taken off Exelon due to side effects Continuing HBOT beginning to resume normal life activities LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Alzheimer s Disease 58 y male Baseline After 89 HBOT Treatments LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 7
Case Presentation Physical Abuse 21 year old female gang raped and beaten extensively at age 12 Significant cognitive deficit though apparently normal motor coordination Severe difficulties with sleep 1st scan SPECT shows significant frontal lobe injury with severe frontal lobe tissue damage 60 HBOT treatments 2nd scan SPECT shows greatly increased blood flow to frontal lobe manifested by thickening filling in on scan Improved cognitive function enables patient to operate in a higher capacity in a mentally demanding job Patient promoted 6 months post treatment Sleep difficulties improved LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Physical Abuse 21 y female Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 8
Case Presentation Mental Retardation 44 year old male Mentally retarded from likely combination of delivery induced trauma and TBI at 2 weeks old Unable to read or spell more than a few words No abstract reasoning ability Difficulty understanding concepts i e food will spoil if left out Seizures bi weekly with constant tremors on medication Worked 2 days week at Goodwill doing menial tasks 1st scan SPECT shows reduction in blood flow to frontal lobe extensive frontal lobe damage 40 HBOT treatments 2nd scan SPECT shows a marked increase in blood flow in the frontal lobe manifest by closure of fissures Work attendance from 2 days to 4 days per week Seizure rate fell to 1 per month on medication Noticeable reduction in motor tremors Presently learning to read at a Kindergarten level Able to understand abstract concepts better i e that food spoils Able to do more complex work tasks Increased rational behavior LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Mental Retardation 44 y male Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 9
Case Presentation Cerebral Palsy 8 year old boy Complicated difficult delivery resulted in ischemic hypoxic injury to brain 1st scan Prominent abnormalities in temporal lobes especially on left side 2nd scan Generalized improvement in blood flow with greater amount of yellow on the slices on far right of picture Improved flow to both temporal lobes Patient s mother reported Some improvement in inappropriate behavior Less leg dragging Markedly improved ability to have bowel movements with no incontinence Muscle tone attention concentration improvements LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Cerebral Palsy 8 y male Scan 1 Scan 2 1 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 10
Case Presentation Stroke 60 year old male 2 years post stroke History of multiple white matter strokes Complaints of body weakness intractable dizziness difficulty swallowing speech problems 1st scan Surface of brain with coarse texture markedly decreased blood flow in right temporal lobe 80 HBOT treatments 2nd scan Improvement in coarse texture greatly increased blood flow Dizziness reduced to point that patient could Leave house Walk without cane Stopped using left knee brace Speech swallowing improved Overall mood improved LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Stroke 60 y male Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 11
Case Presentation Alcoholism and Stroke 68 year old male 1 month post embolic stroke right middle cerebral artery Chronic heavy drinker Developed atrial fibrillation likely secondary to the alcohol Severe weakness left side of body profound left sided neglect Noticeable cognitive deterioration power of attorney to son 1st scan Multiple areas of decreased perfusion in frontal temporal lobes Slightly coarse appearance to brain surface Note large gap on left side of each image denoting right hemispheric stroke 1 month of HBOT treatments Dramatic improvement in cognition speed of thinking decrease in neglect Markedly improved motor function on left side of body Rescinded power of attorney resumed active pursuit of business affairs 2nd scan Improved flow to all lobes Global smoothing of brain surface LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Alcoholism and Stroke 68 y male Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 12
Case Presentation Substance Abuse 19 year old male Extensive drug abuse history for past 4 years since 15 Heavy dosing chronic marijuana LSD 5 6 episodes of hallucinogenic mushrooms Extensive Rohypnol use patient believes caused most memory problems Cocaine crack abuse for 1 month earlier in year of 1st brain scans Extensive use of Valium Concentrated glue sniffing White Out typewriter correction solvent Alcohol abuse Complaints of chronic headaches irritability impulsive behavior and short term memory problems History of loss of consciousness in the past due to trauma and an episode of syncope that same year 5 years before 1st first brain scan 1st scan Grossly heterogeneous pattern of brain blood flow with multiple areas of decreased perfusion in frontal and temporal lobes 2nd scan 1 HBOT Global smoothing improvement in blood flow Inferior frontal lobe defects likely due to patient s trauma Note Single HBOT improvement is predictive that the full course of HBOT treatment 40 HBOTs minimum for treatment of a chronic injury would permanently improve the patient s brain and brain function Patient did limited course of 20 HBOTs then defaulted on treatments due to feeling better and the 200 mile commute LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Substance Abuse 19 y male Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 13
Case Presentation Carbon Monoxide Poisoning 51 year old female Exposed to home gasoline powered generator in poorly ventilated area Complaints of headaches trouble thinking walking talking functioning increasingly somnolent confused Diagnosed with altered mental status At 36 hours blood carboxyhemoglobin elevated at 2 2 upper limits of normal 1 5 1st scan Pattern very coarse with multiple significant deficits in blood flow 1 HBOT 68 hours after admission at 2 atms for 35 mins patient claustrophobic 2nd scan 3 hours later Dramatic improvement in brain blood flow Smoothing of the overall pattern Noticeable improvement in mental and cognitive status LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Carbon Monoxide Poisoning 51 y female Scan 1 top view Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 14
Case Presentation Shaken Baby 6 month old girl 4 months after 2 episodes of trauma by father repetitive slamming on crib bed resolved 3 days later severe trauma with cardiac arrest Problems indicated at initiation of HBOT Never smiled No social interaction Minimum ability to eat Paraplegia Seizures hand and arm twitching many times per day for 45 seconds each 1st scan baseline SPECT Minimal brain blood flow to higher centers of brain 80 HBOT treatments Starting to smile positive social interaction with mother Eating baby food Significant improvement in use of hands and arms Calmer No seizures while off nearly all seizure medication 2nd scan SPECT image shows improved brain blood flow to higher centers Example of savings Nursing care costs reduced and prescription drug cost alone was reduced by at least 500 year with increased savings each year of additional life LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Shaken Baby 6 month female Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 15
Case Presentation Gun Shot Wound to Brain 29 year old female self inflicted 38 caliber hollow point to right temple 6 years post trauma Severe spasticity arms and legs Paraplegia with severe weakness in arms Poor trunk control Insomnia secondary to muscle spasms Intractable constipation Headaches 1st scan baseline SPECT Marked diffuse decrease in blood flow with worst area along path of bullet 80 HBOT treatments Physiatrist reports Generalized decrease in spasticity increase in left hand grip and movement in knees Patient reports Increased trunk and extremity motor function Marked decrease in insomnia Natural bowel movements without constipation Decreased headaches 2nd scan Generalized increase in brain blood flow with pattern of diffuse smoothing LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Gun Shot Wound to Brain 29 y female Scan 1 Scan 2 right view LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 16
Case Presentation Autism 3 year old female born 3 weeks premature to a mother with mild toxemia fetal distress emergency C section Extensive neurological workup over the next year Final diagnoses Persistent Developmental Delay Autism Mild Mental Retardation Can t talk or walk walks on knees Minimum eye contact Afraid of crowds and people No self help Self abusive behavior 1st scan Marked reduction in blood flow to temporal lobes less so to cerebral lobes 80 HBOT treatments Walks with a walker Makes eye contact and is interactive and playful Comfortable in crowds and with people Feeds self Decreased self abusive behavior 2nd scan Marked improvement in blood flow to temporal and cerebral lobes Generalized increase to rest of brain 7 months later Continued generalized improvement Full ambulation Playful interactive affectionate loving Self abusive behavior nearly gone LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Autism 3 y female Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 17
Case Presentation Traumatic Brain Injury from Child Abuse 48 year old male 45 years post injury extensive physical damage to right parietal bone at age 3 Apparently normal motor coordination Difficulty with higher math and remembering names Dreamed in black and white 1st scan Before 63 HBOT treatments 2nd scan After Improved motor coordination math skills and name memory Now dreams in color LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 Case Presentation Traumatic Brain Injury from Child Abuse 48 y male Scan 1 Scan 2 LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 18
Dr Harch s cost effective refined lowpressure Hyperbaric Oxygen Therapy protocols have improved the quality of life for 1 000 s of brain and neurologically injured patients Treatment is here today Dr Harch s success has been replicated by physicians in multiple treatment centers throughout the United States and many other countries around the world For a treatment center near you please visit www hbomedtoday com dbsearch html or call Ken Locklear Executive Director of IHMA at 561 640 4546 For further technical information please visit www hyperbarics org or call Dr Paul Harch President of IHMA at 504 348 1660 Presentation prepared by Anita Poole CPS CAP LHE May 02 2002 Copyright Retained Paul G Harch M D 2002 19
See discussions stats and author profiles for this publication at https www researchgate net publication 38012230 Low pressure hyperbaric oxygen therapy and SPECT brain imaging in the treatment of blast induced chronic traumatic brain injury post concussion syndrome and post traumatic stress Article in Cases Journal June 2009 DOI 10 4076 1757 1626 2 6538 Source PubMed CITATIONS READS 44 666 4 authors including Paul G Harch Edward Francis Fogarty Louisiana State University Health Sciences Center New Orleans University of North Dakota 46 PUBLICATIONS 632 CITATIONS 21 PUBLICATIONS 239 CITATIONS SEE PROFILE Keith William Van Meter Louisiana State University Health Sciences Center New Orleans 47 PUBLICATIONS 823 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects Porcine Tourniquet Injury Ameliorated by HBOT View project All content following this page was uploaded by Paul G Harch on 28 May 2014 The user has requested enhancement of the downloaded file SEE PROFILE
Cases Journal BioMed Central Open Access Case Report Low pressure hyperbaric oxygen therapy and SPECT brain imaging in the treatment of blast induced chronic traumatic brain injury post concussion syndrome and post traumatic stress disorder a case report Paul G Harch 1 Edward F Fogarty2 Paul K Staab1 and Keith Van Meter1 Address 1Section of Emergency Medicine Department of Medicine Louisiana State University Health Sciences Center 2021 Perdido St Room W535 New Orleans Louisiana 70112 USA and 2Department of Radiology University of North Dakota School of Medicine and Health Sciences Post Office Box 1975 515 East Broadway Avenue Suite 106 Bismarck North Dakota 58502 USA Email Paul G Harch paulharchmd aol com Edward F Fogarty efogarty medicine nodak edu Paul K Staab pstaab wjmc org Keith Van Meter kvanmeter aol com Corresponding author Published 9 June 2009 Cases Journal 2009 2 6538 doi 10 1186 1757 1626 0002 0000006538 Received 12 March 2009 Accepted 4 April 2009 This article is available from http www casesjournal com content 2 1 6538 2009 licensee BioMed Central Ltd This is an Open Access article distributed under the terms of the Creative Commons Attribution License http creativecommons org licenses by 3 0 which permits unrestricted use distribution and reproduction in any medium provided the original work is properly cited Abstract A 25 year old male military veteran presented with diagnoses of post concussion syndrome and post traumatic stress disorder three years after loss of consciousness from an explosion in combat The patient underwent single photon emission computed tomography brain blood flow imaging before and after a block of thirty nine 1 5 atmospheres absolute hyperbaric oxygen treatments The patient experienced a permanent marked improvement in his post concussive symptoms physical exam findings and brain blood flow In addition he experienced a complete resolution of posttraumatic stress disorder symptoms After treatment he became and has remained employed for eight consecutive months This case suggests a novel treatment for the combined diagnoses of blast induced post concussion syndrome and post traumatic stress disorder Introduction By January 2008 it was estimated that as many as 300 000 servicemen and women from the current Iraq and Afghanistan Wars have PTSD or major depression 320 000 have experienced a TBI and 82 000 have all three diagnoses 1 Treatment is available for PTSD and depression but there is no proven therapy for the dual diagnoses of PTSD and the residual effects of TBI the PCS 2 HBOT is the use of greater than atmospheric pressure oxygen in an enclosed chamber to treat basic disease processes 3 HBOT has been traditionally applied to certain emergent conditions and chronic wound conditions but not to blast induced TBI PCS or PTSD This case report is the first application of the authors low pressure HBOT protocol for chronic brain injury to blast induced TBI PCS and PTSD An early version of this protocol was recently reported in an animal model of chronic TBI that duplicated the human experience 4 Case presentation A 25 year old retired Caucasian male U S Marine presented with headaches tinnitus and sleep disturbance Three years before evaluation the patient sustained LOC a few minutes from an IED explosion with anterograde memory loss and confusion one hour and persistent right ear tinnitus headaches imbalance and sleep disturbance He developed PTSD symptoms within 3 months Page 1 of 5 page number not for citation purposes
Cases Journal 2009 2 6538 and experienced six more explosions with near LOC within 15 months After medical evaluation diagnoses were TBI PCS PTSD depression hearing loss and tinnitus Prioritized Symptom List 1 Constant headaches with intermittent confusion irritability tunnel vision and dizziness 2 Bilateral tinnitus 3 Sleep disruption 4 Left eye blurred vision 5 Irritability 6 Depression social withdrawal Additional Symptoms 7 Fatigue 8 Decreased hearing 9 Imbalance 10 Cognitive problems memory attention decreased speed of thinking 11 Back pain 12 Bilateral knee pain 13 PTSD symptoms intrusive thoughts combat thoughts nightmares tachycardia Med Surg Medications None FH ROS and PHIS noncontributory or negative PSH Engaged no children lives with parents 3 years college education no tobacco or drugs one to two beers week Neuro PEx Abnormalities Slight deviation of right eye laterally bilateral decreased hearing to softly rubbing fingers at one foot noxious response to 512 Hz tuning fork decreased finger tapping http www casesjournal com content 2 1 6538 speed unstable rotation exam tandem gait and Romberg Treatment and testing MRI brain normal SPECT brain imaging pre HBOT and 72 h after the 39th HBOT The patient underwent 39 HBOT s in 26 calendar days at 1 5 ATA 60 minutes total dive time twice day five days week in a monoplace chamber with 100 oxygen Outcome Headache permanently gone after the 1st HBOT After 12 HBOT s symptoms 3 6 and 7 improved At 25th HBOT absence of PTSD symptoms Re evaluation after 37 HBOT s 1 4 6 primary problems improved s 1 3 5 6 2 6 no change 2 4 7 additional symptoms improved 7 9 10 13 3 7 no change 3 6 6 abnormal exam findings retested improved 1 finding not retested right eye deviation SPECT heterogeneous with bilateral frontal and temporal defects all improved post HBOT See Additional file 1 Figures 1 and 2 Figure 1 PreHBOT SPECT brain scan three dimensional surface reconstruction and processed transverse images Pre HBOT scan was rendered in three dimensional surface reconstruction format by PJT based on the method developed and taught by Picker International using Picker software In this method brain blood flow is computer indexed to frontal Figure 1 SPECT brain scan three dimensional surface reconstruction and processed transverse images Pre HBOT Pre HBOT SPECT brain scan three dimensional surface reconstruction and processed transverse images Note bilateral orbital frontal and temporal lobe defects and diffuse heterogeneous pattern of blood flow Page 2 of 5 page number not for citation purposes
Cases Journal 2009 2 6538 http www casesjournal com content 2 1 6538 Figure 2 SPECT brain scan three dimensional surface reconstruction and processed transverse images Post HBOT Post HBOT SPECT brain scan three dimensional surface reconstruction and processed transverse images Note relative improvement in brain blood flow to bilateral focal frontal and temporal defects and overall normalization of blood flow to a more homogeneous pattern lobe blood flow A frontal lobe surface defect was identified on a selected transverse slice Processed filtered transverse slices were then featured with a 100 window such that all pixels render a white image Counts were slowly subtracted by decreasing the window threshold until the defect was visible as a full thickness black defect in the contour of the cortex As the defect emerged and was registered in proper anatomic proportion to the rest of frontal cortical blood flow the numerical window level was taken as the determination threshold Three separate determinations were made for each scan and the final threshold taken as an average of the three determinations The technologist was blind to the final image reconstruction due to software restrictions that only allow threshold determination The surface reconstruction image at this threshold is featured in the image above Color is aesthetic Note bilateral orbital frontal and temporal lobe defects areas typically injured in traumatic brain injury consistent with processed transverse images in the right hand columns Processed images also show an abnormal diffuse heterogeneous pattern of blood flow Description of processing is in SD1 Figure 2 Post HBOT SPECT brain scan three dimensional surface reconstruction and processed transverse images Three dimensional surface image was prepared in identical fashion to the image in Figure 1 Note relative improvement in brain blood flow to bilateral focal frontal and temporal defects consistent with processed transverse images in the right hand columns Transverse slices also show normalization of the blood flow to a more homogeneous pattern Discussion The present case is the first application of the author s HBOT protocol to blast induced TBI PCS and PTSD The patient s symptomatic physical exam and SPECT improvements are similar to ours 3 5 6 9 and others 7 8 previous cases case series of non blast TBI suggesting common pathophysiology The unexpected result was the complete resolution of PTSD With the overlap of symptoms pathophysiology and anatomy in TBI PCS and PTSD 10 HBOT is likely impacting common shared targets in this case Page 3 of 5 page number not for citation purposes
Cases Journal 2009 2 6538 Conclusion http www casesjournal com content 2 1 6538 Additional material Thirty nine low pressure HBOT s caused a reduction in symptoms and signs of chronic mild moderate blastinduced TBI PCS and PTSD The resolution of symptoms and signs of TBI PCS and PTSD were reflected in global and focal improvements in brain blood flow imaging suggesting a novel treatment for these combined diagnoses Additional file 1 Side by side Pre and Post HBOT processed transverse SPECT brain blood flow images Pre HBOT scan is on the left and post HBOT on the right Click on either image to initialize movie Images were obtained on a Picker Prism 3000 triple head gamma camera Both scans were processed by technologist PJT 25 mCi of ECD was prepared with the standard manufacturer s kit and injected in a peripheral vein in a low noise low light area while the patient was quiet and motionless One hour after injection acquisition proceeded with a 360 degree rotation and 40 stops 20 seconds stop on a 128 x 128 matrix using low energy high resolution fan beam collimators Motion correction was used for minor movement Raw data was processed by transverse reconstruction using 360 degree filtered back projection and a ramp filter followed by a LoPass filter order 2 2 Cutoff was taken at the intersection of the best fit LoPass filter and noise on the power spectrum graph Per file attenuation correction and best fit ellipse were applied Images were oblique reformatted with slice thickness at 4 mm 2 pixels aligned and off center zoom applied 20 cm2 area Images were presented in all 3 orthogonal planes Transverse processed images were analyzed with Osirix Open source software version 3 3 2 and windowed at a level of 1000 with a window width of 2000 They were subsequently rendered in QuickTime movie format starting from vertex and proceeding through the base of the brain Images are in standard SPECT format and orientation Color map is red yellow green blue and violet from highest brain blood flow to lowest Note the marked generalized increase in perfusion on the post HBOT scan Click here for file http www biomedcentral com content supplementary 17571626 0002 0000006538 S1 mov Patient s perspective Patient has declined to submit his perspective due to privacy concerns List of abbreviations ATA Atmospheres absolute ECD Ethyl cysteinate dimer FH Family history HBOT Hyperbaric oxygen therapy HPI History of present illness IED Improvised explosive device LOC Loss of consciousness MRI Magnetic resonance imaging PCS Post concussion syndrome PEx Physical exam PHIS Prior head injury history PMH Past medical history PSH Personal and Social history PTSD post traumatic stress disorder ROS Review of systems SPECT Single photon emission computed tomography TBI Traumatic brain injury Consent Written informed consent was obtained from the patient for publication of this case report and accompanying images A copy of the written consent is available for review by the Editor in Chief of this journal In addition this case was approved by the LSU School of Medicine s Institutional Review Board as a case report Acknowledgements The authors are indebted to nuclear technologist Philip J Tranchina for expert processing and three dimensional thresholding of the SPECT brain imaging Competing interests The authors declare competing interests The primary author has a small corporation Harch Hyperbarics Inc that does hyperbaric consulting Author KVM has a corporation that leases hyperbaric oxygen chambers and a corporation that contracts to provide hyperbaric oxygen and woundcare services None of the authors have personal or financial relationships with people or organizations that would influence the interpretation of data in this report Authors contributions PGH evaluated the patient ordered the treatment and imaging and wrote the draft of the manuscript EFF analyzed and presented the SPECT imaging and assisted in writing the manuscript PKS assisted in the treatment of the patient and assisted in writing the manuscript KVM assisted in development of the hyperbaric protocol and writing the manuscript All authors read and approved the final manuscript References 1 2 3 4 5 6 7 8 9 Invisible Wounds of War Psychological and Cognitive Injuries Their Consequences and Services to Assist Recovery Edited by Tanielian TJaycox LH Center for Military Health Policy Research the Rand Corporation 2008 King NS PTSD and traumatic brain injury Folklore and fact Brain Injury 2008 22 1 5 Harch PG Neubauer RA The Textbook of Hyperbaric Medicine 3rd edition Edited by Jain KK Hogrefe and Huber 1999 318 349 Harch PG Kriedt C Van Meter KW Sutherland RJ Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury Brain Res 2007 1174 120 129 Harch PG Van Meter KW Neubauer RA Gottlieb SF The Textbook of Hyperbaric Medicine 2nd edition Edited by Jain KK Hogrefe and Huber 1996 480 491 Harch PG Neubauer RA Hyperbaric oxygen therapy in global cerebral ischemia anoxia and coma In The Textbook of Hyperbaric Medicine 4th edition Edited by Jain KK Hogrefe Huber 2004 223 262 Neubauer RA Gottlieb SF Pevsner NH Hyperbaric oxygen treatment of closed head injury South Med J 1994 87 933 936 Golden ZL Neubauer RA Golden CJ et al Improvement in cerebral metabol ism in chronic brain injury after hyperbaric oxygen therapy Int J Neurosci 2002 112 119 131 Harch PG Gottlieb SF Van Meter KW Staab P HMPAO SPECT brain imaging and low pressure HBOT in the diagnosis and treatment of chronic traumatic ischemic hypoxic and Page 4 of 5 page number not for citation purposes
Cases Journal 2009 2 6538 10 http www casesjournal com content 2 1 6538 anoxic encephalopathies Undersea Hyperbaric Medicine 1994 21 30 Kennedy JE Jaffee MS Leskin GA et al Posttraumatic stress disorder and posttraumatic stress disorder like symptoms and mild traumatic brain injury J Rehab Res Devel 2007 44 895 920 Page 5 of 5 page number not for citation purposes View publication stats
ORIGINAL RESEARCH published 13 January 2022 doi 10 3389 fpsyt 2021 713141 Brain SPECT as an Imaging Biomarker for Evaluating Effects of Novel Treatments in Psychiatry A Case Series Steven R D Best 1 Natalie Haustrup 2 and Dan G Pavel 3 1 The Neuroscience Center Deerfield IL United States 2 Haustrup Scientific Consulting Cork Ireland 3 PathFinder Brain SPECT Deerfield IL United States Edited by Theodore A Henderson The Synaptic Space Inc and Neuro Luminance Inc United States Reviewed by Daniel Keeser Ludwig Maximilian University of Munich Germany Richard Bruce Bolster University of Winnipeg Canada Correspondence Steven R D Best srdbest neuroscience md Present address Natalie Haustrup Eli Lilly and Company Cork Ireland Posthumously 1934 2021 Specialty section This article was submitted to Neuroimaging and Stimulation a section of the journal Frontiers in Psychiatry Received 21 May 2021 Accepted 13 December 2021 Published 13 January 2022 Citation Best SRD Haustrup N and Pavel DG 2022 Brain SPECT as an Imaging Biomarker for Evaluating Effects of Novel Treatments in Psychiatry A Case Series Front Psychiatry 12 713141 doi 10 3389 fpsyt 2021 713141 Frontiers in Psychiatry www frontiersin org The difficulties of evaluating patients with complex neuropsychiatric conditions and prescribing appropriate treatments are well known Imaging complements clinical assessments and allows a clinician to narrow the differential diagnosis by facilitating accurate and efficient evaluation This is particularly relevant to neuropsychiatric conditions that are often diagnosed using a trial and error process of exclusion Single Photon Emission Computed Tomography SPECT is a functional brain imaging procedure that allows practitioners to measure the functional changes of gray matter structures based on regional cerebral blood flow rCBF The accurate diagnosis and treatment selection in psychiatry is challenging due to complex cases and frequent comorbidities However such complex neuropsychiatric conditions are increasingly benefitting from new treatment approaches in addition to established medications Among these are combination transcranial magnetic stimulation with ketamine infusions CTK hyperbaric oxygen therapy HBOT and perispinal administration of etanercept PSE This article provides readers with six case study examples that demonstrate how brain SPECT imaging can be used both as a diagnostic tool and as a potential biomarker for monitoring and evaluating novel treatments for patients with complex neuropsychiatric conditions Six patients were assessed in our clinic and baseline brain SPECT imagesTourettes and a long history of alcohol were visually compared with SPECT images collected after periods of treatment with CTK or HBOT followed by PSE This retrospective review demonstrates the clinical utility of these novel treatments and describes how SPECT imaging can complement standard diagnostic assessments A novel display technique for SPECT images is described and we argue that SPECT imaging can be used for monitoring biomarker for clinical change Keywords SPECT biomarker CTK HBOT depression psychiatry brain treatment INTRODUCTION While experienced psychiatrists may be able to diagnose patients with neuropsychiatric conditions based on behavioral criteria functional brain imaging tools can inform the clinician of their underlying neurobiology Functional brain imaging can therefore provide clinicians with insightful information that enables them to narrow the differential diagnosis and to monitor and to evaluate any therapeutic benefit of the treatment 1 Single Photon Emission 1 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry precise clinical context given the extent of comorbidities present in many neuropsychiatric conditions Previous studies have demonstrated how SPECT can be utilized to diagnose psychiatric disorders 3 28 29 and to evaluate established treatments 4 30 32 The accurate diagnosis and treatment selection is complicated in psychiatry by complex cases and frequent comorbidities 2 However these conditions are increasingly benefitting from new treatment approaches including Transcranial Magnetic Stimulation TMS combinations of TMS with ketamine infusion CTK and Hyperbaric Oxygen Therapy HBOT with perispinal administration of etanercept PSE 33 36 TMS is a noninvasive technique for stimulation of the brain that can induce antidepressant and anti manic effects however treatment response can be slow 37 39 Ketamine is effective in reducing depressive symptoms 40 via multiple mechanisms of action including modulating signaling that stimulates neurogenesis and neuroplasticity as well as acting as a tumor necrosis factor TNF alpha inhibitor resulting in an anti inflammatory effect 41 43 CTK is a patented procedure and studies have indicated that CTK is an effective long term therapy for patients with various neuropsychiatric conditions whereby the coincident administration of ketamine allowed for higher TMS intensities than otherwise would be tolerated by patients 33 44 46 Treatment with HBOT followed by PSE has also been identified as a possible treatment for cognitive impairment 35 36 47 48 HBOT is believed to have anti inflammatory effects by reducing excess pro inflammatory cytokine activation such as TNF alpha and facilitates improvement by provocation of stem cell activity which can lessen the neurological impact of brain injuries 49 51 PSE injections modulate TNF alpha directly to the central nervous system and act to normalize the inflammatory response in stroke traumatic brain injury and encephalopathic conditions 52 Despite supportive evidence of the clinical utility of novel treatments such as CTK and HBOT with PSE further investigation of these combination treatments is required This article builds on the current literature and presents a retrospective review of a case series including six patients with complex neuropsychiatric presentations Baseline brain SPECT images were visually compared with SPECT images collected after periods of treatment with three novel treatments of CTK or HBOT followed by PSE during routine clinical practice In this article we also describe a novel SPECT imaging display technique present evidence of the clinical utility of CTK and HBOT with PSE and we propose that SPECT can be used as an imaging biomarker for monitoring and evaluating clinical change Computed Tomography SPECT is a functional brain imaging procedure that displays the functional status in the whole gray matter volume A radiotracer is administered to the patient and is transported via the bloodstream and is quickly removed through normal kidney excretion During circulation some radiotracer is taken up by the brain tissue with the uptake of radiotracer dependent on the regional cerebral blood flow rCBF The detection of the radiotracer uptake across the brain allows the clinician to identify areas of both underperfusion hypofunctioning and of hyperperfusion hyperfunctioning Brain SPECT also has the functionality to detect the presence of comorbidity that can occur due to a variety of causes including neurodevelopmental problems traumatic brain injury neuroinflammation non convulsive epilepsy neurotoxic exposure and nutritional deficiencies all of which contribute to altering the blood flow levels in various gray matter structures SPECT generates a three dimensional 3 D mapped representation of the brain that can be presented with colorcoded intensities proportional to rCBF and correlating with the function in that region Accurate and reliable visual interpretation of brain SPECT relies on optimizing the presentation of images using effective display tools and techniques which are demonstrated herein Diagnosis can also benefit from the complementary information exhibited by SPECT images displayed in a variety of formats including slices surfaces and volumes The optimal approach to accomplish accurate and efficient interpretation of brain imaging modalities is debated by researchers and clinicians in the literature 2 7 with discussions primarily centered on either conventional visual analysis by an experienced investigator and or quantification techniques including voxel wise analysis or region of interest ROI approaches 8 12 SPECT image quantification within clinical research typically identifies statistically significant differences based on mean group values which do not always equate to individual differences which is typically the focus in clinical practice 8 Therefore the visual interpretation of individual SPECT images remains a foundational skill within clinical practice and quantification is considered favorable for larger studies for identifying trends 8 13 However SPECT imaging is underutilized in clinical practice despite a growing evidence based foundation for its application in numerous indications relevant to psychiatric practice 14 23 This underutilization is particularly unfortunate as SPECT is an easy to perform non invasive procedure and remains among the least expensive neuroimaging tools available 24 25 The historic underutilization of neuroimaging techniques in psychiatry has also led to the consequential inadequate biological understanding of neuropsychiatric conditions 26 Without such biological understanding it is also difficult to identify meaningful biomarkers for diagnosis prognosis or risk which is particularly relevant as psychiatric treatments can lead to biological changes 24 26 27 In addition neuropsychiatric conditions are often diagnosed using a process of exclusion and additional information from brain SPECT imaging can complement the information gathered from clinical assessments Given the current underutilization of SPECT additional work is required to integrate the brain SPECT information in a more Frontiers in Psychiatry www frontiersin org MATERIALS AND METHODS Study Cases Six patients presented to our clinic with disabling neuropsychiatric conditions of various causes following extensive unsuccessful periods of treatments The conditions and comorbidities differed for each patient I VI Treatments were selected for each patient following the clinical assessment of the patient The six cases presented herein were purposefully 2 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry SPECT Imaging and Visual Analysis selected as they demonstrate the usefulness of brain SPECT imaging in evaluating patients with neuropsychiatric conditions and to monitor their response to treatment An overview of the patients their diagnosis and treatment are presented in Table 1 with more thorough details of patient histories selected treatments and outcomes presented in the Results section All subjects consented to the use of their data and information for the research purposes described herein Brain SPECT was carried out before baseline and after treatment for each patient A triple head gamma SPECT camera Picker Prism 3000XP equipped with low energy ultra high resolution LEUHR fan beam collimators was used to detect the uptake levels of the radiotracer 99mTcD L hexamethylene propylene amine oxime HMPAO which is correlated with rCBF and metabolic activity Reconstructions of multiparametric display were performed on the Picker Odyssey computer using filtered back projection and Chang attenuation correction 54 Once the final distribution is established post injection and without significant change for 2 3 h the visualization of the whole gray matter volume can be completed via a 3 D mapping of perfusion levels Visual analysis was performed by an expert nuclear medicine physician with over 30 years of experience in SPECT In the absence of a qualified biomarker 27 55 this study evaluates SPECT as an imaging biomarker based on the US Food and Drug Administration FDA monitoring biomarker definition 56 Monitoring biomarkers are analyzed at different time points to monitor the status of a disease or medical condition and as a marker of the response to an intervention 56 In this review the monitoring biomarker corresponds to the increase in brain perfusion detected with optimized displays of SPECT images before and after treatment For each patient the baseline SPECT images were compared with the post treatment SPECT images to assess the functional improvements across different areas of the brain The increased perfusion was detected using a purposefully designed discrete color scale DGP40 as a semi quantitative tool that assessed relative perfusion across different displays The distribution of the radiotracer within the brain was visualized in several ways during this study Firstly slicing whereby processing was based on reconstruction filtering reorientation and attenuation correction and led to three orthogonal cuts sagittal coronal and transaxial supplemented by a fourth axial display obtained along the temporal axis Secondly 3D stereotactic surface projections were obtained with the Neurostat software 57 Stereotactic surface projection is a technique used for the analysis of SPECT images to extract functional areas projected onto the brain surface for the visual representation of brain perfusion The discrete DGP40 color scale was applied to the orthogonal slice displays and the surface projection images to facilitate visualization of the level of perfusion The maximum perfusion in the image was scaled to 100 with each color band corresponding to a different level of perfusion as measured in steps of approximately 3 The threshold is set at 40 to suppress background noise Finally thresholded volumetric displays were used to create a surface that represents voxels of a constant value and are therefore also termed iso surface images The region of the brain with the highest uptake of radiotracer was used as the reference value the cerebellum in the majority of cases and a 67 threshold value relative to the reference value was applied to generate 3 D iso surface images with holes in Novel Treatment Options SPECT imaging was used to identify the extent and severity of hypoperfused areas which complemented the standard clinical assessment data collected Treatment decisions were based on the full baseline assessment and patients were either treated with CTK or HBOT followed by PSE The CTK procedure has been described in detail previously 9 Patients who present at our clinic with TRD are treated with CTK before or instead of electroconvulsive therapy ECT or TMS or ketamine administered independently based on evidence that CTK offers benefits over these established treatments for patients with TRD 33 46 In brief four patients treated with CTK received TMS 30 min and 5 min after the commencement of TMS intravenous infusions of the NMDA receptor inhibitor ketamine began 20 min The TMS 1 Hz was applied continuously for 30 min at a power output setting equivalent to 130 of motor threshold MT A biomarker dependent dosing strategy was applied whereby ketamine was gradually titrated in small increments until the patient entered a mildly cataleptic state Catalepsy refers to the neuromuscular condition characterized by muscular rigidity and fixity of posture regardless of external stimuli as well as markedly decreased sensitivity to pain Titrations began at 20 mg with an average dosage range of 0 4 2 3 mg kg full range from 0 2 to 4 7 mg kg Once the patient began to stiffen or posture the ketamine infusions could be discontinued Following the completion of the ketamine infusion the TMS would continue for a further 5 min after which the CTK procedure was complete Frequency of treatment is dependent on patient responsiveness typically 10 30 sessions Two patients who presented to this clinic with treatment refractory illness in the context of traumatic brain injury TBI or mild TBI mTBI were treated with HBOT followed by PSE Previous experiences of treating patients have indicated that the benefits of HBOT and PSE injection may be cumulative 53 HBOT treatments were administered daily in a multi place chamber for 60 min at a depth of 1 75 atmosphere absolute ATA After the first ten HBOT treatments one 25 mg PSE injection was administered approximately once weekly and the number of further HBOT sessions and PSE injections was tailored to the patient The method of perispinal administration of etanercept was used under license from the patent holder TACT IP LLC1 1 The method of perispinal administration of etanercept utilized was used under license from the patent holder TACT IP LLC Boca Raton FL USA TACT IP LLC claim methods of use of etanercept for the treatment of neurological disorders including but not limited to US patents 6419944 6537549 6982089 7214658 7629311 8119127 8236306 and 8349323 Frontiers in Psychiatry www frontiersin org 3 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry TABLE 1 Characteristics of patients with complex neuropsychiatric conditions n 6 with selected treatment Patient Age Sex Diagnosis Treatment I 62 F Treatment resistant depression TRD as well as grief and the effects of prolonged polypharmacy CTK II 34 F Regulatory disorder of childhood post head injury epilepsy reflex sympathetic dystrophy RSD HBOT and PSE III 54 M Childhood onset Tourettes long history of alcohol abuse severe depression fatigue and sleep apnea CTK IV 55 F Major depressive disorder MDD panic agoraphobia chronic back pain frequent headaches CTK V 77 M Dementia with major cognitive deficits and aphasia HBOT and PSE VI 43 M Bipolar II lifelong symptoms of depression anxiety impulsive behavior and family stressors CTK her daily life enthusiastic rational planning for future taking charge of her financial and family situation and a renewed religious sentiment the image corresponding to areas of the cortex with lower perfusion Since the images are continuous the threshold value of 67 was selected as it accentuated corresponding areas in the color images focused attention on hypoperfused areas and allowed for a better estimation of extent and severity A threshold of 67 was applied to the iso surface images shown herein In addition to the 67 threshold which depicts areas of hypoperfusion thresholds of 85 and 90 were also used to create iso surface images that visualized the size and location of areas of hyperperfusion The application of multiple thresholds allowed the visualization of hypo and hyper perfusion areas across the brain The clarity complementarity and user friendliness of these displays enabled a reliable visual evaluation before and after treatment Patient II HBOT and PSE Treatments A 34 year old female presented with lifelong symptoms of regulatory disorder of childhood two concussions post head injury epilepsy and reflex sympathetic dystrophy RSD These ultimately led to marked suffering and extreme disability in activities of daily living For almost 2 years the patient spent each day in a basement with dark glasses and protective hearing equipment due to intense photophobia and misophonia Prior to visiting our clinic the patient s medication history included over 30 types Baseline brain SPECT images for Patient II shown in the top line of Figure 2 indicated extensive diffuse bilateral hypoperfusion of the frontal more accentuated on the left temporal and orbitofrontal lobes and extended into the frontoparietal and parietal vertex areas Additionally there was bilateral hypoperfusion of the occipital lobes and hypoperfusion of the anterior cingulate in the dorsal aspect The patient had robust perfusion of the thalamus and basal ganglia There was also marked hyperperfusion in the cerebellar vermis HBOT was selected for patient II on account of multiple head injuries and a developmental history of a regulatory disorder Following 40 HBOT treatments brain SPECT images Figure 2 middle line indicated increased perfusion in most areas of the cortex and in some subcortical structures At a later stage PSE injections were started as another line of intervention PSE clinical injections were given at weekly intervals Following 4 PSE injections SPECT was performed and images shown in the bottom line of Figure 2 indicated major improvements increased perfusion in all lobes and subcortical areas Specifically the images showed increased perfusion in the orbito frontal and apico mesial temporal areas bilaterally and in the putamen bilaterally and in the mid thalamus In addition there was marked hyperperfusion in the mid posterior inferior occipital area and several areas of moderate cortical hyperperfusion in the lateral posterior aspect of both temporal lobes as well as in the posterior cingulate precuneus area Significantly these improvements were mirrored in the patient s cognition and ability to engage in daily acts of living RESULTS Patient I CTK Treatment A 62 year old female presented at the clinic on the verge of suicide The patient had worked as a nurse prior and following episodes of alcohol abuse The patient had a history of multiple medication trials and polypharmacy physical pain and prolonged family stressors sickness and eventual death of husband and intense grief The patient was classified as treatment non responsive following multiple treatment failures which were intended to address her suffering The patient s formal diagnoses were treatmentresistant depression TRD as well as grief and the effects of prolonged polypharmacy Baseline brain SPECT images for Patient I shown in the top line of Figure 1 indicated a marked and very extensive bilateral hypoperfusion involving all lobes at baseline and most accentuated on the right side The more extensive hypoperfusion were located in the lateral frontal frontoparietal and superior parietal areas There was marked hypoperfusion in the dorsal aspect of the anterior cingulate In the subcortical area there was slight bilateral striatum hyperperfusion and robust perfusion of the thalamus The patient was then treated with a total of 30 CTK sessions SPECT images were subsequently taken following 5 months of CTK treatment 58 sessions and are displayed in the bottom line of Figure 1 These images indicated a markedly improved perfusion across all cortical and subcortical structures These improvements corresponded with dramatic clinical improvement leading to major changes in Frontiers in Psychiatry www frontiersin org 4 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry FIGURE 1 Brain SPECT images from Patient I Top line images relate to brain SPECT images at baseline Bottom line images are taken following 5 months of CTK treatment The six images on each row from left to right include four stereotactic surface projections of the left lateral LLAT vertex underside and right lateral RLAT one iso surface image of the vertex and one axial slice Color coded intensity indicates hyperfunctioning areas blue hues and hypofunctioning areas white and black surrounded by white Images are presented as described in the Methods FIGURE 2 Brain SPECT images for Patient II Top line relates to brain SPECT images at baseline indicating extensive areas of hypofunctioning in all lobes Middle line shows SPECT images post HBOT treatment Bottom line of SPECT images collected post PSE treatment In each row from left to right one temporal axial image two orthogonal slices sagittal and axial one iso surface image of the vertex and two stereotactic surface projections of the left lateral LLAT and underside Frontiers in Psychiatry www frontiersin org 5 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry Patient III CTK Treatment his lifestyle completely at this stage SPECT imaging completed 14 months later as shown in the bottom line of Figures 3 and 4 indicated further significant improvements There were extensive areas of relative increase in blood flow in the lateral aspect of the left hemisphere and bilateral vertex area along with significantly improved perfusion in the orbitofrontal and apico mesial temporal areas Additionally there was increased perfusion in the left striatum and in the cerebellum These apparently minor improvements correlated with significant clinical improvements with the patient having resumed working part time job had significantly changed lifestyle with a stable marriage A 54 year old male emergency room ER nurse presented with childhood onset Tourettes and a long history of alcohol abuse severe depression fatigue and sleep apnea Baseline brain SPECT images for Patient III shown in the top line of Figures 3 and 4 indicated extensive bilateral hypoperfusion with this most accentuated in the left frontal lobe Additionally there was localized hypoperfusion in the occipital and frontal poles On the right side there were multiple localized and confluent areas of hypoperfusion that were more accentuated in part of the frontal lobe extending to the superior aspect of the parietal lobe including the vertex Marked hypoperfusion was also evidenced in the right striatum and right ventral striatum and the thalamus had an asymmetric appearance with localized areas of marked hypoperfusion in the posterior aspect There was moderate hyperperfusion in the anterior and posterior cingulate CTK treatment was selected and SPECT imaging was completed 5 months after the first CTK treatment middle line of Figures 3 and 4 SPECT indicated several improvements including in the area of severe frontal hypoperfusion at baseline Subsequently the patient continued with medication accepted continuous positive airway pressure CPAP treatment and changed his lifestyle Nonetheless he was still unable to change Patient IV CTK Treatment A 55 year old female presented with major depressive disorder MDD panic agoraphobia chronic back pain and frequent headaches The neurological exam did not indicate focal neurological dysfunction of the central nervous system Intermittently she had been treated with varied pharmacologic interventions and psychotherapy for 24 years before presenting to this clinic During that time the patient s symptoms did not respond to Wellbutrin Lexapro Abilify Viibryd Paxil Nardil Vicodin nor conventional psychotherapy Baseline brain SPECT images of Patient IV shown in the top line of Figure 5 indicated extensive bilateral hypoperfusion in the frontal lobes most accentuated on the left side including the dorsolateral prefrontal regions and in the parietal vertex bilaterally Not discernible in the images provided is the hypoperfusion in both orbitofrontal areas and in the mesial aspect of the right temporal lobe There was moderate hyperperfusion of the thalamus and marked hyperperfusion in the mid posterior inferior aspect of the occipital lobes The patient was treated with 30 CTK sessions and SPECT images shown in the bottom line of Figure 5 were taken 14 months thereafter Patient IV also received small amounts of anti panic medicine that was used judiciously The SPECT images indicated major bilateral perfusion improvement in the frontal conexities fronto parietal and anterior cingulate areas as well as bilateral increase in the basal ganglia Not discernible in the images provided is the significant improvement of the orbitofrontal areas There was also significantly increased perfusion in the thalamus and bilaterally in the striatum Following treatment the patient reported markedly improved symptoms major decrease of depression anxiety and back pain and greatly increased levels of life satisfaction At the two year follow up the patient had been practically free of suffering Patient V HBOT and PSE Treatment A 77 year old male presented with onset of dementia induced by general anesthesia with major cognitive physical and emotional impairments Immediately post knee replacement surgery the patient began to show dramatic cognitive physical and emotional impairment as compared with his pre surgical state these symptoms were still present when the patient arrived at our clinic 4 years post surgery Diagnoses of dementia with major cognitive deficits and aphasia was established FIGURE 3 Brain SPECT iso surface images for Patient III Top line relates to brain SPECT images at baseline Middle line shows SPECT images 5 months after the first CTK treatment Bottom line shows SPECT images 14 months following CTK treatment In each row from left to right three iso surface images of the left lateral LLAT vertex and right lateral RLAT Frontiers in Psychiatry www frontiersin org 6 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry FIGURE 4 Brain SPECT stereotactic surface projections for Patient III Top line relates to brain SPECT images at baseline Middle line shows SPECT images 5 months after the first CTK treatment Bottom line shows SPECT images 14 months following CTK treatment In each row from left to right six stereotactic surface projections of LLAT RLAT Vertex Underside right mod sagittal and left mid sagittal FIGURE 5 Brain SPECT images for Patient IV Top line relates to brain SPECT images at baseline Bottom line shows SPECT images 14 months following 30 sessions of CTK treatment In each row from left to right two stereotactic surface projections of the left lateral LLAT and vertex one iso surface image of the vertex one sagittal slice and two axial slices Involvement extended to parts of the dorsolateral prefrontal DLPF cortex There was also significant hypo perfusion in the temporal lobes more pronounced on the left and to a lesser Baseline brain SPECT images of Patient V shown in the top line of Figure 6 indicated extensive hemispheric hypoperfusion and multiple localized hypoperfusion in the left hemisphere Frontiers in Psychiatry www frontiersin org 7 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry extent in the orbitofrontal areas To address these cognitive physical and emotional impairments a treatment plan was prepared including a 40 session course of HBOT and PSE injections After the first 10 HBOT treatments the patient was administered 25 mg PSE injections approximately once weekly for 5 months At 5 months post treatment with HBOT and PSE SPECT images shown in the bottom line of Figure 6 showed an overall similar appearance to baseline However there were localized increases in perfusion as marked by the green arrows in parts of the anterior aspect of the prefrontal cortex including in the ventro mesial aspect right superior parietal right lateral occipital superior aspect of the left fronto parietal area posterior cingulate precuneus and apico mesial aspect of the right temporal In addition there was a significant increase in the striatum bilaterally Despite the follow up SPECT remaining abnormal the improved perfusion in small areas specifically the mesial temporal lobe prefrontal cortex ventro mesial frontal posterior cingulate precuneus and dorsal parietal are known to be key in contributing to memory cognition and behavior Indeed initiating after the first PSE injection the patient began showing progressive clinical improvements in cognitive and physical function A follow up visit 16 months after the end of treatment showed that the same level of clinical improvement had been maintained To further display the utility of SPECT as an evaluative biomarker Figure 8 displays iso surface images clearly indicating the increased perfusion following CTK treatment in almost all previously hypoperfused areas DISCUSSION This article describes a novel display technique for SPECT images and provides readers with six case study examples that demonstrate how brain SPECT imaging can be used both as a complementary diagnostic tool and as a potential biomarker for monitoring and evaluating novel treatments for patients with complex neuropsychiatric conditions Developing and applying clinical tools such as SPECT imaging can provide the clinician with complementary insights into the underlying neurobiology to standard clinical assessments However as SPECT imaging continues to be underutilized in clinical practice more practical evidence guidance and studies such as this one are required to demonstrate how SPECT can be utilized to evaluate the patient and to inform the clinician In this retrospective review six patients presented with complex neuropsychiatric conditions and comorbidities following extensive unsuccessful periods of different treatments While experienced psychiatrists may be able to diagnose patients with neuropsychiatric conditions based on behavioral criteria functional brain imaging tools can inform the clinician of their underlying neurobiology Additionally the examination of different functional areas of the brain using SPECT imaging may provide insights into the patients status that may not identifiable during clinical assessment Particularly in cases of diagnostic dilemma such as those presented herein SPECT images were used to identify areas of hypo and hyper perfusion to complement the initial clinical assessment In the cases presented herein the improved perfusion identified in the post treatment SPECT images whether extensive or localized were mirrored by particular clinical improvements Therefore it is fundamental for the clinician to understand how clinical improvements manifest in the patients underlying neurobiology This case series effectively demonstrates the importance for the clinician to combine clinical assessments evaluating presenting behaviors and symptoms with the underlying neurobiology attainable using SPECT imaging Furthermore building a database that correlates SPECT images with clinical assessments has the potential to develop more targeted treatments and to establish effective biomarkers In these complex cases high quality SPECT images provided valuable insights into the underlying neurobiological status of patients allowing the clinician to narrow the differential diagnosis A high quality brain SPECT will provide detailed information about the location magnitude and extent of areas of hyper and or hypoperfusion s The clinical efficacy of brain SPECT for the monitoring of patients with multiple co morbidities and treatment resistant conditions is greatly enhanced by a standardized comprehensive display of the results This includes a user friendly color multi parametric set of 2D and 3D images Consistency is also critically important not Patient VI CTK Treatment A 43 year old male presented with bipolar II lifelong symptoms of depression anxiety impulsive behavior and family stressors Specifically the patient reported struggling with intense depressed mood substantial life stress including a divorce in progress and the inability to hold a job due to the impairment and distress associated with his symptoms He had received psychopharmacological and psychotherapeutic treatment for the previous 6 years but without improvement Baseline brain SPECT images of Patient VI shown in the top line of Figure 7 indicated hypoperfusion in multiple hemispheric areas most pronounced in the frontal lobes anterior cingulate orbitofrontal and apico mesial areas of the temporal lobes Hyperperfusion was indicated in the right putamen and in parts of the posterior cingulate and right cerebellum and vermis This combination of hypoperfused areas is commonly associated with dysfunctions related to memory executive function social interaction and impulse control and the hyperperfused areas are often associated with anxiety and depression 58 59 Based on the initial assessment CTK treatment was selected and the patient received a total of 24 sessions over 5 months SPECT was performed 5 months after the first CTK treatment and images are displayed in the bottom line of Figure 6 Images indicated significantly improved relative perfusion in almost all previously under perfused areas Previously hyperperfused areas were either unchanged or increasingly hyperperfused The patient also reported substantial improvements in symptoms related to functioning and psychometric assessments showed substantial decreases in symptoms related to both depression and mania Frontiers in Psychiatry www frontiersin org 8 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry FIGURE 6 Brain SPECT images for Patient V Top line relates to brain SPECT images at baseline Bottom line shows SPECT images 5 months post treatment with HBOT and PSE Green arrows indicate areas of increased perfusion In each row from left to right one axial slice and one temporal slice three stereotactic surface projections of the right lateral RLAT left lateral LLAT and right sagittal and one iso surface image of the underside FIGURE 7 Brain SPECT images for Patient VI Top line relates to brain SPECT images at baseline Bottom line shows SPECT images 5 5 months following 24 sessions of CTK treatment In each row from left to right one temporal slice one sagittal slice and one axial slice and three stereotactic surface projections of the underside right lateral RLAT and left lateral LLAT of the presentation of images using effective display tools and techniques In the clinical cases presented we have demonstrated that the optimization of images using a novel set of display tools facilitated the visual interpretation of SPECT imaging data by expert clinicians without the need for quantification or statistical analysis A more detailed description of this display will be published shortly 62 In the absence of a qualified biomarker 27 55 this study evaluates SPECT as an imaging biomarker based on the US Food and Drug Administration FDA monitoring biomarker only in the execution of the procedure itself but also in the processing and display of the images Whilst quantification of SPECT images may facilitate readers with limited experience to interpret SPECT scans and aid in the identification of trends 60 61 it is imperative to also recognize any limitations of such quantitative analysis of imaging techniques particularly within clinical practice and during the assessment of individual cases 8 The visual assessment of SPECT images pertaining to individual cases remains a foundational skill within clinical practice the accuracy and reliability of which relies on the optimization Frontiers in Psychiatry www frontiersin org 9 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry FIGURE 8 Iso surface SPECT images for Patient VI Top line relates to brain SPECT images at baseline and bottom line are brain SPECT images 14 months after CTK treatment began In each row from left to right are iso surface images of the anterior posterior left lateral LLAT vertex underside and right lateral RLAT relative perfusion in previously hypoperfused areas which correlated to the clinical improvements noted for each patient These cases thereby provide further evidence of the clinical utility of these novel treatments for patients with complex neuropsychiatric conditions Despite the growing evidence based foundation for the application of SPECT in numerous indications relevant to psychiatric practice there is a need for clinicians to utilize this powerful tool and contribute to our understanding of the neurobiology relating to different neuropsychiatric conditions and comorbidities Greater biological understanding will result in the identification of meaningful biomarkers for diagnosis prognosis or risk and can further aid the clinician in their evaluation of a patient before and after treatments There is a particular value in sharing methodologies and results regarding the implementation of SPECT in routine practice in clinical settings This retrospective review demonstrated that brain SPECT imaging could represent a potential imaging biomarker since syndrome status was correlated with changes in the perfusion pattern detected Given the display modalities used the relative perfusion assessment with SPECT imaging before and after treatment has acted as a monitoring biomarker that indicated the therapeutic benefit of the novel types of treatments used in this case series Furthermore SPECT images have provided additional information that explains the functional changes that gave rise to the observed clinical improvements This understanding of the topographic functional status is important if we are to further progress to personalized targeted treatments and the development of effective biomarkers This article has some limitations First these cases represent assessments carried out during routine clinical practice and not as part of a pre planned study therefore there is a small number of cases presented without a normalized reference cohort and definition 56 A monitoring biomarker is defined as a biomarker measured repeatedly for assessing status of a disease or medical condition or for evidence of exposure to or effect of a medical product or an environmental agent 56 In this review the monitoring biomarker corresponds to the increase in brain perfusion detected with optimized displays of SPECT images before and after treatment Following treatment all patients demonstrated improvements measured via periodic clinical evaluations and in some cases neuropsychological testing and detailed observations from family members These clinical improvements were also apparent from the increased perfusion evident in the brain SPECT images collected posttreatment compared with those collected at baseline Whilst clinical improvements following treatment may be discernible during standard clinical assessment SPECT was used as a monitoring biomarker to indicate the underlying neurobiological response of each individual to the treatment intervention In this case series SPECT images indicated the specific areas of improved brain perfusion that resulted following treatment and provided additional context to the clinical improvements identified Therefore the SPECT images provided insights into the functioning status of the patient in addition to monitoring symptoms during clinical assessment These follow up scans thereby informed how these novel treatments affected the underlying neurobiology of each individual and how perfusion improvements in specific areas correlated to clinical improvements The application of SPECT imaging as a monitoring biomarker also further contributes to the understanding and the growing literature that describes the clinical utility of these novel treatments for patients with neuropsychiatric conditions In this case series intervention with novel treatments of CTK or HBOT and PSE resulted in marked improvements in Frontiers in Psychiatry www frontiersin org 10 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry DATA AVAILABILITY STATEMENT physicians were not blinded to the clinical context however this does reflect a practical clinical routine Overall this collection of these case studies further substantiates the clinical relevance of brain SPECT imaging in psychiatry and neuropsychiatry This review demonstrates that SPECT imaging can be a valuable tool in cases of diagnostic dilemma and can complement standard assessment techniques and diagnostic tools In our study six patients with complex neuropsychiatric conditions and comorbidities were successfully treated which contributes to the growing literature indicating the clinical utility of the novel therapies of CTK and HBOT with PSE 33 47 The positive outcomes for these patients were facilitated by the detailed initial evaluation of patients that included baseline SPECT imaging that complemented the standard clinical assessment The repetitious clinical approach the novel display technique and positive treatment outcomes in these six cases has also demonstrated how image optimization and visual analysis of SPECT images can be utilized during clinical assessments of individual cases Finally we demonstrated how SPECT images recorded before and after treatment provided valuable insights into the improved neurobiological status of these patients in response to intervention Therefore we argue that perfusion assessed with SPECT images before and after treatment can be used as an imaging biomarker for monitoring evaluating and explaining clinical change The datasets presented in this article are not readily available because HIPAA protected data Requests to access the datasets should be directed to srdbest neuroscience md ETHICS STATEMENT Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements The patients participants provided their written informed consent to participate in this study Written informed consent was obtained from the individual s for the publication of any potentially identifiable images or data included in this article AUTHOR CONTRIBUTIONS SB provided the CTK HBOT and PSE treatments as well as integrated the psychiatric and SPECT data NH co wrote the article and contributed to the discussion of the results DP performed the SPECT imaging as well as analyzed and interpreted the SPECT data Please note that DP sadly passed away during the finalization of this manuscript however all other authors read and approved the final manuscript ACKNOWLEDGMENTS AUTHOR S NOTE This article would not have been possible without the pioneering work of DP who sadly passed away during the finalization of this manuscript This paper is dedicated to his memory The authors would also like to acknowledge Simon DeBruin of Good Lion Imaging for the image processing that resulted in the impressive and clear images displayed herein Proper execution of a brain SPECT scan is an art and requires great attention to detail in order to obtain high quality images such as the ones presented here For specific information regarding imaging and processing protocols please contact the authors directly REFERENCES 7 Nishimiya M Matsuda H Imabayashi E Kuji I Sato N Comparison of SPM and NEUROSTAT in voxelwise statistical analysis of brain SPECT and MRI at the early stage of Alzheimer s disease Ann Nucl Med 2008 22 921 7 doi 10 1007 s12149 008 0211 7 8 Catafau AM Brain SPECT in Clinical Practice Part I Perfusion J Nucl Med 2001 42 259 71 9 Coburn KL Lauterbach EC Boutros NN Black KJ Arciniegas DB Coffey CE 2006 The value of quantitative electroencephalography in clinical psychiatry a report by the committee on research of the American neuropsychiatric association J Neuropsychiatry Clin Neurosci 2006 18 460 500 doi 10 1176 jnp 2006 18 4 460 10 Evans JR Budzynski TH Budzynski HK Abarbanel A Introduction to Quantitative EEG and Neurofeedback Advanced Theory and Applications USA Academic Press 2009 11 Hoffman DA Lubar JF Thatcher RW Sterman MB Rosenfeld PJ Striefel S et al Limitations of the American Academy of Neurology and American Clinical Neurophysiology Society Paper on QEEG J Neuropsychiatry Clin Neurosci 1999 11 401 7 doi 10 1176 jnp 11 3 401 12 Hughes JR John ER Conventional and Quantitative Electroencephalography in Psychiatry J Neuropsychiatry Clin Neurosci 1999 11 190 208 doi 10 1176 jnp 11 2 190 13 Huang C Eidelberg D Habeck C Moeller J Svensson L Tarabula T et al 2007 Imaging markers of mild cognitive impairment 1 Henderson T van Lierop M McLean M Uszler JM Thornton J Siow Y Functional neuroimaging in psychiatry aiding in diagnosis and guiding treatment what the american psychiatric association does not know Front Psychiatry 2020 11 276 doi 10 3389 fpsyt 2020 0027 2 Taber KH Hurley RA Yudofsky SC Diagnosis and treatment of neuropsychiatric disorders Annu Rev Med 2010 61 121 33 doi 10 1146 annurev med 051408 105018 3 Richieri R Boyer L Faget Agius C Farisse J Mundler O Lan on C et al 2015 Determinants of brain SPECT perfusion and connectivity in treatment resistant depression Psychiatry Res 2014 231 134 40 doi 10 1016 j pscychresns 2014 11 013 4 Escobar R Rios A Montoya ID Lopera F Ramos D Carvajal C et al Clinical and cerebral blood flow changes in catatonic patients treated with ECT J Psychosom Res 2000 49 423 9 doi 10 1016 S0022 3999 00 00 190 2 5 Ito H Kawashima R Awata S Ono S Sato K Goto R et al Hypoperfusion in the limbic system and prefrontal cortex in depression SPECT with anatomic standardization technique J Nucl Med 1996 37 410 4 6 Dougherty DD Rauch SL Brain correlates of antidepressant treatment outcome from neuroimaging studies in depression Psychiatr Clin North Am 2006 30 91 103 doi 10 1016 j psc 2006 12 007 Frontiers in Psychiatry www frontiersin org 11 January 2022 Volume 12 Article 713141
Best et al 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 Brain SPECT Biomarker Treatment Psychiatry 32 Raji CA Tarzwell R Pavel D Schneider H Uszler M Thornton et al Clinical utility of SPECT neuroimaging in the diagnosis and treatment of traumatic brain injury a systematic review PLoS ONE 2014 9 e91088 doi 10 1371 journal pone 0091088 33 Best SRD Pavel DG Haustrup N Combination therapy with transcranial magnetic stimulation and ketamine for treatment resistant depression a long term retrospective review of clinical use Heliyon 2019 5 e02187 doi 10 1016 j heliyon 2019 e02187 34 Griffiths C O Neill Kerr A de Vai R Sore T da Silva K Ketamine infusion KI in treatment resistant depression TRD retrospective clinical data analysis Open J Depress 2019 8 59 70 doi 10 4236 ojd 2019 83007 35 Marcinkowska AB Mankowska ND Kot J Winklewski PJ Impact of hyperbaric oxygen therapy on cognitive functions a systematic review Neuropsychol Rev 2021 doi 10 1007 s11065 021 09500 9 Epub ahead of print 36 Tobinick E Perispinal etanercept a new therapeutic paradigm in neurology Expert Rev Neurother 2010 10 985 1002 doi 10 1586 ern 10 52 37 Fitzgerald PB Hoy KE Elliot D McQueen SRN Wambeek LE Daskalakis ZJ Accelerated repetitive transcranial magnetic stimulation in the treatment of depression Neuropsychopharmacology 2018 43 1565 72 doi 10 1038 s41386 018 0009 9 38 O Reardon JP Solvason HB Janicak PG Sampson S Isenberg KE Nahas Z et al Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression a multisite randomized controlled trial Biol Psychiatry 2007 1 1208 16 doi 10 1016 j biopsych 2007 01 018 39 Perera T George MS Grammer G Janicak PG Pascual Leone A Wirecki TS The clinical TMS society consensus review and treatment recommendations for TMS therapy for major depressive disorder Brain Stimul 2016 9 336 46 doi 10 1016 j brs 2016 03 010 40 Singh JB Fedgchin M Daly E Xi L Melman C Bruecker D et al Intravenous esketamine in adult treatment resistant depression a double blind doublerandomization placebo controlled study Biol Psychiatry 2016 80 424 31 doi 10 1016 j biopsych 2015 10 018 41 Xie Z M Wang X M Xu N Wang J Pan W Tang XH et al Alterations in the inflammatory cytokines and brain derived neurotrophic factor contribute to depression like phenotype after spared nerve injury improvement by ketamine Sci Rep 2017 7 3124 doi 10 1038 s41598 017 03590 3 42 Martin JL Finsterwald C Cooperation between BDNF and glutamate in the regulation of synaptic transmission and neuronal development Commun Integr Biol 2011 4 14 6 doi 10 4161 cib 13761 43 Zanos P Mechanisms of ketamine action as an antidepressant Mol Psychiatry 2018 23 801 11 doi 10 1038 mp 2017 255 44 Best SRD Treatment of Thalamocortical Dysrhythmia World Intellectual Property Organization Patent No WO2014081948A1 International Bureau Virginia Commission for patents 2014 45 Best SRD Treatment of thalamocortical dysrhythmia U S Patent No US8974365B2 Washington DC Patent US and Trademark Office 2015 46 Best SRD Combined ketamine and transcranial magnetic stimulation for treatment resistant depression in the context of chronic OCD a case report Neuropsychiatric Electrophysiology 2015 1 2 doi 10 1186 s40810 015 0003 y 47 Best SRD Treatment of post anesthesia dementia with perispinal etanercept injection and hyperbaric oxygen therapy a case report J Med Case Rep 2017 11 doi 10 1186 s13256 017 1259 6 48 Tobinick E Rodriguez Romanacce H Levine A Ignatowski TA Immediate neurological recovery following perispinal etanercept years after brain injury Clin Drug Investig 2014 34 361 6 doi 10 1007 s40261 014 0186 1 49 Gonzales Portillo B Lippert T Nguyen H Lee JY Hyperbaric oxygen therapy A new look on treating stroke and traumatic brain injury Brain circulation 2019 5 101 5 doi 10 4103 bc bc_31_19 50 Golden Z Golden CJ Neubauer RA Improving neuropsychological function after chronic brain injury with hyperbaric oxygen Disabil Rehabil 2006 28 1379 86 doi 10 1080 09638280600638364 51 Huang L Obenaus A Hyperbaric oxygen therapy for traumatic brain injury Med Gas Res 2011 1 21 doi 10 1186 2045 9912 1 21 52 Tobinick E Perispinal etanercept advances as a neurotherapeutic Expert Rev Neurother 18 453 455 doi 10 1080 14737175 2018 1468253 Multivariate analysis of CBF SPECT Neurobiol Aging 2006 28 1062 9 doi 10 1016 j neurobiolaging 2006 05 017 Amen DG Trujillo M Newberg A Willeumier K Tarzwell R Wu JC et al Brain SPECT imaging in complex psychiatric cases an evidence based underutilized tool Open Neuroimaging J 2011 5 40 8 doi 10 2174 1874440001105010040 Amen DG Raji CA Willeumier K Taylor D Tarzwell R Newberg A et al Functional neuroimaging distinguishes posttraumatic stress disorder from traumatic brain injury in focused and large community datasets PLoS ONE 2015 10 e0129659 doi 10 1371 journal pone 0129659 Cohen PF Tarzwell R Numerow L Siow Y H Uszler JM et al CANM Guidelines For Brain Perfusion Single Photon Emission Computed Tomography SPECT Canadian Association of Nuclear Medicine 2021 Available online at https canm acmn ca guidelines accessed October 22 2021 Estudillo Guerra MA Pacheco Barrios K Cardenas Rojas A AdameOcampo G Camprodon JA Morales Quezada L Brain perfusion during manic episode and at 6 month follow up period in bipolar disorder patients Correlation with cognitive functions Brain Behav 2020 10 e01615 doi 10 1002 brb3 1615 Henderson T Cohen P van Lierop M Thornton J McClean M Uszler J et al A reckoning to keep doing what we are already doing with PET and SPECT functional neuroimaging Am J Psychiatry 2020 177 637 8 doi 10 1176 appi ajp 2020 19080801 Henderson T van Lierop M McLean M Uszler JM Thornton J Siow Y et al Functional Neuroimaging in Psychiatry Aiding in diagnosis and guiding treatment What the American Psychiatric Association does not know Front Psychiatry 2020 11 276 doi 10 3389 fpsyt 2020 00276 Raji CA Willeumier K Taylor DT Functional neuroimaging with default mode network regions distinguishes PTSD from TBI in a military veteran population Brain Imaging Behav 2015 9 527 34 doi 10 1007 s11682 015 9385 5 Pavel DG Best SRD Brain SPECT as Imaging Biomarker for Evaluating Effects of Novel Treatments in Psychiatry J Nucl Med 2017 58 supplement 1 1298 Walker Z Moreno E Thomas A Inglis F Tabet N Rainer M et al Clinical usefulness of dopamine transporter SPECT imaging with 123I FP CIT in patients with possible dementia with Lewy bodies Randomised study Br J Psychiatry 2018 206 145 52 doi 10 1192 bjp bp 114 148643 Yeo JM Lim X Khan ZP Systematic review of the diagnostic utility of SPECT imaging in dementia Eur Arch Psychiatry Clin Neurosci 2013 263 539 52 doi 10 1007 s00406 013 0426 z Guinane J Ng BL Clinical utility of MRI and SPECT in the diagnosis of cognitive impairment referred to memory clinic Int Psychogeriatr 2018 30 611 7 doi 10 1017 S1041610217001624 Henderson TA The diagnosis and evaluation of dementia and mild cognitive impairment with emphasis on SPECT perfusion neuroimaging CNS Spectr 2012 17 176 206 doi 10 1017 S1092852912000636 Milham MP Craddock RC Klein A Clinically useful brain imaging for neuropsychiatry How can we get there Depress Anxiety 2017 34 578 87 doi 10 1002 da 22627 Abi Dargham A Horga G The search for imaging biomarkers in psychiatric disorders Nat Med 2016 22 1248 55 doi 10 1038 nm 4190 Camargo EE Brain SPECT in neurology and psychiatry J Nucl Med 2001 42 611 23 Li J Yang Y Zhu Y Zhou L Han Y Yin T et al Towards characterizing the regional cerebral perfusion in evaluating the severity of major depression disorder with SPECT CT BMC Psychiatry 2018 18 70 doi 10 1186 s12888 018 1654 6 Karada g F Kalkan Oguzhanoglu N Y ksel D Kira S Cura zdel O et al The comparison of pre and post treatment 99mTc HMPAO brain SPECT images in patients with obsessive compulsive disorder Psychiatry Res 2013 213 169 177 doi 10 1016 j pscychresns 2012 07 005 Mottaghy FM Keller CE Gangitano M Ly J Thall M Parker JA et al Correlation of cerebral blood flow and treatment effects of repetitive transcranial magnetic stimulation in depressed patients Psychiatry Res 2002 115 1 14 doi 10 1016 S0925 4927 02 00032 X Frontiers in Psychiatry www frontiersin org 12 January 2022 Volume 12 Article 713141
Best et al Brain SPECT Biomarker Treatment Psychiatry 53 Tobinick EL Use and methods of use of etanercept and other TNF binding biologics to improve human cognitive function United States Patent No US20060009450A1 Washington DC Patent US and Trademark Office 2006 54 Chang LT A method for attenuation correction in radionuclide computed tomography IEEE Transactions on Nuclear Science 1978 25 638 43 doi 10 1109 TNS 1978 4329385 55 Botteron K Carter C Castellanos FX Dickstein DP Drevets W Kim KL et al Consensus Report of the APA Work Group on Neuroimaging Markers of Psychiatric Disorders Am Psychiatr Assoc Ed Arlington VA USA 2012 56 FDA NIH Biomarker Working Group BEST Biomarkers EndpointS other Tools Monitoring Biomarker Food and Drug Administration US and National Institutes of Health US 2016 Availabble online at https www ncbi nlm nih gov books NBK402282 accessed January 25 2021 57 Minoshima S Koeppe RA Frey KA K DE Anatomic standardization linear scaling and nonlinear warping of functional brain images J Nucl Med 1994 35 1528 37 58 Pliszka SR Glahn DC Semrud Clikeman M Franklin C Perez III Xiong R et al Neuroimaging of inhibitory control areas in children with attention deficit hyperactivity disorder who were treatment naive or in long term treatment Am J Psychiatry 2006 163 1052 1060 doi 10 1176 ajp 2006 163 6 1052 59 Sheehan W Thurber S Review of two years of experiences with SPECT among psychiatric patients in a rural hospital setting J Psychiatr Pract 2008 14 318 23 doi 10 1097 01 pra 0000336760 88178 e5 60 Booij J Dubroff J Pryma D Yu J Agarwal R Lakhani P et al Diagnostic performance of the visual reading of 123 I Ioflupane SPECT images with or without quantification in patients with movement disorders or dementia J Nucl Med 2017 58 1821 6 doi 10 2967 jnumed 116 189266 61 M kinen E Joutsa J Johansson J M ki M Sepp nen M Kaasinen V Visual versus automated analysis of I 123 FP CIT SPECT scans in parkinsonism Frontiers in Psychiatry www frontiersin org J Neural Transm Suppl 2016 123 1309 18 doi 10 1007 s00702 0161586 6 62 McLean M Henderson TA Pavel DG Cohen P Increase asymmetric perfusion of the cerebral cortices and thalamus indicates individuals at risk for bipolar disorder a family Cohort SPECT neuroimaging study Front Psychiatry 2021 Conflict of Interest NH has since become an employee of Eli Lilly and Company SB holds multiple patents claiming methods of use of CTK for treatment of neurological disorders The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest The handling editor TH declared a past co authorship collaboration with one of the authors DP Publisher s Note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations or those of the publisher the editors and the reviewers Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher Copyright 2022 Best Haustrup and Pavel This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY The use distribution or reproduction in other forums is permitted provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited in accordance with accepted academic practice No use distribution or reproduction is permitted which does not comply with these terms 13 January 2022 Volume 12 Article 713141
Pretreatment with Hyperbaric Oxygen and its effect on neuropsychometric dysfunction and systemic inflammatory response after cardiopulmonary bypass 1 J Thorac Cardiovasc Surg 2005 Dec 130 6 1623 30 Epub 2005 Oct 26 Alex J Laden G Cale AR Bennett S Flowers K Madden L Gardiner E McCollum PT Griffin SC Department of Cardiothoracic Surgery Castle Hill Hospital United Kingdom OBJECTIVE Animal studies have shown that pretreatment with Hyperbaric Oxygen can induce central nervous system ischemic tolerance and also modulate the inflammatory response We evaluated this therapy in patients undergoing cardiopulmonary bypass METHODS Sixty four patients were prospectively randomized to group A n 31 atmospheric air 1 5 atmospheres absolute or group B n 33 hyperbaric oxygen 2 4 atmospheres absolute before on pump coronary artery bypass grafting Age sex body mass index diabetes hypertension smoking coronary disease severity left ventricular function Parsonnet score Euroscore bypass time myocardial ischemia time and number of grafts were comparable in both groups Canadian Cardiovascular Society angina New York Heart Association dyspnea and previous myocardial infarction were significantly higher in group B Inflammatory markers were analyzed before surgery and 2 and 24 hours after bypass Neuropsychometric testing was performed 48 hours before surgery and 4 months after surgery and included trail making A and B the Rey auditory verbal learning test grooved peg board information processing table A and digit span forward and backward Neuropsychometric dysfunction was defined as more than 1 SD deterioration in more than 2 neuropsychometric tests Chi square tests Fisher tests t tests and analysis of variance were used as appropriate for statistical analysis RESULTS Group A had a significant postoperative increase in the inflammatory markers soluble E selectin CD18 and heat shock protein 70 This was not observed in group B Neuropsychometric dysfunction was also significantly higher in group A compared with group B There was no difference in any other early postoperative clinical outcome CONCLUSIONS Our results seem to indicate that pretreatment with Hyperbaric Oxygen can reduce neuropsychometric dysfunction and also modulate the inflammatory response after cardiopulmonary bypass HYPERBARIC OXYGEN IN THE TREATMENT OF THE POSTOPERATIVE LOW CARDIAC OUTPUT SYNDROME M H YACOUB M B Cairo F R C S F R C S E F R C S G SENIOR SURGICAL REGISTRAR G L ZEITLIN M B Cantab F F A R C S SENIOR ANAESTHETIC REGISTRAR LONDON CHEST HOSPITAL LONDON E 2 It has been our experience that patients who develop the low cardiac output syndrome in association with pulmonary hypertension after cardiac surgery seldom recover despite vigorous treatment We report here the case of a patient who was successfully treated by means of hyperbaric oxygen therapy Case report a 50 yr old man was admitted to the London Chest Hospital on Oct 23 1964 He had a history of productive cough recurrent haemoptysis and dyspnoea on exertion for 21 years He had been discharged from the Army 20 years before with mitral valve disease Mr J R Belcher performed the operation on Nov 3 1964 after the operation the patient displayed all the signs of a low cardiac output failure to recover consciousness with no localizing cerebral signs severe peripheral cyanosis and a very slow capillary refill in the limbs Since the patient s condition was now desperate it was decided to use hyperbaric oxygen therapy He was placed in the Vickers mobile chamber at a pressure of 2 atmospheres absolute Since there were no facilities in the chamber for artificial respiration transfusion or drainage these had to be discontinued
The patient s condition began to improve after an hour inside the chamber he was taken out of it every 2 hours to aspirate from his bronchial tree the considerable amount of heavily bloodstained sputum After 12 hours treatment he began to move and gradually recovered consciousness for the first time since the operation Summary and Conclusions In the immediate postoperative period after mitral valvotomy a patient who had shown signs of pulmonary hypertension preoperatively and a raised pulmonary artery pressure at thoracotomy displayed all the signs of low cardiac output In an attempt to lower the pulmonary vascular resistance and raise the cardiac output he was artificially ventilated with 100 oxygen This was ineffective and the patient s death seemed certain Hyperbaric oxygen treatment was then instituted Within an hour his condition began to improve and though artificial ventilation pleural drainage endotracheal suction and intravenous therapy were not feasible he continued to improve while in the chamber This case suggests that hyperbaric oxygen therapy helps to support life during the critical period of post operative low cardiac output in patients with pulmonary hypertension and justifies further trial of the technique in similar cases Abstracted from the Lancet March 13th 1965 pages 581 583 Yacoub is now Prof Sir MH Yacoub N B The patient was treated in an ambulance in the car park of the hospital Philip James M D Wolfson Hyperbaric Medicine Unit The University of Dundee 1999 Cardiac arrest of 30 minutes with defibrillation Male aged 46 had a cardiac arrest in the community Defibrillated by paramedics after about 30 minutes Admitted to CCU and opened his eyes after three days He began to say single words on day 5 Transferred to general ward on day 6 Gradually declined over 5 weeks with the development of spastic paraplegia despite daily physiotherapy Prescribed His leg spasticity became so severe that it was very difficult to bend his legs to allow him to use a wheelchair His arms were also developing mild stiffness He had periods in which he spoke20 words clearly but they made little sense He recognized his family Hyperbaric oxygen therapy was started after 5 weeks 54 daily one hour hyperbaric oxygen sessions were undertaken at 1 75 atm abs His cognition and speech improved and there was dramatic improvement in his spasticity He left hospital walking without assistance Comment This illustrates Ischemia with mid brain edema Giving high dosage oxygen post arrest would on present evidence have prevented the associated the reperfusion injury and spared some of the cortical damage Philip James M D Wolfson Hyperbaric Medicine Unit University of Dundee Hyperbaric Oxygen and Your Heart by Medical Journalist Morton Walker D P M USA
What s the first treatment an emergency room doctor would administer to you if you were wheeled into the E R with angina pain or a heart attack After evaluating my question if your answer is An oxygen mask you are correct In angina pectoris you have a literal suffocation of the heart It simply isn t getting the oxygen it needs because of an insufficient blood supply that ordinarily carries cellular oxygen molecules This deficiency can be from blocked arteries heading toward the heart or from a temporary vasoconstriction of those same arteries as occurs in stress In a heart attack there is an occlusion also due to blockage or constriction but such clogging involves the coronary arteries which actually feed the heart muscle This lake of nourishing blood to the pumping muscle most commonly leads to myocardial infarction development of a dead part within the heart and could very well result in the victim s death Recognition of oxygen s physiological importance is age old knowledge but only recently has medical science provided us with guidelines as to how much and when Simple cause and effect has been the basis of most of our past wisdom For example we feel better when we exercise increasing our oxygen intake Today many doctors are utilizing hyperoxia forcefully increasing oxygen intake by use of an oxygen O2 mask or chamber as a part of their overall therapy in reversing or treating heart disease There are perhaps only two main reasons why all doctors aren t routinely using pressurized oxygen hyperbaric oxygen therapy HBOT First is ignorance as to its efficacy for a wide variety of ailments and second is the unavailability of hyperbaric medicine chambers for the delivery of oxygen under pressure Cardiac Therapy After being exposed to the pioneering work of hyperbaricist George Hart MD at the American Heart Association s AHA 65th Scientific Session held in New Orleans on November 16 1992 the AHA issued a press release praising the use of hyperbaric oxygen to boost emergency treatment for heart attack It advised medical journalists that hyperbaric oxygen HBO as treatment enhances clot dissolving drugs ability to minimize heart damage and save the lives of heart attack patients The addition of HBOT resulted in earlier relief of chest pain and electrocardiogram ECG changes toward normal in patients treated with the clot dissolver tissue plasminogen activator TPA HBOT also tended to preserve more of the heart s blood pumping capacity compared to treatment with TPA alone said Myrvin H Ellestad MD director of research at the Memorial Heart Institute at Long Beach Memorial Medical Center in Long Beach California Laboratory studies have shown that hyperbaric oxygen minimizes cell damage and death by reducing fluid accumulation in the injured cells We believe the same thing happens in patients said Dr Ellestad In heart attacks sort of the last straw that kills cells is increasing cell water which finally breaks the cell membrane We believe hyperbaric oxygen s primary effect in heart attack may be to reduce edema fluid accumulation in heart cells The Long Beach group studied forty six heart attack patients twenty two of whom received only TPA The remaining twenty four patients got TPA followed by two hours of treatment in a hyperbaric chamber It provided a pure oxygen environment with twice the normal atmospheric pressure two atmospheres absolute Patients treated with HBOT felt chest pain relief an average of 271 minutes after the onset of heart attack symptoms a statistically significant difference compared to the 671 minutes for patients who received only TPA Dr Ellestad said patients generally reported an easing of chest pain within ten minutes of entering the hyperbaric chamber
HBO therapy reduced by 50 percent the time required for the heart to resume normal electrical activity as determined by an electrocardiogram ECG finding called ST normalization S and T waves are two points on an ECG tracing The time was 188 minutes for patients who went into the chamber vs 374 for those who did not We ve clearly shown that pain goes away very quickly and ST elevation which we think is a sign of the heart muscle dying returns to normal more rapidly said Dr Ellestad To me the most dramatic aspect of the study was watching as ST elevation returned to normal after a patient went into the chamber That tells me we re salvaging heart muscle cells There s some evidence that HBOT decreases activity by oxygen free radicals These are unstable molecules known to damage or destroy cells Two other findings provided additional evidence of benefits from HBO therapy Patients sent to the chamber had significantly lower blood levels of the enzyme creatine phosphokinase which is released during a heart attack and indicates the extent of heart muscle damage Patients treated in the hyperbaric chamber also had a higher ejection fraction a measurement that reflects how well the heart can pump blood Dr Ellestad sees potential for even better results with HBOT if patients can begin oxygen therapy sooner Transporting patients to the chamber and preparing them for treatment require about thirty minutes He and his colleagues hope to reduce that time at Long Beach Memorial by relocating the hyperbaric chamber to the hospital s emergency room Physician interest in HBO treatment for heart attack patients goes back a number of years however the interest had dwindled after the emergence of TPA and other clot dissolving agents Then an unusual event prompted Dr Ellestad and his colleagues to take another look at HBOT George Hart MD director of the hyperbaric unit at the hospital and an investigator in the study reported at the AHA 1992 New Orleans meeting began having chest pains and decided to treat himself in the oxygen chamber The HBOT relieved his heart pain in minutes Being friends Dr Ellestad checked out what Dr Hart explained about his HBOT experience Hyperbaric chambers are not standard equipment at hospitals and medical centers If HBOT proved beneficial for a hospital most likely it could afford the 80 000 to 90 000 cost for a single patient chamber This is the type used in the test at Long Beach Memorial Hospital HBOT adds about 200 to the daily cost of treating a heart attack patient Dr Ellestad said Besides Drs Ellestad and Hart investigators in the study included Adrian H Shandling MD John C Messenger MD Bruce VanNatta MD Daniel D Whitcraft MD Roger H Rizi MD Ronald H Selvester MD Michael Hayes MD and Clyde W Smith MD More Studies Show the Efficacy of HBO for Heart Disease The Long Beach Memorial Hospital s investigation is just one among thousands proving the efficacy of HBO for heart disease Medical professionals and hyperbaric scientists around the world have proven the benefits of applying HBO for the reduction of actual reversal of most heart disease signs and symptoms Their presentations are highly significant for furthering heart health The renowned Russian hyperbaricist Serge I Rodionov MD who practices HBOT in Moscow told how pharmaceutical agents prescribed for the treatment of cerebrovascular disease cardiomyopathy and heart failure are potentiated by hyperbarics Drug effects increased when the heart patient was placed in a pressure chamber for just one hour per week
By the date of his 1989 lecture Dr Rodionov affirmed there were over 3 000 HBO chambers strategically located around the country which was then the original Union of Soviet Socialist Republics And he said acceptance of the modality was gaining in the medical community for the treatment of heart disease Today just in the newly formed smaller nation of Russia itself 3 000 chambers have been installed and are functioning Thirteen Benefits the Heart Receives from Oxygen Under Pressure The nature of heart disease is such that insufficient oxygen is getting to the heart This results in the various discomforts which affect a patient difficulty breathing inability to exert oneself pressure in the chest and other problems Breathing normal air results in a mere 0 3 ml of oxygen dissolving into each 100 ml of blood Any other oxygen is bound by the hemoglobin attached to red blood cells and it essentially becomes unavailable The need in heart disease is to get more oxygen molecules into the body and brain From the published scientific papers on HBO Dr Steenblock offers thirteen true benefits that the heart receives from exposure to oxygen under pressure Clinical investigations by prime users of HBO from around the world especially from Russian exponents have shown the following heart advantages 1 Hyperbaric oxygen therapy applied to the heart during critical loss of oxygen exerts a remarkable defibrillating effect so that tremulous rapid ineffectual contractions are prevented total death of the heart muscle cells is avoided and abnormal dilation of the blood vessels with subsequent complications is controlled 2 Using HBOT in conjunction with various drugs enhances the effectiveness of both the oxygen and the drugs 3 Combining HBOT with drugs completely arrests or considerably reduces angina attacks in patients otherwise resistant to prolonged drug treatment 4 Patients with cardiac pain from ischemic heart disease experience total relief along with disappearance of dyspnea difficulty breathing when they receive HBOT 5 Administering HBOT lowered elevated blood cholesterol in all 220 patients cited in a study conducted by the Russian internist Dr S A Borukhov and her colleagues 6 HBOT normalized electrocardiograms in all patients in that same Soviet study 7 For diminished muscular power of the heart HBO exerts long term normalizing effects for circulating blood through the body 8 HBOT exerts antiarrhythmic action on the heart 9 HBOT increases heart patients tolerance to hard work and taking on physical loads 10 HBO taken at three atmospheres of pressure a pressure rarely used in the United States protects any individual s heart from damages due to lack of oxygen 11 One s entire heart conduction system functions better from receiving HBO treatment even when prophylactically administered 12 Without taking drugs of any kind breathing oxygen under pressure stabilizes impaired fat metabolism and improves liver function for someone with ischemic heart disease 13 Due to its characteristic of mollifying stress and distress HBO has long term and short term protective effects for a person with a heart problem How HBOT Further Enhances the Ailing Heart As a result of elevating the atmospheric pressure inside the hyperbaric chamber by 1 1 2 to 2 atmospheres absolute ATA plus administering 100 percent oxygen to the cardiac patient by means of a face mask this ill person receives a sharply increased amount of oxygen dissolved in the plasma Such improved blood oxygen content tends to give the damaged heart an assist in oxygenating body tissues which provides time for the myocardium to recover and develop
extra circulation around the area of the infarct a localized area of decay in the heart muscle resulting from the interruption in blood supply As shown in the studies cited above hyperbaric oxygen therapy for the relief of myocardial infarction has tremendous value for recovery of the patient It increases oxygen intake for building collateral circulation in cases of angina pectoris as well HBO should not be reserved only for patients in cardiac intensive care units Family practice physicians sometimes stop themselves from requesting HBO therapy for their cardiac patients because they suspect there s a vasoconstrictive effect of HBO Erroneously the doctors may conclude that such treatment is dangerous and shouldn t be utilized on already constricted blood vessels That s not true Medical studies well performed according to the scientific method show that hyperoxic vasoconstriction occurs in healthy tissue only On the damaged ischemic tissue vasodilation that occurs naturally counteracts any vasoconstriction produced by HBO Higher amounts of blood flowing to areas of hypoxia create the opening of collateral blood vessels Hyperbaric oxygen therapy is an assist to the body s own healing mechanism By itself HBO would probably not offer the desired results Numerous studies on animals conducted in the 1960 s in fact showed unfavorable results using the treatment for heart disease A closer look at the studies however reveals that they were performed on anesthetized dogs laying helplessly on a table with various tubes running in and out of them These animals were given drugs to induce some type of heart malfunction then hyperbaric oxygen was administered usually at far too high a pressure for either too long or too short a time Such procedures on animals don t translate neatly into the human condition The human patient can alter his or her risk factors by improving diet stopping smoking increasing exercise and doing those various other beneficial things that I ve mentioned Definitely chelation therapy taken along with the HBO received at the proper pressure for the time needed to effect heart disease reversal is the ideal way to go Retaining risk factors is ridiculous but that was done in experiments with the anesthetized dogs Such experiments were fated for failure and did fail Still the studies were reported in the clinical journals and threw off physician readers from following the correct path as regarding the use of hyperbaric oxygen as therapy for angina myocardial infarction and other heart ailments As we have stated very little oxygen is dissolved in blood plasma at the normal atmospheric pressure of 102 millimeters of mercury mm Hg HBO therapy forcefully puts oxygen unbound by hemoglobin into the blood plasma This increases the blood oxygen level fourteen times to 1433 mm Hg and thereby delivers much greater quantities of oxygen to oxygen starved tissues Those organs tissues and cells that have been suffering from a lack of oxygen because of poor circulation or damage then will become revitalized and begin to function more effectively The London Westminster Hospital Experience with HBOT In London C J Gavey MD chief of the cardiac department at Westminster Hospital pressurized heart attack patients to save their lives For four days He subjected them to 2 ATA in 100 percent oxygen for two hours followed by a rest of one hour in plain air and then continued the cycle of two hours in the chamber and one hour out His idea was to send oxygen through the unblocked blood vessels to the ischemic tissues at the edge of the infarct area preventing the impending death of additional heart muscle He figured that this procedure might avoid the triggering of fatal arrhythmias Forty men and women who had suffered serious heart attacks within twenty four hours were treated this way by Dr Gavey They ranged in age from thirty five to seventy two years Surviving their cardiovascular accidents as a result of undergoing the HBO procedure directly upon their admittance to London s Westminster Hospital were 92 5 percent of the acutely affected patients Of these thirty seven initial survivors three died within fifteen days giving a final survival rate of 85 percent
Quite significant was the reduction of heart pain experienced by these patients Almost a quarter century before Dr Myrv in Ellestad made his AHA conference presentation Dr Gavey reports that twenty three of his patients arrived in severe pain and fourteen had difficulty breathing Once settled into the pressure chamber none of the patients felt any more pain Within thirty minutes of pressurization their breathing problems eased too Inasmuch as only the really critical cases those who potentially could die on the spot have been administered HBO such results were quite heartening to the Westminster Hospital authorities They considered that HBO therapy saved some patients from fatal cardiogenic shock The optimum hyperbaric regimen for cardiac conditions however was not defined and was still being decided upon twenty five years after Dr Gavey s clinical experiment Dr Ellestad confirmed Dr Gavey s report How Strange It Is That Cardiologists Don t Prescribe HBOT If heart disease allows insufficient oxygen to get into the heart muscle as stated earlier various symptoms that most of us can identify must result With O2 being inhaled at normal atmospheric pressure but not preventing cardiovascular problems for the more than 1 200 000 heart attack victims each year in the United States alone obviously greater amounts of this life giving element must be obtained HBO administered at the established two atmospheres absolute to force O2 into the body allows the doctor to effect 4 3 ml of oxygen being dissolved into each 100 ml of blood Thus a cardiologist or other doctor is furnishing therapeutic oxygen amounting to a fourteenfold increase Simply this is Henry s gas law of physics at work Using modern equipment in this way any skilled physician can safely elevate available oxygen for his patient to provide pain relief to prevent fatal arrhythmias or shock and to allow time for collateral blood circulation to develop Yet HBO seldom is used in the U S to reverse heart disease before it becomes near fatal Isn t it strange that cardiologists don t routinely utilize hyperbaric oxygen as a valid therapy Even odder is that they almost never employ the modality to benefit their cardiac patients at all That s because the average American allopathic physician traditionally trained primarily in the use of drugs and surgery usually fails to have access to and certainly does not personally own a hyperbaric chamber Moreover the doctor probably is unfamiliar with what taking oxygen under pressure can do for promoting human homeostasis We have a most peculiar conundrum here for which the answer would be funny if we were not dealing with matters of life and death Note the irony Of the hundreds of published scientific studies applied to heart disease the set of elements you will seldom read or hear about is the mention of diet exercise smoking and drinking habits of the cardiac patient in conjunction with administering HBOT to him or her This is a commonsense procedure the use of hyperbaric oxygen with one s everyday healthy lifestyle Instead detailed instructions usually are given only for the various drugs being tested with HBO Combining hyperbaric oxygen with those other more vital factors involving lifestyle poor lifestyle practices probably being the source of heart weakness or disease in the first place could optimize the outcome for an involved cardiac patient Reprinted with Permission Research References 1 2 Dmitrieva E M et al Hyperbaric oxygenation in experimental therapy of acute regional hypoxia of the myocardium and brain In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 276 277 Glants B R Therapeutic effects of mercazol in combination with hyperbaric oxygenation in the treatment of acute myocardial hypoxia In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 p 275
3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 Kogan A H et al The question of the use of antioxidants beta adrenergic blockers and cardiac glycosides in oxygen therapy of acute myocardial infarction In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 275 276 Yefuni S N et al The use of hyperbaric oxygenation in combined therapy of acute myocardial infarction In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 264 265 Zamotaev I P et al Hyperbaric oxygenation in the treatment of ischemic heart disease and peptic ulcer of stomach and duodenum In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 p 269 Op Cit Yefuni S N Kolomeitseva S P et al Hyperbaric oxygenation as an adjunct in the treatment of ischemic heart disease In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 p 266 Kuleschova M R et al Physical rehabilitation of patients with ischemic heart disease using hyperbaric oxygenation In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 268 269 Golyakov V N et al Hemostasis in patients with ischemic heart disease during hyperbaric oxygenation Klin Med Mosk 64 2 92 95 1986 Borukhov S A et al HBO effect on clinico biochemical blood indexes in patients with ischemic heart disease In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 271 272 Ashfield R et al Severe acute myocardial infarction treated with hyperbaric oxygen Report on forty patients Postgrad Med J 45 648 654 October 1969 Op Cit Borukhov S A Ibid Isakov Y V et al Hyperbaric oxygenation in combined treatment of paroxysmal tachyarrhythmias in ischemic heart disease Kardiologiia 21 4 42 45 April 1981 Ivleva V I et al Effect of hyperbaric oxygenation on the activity of the sympathoadrenal and Kallikrein Kinin systems of blood in some disorders of cardiac rhythm Ter Arkh 53 5 66 68 1981 Malinovsky N N et al The use of hyperbaric oxygenation in cardiac arrhythmia In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 284 285 Timchuk I D et al Hyperbaric oxygenation in complex treatment of patients with disorders of rhythm and conduction of heart In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 p 286 Op Cit Kolomeitseva S P Kulkybaev G A et al Functional state of the cardiovascular system and lungs of patients with chronic ischemic heart disease under conditions of hyperbaric oxygenation In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 269 270 Kostyukov V V et al Coronary circulation and oxygen regime of the myocardium at a low cardiac output and HBO In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 p 276 Rugenyus Y Y et al The effect of hyperbaric oxygenation on the conductive system of the heart in patients with ischemic heart disease In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 p 271 Zhumanov K D et al A study on metabolic indexes in patients with chronic ischemic heart disease subjected to hyperbaric oxygenation In Abstracts VII Int Cong HBO Medicine Moscow Sept 2 6 1981 pp 270 271 Op Cit Ashfield R Hyperbaric unit puts pressure on heart deaths Medical World News May 24 1968 Tufano R et al Hyperbaric oxygen effects on pain relief in patients with vascular disease J Hyperbaric Medicine Vol 3 No 1 1988 Visona A et al Hyperbaric oxygenation in the treatment of peripheral vascular disease J Hyperbaric Medicine Vol 2 No 4 1987 Trimble V H The Uncertain Miracle Hyperbaric Oxygenation Garden City NY Doubleday 1974 pp 124 127
Autonomic Nervous System in the Patients with Coronary Artery Diseases during Hyperbaric Oxygenation Therapy Stepanov Andrey MD Stepanova Svetlana MD Central Clinical Hospital N5 Department of Blood Purification and Hyperbaric Oxygenation Therapy Cardiology Department Kharkov Ukraine Abstract Introductions Hyperbaric oxygenation therapy HBOT is inhalation of pure oxygen at grate then 1 atm absolute pressure Prior trials detected benefits from HBOT for patients with coronary artery diseases CAD But not all is known about the influence of HBOT on autonomic nervous system ANS Heart rate variability HRV is a proven tool for examining the ANS Objectives The aim of this study was to assess the changes in ANS during HBOT by using the HRV Material and Method The first group of 6 patients with CAD were pressurized up to 1 5 atm absolute pressure aap and remained at this pressure for 40 minutes In the control groupe these 6 patients stayed in HBOT chamber under 1 0 aap in 21 40 oxygen instead sessions 1 and 7 The HRV was recorded using Cardiolab 2000 system during sessions 2 6 and 10 Patients were examined before HBOT and on the first and 40th minute under 1 5 aap TP LF HF and LF HF ratio were analysed for the frequency domain measures Results In the first group we observed significant increase p
September 1998 and it is still in progress This is a preliminary report The first group included 6 patients with CAD stable angina pectoris I III class NYHA and receiving usual treatment Patient were pressurized during 15 20 minute period up to 1 5 atmosphere absolute pressure aap and remained at this pressure for 40 minutes and then depressurized during 15 minute period to normal atmosphere pressure Total time of HBOT was 70 80 minutes In the control group these 6 patients stayed in HBOT chamber under 1 0 aap in the 21 40 oxygen s atmosphere instead first 7th and 11th HBOT sessions during 70 80 minutes We used monoplace chamber OKA MT with 1m3 volume inside Monitoring of electrocardiogram ECG noninvasive blood pressure before and after HBOT in supine position was performed during HBOT sessions Every patient received 10 HBOT sessions in the same time every day HRV was calculated in general agreement with the standards of measurement proposed by Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology 1 The HRV was recorded using computer based electrocardiograph system Cardiolab 2000 during sessions 2 6 and 10 before HBOT on the first minute under the 1 5 aap and on 40th minute under 1 5 aap In the control group the HRV was recorded before HBOT on 15 and 55 minutes of the sessions 1 7 and 11 HRV was analyzed on 5 minute period of stable ECG recording for the frequency domain measures with the use of fast Fourier transform We measured the total power TP of the R R interval 0 0 5 Hz The frequency ranges were subdivided into 0 03 0 15 Hz as a low frequency component LF and 0 15 0 5 Hz as a high frequency HF one TP LF HF was expressed in absolute values ms2 We measured also the LF HF ratio and LF and HF in normalized units LFn HFn respectively calculated as a percentage of TP of the R R interval from which the power of any component with a frequency of less than 0 03 Hz was removed 1 The results are given as mean standard deviation SD A p value
Our preliminary results showed that measurement of HRV was helpful in monitoring during the sessions of HBOT and reflected the effects in the treatment of patients with CAD Adjunctive HBOT can improve prognosis in patients with CAD Based on values of HRV it will be possible in the future to modulate the protocols of HBOT Of course it need to explore the influence of other treatment protocols of HBOT on ANS and in particularly how long changes we detected last In Figure 1 and 2 showed changes in Very LF component that reflected another ways to change HRV but it will be another report The authors wish to thanks the Callahan s and Ockunzzi s family Cleveland Ohio USA for assistance References 1 2 3 4 5 6 7 8 9 10 11 12 13 Task Force of the European Sosiety of Cardiology and the North American Sosiety of Pacing and Electrophysiology Heart Rate Variability Standards of Measurements physiological interpretation and clinical use Circulation 1996 V 93 1043 1065 Ackerman NB Brinkly FB Oxygen tension in normal and ischemic tissues during hyperbaric treatment JAMA 1966 198 1280 3 Kawamura M Sakakibara K Sakakibara B et al Protective effect of hyperbaric oxygen for temporary ischemic myocardium macroscopic and histologic data Cardiovasc Res 1976 10 599 604 Adrian H Shandling MD Myrvin H Ellestad MD et al Hyperbaric oxygen and thrombolysis in myocardial infarction The HOT MI Pilot Study Am Heart J 134 3 544 550 1997 Seriakov VV Feofanova ID Hyperbaric oxygenation and antiaggregants effects on platelet function in patients with ischemic heart disease Anesteziologiia i Reanimatologiia 2 31 3 1997 Mar Apr Maria Vittoria Pitzalis Filippo Mastropasqua et al Assesment of cardiac vagal activity in patient with hyperthyroidism International Journal of Cardiology 64 1998 145 151 Simonetta Scavini Maurizio Volterrani Emanuela Zanelli et al International Journal of Cardiology 67 1998 9 17 Andrew J Burger MD and Masoor Kamalesh MD Effect of Beta Adrenergic Blocer Therapy on the Circadian Rhythm of Heart Rate Variability in Patients with Chronic Stable Angina Pectoris The American Journal of Cardiology vol 83 February 15 1999 Amara C E and Wolfe L A Reliability of Noninvasive Methods to Measure Cardiac Autonomic Function Can J Appl Physiol 23 4 396 408 1998 P J Schwartz The autonomic nervous system and sudden death European Heart Journal 1998 19 Supplement F F72 F80 Nolan James MD Batin Phillip D MD Andrews Richard MRCP et al Prospective Study of Heart Rate Variability and Mortality in Chronic Heart Failure Results of the United Kingdom Heart Failure Evaluation and Assesment of Risk Trial UK Heart Circulation Vol 98 15 October 13 1998 1510 1516 Singh Jagmeet P MD Dphil Larson Martin G ScD O Donnell Christopher J MD MPH et al Circulation Vol 99 17 May 4 1999 2251 2254 Ad Van Boven MD J Wouter Jukema MD Jaap Haaksma BSc Depressed heart rate variability is associated with events in patients with stable coronary artery disease and preservsd left ventricular function American heart Journal Vol 135 Number 4 571 575 Hyperbaric oxygen limits infarct size in ischemic rabbit myocardium in vivo Sterling DL Thornton JD Swafford A Gottlieb SF Bishop SP Stanley AW Downey JM Department of Biological Sciences University of South Alabama Mobile 36688
BACKGROUND We explored the ability of increased oxygen pressure to modify necrosis in an open chest rabbit model of myocardial ischemia and reperfusion METHODS AND RESULTS A branch of the left coronary artery was occluded for 30 minutes followed by 3 hours of reperfusion Infarction was measured by triphenyl tetrazolium staining and expressed as a percentage of the ischemic zone Untreated rabbits were ventilated with 100 oxygen at 1 atm absolute Treatment animals were exposed to hyperbaric oxygen at 2 5 atm absolute The 1 0 atm control hearts developed 41 5 4 6 infarction of the ischemic zone Animals exposed to hyperbaric oxygen during ischemia only reperfusion only or ischemia and reperfusion had significantly smaller infarcts with respect to control animals 16 2 2 9 14 5 3 7 and 9 8 2 7 respectively P
Adjunctive effect of hyperbaric oxygen treatment after thrombolysis on left ventricular function in patients with acute myocardial infarction October 2004 Volume 148 Number 4 Milica Dekleva MD PhDAleksandar Neskovic MD PhD FESC Alja Vlahovic MD Biljana Putnikovic MD PhD Branko Beleslin MD FESC Miodrag Ostojic MD PhD FESC FACC Cardic Abstract Background The role of hyperbaric oxygen in patients with acute myocardial infarction is controversial ranging from not beneficial to having a favorable effect This randomized study was conducted to further assess the benefit of hyperbaric oxygen treatment after thrombolysis on left ventricular function and remodeling in patients with acute myocardial infarction Methods Seventy four consecutive patients with first acute myocardial infarction were randomly assigned to treatment with hyperbaric oxygen treatment combined with streptokinase HBO or streptokinase alone HBO Results There was a significant decrease of end systolic volume index from the first day to the third week in HBO patients compared with HBO patients from 30 40 to 28 18 vs from 30 89 to 36 68 mL m2 P
To determine the rate of comorbid mental disorders among Medicare patients who were hospitalized for HF Dr Sayers and colleagues examined a 5 sample of Medicare records He presented the results of that examination on September 20th Of 13 169 patients with HF identified in that sample the database indicated that about 1556 11 8 patients had comorbid mental disorders Depression accounted for 52 8 of patients with mental disorders 22 had anxiety disorders and 16 7 had psychoses Alcohol abuse was identified in 16 3 of patients with heart failure and comorbid mental disorders Comorbid depression and psychoses appear to be associated with longer hospitalizations almost 3 days more he said All patients with comorbid mental disorders tended to have more annual hospitalizations than patients with heart failure who did not have mental disorders He said that his analysis shows that while patients with comorbid mental disorders tend to use more resources except for patients with psychoses there are no increased mortality risks Patients with alcohol abuse disorder did not increase costs associated with their hospitalizations he said It is likely that the actual rates of psychiatric comorbidity in this sample are higher than the rates we estimated from administrative data due to common problems of underdetection and underdocumentation of mental disorders Dr Sayers noted He suggested that this type of comorbidity may represent an important addressable source of increased costs of healthcare for patients with heart failure Presentation title Comorbid Mental Disorder among Patients Hospitalized with Heart Failure Abstract 283 German Study Links Infection Heart Disease By Maggie Fox Health and Science Correspondent WASHINGTON Reuters Researchers in Germany said on Monday they had found more evidence that infections with bacteria that cause pneumonia ear infections and other diseases may also cause heart disease The study in the American Heart Association journal Circulation adds to a growing body of evidence that the body s response to some infections may help cause heart disease We showed a significant association between the number of infections to which a patient has been exposed and the extent of atherosclerosis in the arteries in the heart neck and legs Dr Hans Rupprecht and Dr Christine Espinola Klein of Johannes Gutenberg University in Mainz Germany who conducted the study said in a statement The risk for death was increased by the number of infectious agents especially in people with advanced artery disease Researchers believe it is the body s inflammatory response to an infection that helps along with a fatty diet to clog arteries The plaques that form these clogs are created when immune system cells latch onto fat cells in the blood and try to pull them out through the cell wall The fat cell is often too big and it gets caught Thetrapped immune and fat cells build up in the artery wall harden and can block blood flow or break off into clots
Inflammatory responses to infection can send more of these immune cells circulating looking for something to do Rupprecht s team tested 572 patients with heart disease most of whom had chest pain or heart attack EIGHT MICROBES ASSOCIATED WITH HEART DEATH They looked herpes simplex virus 1 and 2 which cause cold sores and genital herpes cytomegalovirus which is another herpes virus Epstein Barr virus which causes mononucleosis Hemophilus influenzae a bacteria that causes ear and upper respiratory infections Chlamydia pneumoniae which can cause pneumonia Mycoplasma pneumoniae another cause of pneumonia and Helicobacter pylori which causes most stomach ulcers Over the next three years Rupprecht s team wrote they found a clear correlation between how many infections a person had and his or her risk of dying from heart disease The antibody titers levels for C pneumoniae H pylori H influenzae cytomegalovirus and herpes simplex virus type 2 were related to the extent of atherosclerosis Espinola Klein said in an interview conducted by e mail In patients who tested positive for up to three infections the death rate was 3 1 percent The death rate was 9 8 percent for those infected with four to five agents and 15 percent for those with six to eight pathogens Twenty percent of the patients with advanced atherosclerosis who had six to eight infections died compared to 7 percent of those with three exposures or fewer Based on these results we think that the number of infections to which an individual has been exposed may be involved in the development and progress of atherosclerosis Both bacterial and viral pathogens seem to be involved Espinola Klein said But Dr Paul Ridker director of the Center for Cardiovascular Disease Prevention at Brigham and Women s Hospital in Boston said the link may not necessarily mean that infections cause heart disease They could just be a marker for something else For example Ridker said in a commentary people with a lot of infections could be in poorer health in general Ridker who also studies links between infection and heart disease has found that healthy people with high levels of inflammatory cells are more likely to develop heart disease Our results suggested that inflammation seems to be a fundamental issue he said and noted that other studies indicate that aspirin and cholesterol lowering statin drugs may prevent heart disease at least in part by reducing inflammation Last November a Swedish team reported in the Journal of the American Medical Association that elevated levels of interleukin 6 one of the body s inflammatory signaling chemicals could predict deaths from heart disease And last February an Austrian team reported that people who get infections over and over again such as sinus infections or bronchitis may also be more prone to clogged arteries But although several studies have linked infection with heart disease none has shown that people who took antibiotics had a lower risk of heart disease
Hirai et al Pancreatic Dis Ther 2013 S4 10 4172 2165 7092 S4 006 erapy Th Pancre at Disorders ic Pancreatic Disorders Therapy ISSN 2165 7092 Research Article Open Access Hyperbaric Oxygen Therapy for Pancreatic and Gastrointestinal Disease Ichiro Hirai Wataru Kimura Toshihiro Watanabe Koji Tezuka Toshiyuki Moriya Tsuyoshi Fukumoto Hiroto Fujimoto Akiko Takeshita Shuichiro Sugawara Shinji Okazaki Masaomi Mizutani Hideki Isobe and Osamu Hachiya First Department of Surgery Yamagata University Iida Nishi Yamagata City 990 9585 Japan Abstract We report the results of hyperbaric oxygen therapy HBO for pancreatic and gastrointestinal disease Thirty nine patients received 100 oxygen at 2 atmospheres absolute pressure for 60 min Results In all four patients with liver abscess feverishness subsided within 2 7 days after the start of HBO All of effective in four but ineffective in one Five of six cases of infection after pancreatic resection were cured immediately after HBO Conclusions HBO is sometimes effective for treatment of refractory gastro enteric infections especially those for generally cost effective it should be considered as an adjunct therapy for all gastro enteric infections Keywords Hyperbaric oxygen therapy Pancreatitis Abdominal infection Pneumonia Introduction In the field of abdominal surgery hyperbaric oxygen therapy HBO is used mainly for adhesive ileus 1 and peumatosis intestinalis 2 3 However few reports have documented the use of HBO in other fields of gastroenterology HBO has been shown to be especially effective for healing of complex ischemic wounds in patients with atherosclerosis or diabetes mellitus 4 Recently HBO has also been used in cases of liver failure and liver transplantation 5 HBO with 100 oxygen at twice sea level atmospheric pressure can create an arterial oxygen tension in excess of 2000 mmHg and almost 400 mmHg in tissues 6 Here we examined the utility of HBO for various gastroenteric diseases Methods Thirty nine patients with gastro enteric conditions that had proved refractory to conservative therapies such as antibiotics or drainage were treated with HBO between 2007 and 2012 in our department Table 1 Patients were treated once a day in a hyperbaric chamber BARA MED Koike Medical Tokyo Japan at a pressure of 2 0 atmospheres absolute and received 100 oxygen Figure 1 Session duration was 60 min and decompression was initiated at 15 min Each patient provided written informed consent to undergo HBO The clinical parameters recorded for each patient included the period between onset of fever more than 38 degree and the start of HBO body temperature at the time of HBO initiation number of sessions days of HBO period between the start of HBO and fever resolution less than 38 degrees white blood cell count CRP levels before and after HBO types of bacteria responsible for inflammation and clinical outcome number of sessions days of HBO was 15 3 range 4 to 28 and the period between onset of fever and the start of HBO was 4 to 14 days In all four cases the fever decreased to less than 38 degree within 1 to 4 days after the start of HBO mean 2 7 days The mean white blood cell count decreased from 11565 to 4415 micro little and the mean CRP level from 15 0 to 0 4 mg dl The causative bacteria included Citrobacter Enterococcus and Staphylococcus All four cases were resolved without percutaneous transhepatic abscess drainage Figures 2a 2d HBO was also performed for three post hepatectomy patients all of whom had undergone segmentectomy of S8 One of the three had MRSA infection and SIRS but his condition improved 3 days after starting HBO The other two patients with abscesses were also cured after 13 and 14 sessions of HBO respectively Acute appendicitis HBO was applied to 7 cases of acute appendicitis Appendectomy was not performed for 2 of these cases because of severe extension of retroperitoneal abscess or phlegmon The other cases involved postappendectomy abscesses The mean number of HBO sessions was 9 9 range 7 to 14 Pyrexia decreased to below 38 degrees 1 8 days range 1 to 3 days after initiation of HBO The mean white blood cell count decreased from 13183 to 7185 micro little and the CRP level from 13 7 to 0 7 mg dl All seven patients were discharged without further drainage surgery Figures 3a and 3b Corresponding author wkimura med id yamagata u ac jp Received Published May 10 Citation Hirai I Kimura W Watanabe T Tezuka K Moriya T Fukumoto T et al Results 6 Liver abscess and abscess after hepatectomy HBO was performed for four cases of liver abscess The mean Pancreatic Dis Ther Accepted May Copyright Hirai I et al This is an open access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use distribution and reproduction in any medium provided the original author and source are credited Pancreatic Cancer and Diagnosis ISSN 2165 7092 PDT an open access journal
Citation Hirai I Kimura W Watanabe T Tezuka K Moriya T Fukumoto T et al 6 Page 2 of 5 Disease Number of Days Mean of Cases not patients required for HBO effective to pyrexia to sessions
Citation Hirai I Kimura W Watanabe T Tezuka K Moriya T Fukumoto T et al 6 Page 3 of 5 Figure 3b Abscess was improved after 10 sessions of HBO same case Figure 5a Abscess of pseudocyst due to alcoholic pancreatitis before HBO Figure 4a Mediastinal abscess after esophagectomy before HBO Figure 5b Figure 4b Esophageal disease HBO was employed for three cases of esophagieal disease Two of them involved mediastinal abscess and peritoneal abscess after esophagectomy and the other was esophago tracheal fistula due to radiation for lung cancer Pyrexia was resolved within one day after HBO in all three patients Figures 4a and 4b However the esophagotracheal fistula was not cured Pancreatic disease Figure 6 Changes in body temperature in a patient after pancreatoduodenectomy After addition of HBO the body after HBO in two cases the abscess was not cured and re operation was required in one case Pyrexia was resolved by HBO within 2 days in a patient with an infected pseudocyst due to alcoholic pancreatitis Figures 5a and 5b Ileus HBO was also applied to three patients after pancreatoduodenectomy In one of them although CT showed absence of abscess formation in the abdominal cavity pyrexia was refractory requiring daily NSAIDs and antibiotic infusion after surgery Three days after the introduction of HBO therapy the fever was resolved Figure 6 Three cases of ileus were treated with HBO being effective in one case and not effective in two Paralytic ileus was cured within 5 days after HBO An ileus tube was required in one case because HBO was not effective Reoperation was performed for ileus after resection of transverse colon cancer HBO was also used for three patients with intra abdominal abscess after distal pancreatectomy Although the fever was resolved one day Pancreatic Dis Ther Other diseases HBO was very effective for treatment of abdominal wall infection Pancreatic Cancer and Diagnosis ISSN 2165 7092 PDT an open access journal
Citation Hirai I Kimura W Watanabe T Tezuka K Moriya T Fukumoto T et al 6 Page 4 of 5 These have included its use for proctitis caused by irradiation of the pelvic area including the rectum and anus 15 and healing or clinical improvement of chronic radiation enteritis in two thirds of treated patients 16 Supplementary systemic oxygen has been reported to decrease the rate of infection after colorectal surgery 4 We consider that HBO is effective for management of diverticulitis or remnant peritoneal abscess separate from the digestive tract after colorectal surgery On the other hand we observed that HBO is not effective without surgical intervention for abscesses showing continuity with the digestive tract resection and anastomosis of the perforation site or colostomy should be scheduled for such cases In the esophageal field mediastinal gas gangrene due to esophageal perforation has been treated successfully with HBO 17 In our experience HBO is also useful for management of mediastinal abscess after esophagectomy HBO has been used to treat radiation induced hemorrhagic gastritis of the gastric conduit after esophagectomy 18 In our present series esophago tracheal fistula was not cured by HBO This is not because HBO failed but some illnesses are refractory to all man made treatments simply due to the severity of the disease One previous report has described that HBO was used successfully to treat a case of esophagotracheal fistula after ingestion of a lithium disc battery in 12 month old child 19 Figure 7a In the pancreatic field the effectiveness of HBO has been examined mainly using a rat model 10 HBO for management of severe acute pancreatitis is reportedly safe and may have a role in improving treatment outcomes 20 We also experienced a case of infected pseudocyst in a patient with alcoholic pancreatitis for which HBO proved effective apparently ameliorating infection and local edema Figure 7b subcutaneous phlegmon around the drainage T tube and pyogenic spondylitis Figure 7a after cholecystectomy due to spontaneous gallbladder rupture Figure 7b However HBO was not effective for pelvic abscess after resection of an irradiated small intestine or for abdominal abscess after gastric perforation Reoperations were required in both cases There were no complications such as oxygen intoxication inflammation of the middle ear or pneumothorax in this series Discussion The use of HBO is reportedly beneficial for chronic non healing diabetic wounds compromised skin grafts bone and soft tissue radiation necrosis and gas gangrene 7 8 HBO therapy has been reported for a patient with perinephritic abscess due to polycystic kidney disease 9 Therefore HBO may also have potential therapeutic benefits for gastroenteric conditions HBO is reportedly effective for clearance of not only anaerobic but also aerobic bacteria 10 HBO has been reported to ameliorate hepatic ischemia reperfusion injury in a rat model 11 HBO also helps to enhance liver regeneration in living donor adult liver transplantation 12 HBO after hepatectomy reduces the need for perioperative erythrocyte transfusion and also the incidence of postoperative complications as well as affecting postoperative immunological responses 13 HBO is reported to effectively prevent both bacterial overgrowth and translocation in rats with jaundice 14 In the present study we found that a combination of antibiotics and HBO was effective for management for intractable liver abscess There have been a number of reports of HBO for colorectal diseases Pancreatic Dis Ther Recently the number of patients undergoing surgery for intraductal papillary mucinous neoplasm of the pancreas has been increasing 21 22 In such cases the pancreatic parenchyma is soft and this makes pancreatic fistula after pancreatectomy a potentially lethal complication The importance of drainage for pancreatic fistula after pancreatectomy has been reported 23 It is indisputable that surgical or interventional drainage and antibiotics are essential for the treatment of gastroenteric infection However concurrent HBO seems to confer an additional anti infection effect In this series a case of pyrexia after pancreatectomy was cured promptly by HBO probably due to the bactericidal effect of high tissue oxygen pressure High oxygen pressure also alleviates insufficiency of the peripheral circulation allowing antibiotics to reach wider areas of tissue and providing oxygen to devitalized tissue HBO is reportedly effective for ileus However two of three such cases in our present series were not cured by HBO An ileus tube or surgery may be more appropriate for treatment of mechanical ileus whereas HBO may have better applicability for paralytic ileus HBO is usually used in combination with other treatments such as antibiotics or drainage Because randomized studies of HBO have been rare there is insufficient evidence to indicate the optimal timing of therapy or for establishing criteria that would allow selection of patients who would benefit from it 7 In conclusion HBO is effective for management of refractory infections in the gastroenteric field HBO is especially effective for infections that are difficult to drain such as retroperitonitis or phlegmon In most of the present cases pyrexia improved within 2 3 days after the start of HBO HBO should be considered as an additional treatment for patients with infections that are refractory to standard antibiotics or drainage Pancreatic Cancer and Diagnosis ISSN 2165 7092 PDT an open access journal
Citation Hirai I Kimura W Watanabe T Tezuka K Moriya T Fukumoto T et al 6 Page 5 of 5 References 1 transfusions in patients with HCC who have undergone partial hepatectomy treatment of postoperative paralytic ileus and adhesive intestinal obstruction oxygen prevents bacterial translocation in rats with obstructive jaundice Dig 2 16 gastrointestinal radiation injury with hyperbaric oxygen Undersea Hyperb 17 6 7 20 Christophi C Millar I Nikfarjam M Muralidharan V Malcontenti Wilson Hyperbaric oxygen therapy in a patient with autosomal dominant polycystic 21 10 type of mucin producing tumor of the pancreas new concept of pancreatic 11 22 12 of hyperbaric oxygen treatment on postoperative morbidity of left lobe donor Pancreatic Dis Ther the pancreas and how to achieve zero mortality for pancreaticoduodenectomy Pancreatic Cancer and Diagnosis ISSN 2165 7092 PDT an open access journal
APRIL 2017 C L I N I C A L M A e xtra N A G E M E N T Hyperbaric Oxygen Therapy Exploring the Clinical Evidence C M E 1 AMA PRA Category 1 CreditTM ANCC 1 0 Contact Hour Gretl Lam BA Fourth year Medical Student New York University School of Medicine New York New York Rocky Fontaine CHT Certified Hyperbaric Technologist Healogics Philadelphia Pennsylvania Frank L Ross MD Associate Professor Department of Surgery New York University School of Medicine New York New York Associate Director Helen L and Martin S Kimmel Hyperbaric and Advanced Wound Healing Center New York New York Ernest S Chiu MD Associate Professor Department of Surgery New York University School of Medicine New York New York Director Helen L and Martin S Kimmel Hyperbaric and Advanced Wound Healing Center New York New York All authors faculty staff and planners including spouses partners if any in any position to control the content of this CME activity have disclosed that they have no financial relationships with or financial interests in any commercial companies pertaining to this educational activity To earn CME credit you must read the CME article and complete the quiz online answering at least 13 of the 18 questions correctly This continuing educational activity will expire for physicians on April 30 2018 and for nurses on April 30 2020 All tests are now online only take the test at http cme lww com for physicians and www nursingcenter com for nurses Complete CE CME information is on the last page of this article GENERAL PURPOSE To provide information about hyperbaric oxygen therapy HBOT its mechanisms indications and safe applications based on clinical evidence TARGET AUDIENCE This continuing education activity is intended for physicians physician assistants nurse practitioners and nurses with an interest in skin and wound care LEARNING OBJECTIVES OUTCOMES After participating in this educational activity the participant should be better able to 1 Recall the physiology of wound healing and the mechanisms of action of HBOT 2 Identify current applications of HBOT based on clinical evidence as well as its risks and contraindications WWW WOUNDCAREJOURNAL COM 181 ADVANCES IN SKIN WOUND CARE APRIL 2017 Copyright 2017 Wolters Kluwer Health Inc All rights reserved
History of Hyperbaric Oxygen Therapy ABSTRACT The use of HBOT has been attempted since the 1600s but for many decades its use was unfounded as enterprising individuals marketed HBOT as a miracle treatment for a variety of ailments ranging from nervous disorders to influenza to carcinoma In 1956 however Ite Boerema published the first clinical paper on HBOT and for this reason he is recognized as the father of hyperbaric medicine Boerema was the chief of surgery at the University of Amsterdam the Netherlands and he initially wrote about the intraoperative use of hyperbaric oxygen to prolong safe operating times during cardiac surgery 3 4 Boerema and his colleagues at the University of Amsterdam continued to study HBOT and later reported on its beneficial effects for the treatment of necrotizing infections and ischemic leg ulcers 5 6 Since that time numerous groups have investigated this therapy and scientifically sound guidelines for the use of HBOT have been developed Treating chronic wounds and infections are challenging medical problems worldwide Hyperbaric oxygen therapy HBOT the administration of 100 oxygen at pressures greater than 1 4 atmosphere absolute in a series of treatments can be used as an adjunctive therapy in many wound care settings because it improves oxygenation and neovascularization and decreases inflammation in chronic wounds A growing number of studies support the benefits of HBOT for enhancing wound healing and decreasing the likelihood of negative events such as amputation However many practitioners are unfamiliar with HBOT This article provides a general introduction to HBOT reviews the physiology and mechanisms of behind HBOT discusses all the indications for HBOT and explores in depth the clinical evidence for HBOT in the treatment of arterial insufficiencies diabetic ulcers delayed radiation injury and chronic refractory osteomyelitis KEYWORDS chronic wounds diabetic ulcers delayed radiation injury chronic osteomyelitis hyperbaric chamber hyperbaric oxygen therapy nonhealing wounds PHYSIOLOGY AND MECHANISMS The mechanisms that make HBOT an effective treatment for decompression sickness and arterial gas embolism are different from the mechanisms that make HBOT an effective treatment for chronic wounds osteomyelitis and other related conditions This article briefly discusses the mechanisms by which HBOT relieves illnesses caused by gas bubbles and then explores the phases of normal wound healing and how HBOT improves impaired wound healing ADV SKIN WOUND CARE 2017 30 181 90 INTRODUCTION Definition Treatment of Illnesses Caused by Gas Bubbles Hyperbaric oxygen therapy HBOT is a treatment in which patients breathe 100 oxygen while inside a hyperbaric chamber pressurized to greater than sea level 1 atmosphere absolute ATA 1 For clinical efficacy the Undersea and Hyperbaric Medical Society specifies that the pressure must be greater than or equal to 1 4 ATA in clinical practice pressures applied usually range from 2 to 3 ATA 1 2 Treatment is delivered in multiplace chambers Figure 1 or in monoplace chambers Figure 2 In a monoplace chamber a single patient breathes compressed pure oxygen In a multiplace chamber multiple patients are exposed to pressurized air together while they each breathe pure oxygen through a face mask hood or endotracheal tube 1 2 Depending on the indication patients can be treated with up to 3 sessions of HBOT daily 2 In wound care HBOT is used as an adjunct to standard wound care treatment and protocols typically involve HBOT treatments of 1 5 to 2 hours per treatment for 20 to 40 treatments2 and can go even up to 60 treatments Because patients must be subjected to increased atmospheric pressures 1 ATA during true HBOT treatments it is important to note that breathing 100 oxygen at 1 ATA or exposing isolated parts of the body to 100 oxygen does not constitute HBOT 1 ADVANCES IN SKIN WOUND CARE VOL 30 NO 4 Exposing patients to increased pressures causes the reduction in volume of gas filled spaces within the body according to Boyle_s law which states that the pressure and volume of an ideal gas are inversely proportional 2 Reducing the volume of gas bubbles plays an important role in the acute treatment of arterial gas embolism and decompression sickness 2 In a 2014 review of HBOT for air or gas embolism Moon7 reported that a review of 597 cases of arterial gas embolism demonstrated superior patient outcomes with use of HBOT compared with nonrecompression treatment 7 Good outcomes are most likely to occur when patients are treated with HBOT as early as possible following embolism formation 7 Phases of Normal Wound Healing Before discussing how HBOT may improve wound healing it is important to review the phases of normal wound healing These phases are hemostasis inflammation proliferation and maturation Figure 3 Immediately after injury platelets attach to the injured endothelium and the subsequent coagulation cascade triggers the formation of a provisional wound matrix to achieve 182 Copyright 2017 Wolters Kluwer Health Inc All rights reserved WWW WOUNDCAREJOURNAL COM
Figure 1 MULTIPLACE CHAMBER Figure 2 MONOPLACE CHAMBER WWW WOUNDCAREJOURNAL COM 183 ADVANCES IN SKIN WOUND CARE APRIL 2017 Copyright 2017 Wolters Kluwer Health Inc All rights reserved
Figure 3 FOUR PHASES OF NORMAL WOUND HEALING increased oxygen supply to hypoxic tissues has multiple beneficial effects on wound healing 13 Because oxygen cannot be stored in tissue daily HBOT supports an adequate oxygen supply to the site of injury to promote wound healing progression from the inflammatory phase to the proliferative phase Increased oxygen concentrations lead to an increased production of reactive oxygen species and reactive nitrogen species which play important roles in signaling pathways for promoting neovascularization matrix formation and decreasing inflammation Figure 4 2 Hypoxia is a stimulus for angiogenesis New blood vessel formation however is dependent on normal levels of oxygenation Hyperbaric oxygen therapy creates a gradient between tissues of low oxygenation in the center to higher concentrations at the periphery thus creating a driving force conducive to neovascularization Improved neovascularization occurs through both local and distant processes Locally reactive oxygen species and reactive nitrogen species signal an increased production of wound growth factors such as vascular endothelial growth factor the most specific factor for neovascularization transforming growth factor 1 and angiopoietin 2 2 13 Endothelial cells exposed to hyperbaric oxygen exhibit enhanced capillary tube formation and enhanced oxidative stress resistance 2 Although hypoxia stimulates neovascularization chronic hypoxia actually inhibits new vessel formation For this reason hyperoxia induced by HBOT promotes the neovascularization and healing of chronic wounds 12 In addition it is important to distinguish between oxidative stress and oxygen toxicity Excessive reactive oxygen species are associated with harmful effects however studies have shown that the body_s antioxidant defenses protect against the limited number of reactive oxygen species generated by HBOT treatment sessions 2 Hyperbaric oxygen therapy improves neovascularization by acting more distantly from the wound site Increased oxygen leads to increased production of nitric oxide in the bone marrow and multiple studies have shown that this stimulates increased hemostasis This process also activates the inflammatory response which includes leukocyte neutrophil and macrophage migration and activation The inflammatory phase ends a few days after the initial injury with apoptosis of the aforementioned inflammatory response cells 8 9 The proliferative phase begins as the inflammatory phase subsides During the proliferative phase neovascularization occurs via vasculogenesis the recruitment of endothelial progenitor cells from the bone marrow that differentiate into capillaryforming endothelial cells and via angiogenesis the formation of new blood vessels from existing endothelial cells in the wound capillary network 10 Robust neovascularization is vital to the formation of granulation tissue because it supplies the migrating and proliferating dermal and epidermal cells in the wound bed with oxygen and nutrients Key proliferating cells are fibroblasts which create a new matrix of connective tissue to close wound gaps and restore mechanical strength to the wound 9 In the final phase wound contraction and matrix remodeling occur resulting in scar tissue with 80 the tensile strength of unwounded skin 8 9 11 Chronic wounds are characterized by a prolonged inflammatory phase with an inability to progress to the proliferative phase or form newly vascularized granulation tissue 8 9 Accelerating Impaired Healing In HBOT increasing the partial pressure of oxygen inhaled by a patientVby administering 100 oxygen and elevating the pressureVincreases the amount of oxygen that can be dissolved in a patient_s blood serum in accordance with Henry_s law which states that the amount of ideal gas dissolved in solution is directly proportional to its partial pressure 12 During treatment arterial oxygen tension often exceeds 2000 mm Hg and oxygen levels of 200 to 400 mm Hg occur in tissues 2 During tissue repair and wound healing oxygen demand and utilization rates are increased and chronic hypoxia in a wound is associated with reduced or absent wound healing 12 Conversely ADVANCES IN SKIN WOUND CARE VOL 30 NO 4 184 Copyright 2017 Wolters Kluwer Health Inc All rights reserved WWW WOUNDCAREJOURNAL COM
Figure 4 MECHANISMS OF HYPERBARIC OXYGEN THERAPY IN WOUND HEALING neutrophilsVand by inducing vasoconstriction to decrease local edema 13 Macrophages are impacted in 2 very different ways First HBOT has been shown to reduce expression of proinflammatory cytokines by monocyte macrophages in both animal and human studies 2 13 Second HBOT promotes macrophage chemotaxis to facilitate the clean up of cellular debris at the wound site Increased oxygen also enhances the bactericidal activity of leukocytes 12 13 Finally HBOT inhibits neutrophil 2 integrin adhesion in both animals and humans and this mechanism has been shown to decrease tissue reperfusion injuries without reducing the neutrophils_ antibacterial function 2 In summary chronic wounds are characterized by hypoxia impaired angiogenesis and prolonged inflammation Hyperbaric oxygen therapy is a successful adjunctive treatment for wound healing because it acts through diverse mechanisms to promote angiogenesis and decrease inflammation vasculogenic stem progenitor cell mobilization from the bone marrow in healthy human subjects diabetic patients and patients previously treated with radiation therapy leading to more stem cells recruited to skin wounds and accelerated blood vessel formation 2 14 15 Hyperoxia also improves the function of endothelial progenitor cells once they arrive at the wound site to differentiate into capillary forming endothelial cells 2 Extracellular matrix formation is an oxygen dependent process linked closely to neovascularization 2 Fibroblast growth factor production is also increased by HBOT promoting fibroblast migration and proliferation 2 12 13 Increased oxygen stimulates the proliferating fibroblasts to produce collagen at increased rates and also enhances collagen cross linking to improve tissue tensile strengths 2 12 Hyperoxia also promotes decreased inflammation by impacting 3 major inflammatory cell typesVmacrophages leukocytes and WWW WOUNDCAREJOURNAL COM 185 ADVANCES IN SKIN WOUND CARE APRIL 2017 Copyright 2017 Wolters Kluwer Health Inc All rights reserved
HYPERBARIC OXYGEN THERAPY INDICATIONS ulcer and more than 10 of these ulcers will lead to amputation 13 More than 60 of nontraumatic lower extremity amputations occur in patients with diabetes 17 In addition long term studies have found that 45 of patients with a diagnosis of diabetic foot ulcers are deceased at 5 year follow up 18 Diabetic peripheral neuropathy that leads to the loss of protective sensation in the foot peripheral arterial disease PAD limited foot mobility and foot deformities are the main challenges to the prevention and treatment of diabetic foot ulcers 19 The National Health and Nutrition Examination Survey of 4769 participants found that 13 9 of patients with diabetes also had PAD 20 Because PAD independently impairs wound healing it significantly increases the risk of lower extremity amputation in patients odds ratio OR 12 97 95 confidence interval CI 3 44 48 88 21 These nonhealing wounds also put patients at continuous risk of local and systemic infection sepsis and death 19 Treatment of diabetic and or ischemic foot ulcers requires a multimodal approach involving local wound care good glycemic control revascularization of ischemic limbs treatment of infections and pressure off loading 13 Unfortunately even with optimal care complete wound healing rates can be as low 60 a year 13 Hyperbaric oxygen therapy has been used as an adjunctive therapy for patients with refractory ulcers A range of studies have examined the efficacy of HBOT for improving wound healing and reducing amputation rates in patients with diabetic ulcers Earlier studies reported very favorable results which are summarized in a 2009 systematic review by Goldman et al 13 22 Goldman et al22 considered data from 8 studies ranging from retrospective case series to randomized controlled trials and concluded that in diabetic patients HBOT significantly improved chances of wound healing OR 9 992 95 CI 3 972 25 123 and reduced chances of amputation OR 0 242 95 CI 0 137 0 428 22 In 2014 Stoekenbroek et al13 performed a systematic review of randomized controlled trials that included 3 studies of ischemic diabetic ulcers measured by ankle brachial index great toebrachial index ankle blood pressure or toe blood pressure 2 studies of nonischemic ulcers and 2 studies that did not specify ulcer type Two of the studies on ischemic diabetic ulcers found that HBOT improved rates of complete wound healing at 1 year follow up number needed to treat NNT 1 8 95 CI 1 1 4 6 but did not impact amputation rates whereas the third study did not report on wound healing rates but found that HBOT significantly decreased major amputation rates NNT 4 2 95 CI 2 4 17 13 23 25 The 2 studies on nonischemic ulcers reported no significant differences in wound healing or amputation rates after HBOT 13 26 27 Finally 1 of the studies that did not specify ulcer type reported a significant decrease in major amputation rates following HBOT NNT 2 9 95 CI 2 1 4 8 13 28 In 1976 the Undersea and Hyperbaric Medical Society at the time Undersea Medical Society began maintaining a list of conditions for which HBOT is medically indicated since its development this list is updated every 2 years to include new indications based on available clinical evidence Table 1 5 This review focuses on HBOT_s applications in wound care Some of the most common chronic wounds encountered in medical practice result from diabetes arterial and or venous disease and radiation therapy 6 The authors discuss the clinical evidence for HBOT in the treatment of arterial insufficiencies diabetic wounds radiation injury and chronic refractory osteomyelitis APPLICATIONS OF HYPERBARIC OXYGEN THERAPY IN THE WOUND CARE SETTING Arterial Insufficiency and Diabetic Wounds The Undersea and Hyperbaric Medical Society categorizes diabetic wounds under the indication of arterial insufficiencies because much of the existing HBOT literature discusses wounds that are concurrently diabetic and ischemic 1 Consequently this article discusses the clinical evidence for these conditions together Treating diabetic ulcers of the lower extremity is an important issue in healthcare According to the World Health Organization an estimated 347 million people suffer from diabetes mellitus 16 Approximately 1 in 20 persons with diabetes will develop a foot Table 1 INDICATIONS FOR HYPERBARIC OXYGEN THERAPY 1 Air or gas embolism 2 Carbon monoxide poisoning 3 Clostridial myositis and myonecrosis gas gangrene 4 Crush injury compartment syndrome and other acute traumatic ischemias 5 Decompression sickness 6 Arterial insufficiencies 7 Severe anemia 8 Intracranial abscess 9 Necrotizing soft tissue infections 10 Osteomyelitis refractory 11 Delayed radiation injury soft tissue and bony necrosis 12 Compromised grafts and flaps 13 Acute thermal burn injury 14 Idiopathic sudden sensorineural hearing loss ADVANCES IN SKIN WOUND CARE VOL 30 NO 4 186 Copyright 2017 Wolters Kluwer Health Inc All rights reserved WWW WOUNDCAREJOURNAL COM
and anus In 1 randomized controlled trial significantly more patients receiving HBOT versus a sham treatment experienced at least Bmoderate healing of proctitis 87 5 vs 62 5 P 0009 30 33 In the head and neck a randomized controlled trial of patients who had soft tissue flap reconstruction in previously irradiated areas found that patients treated with HBOT were less likely to develop wound infection wound dehiscence and delayed wound healing 30 Neither the Cochrane review nor the systematic review by Hoggan and Cameron30 found strong evidence supporting the use of HBOT for radiation injury to other tissues such as radiationinduced cystitis and irradiated neurologic tissue 30 32 As in the case of diabetic ulcers the number of studies on HBOT for radiation injury is limited and they involve only a small number of patients However the body of literature increases yearly and these studies generally support the benefit of HBOT For example a 2015 retrospective study reported successful or improved outcomes following HBOT in 95 7 of patients with osteoradionecrosis n 23 and 88 1 with soft tissue radiation necrosis n 42 34 Thus HBOT is a promising adjunctive treatment for several types of radiation injuries More recently the 2015 Cochrane review of HBOT for chronic wounds examined 8 randomized controlled trials of patients with diabetic ulcers Based on these studies they reported that HBOT appeared to improve short term wound healing up to 6 weeks and might decrease rates of major amputation More studies on long term wound healing were needed to draw further conclusions and there were no trials that studied arterial ulcers independently 6 Ultimately the literature most strongly supports use of HBOT in cases of ischemic diabetic ulcers to improve wound healing and decrease amputation rates Current evidence for the use of HBOT in nonischemic diabetic ulcers and in nondiabetic arterial ulcers is more limited A recent study by Margolis et al29 used a longitudinal cohort study looking at more than 6000 patients with diabetic foot ulcers and adequate arterial inflow and response to HBOT They concluded that HBOT neither reduced the risk of amputation nor improved the likelihood that the wound would heal 29 Past studies have generally been hindered by small sample sizes variable HBOT regimens and differing outcome measures leading to inconsistent results 6 13 Chronic diabetic and or ischemic ulcers are a major healthcare challenge that HBOT can help to address and additional studies would clarify and perhaps expand its clinical applications Chronic Refractory Osteomyelitis Osteomyelitis is an infection of bone or bone marrow usually caused by pyogenic bacteria or mycobacteria Refractory osteomyelitis is defined as a chronic osteomyelitis that persists or recurs after appropriate interventions have been performed or where acute osteomyelitis has not responded to accepted management techniques 35 Staphylococcus aureus is the most common cause of bone infection in adults Staphylococcus epidermidis Pseudomonas aeruginosa Serratia marcescens and Escherichia coli may also be isolated especially in cases of chronic osteomyelitis caused by contiguous soft tissue infection 35 Standard treatment of chronic osteomyelitis involves appropriate antibiotic therapy and surgical debridement of infected or necrotic tissue However overall recurrence rates after prolonged antibiotic therapy and surgical debridement remain approximately 30 at 1 year and recurrence rates for cases caused by P aeruginosa are close to 50 35 Hyperbaric oxygen therapy is an adjunctive treatment for patients with chronic refractory osteomyelitis Because chronic refractory osteomyelitis is less common than diabetic ulcers and radiation injury it is more difficult to study and at the time of writing no randomized controlled trials have evaluated the efficacy of HBOT for this indication However a number of case series and cohort studies suggest that HBOT improves clinical outcomes A systematic review by Goldman et al22 summarized the findings of 15 observational studies on HBOT for recalcitrant osteomyelitis 14 of these studies reported positive findings Delayed Radiation Injury Radiation therapy is a common and well established treatment for many malignancies 30 Although it is an effective treatment radiation injury can occur to the normal tissues surrounding the tumor This injury can occur months to years after radiation therapy and occurs as a result of microvasculature deterioration and increased fibrosis leading to tissue ischemia 30 31 Without sufficient oxygenation the tissue cannot maintain normal function and integrity and ulcers or areas of radionecrosis can develop Some of the most common radiation injuries are osteoradionecrosis laryngeal radionecrosis dermal soft tissue radionecrosis radiationinduced cystitis and radiation induced proctitis 32 Because HBOT increases oxygen delivery to tissues it was proposed as an adjunctive treatment for such injuries The current literature supports the use of HBOT for several different types of radiation related injuries The 2012 Cochrane review on HBOT for late radiation tissue injury examined 11 randomized controlled trials and concluded that HBOT may improve outcomes in patients with radiation injury to the head neck rectum and anus such as after hemimandibulectomy with mandible reconstruction and in cases of radiation proctitis 32 Subsequently Hoggan and Cameron30 conducted a systematic review in 2014 that yielded similar findings supporting the use of HBOT for radiation tissue injury to the head neck rectum WWW WOUNDCAREJOURNAL COM 187 ADVANCES IN SKIN WOUND CARE APRIL 2017 Copyright 2017 Wolters Kluwer Health Inc All rights reserved
whereas 1 study reported equivocal findings Overall the median remission rate was 89 range 37 100 for the 309 patients in the 15 studies 22 A subsequent retrospective study reported successful or improved outcomes in 82 6 of patients n 23 who received HBOT for chronic refractory osteomyelitis 34 Thus current data suggest that HBOT is a useful adjunct in the treatment of chronic refractory osteomyelitis Additional studies particularly randomized controlled trials would help to validate its efficacy Figure 5 RIGHT MID PLANTAR DIABETIC FOOT ULCER RISKS AND CONTRAINDICATIONS Hyperbaric oxygen therapy is a safe treatment modality with few serious adverse effects and contraindications Table 2 Most adverse effects are minor and reversible Patients may experience progressive myopia during treatment due to pressure induced lens deformity but this typically reverses within 6 weeks of treatment termination 2 12 22 Hyperbaric oxygen therapy can also cause cataracts to mature more quickly but does not cause new cataract formation 22 Barotrauma to the ear and sinuses is another common adverse effect particularly in older patient populations but most cases are mild and reversible 12 22 Serious adverse effects of HBOT resulting from oxygen toxicity are seizures congestive heart failure CHF exacerbation pulmonary edema and retinal changes but these are rare 12 For example reported incidences of grand mal seizures following HBOT range from 1 to 4 cases in 10 000 patient treatments 2 The most serious contraindication to HBOT is an unrecognized and or untreated pneumothorax which would worsen under chamber pressure 12 Relative contraindications to HBOT include febrile illness which lowers the central nervous system seizure toxicity threshold poorly controlled seizure disorder and hyperthyroidism 22 Because oxygen is a vasoconstrictor and HBOT may increase cardiac afterload CHF is also a relative contraindication for anyone with an ejection fraction of less than 30 Other relative contradictions include patients with underlying pulmonary disease such as chronic obstructive pulmonary disease and severe claustrophobia 22 Table 2 POSSIBLE ADVERSE EVENTS AND CONTRAINDICATIONS OF HYPERBARIC OXYGEN THERAPY Minor Adverse Events Barotrauma to ears and sinuses Myopia Accelerated cataract maturation Major Adverse Events Seizures Congestive heart failure CHF exacerbation SAFETY PRECAUTIONS Pulmonary edema The primary safety concern during the administration of HBOT is the prevention of fire For a fire to occur in a hyperbaric chamber 3 elements must exist heat ignition source oxygen This is known as the fire triangle Patients must go through a daily checklist prior to entering the chamber In addition they are required to wear cotton based hospital gowns scrubs 100 cotton or 50 50 cotton polyester blend No outside clothing or shoes are allowed in the chamber Patients undergo a pretreatment education process and a list of items materials that are Retinal changes Relative Contraindications Febrile illness Seizure disorder Hyperthyroidism CHF Pulmonary disease eg chronic obstructive pulmonary disease Severe claustrophobia Absolute Contraindications Untreated pneumothorax ADVANCES IN SKIN WOUND CARE VOL 30 NO 4 188 Copyright 2017 Wolters Kluwer Health Inc All rights reserved WWW WOUNDCAREJOURNAL COM
CONCLUSIONS Figure 6 Hyperbaric oxygen therapy has been in medical use for half a century Its mechanisms of action in the healing of chronic wounds include promoting neovascularization and decreasing inflammation Clinical studies have demonstrated its efficacy in treating various conditions and it is currently used for 14 different indications For example it is a useful adjunctive therapy in the treatment of ischemic diabetic wounds radiation induced wounds and chronic osteomyelitis Additional studies are needed to determine the full benefits of HBOT HEALED RIGHT MID PLANTAR DIABETIC FOOT ULCER PRACTICE PEARLS Hyperbaric oxygen therapy is a treatment in which patients breathe 100 oxygen while inside a pressurized hyperbaric chamber For wound care HBOT treatment regimens consist of 1 5 to 2 hours per treatment for 20 to 40 treatments and up to 60 treatments if needed The Undersea and Hyperbaric Medical Society maintains an evidence based list of indications for HBOT there are currently 14 indications These 14 indications include arterial insufficiency wounds ie ischemic diabetic ulcers delayed radiation injury ie to the soft tissue osteoradionecrosis cystitis proctitis and chronic refractory osteomyelitis Common and reversible adverse effects of HBOT include barotrauma to the ear and myopia Serious adverse events are rare but include seizures CHF exacerbation pulmonary edema and retinal changes Untreated pneumothorax is an absolute contraindication to HBOT forbidden in the chamber is provided to them Examples include newspaper hairspray nail polish cell phones hand warmers heating pads and perfume Items that may cause sparks or damage the acrylic tube of monoplace chambers are also prohibited Examples include keys coins jewelry and toys REFERENCES 1 Undersea and Hyperbaric Medical Society Indications for hyperbaric oxygen therapy https www uhms org resources hbo indications html Last accessed January 25 2017 2 Thom SR Hyperbaric oxygen its mechanisms and efficacy Plast Reconstr Surg 2011 127 Suppl 1 131S 41S 3 Camporesi EM Bosco G Mechanisms of action of hyperbaric oxygen therapy Undersea Hyperb Med 2014 41 247 52 4 Oztrk F Ermertcan AT Inanir I Hyperbaric oxygen therapy for the management of chronic wounds Cutan Ocul Toxicol 2013 32 72 7 5 Dauwe PB Pulikkottil BJ Lavery L Stuzin JM Rohrich RJ Does hyperbaric oxygen therapy work in facilitating acute wound healing a systematic review Plast Reconstr Surg 2014 133 208e 15e 6 Kranke P Bennett MH Martyn St James M Schnabel A Debus SE Weibel S Hyperbaric oxygen therapy for chronic wounds Cochrane Database Syst Rev 2015 6 CD004123 7 Moon RE Hyperbaric oxygen treatment for air or gas embolism Undersea Hyperb Med 2014 41 159 66 8 Demidova Rice TN Hamblin MR Herman IM Acute and impaired wound healing pathophysiology and current methods for drug delivery part 1 normal and chronic wounds biology causes and approaches to care Adv Skin Wound Care 2012 25 304 14 9 Reinke JM Sorg H Wound repair and regeneration Eur Surg Res 2012 49 35 43 10 Stavrou D Neovascularization in wound healing J Wound Care 2008 17 298 300 CASE EXAMPLE The patient is a 46 year old man employed in a job that requires him to be on his feet most of the day lifting heavy parcels He has type 2 diabetes mellitus and a prior amputation of his right fifth toe from a diabetic foot infection He presented with a large ulcer on the plantar surface of his right foot that penetrated to the joints of his third and fourth right toes and was classified as a grade III Wagner diabetic foot ulcer When other therapies failed the wound was treated topically with a silver alginate and off loading was provided by total contact casting He received 30 90 minute treatments of HBOT at 2 0 ATA The patient progressed to complete wound healing after 10 weeks which included the HBOT Pretreatment and posttreatment photographs are provided Figures 5 and 6 WWW WOUNDCAREJOURNAL COM 189 ADVANCES IN SKIN WOUND CARE APRIL 2017 Copyright 2017 Wolters Kluwer Health Inc All rights reserved
23 Lo ndahl M Katzman P Nilsson A Hammarlund C Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes Diabetes Care 2010 33 998 1003 24 Abidia A Laden G Kuhan G et al The role of hyperbaric oxygen therapy in ischemic diabetic lower extremity ulcers a double blind randomised controlled trial Eur J Vasc Endovasc Surg 2003 25 513 8 25 Faglia E Favales F Aldeghi A et al Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer a randomized study Diabetes Care 1996 19 1338 43 26 Kessler L Bilbault P Ortga F et al Hyperbaric oxygenation accelerates the healing rate of nonischemic chronic diabetic foot ulcers a prospective randomized study Diabetes Care 2003 26 2378 82 27 Ma L Li P Shi Z Hou T Chen X Du J A prospective randomized controlled study of hyperbaric oxygen therapy effects on healing and oxidative stress of ulcer tissue in patients with a diabetic foot ulcer Ostomy Wound Manage 2013 59 3 18 24 28 Duzgan AP Satir HZ Ozozan O Saylam B Kulah B Coskun F Effect of hyperbaric oxygen therapy on healing of diabetic foot ulcers J Foot Ankle Surg 2008 47 515 9 29 Margolis DJ Gupta J Hoffstad O Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and the prevention of amputation a cohort study Diabetes Care 2013 36 1961 66 30 Hoggan BL Cameron AL Systematic review of hyperbaric oxygen therapy for the treatment of non neurological soft tissue radiation related injuries Support Care Cancer 2014 22 1715 26 31 Niezgoda JA Serena TE Carter MJ Outcomes of radiation injuries using hyperbaric oxygen therapy an observational cohort study Adv Skin Wound Care 2016 29 12 9 32 Bennett MH Feldmeier J Hampson NB Smee R Milross C Hyperbaric oxygen therapy for late radiation tissue injury Cochrane Database Syst Rev 2012 5 CD005005 33 Clarke RE Tenorio LM Hussey JR et al Hyperbaric oxygen treatment of chronic refractory radiation proctitis a randomized and controlled double blind crossover trial with long term follow up Int J Radiat Oncol Biol Phys 2008 72 134 43 34 Skeik N Porten BR Isaacson E et al Hyperbaric oxygen treatment outcome for different indications at a single center Ann Vasc Surg 2015 29 206 214 35 Hatzenbuehler J Pulling TJ Diagnosis and management of osteomyelitis Am Fam Physician 2011 84 1027 33 11 Levenson SM Geever EF Crowley LV Oates JF 3rd Berard CW Rosen H The healing of rat skin wounds Ann Surg 1965 161 293 308 12 Howard MA Asmis R Evans KK Mustoe TA Oxygen and wound care a review of current therapeutic modalities and future direction Wound Repair Regen 2013 21 503 11 13 Stoekenbroek RM Santema TB Legemate DA Ubbink DT van den Brink A Koelemay MJ Hyperbaric oxygen for the treatment of diabetic foot ulcers a systematic review Eur J Vasc Endovasc Surg 2014 47 647 55 14 Thom SR Bhopale VM Velazquez OC Goldstein LJ Thom LH Buerk DG Stem cell mobilization by hyperbaric oxygen Am J Physiol Heart Circ Physiol 2006 290 H1378 86 15 Thom SR Milovanova TN Yang M et al Vasculogenic stem cell mobilization and wound recruitment in diabetic patients increased cell number and intracellular regulatory protein content associated with hyperbaric oxygen therapy Wound Repair Regen 2011 19 149 61 16 World Health Organization Diabetes www who int mediacentre factsheets fs312 en Last accessed January 25 2017 17 National Diabetes Fact Sheet 2011 Center for Disease Control Web site https www cdc gov diabetes pubs pdf ndfs_2011 pdf Last accessed January 25 2017 18 Morbach S Furchert H Groblinghoff U et al Long term prognosis of diabetic foot patients and their limbs amputation and death over the course of a decade Diabetes Care 2012 35 2021 7 19 Fedorko L Bowen JM Jones W et al Hyperbaric oxygen therapy does not reduce indications for amputation in patients with diabetes with nonhealing ulcers of the lower limb a prospective double blind randomized controlled clinical trial Diabetes Care 2016 39 392 9 20 Cheung CL Lam KS Cheung BM Diabetes is associated with increased risks of low lean mass and slow gait speed when peripheral artery disease is present J Diabetes Complications 2016 30 306 11 21 Pemayun TG Naibaho RM Novitasari D Amin N Minuljo TT Risk factors for lower extremity amputation in patients with diabetic foot ulcers a hospital based case control study Diabet Foot Ankle 2015 6 29629 22 Goldman RJ Hyperbaric oxygen therapy for wound healing and limb salvage a systematic review PM R 2009 1 471 89 For more than 153 additional continuing education articles related to Skin and Wound Care topics go to NursingCenter com CE DOs only All other healthcare professionals participating in this activity will receive a certificate of participation that may be useful to your individual profession s CE requirements CONTINUING MEDICAL EDUCATION INFORMATION FOR PHYSICIANS Lippincott Continuing Medical Education Institute Inc is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians CONTINUING EDUCATION INSTRUCTIONS Lippincott Continuing Medical Education Institute Inc designates this journal based CME activity for a maximum of 1 AMA PRA Category 1 CreditTM Physicians should claim only the credit commensurate with the extent of their participation in the activity PROVIDER ACCREDITATION INFORMATION FOR NURSES Lippincott Williams Wilkins publisher of the Advances in Skin Wound Care journal will award 1 0 contact hour for this continuing nursing education activity the article beginning on page 181 For nurses who wish to take the test for CE contact Read hours visit www nursingcenter com For physicians who wish to take the test for CME credit visit http cme lww com will need to register your personal CE Planner account before taking online tests Your planner You will keep track of all your Lippincott Williams Wilkins online CE activities for you is only one correct answer for each question A passing score for this test is 13 correct There answers If you pass you can print your certificate of earned contact hours or credit and access the answer key Nurses who fail have the option of taking the test again at no additional cost Only the first entry sent by physicians will be accepted for credit LWW is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center s Commission on Accreditation This activity is also provider approved by the California Board of Registered Nursing Provider Number CEP 11749 for 1 0 contact hour LWW is also an approved provider by the District of Registration Deadline April 30 2019 nurses April 30 2018 physicians Columbia Georgia and Florida CE Broker 50 1223 Your certificate is valid in all states PAYMENT AND DISCOUNTS OTHER HEALTH PROFESSIONALS This activity provides ANCC credit for nurses and AMA PRA Category 1 CreditTM for MDs and ADVANCES IN SKIN WOUND CARE VOL 30 NO 4 The registration fee for this test is 12 95 for nurses 22 for physicians 190 Copyright 2017 Wolters Kluwer Health Inc All rights reserved WWW WOUNDCAREJOURNAL COM
medicina Review A General Overview on the Hyperbaric Oxygen Therapy Applications Mechanisms and Translational Opportunities Miguel A Ortega 1 2 3 Oscar Fraile Martinez 1 2 Cielo Garc a Montero 1 2 Enrique Callej n Pel ez 4 Miguel A S ez 1 2 5 Miguel A lvarez Mon 1 2 Natalio Garc a Honduvilla 1 2 Jorge Monserrat 1 2 Melchor lvarez Mon 1 2 6 Julia Bujan 1 2 and Mar a Luisa Canals 7 1 2 3 4 5 6 Citation Ortega M A Fraile Martinez O Garc a Montero C Callej n Pel ez E S ez M A lvarez Mon M A Garc a Honduvilla N Monserrat J lvarez Mon M Bujan J et al A General Overview on the Hyperbaric Oxygen Therapy Applications Mechanisms and Translational Opportunities Medicina 2021 57 864 https doi org 10 3390 medicina57090864 Academic Editors Costantino Balestra and Jacek Kot Received 26 July 2021 Accepted 20 August 2021 Published 24 August 2021 Publisher s Note MDPI stays neutral with regard to jurisdictional claims in 7 Department of Medicine and Medical Specialities Faculty of Medicine and Health Sciences University of Alcal 28801 Alcala de Henares Spain cielo gmontero gmail com C G M msaega1 oc mde es M A S maalvarezdemon icloud com M A M natalio garcia uah es N G H jorge monserrat uah es J M mademons gmail com M M mjulia bujan uah es J B Ram n y Cajal Institute of Sanitary Research IRYCIS 28034 Madrid Spain Cancer Registry and Pathology Department Hospital Universitario Principe de Asturias 28806 Alcala de Henares Spain Underwater and Hyperbaric Medicine Service Central University Hospital of Defence UAH Madrid 28801 Alcala de Henares Spain ecalpel fn mde es Pathological Anatomy Service Central University Hospital of Defence UAH Madrid 28801 Alcala de Henares Spain Immune System Diseases Rheumatology Oncology Service an Internal Medicine University Hospital Pr ncipe de Asturias CIBEREHD 28806 Alcala de Henares Spain ISM IMHA Research Chair Former of IMHA International Maritime Health Association 43001 Tarragona Spain mlcanalsp gmail com Correspondence miguel angel ortega92 gmail com M A O oscarfra 7 hotmail com O F M Tel 34 91 885 40 45 M A O Fax 34 91 885 48 85 M A O Abstract Hyperbaric oxygen therapy HBOT consists of using of pure oxygen at increased pressure in general 2 3 atmospheres leading to augmented oxygen levels in the blood Hyperoxemia and tissue Hyperoxia The increased pressure and oxygen bioavailability might be related to a plethora of applications particularly in hypoxic regions also exerting antimicrobial immunomodulatory and angiogenic properties among others In this review we will discuss in detail the physiological relevance of oxygen and the therapeutical basis of HBOT collecting current indications and underlying mechanisms Furthermore potential areas of research will also be examined including inflammatory and systemic maladies COVID 19 and cancer Finally the adverse effects and contraindications associated with this therapy and future directions of research will be considered Overall we encourage further research in this field to extend the possible uses of this procedure The inclusion of HBOT in future clinical research could be an additional support in the clinical management of multiple pathologies Keywords hyperbaric oxygen therapy HBOT Hyperoxia wound healing antimicrobial properties Coronavirus Disease 19 COVID 19 published maps and institutional affiliations 1 Introduction Copyright 2021 by the authors Licensee MDPI Basel Switzerland This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution CC BY license https creativecommons org licenses by 4 0 Hyperbaric oxygen therapy HBOT is a therapeutical approach based on exposure to pure concentrations of oxygen O2 in an augmented atmospheric pressure According to the Undersea and Hyperbaric Medical Society UHMS this pressure may equal or exceed 1 4 atmospheres atm 1 However all current UHMS approved indications require that patients breathe near 100 oxygen while enclosed in a chamber pressurized to a minimum of 2 ATA 2 The first documented use of hyperbaric medical therapy was in 1662 by Henshaw a British physician who placed patients in a container with pressurized air Interestingly it was conducted before the formulation of the Boyle Mariotte Law which described the Medicina 2021 57 864 https doi org 10 3390 medicina57090864 https www mdpi com journal medicina
Medicina 2021 57 864 2 of 25 relationship between the pressure and volume of a gas and prior to the discovery of O2 by John Priestly over 100 years later 3 Afterwards the pathway of HBOT in medical care was retarded by the observation of possible O2 derived adverse effects at 100 concentrations by Lavoisier and Seguin in 1789 Years later in 1872 Paul Bert considered the father of the hyperbaric physiology described the physiological basis of pressurized air in the human body also defining the neurotoxic effects of O2 in the human body consequently named the Paul Bert effect 4 followed by the description of the pulmonary toxicity of O2 by Lorrain Smith 5 Simultaneously a growing interest in the use of HBOT in the treatment of different affections was reported including treatment for divers who suffered decompression sickness during World War II 6 Since then a plethora of studies were prompted with hundreds of facilities based on HBOT being established at the beginning of the 21st century 7 Currently there are 14 approved indications for HBOT including a wide variety of complications like air embolism severe anemia certain infectious diseases or idiopathic sensorial hearing loss In addition in the last European Consensus Conference on Hyperbaric Medicine highlighted the use of HBOT as a primary treatment method for certain conditions according to their moderate to high degree of evidence e g after carbon monoxide CO poisoning or as a potential adjuvant to consider in other conditions with a moderate amount of scientific evidence e g Diabetic foot 8 In this work we will review in detail the basis of O2 as a therapeutical agent and the principles of hyperbaric medicine regarding most relevant applications concerning HBOT and potential implications for different approaches including COVID 19 2 Physiological Role of Oxygen in the Organism O2 is a frequently disregarded nutrient because of its particular access inside the human body through the lungs instead of the gastrointestinal tract typical of all other nutrients 9 O2 is key for human cells to perform so called aerobic respiration which takes places in the mitochondria Here O2 acts as an electron acceptor finally leading to ATP synthesis in a process known as oxidative phosphorylation From an evolutionary perspective the uptake of O2 was the origin of eukaryotic cells emerging as a result of an endosymbiotic relationship between prokaryotic cells archaea and eubacteria which were capable of using this nutrient 10 This fact represented an adaptative advantage with regard to those cells unable to utilize it complex organisms were coevolving with O2 thus becoming an essential nutrient for our cells 11 In a simple manner O2 is introduced in our body by two distinguished process ventilation in which gases are transported from the environment to the bronchial tree and diffusion where an equilibrium in the distribution of O2 between alveoli space and blood is reached Given that the partial pressure of O2 PO2 here is low and rich in carbon dioxide CO2 gas exchange occurs 12 Simultaneously the difference in the pressure and volume in the chest wall and lungs are essential to permit the oxygen flow as atmospheric pressure does not vary at all 13 Once in the bloodstream O2 is mostly bound to haemoglobin Hb in the erythrocytes and to a little extent in a dissolved form being systemically distributed Then oxygen exchange is produced between the microcirculatory vessels Not only capillaries but also arterioles and venules and the rest of the tissues due to the different partial pressure of O2 and the Hb oxygen saturation SO2 which is also dependant on other variables like temperature PCO2 and pH among others 14 If however there is a lack of oxygen in the tissue it may appear a condition designed as hypoxia This may be due to low O2 content in the blood Hypoxemia which may be a consequence of either a disruption in the blood flow to the lungs Perfusion airflow to the alveoli Ventilation or problems in the gas diffusion in the haemato alveolar barrier Furthermore low blood supply ischaemia or difficulties in the O2 delivery may also be responsible for tissue hypoxia 15 Consequently within cells there are specific sensors named as Hypoxia inducible factors HIF that under hypoxic conditions will bind to the hypoxia response element HRE thereby regulating a wide variety of cellular pro
Medicina 2021 57 864 3 of 25 cesses 16 Occasionally hypoxia might provide favourable implications for health for instance during early developmental stages 17 or in the case of intermittent exposures 18 Nonetheless hypoxia mostly induce a pathological stress for cells that is closely related with the appearance and progress of a broad spectrum of diseases 19 As a result oxygen has been proposed as a potential therapeutic agent for patients undergoing different acute or chronic conditions 20 21 As targeting cellular hypoxia is a promising but still an emerging approach 22 clinical management of hypoxia is directed to modulate global hypoxemia and oxygen delivery within the tissues 23 In this context HBOT arises as an extraordinary support in the handling of hypoxia and other hypoxia related phenomena by increasing blood and tissue levels of oxygen 24 Hereunder we will describe the principles and mechanisms of action of HBOT regarding its therapeutical basis and specific considerations of this therapy 3 Principles of Hyperbaric Oxygen Therapy Therapeutical Basis As above mentioned HBOT consist of the supply of pure oxygen under augmented pressure This procedure is conducted in a monoplace or multiplace chamber if there are only one or various patients undergoing this procedure respectively In the first case the chambers are usually compressed with O2 whereas in the second people breath oxygen individually through a face mask hood or an endotracheal tube 25 In the case of critically ill patients it seems that multiplace chambers allow a better monitoring of the vital functions in comparison to monoplace chambers although the use of the latter are also safe and well tolerated by patients 26 27 Depending on the protocol the estimated duration of session varies from 1 5 to 2 h and may be performed from one to three times daily being given among 20 to 60 therapeutical doses depending on the condition 28 Frequently this method utilizes between 2 to 3 atms of pressure Nevertheless it has also been obtained promising results in some studies from 3 atms as it may be associated with a plethora of adverse effects 31 Moreover it is not possible to breath pure O2 at higher pressures than 2 8 atm and in those cases it is accompanied with other gases like helium nitrogen or ozone The alternative normobaric oxygen therapy NBOT utilizes oxygen at 1 atm of pressure In comparison with HBOT NBOT is cheaper and easier to apply and it could be found in almost all hospitals as it does not require hyperbaric chambers 32 However some studies have reported a reduced efficacy of NBOT in comparison with HBOT 33 34 therefore showing the relevance of HBOT for certain conditions Conversely the use of NBOT could be critical for patients suffering from some maladies in absence of HBOT facilities The therapeutical basis of hyperbaric oxygenation are consequence of three main factors 1 By breathing 100 O2 a positive gradient is created hence favouring diffusion for hyperoxigenated lungs to hypoxic tissues 2 due to the high pressure O2 concentration in the blood raises according to Henry s Law the amount of dissolved gas within a liquid is directly proportional to its partial pressure and 3 it decreases the size of gas bubbles in the blood following Boyle Mariotte Law and Henry s Law 6 In other words the creation of a hyperbaric environment with pure oxygen permits a significant increment of the oxygen supply to blood Hyperoxemia and to the tissues Hyperoxia even without the contribution from Hb 35 Thus HBOT provides multiple effects in the organism and it could be used to correct tissue hypoxia chronic hypoxemia and to aid in the clinical management of different pathological processes including wound healing necrosis or reperfusion injuries 36 Contrary to hypoxia the human body has not developed any specific adaptation to hyperoxia Interestingly the exposure to intermittent hyperoxia share many of the mediators and cellular mechanisms which are induced by hypoxia This is called the hyperoxic hypoxic paradox 37 Importantly it does not have to be considered a negative
Medicina 2021 57 864 4 of 25 property As occurring with intermittent hypoxia the submitting of short term hyperoxia may provide favourable outcomes in the cell The explanation resides in a crucial concept in biology the hormesis which correlates the type of response obtained with the dose received 38 From a molecular perspective high PO2 in the tissues may have important implications in the cellular signalling particularly through increasing the production of reactive oxygen species ROS and reactive nitrogen species RNS These changes induce multiple effects in the organism including the synthesis of different growth factors improving neovascularization or showing immunomodulatory properties among others therefore exerting its clinical efficacy 39 40 Moreover HBOT upregulates HIF by ROS RNS and Extracellular Regulated Kinases ERK1 ERK2 pathway 37 41 In the same manner an excessive production of ROS and RNS due to hyperoxia may lead to the appearance of oxidative stress DNA damage metabolic disturbances endothelial dysfunction acute pulmonary injury and neurotoxicity 42 As hyperbaric O2 may provide both beneficial and adverse effects it is essential to balance the different factors to clinically recommend or reject HBOT 43 Due to the physics of HBOT it is not easy to design adequate studies and clinical trials to fully endorse its use Despite this there are some predictive models that may be an additional tool to evaluate what patients may benefit the most from receiving this therapy considering distinct therapeutical approaches if necessary 44 In Figure 1 conditions and characteristics of hyperbaric chambers are illustrated besides the main effect of pressurized O2 administration Below main applications and translational applications of HBOT will be subsequently discussed in order to review the actual importance of this procedure in current clinical practice and potential uses Figure 1 Illustration of a monoplace hyperbaric chamber and the effect of hyperbaric O2 Pressurized O2 2 3 atm at 100 concentration is administered normally during 1 5 2 h per session and repeated three times a day Depending on the clinical condition sessions vary in number from 20 to 60 The inhalated air comes from an external elevated PO2 hence positive gradient allows higher O2 entry which per diffusion will be higher also in alveoli bloodstream and therefore there will be greater arrival to tissues This effect of hyperoxemia and hyperoxia is independent from haemoglobin Hb then will lessen hypoxia in tissues This will result in a major supply of reactive oxygen species ROS and reactive nitrite species RNS with a consequent higher expression of growth factors and promotion of neovascularization and enhanced immunomodulatory properties
Medicina 2021 57 864 5 of 25 4 Approved Indications for HBOT Due to the multiple characteristics of HBOT the possible applications of this procedure are numerous For instance HBOT may be used as an urgent treatment for acute pathologies but also as an additional support for chronic diseases 41 Currently there are 14 approved indications for HBOT are represented in Table 1 Most of these uses can be grouped according to three main effects a in the wound healing acceleration and angiogenesis enhancement b exerting antimicrobial effects and c as a medical emergency Table 1 Approved indications for HBOT Air or gas embolism Acute thermal burn injury Carbon monoxide poisoning Carbon monoxide poisoning complicated by cyanide poisoning Central retinal artery occlusion Clostridial myositis and myonecrosis gas gangrene Compromised grafts and Flaps Crush injury Compartment Syndrome and other acute traumatic ischemia Decompression sickness Delayed radiation injury soft tissue and bony necrosis Enhancement of healing in selected problem wounds Idiopathic sudden sensorineural hearing loss Intracranial abscess Necrotizing soft tissue infections Refractory osteomyelitis Severe anaemia 4 1 HBOT and Wound Healing The Angiogenesis Enhancement In clinical practice it has been observed how HBOT can speed wound healing As wounds need oxygen to regenerate tissues properly an exposure of 100 oxygen accelerates this process The application in this field is quite extensive comprising microbial infected wounds e g Clostridial myonecrosis and Fournier s gangrene traumatic wounds thermal burns skin grafts radiation induced wounds diabetic and vascular insufficiency ulcers 45 In the field of diabetes there is a critical complication called diabetic foot ulcers an open wound at the bottom of the foot that affects 15 of patients HBOT has been specially regarded for this injury being implicated many inflammatory and tissue repairing parameters For instance there was some evidence that HBOT may improve the healing rate of wounds by increasing nitric oxide NO levels and the number of endothelial progenitor cells in the non healing vasculitis calcific uremic arteriolopathy CUA livedoid vasculopathy LV pyoderma gangrenosum PG ulcers 46 Some trials show a prominent angiogenesis while reducing inflammation angiogenic markers like epithelial growth factor EGF and VEGF become enhanced and positively associates to Nrf2 transcription factor increase 47 Furthermore anaerobic infections have a lower occurrence and amputation rates immensely decrease 48 49 Different systematic reviews support the adjuvant use of systemic but not topical HBOT in the wound healing of diabetic foot ulcers 50 51 However studies results are quite heterogeneous and it is still necessary to define which group of patients may benefit most from this intervention 52 For instance patients with diabetic foot ulcers and peripheral arterial occlusive disease may not improve wound healing 53 Another recent study demonstrated that the use of HBOT may be associated with improved six year survival in patients with diabetic foots 54 Further studies and greater samples are required to identify the most suitable candidates for HBOT Additionally HBOT may be an excellent adjuvant in surgery injuries resolutions and it is key as it may provide better outcomes if it is earlier administered When wounds do not follow conventional treatments for healing an extra aid can be found in HBOT
Medicina 2021 57 864 6 of 25 Animal models have described the importance of this procedure in the wound healing by the acceleration of epithelialization and neovascularization 55 56 Reported effects on these events resides in the up regulation of host factors like tumour necrosis factor TNF matrix metallopeptidase 9 MMP 9 and tissue inhibitor of metalloproteinase 1 TIMP 1 57 In a rabbit model of irradiated tissue NBOT O2 was compared to hyperbaric demonstrating once again that O2 is required at higher pressures to provoke an angiogenic effect 56 More studies in vivo have alleged tension exerted by hyperbaric O2 modulates proliferation rate of stem cells in small intestinal crypts and raises angiogenesis in chorioallantonic membrane in Gallus gallus embryos 58 In a clinical trial of patients with chronic non healing wounds more than 20 months without healing HBOT was standardized for 20 sessions five sessions week The results were increased levels of vascular endothelial growth factor VEGF and interleukine 6 IL 6 and lower levels of endothelin 1 These facts entail an activation of host wound resolution factors angiogenesis and vascular tone 59 Vasculogenesis gains efficiency thanks to HBOT upregulation of nitric oxide NO and associates to a decrease in lesions area 60 Multiple lines of research have also been opened to evaluate the enhanced angiogenesis and healing of tissues following HBOT For instance a phase 2A clinical trial demonstrated the possible benefits from HBOT in combination with steroids for patients with ulcerative colitis in terms of achieving higher rates of clinical remission and a reduced probability of progression to second line therapy during the hospitalization 61 However there are few studies in this field and soon an updated meta analysis and systematic review of the available evidence will be published 62 Similar conclusions might be extrapolated to radiation induced hemorrhagic cystitis and proctitis 63 Osteoradionecrosis is also a frequent and worrisome condition in oncological patients after receiving radiotherapy Frequently this condition affects to the jaw and consists of the development aseptic avascular necrosis which can lead to infection tooth loss and even pathological fracture of the jaw Moreover it often results in an ulceration and necrosis of the mucosa with exposed bone HBOT plays a critical role in the treatment of this condition improving the tissue response to surgical wounding and even as prophylactic approach in patients with previous head and neck irradiation undergoing dental extractions or complete exodontia 64 The enhancing angiogenesis and wound healing make HBOT an adequate adjuvant treatment in a wide variety of conditions although future studies should be directed to evaluate the most effective dose and to identify the most suitable candidates for submitting this procedure 4 2 HBOT and Infections The Antimicrobial Activity The use of HBOT as an antimicrobial adjuvant is particularly useful in healing context now that microbial infections are the most important cause of non healing wounds meta analysis affirm that prevalence of bacterial biofilms in chronic wounds is 78 2 65 HBOT is considered a non conventional strategy for non healing wounds consisting in a modification of biophysical parameters in the wound microenvironment breaking the bacterial biofilms 66 HBOT upregulates HIF that induces the expression of Nitric Oxide Synthases NOS and virus killing peptides defensins and cathelicidins such as cathelinrelated antimicrobial peptide with consequent neutrophil and monocyte phagocytosis of the microbes 67 69 Increased cathelicidins in mice lungs provide a better response to the flu virus 70 Cathelicidin deficient mice show higher susceptibility to viral damage 71 The most important applications of the antimicrobial activity of HBOT are under necrotizing soft tissue infections NSTIs including necrotizing fasciitis Fournier s gangrene and gas gangrene There is a calamitous soft tissue infection implying a wide variety of gram positive gram negative aerobic and anaerobic bacteria It happens under conditions of trauma or minor lesions that become more complicated normally due to systemic problems like diabetes or vascular disfunctions 45 72 An early and combined HBOT therapy plus current practices may be crucial as a lifesaving and cost efficacy therapy particularly in the most critical patients 73 Clinical practice agrees on the necessity of HBOT in the event of an anaerobic infection as anaerobic bacteria are killed by a much
Medicina 2021 57 864 7 of 25 higher amount of pressurized O2 74 75 For instance the use of HBOT in the anaerobic Clostridium perfringens bacteria is specially recommended 76 This bacterium produces more than 20 recognized toxins However two toxins alpha and theta are the main mediators of the infection caused by this agent Clostridium perfringens growth is restricted at O2 tensions up to 70 mm Hg and alpha toxin production is halted at tensions of 250 mm Hg also achieving bacteriostasis and other antimicrobial effects Thus recommended treatment is O2 at 3 ATA for 90 min three times in the first 24 h and twice a day for the next 2 to 5 days always in combination with proper antibiotic use 77 The anti inflammatory potential of HBOT also aids to lessen tissue damage and infection expansion 72 also explained by a decrease in neutrophil activation eviting rolling and accumulation of white blood cells WBCs hence limiting the production of ROS by neutrophils and avoiding reperfusion injury 45 Moreover this is observed in In vitro studies having been demonstrated the biofilm shrinkage ability with the significant decreases in cellular load of anaerobic bacteria and fungi after HBOT 75 A sepsis mouse model showed a significant increase in survival rate 50 with early HBOT compared to a control group that did not receive the treatment and was associated with lower expression of TNF IL 6 and IL 10 78 Translation to clinical experience reports that the improvements in oxygenation follow the neovascularization which avoid undesired events like amputation 28 This is the case for example of Fournier s gangrene where bacteremia and sepsis are top factors of fatality which can be avoided by adjuvant HBOT providing much higher survival rates in clinical trials 79 Sometimes unwanted events are underestimated until it is late and polymicrobial infection has bursted into surgical bone and joint lesions 80 For that reason molecular assessments of bacterial identification like mass spectrometry are every time more accomplished to consider if HBOT is worthy for patients better recovering On the other hand the use of HBOT might provide a central therapeutical option in the intracranial abscess ICA ICA presentation includes cerebral abscess subdural empyema and epidural empyema and it is caused by an encapsulated infection in which the proper inflammatory response may damage the surrounding brain parenchyma 81 The etiological agent might be bacteria fungi or a parasite and it might appear as a consequence of a dissemination of previous infections like sinusitis otitis mastoiditis dental infection hematogenous seeding or cranial trauma 82 Due to the high morbidity and mortality along with the urgency of a non invasive and effective method HBOT has been proposed as a well accepted adjunctive therapy for ICA being regarded as a safe and tolerated method 83 The main mechanisms by which HBOT represent an additional tool in the management of ICA resides on the impairment of the acidotic and hypoxic environment in ICAs due to the proper infection and the use of antibiotics 84 Similarly osteomyelitis is a chronic infection in the bone marrow frequently caused by bacteria or mycobacteria It is a difficult condition to treat as many antimicrobials do not penetrate in the bone properly When this condition does not respond to the treatment or reemerge after receiving the therapy it is designed refractory osteomyelitis 85 HBOT is a potential indication of refractory osteomyelitis as it provides synergist antibiotic activity while enhancing angiogenesis leukocyte oxidative killing and osteogenesis process 86 A recent systematic review 87 reported that adjuvant HBOT provided almost a 75 of therapeutic success in patients with chronic refractory osteomyelitis hence showing the importance of this treatment in bacterial infections Malignant otitis externa another infection a necrotizing infection of the soft tissue of the external auditory canal which may rapidly cause skull base osteomyelitis may also benefit from the use of HBOT although further studies are needed to conclude its effects 88 Finally some authors have also proposed a potential clinical use of HBOT as a medical emergency treatment of mucormycosis a fungal infection 89 Despite there still being few studies supporting its use a compelling evidence show its potential use in a similar manner than necrotizing fasciitis although further research is needed in this area
Medicina 2021 57 864 8 of 25 4 3 HBOT in Medical Emergencies Apart from the previously discussed applications there has been further conditions in which HBOT may be considered Some of them are designed as medical emergencies in which the use of HBOT is an urgent indication for these patients These are the cases of some infections above mentioned decompression sickness air or gas embolism acute arterial insufficiencies such as central retinal arterial occlusion CRAO crush injury compartment syndrome and acute traumatic ischemia along with CO Cyanide poisoning 89 In this context the central role of HBOT is derived from the rapid and effective response of the tissues under certain conditions that may be severe and even life threatening 90 A Decompression sickness is a condition occurring due to the formation of bubbles caused by a reduction in ambient pressure that introduced dissolved gases within the body accidents In turn these bubbles drive to mechanical disruption of tissues blood flow occlusion endothelial dysfunction platelet activation and capillary leakage 91 However the term decompression sickness has been abandoned by the ECHM to be replaced by Decompression illness DCI 92 so in this article we will refer this malady as DCI Clinical manifestations are at least one of more of the following generalized fatigue or rash joint pain hypesthesia and in serious cases motor weakness ataxia pulmonary edema shock and death 71 DCI can occur in aviators divers astronauts compressed air workers and in some cases it may appear due to iatrogenic causes 93 HBOT recompression therapy tables US Navy Treatment Table 6 or helium oxygen Heliox Comex Cx30 or equivalent are recommended for the initial treatment of DCI Type 1 recommendation Level C evidence US Navy Treatment Table 5 can be used as the first recompression schedule for selected mild cases 94 Therapies at higher pressure could be administered in exceptional cases but it entails higher difficulties and risks To maximize its efficacy different adjunctive therapies are used in combination with HBOT including fluid administration non steroidal anti inflammatory drugs and prophylactic agents to prevent venous thromboembolism events particularly in paralyzed patients 93 95 Overall because of the high pressure HBOT provide the opposite effects of the pathological mechanisms of DCIs therefore exerting its therapeutical efficacy B Air embolism Apart from DCI bubble formation of large arterial air embolism during operations are unusual occurrences but also ruinous and life threatening For bubble gas formation in veins from lung biopsy arterial catheterization cardiopulmonary bypass HBOT is strictly necessary as there are no better alternatives in time It provides tissue oxygenation by promoting gas reabsorption and hence reduces ischemic injuries 96 In this context retrograde cerebral air embolism is a worrisome condition that may appear in major procedures neurosurgery and cardiovascular operations endoscopy or during minor interventions peripheral or central venous access being particularly lethal when presented with encephalopathy 97 The therapeutic basis of air embolism is similar to DCS with HBOT as first line therapy 98 Some reports have emphasized the importance of an early HBOT in the first 6 h since diagnosis for this complication to obtain better outcomes less sequelae or death rate 99 However there is some evidence of late benefits from its use up to 60 h after the onset 100 Even when there is no gas seen in on image test patients may benefit from the use of HBOT 101 On the other hand recent data indicates that less cases appears to be treated by HBOT probably by the lack of belief of some physicians in HBOT particularly in UK 102 However available evidence supports the use of this therapy to prevent and improve the outcome of such a dangerous condition C CRAO is an ophthalmological complication caused by a permanent occlusion of the central retinal artery mostly due to a embolus at its narrowest part that is typically associated with a sudden massive loss of vision in the affected eye 103 Prognosis for visual recovery is poor as the retinal tissue is not tolerant to hypoxia and it presents the highest oxygen consumption rate in the body at 13 mL 100 g per min 104 As a result HBOT is a robust indication for patients with CRAO and many studies have reported encouraging results from its use minimum at eight sessions with some advantages presented in comparison to other lines of treatment such as being a non invasive method with low
Medicina 2021 57 864 9 of 25 adverse effects 104 107 However and despite these benefits HBOT is rarely offered for patients with CRAO 108 probably due to the lack of facilities in the hospital services D Another approved indication for HBOT is crush injury and acute ischemia occurred as result of a trauma Presentations of these damage vary from mild contusions to limb threatening damage involving multiple tissues from skin to muscles and bones A severe consequence of trauma is the skeletal muscle compartment syndrome SMCS a condition affecting both muscle and nerves 1 Subsequently to trauma the affected tissue will suffer from hypoxia edema and ischemia Here the efficacy of angiogenesis has been also proved to be boosted by HBOT in animal models for ischemic limbs when combined with bone marrow derived mononuclear cells transplantation 109 Some translational studies of multicenter randomized trials did not show a significant complete progress of healing 110 but in contrast other trials showed the advantage of HBOT as adjunct for ischemic limbs when reconstructive surgery was not possible 111 Evaluating skin peripheral circulation as well the outcomes showed significant improvements in revascularization 112 therefore demonstrating the important role of HBOT in this condition E CO poisoning is a problem that happens when household devices which use gas or coal produce CO due to an uncomplete combustion Inhalation of this gas can be lethal and cause long term problems particularly cognitive and brain deficits presented up to a 40 of the patients and approximately one in three people develop cardiac dysfunction like arrhythmia left ventricular systolic dysfunction and myocardial infarction 113 To address these problems HBOT has been applied 114 being associated to neurological sequelae reduction 115 and when applied in the first 24 h can reduce the risk of cognitive sequelae months later more efficiently 116 In general NBOT is immediately used after CO poisoning until HBOT is available 117 Evidence indicates that HBOT should be considered for all cases of serious acute CO poisoning loss of consciousness ischemic cardiac changes neurological deficits significant metabolic acidosis or COHb greater than 25 113 Another kind of poisoning in which HBOT has its application is cyanide toxicity This issue appears with uncomplete combustion this time of materials like plastics vinyl acrylics nylon etc HBOT is the primary treatment but it exceeds when is combined with the antidote hydroxycobalamin ameliorating mitochondrial oxidative phosphorylation function 118 119 Potential uses of HBOT in a wide range of urgent conditions at least might be considered as an important tool in medical emergencies F Severe anemias and idiopathic sudden sensorineural hearing loss Despite not being considered a medical emergency the use of HBOT is also indicated for these conditions 89 In the first case as Hb levels critically drops O2 delivery to the tissues may be impaired In this line the use of 100 hyperbaric O2 might solve this issue simultaneously exerting a wide range of favorable effects in the hematological profile 120 This could be especially important in patients who cannot be transfused for religion immunologic reasons or blood availability problems Idiopathic sudden sensorineural hearing loss or acute acoustic trauma AAT are also important conditions in which HBOT could be a valuable tool In fact a recent systematic review and meta analysis conducted by Rhee et al 121 showed that the addition of HBOT to standard medical therapy is a valuable treatment option particularly for patients with severe to profound hearing loss and in those patients which received at least 1200 min of HBOT Apart from the regulation of ROS and inflammatory response previous research has demonstrated the protective role of HBOT in the hair cell stereocilia probably through hormetic mechanisms 122 G Finally HBOT can significantly improve symptoms and quality of life of patients affected by femoral head necrosis ECHM recommendation type II level of evidence B 123 as well as the previously mentioned NSTI gas gangrene and urgent HBO alpha toxin neutralized
Medicina 2021 57 864 10 of 25 5 Translational and Potential Applications of HBOT Besides approved indications further lines of research have demonstrated the potential applications and translation of HBOT in the field of inflammatory and systemic conditions cancer COVID 19 and other conditions are summarized 5 1 HBOT and Inflammation Immunomodulatory Properties HBOT might also be applicated in the regulation of inflammatory responses and its derived complications Among the most important immunomodulatory effects HBOT drives an alteration in CD4 CD8 ratio a reduced proliferation of lymphocytes and an activation of neutrophils with migration to hyperoxic regions 124 Thus HBOT might be used in a wide variety of conditions presenting an altered immune system as part of its pathogenesis In this sense it has been proposed the role of HBOT in the management of autoimmune diseases ADs A study conducted by Xu et al 125 observed the overall effect of HBOT in general immune populations and particular Th1 and B lymphocytes subsets proving its promising role in certain ADs Furthermore long term exposure to HBOT was proven to supress the development of autoimmune symptoms including proteinuria facial erythema and lymphadenopathy 126 In the same manner the use of HBOT in early and middle stage of disease mice also show a significant increase in survival with a decrease in inflammatory cells anti dsDNA antibody titers and amelioration of immune complex deposition in comparison to later stage of disease 127 The use of HBOT has also proven its efficacy on rheumatoid arthritis particularly due to the polarization of Th17 cells to T reg with a significative reduction of cell hypoxia 128 Similarly these results could be extrapolated to other inflammatory conditions For instance HBOT provides an anti inflammatory response in DSS induced colitis Through direct effects on HIF HBOT induces antioxidant expression and the downregulation of proinflammatory cytokines like IL 6 therefore reducing colonic inflammation 129 In vitro studies with lymphocytes from type 1 diabetes mellitus have proved effects of HBOT on inducible NOS expression observing lower activity with a consequent decreased levels of NFkB 130 Additionally HBOT comprises another potential approach regarding musculoskeletal dysfunctions Fibromyalgia represents an incapacitant disorder characterized by a widespread muscle and joint pain frequently accompanied by systemic symptoms including cognitive dysfunction mood disorders fatigue and insomnia 131 HBOT exerts direct effects on brain activity chronic pain and immune dysregulation therefore improving quality of life of affected patients 132 Interestingly Woo et al 133 also observed that HBOT could be considered an interesting alternative to attenuate exercise induced inflammation and muscle damage Overall previous research has indicated the favourable effects of HBOT in the immune system and also on the whole body 5 2 Role of HBOT in the COVID 19 Pandemic COVID 19 pandemic has challenged healthcare systems worldwide overloading them with a huge burden in economy and our normalcy 134 135 The urge of conducting massive vaccination programs besides finding better therapies for clinical management have been the focus these months In this context HBOT has been proposed as an adjuvant for clinical practice in severe patients and also for recovery after SARS CoV 2 infection Results from clinical trials have already demonstrated the potential uses of this treatment to redirect O2 diffusion avoided by hypoxemia and its ability to eliminate inflammatory cytokines Nevertheless not only hyperbaric O2 may be worthy for severe patients but also for treating the named silent hypoxemia in those patients that do not have a bad clinical course yet 136 This silent hypoxemia is not characterized by typical respiratory distress in critically ill patients but it may be dangerous if it is not sooner detected as a prompt deterioration can occur without noticing 137 In fact previous studies have demonstrated the association between hypoxemia with fatal outcomes in patients with COVID 19 138
Medicina 2021 57 864 11 of 25 In the same manner physicians observed that patients exhibit hypoxemia without dyspnea being crucial to find care solutions to anticipate a problem with more patients at important risk 139 Some cases of people with mild or even without symptoms that contracted multi organ failure and then died have emphasized the importance of self monitoring of pulse oximetry which typically presents reduced readings in these patients 140 Collected data from patients that did not present problems of breathing at admission agreed with the suggestion of utilizing pulse oximetry to predict the outcome of hypoxemia hypocapnia syndrome that defines asymptomatic hypoxia 141 Steps forward in the understanding of our complex respiratory system have also launched reviews about the higher oxygenation rate in prone position concerning variables like gravity lung structure and the higher expression of nitric oxide NO in dorsal lung vessels than in ventral ones 142 It has been demonstrated that HBOT increases the production of NO and ROS RNS inhibiting SARS CoV 2 replication in previous In vitro models 41 Moreover all these facts have shed a light on finding better treatments to prevent fast hypoxia fatality or even the need for mechanical ventilation 143 144 being HBOT a suggested adjuvant for its promising outcomes from previous animal models and clinical cases of sepsis and inflammatory diseases 145 Preliminary comparisons of HBOT applications in COVID 19 to other maladies like livedoid vasculopathy have exposed the possible mechanisms that may occur anti inflammatory actions decreased ICAM 1 proinflammatory cytokines and neutrophil rolling anticoagulant actions boosted fibrinolysis and increased plasminogen activator and tissue healing actions increased fibroblasts and stem cells 146 First studies in a severe patient affirmed that compared to normobaric oxygen supply the better empiric outcome agreed with the theoretic expectance of the potential uses of HBOT in COVID 19 147 Although it is still being evaluated scientifically positive results are arising for COVID 19 treatment finding an attenuation of the innate immune system and increasing hypoxia tolerance 148 In every report this therapy has been rated as a potential support in the relieving of cytokine storm 149 Now that mechanical ventilation may be long lasting and preferably avoided in a controlled trial safety and efficacy of HBOT for COVID 19 patients was successfully evaluated 150 Another preliminary study showed rapid alleviation of hypoxemia from the beginning of the treatment in patients with COVID 19 pneumonia 151 Anatomically pathologic examinations of lung with early phase COVID 19 have shown edema proteinaceous exudate inflammatory cellular infiltration and interstitial thickening that entails a disproportional gas exchange This is due to CO2 diffuses through tissues much faster than O2 about 20 times what leads to hypocapnia 152 Alveolar structure is altered in the COVID 19 patient there is also hyaline membrane formation there is thickness in alveolar membrane and the space for the diffusion of oxygen generates a lot of exudate and inflammation Hence diffusion from the alveolus through the haematoalveolar membrane does not occur correctly the concentration of oxygen in the blood and in the tissues begins to fall and the exchange of the dioxide also becomes difficult Due to possible viral interactions with Hb 153 and a hypoxemia induced shift in the oxyhemoglobin dissociation curve to the left there is O2 saturation but low arterial blood pressure 154 Clinical evidence from few studies about COVID 19 patients undergoing HBOT notes that this therapy may make possible to contribute to reverse hypoxemia and ameliorating the pulmonary capillary circulation diffusion despite the thickness in alveolar membrane in disease According to Henry s Law HBOT allows to increase pressure of O2 in the alveoli above ambient pressure In this way there will be a large increase of O2 diffusion into the pulmonary capillary circulation more than 10 times for its arrival in the plasma and reach the tissues independently of Hb There will be a gain of O2 supply to the tissues mediated by the increase in pressure Experimentally hematological biochemical and inflammatory parameters were significantly improved after HBOT In first trials the observation of lymphocyte count was increased whereas lactate and fibrinogen were decreased 147 151
Medicina 2021 57 864 12 of 25 However during this procedure patients may suffer from desaturation reflexes Despite the etiology of this reflex is unclear it might be probably caused by a vasoconstriction affecting the pulmonary arteries due to the oxidative stress as well as direct damage in type II pneumocytes and thrombus associated with COVID 19 124 Notwithstanding the ongoing clinical trials and the efforts of standardize better protocols for safety COVID 19 is not yet an accepted indication for HBOT but this may be recommended for post viral sequelae 155 In order to guarantee its beneficial effects there is still a need of more controlled trials to measure different inflammatory and hematological parameters that demonstrate that exudate and inflammation are reduced besides the improvements in alveolar circulation diffusion This would confirm the potential of this adjuvant also for considering the financial investment in hyperbaric chambers in hospitals 5 3 HBOT and Cancer Cancer is a complex entity which encompasses a broad spectrum of unique pathologies that share the following hallmarks Immune system evasion tumor promoting inflammation genome instability enabling replicative immortality activating invasion and metastasis sustaining proliferative signaling evading growth suppressors resisting cell death inducing angiogenesis and metabolic reprogramming 156 Tumor hypoxia plays a central role in many of these carcinogenic features promoting an aggressive phenotype besides limit the effectiveness of radiotherapy chemotherapy and immunotherapy thereby worsening prognosis in the oncological patients 157 Thus targeting tumoral hypoxia and its downstream effectors have been proposed as a potential therapeutical approach in cancer management 158 160 In this line accumulating evidence supports the role of HBOT in the inhibition of tumor growth and therapy success by three main mechanisms 1 By limiting cancer associated hypoxia 2 through the generation of ROS and RNS and 3 restoring immune function 161 Actual investigations show the promising role of HBOT in a wide variety of malignancies including breast cancer prostate cancer head and neck cancer colorectal cancer leukemia brain tumors cervical cancer and bladder cancer 162 Main applications derived from HBOT in oncology may be a As part of the treatment b as a radiotherapy adjuvant and c as a chemotherapy adjuvant 163 The use of HBOT as part of the cancer therapy is not currently an approved indication although some promising results have arisen recently In this context Thews Vaupel 164 compared the efficacy of NBOT 1 atm versus HBOT 2 atm oxygenation reporting broader reductions of hypoxia under hyperbaric conditions However even at high pressure oxygenation tumor hypoxia was not completely removed hence showing that HBOT alone efficacy is limited Importantly as previously described HBOT was associated with increased angiogenesis these effects are not significative in tumour cells so its use could be important in the cancer management 165 Conversely a study conducted by Pande et al 166 revealed that notwithstanding HBOT treated mice initially induced a decrease in tumor progression a tumorigenic effect was observed post therapy probably due to impaired DNA repair mutagenicity and chromosomic aneuploidies together with an altered blood supply and nutrients On the other hand some authors suggest that the lack of therapeutical efficacy of HBOT might be due to the difficulty on creating a hyperoxic environment in the tumor and that by combining HBOT with other methods it could act a as a potential cure in certain types of cancer In this line Lu et al 167 proposed a combined use in prostate cancer patients of HBOT with ultrasound guided transrectal prostate puncture in order to create a hyperoxic environment within the tumor which may lead to DNA damage and a detention in the G2 M cycle hence establishing the basis for future research Similarly tumor hypoxia is associated with the metabolic reprogramming of tumour cells also known as the aerobic glycolysis or Warburg effect This consists of a glycolytic switch of cancer cells which refrain from performing oxidative phosphorylation 168 In this sense Poff et al 169 described the combined effects of HBOT in combination with ketogenic diet in a murine model preventing tumoral metastasis while expanding overall survival Furthermore HBOT alone or combined with
Medicina 2021 57 864 13 of 25 low glucose and ketone supplementation also exert multiple benefits against late stage metastatic cancers by increasing the production of ROS and oxidative stress 170 Despite the encouraging results further research is required to establish the efficacy of HBOT in the different types of cancer also searching for the most adequate use of this therapy in a global context Radiotherapy RT is a central component in cancer management with approximately 50 of patients receiving this therapy contributing up to a 40 of curative success for cancer 171 Through ionizing radiation it creates a ROS and RNS overproduction leading to double strand breaks chromosomal aberrations and rearrangements with subsequent cell death or dysfunction thus exerting its anti tumoral effects The effect of HBOT on human glioblastoma GBM was investigated in laboratory on patient derived cells and on microglia cell biology CHME 5 The results obtained from the combination of HBO and RT clearly showed a radiosensitising effect of HBO on GBM cells grown 172 Hypofractionated stereotactic radiotherapy HSRT after HBO HBO RT appears to be effective for the treatment of recurrent high grade glioma rHGG as pointed out on a cohort of 9 adult rHGG patients It could represent an alternative with low toxicity to systemic therapies for patients who cannot or refuse to undergo such treatments 173 However although non tumour cells are less sensitive radiation could also affect them altering multiple cellular signaling pathways or inducing apoptosis hence explaining its multiple adverse effects 174 One of the most severe consequences resulted from irradiation is the appearance of post radiation injuries a process starting during radiotherapy that involves the dysregulation of multiple bioactive compounds particularly fibrogenic cytokines like TGF 175 Similarly almost all tissues with delayed irradiation injury present a histological feature named as obliterative endarteritis finally leading to a tissue damage characterized by hypoxia hypovascularity and hypocellularity 176 In this line HBOT has consistently demonstrated its therapeutical effectivity against radiation induced injury also approved by the UHMS 177 and the ECHM 8 Last 2016 Cochrane review 178 evidenced that the use of HBOT in head neck anus and rectum injured tissues were associated with improved outcomes and at some extent with osteoradionecrosis following tooth extraction in an irradiated field According to ECHM recommendation the use of HBOT is recommended in the treatment of radiation proctitis Type 1 recommendation Level A evidence mandibular osteoradionecrosis and haemorrhagic radiation cystitis Type 1 recommendation Level B evidence and suggested in the treatment of osteoradionecrosis of other bone than the mandible for preventing loss of osseointegrated implants in irradiated bone and in the treatment of soft tissue radionecrosis other than cystitis and proctitis in particular in the head and neck area Type 2 recommendation Level C evidence Furthermore it would be reasonable to use HBOT for treating or preventing radio induced lesions of the larynx in the treatment of radio induced lesions of the central nervous system Type 3 recommendation Level C evidence 8 Finally the combined use of HBOT plus chemotherapy have reported certain benefits In this line a recent study conducted by Brewer et al 179 demonstrated the effectiveness of using HBOT to prevent chemotherapy induced neuropathy In vivo This fact appears to be due to the various implications of HBOT in the neuronal activity and signaling 180 182 Kawasoe et al also observed 183 that an integrative strategy of carboplatin plus HBOT significantly reduced mortality in C3H mice with inoculated osteosarcoma cells Similar results were obtained with HBOT and chemotherapy in lung cancer cultures and animal models 184 In particular the combination of paclitaxel and carboplatin plus HBOT and hyperthermia show promising results for treating patients with non small cell lung cancer and multiple metastasis 185 Despite these results the use of HBOT and chemotherapy may also represent a contraindication for the patients For instance the combination of HBOT with doxorubicin bleomycin or cisplatin may exert synergic cardiotoxicity pulmonary toxicity or impaired wound healing respectively 186 This is an important issue to address in the oncologic patient In these cases it is important to separate chemotherapy from the use of necessary HBOT to avoid undesired effects In addition further strategies
Medicina 2021 57 864 14 of 25 could be considered targeting tumour hypoxia and functioning as therapeutic adjuvants like physical activity 187 Overall the benefits of HBOT in cancer management is a potential field to keep on exploring 5 4 Other Applications In the same manner other novel lines of research are exploring potential uses of HBOT in a plethora of conditions For instance some studies related to microvascular or macrovascular insufficiencies causing erectile dysfunction ED have hypothesized the effects of HBOT in patients with this problem Empirical data suggests that it can induce penile angiogenesis and improve erectile function in men suffering from ED This is due to vasodilatation relies on proper blood vessels in corpora cavernosa Then being a major concentration of oxygen in tissues there is an increased angiogenesis by VEGF and endothelial cells differentiation 188 This application has not provided significant data on rehabilitation after prostatectomy 189 but it has obtained good symptoms resolution for other clinical manifestations like ED in diabetes mellitus 190 or in recovery after urethral reconstruction 191 Equally the use of HBOT for ischemic stroke and brain injury is an interesting point of study For instance different studies have demonstrated the importance of this procedure as a prophylactic approach for sequestration of inflammation inherent in stroke and traumatic brain injury preventing neuronal death 192 Other uses such as brain preconditioning before stem cells transplantation have also been explored 193 However the efficacy and safety of HBOT in these conditions remains to be fully elucidated although some basic and clinical research have shown encouraging results 194 Finally the use of HBOT could be potentially extended to novel fields like aging Hachmo et al 195 reported the effect of hyperbaric oxygen in the prevention of telomere shortening and immunosenescence by the clearance of senescent immune cells In this line other studies have reported the same results in the aging skin through the acceleration of epidermal basal cells proliferation 196 in the endothelial cells where it induces antioxidants expression 197 and also in the brain where HBOT appears to improve the cerebral blood flow 198 restoring cognitive parameters hippocampal functions and even improved insulin resistance in both normal weigh and obese aging rats 199 As summarized in Figure 2 the main consequences of HBOT and its related hyperoxemia and hyperoxia in the human body could be related with the angiogenesis enhancement antimicrobial properties and immunomodulatory effects Approved indications for this therapy could also be grouped according to its emergency
Medicina 2021 57 864 15 of 25 Figure 2 Summary of top properties of HBOT and its clinical applications Firstly it can provide an angiogenesis enhancement observed by the prime production of NO which subsequently brings an upregulation of Nrf2 and growth factors like epidermal growth factor EGF vascular endothelial growth factor VEGF and endothelin 1 TNF matrix metallopeptidase 9 MMP 9 and tissue inhibitor of metalloproteinase 1 TIMP 1 will be boosted too Secondly the antimicrobial activity is visible due to bacterial killing by O2 removing biofilm and lessening white blood cells WBCs rolling and neutrophils recruitment hence promoting a downregulation of proinflammatory cytokines TNF IL 6 and IL 10 The immunomodulation properties are observed by a downregulation of transcriptional factor NFkB involving a proinflammatory response switch off IL 6 and a polarization from Th17 lymphocytes to Treg Summarized applications include indications for which HBOT is approved mostly wound healing and infections primary emergencies like CO CN poisoning or air embolism and translational research comprising COVID 19 cancer inflammatory conditions or aging among others 6 Adverse Effects and Contraindications Notwithstanding the multiple benefits and applications of HBOT there are important adverse effects that may appear during this procedure As a result of the hyperoxia and the hyperbaric environment there are some issues when using this therapy The two most common complications during HBOT are claustrophobia and barotrauma Both occur during monoplace or multiplace chamber compression 200 In the case of barotrauma it could be defined as an injury caused by an inability to equalize pressure from an air containing space and the surrounding environment Ear barotrauma is the most frequent condition affecting the middle ear although sinus paranasal dental or pulmonary barotrauma could also be reported 201 Despite the incidence of this complication being extremely rare 202 its seriousness should be taken into account considering clinical history of patients at risk of suffering from these complications while implementing different strategies to prevent this complication such as anti epileptic therapy prolonged air brakes or controlling treatment pressure 203 The last event is associated with the appearance of the Paul Bert effect because of the formation of seizures that may bring transient but negative consequences for cognitive functioning and behavioural patterns 204 These effects are primarily due to the toxic properties of oxygen at high concentrations However to date no threshold has been described to precisely assess the pathological levels of oxygen which could be an important issue for critical patients 205 Pulmonary toxicity is not associated with the use of repeated hyperbaric oxygen following current protocols 206 Ocular manifestations
Medicina 2021 57 864 16 of 25 from HBOT may also be described particularly hyperbaric myopia transitory in most cases Other ophthalmological complications less frequent observed are cataracts keratoconus or retinopathy of prematurity in the case of pregnant women exposed to HBOT 207 208 All these adverse effects may be ameliorated prominently by an adequate screening through the use of certain devices and the adjustment of the treatment protocols 200 201 On the other hand there are certain conditions in which HBOT might be absolutely contraindicated or relatively contraindicated The first case is exclusively represented by untreated pneumothorax as it could be a life threatening procedure 209 The rest of contraindications are relative its indication will depend on the real necessity of this therapy Aside from the chemotherapheutic agents previously described other treatments like sulfamylon Mafenide could also share the same action than cisplatin impeding wound healing effects derived from HBOT and it should also be interrupted before this therapy 45 If patient has a pacemaker or any type of implantable devices it is necessary to verify its safety with increased pressure or with pure concentrations of oxygen Hereditary spherocytosis may also be a contraindication as hyperbaric oxygen could cause severe haemolysis 43 Pregnancy is another potential contraindication for this therapy in exception of CO poisoning 210 Although rare in non diabetic individuals patients may also suffer from hypoglycaemia during this procedure and it is important to evaluate their blood glucose levels before HBOT as it could aggravate their hypoglycaemic profile 211 Similarly patients with underlying respiratory pathologies like chronic obstructive pulmonary disease COPD asthma and even upper respiratory infections might be also possible contraindications from receiving HBOT as it could increase the risk of hypercapnia pulmonary barotrauma and sinus or middle ear barotrauma respectively 209 An additional effect derived from HBOT is the increment of blood pressure 212 Hyperbaric oxygen may also induce pulmonary oedema and cardiovascular difficulties in patients with heart failure or in patients with reduced cardiac ejection fractions 213 Finally the history of epilepsy hypoglycaemia hyperthyroidism current fever and certain drugs such as penicillin and disulfiram are also thought to lower the seizure threshold during this therapy 214 Diabetic patients may be warned from regulating its doses of HBOT in order to prevent the hypoglycaemic effect of this therapy To summarize despite the multiple applications of HBOT it is equally important to consider its potential adverse effects and underlying conditions in which this therapy is not going to exert its efficacy also representing a potential risk for these patients 7 Conclusions and Future Directions HBOT is an effective method to increase blood and tissue oxygen levels independently from Hb transportation Its therapeutical basis could be understood from three different perspectives Physical Hyperbaric 100 oxygen physiological Hyperoxia and hyperoxemia and cellular molecular effects All these effects provide HBOT its efficacy in the management of hypoxia derived conditions and hypoxemia respectively also exerting direct effects in infectious agents and immune cells modulating a wide variety of cellular signaling pathways cytokine production and tissue processes such as angiogenesis Herein the use of HBOT might be extended to a broad spectrum of pathologies from infections and inflammatory systemic maladies to wound healing and vascular complications also reporting its efficacy in the management of medical emergencies like air embolism or gas poisoning Although respiratory infections and diseases have been mentioned as contraindications for HBOT the case of SARS CoV 2 is an exception Nowadays the potential use of HBOT in the COVID 19 has been specially regarded exposing results in numerous controlled clinical trials Moreover the use of this procedure in different types of malignancies represents an important support in the delayed radiation injury In the same manner the use of HBOT as a therapeutical agent have shown promising results in trials as an adjunctive substance with other approved treatments like chemotherapy and even recent research have also reported significative improvements in nanomedicine approaches when combined with HBOT 215
Medicina 2021 57 864 17 of 25 Despite its benefits there are still certain challenges which need to be overcome to improve the current and potential applications of HBOT In this line a worrisome issue would be to develop sophisticated strategies to address tissue hypoxia as for certain conditions like tumoral cells the HBOT induced hyperoxia does not completely eliminate tumour hypoxia An adequate combination of HBOT with another procedure might be interesting to targeting this problem 167 On the other hand it is equally important to determine and quantify potential adverse effects derived from HBOT as well as potential contraindications from receiving this therapy Future research should be destinated on developing accurate systems to determine potential benefits and risks for patients before submitting HBOT In this line the development of predictive models as previously mentioned or novel strategies could be interesting approaches in these fields Currently there are only 14 approved indications for this therapeutical approach We encourage further studies to extend the possible uses of this procedure always considering individual benefits and risks from receiving this therapy The inclusion of HBOT in future clinical research could be an additional support in the clinical management of multiple pathologies Author Contributions Conceptualization M A O O F M C G M M M J B M L C Methodology M A O O F M C G M Formal Analysis M A O O F M C G M Investigation M A O O F M C G M E C P M A S M A M N G H J M M M J B M L C Data Curation M A O O F M C G M Writing Original Draft Preparation M A O O F M C G M E C P M A S M A M N G H J M M M J B M L C Writing Review Editing M A O O F M C G M E C P M A S M A M N G H J M M M J B M L C Supervision M M J B M L C Project Administration M M J B Funding Acquisition M M J B All authors have read and agreed to the published version of the manuscript Funding The study was supported by the Comunidad de Madrid B2017 BMD 3804 MITIC CM Univer sidad de Alcal 32 2013 22 2014 26 2015 and Halekulani S L Institutional Review Board Statement Not applicable Informed Consent Statement Not applicable Data Availability Statement The data used to support the findings of the present study are available from the corresponding author upon request Acknowledgments Oscar Fraile Martinez had a predoctoral fellowship from the University of Alcal during the course of this work Conflicts of Interest The authors declare no conflict of interest References 1 2 3 4 5 6 7 8 9 HBO Indications Undersea Hyperbaric Medical Society Available online https www uhms org resources hbo indications html accessed on 3 April 2021 UHMS Position Statement Low Pressure Fabric Hyperbaric Chambers Title Low Pressure Fabric Hyperbaric Chambers 2017 Available online https www uhms org images Position Statements UHMS_Position_Statement_LP_chambers_revised pdf accessed on 23 May 2021 Edwards M L Hyperbaric Oxygen Therapy Part 1 History and Principles J Vet Emergy Crit Care 2010 20 284 288 CrossRef PubMed Dejours P Dejours S The Effects of Barometric Pressure According to Paul Bert The Question Today Int J Sports Med 1992 13 S1 S5 CrossRef PubMed Hedley Whyte J Pulmonary Oxygen Toxicity Investigation and Mentoring Ulst Med J 2008 77 39 42 Jones M W Wyatt H A Hyperbaric Physics StatPearls Publishing Treasure Island FL USA 2019 Moon R E Camporesi E M Hyperbaric Oxygen Therapy From the Nineteenth to the Twenty First Century Respir Care Clin N Am 1999 5 1 5 Mathieu D Marroni A Kot J Tenth European Consensus Conference on Hyperbaric Medicine Recommendations for Accepted and Non Accepted Clinical Indications and Practice of Hyperbaric Oxygen Treatment Diving Hyperb Med 2017 47 24 31 CrossRef Trayhurn P Oxygen The Forgotten Nutrient J Nutr Sci 2017 6 e47 CrossRef
Medicina 2021 57 864 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 18 of 25 Martin W F Garg S Zimorski V Endosymbiotic Theories for Eukaryote Origin Philos Trans R Soc B Biol Sci 2015 370 20140330 CrossRef Trayhurn P Oxygen A Critical but Overlooked Nutrient Front Nutr 2019 6 10 CrossRef Butler J P Tsuda A Transport of Gases between the Environment and Alveoli Theoretical Foundations Compr Physiol 2011 1 1301 1316 CrossRef Harris R S Pressure Volume Curves of the Respiratory System Respir Care 2005 50 78 99 Pittman R N Oxygen Gradients in the Microcirculation Acta Physiol 2011 202 311 322 CrossRef Gossman W Alghoula F Berim I Anoxia Hypoxic Hypoxia StatPearls Publishing Treasure Island FL USA 2019 Choudhry H Harris A L Advances in Hypoxia Inducible Factor Biology Cell Metab 2018 27 281 298 CrossRef Soares M J Iqbal K Kozai K Hypoxia and Placental Development Birth Defects Res 2017 109 1309 1329 CrossRef Navarrete Opazo A Mitchell G S Therapeutic Potential of Intermittent Hypoxia A Matter of Dose Am J Physiol Regul Integr Comp Physiol 2014 307 R1181 R1197 CrossRef Chen P S Chiu W T Hsu P L Lin S C Peng I C Wang C Y Tsai S J Pathophysiological Implications of Hypoxia in Human Diseases J Biomed Sci 2020 27 63 CrossRef Horner D O Driscoll R Oxygen Therapy for Medical Patients BMJ 2018 363 CrossRef Daste T The Oxygen Therapy Prat Vet 2013 20 30 32 CrossRef Lee J W Ko J Ju C Eltzschig H K Hypoxia Signaling in Human Diseases and Therapeutic Targets Exp Mol Med 2019 51 1 13 CrossRef Macintyre N R Tissue Hypoxia Implications for the Respiratory Clinician Respir Care 2014 59 1590 1596 CrossRef Choudhury R Hypoxia and Hyperbaric Oxygen Therapy A Review Int J Gen Med 2018 11 431 442 CrossRef Kirby J P Snyder J Schuerer D J E Peters J S Bochicchio G V Essentials of Hyperbaric Oxygen Therapy 2019 Review Mol Med 2019 116 176 179 Lind F A pro Con Review Comparing the Use of Mono and Multiplace Hyperbaric Chambers for Critical Care Diving Hyperb Med 2015 45 56 60 Weaver L K Monoplace Hyperbaric Chamber Use of U S Navy Table 6 A 20 Year Experience Undersea Hyperb Med 2006 33 85 Lam G Fontaine R Ross F L Chiu E S Hyperbaric Oxygen Therapy Exploring the Clinical Evidence Adv Ski Wound Care 2017 30 181 190 CrossRef Harch P G Andrews S R Fogarty E F Amen D Pezzullo J C Lucarini J Aubrey C Taylor D V Staab P K Van Meter K W A Phase I Study of Low Pressure Hyperbaric Oxygen Therapy for Blast Induced Post Concussion Syndrome and Post Traumatic Stress Disorder J Neurotrauma 2012 29 168 185 CrossRef Izquierdo Alventosa R Ingl s M Cort s Amador S Gimeno Mallench L Sempere Rubio N Chirivella J Serra A P Comparative Study of the Effectiveness of a Low Pressure Hyperbaric Oxygen Treatment and Physical Exercise in Women with Fibromyalgia Randomized Clinical Trial Ther Adv Musculoskelet Dis 2020 12 1759720X20930493 CrossRef Camporesi E M Mascia M F Thom S R Physiological Principles of Hyperbaric Oxygenation In Handbook on Hyperbaric Medicine Springer Milan Italy 1996 pp 35 58 Bennett M H French C Schnabel A Wasiak J Kranke P Weibel S Normobaric and Hyperbaric Oxygen Therapy for the Treatment and Prevention of Migraine and Cluster Headache Cochrane Database Syst Rev 2015 2015 CD005219 CrossRef Lin C H Su W H Chen Y C Feng P H Shen W C Ong J R Wu M Y Wong C S Treatment with Normobaric or Hyperbaric Oxygen and Its Effect on Neuropsychometric Dysfunction after Carbon Monoxide Poisoning Medicine 2018 97 e12456 CrossRef Casillas S Galindo A Camarillo Reyes L A Varon J Surani S R Effectiveness of Hyperbaric Oxygenation Versus Normobaric Oxygenation Therapy in Carbon Monoxide Poisoning A Systematic Review Cureus 2019 11 e5916 CrossRef Leach R M Rees P J Wilmshurst P ABC of Oxygen Hyperbaric Oxygen Therapy Br Med J 1998 317 1140 1143 CrossRef Brugniaux J V Coombs G B Barak O F Dujic Z Sekhon M S Ainslie P N Highs and Lows of Hyperoxia Physiological Performance and Clinical Aspects Am J Physiol Regul Integr Comp Physiol 2018 315 R1 R27 CrossRef PubMed Amir H Shai E The Hyperoxic hypoxic Paradox Biomolecules 2020 10 958 Calabrese E J Hormesis Path and Progression to Significance Int J Mol Sci 2018 19 2871 CrossRef PubMed Thom S R Hyperbaric Oxygen Its Mechanisms and Efficacy Plast Reconstr Surg 2011 127 131S 141S CrossRef Camporesi E M Bosco G Mechanisms of Action of Hyperbaric Oxygen Therapy Undersea Hyperb Med 2014 41 247 252 Longobardi P Hoxha K Perreca F Is Hyperbaric Oxygen an Effective Treatment for the Prevention of Complications in SARS CoV 2 Asymptomatic Patients Infect Microbes Dis 2021 3 109 111 CrossRef Chen W Liang X Nong Z Li Y Pan X Chen C Huang L The Multiple Applications and Possible Mechanisms of the Hyperbaric Oxygenation Therapy Med Chem 2019 15 459 471 CrossRef DuBose K J Cooper J S Hyperbaric Patient Selection StatPearls Publishing Treasure Island FL USA 2018 Fife C E Eckert K A Carter M J An Update on the Appropriate Role for Hyperbaric Oxygen Indications and Evidence Plast Reconstr Surg 2016 138 107S 116S CrossRef Bhutani S Vishwanath G Hyperbaric Oxygen and Wound Healing Indian J Plast Surg 2012 45 316 324 CrossRef
Medicina 2021 57 864 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 19 of 25 Longobardi P Hoxha K Bennett M H Is There a Role for Hyperbaric Oxygen Therapy in the Treatment of Refractory Wounds of Rare Etiology Diving Hyperb Med 2019 49 216 224 CrossRef Dhamodharan U Karan A Sireesh D Vaishnavi A Somasundar A Rajesh K Ramkumar K M Tissue Specific Role of Nrf2 in the Treatment of Diabetic Foot Ulcers during Hyperbaric Oxygen Therapy Free Radic Biol Med 2019 138 53 62 CrossRef L ndahl M Katzman P Nilsson A Hammarlund C Hyperbaric Oxygen Therapy Facilitates Healing of Chronic Foot Ulcers in Patients with Diabetes Diabetes Care 2010 33 998 1003 CrossRef Salama S E Eldeeb A E Elbarbary A H Abdelghany S E Adjuvant Hyperbaric Oxygen Therapy Enhances Healing of Nonischemic Diabetic Foot Ulcers Compared With Standard Wound Care Alone Int J Low Extrem Wounds 2019 18 75 80 CrossRef Sharma R Sharma S K Mudgal S K Jelly P Thakur K Efficacy of Hyperbaric Oxygen Therapy for Diabetic Foot Ulcer a Systematic Review and Meta Analysis of Controlled Clinical Trials Sci Rep 2021 11 2189 CrossRef Game F L Apelqvist J Attinger C Hartemann A Hinchliffe R J L ndahl M Price P E Jeffcoate W J Effectiveness of Interventions to Enhance Healing of Chronic Ulcers of the Foot in Diabetes A Systematic Review Diabetes Metab Res Rev 2016 32 Suppl 1 154 168 CrossRef Lalieu R C Brouwer R J Ubbink D T Hoencamp R Raap R B Van Hulst R A Hyperbaric Oxygen Therapy for Nonischemic Diabetic Ulcers A Systematic Review Wound Repair Regen Off Publ Wound Health Soc Eur Tissue Repair Soc 2020 28 266 275 CrossRef Brouwer R J Lalieu R Hoencamp R van Hulst R A Ubbink D T A Systematic Review and Meta Analysis of Hyperbaric Oxygen Therapy for Diabetic Foot Ulcers with Arterial Insufficiency J Vasc Surg 2020 71 682 692 CrossRef Londahl M Fagher K Nilson A Katzman P Hyperbaric Oxygen Therapy Is Associated with Improved Six Year Survival in People with Chronic Diabetic Foot Ulcers Diabetes 2018 67 2225 CrossRef Edwards M L Hyperbaric Oxygen Therapy Part 2 Application in Disease J Vet Emergy Crit Care 2010 20 289 297 CrossRef Marx R E Ehler W J Tayapongsak P Pierce L W Relationship of Oxygen Dose to Angiogenesis Induction in Irradiated Tissue Am J Surg 1990 160 519 524 CrossRef Sander A L Henrich D Muth C M Marzi I Barker J H Frank J M In Vivo Effect of Hyperbaric Oxygen on Wound Angiogenesis and Epithelialization Wound Repair Regen 2009 17 179 184 CrossRef Pe a Villalobos I Casanova Maldonado I Lois P Prieto C Pizarro C Lattus J Osorio G Palma V Hyperbaric Oxygen Increases Stem Cell Proliferation Angiogenesis and Wound Healing Ability of WJ MSCs in Diabetic Mice Front Physiol 2018 9 995 CrossRef Sureda A Batle J M Martorell M Cap X Tejada S Tur J A Pons A Antioxidant Response of Chronic Wounds to Hyperbaric Oxygen Therapy PLoS ONE 2016 11 e0163371 CrossRef Boykin J V Baylis C Hyperbaric Oxygen Therapy Mediates Increased Nitric Oxide Production Associated with Wound Healing Adv Ski Wound Care 2007 20 382 389 CrossRef Dulai P S Buckey J C Raffals L E Swoger J M Claus P L O Toole K Ptak J A Gleeson M W Widjaja C E Chang J et al Hyperbaric Oxygen Therapy Is Well Tolerated and Effective for Ulcerative Colitis Patients Hospitalized for Moderate Severe Flares A Phase 2A Pilot Multi Center Randomized Double Blind Sham Controlled Trial Am J Gastroenterol 2018 113 1516 1523 CrossRef Wang W He Y Wen D Jiang S Zhao X Efficacy and Safety Evaluation of Hyperbaric Oxygen Therapy for Patients with Ulcerative Colitis A Protocol of Systematic Review and Meta Analysis Medicine 2021 100 e23966 CrossRef Oliai C Fisher B Jani A Wong M Poli J Brady L W Komarnicky L T Hyperbaric Oxygen Therapy for Radiation Induced Cystitis and Proctitis Int J Radiat Oncol Biol Phys 2012 84 733 740 CrossRef Davis D D Hanley M E Cooper J S Osteoradionecrosis Curr Otorhinolaryngol Rep 2021 6 285 291 Malone M Bjarnsholt T McBain A J James G A Stoodley P Leaper D Tachi M Schultz G Swanson T Wolcott R D The Prevalence of Biofilms in Chronic Wounds A Systematic Review and Meta Analysis of Published Data J Wound Care 2017 26 20 25 CrossRef Kadam S Shai S Shahane A Kaushik K S Recent Advances in Non Conventional Antimicrobial Approaches for Chronic Wound Biofilms Have We Found the Chink in the Armor Biomedicines 2019 7 35 CrossRef Ko sciuczuk E M Lisowski P Jarczak J Strza kowska N J zwik A Horbanczuk J Krzyzewski J Zwierzchowski L Bagnicka E Cathelicidins Family of Antimicrobial Peptides A Review Mol Biol Rep 2012 39 10957 10970 CrossRef PubMed Peyssonnaux C Datta V Cramer T Doedens A Theodorakis E A Gallo R L Hurtado Ziola N Nizet V Johnson R S HIF 1 Expression Regulates the Bactericidal Capacity of Phagocytes J Clin Investig 2005 115 1806 1815 CrossRef PubMed Zarember K A Malech H L HIF 1alpha A Master Regulator of Innate Host Defenses J Clin Investig 2005 115 1702 1704 CrossRef PubMed Tecle T Tripathi S Hartshorn K Review Defensins and Cathelicidins in Lung Immunity Innate Immun 2010 16 151 159 CrossRef Gaudreault Gosselin J Leukotriene B4 Induces Release of Antimicrobial Peptides in Lungs of Virally Infected Mice J Immunol 2008 180 6211 6221 CrossRef
Medicina 2021 57 864 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 20 of 25 Memar M Y Yekani M Alizadeh N Baghi H B Hyperbaric Oxygen Therapy Antimicrobial Mechanisms and Clinical Application for Infections Biomed Pharmacother 2019 109 440 447 CrossRef Shaw J J Psoinos C M Emhoff T A Shah S A Santry H Not Just Full of Hot Air Hyperbaric Oxygen Therapy Increases Survival in Cases of Necrotizing Soft Tissue Infections Surg Infect 2014 15 328 335 CrossRef Nedreb T Bruun T Skj stad R Holmaas G Skrede S Hyperbaric Oxygen Treatment in Three Cases of Necrotizing Infection of the Neck Infect Dis Rep 2012 4 73 76 CrossRef Sanford N E Wilkinson J E Nguyen H Diaz G Wolcott R Efficacy of Hyperbaric Oxygen Therapy in Bacterial Biofilm Eradication J Wound Care 2018 27 S20 S28 CrossRef Gibson A Davis F M Hyperbaric Oxygen Therapy in the Management of Clostridium Perfringens Infections N Z Med J 1986 99 617 620 Sison Martinez J Hendriksen S Cooper J S Hyperbaric Treatment Of Clostridial Myositis And Myonecrosis 2021 Available online https europepmc org article nbk nbk500002 accessed on 13 May 2021 Halbach J L Prieto J M Wang A W Hawisher D Cauvi D M Reyes T Okerblom J Ramirez Sanchez I Villarreal F Patel H H et al Early Hyperbaric Oxygen Therapy Improves Survival in a Model of Severe Sepsis Am J Physiol Regul Integr Comp Physiol 2019 317 R160 R168 CrossRef Hung M C Chou C L Cheng L C Ho C H Niu K C Chen H L Tian Y F Liu C L The Role of Hyperbaric Oxygen Therapy in Treating Extensive Fournier s Gangrene Urol Sci 2016 27 148 153 CrossRef Walter G Vernier M Pinelli P O Million M Coulange M Seng P Stein A Bone and Joint Infections Due to Anaerobic Bacteria An Analysis of 61 Cases and Review of the Literature Eur J Clin Microbiol Infect Dis 2014 33 1355 1364 CrossRef Muzumdar D Jhawar S Goel A Brain Abscess An Overview Int J Surg 2011 9 136 144 CrossRef Tomoye E O Moon R E Hyperbaric Oxygen for Intracranial Abscess Undersea Hyperb Med 2021 48 97 102 CrossRef Bartek J Jakola A S Skyrman S F rander P Alpkvist P Schechtmann G Glim ker M Larsson A Lind F Mathiesen T Hyperbaric Oxygen Therapy in Spontaneous Brain Abscess Patients A Population Based Comparative Cohort Study Acta Neurochir 2016 158 1259 1267 CrossRef M Das J Tommeraasen M A Cooper J S Hyperbaric Evaluation and Treatment of Intracranial Abscess StatPearls Publishing Treasure Island FL USA 2020 Hanley M E Hendriksen S Cooper J S Hyperbaric Treatment of Chronic Refractory Osteomyelitis StatPearls Publishing Treasure Island FL USA 2021 Rose D Hyperbaric Oxygen Therapy for Chronic Refractory Osteomyelitis Am Fam Physician 2012 86 888 893 Savvidou O D Kaspiris A Bolia I K Chloros G D Goumenos S D Papagelopoulos P J Tsiodras S Effectiveness of Hyperbaric Oxygen Therapy for the Management of Chronic Osteomyelitis A Systematic Review of the Literature Orthopedics 2018 41 193 199 CrossRef Byun Y J Patel J Nguyen S A Lambert P R Hyperbaric Oxygen Therapy in Malignant Otitis Externa A Systematic Review of the Literature World J Otorhinolaryngol Head Neck Surg 2020 CrossRef Kirby J P Hyperbaric Oxygen Therapy Emergencies Mol Med 2019 116 180 183 Leung J K S Lam R P K Hyperbaric Oxygen Therapy Its Use in Medical Emergencies and Its Development in Hong Kong Hong Kong Med J 2018 24 191 199 CrossRef Cooper J S Hanson K C Decompression Sickness DCS Bends Caisson Disease StatPearls Publishing Treasure Island FL USA 2019 Pollock N W Buteau D Updates in Decompression Illness Emerg Med Clin N Am 2017 35 301 319 CrossRef Vann R D Butler F K Mitchell S J Moon R E Decompression Illness Lancet 2011 377 153 164 CrossRef Moon R E Hyperbaric Oxygen Treatment for Decompression Sickness Undersea Hyperb Med 2014 41 151 157 Moon R E Adjunctive Therapy for Decompression Illness A Review and Update Diving Hyperb Med 2009 39 81 87 Malik N Claus P L Illman J E Kligerman S J Moynagh M R Levin D L Woodrum D A Arani A Arunachalam S P Araoz P A Air Embolism Diagnosis and Management Future Cardiol 2017 13 365 378 CrossRef Yesilaras M At lla O D Aksay E Kilic T Y Atilla O D Retrograde Cerebral Air Embolism Am J Emerg Med 2014 32 1562 e1 1562 e2 CrossRef Moon R E Hyperbaric Treatment of Air or Gas Embolism Current Recommendations Undersea Hyperb Med 2019 46 673 683 CrossRef Blanc P Boussuges A Henriette K Sainty J Deleflie M Iatrogenic Cerebral Air Embolism Importance of an Early Hyperbaric Oxygenation Intensive Care Med 2002 28 559 563 CrossRef Bitterman H Melamed Y Delayed Hyperbaric Treatment of Cerebral Air Embolism Isr J Med Sci 1993 29 22 26 Schlimp C J Bothma P A Brodbeck A E Cerebral Venous Air Embolism What Is It and Do We Know How to Deal With It Properly JAMA Neurol 2014 71 243 CrossRef PubMed Bothma P A Schlimp C J II Retrograde Cerebral Venous Gas Embolism Are We Missing Too Many Cases Br J Anaesth 2014 112 401 404 CrossRef PubMed Hayreh S S Central Retinal Artery Occlusion Indian J Ophthalmol 2018 66 1684 1694 CrossRef PubMed Hanley M E Cooper J S Hyperbaric Central Retinal Artery Occlusion StatPearls Publishing Treasure Island FL USA 2018
Medicina 2021 57 864 21 of 25 105 Bagl B S evik S G evik M T Effect of Hyperbaric Oxygen Treatment in Central Retinal Artery Occlusion Undersea Hyperb Med 2018 45 421 425 CrossRef 106 Olson E A Lentz K Central Retinal Artery Occlusion A Literature Review and the Rationale for Hyperbaric Oxygen Therapy Mol Med 2016 113 53 57 107 Kim S H Cha Y S Lee Y Kim H Yoon I N Successful Treatment of Central Retinal Artery Occlusion Using Hyperbaric Oxygen Therapy Clin Exp Emerg Med 2018 5 278 281 CrossRef 108 Youn T S Lavin P Patrylo M Schindler J Kirshner H Greer D M Schrag M Current Treatment of Central Retinal Artery Occlusion A National Survey J Neurol 2018 265 330 335 CrossRef 109 Yu M Yuan H S Li Q Li Q Teng Y F Combination of Cells Based Therapy with Apelin 13 and Hyperbaric Oxygen Efficiently Promote Neovascularization in Ischemic Animal Model Eur Rev Med Pharmacol Sci 2019 23 2630 2639 CrossRef 110 Santema K T B Stoekenbroek R M Koelemay M J W Reekers J A Van Dortmont L M C Oomen A Smeets L Wever J J Legemate D A Ubbink D T Hyperbaric Oxygen Therapy in the Treatment of Ischemic Lower Extremity Ulcers in Patients with Diabetes Results of the DAMO2CLES Multicenter Randomized Clinical Trial Diabetes Care 2018 41 112 119 CrossRef 111 Abidia A Laden G Kuhan G Johnson B F Wilkinson A R Renwick P M Masson E A McCollum P T The Role of Hyperbaric Oxygen Therapy in Ischaemic Diabetic Lower Extremity Ulcers A Double Blind Randomized Controlled Trial Eur J Vasc Endovasc Surg 2003 25 513 518 CrossRef 112 Nakamura H Makiguchi T Atomura D Yamatsu Y Shirabe K Yokoo S Changes in Skin Perfusion Pressure After Hyperbaric Oxygen Therapy Following Revascularization in Patients With Critical Limb Ischemia A Preliminary Study Int J Low Extrem Wounds 2020 19 57 62 CrossRef 113 Rose J J Wang L Xu Q McTiernan C F Shiva S Tejero J Gladwin M T Carbon Monoxide Poisoning Pathogenesis Management and Future Directions of Therapy Am J Respir Crit Care Med 2017 195 596 606 CrossRef 114 Martani L Cantadori L Paganini M Camporesi E M Bosco G Carbon Monoxide Intoxication Prehospital Diagnosis and Direct Transfer to the Hyperbaric Chamber Minerva Anestesiol 2019 85 920 922 CrossRef 115 Rose J J Nouraie M Gauthier M C Pizon A F Saul M I Donahoe M P Gladwin M T Clinical Outcomes and Mortality Impact of Hyperbaric Oxygen Therapy in Patients With Carbon Monoxide Poisoning Crit Care Med 2018 46 e649 e655 CrossRef 116 Weaver L K Hopkins R O Chan K J Churchill S Elliott C G Clemmer T P Orme J F Thomas F O Morris A H Hyperbaric Oxygen for Acute Carbon Monoxide Poisoning N Engl J Med 2002 347 1057 1067 CrossRef 117 Hampson N B Piantadosi C A Thom S R Weaver L K Practice Recommendations in the Diagnosis Management and Prevention of Carbon Monoxide Poisoning Am J Respir Crit Care Med 2012 186 1095 1101 CrossRef 118 Hanley M E Murphy Lavoie H M Hyperbaric Cyanide Toxicity StatPearls Publishing Treasure Island FL USA 2019 119 Lawson Smith P Jansen E C Hilsted L Johnsen A H Hyldegaard O Effect of Acute and Delayed Hyperbaric Oxygen Therapy on Cyanide Whole Blood Levels during Acute Cyanide Intoxication Undersea Hyperb Med 2011 38 17 26 120 Van Meter K W The Effect of Hyperbaric Oxygen on Severe Anemia Undersea Hyperb Med 2012 39 937 942 121 Rhee T M Hwang D Lee J S Park J Lee J M Addition of Hyperbaric Oxygen Therapy vs Medical Therapy Alone for Idiopathic Sudden Sensorineural Hearing Loss A Systematic Review and Meta Analysis JAMA Otolaryngol Head Neck Surg 2018 144 1153 1161 CrossRef 122 Bayoumy A B de Ru J A The Use of Hyperbaric Oxygen Therapy in Acute Hearing Loss A Narrative Review Eur Arch Oto Rhino Laryngol 2019 276 1859 1880 CrossRef 123 Paderno E Zanon V Vezzani G Giacon T Bernasek T Camporesi E Bosco G Evidence Supported HBO Therapy in Femoral Head Necrosis A Systematic Review and Meta Analysis Int J Environ Res Public Health 2021 18 2888 CrossRef 124 Brenner I Shephard R J Shek P N Immune Function in Hyperbaric Environments Diving and Decompression Undersea Hyperb Med 1999 26 27 39 125 Xu X Yi H Kato M Suzuki H Kobayashi S Takahashi H Nakashima I Differential Sensitivities to Hyperbaric Oxygen of Lymphocyte Subpopulations of Normal and Autoimmune Mice Immunol Lett 1997 59 79 84 CrossRef 126 Saito K Tanaka Y Ota T Eto S Yamashita U Suppressive Effect of Hyperbaric Oxygenation on Immune Responses of Normal and Autoimmune Mice Clin Exp Immunol 1991 86 322 327 CrossRef 127 Chen S Y Chen Y C Wang J K Hsu H P Ho P S Chen Y C Sytwu H K Early Hyperbaric Oxygen Therapy Attenuates Disease Severity in Lupus Prone Autoimmune NZB NZW F1 Mice Clin Immunol 2003 108 103 110 CrossRef 128 Harnanik T Soeroso J Suryokusumo M G Juliandhy T Effects of Hyperbaric Oxygen on t Helper 17 Regulatory t Polarization in Antigen and Collagen Induced Arthritis Hypoxia Inducible Factor 1 as a Target Oman Med J 2020 35 e90 CrossRef PubMed 129 Novak S Drenjancevic I Vukovic R Kellermayer Z Cosic A Tolusic Levak M Balogh P Culo F Mihalj M AntiInflammatory Effects of Hyperbaric Oxygenation during DSS Induced Colitis in BALB c Mice Include Changes in Gene Expression of HIF 1 Proinflammatory Cytokines and Antioxidative Enzymes Mediat Inflamm 2016 2016 7141430 CrossRef PubMed 130 Resanovic I Gluvic Z Zaric B Sudar Milovanovic E Jovanovic A Milacic D Isakovic R Isenovic E R Early Effects of Hyperbaric Oxygen on Inducible Nitric Oxide Synthase Activity Expression in Lymphocytes of Type 1 Diabetes Patients A Prospective Pilot Study Int J Endocrinol 2019 2019 2328505 CrossRef PubMed
Medicina 2021 57 864 22 of 25 131 Bellato E Marini E Castoldi F Barbasetti N Mattei L Bonasia D E Blonna D Fibromyalgia Syndrome Etiology Pathogenesis Diagnosis and Treatment Pain Res Treat 2012 2012 17 CrossRef 132 Guggino G Schinocca C Lo Pizzo M Di Liberto D Garbo D Raimondo S Alessandro R Brighina F Ruscitti P Giacomelli R et al T Helper 1 Response Is Correlated with Widespread Pain Fatigue Sleeping Disorders and the Quality of Life in Patients with Fibromyalgia and Is Modulated by Hyperbaric Oxygen Therapy Clin Exp Rheumatol 2019 37 Suppl 116 81 89 133 Woo J Min J H Lee Y H Roh H T Effects of Hyperbaric Oxygen Therapy on Inflammation Oxidative Antioxidant Balance and Muscle Damage after Acute Exercise in Normobaric Normoxic and Hypobaric Hypoxic Environments A Pilot Study Int J Environ Res Public Health 2020 17 7377 CrossRef 134 Ortega M A Fraile Mart nez O Garc a Montero C Garc a Gallego S S nchez Trujillo L Torres Carranza D lvarez Mon M Pekarek L Garc a Honduvilla N Bujan J et al An Integrative Look at SARS CoV 2 Review Int J Mol Med 2021 47 415 434 CrossRef 135 del Barco A A Ortega M A Epidemiology and Public Health in the COVID 19 Epidemic Medicine 2020 13 1297 1304 CrossRef 136 Chandra A Chakraborty U Pal J Karmakar P Silent Hypoxia A Frequently Overlooked Clinical Entity in Patients with COVID 19 BMJ Case Rep 2020 13 237207 CrossRef 137 Dhont S Derom E Van Braeckel E Depuydt P Lambrecht B N The Pathophysiology of happy Hypoxemia in COVID 19 Respir Res 2020 21 198 CrossRef 138 lvarez Mon M Ortega M A Gasulla Fortuny Profit s J Mazaira Font F A Saurina P Monserrat J Plana M N Troncoso D Moreno J S et al A Predictive Model and Risk Factors for Case Fatality of Covid 19 J Pers Med 2021 11 36 CrossRef 139 Tobin M J Laghi F Jubran A Why COVID 19 Silent Hypoxemia Is Baffling to Physicians Am J Respir Crit Care Med 2020 202 356 360 CrossRef 140 Wilkerson R G Adler J D Shah N G Brown R Silent Hypoxia A Harbinger of Clinical Deterioration in Patients with COVID 19 Am J Emerg Med 2020 38 2243 e5 2243 e6 CrossRef 141 Brouqui P Amrane S Million M Cortaredona S Parola P Lagier J C Raoult D Asymptomatic Hypoxia in COVID 19 Is Associated with Poor Outcome Int J Infect Dis 2021 102 233 238 CrossRef 142 Lindahl S G E Using the Prone Position Could Help to Combat the Development of Fast Hypoxia in Some Patients with COVID 19 Acta Paediatr Int J Paediatr 2020 109 1539 1544 CrossRef 143 Oliaei S SeyedAlinaghi S Mehrtak M Karimi A Noori T Mirzapour P Shojaei A Mohsseni Pour M Mirghaderi S P Alilou S et al The effects of hyperbaric oxygen therapy HBOT on coronavirus disease 2019 COVID 19 A systematic review Eur J Med Res 2021 26 96 CrossRef PubMed 144 Paganini M Bosco G Perozzo F A G Kohlscheen E Sonda R Bassetto F Garetto G Camporesi E M Thom S R The Role of Hyperbaric Oxygen Treatment for COVID 19 A Review Adv Exp Med Biol 2021 1289 27 35 CrossRef PubMed 145 De Maio A Hightower L E COVID 19 Acute Respiratory Distress Syndrome ARDS and Hyperbaric Oxygen Therapy HBOT What Is the Link Cell Stress Chaperones 2020 25 717 720 CrossRef PubMed 146 Criado P R Miot H A Pincelli T P H Fabro A T From Dermatological Conditions to COVID 19 Reasoning for Anticoagulation Suppression of Inflammation and Hyperbaric Oxygen Therapy Dermatol Ther 2021 34 e14565 CrossRef 147 Xiaoling Z Xiaolan T Yanchao T Ruiyong C The Outcomes of Hyperbaric Oxygen Therapy to Retrieve Hypoxemia of Severe Novel Coronavirus Pneumonia First Case Report Chin J Naut Med Hyperb Med 2020 27 E001 CrossRef 148 Kjellberg A De Maio A Lindholm P Can Hyperbaric Oxygen Safely Serve as an Anti Inflammatory Treatment for COVID 19 Med Hypotheses 2020 144 110224 CrossRef 149 Senniappan K Jeyabalan S Rangappa P Kanchi M Hyperbaric Oxygen Therapy Can It Be a Novel Supportive Therapy in COVID 19 Indian J Anaesth 2020 64 835 841 150 Thibodeaux K Speyrer M Raza A Yaakov R Serena T E Hyperbaric Oxygen Therapy in Preventing Mechanical Ventilation in COVID 19 Patients A Retrospective Case Series J Wound Care 2020 29 S4 S8 CrossRef 151 Guo D Pan S Wang M Guo Y Hyperbaric Oxygen Therapy May Be Effective to Improve Hypoxemia in Patients with Severe COVID 2019 Pneumonia Two Case Reports Undersea Hyperb Med J Undersea Hyperb Med Soc Inc 2020 47 181 187 CrossRef 152 Tian S Hu W Niu L Liu H Xu H Xiao S Y Pulmonary Pathology of Early Phase 2019 Novel Coronavirus COVID 19 Pneumonia in Two Patients With Lung Cancer J Thorac Oncol 2020 15 700 704 CrossRef 153 Cavezzi A Troiani E Corrao S COVID 19 Hemoglobin Iron and Hypoxia beyond Inflammation A Narrative Review Clin Pract 2020 10 24 30 CrossRef 154 Allali G Marti C Grosgurin O Mor lot Panzini C Similowski T Adler D Dyspnea The vanished warning symptom of COVID 19 pneumonia J Med Virol 2020 92 2272 2273 CrossRef 155 El Hawa A A A Charipova K Bekeny J C Johnson Arbor K K The Evolving Use of Hyperbaric Oxygen Therapy during the COVID 19 Pandemic J Wound Care 2021 30 S8 S11 CrossRef 156 Hanahan D Weinberg R A Hallmarks of Cancer The next Generation Cell 2011 144 646 674 CrossRef
Medicina 2021 57 864 23 of 25 157 Muz B de la Puente P Azab F Azab A K The Role of Hypoxia in Cancer Progression Angiogenesis Metastasis and Resistance to Therapy Hypoxia 2015 3 83 CrossRef 158 Ortega M A Fraile Mart nez O As nsolo Buj n J Garc a Honduvilla N Coca S Signal Transduction Pathways in Breast Cancer The Important Role of PI3K Akt MTOR J Oncol 2020 2020 9258396 CrossRef 159 Jing X Yang F Shao C Wei K Xie M Shen H Shu Y Role of Hypoxia in Cancer Therapy by Regulating the Tumor Microenvironment Mol Cancer 2019 18 157 CrossRef 160 Dhani N Fyles A Hedley D Milosevic M The Clinical Significance of Hypoxia in Human Cancers Semin Nucl Med 2015 45 110 121 CrossRef 161 Kim S W Kim I K Lee S H Role of Hyperoxic Treatment in Cancer Exp Biol Med 2020 245 851 860 CrossRef 162 Moen I Stuhr L E B Hyperbaric Oxygen Therapy and Cancer A Review Target Oncol 2012 7 233 242 CrossRef 163 St epien K Ostrowski R P Matyja E Hyperbaric Oxygen as an Adjunctive Therapy in Treatment of Malignancies Including Brain Tumours Med Oncol 2016 33 101 CrossRef PubMed 164 Thews O Vaupel P Spatial Oxygenation Profiles in Tumors during Normo and Hyperbaric Hyperoxia Strahlenther Onkol 2015 191 875 882 CrossRef PubMed 165 Feldmeier J Carl U Hartmann K Sminia P Hyperbaric Oxygen Does It Promote Growth or Recurrence of Malignancy Undersea Hyperb Med 2003 30 1 18 PubMed 166 Pande S Sengupta A Srivastava A Gude R P Ingle A Re Evaluate the Effect of Hyperbaric Oxygen Therapy in Cancer A Preclinical Therapeutic Small Animal Model Study PLoS ONE 2012 7 e48432 CrossRef 167 Lu Q Z Li X Ouyang J Li J Q Chen G Further Application of Hyperbaric Oxygen in Prostate Cancer Med Gas Res 2018 8 167 171 168 Batra S Adekola K Rosen S Shanmugam M Cancer Metabolism as a Therapeutic Target Oncology 2013 27 460 467 169 Poff A M Ari C Seyfried T N D Agostino D P The Ketogenic Diet and Hyperbaric Oxygen Therapy Prolong Survival in Mice with Systemic Metastatic Cancer PLoS ONE 2013 8 e65522 CrossRef 170 Poff A M Ward N Seyfried T N Arnold P D Agostino D P Non Toxic Metabolic Management of Metastatic Cancer in VM Mice Novel Combination of Ketogenic Diet Ketone Supplementation and Hyperbaric Oxygen Therapy PLoS ONE 2015 10 e0127407 CrossRef 171 Baskar R Lee K A Yeo R Yeoh K W Cancer and Radiation Therapy Current Advances and Future Directions Int J Med Sci 2012 9 193 199 CrossRef 172 Arienti C Pignatta S Zanoni M Zamagni A Cortesi M Sarnelli A Romeo A Arpa D Longobardi P Bartolini D et al High Pressure Oxygen Rewires Glucose Metabolism of Patient Derived Glioblastoma Cells and Fuels Inflammasome Response Cancer Lett 2021 506 152 166 CrossRef 173 Arpa D Parisi E Ghigi G Cortesi A Longobardi P Cenni P Pieri M Tontini L Neri E Micheletti S et al Role of Hyperbaric Oxygenation Plus Hypofractionated Stereotactic Radiotherapy in Recurrent High Grade Glioma Front Oncol 2021 11 964 CrossRef 174 Majeed H Gupta V Adverse Effects of Radiation Therapy StatPearls Publishing Treasure Island FL USA 2020 175 Brush J Lipnick S L Phillips T Sitko J McDonald J T McBride W H Molecular Mechanisms of Late Normal Tissue Injury Semin Radiat Oncol 2007 17 121 130 CrossRef 176 Cooper J S Hanley M E Hendriksen S Robins M Hyperbaric Treatment of Delayed Radiation Injury StatPearls Publishing Treasure Island FL USA 2020 177 Feldmeier J J Hyperbaric Oxygen Therapy and Delayed Radiation Injuries Soft Tissue and Bony Necrosis 2012 Update Undersea Hyperb Med 2012 39 1121 1139 178 Bennett M H Feldmeier J Hampson N B Smee R Milross C Hyperbaric Oxygen Therapy for Late Radiation Tissue Injury Cochrane Database Syst Rev 2016 2016 CD005005 CrossRef 179 Brewer A L Shirachi D Y Quock R M Craft R M Effect of Hyperbaric Oxygen on Chemotherapy Induced Neuropathy in Male and Female Rats Behav Pharmacol 2020 31 61 72 CrossRef 180 Fu H Li F Thomas S Yang Z Hyperbaric Oxygenation Alleviates Chronic Constriction Injury CCI Induced Neuropathic Pain and Inhibits GABAergic Neuron Apoptosis in the Spinal Cord Scand J Pain 2017 17 330 338 CrossRef 181 Zhang Y Brewer A L Nelson J T Smith P T Shirachi D Y Quock R M Hyperbaric Oxygen Produces a Nitric Oxide Synthase Regulated Anti Allodynic Effect in Rats with Paclitaxel Induced Neuropathic Pain Brain Res 2019 1711 41 47 CrossRef 182 Gibbons C R Liu S Zhang Y Sayre C L Levitch B R Moehlmann S B Shirachi D Y Quock R M Involvement of Brain Opioid Receptors in the Anti Allodynic Effect of Hyperbaric Oxygen in Rats with Sciatic Nerve Crush Induced Neuropathic Pain Brain Res 2013 1537 111 116 CrossRef 183 Kawasoe Y Yokouchi M Ueno Y Iwaya H Yoshida H Komiya S Hyperbaric Oxygen as a Chemotherapy Adjuvant in the Treatment of Osteosarcoma Oncol Rep 2009 22 1045 1050 CrossRef 184 Petre P M Baciewicz F A Tigan S Spears J R Patterson G A Swisher S G Harpole D H Goldstraw P Hyperbaric Oxygen as a Chemotherapy Adjuvant in the Treatment of Metastatic Lung Tumors in a Rat Model J Thorac Cardiovasc Surg 2003 125 85 95 CrossRef
Medicina 2021 57 864 24 of 25 185 Ohguri T Imada H Narisada H Yahara K Morioka T Nakano K Miyaguni Y Korogi Y Systemic Chemotherapy Using Paclitaxel and Carboplatin plus Regional Hyperthermia and Hyperbaric Oxygen Treatment for Non Small Cell Lung Cancer with Multiple Pulmonary Metastases Preliminary Results Int J Hyperth 2009 25 160 167 CrossRef 186 Baude J Cooper J S Hyperbaric Contraindicated Chemotherapeutic Agents StatPearls Publishing Treasure Island FL USA 2020 187 Ortega M A Fraile Mart nez O Garc a Montero C Pekarek L Guijarro L G Castellanos A J Sanchez Trujillo L Garc aHonduvilla N lvarez Mon M Buj n J et al Physical Activity as an Imperative Support in Breast Cancer Management Cancers 2021 13 55 CrossRef 188 Hadanny A Lang E Copel L Meir O Bechor Y Fishlev G Bergan J Friedman M Zisman A Efrati S Hyperbaric Oxygen Can Induce Angiogenesis and Recover Erectile Function Int J Impot Res 2018 30 292 299 CrossRef 189 Chiles K A Staff I Johnson Arbor K Champagne A McLaughlin T Graydon R J A Double Blind Randomized Trial on the Efficacy and Safety of Hyperbaric Oxygenation Therapy in the Preservation of Erectile Function after Radical Prostatectomy J Urol 2018 199 805 811 CrossRef 190 Cormier J Theriot M Patient Diagnosed with Chronic Erectile Dysfunction Refractory to PDE 5 Inhibitor Therapy Reports Improvement in Function after Hyperbaric Oxygen Therapy Undersea Hyperb Med 2016 43 463 465 191 Yuan J B Yang L Y Wang Y H Ding T Chen T D Lu Q Hyperbaric Oxygen Therapy for Recovery of Erectile Function after Posterior Urethral Reconstruction Int Urol Nephrol 2011 43 755 761 CrossRef 192 Lippert T Borlongan C V Prophylactic Treatment of Hyperbaric Oxygen Treatment Mitigates Inflammatory Response via Mitochondria Transfer CNS Neurosci Ther 2019 25 815 823 CrossRef 193 Liska G M Lippert T Russo E Nieves N Borlongan C V A Dual Role for Hyperbaric Oxygen in Stroke Neuroprotection Preconditioning of the Brain and Stem Cells Cond Med 2018 1 151 166 194 Ding Z Tong W C Lu X X Peng H P Hyperbaric Oxygen Therapy in Acute Ischemic Stroke A Review Interv Neurol 2014 2 201 211 CrossRef 195 Hachmo Y Hadanny A Abu Hamed R Daniel Kotovsky M Catalogna M Fishlev G Lang E Polak N Doenyas K Friedman M et al Hyperbaric Oxygen Therapy Increases Telomere Length and Decreases Immunosenescence in Isolated Blood Cells A Prospective Trial Aging 2020 12 22445 22456 CrossRef 196 Nishizaka T Nomura T Higuchi K Takemura A Ishihara A Mild Hyperbaric Oxygen Activates the Proliferation of Epidermal Basal Cells in Aged Mice J Dermatol 2018 45 1141 1144 CrossRef PubMed 197 Godman C A Joshi R Giardina C Perdrizet G Hightower L E Hyperbaric Oxygen Treatment Induces Antioxidant Gene Expression Ann N Y Acad Sci 2010 1197 178 183 CrossRef PubMed 198 Amir H Malka D K Gil S Rahav B G Merav C Kobi D Yafit H Ramzia A H Efrat S Gregory F et al Cognitive Enhancement of Healthy Older Adults Using Hyperbaric Oxygen A Randomized Controlled Trial Aging 2020 12 13740 13761 CrossRef PubMed 199 Shwe T Bo Htay C Ongnok B Chunchai T Jaiwongkam T Kerdphoo S Kumfu S Pratchayasakul W Pattarasakulchai T Chattipakorn N et al Hyperbaric Oxygen Therapy Restores Cognitive Function and Hippocampal Pathologies in Both Aging and Aging Obese Rats Mech Ageing Dev 2021 195 111465 CrossRef 200 Camporesi E M Side Effects of Hyperbaric Oxygen Therapy Undersea Hyperb Med 2014 41 253 257 201 Heyboer M Sharma D Santiago W McCulloch N Hyperbaric Oxygen Therapy Side Effects Defined and Quantified Adv Wound Care 2017 6 210 224 CrossRef 202 Hadanny A Meir O Bechor G Fishlev J Efrati S Seizures during Hyperbaric Oxygen Therapy Retrospective Analysis of 62 614 Treatment Sessions Undersea Hyperb Med 2016 43 21 28 203 Cooper J S Phuyal P Shah N Oxygen Toxicity StatPearls Publishing Treasure Island FL USA 2021 Available online https www ncbi nlm nih gov books NBK430743 accessed on 28 March 2021 204 Domachevsky L Rachmany L Barak Y Rubovitch V Abramovich A Pick C G Hyperbaric Oxygen Induced Seizures Cause a Transient Decrement in Cognitive Function Neuroscience 2013 247 328 334 CrossRef 205 Nakane M Biological Effects of the Oxygen Molecule in Critically Ill Patients J Intensive Care 2020 8 95 CrossRef 206 Hadanny A Zubari T Tamir Adler L Bechor Y Fishlev G Lang E Polak N Bergan J Friedman M Efrati S Hyperbaric Oxygen Therapy Effects on Pulmonary Functions A Prospective Cohort Study BMC Pulm Med 2019 19 148 CrossRef 207 Mcmonnies C W Hyperbaric Oxygen Therapy and the Possibility of Ocular Complications or Contraindications Clin Exp Optom 2015 98 122 125 CrossRef 208 Sola A Chow L Rogido M Retinopathy of Prematurity and Oxygen Therapy A Changing Relationship An Pediatr 2005 62 48 63 CrossRef 209 Gawdi R Cooper J S Hyperbaric Contraindications StatPearls Publishing Treasure Island FL USA 2020 210 Arslan A Hyperbaric Oxygen Therapy in Carbon Monoxide Poisoning in Pregnancy Maternal and Fetal Outcome Am J Emerg Med 2021 43 41 45 CrossRef 211 Stevens S L Narr A J Claus P L Millman M P Steinkraus L W Shields R C Buchta W G Haddon R Wang Z Murad M H The Incidence of Hypoglycemia during HBO2 Therapy A Retrospective Review Undersea Hyperb Med 2015 42 191 196 212 Al Waili N S Butler G J Beale J Abdullah M S Finkelstein M Merrow M Rivera R Petrillo R Carrey Z Lee B et al Influences of Hyperbaric Oxygen on Blood Pressure Heart Rate and Blood Glucose Levels in Patients with Diabetes Mellitus and Hypertension Arch Med Res 2006 37 991 997 CrossRef
Medicina 2021 57 864 25 of 25 213 Weaver L K Churchill S Pulmonary Edema Associated with Hyperbaric Oxygen Therapy Chest 2001 120 1407 1409 CrossRef 214 Kahle A C Cooper J S Hyperbaric Physiological And Pharmacological Effects Gases StatPearls Publishing Treasure Island FL USA 2019 215 Wang X Li S Liu X Wu X Ye N Yang X Li Z Boosting Nanomedicine Efficacy with Hyperbaric Oxygen Therapy In Advances in Experimental Medicine and Biology Springer Berlin Heidelberg Germany 2021 Volume 1295 pp 77 95
Huang and Obenaus Medical Gas Research 2011 1 21 http www medicalgasresearch com content 1 1 21 MEDICAL GAS RESEARCH REVIEW Open Access Hyperbaric oxygen therapy for traumatic brain injury Lei Huang1 and Andre Obenaus1 2 3 4 5 Abstract Traumatic brain injury TBI is a major public health issue The complexity of TBI has precluded the use of effective therapies Hyperbaric oxygen therapy HBOT has been shown to be neuroprotective in multiple neurological disorders but its efficacy in the management of TBI remains controversial This review focuses on HBOT applications within the context of experimental and clinical TBI We also discuss its potential neuroprotective mechanisms Early or delayed multiple sessions of low atmospheric pressure HBOT can reduce intracranial pressure improve mortality as well as promote neurobehavioral recovery The complimentary synergistic actions of HBOT include improved tissue oxygenation and cellular metabolism anti apoptotic and anti inflammatory mechanisms Thus HBOT may serve as a promising neuroprotective strategy that when combined with other therapeutic targets for TBI patients which could improve long term outcomes Keywords intracranial pressure metabolism apoptosis inflammation tissue oxygenation cerebral blood flow Introduction Hyperbaric oxygen therapy HBOT is a treatment by which 100 oxygen is administered to a patient at a pressure greater than atmospheric pressure at sea level i e one atmosphere absolute ATA 1 The increased partial pressure of oxygen pO2 within the blood and subsequent improved mitochondrial metabolism tissue oxygenation constitutes the net effect of HBOT 2 6 Given that the dissolved oxygen content in the plasma increases linearly after hemoglobin is 100 saturated 7 8 plasma bound oxygen can be used more readily than that bound to hemoglobin which enables tissue oxygen delivery even in the absence of red blood cells 7 9 Thus HBOT induces a much larger oxygen carrying capacity in the blood that dramatically increases the driving force of oxygen diffusion to tissues Although HBOT induced cerebral vasoconstriction appears to be undesirable within the context of ischemic conditions 10 11 this may not be necessarily deleterious due to increased oxygen availability to injured tissues HBOT may also counter vasodilation of the capillaries within hypoxic tissues thereby minimizing collection of extravascular fluids edema which ultimately reduces brain vasogenic edema and the ensuing decrease in intracranial pressure ICP 5 12 14 Emerging evidence has shown the neuroprotective effects of HBOT in a range of multiple injuries and or disorders Additional file 1 Table S1 15 The most common clinical applications include decompression sickness carbon monoxide poisoning minimization of radiation therapy induced tissue damage and enhancing skin grafts 1 16 which are all covered by insurance Medicare There are numerous unapproved uses of HBOT that focus on more complex neurological disorders including autism multiple sclerosis and stroke which have shown promising results in experimental settings but clinical efficacy is still elusive Recent efforts have applied HBOT to traumatic brain injury 5 14 17 While significant research on HBOT therapy has been undertaken 10 000 citations on PubMed very little has been reported for HBOT within the setting of TBI 30 citations We now briefly review the experimental and clinical HBO research relevant to TBI HBOT in animal models of TBI Correspondence aobenaus llu edu 1 Department of Biophysics Bioengineering Loma Linda University Griggs Hall Room 227 11065 Campus St Loma Linda California 92354 USA Full list of author information is available at the end of the article Early experimental research focused on the effects of HBO on brain edema ICP and cerebral blood flow 2011 Huang and Obenaus licensee BioMed Central Ltd This is an Open Access article distributed under the terms of the Creative Commons Attribution License http creativecommons org licenses by 2 0 which permits unrestricted use distribution and reproduction in any medium provided the original work is properly cited
Huang and Obenaus Medical Gas Research 2011 1 21 http www medicalgasresearch com content 1 1 21 CBF Dunn and colleagues first demonstrated the neuroprotective effects of hyperoxia in a dog freeze lesion model of brain injury that simulated a brain contusion Hyperoxia significantly improved outcomes by reducing mortality 18 Reduced ICP 30 decrease and CBF 19 were also reported in a dog model of brain injury treated by HBOT 2 ATA for 4 hrs 19 The absence of changes in cerebrospinal fluid CSF lactate a marker of brain injury following HBOT further supported the notion that HBO improved tissue oxygen delivery despite the undesirable decrease in CBF subsequent to vasoconstriction 10 Expanding on the original model various methods psyllium seed extradural balloon were used to induce brain edema in dogs followed by HBOT 20 23 Using HBOT at 3 ATA for 45 min 20 21 or at 2 ATA for 4 hrs 22 resulted in a significant decrease 50 in mortality relative to non treated injured animals They also reported significantly less brain edema 20 and reduced cisternal CSF pressure 21 in the HBOT groups Sukoff and colleagues suggested that the improvement seen in their model was due to the effectiveness of HBOT against ischemia secondary to the induced cerebral edema 21 Hayakawa et al however found that HBOT 3 ATA for 1 hr did not or barely changed CSF pressure and CBF in most injured dogs 23 In a rat model of moderate fluid percussion injury the neuroprotection afforded by HBOT translated into long term cognitive improvements characterized by a shorter latency to find a hidden platform in Morris water maze MWM performance 2 Within brain tissues HBOT showed significant protection against hippocampal neuronal loss compared to normobaric oxygen treatment 2 Importantly there was no increased free radial peroxide and peroxynitrite production suggesting the absence of oxygen toxicity after HBOT 2 Studies in a model of cerebral ischemia concurred that HBOT did not exacerbate lipid peroxidation 24 The aforementioned neuroprotective efficacy of HBOT was all achieved when intervention was administered during the acute phase within hours of post TBI The prolonged therapeutic time window of HBOT was further investigated in studies using a focal cortical weigh drop model of TBI 25 27 Wang and colleagues have demonstrated that multiple HBOT 3 ATA hourly for 3 or 5 days delivered at latest 2 days post injury resulted in significantly reduced overall neurological deficit scores and neuronal apoptosis within brain tissue But the authors also showed that twelve hours post TBI is the latest effective window for neuroprotection when a single episode of HBOT was delivered 27 Moreover Harch et al 25 26 have tested the effects of low pressure HBOT 90 min twice a day at 1 5 ATA which started at 50 days after the initial brain injury for a total duration of 40 days At end Page 2 of 7 of the treatment 100 days post injury MWM spatial learning performance in the HBOT groups improved significantly and was highly correlated with increased ipsilateral hippocampal blood volume cerebrovascular density measured by diaminobenzadine blood stain 25 26 Given the well described presence of angiogenesis in HBOT in other brain injury models 28 29 the authors suggested that angiogenesis was the most likely explanation for the HBOT induced recovery of function They claimed that coupling of blood flow and metabolism and metabolism and function were potential mechanisms as both were increased in animals receiving HBOT This hypothesis is consistent with the pattern of HBOT induced increases in blood flow seen on single photon emission computed tomography brain imaging in patients with chronic TBI 30 31 A caveat is that HBOT failed to improve forelimb placing function likely due to the reported tissue loss within the sensorimotor cortex following TBI 26 We recently investigated both prophylactic pre treatment hyperbaric oxygen HBO strategy and HBOT posttreatment for treatment of repetitive mild traumatic brain injury rmTBI personal communication Drs Lei Huang and Andre Obenaus Repetitive mTBI is an important public health concern for sports athletes and active military personnel as subsequent injuries are thought to exacerbate existing neuropathology Mild controlled cortical impact CCI was used to model rmTBI in adult rats In rmTBI animals a second mild CCI was delivered at the same location at 3 or 7 days after the initial impact HBO pre treatment or HBOT was given 1 hr daily at 2 ATA for 3 consecutive days either prior to or 24 hrs after the initial TBI respectively T2 weighted imaging T2WI and susceptibility weighted imaging SWI were acquired noninvasively from which lesion and hemorrhage volumes were quantified Our results clearly demonstrated that both HBO pre treatment and HBOT improved neuroimaging outcomes following rmTBI in contrast to those seen in tissues without HBO intervention There were significant reductions in the T2WI derived lesion and SWI identified hemorrhage volumes at 24 hrs after rmTBI Figures 1 2 The most dramatic neuroprotective effects were observed in animals receiving rmTBI 3 days apart where a 3 fold reduction in hemorrhage volumes was observed compared to Shams Figure 2 Given that the pathophysiological processes underlying rmTBI likely involves cellular metabolic perturbations in the injured brain 32 a neuroprotective approach namely HBO pre treatment or HBOT favoring cerebral aerobic metabolism could be beneficial Similar findings have been reported in HBOT for human severe TBI 14 Clinical HBOT for human TBI A variety of human injuries and neurological diseases have applied HBOT to improve outcomes More overt
Huang and Obenaus Medical Gas Research 2011 1 21 http www medicalgasresearch com content 1 1 21 Page 3 of 7 Figure 1 HBO reduces rmTBI lesion volumes Pre and post treatment with HBO reduces lesion volume identified from magnetic resonance imaging MRI T2 weighted images Repetitive mild traumatic brain injury rmTBI was induced 3 days apart and resulted in ipsilateral tissue damage On T2WI hypointensities white arrow are consistent with bleeding while hyperintensities black arrow suggest edema formation At 24 hrs after the rmTBI HBO pre or post treatment significantly reduced the lesion size compared to untreated animals The neuroprotective effects persisted to 14 days after the initial mTBI neurological injuries such as stroke or TBI have not been aggressively pursued partly due to apparent or perceived contraindications While a complete listing of the absolute and relative contraindications for clinical applications are beyond the scope of this review it should be noted that certain drugs fever and respiratory ailments limit clinical application of HBOT However within the realm of clinically applied HBOT for TBI very little research has been conducted Enthusiasm for HBOT for brain injured patients was dampened by the findings of a meta analysis of TBI patients receiving HBOT 33 Their sobering conclusions were that the risk of death was reduced but there was no apparent change in clinical outcomes However as these authors acknowledged variance in treatment protocols and the limited number of patients in the studies reviewed hampered their analysis Based on their findings they suggested that HBOT could not be justified for TBI patients The poor clinical outcomes of earlier HBOT studies combined with the relative success of normobaric oxygen therapy NBOT in TBI have lead some to propose that normobaric oxygen therapy should be used preferentially in brain injured patients There are numerous studies that demonstrate an enhanced clinical outcomes by treatment with normobaric oxygen 34 Much of the enthusiasm for use of NBOT is based on a prospective study of severe TBI patients 4 Narotam and colleagues 35 evaluated brain tissue oxygen concentrations in patients with severe TBI Using Licox oxygen probes 139 patients were studied using a pO2 protocol that maintained brain oxygen levels to 20 mm Hg They elegantly demonstrated that normobaric oxygen therapy significantly reduced mortality but moreover they showed improved clinical outcomes at 6 mo post severe TBI A similar study found that hyperoxia improved the cerebral metabolic rate of oxygen in severe TBI patients using
Huang and Obenaus Medical Gas Research 2011 1 21 http www medicalgasresearch com content 1 1 21 Page 4 of 7 Figure 2 HBOT reduces extravascular blood after rmTBI HBO pre and post treatment improved susceptibility weighted imaging SWI identified intracerebral hemorrhage following repetitive mild traumatic brain injury rmTBI 3 days apart At 24 hrs after rmTBI HBO pre or posttreatment significantly ameliorated the hemorrhage hypointensity asterisks compared to untreated animals which persisted to 14 days after the initial mTBI O15 postiron emission tomography but they did not compare to HBOT treated patients 36 Thus at a minimum NBOT could be beneficial for TBI patients The most extensive research into clinical application of HBOT for TBI patients has been conducted by the Rockswolds 5 14 17 37 Almost 30 years ago they undertook one of the first clinical trials in evaluating the benefits of HBOT for severe head injured patients 17 In that early study they demonstrated a 50 decrease in mortality but found no changes in the clinical outcome status i e good recovery and moderate disability As noted above a metaanalysis of several studies concluded the same findings reduced mortality but no change in clinical status 33 While survival was increased functional recovery was not changed leading to questions about the timing of the HBOT In addition the mechanism s underlying HBOT and its effects on cerebral metabolism had not been previously established in severely brain injured patients In another prospective clinical trial Rockswold et al 5 reported increased cerebral metabolic rate of oxygen and decreased lactate measured from cerebrospinal fluid after HBOT 1 5 ATA 1 hr day every 24 hrs with a maximum of seven sessions ICP was also reduced but a caveat was noted that these changes did not last till the next session 5 It also serves to remind the reader that similar results had also been previously reported in NBOT 36 Based on evidence that NBOT of human TBI patients appeared to have similar outcomes as patients who underwent HBOT a follow up study was conducted to compare these two groups after severe TBI to assess the efficacy of therapy 14 It is important to note that the standard of care is neither NBOT nor HBOT Thus their study design included controls standard of care normobaric 3 hrs 100 O2 and HBOT 1 5 ATA for 60 min that received their initial treatment within 24 hrs of a severe TBI Treatments were then conducted daily for 3 consecutive days
Huang and Obenaus Medical Gas Research 2011 1 21 http www medicalgasresearch com content 1 1 21 The pO2 levels within the brain were nearly 3 fold higher in the HBOT compared to the NBOT groups and significantly different from controls 14 As previously reported they found increased cerebral metabolic rate of oxygen decreased lactate and decreased intracranial pressure They also reported that HBOT increased cerebral blood flow Perhaps the most important finding was that an indicator of mitochondrial dysfunction lactate pyruvate ratios were significantly decreased only in the HBOT group They also demonstrated no adverse outcomes or harmful effects in patients receiving HBOT 14 Thus HBOT for severe TBI appears to improve cellular survival which was not observed in NBOT group Based on these limited studies it is clear that HBOT could be an effective therapy for clinical severe TBI Compared to NBOT HBOT assists in improving brain functions such as cerebral metabolism and blood flow However additional studies are needed not only during the acute phase of the injury but also long term studies evaluating outcomes to determine if HBOT is beneficial to TBI patients Putative mechanisms underlying the neuroprotection of HBOT following TBI Over the past several decades the neuroprotective mechanisms of HBOT have been investigated in a variety of animal models of TBI The initial work in dogs see above have shown the HBOT was able to increase tissue oxygen delivery 10 as well as to protect penumbra tissue from secondary ischemia 21 Based on the dog model a similar freeze induced brain injury was conducted in rats to evaluate local cerebral glucose utilization using the autoradiographic 2 deoxyglucose technique Compared to animals that underwent NBOT a four day HBOT course 2 ATA for 90 minutes daily significantly reversed the depressed glucose utilization within gray matter ipsilateral to the lesion 38 Interestingly HBOT tended to decrease glucose utilization in the sham operated animals However it was still uncertain whether the favorable outcomes were directly attributable to improved glucose metabolism associated with HBOT HBO improvements in tissue oxygenation and mitochondrial metabolic function were further investigated in a rat model of fluid percussion injury FPI 3 HBOT 1 hr 1 5 ATA with 3 hrs 100 normobaric oxygen treatments significantly improved 1 brain tissue pO2 more than 6 fold near the site of injury 2 ex vivo brain tissue oxygen consumption vO2 more than 1 fold and 3 recovery of synaptosomal mitochondrial metabolic activity 39 40 Given that the prognosis of TBI clearly depends on the processes of cell death and survival that occur within the traumatized tissues neuroprotective therapies need to mitigate and improve survival and function within the remaining viable perilesional brain tissue 41 The Page 5 of 7 neuroprotective effects of HBOT against secondary brain damage in the penumbra region have been extensively investigated 6 41 43 Using a model of dynamic cortical deformation DCD to produce focal cerebral contusion in rats HBOT 2 sessions at 2 8 ATA for 45 min each were administered at 3 hrs after TBI and compared to the effects of NBOT There were significantly smaller lesion volumes and decreased numbers of terminal deoxynucleotidyl transferase dUTP nick end labeling TUNEL a biomarker for apoptosis positive cells after HBOT Normobaric oxygen therapy 100 also improved tissue measures but not to the extent found after HBOT 43 The anti apoptotic modulator B cell lymphoma Bcl 2 was increased after HBOT and correlated to reduced tissue apoptosis 41 Similar changes were found for B cell lymphoma extra large Bcl xl expression while the proinflammatory protein B cell lymphoma associated X protein Bax was observed primarily in astrocytes instead of neurons The ratio between pro apoptotic Bax and antiapoptotic Bcl 2 Bcl xl proteins has been shown to act as a rheostat that sets the threshold 44 of susceptibility to apoptosis by competitively modulating the opening of the mitochondrial permeability transition pore mPTP 45 46 Enhanced Bcl 2 expression inhibits the mPTP that subsequently preserves mitochondrial homeostasis and therefore the integrity of the electron transport chain 6 Palzur et al thus hypothesized that HBOT induced increases in Bcl 2 expression and the resultant increase in intracellular oxygen bio availability may contribute both to preserve mitochondrial integrity and to reduce the activation of the mitochondrial mediated apoptotic pathway following TBI 6 In the same animal model HBOT 2 8 ATA for 45 min at 3 and 24 hrs post injury substantially facilitated the recovery of mPTP expression Subsequently TBI induced injury to tissue morphology was reversed with enhanced neuronal survival and preserved axonal architecture within perislesional tissues 6 Similar findings of improved mitochondrial redox after HBOT in the FPI model of TBI have also been reported 3 The preservation of mitochondrial integrity by HBOT hindered the activation of mitochondria associated apoptotic pathways by significantly lowering caspase 3 and 9 but not caspase 8 expression critical for non mitochondrial apoptotic pathway in injured brain tissues 6 These results underscore the importance of HBOT induced reductions in delayed cell death within the tissue penumbra after TBI Such mechanisms echo the neuroprotection of HBO seen in brain ischemia and subarachnoid hemorrhage 47 48 Acute inflammation also plays an important role in secondary brain damage after TBI An influx of inflammatory cells induced by TBI provides the primary source of matrix metalloproteinases MMPs activity 49 MMPs in the injured brain further play a deleterious role and promote cell death including apoptosis 50 The effects
Huang and Obenaus Medical Gas Research 2011 1 21 http www medicalgasresearch com content 1 1 21 Page 6 of 7 of HBOT on inflammatory infiltration and the expression of MMPs have been explored in a rat model of DCD Both HBOT 2 8 ATA for 45 min at 3 hrs after injury and twice a day thereafter for 3 consecutive days and NBOT significantly decreased myeloperoxidase positive neutrophils within the traumatic penumbra but HBOT had a more pronounced effect HBOT also significantly reduced the elevation of MMP 9 expression associated with neutrophilic infiltration 42 Thus HBOT substantially decreases the harmful effects of inflammation by reducing MMP 9 over expression that then results in a reduction of delayed cell death in penumbral tissues surrounding the site of injury Interestingly reduced MMP 9 has also been proposed to be the underlying mechanism associated with HBO pretreatment induced neuroprotection against TBI at high altitude in a rat model 51 However what is still unresolved is whether the decreased numbers of apoptotic cells following HBOT is a direct anti apoptotic effect or secondary consequence due to HBOT anti inflammatory effects Further studies are warranted to disclose the complex mechanisms underlying the neuroprotective effects of HBOT after TBI MWM Morris water maze NBOT Normobaric therapy pO2 Partial pressure of oxygen rmTBI Repetitive mild traumatic brain injury SWI susceptibility weighted imaging TBI Traumatic brain injury TIMP 1 metallopeptidase inhibitor 1 TUNEL Terminal deoxynucleotidyl transferase dUTP nick end labeling T2WI T2 weighted imaging vO2 Oxygen consumption Conclusions Translational research of HBOT in a variety of TBI models has shown neuroprotective effects in the absence of increased oxygen toxicity when administered at pressures less than 3 ATA Due to the heterogeneity of human TBI the efficacy of clinical HBOT and an optimal regimen for HBOT remains elusive However all human studies have involved severe TBI patients and it is likely that there may be increased efficacy in mild or moderate TBI patients Recent clinical trials favor HBOT as promising safe therapeutic strategy for severe TBI patients Although both NBOT and 1 5 ATA HBOT can be neuroprotective HBOT exerts more robust and long lasting effects in the absence of pulmonary or cerebral oxygen toxicity The improved tissue oxygenation and cellular metabolism anti apoptotic as well as anti inflammatory effects may constitute the multiple and complementary mechanisms underlying HBOT induced neuroprotection Received 2 May 2011 Accepted 6 September 2011 Published 6 September 2011 Additional material Additional file 1 Table S1 Current clinical uses for HBOT List of abbreviations ATA One atmosphere absolute Bax B cell lymphoma associated X protein Bcl 2 B cell lymphoma Bcl xl B cell lymphoma extra large CBF Cerebral blood flow CCI Controlled cortical impact CSF Cerebrospinal fluid DCD Dynamic cortical deformation FPI Fluid percussion injury HBO Hyperbaric oxygen HBOT Hyperbaric oxygen therapy ICP Intracranial pressure MMPs Matrix metalloproteinases mPTP Mitochondrial permeability transition pore Acknowledgements The HBO research in rmTBI was supported by the Department of Defense DCMRP DR080470 The authors acknowledge Jacqueline Coats Alena Mohad Yousof and Yufang Yin for experimental rmTBI and data analysis We also acknowledge the imaging assistance of Kamalakar Ambadipudi and Sonny Kim Author details Department of Biophysics Bioengineering Loma Linda University Griggs Hall Room 227 11065 Campus St Loma Linda California 92354 USA 2 Department of Pediatrics Loma Linda University CSP A1010 11175 Campus St Loma Linda California 92354 USA 3Department of Radiology Loma Linda University Medical Center CSP A1010 11175 Campus St Loma Linda California 92354 USA 4Department of Radiation Medicine Loma Linda University CSP A1010 11175 Campus St Loma Linda California 92354 USA 5 Department of Neuroscience University of California Riverside 1140 Batchelor Hall University of California Riverside California 92521 USA 1 Authors contributions Both LH and AO contributed intellectually to this review LH reviewed the HBO studies in animal models of TBI and AO reviewed clinical trials of HBO in severe TBI patients All authors read and approved the final manuscript Competing interests The authors declare that they have no competing interests References 1 Gill AL Bell CN Hyperbaric Oxygen Its Uses Mechanisms of Action and Outcomes QJM 2004 97 385 395 2 Zhou Z Daugherty WP Sun D Levasseur JE Altememi N Hamm RJ et al Protection of Mitochondrial Function and Improvement in Cognitive Recovery in Rats Treated with Hyperbaric Oxygen Following Lateral Fluid Percussion Injury J Neurosurg 2007 106 687 694 3 Daugherty WP Levasseur JE Sun D Rockswold GL Bullock MR Effects of Hyperbaric Oxygen Therapy on Cerebral Oxygenation and Mitochondrial Function Following Moderate Lateral Fluid Percussion Injury in Rats J Neurosurg 2004 101 499 504 4 Tolias CM Reinert M Seiler R Gilman C Scharf A Bullock MR Normobaric Hyperoxia Induced Improvement in Cerebral Metabolism and Reduction in Intracranial Pressure in Patients with Severe Head Injury A Prospective Historical Cohort Matched Study J Neurosurg 2004 101 435 444 5 Rockswold SB Rockswold GL Vargo JM Erickson CA Sutton RL Bergman TA et al Effects of Hyperbaric Oxygenation Therapy on Cerebral Metabolism and Intracranial Pressure in Severely Brain Injured Patients J Neurosurg 2001 94 403 411 6 Palzur E Zaaroor M Vlodavsky E Milman F Soustiel JF Neuroprotective Effect of Hyperbaric Oxygen Therapy in Brain Injury Is Mediated by Preservation of Mitochondrial Membrane Properties Brain Res 2008 1221 126 133 7 Jain KK Origin of Textbook of Hyperbaric Medicine Cambrige MA Hogrefe Huber 2004 8 van Hulst RA Haitsma JJ Klein J Lachmann B Oxygen Tension under Hyperbaric Conditions in Healthy Pig Brain Clin Physiol Funct Imaging 2003 23 143 148 9 Calvert JW Cahill J Zhang JH Hyperbaric Oxygen and Cerebral Physiology Neurol Res 2007 29 132 141 10 Miller JD Ledingham IM Reduction of Increased Intracranial Pressure Comparison between Hyperbaric Oxygen and Hyperventilation Arch Neurol 1971 24 210 216 11 Lambertsen CJ Dough RH Cooper DY Emmel GL Loeschcke HH Schmidt CF Oxygen Toxicity Effects in Man of Oxygen Inhalation at 1
Huang and Obenaus Medical Gas Research 2011 1 21 http www medicalgasresearch com content 1 1 21 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 and 3 5 Atmospheres Upon Blood Gas Transport Cerebral Circulation and Cerebral Metabolism J Appl Physiol 1953 5 471 486 Sukoff MH Ragatz RE Hyperbaric Oxygenation for the Treatment of Acute Cerebral Edema Neurosurgery 1982 10 29 38 Kohshi K Yokota A Konda N Kinoshita Y Kajiwara H Intracranial Pressure Responses During Hyperbaric Oxygen Therapy Neurol Med Chir Tokyo 1991 31 575 581 Rockswold SB Rockswold GL Zaun DA Zhang X Cerra CE Bergman TA et al A Prospective Randomized Clinical Trial to Compare the Effect of Hyperbaric to Normobaric Hyperoxia on Cerebral Metabolism Intracranial Pressure and Oxygen Toxicity in Severe Traumatic Brain Injury J Neurosurg 2010 112 1080 1094 Edwards ML Hyperbaric Oxygen Therapy Part 2 Application in Disease J Vet Emerg Crit Care San Antonio 2010 20 289 297 Mandal NG White N Wee MY Carbon Monoxide Poisoning in a Parturient and the Use of Hyperbaric Oxygen for Treatment Int J Obstet Anesth 2001 10 71 74 Rockswold GL Ford SE Anderson DC Bergman TA Sherman RE Results of a Prospective Randomized Trial for Treatment of Severely Brain Injured Patients with Hyperbaric Oxygen J Neurosurg 1992 76 929 934 Dunn JE Lawson DD Effects of Hypobaric and Hyperbaric Oxygen on Experimental Brain Injury In Origins of Hyperbaric Medicine Edited by Brown IW Cox BGs Washington DC National Research Council 1966 447 454 Miller JD Fitch W Ledingham IM Jennett WB The Effect of Hyperbaric Oxygen on Experimentally Increased Intracranial Pressure J Neurosurg 1970 33 287 296 Hollin SA Sukoff MH Jacobson JH The Protective Effect of Hyperbaric Oxygenation in Experimentally Produced Cerebral Edema and Compression Prog Brain Res 1968 30 479 489 Sukoff MH Hollin SA Espinosa OE Jacobson JH The Protective Effect of Hyperbaric Oxygenation in Experimental Cerebral Edema J Neurosurg 1968 29 236 241 Moody RA Mead CO Ruamsuke S Mullan S Therapeutic Value of Oxygen at Normal and Hyperbaric Pressure in Experimental Head Injury J Neurosurg 1970 32 51 54 Hayakawa T Kanai N Kuroda R Yamada R Mogami H Response of Cereborspinal Fluid Pressure to Hyperbaric Oxygenation J Neurol Neurosurg Psychiatry 1971 34 580 586 Mink RB Dutka AJ Hyperbaric Oxygen after Global Cerebral Ischemia in Rabbits Does Not Promote Brain Lipid Peroxidation Crit Care Med 1995 23 1398 1404 Harch PG Kriedt GL Weisand MP Van Meter KW Sutherland RJ Low Pressure Hyperbaric Oxygen Therapy Induces Cerebrovascular Changes and Improves Complex Learning Memory in a Rat Open Head Bonk Chronic Brain Contusion Model Undersea Hyperb Med 1996 23 Harch PG Kriedt C Van Meter KW Sutherland RJ Hyperbaric Oxygen Therapy Improves Spatial Learning and Memory in a Rat Model of Chronic Traumatic Brain Injury Brain Res 2007 1174 120 129 Wang GH Zhang XG Jiang ZL Li X Peng LL Li YC et al Neuroprotective Effects of Hyperbaric Oxygen Treatment on Traumatic Brain Injury in the Rat J Neurotrauma 2010 27 1733 1743 Marx RE Ehler WJ Tayapongsak P Pierce LW Relationship of Oxygen Dose to Angiogenesis Induction in Irradiated Tissue Am J Surg 1990 160 519 524 Myers RA Marx RE Use of Hyperbaric Oxygen in Postradiation Head and Neck Surgery NCI Monogr 1990 151 157 Golden ZL Neubauer R Golden CJ Greene L Marsh J Mleko A Improvement in Cerebral Metabolism in Chronic Brain Injury after Hyperbaric Oxygen Therapy Int J Neurosci 2002 112 119 131 Neubauer RA Gottlieb SF Miale A Jr Identification of Hypometabolic Areas in the Brain Using Brain Imaging and Hyperbaric Oxygen Clin Nucl Med 1992 17 477 481 Giza CC Hovda DA The Neurometabolic Cascade of Concussion J Athl Train 2001 36 228 235 Bennett MH Trytko B Jonker B Hyperbaric Oxygen Therapy for the Adjunctive Treatment of Traumatic Brain Injury Cochrane Database Syst Rev 2004 CD004609 Kumaria A Tolias CM Normobaric Hyperoxia Therapy for Traumatic Brain Injury and Stroke A Review Br J Neurosurg 2009 23 576 584 Page 7 of 7 35 Narotam PK Morrison JF Nathoo N Brain Tissue Oxygen Monitoring in Traumatic Brain Injury and Major Trauma Outcome Analysis of a Brain Tissue Oxygen Directed Therapy J Neurosurg 2009 111 672 682 36 Nortje J Coles JP Timofeev I Fryer TD Aigbirhio FI Smielewski P et al Effect of Hyperoxia on Regional Oxygenation and Metabolism after Severe Traumatic Brain Injury Preliminary Findings Crit Care Med 2008 36 273 281 37 Rockswold SB Rockswold GL Defillo A Hyperbaric Oxygen in Traumatic Brain Injury Neurol Res 2007 29 162 172 38 Contreras FL Kadekaro M Eisenberg HM The Effect of Hyperbaric Oxygen on Glucose Utilization in a Freeze Traumatized Rat Brain J Neurosurg 1988 68 137 141 39 Azbill RD Mu X Bruce Keller AJ Mattson MP Springer JE Impaired Mitochondrial Function Oxidative Stress and Altered Antioxidant Enzyme Activities Following Traumatic Spinal Cord Injury Brain Res 1997 765 283 290 40 Springer JE Azbill RD Carlson SL A Rapid and Sensitive Assay for Measuring Mitochondrial Metabolic Activity in Isolated Neural Tissue Brain Res Brain Res Protoc 1998 2 259 263 41 Vlodavsky E Palzur E Feinsod M Soustiel JF Evaluation of the ApoptosisRelated Proteins of the Bcl 2 Family in the Traumatic Penumbra Area of the Rat Model of Cerebral Contusion Treated by Hyperbaric Oxygen Therapy A Quantitative Immunohistochemical Study Acta Neuropathol 2005 110 120 126 42 Vlodavsky E Palzur E Soustiel JF Hyperbaric Oxygen Therapy Reduces Neuroinflammation and Expression of Matrix Metalloproteinase 9 in the Rat Model of Traumatic Brain Injury Neuropathol Appl Neurobiol 2006 32 40 50 43 Palzur E Vlodavsky E Mulla H Arieli R Feinsod M Soustiel JF Hyperbaric Oxygen Therapy for Reduction of Secondary Brain Damage in Head Injury An Animal Model of Brain Contusion J Neurotrauma 2004 21 41 48 44 Korsmeyer SJ Shutter JR Veis DJ Merry DE Oltvai ZN Bcl 2 Bax A Rheostat That Regulates an Anti Oxidant Pathway and Cell Death Semin Cancer Biol 1993 4 327 332 45 Sharpe JC Arnoult D Youle RJ Control of Mitochondrial Permeability by Bcl 2 Family Members Biochim Biophys Acta 2004 1644 107 113 46 Shimizu S Narita M Tsujimoto Y Bcl 2 Family Proteins Regulate the Release of Apoptogenic Cytochrome C by the Mitochondrial Channel Vdac Nature 1999 399 483 487 47 Calvert JW Zhou C Nanda A Zhang JH Effect of Hyperbaric Oxygen on Apoptosis in Neonatal Hypoxia Ischemia Rat Model J Appl Physiol 2003 95 2072 2080 48 Yin D Zhou C Kusaka I Calvert JW Parent AD Nanda A et al Inhibition of Apoptosis by Hyperbaric Oxygen in a Rat Focal Cerebral Ischemic Model J Cereb Blood Flow Metab 2003 23 855 864 49 Cuzner ML Opdenakker G Plasminogen Activators and Matrix Metalloproteases Mediators of Extracellular Proteolysis in Inflammatory Demyelination of the Central Nervous System J Neuroimmunol 1999 94 1 14 50 Wennersten A Holmin S Mathiesen T Characterization of Bax and Bcl 2 in Apoptosis after Experimental Traumatic Brain Injury in the Rat Acta Neuropathol 2003 105 281 288 51 Hu SL Hu R Li F Liu Z Xia YZ Cui GY et al Hyperbaric Oxygen Preconditioning Protects against Traumatic Brain Injury at High Altitude Acta Neurochir Suppl 2008 105 191 196 doi 10 1186 2045 9912 1 21 Cite this article as Huang and Obenaus Hyperbaric oxygen therapy for traumatic brain injury Medical Gas Research 2011 1 21
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU A clinical practice guideline for the use of hyperbaric oxygen therapy in the treatment of diabetic foot ulcers CPG Authors Enoch T Huang Jaleh Mansouri M Hassan Murad Warren S Joseph Michael B Strauss William Tettelbach Eugene R Worth UHMS CPG Oversight Committee Enoch T Huang John Feldmeier Ken LeDez Phi Nga Jeannie Le Jaleh Mansouri Richard Moon M Hassan Murad CORRESPONDING AUTHOR Dr Enoch T Huang enoch huang mac com ______________________________________________________________________________________________________________________________________________________ ABSTRACT Background The role of hyperbaric oxygen HBO2 for the treatment of diabetic foot ulcers DFUs has been examined in the medical literature for decades There are more systematic reviews of the HBO2 DFU literature than there have been randomized controlled trials RCTs but none of these reviews has resulted in a clinical practice guideline CPG that clinicians patients and policy makers can use to guide decision making in everyday practice Methods The Undersea and Hyperbaric Medical Society UHMS following the methodology of the Grading of Recommendations Assessment Development and Evaluation GRADE Working Group undertook this systematic review of the HBO2 literature in order to rate the quality of evidence and generate practice recommendations for the treatment of DFUs We selected four clinical questions for review regarding the role of HBO2 in the treatment of DFUs and analyzed the literature using patient populations based on Wagner wound classification and age of the wound i e acute post operative wound vs non healing wound of 30 or more days Major amputation and incomplete healing were selected as critical outcomes of interest Results This analysis showed that HBO2 is beneficial in preventing amputation and promoting complete healing in patients with Wagner Grade 3 or greater DFUs who have just undergone surgical debridement of the foot as well as in patients with Wagner Grade 3 or greater DFUs that have shown no significant improvement after 30 or more days of treatment In patients with Wagner Grade 2 or lower DFUs there was inadequate evidence to justify the use of HBO2 as an adjunctive treatment Conclusions Clinicians patients and policy makers should engage in shared decision making and consider HBO2 as an adjunctive treatment of DFUs that fit the criteria outlined in this guideline The current body of evidence provides a moderate level of evidence supporting the use of HBO2 for DFUs Future research should be directed at improving methods for patient selection testing various treatment protocols and improving our confidence in the existing estimates ______________________________________________________________________________________________________________________________________________________ Executive Summary Recommendations for the use of hyperbaric oxygen therapy in diabetic foot ulcers Recommendation 1 In patients with Wagner Grade 2 or lower diabetic foot ulcers we suggest against using hyperbaric oxygen therapy very low level evidence in support of HBO2 conditional recommendation Recommendation 2 In patients with Wagner Grade 3 or higher diabetic foot ulcers that have not shown significant improvement after 30 days of treatment we suggest adding hyperbaric oxygen therapy to the standard of care to reduce the risk of major amputation and incomplete healing moderate level evidence conditional recommendation Recommendation 3 In patients with Wagner Grade 3 or higher diabetic foot ulcers who have just had a surgical debridement of an infected foot e g partial toe or ray amputation debridement of ulcer with underlying bursa cicatrix or bone foot amputation incision and drainage I D of deep space abscess or necrotizing soft tissue infection we suggest adding acute post operative hyperbaric oxygen therapy to the standard of care to reduce the risk of major amputation and incomplete healing moderatelevel evidence conditional recommendation Copyright 2015 Undersea Hyperbaric Medical Society Inc 205
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU Introduction The Centers for Disease Control CDC estimates that approximately 25 8 million people or roughly 8 3 of the U S population are affected by diabetes 1 More than 60 of non traumatic amputations in the United States occur in people with diabetes and a foot ulcer precedes 85 of lower limb amputations in patients with diabetes Contralateral leg amputation follows for 56 of patients within three to five years and the five year mortality rate for diabetic patients who have had a single leg amputation is 60 2 This figure is higher than the overall five year mortality rate of breast cancer 10 bladder cancer 19 colorectal cancer 33 and all cancers combined 32 3 Examination of the literature provides nine randomized controlled trials RCTs 4 12 over 20 observational OBS studies 13 36 and nearly a dozen review articles 37 48 These studies are hampered by small sample sizes inconsistent treatment protocols and less than rigorous methodology leading to continuous debate about the role of hyperbaric oxygen HBO2 for the treatment of DFUs What is not debated is that HBO2 should be considered an adjunctive treatment and cannot take the place of surgical removal of devitalized tissue and high quality wound management The use of comprehensive foot care programs that included early screening and evaluation of problems foot care education preventive therapy and referral to specialists has been shown to reduce amputation rates by 49 85 49 After reviewing the literature it is obvious that standard wound care is highly variable The International Working Group on the Diabetic Foot IWGDF guidelines for the best practice treatment of DFUs includes four tenets treatment of underlying infection revascularization if appropriate and feasible offloading to minimize trauma to the ulcer site and management of the wound bed to promote healing 46 Failure to address these tenets obviates any discussion about the utility of HBO2 for DFUs One difficulty in analyzing the existing body of literature lies in the heterogeneity of the patient populations being studied the interventions being used and the outcomes being compared Wound classification is not standardized comorbidities are not screened consistently and subgroups of patient acuity are not con 206 sistently reported Modern use of the Wagner classification system Table 1 grades wounds on observations such as deformity depth infection gangrene and location 51 The University of Texas classification system Table 1 combines the presence or absence of infection plus perfusion in a vertical scale and the depth of the wound on a horizontal scale to generate a 16 choice matrix 52 The Infectious Disease Society of America IDSA bases its classification system Table 1 on the severity of diabetic foot infections and has shown an increased trend for more frequent and higher levels of amputation with the seriousness of infection 53 It is difficult to find a single classification system that addresses all of the relevant comorbidities contributing to the pathology of a diabetic foot ulcer but the IWGDF attempted to do this by developing a classification system Table 1 for research purposes based on five key categories perfusion extent size depth tissue loss infection and sensation PEDIS 54 55 Strauss described a similar system Table 1 but adds an assessment of the wound base using a 0 to 10 scoring system to make logical decisions between limb salvage or major amputation 56 A recent guideline by the Society for Vascular Surgery Table 1 published similar risk stratification based on three major factors that impact amputation risk and clinical management wound ischemia and foot infection WIfI to generate a matrix of 32 permutations of wound categories that generally have worse outcomes as one moves down and to the right 57 Despite consensus between foot and ankle surgeons and hyperbaric physicians that the Wagner grade is archaic and inadequate most of the historical and contemporary studies and most reimbursement determinations with regard to the use of HBO2 for DFUs are based on the Wagner DFU wound appearances Methods The Institute of Medicine published eight standards for the development of reliable Clinical Practice Guidelines 58 These standards include conducting a systematic review appropriate management of existing conflicts of interest transparent guideline development process and clearly articulated recommendations derived and E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU _____________________________________________________________________________________________________________________________________________________________ Table 1 Features of wound grading systems GRADING GRADE TIER GRADING SYSTEM CLASSIFICATION _____________________________________________________________________________________________________________________________________________________________ Classic Wagner 6 grades based Grade 0 no open lesion may have healed lesions Grading System on anatomy and Grade 1 superficial ulcer without penetration to deeper layers presence of Grade 2 deeper ulcer reaching tendon bone or joint capsule infection Grade 3 deeper tissues are involved and there is abscess osteomyelitis or tendonitis Grade 4 there is gangrene of some part of the toe toes and or forefoot Grade 5 gangrene involves the whole foot or enough of the foot that no local procedures are possible and BKA is indicated _____________________________________________________________________________________________________________________________________________________________ University of Texas Health Science Center at San Antonio 4 stages based on absence or presence of ischemia and infection Stage A Stage B Stage C Stage D no infection infection ischemia infection and ischemia Grade 0 Grade 1 Grade 2 Grade 3 epithelialized wound superficial wound wound penetrating tendon or capsule wound penetrating bone or joint ___________________________________________________________________________________________________________________________________ 4 grades based on extent and depth of wound _____________________________________________________________________________________________________________________________________________________________ IDSA Infectious 4 grades Grade 1 infection with at least two of following criteria localized swelling erythema pain Disease Society 4 IDSA levels of warmth purulent discharge PEDIS 1 IDSA infection severity uninfected of America based on severity Grade 2 local infection involving only skin and subcutaneous tissue with erythema of severity of 0 5 cm and 2 cm around ulcer PEDIS 2 IDSA infection severity mild infection Grade 3 local infection with erythema 2 cm or involving structures deeper to skin and subcutaneous tissue with no signs of systemic inflammation PEDIS 3 IDSA infection severity moderate Grade 4 local infection with systemic inflammation response signs SIRS with two or more of the following criteria temp 38 degrees or 36 degrees heart rate 90 beats min respiratory rate 20 breaths min or PaCO2 32 mm Hg white blood count WBC 12 000 or 4000 cells microliter or 10 immature band forms PEDIS 4 IDSA infection severity severe _____________________________________________________________________________________________________________________________________________________________ continued rated in a standardized fashion The review and the guideline should be developed by a multidisciplinary group of content and methodological experts Guideline Development Group followed by external assessment of recommendations and frequent regular updates The Undersea and Hyperbaric Medical Society has sought to adhere to these standards by using the following protocol Oversight Committee The Oversight Committee consists of a representative from the UHMS Board of Directors the UHMS Oxygen Therapy Committee the UHMS Quality Utilization Authorization and Reimbursement Committee the UHMS Publications Committee the UHMS International Membership and a member of the GRADE Working Group The Oversight Committee is tasked E T Huang J Mansouri M H Murad et al with the development of a series of clinical practice guidelines CPGs for the appropriate use of HBO2 The Oversight Committee invites potential members of the CPG review committee based on individual areas of expertise which may or may not include HBO2 The Oversight Committee reviews curriculum vitae of potential members and evaluates each candidate for potential conflicts of interest using responses to a questionnaire detailing the potential reviewers financial interests involving the HBO2 indication in question Any reviewer who is deemed to have an unacceptable conflict of interest is not included on the review committee In addition the Oversight Committee also serves in the internal review process of manuscripts for publication resulting from the systematic reviews 207
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU _____________________________________________________________________________________________________________________________________________________________ Table 1 Features of wound grading systems continued from previous page GRADING GRADE TIER GRADING SYSTEM CLASSIFICATION _____________________________________________________________________________________________________________________________________________________________ International Five categories Perfusion Working scored based Grade 1 no signs symptoms of PAD Group on the on different Grade 2 symptoms or signs of PAD but not of critical limb ischemia CLI Diabetic Foot criteria Grade 3 critical limb ischemia as defined by systolic ankle blood pressure 38 C or 90 beats minute respiratory rate 20 breaths minute PaCO2 12 000 or25 V using semi quantitative techniques both tested on the hallux _____________________________________________________________________________________________________________________________________________________________ continued Review Committee CPG review committee members were oriented to the review process and GRADE methodology using slide presentations reading lists and webcasts Review committee members were then asked to participate in the multistep process outlined below GRADE methodology The Grading of Recommendations Assessment Development and Evaluation GRADE framework is based on the clear separation between quality of evidence and 208 strength of recommendations an explicit evaluation of the importance of outcomes or alternative management strategies explicit and comprehensive criteria for downgrading and upgrading the quality of evidence rating a transparent system of moving from evidence to recommendations explicit acknowledgment of values and preferences of patients and clear pragmatic interpretation of strong versus conditional recommendations for clinicians patients and policy makers Table 2 59 73 This methodology has been adopted E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU _____________________________________________________________________________________________________________________________________________________________ Table 1 Features of wound grading systems continued from previous page GRADING GRADE TIER GRADING SYSTEM CLASSIFICATION _____________________________________________________________________________________________________________________________________________________________ Strauss Wound Score Five assessments each graded 0 2 points half points used for mixed or intermediate findings Appearance wound base 2 points for red 1 point for white biofilm fibrous membrane yellow exudate 0 points for black necrotic wet gangrene or fluctuant eschar __________________________________________________________________________________________________________________________________________ Healthy wound 7 5 10 points Problem wound 3 5 7 points Futile wound 0 3 points Size 2 points for less than the surface area of patient s thumbprint 1 point for thumbprint to fist size 0 points for larger than fist size ________________________________________________________________________________________________________________ Depth including maximum depth of probe 2 points for skin coverage and 1 5 points for subcutaneous tissue 1 point for muscle and or tendon 0 points for bone and or joint ________________________________________________________________________________________________________________ Bioburden 2 points for colonized 1 point for cellulitis maceration and or deep infection bone joint bursa or cicatrix 0 points for septic unstable blood sugars leukocytosis positive blood cultures fever chills ________________________________________________________________________________________________________________ Perfusion use secondary findings of color temperature capillary refill if exam obscured by edema scar hidebound skin and or previous surgery 2 points for palpable pulses 1 point for biphasic or triphasic dopplerable pulses cool pale or dusky capillary refill 2 5 secs 0 points for monophasic or imperceptible pulses cold black cyanotic purplish capillary refill 5 secs _____________________________________________________________________________________________________________________________________________________________ Society for 4 grades for each Wound Vascular of three criteria of Grade 0 no ulcer or gangrene Surgery wound ischemia Grade 1 shallow ulcer no gangrene Wound and foot infection Grade 2 deeper ulcer with exposed joint or tendon gangrene limited to digits Ischemia WIfI Grade 3 deep ulcer involving forefoot midfoot heel extensive gangrene involving forefoot Foot midfoot or heel Infection _____________________________________________________________________________________________________________________ WIfI System Ischemia Grade 0 ABI 0 80 arterial systemic pressure 100 mm Hg and or TcPO2 60 mm Hg Grade 1 ABI 0 6 0 79 arterial systemic pressure 70 100 mm Hg and or TcPO2 40 59 mm Hg Grade 2 ABI 0 4 0 59 arterial systemic pressure 50 70 mm Hg and or TcPO2 30 39 mm Hg Grade 3 ABI 0 39 arterial systemic pressure 50 70 mm Hg and or TcPO2 0 5 cm and 2 cm with pain warmth purulent discharge mild local infection with 2 cm erythema involves deeper structures moderate local infection with signs of SIRS refer to IDSA definition severe _____________________________________________________________________________________________________________________________________________________________ by over 70 organizations including the Cochrane Collaboration the World Health Organization WHO the Centers for Disease Control CDC and the Agency for Healthcare Research and Quality AHRQ Formulation of questions and selection of outcomes The first task of the Review Committee is to create a list of clinically relevant questions to be answered in E T Huang J Mansouri M H Murad et al the guideline These questions are created using the Patient Intervention Comparison and Outcomes PICO format This allows for the creation of a clearly defined patient population an intervention to be compared with an alternative treatment and a set of clinical outcomes rated on a nine point scale defining that outcome as critical important or not important 209
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________ ____________________________________________________________________________ Table 2 Steps of the GRADE review methodology Table 3 Outcomes of interest n Formulate question PICO format n Select outcomes of importance n Rate importance of outcomes 1 9 n Literature review create evidence profile of outcomes across studies summary of findings and estimate of effect for each outcome n Rate quality of evidence for each outcome using criteria in Table 3 rate overall quality of evidence across outcomes based on the lowest quality of critical outcomes n Formulate recommendations for or against strong or conditional taking into account quality of evidence balance of harms vs benefits and the values and preferences of patients and clinicians recommendations may also take into account resource use cost ____________________________________________________________________________ The term standard wound care is meant to represent the optimal management of surgical debridement mechanical offloading infection control revascularization and metabolic control Pre HBO2 treatment of Wagner Grade 3 and 4 DFUs is assumed to include surgical excision of all devitalized tissues These four questions were formulated by the Review Committee 1 For a patient with a diabetic foot ulcer is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest 2 For a patient with a Wagner Grade 2 or lower DFU that has not shown significant improvement after 30 days of treatment is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest 3 For a patient with a Wagner Grade 3 or higher DFU that has not shown significant improvement after 30 days of treatment is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest 4 For a patient with a Wagner Grade 3 or higher DFU who has just had a surgical debridement of the foot e g partial toe or ray amputation debridement of ulcer with underlying bursa cicatrix or bone foot amputation I D of deep space abscess or necro tizing soft tissue infection is acute postoperative HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest 210 n Critical outcomes major amputation incomplete healing at one year n Important outcomes resolution of infection quality of life SF36 minor amputation ____________________________________________________________________________ Outcomes of interest The outcomes of interest selected by the Review Committee are listed in Table 3 Each member of the Review Committee rated outcomes for clinical importance using a nine point scale A consensus on critical outcomes was then obtained via group discussions Search strategy We identified published systematic reviews of HBO2 for DFU 37 47 and cross referenced them to identify RCTs and OBSs of interest Table 4 Observational studies OBSs included any non randomized comparative studies using either historical or contemporary control groups We decided to include OBSs because the number of available RCTs was small and was unlikely to answer all our questions about the various types of patients included in the scope of this guideline We then performed a subsequent librarian assisted search of the Medline Embase and Cochrane databases to identify if there were any RCTs that were not included in the published systematic reviews Search dates included articles published up through April 2015 Medical Subject Headings MeSH terms were used The keywords leg ulcers diabetes and hyperbaric oxygenation were used along with their synonyms A detailed search strategy is included in Appendix A Trial selection Titles and abstracts from the search results were independently reviewed by two panelists E H and E W to select potentially relevant articles The inclusion criteria were RCTs comparing patients with diabetic foot ulcers with a control group We eliminated studies if they did not include the populations as defined by the PICO questions if they did not include the outcomes of interest or if they did not include a comparison group E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU _____________________________________________________________________________________________________________________________________________________________________ Table 4 Systematic reviews of HBO2 as adjunctive treatment for DFU Systematic Databases used RCT Non review RCT Systematic Databases used RCT Non review RCT Wunderlich Medline Doctor et al Faglia 2000 Baroni Oriani Wattel Zamboni Game et al 2012 Wang Medline Doctor 2003 Faglia Baroni Faglia Oriani Wattel Zamboni ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ Roeckl Medline Embase Wiedmann Cochrane Library et al DORCTHIM 2005 Abidia none Doctor Faglia Kessler Lin ___________________________________________________________________________ Goldman Ovid Medline Abidia 2009 Doctor Faglia Kessler Baroni Faglia Fife Kalani Oriani Zamboni ___________________________________________________________________________ Kranke et al Central Ebsco 2012 Ovid Medline Ovid Embase CINAHL Abidia none Doctor Duzgun Faglia Kessler Lin L ndahl ___________________________________________________________________________ Bishop and PubMed Abidia Mudge CINAHL Duzgun 2012 Faglia Kessler L ndahl Baroni Cianci Faglia Fife Kalani Lyon Ong Oriani Oubre Zamboni Zgonis ___________________________________________________________________________ Medline Embase Duzgun L ndahl Chen Abidia Doctor Duzgun Faglia Kessler L ndahl Baroni Kalani Oriani Zamboni L ndahl Not given Abidia 2013 Doctor Duzgun Faglia Kessler L ndahl Baroni Chen Kalani Kaya Lyon Margolis Oriani Wattel Zamboni Murad Medline 2013 Embase Cochrane Library Scopus Abidia Doctor Duzgun Faglia Kessler L ndahl none O Reilly et al 2014 Medline Embase CINAHL PubMed Biosis Cochrane Library Abidia Doctor Duzgun Faglia Kessler L ndahl Baroni Faglia Kalani Lyon Oriani Zamboni Stoekenbroeck Medline et al 2014 Embase Cochrane Library Abidia Doctor Duzgun Faglia Kessler L ndahl Ma none ___________________________________________________________________________ Liu et al Medline 2013 Embase Cochrane Library ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ Data extraction Two panelists E H and E W independently extracted the data using predetermined criteria and presented the summary of evidence to the remainder of the panel to reach consensus We attempted to contact authors of studies to obtain original trial data if we could not identify clear patient groups but we did not receive any replies to our inquiries E T Huang J Mansouri M H Murad et al Statistical techniques Meta analysis of relevant RCTs and observational studies was carried out using the Revman software package Review Manager version 5 2 A description of statistical terms is provided in Table 5 We pooled outcome data using the number of events and sample size of the control and experimental groups reported in published manuscripts The results were depicted in a forest plot showing the individual effect sizes as well as the weighted pooled summary effect size with con 211
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________________________________________________________________________________________ TABLE 5 Summary of statistical techniques in forest plots 1 Statistical Definition Purpose parameter technique Application in GRADE methodology ___________________________________________________________________________________________________________________________________________________________ Forest plot A graphical representation of the individual results of each study included in a meta analysis together with the combined meta analysis result Used to evaluate for GRADE criteria including imprecision inconsistency and large effect size Odds ratio The ratio of the odds of an event in one group to the odds Used for dichotomous data of an event in another group In studies of treatment effect the odds in the treatment group are usually divided by the odds in the control group An odds ratio of one indicates no difference between comparison groups For undesirable outcomes an OR that is less than one indicates that the intervention was effective in reducing the risk of that outcome When the risk is small odds ratios are very similar to risk ratios Risk ratio The ratio of risks in two groups In intervention studies it is the ratio of the risk in the intervention group to the risk in the control group A risk ratio of one indicates no difference between comparison groups For undesirable outcomes a risk ratio that is less than one indicates that the intervention was effective in reducing the risk of that outcome Used for dichotomous data Confidence intervals A measure of the uncertainty around the main finding of a statistical analysis Estimates of unknown quantities such as the odds ratio comparing an experimental intervention with a control are usually presented as a point estimate and a 95 confidence interval This means that if someone were to keep repeating a study in other samples from the same population 95 of the confidence intervals from those studies would contain the true value of the unknown quantity Wide confidence intervals suggest imprecision non overlapping confidence intervals suggest inconsistency heterogeneity Tests of heterogeneity I 2 A measure used to quantify heterogeneity It describes the percentage of the variability in effect estimates that is due to heterogeneity rather than sampling error chance A value greater than 50 may be considered to represent substantial heterogeneity I statistic used to determine level of inconsistency across studies i e degree of heterogeneity Random effects model A statistical model in which both within study sampling error variance and between studies variation are included in the assessment of the uncertainty confidence interval of the results of a meta analysis Used in meta analysis when there is variation in effect size Fixed effects model A model that calculates a pooled effect estimate using the assumption that all observed variation between studies is caused by the play of chance Used in meta analysis when there is similarity in effect size ___________________________________________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________________________________________ 2 ___________________________________________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________________________________________ ___________________________________________________________________________________________________________________________________________________________ Peto method A way of combining odds ratios that has become widely odds ratio used in meta analysis It is a fixed effects model analysis Peto odds ratio effect size used in meta analysis with experimental or control groups with low or zero number of events ___________________________________________________________________________________________________________________________________________________________ 1 Definitions of statistical terms provided are taken from the Glossary of Terms in the Cochrane Collaboration Version 4 2 5 Cochrane Collaboration 2006 https www cochrane org sites default files uploads glossary pdf 212 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________ ___________________________________________________________________________ Table 6 Factors that affect the rating of the quality of evidence Table 7 Levels of evidence n Rate Down risk of bias lack of blinding stopping early for benefit no allocation concealment patients lost to follow up no intention to treat analysis inconsistency indirectness imprecision publication bias n Rate Up large magnitude of effect evidence of dose response effect all plausible confounders would increase confidence in the magnitude of effect ___________________________________________________________________________ fidence intervals We calculated the I2 as a measure of heterogeneity The I2 statistic represents the proportion of variability that is attributable to heterogeneity rather than chance or random error The higher the I2 statistic is the greater the degree of heterogeneity When heterogeneity was judged to be substantial we rated down the quality of evidence There is no specific I2 cutoff point above which the evidence is rated down for heterogeneity An arbitrary cutoff of 50 is often used but this is paired with a judgment of whether the majority of studies support a specific action and whether the observed heterogeneity is clinically meaningful i e a very high I2 may not be important if the difference in effect size is not clinically important across studies We presented results using risk ratios i e relative risk for binary outcomes and mean differences for continuous outcomes Peto odds ratio was used when events were rare small or zero events Considering the heterogeneity of available studies we decided a priori to use the random effects model for metaanalysis The random effects model takes into account the variation in effect size between studies In cases where there was only one study to analyze we calculated a simple odds ratio and confidence interval Rate quality of evidence for each outcome The committee constructed summary of evidence tables and assessed the risk of bias of the studies Whenever possible we used intention to treat analysis even if the original manuscripts did not report it in this man E T Huang J Mansouri M H Murad et al High Further research is very unlikely to change our confidence in the estimate of effect Moderate Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate of effect Low Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate of effect Very low Any estimate of effect is very uncertain ___________________________________________________________________________ ner by using a worst case scenario assuming healing in the control group and failure to heal in the study group This data matrix allowed reviewers to extract evidence profiles for each of the five outcomes from the entire body of literature Randomized controlled trials and observational studies were both analyzed and the body of literature RCT vs OBS with the highest level of evidence was used for decision making If there was equivalent level of evidence and the magnitude of effect was similar the RCT and OBS studies were analyzed together If there was equivalent level of evidence but the magnitude of effect was dissimilar only the RCT studies were used The committee applied the relevant factors outlined in the GRADE methodology to rate the quality of evidence up more reliable or down less reliable Table 6 and assigned a final rating for each outcome for each PICO question In many analyses the effect size was large or very large i e two to five times reduction in relative effect We opted to rate up only one level as opposed to two for very large effect It is also reasonable to not rate up in the presence of factors that lead to rating down This decision is explicit in the tables that describe our judgments and process This semi quantitative score corresponds to an overall quality of evidence rating using the four tiered GRADE quality levels very low low moderate and high Table 7 Formulating recommendations A final rating of the quality of evidence across all outcomes was given based on the critical outcome with the lowest level of evidence The Review Committee then formulated recommendations for each PICO question This step required assigning a level of strength 213
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________ Table 8 Strength of recommendations and implications for the general population healthcare workers and policy makers Strong Population Most people in this situation would want the recommended course of action and only a small proportion would not Healthcare workers Most people should receive the recommended course of action Policy makers The recommendation can be adapted as a policy in most situations Conditional Population The majority of people in this situation would want the recommended course of action but many would not Healthcare workers Be prepared to help people to make a decision that is consistent with their own values decision aids and shared decision making Policy makers There is a need for substantial debate and involvement of stakeholders ___________________________________________________________________________ for each recommendation using the two tiered GRADE levels conditional or strong see Table 8 The final recommendations were agreed upon by consensus External review The UHMS Oversight Committee reviewed the document before undergoing additional review by content experts Content experts included specialists who treat DFUs but who do not provide HBO2 Once the review committee addressed any concerns the document was posted for public comment After the review committee addressed any public comments the manuscript was submitted for publication All public comments and committee responses are posted on the UHMS website www uhms org cpg Patient engagement Two groups of patients with DFU were invited to participate in the formulation of this guideline Both patients who had received HBO2 and patients who 214 had not received HBO2 were included The first group was recruited from a wound and hyperbaric medicine clinic to answer an online survey rating the outcomes selected by the Review Committee using a nine point scale This was an IRB approved approach The second group was recruited from a wound and hyperbaric medicine clinic to attend a face to face meeting with members of the Review Committee using video conferencing technology The CPG development process and recommendations were presented to the patients The Review Committee solicited patient perspective on multiple issues ranging from their fears and concerns at their initial consultation to their view of the successes and failures of their treatment course The values opinions and perspectives of these patients are reported below Results Patient survey results An IRB approved survey was offered to all diabetic patients of one of the authors hospital system Six patients completed the online survey No patients had any financial relationship with a hyperbaric chamber manufacturer or hyperbaric operations Three patients had a DFU and three did not By chance all three patients with a DFU had received HBO2 or were scheduled to receive HBO2 One patient had an incomplete course of HBO2 based on a clinical decision regarding the wound progress No patients had any portion of their foot amputated When rating the outcomes of interest for importance three of the three patients who answered this question rated all of the outcomes nine of nine of critical importance Evidence review The review committee used published systematic reviews to identify nine randomized controlled trials and 21 observational studies for initial review The subsequent formal review included 655 references but did not identify any additional RCTs that were not previously identified from the systematic reviews Studies were eliminated from consideration if they did not report data on the outcomes of interest or did not include patients in the specific study populations Table 9 Five of the RCTs Doctor 1992 Faglia 1996 Abidia 2003 Duzgun 2008 and L ndahl 2010 were included for this analysis Table 10 Of note the Doctor study did not report the number of patients in each E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ______________________________________________________________________________________________________________________________________________________________________ Table 9 Outcomes reported by study _______________________________________________________________________________________________________ outcome reported comments ______________________________________________________________________________________________________________________________________________________________________________ type study major incomplete minor persistent no change in amputation healing 1 yr amputation infection quality of life ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ RANDOMIZED CONTROLLED TRIALS Doctor 1992 included Faglia 1996 included Lin 2001 excluded abstract only without any outcomes of interest ________________________________________________________________________________________________________________________________________________________________________ Abidia 2003 included data on quality of life were not able to be included ________________________________________________________________________________________________________________________________________________________________________ Kessler 2003 excluded reported only for short term outcomes 6 weeks ________________________________________________________________________________________________________________________________________________________________________ Duzgun 2008 included ________________________________________________________________________________________________________________________________________________________________________ L ndahl 2010 included data on quality of life were able to be included ________________________________________________________________________________________________________________________________________________________________________ Kaur 2012 excluded did not include populations of interest and did not include outcomes of interest ________________________________________________________________________________________________________________________________________________________________________ ______________________________________________________________________________________________________________________________________________________________________________ Ma 2013 excluded did not include outcomes of interest ________________________________________________________________________________________________________________________________________________________________________ Hart 1979 Davis 1987 excluded did not include outcomes of interest ________________________________________________________________________________________________________________________________________________________________________ excluded did not include outcomes of interest Baroni 1987 included these studies may have had overlapping patients so the last dataset for 1990 was used Oriani 1990 for analysis ___________________________________________________________________________________________________________________________________________________________ Oriani 1992 excluded did not include non HBO comparison grp Wattel 1991 excluded did not include non HBO comparison grp 2 ________________________________________________________________________________________________________________________________________________________________________ 2 ________________________________________________________________________________________________________________________________________________________________________ Cianci 1994 excluded did not include any outcomes of interest ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ 2 ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ Grollman 2001 excluded did not include any outcomes of interest ________________________________________________________________________________________________________________________________________________________________________ 2 ________________________________________________________________________________________________________________________________________________________________________ 2 ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ Fife 2007 excluded did not include any outcomes of interest ________________________________________________________________________________________________________________________________________________________________________ 2 ________________________________________________________________________________________________________________________________________________________________________ 2 ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ Kaya 2009 excluded did not include non HBO2 comparison grp ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________________ OBSERVATIONAL TRIALS Zamboni 1997 included Faglia 1998 excluded did not include non HBO comparison grp Kalani 2001 included Fife 2002 excluded did not include non HBO comparison grp Strauss 2002 excluded did not include non HBO comparison grp Niinikoski 2003 excluded did not include any outcomes of interest Oubre 2007 excluded did not include non HBO comparison grp Ong 2008 excluded did not include non HBO comparison grp Lyon 2008 excluded did not include any outcomes of interest Chen 2010 excluded did not include any outcomes of interest Margolis 2013 included Tongson 2013 excluded did not include any outcomes of interest _______________________________________________________________________________________________________ Bishop 2013 excluded did not include non HBO2 comparison grp E T Huang J Mansouri M H Murad et al 215
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU _________________________________________________________________________________________________________________________________________________________________ Table 10 Summary of evidence table included randomized controlled trials ________________________________________________________________________________________________________________________________________________________________ Study Treatment groups Results Outcomes HBO2 group vs Standard care group HBO2 protocol Comment ________________________________________________________________________________________________________________________________________________________________ Doctor 15 HBO2 Sub Major Incomplete Minor Persistent No change in Patients were all inpatients 1992 vs 15 SC groups amputation healing All 2 15 vs 7 15 1 11 vs 3 11 _______________________________________________ 3 atm abs x 45 min 4 treatments over 2 weeks ___________ amputation infection quality of life Wagner 2 HBO2 protocol is not a standard treatment protocol ___________ Wagner 3 ___________ Wagner 4 2 15 vs 7 15 4 15 vs 2 15 3 19 vs 12 16 ________________________________________________________________________________________________________________________________________________________________ Faglia 1996 36 HBO2 vs 34 SC Sub groups Major Incomplete amputation healing Minor amputation Persistent No change in infection quality of life ____________________________________________________________________________________________________ 2 2 2 5 atm abs x 90 min 5 7 days week All 3 36 vs 11 34 21 35 vs 12 33 _____________________________ Wagner 2 9 35 vs 16 33 0 4 vs 0 5 _____________________________ Wagner 3 1 4 vs 0 8 _____________________________ Wagner 4 Patients were all inpatients Wagner subgroup analysis did not use intention to treat analysis resulting in discrepancy in the denominator 2 22 vs 11 20 ________________________________________________________________________________________________________________________________________________________________ Abidia 2003 9 HBO2 vs 9 HBAir sham Sub groups Major Incomplete amputation healing Minor amputation 1 9 vs 1 9 4 9 vs 9 9 1 9 vs 0 9 1 9 vs 1 9 4 9 vs 9 9 1 9 vs 0 9 Persistent No change in infection quality of life ________________________________________________________________ 2 4 atm abs daily x 90 min 5 days week vs 30 sham All Double blinded trial with use of sham hyperbaric air treatments ________________________________________________________________ Wagner 2 ________________________________________________________________ Wagner 3 ___________ Wagner 4 ________________________________________________________________________________________________________________________________________________________________ Duzgun 2008 50 HBO2 vs 50 SC Sub groups Major Incomplete amputation healing Minor amputation Persistent No change in infection quality of life ________________________________________________________________ 2 2 2 5 atm abs x 90 min 5 7 days wk 0 50 vs 17 50 19 50 vs 50 50 Wagner 2 All 0 6 vs 0 12 6 6 vs 12 12 4 50 vs 24 50 0 6 vs 4 12 Wagner 3 0 19 vs 0 18 6 19 vs 18 18 1 19 vs 17 18 Wagner 4 0 25 vs 17 20 7 25 vs 20 20 3 12 vs 3 18 L ndahl 2010 Sub groups Major Incomplete amputation healing ________________________________________________________________ Randomized trial of HBO2 or SC but no sham treatments or blinding of investigators ________________________________________________________________ ________________________________________________________________ ________________________________________________________________________________________________________________________________________________________________ 49 HBO2 vs 45 HBAir sham 2 2 2 5 atm abs x 90 min 5 7 days wk Minor amputation Persistent No change in infection quality of life ____________________________________________________________________________________________________ All 3 49 vs 1 44 24 49 vs 33 45 4 49 vs 4 45 ________________________________________________________________ 26 49 vs 35 45 Double blinded trial with use of sham hyperbaric air treatments Wagner 2 ___________ Wagner 3 ___________ Wagner 4 ________________________________________________________________________________________________________________________________________________________________ Whenever possible intention to treat analysis was used if denominator of each group could be extrapolated from the manuscript __________________________________________________________________________________________________ Table 11 Risk of bias table __________________________________________________________________________________________________ Doctor 1992 Faglia 1996 Abidia 2003 Duzgun 2008 L ndahl 2010 __________________________________________________________________________________________________ no stopping early for benefit __________________________________________________________________________________________________ strict allocation concealment __________________________________________________________________________________________________ none lost to follow up __________________________________________________________________________________________________ blinded study __________________________________________________________________________________________________ intention to treat analysis __________________________________________________________________________________________________ risk of bias MOD MOD MOD MOD LOW __________________________________________________________________________________________________ 216 study arm 5 For the purposes of this analysis we assumed an equal distribution in each group The remaining studies were excluded because they did not report data on the preselected outcomes Risk of bias was evaluated for the remaining RCTs using five criteria Table 11 An indeterminate score was assigned if a study did not explicitly state whether it did or did not adhere to one of the criteria E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ______________________________________________________________________________________________________________________________________________________________________ Table 12 Summary of evidence table included observational studies ___________________________________________________________________________________________________________________________________________________________ Outcomes HBO2 group vs Standard group ___________________________________________________________________________________________________________________________________________________________ study treatment groups HBO2 protocol major amputation incomplete healing minor persistent no change in amputation infection quality of life comment ___________________________________________________________________________________________________________________________________________________________ Oriani 1990 2 8 2 5 atm abs 3 62 vs 6 19 x 90 min multiplace Surgical staff performing debridements were blinded to treatment group all patients were admitted for duration of study inpatients only ___________________________________________________________________________________________________________________________________________________________ Zamboni 1997 2 0 atm abs 0 5 vs 0 5 0 5 vs 0 5 x 120 min All wounds 6 months old only 5 patients in each group Kalani 2001 2 5 atm abs 2 17 vs 7 21 4 17 vs 11 21 x 90 min Followed patients out to 3 years all Wagner
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________________________________________________________________________ Figure 1 Forest plots and GRADE analysis for Question 1 For a patient with a diabetic foot ulcer is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control Critical Outcome Incomplete healing at one year Figure 1 All RCTs reported the proportion of ulcers healed at various time points but only three Abidia 2003 Duzgun 2008 and L ndahl 2010 reported healing at one year All studies reported results as the rate of complete 218 healing However the review committee felt that for the sake of consistency the data should be reported as the risk of adverse outcomes i e risk of incomplete healing or wound persistence This analysis did result in differences in the estimate of effect but ultimately had no difference in the overall quality of evidence Supplemental Figures 2 and 3 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU The final rating of the quality of evidence was moderate Again there was a large magnitude of effect present Figure 1 Outcome Minor amputation Supplemental Figure 4 Five RCTs reported data on minor amputation defined as amputation distal to the ankle Doctor 1992 Faglia 1996 Abidia 2003 Duzgun 2008 and L ndahl 2010 Forest plots using both random effects risk ratio and Peto odds ratio were constructed The use of Peto OR resulted in a slightly more significant estimate of effect 0 96 vs 0 72 and narrower confidence intervals Neither the risk ratio nor odds ratio estimate of effect for minor amputation was statistically significant The final quality of evidence for this outcome was very low Outcome Persistent infection Supplemental Figure 5 Two RCTs Doctor 1992 Faglia 1996 addressed the outcome of persistent infection Both of these studies used wound cultures as a surrogate marker for infection instead of the IDSA criteria for clinical infection This feature of these studies resulted in downgrading the quality of evidence for indirectness The final quality of evidence for this outcome was very low Outcome Quality of life Two studies Abidia 2003 L ndahl 2010 addressed the outcome of quality of life but data were not available to conduct a meta analysis Question 2 For a patient with a Wagner Grade 2 diabetic foot ulcer that has not shown significant improvement after 30 days of treatment is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest RESPONSE There were three randomized controlled Faglia 1996 Abidia 2003 and Duzgun 2008 and one observational study Kalani 2001 that were reviewed for this question While it did not specify that it included only patients with Wagner Grade 2 or lower DFUs the Kalani study reported that none of the patients in that E T Huang J Mansouri M H Murad et al study had a deep infection or gangrene Additional studies included patients with Wagner Grade 2 or lower DFUs L ndahl 2010 Margolis 2013 but the data were not reported in such a way that it could be analyzed The quality of evidence of both study designs was equal but the effect sizes were not similar thus they were not combined and only the RCTs were included Supplemental Figures 6 and 7 Critical Outcome Major Amputation Figure 2 Three RCTs Faglia 1996 Abidia 2003 and Duzgun 2008 reported rates of major amputation Two of the studies Faglia 1996 and Duzgun 2008 had zero incidences of major amputation and the remaining study Abidia 2003 had equal number of amputations in each group There was no evidence that HBO2 had any effect on major amputation in this population Results were similar using a risk ratio or Peto odds ratio Supplemental Figure 8 The final GRADE quality of evidence for this outcome was very low Critical Outcome Incomplete healing Figure 2 Only one RCT reported this outcome Duzgun 2008 It may be noted that although the estimate of effect was very large there was a wide confidence interval and no blinding of the study participants leading to concerns about increased risk of bias If this outcome was presented as complete healing instead of the reciprocal incomplete healing the results are the same Supplemental Figure 8 The final GRADE quality of evidence for this outcome was very low Outcome Minor amputation Supplemental Figure 9 One RCT Duzgun 2008 reported the outcome of minor amputation A simple odds ratio was used for analysis The final GRADE quality of evidence for this outcome was low Outcome Persistent infection There were no RCTs or OBS studies that reported this outcome Outcome Quality of life There were no RCTs or OBS studies that reported this outcome 219
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________________________________________________________________________________________ Figure 2 Forest plots and GRADE analysis for Question 2 For a patient with a Wagner Grade 2 diabetic foot ulcer that has not healed in 30 days of treatment is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control Question 3 For a patient with a Wagner Grade 3 or higher diabetic foot ulcer that has not shown significant improvement after 30 days of treatment is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest RESPONSE There was one randomized controlled trial Duzgun 2008 and two observational studies Zamboni 1997 and Kalani 2001 that were reviewed for this question After comparing the quality of evidence data from RCTs were used for the analysis Supplemental Figures 10 12 Critical Outcome Major amputation Figure 3 While additional RCTs L ndahl 2010 and Faglia 1996 included patients with these criteria the data 220 were not reported in such a way that they could be analyzed As a result only one RCT was analyzed This RCT had the largest number of subjects and had zero major amputations in the HBO2 group There is some concern about risk of bias as this single study was unblinded The remaining criteria for risk for bias were low leading to an intermediate risk of bias The final quality of evidence for this outcome was moderate Critical Outcome Incomplete healing Figure 3 The same RCT Duzgun 2008 was also analyzed for the outcome incomplete healing This study showed that no patients in the standard wound care group had complete healing at one year The analysis for wound healing had similar odds ratios when reported as complete healing Supplemental Figures 11 and 12 The final quality of evidence for this outcome was moderate E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________________________________________________________________________________________ Figure 3 GRADE analysis for Question 3 For a patient with a Wagner Grade 3 diabetic foot ulcer that has not healed in 30 days of treatment is HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest Outcome Minor amputation There were no RCTs or OBS studies that reported this outcome Outcome Persistent infection There were no RCTs or OBS studies that reported this outcome Outcome Quality of life There were no RCTs or OBS studies that reported this outcome Question 4 For a patient with a Wagner Grade 3 or higher diabetic foot ulcer who has just had a surgical debridement of the foot e g partial toe or ray amputation debridement of ulcer with underlying bursa cicatrix or bone foot amputation I D of deep space abscess or necrotizing soft tissue infection is acute post operative HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest E T Huang J Mansouri M H Murad et al RESPONSE There were two randomized controlled trials Doctor 1992 and Faglia 1996 and one observational study Oriani 1990 that were reviewed for this question The effect sizes of the two study designs were similar thus they were combined Figure 4 Critical Outcome Major amputation Figure 4 In all three of the studies analyzed patients were treated as inpatients with lengthy hospital stays This in and of itself did not lead to a high level of indirectness as the advantages of extended inpatient care were for enforced offloading glycemic control aggressive surgical debridement and infection control all of which are tenets of optimal wound care All of these studies included HBO2 as part of an aggressive surgical algorithm where patients would be treated with HBO2 soon after surgery as opposed to having a delay of 30 days One of the studies Doctor 1992 however had an atypical treatment protocol using only four 45 minute treatments at 3 atmospheres absolute atm abs in a two week span As a result there may 221
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________________________________________________________________________________________ Figure 4 Forest plot and GRADE analysis for Question 4 For a patient with a Wagner Grade 3 diabetic foot ulcer who has just had a surgical debridement of the foot e g partial toe or foot amputation incision and drainage of deep space abscess progressive necrotizing soft tissue infection is acute post operative HBO2 with standard wound care more effective than standard wound care alone for the outcomes of interest HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control be an element of indirectness as the treatment profile in this study is not the one used in current practice When a meta analysis of a combination of RCTs and OBSs was conducted the effect size was slightly larger lower relative risk favoring HBO2 over standard wound care This effect size was statistically significant and the I2 was 0 indicating homogeneity of the results 222 The final quality of evidence for this outcome was moderate Critical Outcome Incomplete healing There were no RCTs or OBS studies that reported this outcome E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU Outcome Minor amputation Supplemental Figure 13 Only two RCTs Doctor 1992 and Faglia 1996 reported data on minor amputation rate in this patient population It is important to note that there were other studies that included patients with Wagner Grade 3 or higher but these patients were not stratified in the study so subgroup analysis was not possible The outcome of minor amputation was actually more common in the HBO2 group This result is consistent with what is found in clinical practice as patients in this group may often undergo minor amputation instead of major amputation The final quality of evidence for this outcome was low Outcome Persistent infection There were no RCTs or OBS studies that reported this outcome Outcome Quality of life There were no RCTs or OBS studies that reported this outcome From Evidence to Recommendations This guideline starts with the assumption that practitioners have aggressively addressed revascularization of the ischemic foot debrided devitalized tissue managed deformities by offloading the neuropathic foot and utilized anti infective therapies either before or concurrently with adjunctive hyperbaric oxygen therapy We have summarized how each RCT addressed these four tenets in their study protocol Table 13 Previously published clinical practice guidelines have outlined the necessity of these interventions as part of the best practices treatment of diabetic foot ulcers 50 74 77 and readers are referred to these guidelines for further clarification of this issue For patients with diabetic foot ulcers we were able to find moderate level evidence that hyperbaric oxygen therapy reduced major amputations and promoted complete healing We considered studies that included patients with the broadest definition of DFU including Wagner Grade 2 through Wagner Grade 4 ulcers These studies included inpatient and outpatient HBO2 treatment groups which resulted in the increased hetero E T Huang J Mansouri M H Murad et al geneity of both patient populations and interventions With regard to other outcomes of interest there was a very low quality of evidence that HBO2 reduced infection reduced minor amputation or improved quality of life We opted to not provide an overarching recommendation based on Question 1 due to the heterogeneity of included population and attempt to better stratify patients questions 2 4 to develop more implementable recommendations Nevertheless the quality of evidence derived from Question 1 was supportive of subsequent recommendations The Review Committee s next step was to try to standardize patient populations by using variations of the PICO question Experts disagree on the best method of classifying diabetic foot ulcers and infections as there are inherent strengths and weaknesses to these various systems 78 The review committee felt that the Wagner scale was an inadequate tool by which patients should be stratified so we attempted to stratify patients using different clinical grading systems in order to create stronger recommendations Table 14 This attempt to reclassify patients using other systems was impossible based on the limited information reported in the source documents As a result we were left with only the Wagner classification system for review Recent publications have shown that there is an incomplete understanding of the Wagner scale even by experienced hyperbaric practitioners 79 First there is a failure to recognize that a Wagner Grade 3 DFU includes either deep space abscess or tendonitis and not solely osteomyelitis and the hyperbaric oxygen community with CMS endorsement has utilized Wagner s original DFU classification system differently than originally proposed Assigning a Wagner Grade to a foot ulcer is an incomplete utilization of Wagner s classification system as Wagner intended the Grade to be incorporated into a decision making algorithm Aggressive surgical management for the Wagner Grade 3 or greater DFU is recommended by Wagner s algorithm as opposed to conservative medical management Figure 5 We recommend that if one is to use the Wagner classification system one should follow the management algorithms of the Wagner system while supplementing with HBO2 if indicated 51 Current clinical practice among many practitioners is to risk stratify patients using periwound transcutaneous oximetry measurements PtcO2 25 80 Data from multiple studies showed that for patients who had a 223
224 Unknown There was no documentation of revascularization attempts vascular assessment was limited to normal or absence of distal pulses VASCULAR Unknown There was no mention of any standard offloading however all patients were admitted for the duration of their treatment OFFLOADING Good Antibiotics were administered along with metronidazole for 3 days Antibiotics commonly used were cephalosporins and aminoglycosides and were changed according to sensitivity patterns INFECTION Good All patients received regular surgical treatment consisting of incision and drainage of abscesses and debridement of the wound DEBRIDEMENT All patients were admitted so glucose control and offloading were better able to be enforced Antibiotic coverage and debridement were addressed COMMENT Poor We did not distinguish between foot ulcers that were primarily attributable to ischemia vs those attributable to both peripheral ischemia and prolonged pressure that went undetected due to neuropathy Good Study treatment was given as an adjunct to regular treatment at the multidisciplinary diabetes foot clinic which included treatment of infection revascularization debridement offloading and metabolic control according to high international standards Moderate All patients underwent diagnostic angiography as part of their diagnostic assessment Vascular intervention was by clinician choice Vascular surgeons are generally aggressive toward distal revascularization Any patient for whom vascular surgery angioplasty or thrombolysis was planned was excluded Occlusive arterial disease was confirmed by an ankle brachial pressure index 0 8 or great toe brachial index pressure index 0 9 if calf vessels were incompressible Poor We did not distinguish between foot ulcers that were primarily attributable to ischemia vs those attributable to both peripheral ischemia and prolonged pressure that went undetected due to neuropathy Abidia 2003 Duzgun 2008 L ndahl Good All patients were assessed by a vascular surgeon at the time of inclusion and only patients 2010 Excellent On admission to the hospital all patients after collecting a specimen of the ulcer for culture examination were given empirical broad spectrum antibiotic therapy subsequently modified if necessary according to susceptibility testing results The antibiotic therapy was continued during the hospital stay until the culture exam repeated each week was negative After discontinuation of the antibiotic therapy reculturing to assess the cure was performed every two days a total of three times Excellent In all subjects an aggressive and radical debridement was performed by a consultant surgeon After surgical curettage the wound was cleaned with uncolored topical antimicrobial agents and wadded with occlusive dressing Dressing with debridement if necessary was carried out no less than twice a day when necrosis or exudate was present daily when the ulcer was clean and every two days during the granulation period All patients were admitted so glucose control and offloading were better able to be enforced The investigators aggressively managed peripheral arterial disease and addressed all four tenets of DFU care even before the IWGDF came out with its recommendations Moderate Antibiotic therapy was given if there were clinical signs of infection Moderate Wound care was standardised for all patients and included offloading aggressive debridement and dressing which ensured that a moist wound environment was maintained Any patient for whom revascularization was planned was excluded so this patient population represented those who has exhausted their vascular options Standard care was stated to address offloading infection control and aggressive debridement but no specifics were given Moderate ST standard therapy entailed daily wound care including dressing changes and local debridement at bedside or in the operating room as well as amputations when indicated Did not describe vascular status or offloading status of study participants E T Huang J Mansouri M H Murad et al Good Study treatment was given as an adjunct to regular treatment at the multidisciplinary diabetes foot clinic which included treatment of infection revascularization debridement offloading and metabolic control according to high international standards All four tenets of good DFU care were followed although there were not details as to how they were accomplished ___________________________________________________________________________________________________________________________________________________________________________________________________________________________ with adequate distal perfusion or non reconstructable peripheral vascular disease were included in the study Study treatment was given as an adjunct to regular treatment at the multidisciplinary diabetes foot clinic which included treatment of infection revascularization debridement offloading and metabolic control according to high international stds Good Study treatment was given as an adjunct to regular treatment at the multidisciplinary diabetes foot clinic which included treatment of infection revascularization debridement offloading and metabolic control according to high international standards ___________________________________________________________________________________________________________________________________________________________________________________________________________________________ Good Infection controls were carried out by clinical follow up and by performing culture antibiograms of surgically obtained specimens to determine appropriate antibiotic therapy ___________________________________________________________________________________________________________________________________________________________________________________________________________________________ Moderate Wound care was standardised for all patients and included offloading aggressive debridement and dressing which ensured that a moist wound environment was maintained ___________________________________________________________________________________________________________________________________________________________________________________________________________________________ Excellent During hospitalization all patients were provided with orthopedic devices to remove mechanical stress and pressure at the site of the ulcer while maintaining ambulation The orthoesis was made up of an alkaform insole molded in a plastic cast and an extra deep special shoe with a rigid sole Buratto Italy allowing the insertion of a bandaged foot Excellent In the subjects with ABI 0 0 and or TcPO2 5 mm HG a therapy with prostacyclin was established and arteriography by intra arterial digital subtraction technique was performed if there were no contraindications creatinine 221 mol l or paraproteinemia In these subjects the opportunity and possibility of carrying out a percutaneous transluminal angioplasty PTA or a bypass graft BPG was assesses The presence of focal stenosis involving 50 of vessel lumen was considered an indication of PTA The stenosis completely occluding the lumen or with length 10 cm was respectively considered as an impossibility or a contraindication for PTA When there was an impossibility of performing PTA the angiogram was evaluated by vascular surgeons to carry out a BPG Based on angiographic criteria bypasses were performed when a patent vessel in continuity with the foot was present Faglia 1996 ___________________________________________________________________________________________________________________________________________________________________________________________________________________________ Doctor 1992 STUDY Table 13 Four tenets of pre hyperbaric diabetic ulcer foot care ___________________________________________________________________________________________________________________________________________________________________________________________________________________________ UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU group Table 14 RCT subgroups by wound classification systems _________________Population by Grading System_________________ comment ____________________________________________________________________________________________________________________________________________________________________________________________________________________________ study treatment groups HBO2 protocol II 0 unable to unable to unable to unable to unable to III 15 stratify 2 stratify 2 stratify 3 stratify 4 stratify 2 IV 15 II 0 unable to unable to unable to unable to unable to III 15 stratify 2 stratify 2 stratify 3 stratify 4 stratify 2 IV 15 Documentation of infection was solely by positive or negative wound culture so we were unable to use the UT IDSA or WIfI scales Vascular assessment was limited to presence or absence of normal pulses which was inadequate to stratify on the UT IWGDF Strauss or WIFI scales Wagner Univ Texas IWGDF IDSA Strauss WIfI ____________________________________________________________________________________________________________________________________________________________________________________________________________________________ Doctor 15 HBO2 vs 15 SC HBO2 1992 3 atm abs x 45 min 4 treatments over 2 weeks No HBO2 II 4 unable to unable to unable to unable to unable to III 4 stratify 2 stratify 2 stratify 3 stratify 4 stratify 2 IV 22 II 5 unable to unable to unable to unable to unable to III 8 stratify 2 stratify 2 stratify 3 stratify 4 stratify 2 IV 20 Documentation of infection was solely by positive or negative wound culture so we were unable to use the UT IDSA or WIfI scales ABI and TcPO2 were measured but no breakdown within each group was given for the UT IWGDF Strauss or WIfI scales ____________________________________________________________________________________________________________________________________________________________________________________________________________________________ Faglia 36 HBO2 vs 34 SC HBO2 1996 2 2 2 5 atm abs x 90 min 5 7 days wk No HBO2 II 9 unable to unable to unable to unable to unable to stratify 2 stratify 3 stratify 4 stratify 2 III 0 stratify 2 IV 0 II 9 unable to unable to unable to unable to unable to III 0 stratify 2 stratify 2 stratify 3 stratify 4 stratify 2 IV 0 There was no documentation of infection severity in either group so we could not use the UT IDSA Strauss or WIfI scales All patients had ABI
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________ Figure 5 Wagner s Grade 3 DFU algorithm had any regular role in the treatment of DFUs This conclusion mirrors clinical practice for the majority of hyperbaric physicians however a recent retrospective review of a national wound management database showed that over 50 of patients who received HBO2 had a Wagner Grade 2 DFU 22 This is an alarming statistic as it would seem to indicate an unsubstantiated use of HBO2 and highlight the concern that some have had regarding the potential overuse of HBO2 81 The Review Committee did feel that there might be selected clinical situations where patients with a previous DFU of greater severity presenting with a subsequent Wagner Grade 2 DFU may be candidates for HBO2 but this would be the exception rather than the rule RECOMMENDATION 2 Algorithm for Grade 3 foot deep abscess or osteomyelitis Used with permission from Wagner FW Jr The Dysvascular Foot A System for Diagnosis and Treatment Foot and Ankle 2 2 64 122 1981 DFU PtcO2 200 mm Hg under hyperbaric conditions predicted whether the wound would heal with 75 to 80 accuracy when hyperbaric oxygen was used as an adjunct to wound management 19 25 Unfortunately we were not able to find any publications that provided comparative outcome data stratified on this variable and PtcO2 stratification is not included in these CPGs RECOMMENDATION 1 In patients with Wagner Grade 2 or lower diabetic foot ulcers we suggest against using hyperbaric oxygen therapy very low conditional Six of the RCTs included patients with Wagner Grade 2 DFUs but we were able to extract data from only three of these studies for analysis These three studies showed no evidence that HBO2 reduced major amputation or increased complete healing of DFUs in this population The quality of evidence for these studies was very low and we did not feel that adjunctive HBO2 226 In patients with Wagner Grade 3 or higher diabetic foot ulcers that have not healed after 30 days of treatment we suggest adding hyperbaric oxygen therapy to the standard of care with regard to preventing major amputation and promoting complete healing moderate conditional The biggest discrepancy between the classic Wagner scale and the modern utilization of Wagner s grading system is defining which patients meet the Wagner Grade 3 criteria 79 The source of this confusion is unclear but the Wagner Grade 3 cutoff is one that has been utilized in algorithms of hyperbaric physicians because of United States reimbursement guidelines Although four of the RCTs included patients with Wagner Grade 3 or higher DFU we were able to exclude only Wagner Grade 2 or lower DFU from one of these RCTs leading to an analysis of a single RCT for this patient population Based on this analysis we did find moderate quality evidence that HBO2 reduced major amputation rates and increased complete healing We also noted a decrease in the rate of minor amputations although this was not one of the critical outcomes upon which we based this recommendation The potential for overuse of HBO2 is of concern as patients may receive a prolonged course of therapy before ultimately getting an amputation 22 One of the greatest clinical challenges is identifying patients who have confounding factors such as uncontrolled deformities deep infections wound ischemia hypoxia or combinations of these that need to be managed to achieve satisfactory out E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU comes Hyperbaric oxygen is an intervention that addresses wound hypoxia For this reason the wound characteristics with confounding factors must be documented before making decisions about HBO2 RECOMMENDATION 3 In patients with Wagner Grade 3 or higher diabetic foot ulcers who have just had a surgical debridement of the foot e g partial toe or ray amputation debridement of ulcer with underlying bursa cicatrix or bone foot amputation I D of deep space abscess or necrotizing soft tissue infection we suggest adding acute postoperative hyperbaric oxygen therapy to the standard of care with regard to preventing major amputation and promoting complete healing moderate conditional The review of the DFU literature revealed a historical shift in the treatment of DFUs from a primarily surgical inpatient based approach to a less surgical outpatientbased approach Treatment paradigms seemed to follow an arbitrarily mandated delay in initiation of HBO2 based on reimbursement related issues such as insurance coverage While this CPG is intended to avoid reimbursement driven recommendations it is possible that financially motivated practice patterns may have influenced the evidence based practice of hyperbaric medicine Analysis of patients who were treated using the classic Wagner DFU treatment algorithm shows that aggressive surgical intervention revascularization metabolic control infection control and initiation of HBO2 soon after I D debridement or amputation of a limb with Wagner Grade 3 or higher DFU had superior results with regard to reducing major amputation rates and increased wound healing 7 Conversely there was an increase in the minor amputation rate but this trend was recognized as an acceptable alternative to major amputation rather than as a negative result While HBO2 has many antimicrobial properties i e enhancing leukocyte killing activity direct bacteriostatic effect on anaerobic organisms 82 a common misconception in the community is that the primary role of HBO2 is intended to help resolve the diabetic foot infection This impression is illustrated by comments from physicians that a patient does not require HBO2 after amputation of an infected toe because the infected bone is gone In such situations the rationale for hyperbaric oxygen changes to salvaging limbs by E T Huang J Mansouri M H Murad et al preserving flaps threatened by reduced perfusion healing of the residual ischemic wound or a combination of the two This misconception is the result of the requirement by many insurance companies that patients fit into a pigeonhole of being diagnosed with a Wagner Grade 3 DFU in order to receive HBO2 with the defining characteristic of a Wagner 3 DFU as the presence of osteomyelitis although the classic Wagner classification would also include abscess and tendonitis A deeper understanding of the original Faglia study shows that infection is only the instigating event for immediate surgical intervention of the dysvascular foot and the actual benefit of HBO2 is to allow the wound to heal and avoid major amputation by providing oxygenation of ischemic tissue This recommendation is in direct contrast to what is commonly practiced namely the utilization of HBO2 in an outpatient setting for DFUs that have not shown significant healing after 30 days The reason for this may be economically driven as reimbursement policies may have unfortunately abrogated clinic decision making The lack of acute inpatient HBO2 for Wagner Grade 3 or higher DFUs may also be the reason that more recent trials have shown an increase in wound healing but no improvement in major amputation rate This factor may also be the reason that the Margolis study did not show the effectiveness of HBO2 22 although numerous studies have demonstrated superior efficacy compared to standard of care Adverse events We considered benefits and harms when developing recommendations The analysis of the RCTs for occurrence of adverse events yielded few meaningful results as the overall incidence of adverse events was very low and the sample size of these studies was too low to be useful The RCTs included in this analysis predominantly reported adverse events only related to HBO2 although there were several studies that reported non HBO2 related side effects In general large retrospective studies are more useful for identifying serious adverse events related to HBO2 National registries like the U S Wound Care Registry as well as proprietary databases from for profit management companies also allow for reporting of adverse events related to HBO2 from a larger sample of patients treated with HBO2 There are obviously some adverse events that are solely related to HBO2 and would not be seen in patients treated with alternative therapies i e baro 227
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU trauma central nervous system oxygen toxicity hyperoxic myopia Data from one management company revealed 463 293 monoplace hyperbaric chamber treatments of 17 267 patients from 2009 2010 In 2009 there were 916 adverse events reported for 207 479 treatments in 7 781 patients adverse event rate of 0 44 and in 2010 there were 954 adverse events reported for 255 814 treatments in 9 296 patients adverse event rate of 0 37 In order of decreasing rate of occurrence were ear pain 20 per 10 000 treatments confinement anxiety eight per 10 000 hypoglycemic events five per 10 000 shortness of breath two per 10 000 seizures two per 10 000 sinus pain one per 10 000 and chest pain one per 10 000 Overall the risk of adverse events from HBO2 can be considered to be very low and self limited when they do occur 83 Cost effectiveness Few studies have been published regarding the costeffectiveness of HBO2 in the treatment of DFUs Cianci reported in a cohort study of 41 patients that the estimated cost in 1991 dollars of below knee amputation US 40 000 plus rehabilitation US 30 000 was greater than the cost of HBO2 to salvage a limb US 31 265 16 Bennett reported 2003 2004 Australian data that the average cost for wound care and HBO2 was AUS 14 928 for each amputation prevented and that HBO2 might decrease the overall cost of health care when the costs of amputation and rehabilitation were considered 85 Chuck used 2008 Canadian data on DFU prevalence and HBO2 efficacy data to create a computer model that estimated the 12 year cost for patients receiving HBO2 was CND 40 695 compared with CND 49 786 for standard care alone This study concluded that adjunctive HBO2 for DFU was cost effective when compared to standard care 86 Only a single RCT prospectively addressed the cost effectiveness of the use of HBO2 in the treatment of DFUs Abidia 2003 This study evaluated the cost of ulcer dressings per visit per patient for one year in both the treatment and control groups and found an average savings of UK 2 960 per patient treated with HBO2 This analysis took into account the additional costs of HBO2 and treatment of any associated complications The Review Committee was unable to obtain the raw data for this study to include it in our GRADE analysis Due to recent trends in insurance coverage and 228 reimbursement policies the cost effectiveness of HBO2 is likely to become an important factor in any discussions focusing on the use of HBO2 in clinical practice Cost effectiveness studies are often conducted using decision modeling and simulations e g Markov Monte Carlo due to the complex economic variables and uncertainty involved Thus it is somewhat challenging to interpret the significance of cost effectiveness data using these existing studies Patient perspective Two patients one who received HBO2 and one who was eligible for but did not receive HBO2 were invited to attend a CPG Committee Meeting to give their perspective on several aspects of the process Neither patient had a financial interest in any hyperbaric chamber manufacturer or operations The patients were given a brief overview of the scope and nature of the purpose and methodology of this CPG The patients were given the opportunity to describe their impressions of the outcomes of interest and rank order them without knowing what reviewers had chosen The patients were in agreement that major amputation rate and healing percentage at the one year mark ranked high in their lists but they also felt that mortality quality of life healing durability and time to heal were also important outcomes Once revealed they concurred with the committee s rank order of the outcomes and the reasons some outcomes of interest were not deemed as critical as others Specifically they understood that a minor amputation could be an acceptable outcome when done to prevent a more serious proximal limb amputation and that a healed wound at the one year mark was a surrogate measure for healing durability These opinions are in contrast to the online survey results rating all outcomes as critical which highlight the importance of having a conversation between patient and provider The patients comments about the components of standard care indicated that while it was easily understood why each component was important it could be very difficult to carry out in practice Overall they agreed that the CPG would be an important tool for clinicians and patients but stressed that the greatest need was information about their treatment options presented in language that was understandable to the patient While patients would in most cases defer to the recommendations of the medical professionals E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU their comfort level in the treatment choice was influenced greatly by the amount of information provided to them at the time of the decision They understood that the CPG was designed to provide busy clinicians a summary of the data in a way that could be passed along to patients This perspective reinforces the concept that shared decision making between the patient and provider is an essential part of any CPG Differences from other technology reviews and potential for bias The UHMS advocates for the responsible evidencebased use of hyperbaric oxygen therapy As experts in the field we possess the experience to analyze the hyperbaric literature with clinical perspective Nonhyperbaric physicians are included in the review committee to provide even more objectivity in the analysis The results of this review utilizing the same source material differs from similar reviews conducted by Cochrane and the Canadian Program for Assessment of Technology in Health PATH because of differences in purpose and judgment The Cochrane review is a summary of the evidence that does not seek to make clinical recommendations The PATH review based their inferences on statistical significance p values whereas we considered how precise the estimates were to support a particular decision The GRADE methodology and the transparency that is employed in this extensive statistical analysis allows others to make their own judgments and compare them with the conclusions of this review committee Technical Comments RECOMMENDATION 1 In patients with Wagner Grade 2 or lower diabetic foot ulcers we suggest against adding hyperbaric oxygen therapy to the standard of care with regard to preventing major amputation and promoting complete healing very low conditional Patients with Wagner Grade 2 or lower DFU should receive optimal wound care but HBO2 should not typically be part of the treatment plan There may be cases where a patient has previously required HBO2 for a Wagner Grade 3 or higher DFU and is now presenting with another ulcer In rare cases it may be advisable to incorporate HBO2 before the ulcer progresses but this should be the exception and not E T Huang J Mansouri M H Murad et al the rule As in all other cases this will be in combination with addressing mechanical offloading optimizing revascularization elimination of infection debriding devitalized tissue and improving metabolic control RECOMMENDATION 2 In patients with Wagner Grade 3 or higher diabetic foot ulcers who have not shown significant improvement after 30 or more days we suggest adding hyperbaric oxygen therapy to the standard of care with regard to preventing major amputation and promoting complete healing moderate conditional Patients who have not shown significant improvement after 30 days of optimal wound care should receive adjunctive HBO2 Treatment pressure of 2 0 2 4 atm abs is recommended for 90 120 minutes A course of 30 sessions is recommended but is dependent on ensuring that other barriers to healing i e infection vascular status removal of devitalized tissue etc have been adequately addressed Additional HBO2 can be considered if there has been improvement in the wound but concerns about the above factors have not been resolved completely It should be explained to patients that HBO2 is only a part of the treatment plan and will not necessarily be used until the DFU is completely healed Patients who receive HBO2 should have continued offloading optimization of revascularization elimination of infection debridement of devitalized tissue and excellent diabetes management RECOMMENDATION 3 In patients with Wagner Grade 3 or higher diabetic foot ulcers that require immediate surgery we suggest adding inpatient postoperative hyperbaric oxygen therapy to the standard of care with regard to preventing major amputation and promoting complete healing moderate conditional Patients who require surgery for a Wagner Grade 3 or higher DFU should receive HBO2 within 24 hours of the time of surgery Treatment pressure of 2 0 2 4 atm abs is recommended for 90 120 minutes A course of 30 sessions is recommended but is subject to the goals being sought such as survival of a flap seven or less days of treatments angiogenesis two weeks 229
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________ Figure 6 Algorithm for the use of HBO2 All DFU Wagner 2 YES Suggest against adding HBO2 very low conditional NO Wagner 3 with acute surgical intervention YES Suggest adding HBO2 urgently after surgery moderate conditional NO Wagner 3 that has not healed after 30 days YES Suggest adding HBO2 to standard of care Research recommendations This analysis of the HBO2 DFU body of literature indicates that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate of effect This echoes numerous systematic reviews that call for more studies Other than the Cochrane Review those reviews lacked specific recommendations to guide future research We provide some specific recommendations here moderate conditional NO Insufficient data to make a recommendation ____________________________________________________________________________ of treatments or refractory osteomyelitis 30 to 40 treatments Additional HBO2 can be considered if there has been improvement in the wound but concerns about the above factors have not been resolved It should be explained to patients that HBO2 is only a part of the treatment plan and would not necessarily be used until the DFU was completely healed Patients who receive HBO2 should have continued offloading optimization of revascularization elimination of infection debridement of devitalized tissue and excellent diabetes management Conclusions The use of HBO2 for DFU is founded on the assumption that practitioners have aggressively addressed revascularization of the ischemic foot debridement of devitalized tissue offloading of the neuropathic foot lesion and appropriate anti infective therapies before utilizing adjunctive HBO2 Hyperbaric oxygen should be included as part of a comprehensive diabetic foot ulcer program The level of evidence is of moderate quality and the Review Committee felt that taking patient values and preferences into account justified conditional recommendations to add HBO2 to the 230 standard of wound care management of diabetic foot ulcers Proper selection of patients should pair these guidelines with clinical acumen to identify patients who will heal without HBO2 and exclude patients who will not heal even after receiving HBO2 An algorithm that incorporates all of the recommendations is provided in Figure 6 Methodology Future studies need to be scientifically rigorous and well designed GRADE penalizes RCTs that have high risk of bias Future studies should be designed with strict allocation concealment blinding of study groups and intention to treat analysis Data reporting should follow the Consolidated Standards of Reporting Trials CONSORT so that outcome data can be more easily interpreted Study populations In order to better establish the efficacy of HBO2 for the various populations of patients with DFUs future studies must include discrete subgroups of patients upon which treatment groups are stratified While imperfect the Wagner classification is the most widely used If alternative wound classification systems are to be accepted as criteria for utilizing HBO2 future studies will need to be randomized on these new wound classifications Treatment standards Both hyperbaric treatment standards and standard wound care need to be better defined A standard treatment pressure length frequency and duration should be chosen for future studies Hyperbaric air sham therapy should be standardized so that all studies can be properly blinded Standard wound care needs to be clearly defined for future studies and should include optimization of vascular status offloading of the neuropathic foot diabetes control aggressive sur E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU gical debridement and infection control Adherence to standard wound care should also be reported as the patient contributors to this CPG have indicated that it is difficult to follow recommendations all of the time Outcomes of interest Critical outcomes of major amputation and incomplete healing should be reported for all future studies Additional data on minor amputation rate quality of life and persistence of infection should be reported so that more evidence can be collected about these outcomes Cost effectiveness studies are needed to provide more concrete analysis rather than through extrapolations based on limited data from surrogate markers of healthcare costs Treatment of infection As noted above under Recommendation 3 a common misconception in the community is that the primary role of HBO2 is intended to help resolve the diabetic foot infection Surprisingly there is little to no direct evidence to support the role of HBO2 in the treatment of infection The studies that did include infected patients did not stratify the severity of the infection by any one of the recognized systems i e IDSA or PEDIS Some used surrogate markers 5 7 such as changes in culture results as opposed to more widely accepted clinical endpoints such as the presence or absence of clinical signs and symptoms of infection Before a recommendation can be made in the effectiveness of HBO2 specifically for the treatment of diabetic foot infection we believe that a well designed trial utilizing widely recognized evidencedbased diagnostic criteria and endpoints is needed E T Huang J Mansouri M H Murad et al Proposed studies Recommendation 3 identifies that there is a population of DFU patients who should receive acute postoperative HBO2 without waiting 30 days from the time of diagnosis A study that would confirm this could be designed to randomize all patients who have an incision and debridement Group A amputation at level of the metatarsal phalangeal joint Group B amputation at the metatarsal level Group C to either HBO2 or to HBAir sham therapy Outcomes of major amputation and incomplete healing would be recorded for all patients using intention to treat analysis Additional outcomes of cost effectiveness quality of life persistence of infection and minor amputation would be recorded as well Patient selection based on tissue oxygenation PtcO2 stratification has been proposed to allow more judicious use of HBO2 This has not been evaluated prospectively but a study that would allow for this to be tested would be to take patients with a Wagner Grade 3 or higher DFU and stratify them based on baseline sea level air PtcO2 greater than 40 mm Hg Group I or 40 mm Hg or less Group 2 Group 2 could be then stratified on whether a single in chamber PtcO2 at 2 0 atm abs rises over 200 mm Hg Group 2a or fails to rise over 200 mm Hg Group 2b Each group would then be randomized to HBO2 or HBAir sham therapy Outcomes of major amputation and incomplete healing would be recorded for all patients using intention to treat analysis Additional outcomes of cost effectiveness quality of life persistence of infection and minor amputation would be recorded as well n 231
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU _____________________________________________________________________________________________________________________________________________________________________ Contributors to this Clinical Practice Guideline Enoch T Huang MD MPH TM Michael B Strauss MD Medical Director Wound Healing and Hyperbaric Medicine Adventist Medical Center Portland Oregon Affiliate Assistant Professor Emergency Medicine Oregon Health and Sciences University Portland Oregon Medical Director Hyperbaric Medicine Program Long Beach Memorial Medicine Center Long Beach California Clinical Professor of Orthopaedic Surgery University of California Irvine School of Medicine Irvine California Orthopaedic Consultant PAVE Prevention Amputation Veterans Everywhere Clinic Long Beach California Contributions to this CPG Dr Huang was lead author and reviewer for this CPG on DFU and chairs the UHMS CPG Oversight Committee Dr Huang assisted in adapting the GRADE protocols for use in the UHMS CPG Project search strategy development and execution data extraction and critical appraisal of evidence Contributions to this CPG Dr Strauss participated in data extraction critical appraisal of evidence and editorial support Practice background Undersea and Hyperbaric Medicine Wound Medicine Emergency Medicine Practice background Orthopedic Surgery focusing on Limb Salvage and Foot Ankle Reconstruction Wound Management and Undersea and Hyperbaric Medicine Conflict of interest Less than 25 of Dr Huang s clinical practice income involves HBO2 as an adjunctive therapy for managing DFU Conflict of interest Less than 10 of Dr Strauss s clinical practice income involves HBO2 as an adjunctive therapy for managing DFU Warren S Joseph DPM William H Tettelbach MD Roxborough Memorial Hospital Philadelphia Pennsylvania Medical Director of Wound Care Ostomy Intermountain Healthcare Salt Lake City Utah Program Director of Duke University Hyperbaric Medicine Satellite Fellowship Salt Lake City Utah Adjunct Assistant Professor Duke University School of Medicine Durham North Carolina Contributions to this CPG Dr Joseph participated in data extraction critical appraisal of evidence and editorial support Practice background Podiatric Medicine Infectious Disease Conflict of interest Dr Joseph has no financial relationship with the clinical practice of hyperbaric medicine Jaleh Mansouri MD MPH Contributions to this CPG Dr Mansouri provides methodological and logistical support for the UHMS CPG Project Dr Mansouri assisted in adapting the GRADE protocols for use in the UHMS CPG Project search strategy development and execution data extraction and critical appraisal of evidence Practice background Pathology Conflict of interest Dr Mansouri is contracted to be the methodologist for the UHMS CPG Project Dr Mansouri has no financial relationship with the clinical practice of hyperbaric medicine M Hassan Murad MD MPH TM Professor of Medicine Program Director Preventive Medicine Residency Mayo Clinic Rochester Minnesota Contributions to this CPG Dr Murad provided evidence based medicine and methodology expertise to the development of the UHMS CPG Project Practice background Preventive Medicine Hyperbaric Med Conflict of interest Less than 5 of Dr Murad s clinical practice income involves HBO2 as an adjunctive therapy for managing DFU 232 Contributions to this CPG Dr Tettelbach participated in data extraction critical appraisal of evidence and editorial support Practice background Undersea and Hyperbaric Medicine Wound Medicine Infectious Disease Conflict of interest Less than 25 of Dr Tettelbach s clinical practice income involves HBO2 as an adjunctive therapy for managing DFU Eugene R Worth MD Medical Director Hyperbaric Medicine Dixie Regional Medical Center St George Utah Adjunct Assistant Professor of Anesthesiology Duke University Undersea and Hyperbaric Medicine Fellowship Durham North Carolina Contributions to this CPG Dr Worth participated in data extraction critical appraisal of evidence and editorial support Practice background Undersea and Hyperbaric Medicine Wound Medicine Anesthesiology Conflict of interest Less than 25 of Dr Worth s clinical practice income involves HBO2 as an adjunctive therapy for managing DFU n E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU _____________________________________________________________________________________________________________________________________________________________________ Appendix A Detailed search strategy PubMed 4 30 15 Total 377 Diabetic Foot Mesh OR Foot Ulcer Mesh OR Leg Ulcer Mesh OR diabetes tiab OR diabetic tiab AND foot tiab OR feet tiab OR ulcer tiab OR wound tiab OR foot tiab AND ulcer tiab OR feet tiab AND ulcer tiab OR plantar ulcer tiab OR leg ulcer tiab OR ulcus cruris tiab OR crural ulcer tiab AND Hyperbaric Oxygenation Mesh OR hyperbaric tiab AND oxygen tiab OR HBO tiab OR HBOT tiab OR oxygen tiab AND high pressure tiab OR high tension tiab OR hyperbaric chamber tiab NOT case report Embase 4 30 15 Total 200 leg ulcer exp OR foot ulcer exp OR diabetic foot exp OR diabetic feet ti ab OR diabetes NEAR 3 ulcer ti ab OR diabetic NEAR 3 ulcer ti ab OR diabetic NEAR 3 wound ti ab OR diabetes NEAR 3 wound ti ab OR leg NEAR 3 ulcer ti ab OR foot NEAR 3 ulcer ti ab OR ulcer NEAR 3 feet ti ab OR plantar NEAR 3 ulcer ti ab OR ulcus cruris ti ab OR crural ulcer ti ab OR crural ulcers ti ab OR diabetic NEAR 3 foot ti ab OR diabetic NEAR 3 feet ti ab AND hyperbaric oxygen exp OR hyperbaric NEAR 1 oxygen ti ab OR hbo ti ab OR hbot ti ab OR hyperbaric chamber ti ab OR hyperbaric chambers ti ab OR oxygen and high pressure OR high tension ti ab NOT case report exp AND embase lim NOT medline lim Cochrane 4 30 15 Search Terms mh diabetic foot or mh foot ulcer or mh leg ulcer _____________________________________________________________________________________________________________________________________________________________________ 1 1228 _____________________________________________________________________________________________________________________________________________________________________ 2 diabet ti ab kw and foot ti ab kw or feet ti ab kw or ulcer ti ab kw or wound ti ab kw or plantar ulcer ti ab kw or ulcus cruris ti ab kw or crural ulcer ti ab kw 1884 3 1 AND 2 4 mh hyperbaric oxygenation _____________________________________________________________________________________________________________________________________________________________________ 2546 _____________________________________________________________________________________________________________________________________________________________________ 379 _____________________________________________________________________________________________________________________________________________________________________ 5 hyperbaric ti ab kw and oxygen ti ab kw or hbo ti ab kw or hbot ti ab kw or oxygen ti ab kw or high pressure ti ab kw or high tension ti ab kw or hyperbaric chamber ti ab kw 28857 6 4 or 5 28857 7 3 and 6 150 _____________________________________________________________________________________________________________________________________________________________________ _____________________________________________________________________________________________________________________________________________________________________ _____________________________________________________________________________________________________________________________________________________________________ E T Huang J Mansouri M H Murad et al 233
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU __________________________________________________________________________________________________________________________________________________ Supplemental Figure 1 Alternate forest plots and GRADE analysis for Question 1 Comparison of observational studies vs randomized controlled trials HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control continued 234 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU __________________________________________________________________________________________________________________________________________________ Supplemental Figure 1 Alternate forest plots and GRADE analysis for Question 1 Comparison of observational studies vs randomized controlled trials HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control E T Huang J Mansouri M H Murad et al 235
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________________________________________________________________________ Supplemental Figure 2 Alternate forest plots and GRADE analysis for Question 1 Comparison of observational studies vs randomized controlled trials HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control 236 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________________________________________________________________________ Supplemental Figure 3 Alternate forest plots and GRADE analysis for Question 1 Comparison of observational studies vs randomized controlled trials HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control E T Huang J Mansouri M H Murad et al 237
CRITICAL REVIEW Hyperbaric Oxygen Therapy Side Effects Defined and Quantified Marvin Heyboer III Deepali Sharma William Santiago and Norman McCulloch Division of Hyperbaric Medicine and Wound Care Department of Emergency Medicine SUNY Upstate Medical University Syracuse New York Marvin Heyboer III MD FACEP FUHM FACCWS Submitted for publication December 1 2016 Accepted in revised form January 26 2017 Correspondence Division of Hyperbaric Medicine and Wound Care Department of Emergency Medicine SUNY Upstate Medical University 550 East Genesee Street Suite 103 Syracuse NY 13202 e mail heyboerm upstate edu Significance Hyperbaric oxygen therapy HBOT is an important advanced therapy in the treatment of problem wounds including diabetic foot ulcers and late effect radiation injury HBOT remains among the safest therapies used today Nonetheless there are side effects associated with HBOT It is important for providers to be able to identify understand and quantify these side effects for prevention management and informed consent Recent Advances The past two decades have seen significant advancements in our understanding of the underlying mechanisms of HBOT This has led to a better understanding of the underlying reason for clinical benefit It has also led to a better understanding of its side effects Moreover more recent literature allows for better quantification of these side effects This review will highlight these side effects Critical Issues Wound healing in the case of problem nonhealing wounds requires the use of various advanced treatment modalities including HBOT HBOT has been shown to significantly improve healing rates in certain problem wounds including advanced diabetic foot ulcers and late effect radiation injury It is provided in a variety of clinical settings by providers with varying levels of expertise It is important for those providing this therapy to understand the potential side effects Future Directions Research in HBOT has led to significant advancements in the area of wound healing At the same time there remains a variety of treatment protocols used at different institutions It is important to quantify risk and benefit at different treatment pressures and times to better standardize treatment and improve patient care Keywords hyperbaric oxygen side effects SCOPE AND SIGNIFICANCE Hyperbaric oxygen therapy HBOT has been identified as a useful advanced adjunctive therapy in the promotion of healing in certain problem wounds in addition to its application to a variety of other medical conditions As with all medical treatments HBOT has known potential side effects as a result of treatment A side effect here is considered a known potential secondary and 210 j ADVANCES IN WOUND CARE VOLUME 6 NUMBER 6 Copyright 2017 by Mary Ann Liebert Inc usually adverse effect This review will attempt to describe and quantify these side effects This should lead to better consideration of risk and benefit in discussions with the patient when considering HBOT TRANSLATIONAL RELEVANCE HBOT works through both primary and secondary effects Primary effects involve both increased pres DOI 10 1089 wound 2016 0718
HYPERBARIC OXYGEN SIDE EFFECTS sure and hyperoxia Secondary effects as a result of a controlled oxidative stress include antimicrobial effects blunting of ischemia reperfusion injury and wound healing Wound healing is the result of both local and systemic effects Local effects include a steepened oxygen gradient macrophage recruitment and release of multiple growth factors Systemic effects result in progenitor stem cell mobilization and release from bone marrow in addition to improved homing to the site of injury by these cells 1 4 The results of both local and systemic effects include neovasculogenesis and collagen formation which promote wound healing 1 4 These same mechanisms that result in HBOT beneficial effects can also cause the known side effects in some patients CLINICAL RELEVANCE The use of HBOT has grown significantly in the past 2 decades Its application has a variety of recognized indications as outlined by the Undersea and Hyperbaric Medicine Society 5 although a majority of patients are receiving treatment for late effect radiation injury and problem wounds primarily advanced diabetic foot ulcers Treatment is provided in a variety of clinical settings by providers and staff with differing levels of expertise Having an understanding of the potential side effects of HBOT is critical to providing safe medical care with complete patient informed consent BACKGROUND AND OVERVIEW HBOT is the treatment of patients with 100 oxygen at higher than atmospheric pressure 1 This is provided in either a monoplace single person chamber typically compressed with oxygen or a multiplace chamber multiple persons compressed with air where oxygen is delivered by either a hood or mask The benefits of treatment are the result of both primary and secondary effects Primary effects are the result of increased pressure and hyperoxia Indeed PaO2 can increase from less than 200 mmHg at 1 atmospheres absolute ATA room air to more than 2 000 mmHg at 3 ATA This also translates into significant increases in tissue oxygen partial pressure 6 Meanwhile secondary effects are the result of a controlled oxidative stress HBOT produces reactive oxygen species ROS and reactive nitrogen species which function as signaling molecules in multiple pathways including those involved in wound healing 1 The result is an array of secondary effects that include improved leukocyte function amelioration of ischemia reperfusion injury and neovascularization as a 211 result of increased local growth factors and release of autologous progenitor stem cells 7 It is these very same primary and secondary effects that can cause the side effects associated with HBOT These include various forms of barotrauma central nervous system CNS and pulmonary oxygen toxicity and ocular side effects There are additionally issues of claustrophobia It is important to understand and quantify these side effects This assists with creating protocols to minimize risk in addition to better weighing risk and benefit of treatment for the patient It is important to note that HBOT remains among the safest therapies used today 8 The following is an exhaustive list of potential side effects some of which are more common middle ear barotraumas MEB claustrophobia and others that are theoretical risks unlikely to occur clinically with appropriate screening precautions pulmonary barotrauma PBT DISCUSSION Effects of pressure HBOT by definition means treatment with 100 oxygen at higher than atmospheric pressure where increased pressures depend on treatment guidelines and indications Hence the side effects of HBOT are based on the physiologic response to this high pressure high oxygen environment and the psychological response that patients experience from the closed confines of the treatment chamber monoplace or multiplace Boyle s Law states that the volume of a gas at a fixed temperature is inversely proportional to the ambient pressure Lowering the ambient pressure causes increased gas volume the converse is also true Fig 1 These effects of pressure are experienced within physiologic and pathologic air cavities including the middle ear paranasal sinuses pathologic dental spaces and emphysematous bulla Figure 1 Gas volume change with pressure
212 HEYBOER ET AL Middle ear barotrauma MEB is one of the most common side effects of HBOT Patients may report difficulty with ear equalization a feeling of pressure ear pain and discomfort during compression which is the initial phase of HBOT 9 If not attended to this can lead to edema in the middle ear retraction and in rare cases rupture of the tympanic membrane with conductive hearing deficit In rare cases MEB can be transmitted to the inner ear with risk of rupture of the round or oval window membranes and impairment of inner ear function causing vertigo and sensorineural hearing loss 10 MEB is most commonly classified using the modified TEED score Table 1 More recently the O Neill grading system was proposed as a newer and more practical grading system 11 For effective air equalization in the middle ear to occur the Eustachian tube ET which connects the middle ear to the nasopharynx positioned superior posterior and lateral to the nasopharynx needs to be open and functioning Fig 2 12 The ET is collapsed at rest and needs to be actively opened by the patient using valsalva maneuvers swallowing chewing or by attempting to create positive pressure by blowing air against the pinched nares thereby opening the collapsed ET 10 During compression the relative negative middle ear pressure compared with the dive chamber pressure causes collapse and closure of the ET 13 Inability to open the ET prevents equalization of the middle ear pressure with the higher outside pressure This results in gas volume contraction in the middle ear which initially causes pain Subsequent inward retraction of the tympanic membrane and adjoining ossicles followed by middle ear mucosal swelling capillary dilation and transudate leakage causes fluid extravasation into the middle ear space with blood vessel rupture resulting in hemotympanum and possible tympanic membrane perforation 10 13 Alternatively if air equalization on either side of the tympanic membrane TM does not occur during decompression positive pressure increase in the middle ear may also lead to similar middle ear trauma although less likely since the positive pressure helps to open the ET Table 1 Modified TEED score Grade 0 1 2 3 4 5 Findings on Otoscopy Normal examination TM injection or retraction Slightly hemorrhagic TM Grossly hemorrhagic TM Hemotympanum TM perforation Causes of ET dysfunction may be inherent craniofacial features such as palatal muscle anomalies or a result of infectious or allergic reactions These include upper respiratory infections environmental allergies or enlarged adenoids to name a few 14 The reported incidence of MEB in patients undergoing HBOT varies significantly from 2 to 84 in nonintubated and upward of 94 in intubated patients making MEB one of the most common side effects of HBOT 8 15 The wide range of incidence is due to varying criteria used to define MEB variations in patient population and variation in patient instruction of how to equalize pressure in the middle ear 8 A recent publication of a large number of patient treatments demonstrated an overall incidence of 43 The vast majority of cases were minor 84 were TEED 1 TM injection retraction or TEED 2 TM slight hemorrhage with no episodes of TM rupture 8 Rate of compression does play a role in risk of MEB A previous study demonstrated that a high rate of compression 4 1 psi min increased risk of MEB 16 On the other hand a more recent study suggested that a very slow rate of compression 1 psi min also increases risk of MEB It found that 2 psi min was the best compression rate for minimizing MEB 8 There is an increased risk of MEB during initial treatments and no increased risk associated with a longer treatment course 8 17 Other risk factors indentified include intubation active upper respiratory infection diabetes presumptively due to neuropathy and a history of head and neck malignancy 8 15 18 Intuitively there is higher risk of MEB in intubated patients with mixed evidence in the literature supporting this 8 19 20 MEB can be avoided and its incidence reduced Adequate patient education training and assistance through active coaching during compression can help mitigate MEB cases In instances where patients are unable to successfully equalize air pressure across the middle ear needle myringotomy may be performed for emergent patients or tympanostomy tubes placed for the duration of extended treatments 10 For patients with inherent ET dysfunction with known allergic or inflammatory etiology the use of decongestants and antihistamines can reduce obstruction and facilitate successful pressure equalization Most cases of MEB resolve in the absence of repetitive trauma 8 Long term sequelae from MEB during HBOT are rare The sequelae reported include sensorineural hearing loss ossicular disruption and perilymphatic fistula Management requires referral to otolaryngology for possible
HYPERBARIC OXYGEN SIDE EFFECTS 213 Figure 2 Anatomy of the ear D S surgical interventions such as tympanoplasty or surgical repair of the round or oval window 10 Most injuries including tympanic membrane rupture serous otitis and tympanic membrane edema heal spontaneously and medications such as antibiotics decongestants and steroids are not indicated Although MEB is the most common of HBOT side effects it is also most easily and effectively ameliorated with patient coaching topical medications and in less common circumstances relatively benign surgical intervention Sinus paranasal barotrauma Sinus and paranasal barotrauma is the second most common manifestation of barotrauma after MEB often occurring in the setting of upper respiratory infections or allergic rhinitis 15 Barotrauma of the paranasal sinuses is characterized by pressure sensation most commonly felt over the frontal sinuses resulting in barosinusitis The ostea draining the sinuses into the nasal cavity are small in diameter compared with the spaces they drain With HBOT changes in pressure occur during the compression phase inside sinus cavities similar to those described in MEB above A nega tive pressure gradient causes inflammation of the mucosal surfaces of sinuses and osteal openings thereby occluding these sinuses This compression of the sinus space leads to congestion and edema which is accompanied by facial pain and relieved as the pressure is eliminated Fig 3 21 The resulting edema can create a closed air space within the sinuses resulting in paradoxical pain during chamber decompression as the air volume expands but is unable to escape Barosinusitis can lead to epistaxis although such cases are rare with incidence reported at 1 case per 10 000 treatments 15 The pressure changes that occur during HBOT are similar to pressure changes that occur during underwater recreational diving up to 60 feet in sea water 2 8 ATA A case report for optic neuropathy was reported from possible ethmoidal and sphenoidal barotrauma after recreational diving with resolution of symptoms 22 There is a propensity for barosinusitis to occur in the setting of upper airway inflammation due to underlying upper respiratory infections allergic rhinitis or mucociliary dysfunction Indeed acute upper respiratory infection is a relative contraindi
214 HEYBOER ET AL Figure 3 Anatomy of sinuses D S cation to elective HBOT When HBOT is provided symptoms should be controlled with a regimen of decongestant nasal spray antihistamines and or steroid nasal spray just before compression 15 Dental barotrauma Dental barotrauma barodontalgia odontocrexis which is commonly called tooth squeeze is pain in a tooth caused by a change in atmospheric pressure This phenomenon was first observed in air crews during World War II and subsequently reported in divers 23 Dental pain can occur during either compression or decompression It is classically experienced as a decrease in pressure during decompression causes expansion of air bubbles trapped under a root filling or against dentin activating nociceptors It can also be referred to pain with stimulation of nociceptors in the maxillary sinuses If expanding trapped gas results in dental stress it may cause tooth fracture a process called odontecrexis tooth explosion in Greek 24 Possible etiologies include dental infections sinusitis differences in the expansion behavior of dental enamel and pulp and pressure induced movement of fluids from exposed dentine to the pulp 23 Barodontalgia can occur as a result of any change in pressure including HBOT However the majority of studies evaluating this side effect come from aviation and dive medicine It has been reported during flying at altitudes higher than 600 m and during diving at depths of more than 10 m with incidence at 0 26 2 8 in aircraft personnel air passengers and divers 23 Barodontalgia has been reported by 9 2 21 6 of American and Australian civilian divers 25 Preventive measures should include a dental examination by the hyperbaric medicine physician before HBOT and treatment of carious lesions and defective restorations when known before HBOT 23 Pulmonary barotrauma As previously mentioned Boyle s Law states that the volume of a gas at a fixed temperature is inversely proportional to the ambient pressure Similar volume changes can be seen in the lungs of patients undergoing HBOT if a closed system is created Normally there is no risk of PBT in patients with normal lungs and an open glottis The potential exists for PBT from lung overinflation for patients at risk for air trapping during decompression asthma or chronic obstructive pulmonary disease COPD with active bronchospasm mucous plugging and bullous lung disease and those with a prolonged closed glottis
HYPERBARIC OXYGEN SIDE EFFECTS Should the lung parenchyma be disrupted from overinflation during decompression the potential manifestations are pneumomediastinum subcutaneous emphysema intrapulmonary hemorrhage simple pneumothorax PTX and tension PTX Pneumomediastinum and intrapulmonary hemorrhage are generally self limited and require only conservative management with supplemental oxygen to achieve resolution PTX however is a potentially life threatening phenomenon especially given the increased risk of exacerbating a simple PTX into a tension PTX during decompression in a hyperbaric chamber Tension PTX can rapidly lead to cardiovascular collapse and death if not treated quickly with thoracostomy tube insertion Cases of tension PTX during hyperbaric oxygen treatment are very rare but have been reported 26 27 Arterial gas embolism AGE can result from PBT when alveolar air passes into the ruptured pulmonary vessels The air bubbles then enter the left heart and embolize through systemic arteries leading potentially to vascular occlusion in the brain or heart 28 The most severe clinical manifestations of AGE include apnea unconsciousness and cardiac arrest Other symptoms include loss of consciousness confusion aphasia dysarthria vertigo visual disturbance unilateral sensory and motor changes and seizure Cases of PBT resulting in AGE have been reported in the medical literature 29 Treatment of choice for AGE from any etiology is HBOT 5 6 The lung is an open air space system As such PBT is not expected with HBOT in the absence of pulmonary disease As such all potential candidates for HBOT must be thoroughly screened for pulmonary disease which may increase the risk of PBT Screening begins with a thorough history and physical examination Historical features including COPD asthma bronchiectasis cancer prior spontaneous PTX or prior chest surgery should prompt further investigation inclusive of at minimum a chest x ray Indeed an unvented PTX is an absolute contraindication to HBOT due to the potential of creating a tension PTX during the decompression phase of treatment This requires treatment to create an open system before any hyperbaric treatment Other pulmonary historical features may not preclude a potential patient from HBOT but treatment protocols may need adjustment such as a slower decompression rate to suit the needs of a particular patient This may be the case in a patient with significant blebs who is decompressed at a slow 1 psi min rate Additionally a careful evaluation of risk versus benefit should be 215 undertaken in circumstances where significant pulmonary disease is present to mitigate any potential untoward outcome during HBOT CNS oxygen toxicity As we have stated HBOT is the treatment of patients with 100 oxygen at higher than atmospheric pressures HBOT can result in arterial oxygen tensions of greater than 2 000 mmHg and tissue levels of 200 400 mmHg and higher 6 HBOT has many of its therapeutic benefits through controlled oxidative stress Antioxidant defenses are usually adequate during the hyperoxic exposure created by a typical clinical hyperbaric oxygen treatment 1 Nonetheless CNS oxygen toxicity does occur The recognized presentation of CNS oxygen toxicity during clinical hyperbaric oxygen treatment is an oxygen toxicity seizure The link between hyperbaric oxygen and seizure was first recognized by Paul Bert in 1878 30 31 Dr Christian J Lambertsen described it in this way The convulsion is usually preceded but not always by the occurrence of localized muscular twitching Eventually an abrupt spread of excitation occurs and the rigid tonic phase of the convulsions begins Vigorous clonic contractions of the muscle groups of the head and neck trunk and limbs then occur becoming progressively less violent over 1 minute 32 33 The exact underlying pathophysiology is not understood It appears to be the result of direct oxygen toxicity The increased ROS and free radical intermediates interact with the neuronal cell plasma membrane 34 36 This causes lipid peroxidation at the plasma membrane resulting in a change in brain electrical activity 35 Nitric oxide NO has been implicated as a mediator for CNS oxygen toxicity through formation of peroxynitrite ONOO In addition there is vasodilation secondary to NO which counteracts the cerebral vasoconstriction normally seen secondary to hyperoxia 37 Gross retention of carbon dioxide CO2 in brain tissue and intense vasoconstriction have been shown to be unlikely causes 34 Prodromal symptoms have been reported although they appear in
HEYBOER ET AL 216 varies inversely with the PO2 breathed 34 No pathologic changes have been found to be associated with an isolated oxygen mediated seizure 36 An oxygen toxicity seizure is relatively rare at typical clinical treatment pressures 2 ATA 3 ATA It is difficult to predict on an individual basis It was traditionally reported at 1 in 10 000 treatments 40 However more recent evidence over the past 15 years puts the incidence at 1 in 2 000 3 000 treatments 7 38 41 42 The reason for the increased incidence over the past 15 20 years appears to be related to patient selection sicker patients with more comorbid illness and changes in hyperbaric oxygen treatment protocols 42 Risk factors identified include higher treatment pressure CO2 retention brain tumor brain soft tissue radionecrosis hypoglycemia hyperthyroid and carbon monoxide poisoning 7 38 43 46 No link to increased risk has been identified with monoplace versus multiplace chamber neurologic versus non neurologic treatment indication or past medical history of stroke diabetes alcoholism or epilepsy 7 38 47 Table 2 shows the incidence reported in published studies Table 3 lists risk factors to having an oxygen toxicity seizure that have been identified Preventive measures include the use of air breaks at given intervals during hyperbaric oxygen breathing This allows for interval breaks in overt exposure to oxygen free radicals and resulting seizure While the use of air breaks to decrease the incidence of CNS oxygen toxicity has not been directly demonstrated there is a large amount of published data on the cause of oxygen toxicity related directly Table 2 Incidence of oxygen toxicity seizure Study Incidence Percent Tx Pressure Hart 1987 1 in 12 253 0 8 per 10 000 0 008 2 3 ATA Davis40 1 in 10 552 0 95 per 10 000 0 01 2 4 ATA All Welslau and Almeling44 1 in 6 704 1 5 per 10 000 0 05 2 4 2 8 ATA All Plafki et al 41 1 in 2 844 3 5 per 10 000 0 035 2 4 2 5 ATA All Hampson and Atik42 1 in 3 388 3 per 10 000 0 03 2 2 8 ATA All Yildiz et al 43 1 in 40 339 0 25 per 10 000 0 0025 2 2 8 ATA All Banham38 1 in 1 651 6 per 10 000 0 06 1 9 4 ATA All Heyboer et al 7 1 in 2 121 5 per 10 000 0 05 2 2 8 ATA All Hadanny et al 47 1 in 8 945 1 1 per 10 000 0 011 1 5 2 8 ATA All 89 ATA atmospheres absolute Indications All Table 3 Risk factors for oxygen toxicity seizure Risk Factors Increased treatment pressure 2 vs 2 4 2 5 vs 2 8 ATA Other CNS brain tumor STRN brain Air break Increased treatment pressure 2 vs 2 4 ATA Carbon monoxide poisoning Increased treatment pressure 1 5 vs 2 vs 2 4 vs 2 8 ATA Carbon monoxide poisoning Hypoglycemia hyperthyroid Hood over mask multiplace chamber Study Heyboer et al 7 Banham38 Hadanny et al 47 Hampson et al 45 Welslau and Almeling44 Yildiz et al 43 CNS central nervous system to a combination of the level of PO2 exposure and time As such these air breaks limit the interval time exposure and are expected to decrease the risk of oxygen toxicity 34 Indeed the U S Navy has used air breaks successfully for many years Yildiz found that the use of masks was protective over hoods due to less risk of CO2 retention when undergoing treatment in a multiplace chamber 43 Finally screening for risk factors and optimizing antiseizure medications in known epileptics before hyperbaric oxygen treatment are thought to be protective There are no long term sequelae as a result of an oxygen toxicity seizure No pathophysiologic changes have been found to be associated with an isolated oxygen mediated seizure 36 Indeed patients who have had an oxygen toxicity seizure may still go on to complete their recommended course of treatment While their risk of subsequent oxygen toxicity seizure is increased it is still less than 10 7 38 44 47 Adjustments can be made to subsequent treatments including lower treatment pressure and additional air breaks While oxygen toxicity seizure is one of the more feared side effects of HBOT its incidence remains low with no evidence of long term sequelae as a result of an episode Pulmonary oxygen toxicity Continuous exposure of the lungs to elevated levels of oxygen either at atmospheric or hyperbaric pressure leads to progressively severe toxic effects as the duration of exposure FiO2 or pO2 increases Pathological manifestations of pulmonary oxygen toxicity are differentiated into two overlapping phases the acute exudative phase and the subacute proliferative phase Pulmonary changes in the acute exudative phase include interstitial and alveolar edema intraalveolar hemorrhage fibrinous exudate hyaline membrane swelling and destruction of capillary endothelial cells and type I alveolar epithelial cells Interstitial fibrosis fibroblastic proliferation and hyperplasia of type II alveolar epithelial cells characterize the subacute proliferative phase Table 4 48
HYPERBARIC OXYGEN SIDE EFFECTS Table 4 Pathologic manifestations of pulmonary oxygen toxicity Acute Exudative Phase Subacute Proliferative Phase Interstitial edema Alveolar edema Intra alveolar hemorrhage Interstitial fibrosis Fibroblastic proliferation Type II alveolar epithelial cell hyperplasia Fibrinous exudate Capillary endothelium destruction Type I alveolar epithelial cell destruction Pulmonary mechanical function is negatively affected by these pathological changes Table 5 Changes in pulmonary function include decreased lung compliance decrements in inspiratory and expiratory lung volumes and rates and decreased CO2 diffusing capacity Progressive reduction in vital capacity is seen in pulmonary oxygen toxicity Indeed decreased vital capacity remains a consistent and sensitive manifestation of pulmonary oxygen toxicity The rate of pulmonary oxygen toxicity development correlates with pO2 and the duration of exposure 49 Symptoms of toxicity typically begin after 12 16 h at 1 0 ATA 8 14 h at 1 5 ATA and 3 6 h at 2 0 ATA Symptoms occur earlier at 2 5 and 3 0 ATA but are milder since exposure time is limited by neurologic oxygen toxicity 48 51 Symptoms of pulmonary oxygen toxicity are insidious in onset and present as mild substernal chest discomfort accentuated by inspiration As oxygen exposure continues this progresses to widespread pleuritic chest pain cough chest tightness and dyspnea 49 51 The severity of symptoms diminishes quickly within the first few hours postexposure and the sensation of pulmonary irritation completely disappears over the next 1 3 days 51 Pulmonary oxygen toxicity is not expected from routine daily HBOT The possibility of development does exist with prolonged exposure most typically related to long treatment tables such as US Navy Treatment Table 6 used for decompression illness but even these cases would be mild and self limiting Pulmonary oxygen toxicity can be avoided if oxygen is provided in the proper dose Humans exposed to hyperoxia at 0 55 ATA for 7 days showed no manifestations of pulmonary toxicity 52 Likewise exposure to 0 3 ATA for 30 days produced no toxicity 53 Most current apTable 5 Pulmonary function changes in oxygen toxicity Decreased Decreased Decreased Decreased Decreased lung compliance inspiratory lung volume and rate expiratory lung volume and rate carbon monoxide diffusing capacity vital capacity 217 plications of HBOT do not cause pulmonary symptoms or clinically significant pulmonary functional deficits 54 Ocular side effects Increased partial pressures of oxygen can potentially pose harm to multiple body tissues including the eye Under normoxic conditions oxygen metabolism produces superoxide radicals and other toxic reactive species Removal of these harmful substances is mediated by superoxide dismutase and other cellular defense mechanisms Under hyperoxic conditions these defense mechanisms may become overwhelmed due to the increased free radical production leading to oxygen toxicity and subsequent ocular side effects 55 In addition to the inspired PO2 and exposure duration many other variables can play a role in the development of ocular manifestations of oxygen toxicity These include the age of the exposed individual whether advanced age i e cataract promotion or young age i e retrolental fibroplasia the method use for oxygen delivery and the presence of undiagnosed comorbid conditions that may affect the patient s susceptibility to oxygen toxicity 56 57 Hyperoxic myopia Myopia can have direct toxic effects of oxygen on the crystalline lens and is one of the most common side effects 57 58 An acute myopic shift may be due to osmotic changes in the lens of the eye systemic medications i e diuretics miotic eye medications and ciliary spasm Under repeated exposures to hyperoxia hyperoxic myopia is also included in the list of differential diagnoses 59 Progressive myopic changes are a known side effect of repetitive treatments with HBOT 59 The rate of this change has been reported in the literature to be 0 25 diopter per week and progressive throughout the course of ongoing treatment 60 Myopia has been reported in 25 100 of patients undergoing HBOT after several weeks at pressures of 2 0 ATA and greater 61 The exact mechanisms for myopic change are not fully known Proposed hypotheses have included a reduction in backscattered light and lens optical density with hyperbaric oxygen through oxidative damage to the crystalline structure of the lens proteins and high partial pressures of oxygen in direct contact with the eye resulting in oxygen toxicity due to local hyperoxia 62 64 A thorough ocular examination by the diving and hyperbaric physician can provide an objective assessment of visual status and ocular function before the patient beginning HBOT If the patient is likely to undergo a prolonged course of treat
218 HEYBOER ET AL ment one may consider a more thorough examination by an optometrist or ophthalmologist that includes documentation of corrected and uncorrected visual acuity refraction color vision status of the crystalline lens and fundus examination By accurately documenting ocular function the benefit of HBOT can be weighed against any adverse effects on visual acuity and thus be used to guide therapeutic decisions Clinical experience suggests that such a change in a patient s vision may affect their overall quality of life Their driving habits may be affected routine tasks may become more challenging and patient safety becomes a concern placing those with mobility issues at an increased risk of falls and subsequent injury One may consider optometry evaluation for temporary visual correction during HBOT when the degree of myopia becomes a safety concern Utilizing 5 min periods of air breathing every 20 25 min can reduce the risk of oxygen toxicity 57 In addition the use of mask over hood in a multiplace chamber setting would theoretically decrease the risk due to a lower topical PO2 It is important to note that this myopic shift is reversible after discontinuation of HBOT usually returning to baseline within 3 6 weeks but as long as 6 12 months 59 Cataracts HBOT leads to an increase in pO2 and concentration of ROS in blood and tissues including the lens stroma of the cornea where it plays a role in cataractogenesis 57 The relationship between senile nuclear cataract formation and myopia is well known and reported and both can be considered to represent two levels of severity of lenticular oxygen toxicity The development of cataracts in humans has been reported only after prolonged exposure to hyperbaric oxygen usually 150 treatments or more 65 In the United States de novo cataract genesis is rare as the maximum number of treatments rarely exceeds 75 66 Cataracts remain the leading cause of visual impairment and blindness worldwide and usually present after age 65 67 Risk factors include advanced age female gender smoking diabetes ethanol use and corticosteroids Incidence increases over the age of 65 Three types of cataracts have been identified which are cortical subcapsular and nuclear which is the most common 68 They are identified by a yellow brown discoloration and hazy appearance of the lens in conjunction with the visual changes experienced by the patient The exact mechanism of cataractogenesis is not completely understood As reported long term exposure to HBOT resulting in oxidative damage to the lens proteins plays a critical role 69 Oxidative stress occurs when the production of ROS overwhelms the normal capacity of antioxidant defense mechanisms to facilitate their elimination Glutathione is an important antioxidant that functions to prevent damage to cellular structures caused by ROS such as free radicals peroxides and lipid peroxides Fig 4 Glutathione in its reduced form plays a critical role in the lens stroma by maintaining the transparency of lens crystalline proteins 70 71 When oxidized this can promote abnormal protein cross linking increased production of insoluble proteins and abnormal colorization resulting in nuclear light scatterings an early finding in cataract formation 69 To date there has only been one report of nuclear cataract development in a human receiving less than 50 HBOT treatments This occurred in a 49 year old woman who had received 48 treatments over a period of 11 weeks 69 This appears to be an exception to the general observation that cataract formation occurs only in treatment series greatly exceeding 20 60 treatments Undiagnosed pre existing conditions may play a role in such circumstances Increased pO2 in the precorneal gas space has been reported to play a more significant role than inspired PO2 in determining the physiologic effects of the gas mix on the cornea 72 Thus the use of a oronasal mask in lieu of a hood as an oxygen delivery device in a multiplace chamber should reduce the amount of oxygen to the eye keeping the precorneal gas closer to normal oxygen fraction This was shown to result in a 50 reduction in myopic shift and overall lenticular oxygen toxicity 63 Patients therefore should be offered the choice between delivery systems when available and clinically appropriate Retrolental fibroplasia following hyperoxic exposure Retrolental fibroplasia also known as retinopathy of prematurity is a potentially blinding condition affecting the retina of premature infants caused by exposure to hyperoxia It is vasoproliferative retinopathy that occurs in preterm babies with immature retinal vasculature 73 74 In the 1950s it was associated with the use of high amounts of oxygen in the premature infant 75 The two factors associated with pathophysiologic development are an incompletely vascularized retina and increased arterial pO2 with relative retinal hyperoxia Both of these contribute to vasoconstriction of the developing retinal vessels and a decrease in growth factors most notably insulinlike growth factor IGF 1 and vascular endothelial growth factor VEGF Consequently there is arrest of retinal neovascularization and capillary obliteration leading to a decrease in perfusion and
HYPERBARIC OXYGEN SIDE EFFECTS 219 Figure 4 Oxygen free radical effect on ocular lens subsequent retinal ischemia and hypoxia Normal response to these changes is an upregulation of various growth and angiogenic factors including IGF 1 and VEGF Fig 5 If this response is exaggerated abnormal and disorganized angiogenesis may ensue leading to inflammation proliferative retinopathy significant fibrosis and ultimately irreversible retinal detachment and permanent blindness 76 The incidence in premature infants in Western countries has been reported to vary between 35 and 60 74 Despite current neonatal care management maintaining moderate oxygenation with arterial pO2 in the range of 60 80 mmHg in attempts to curb Figure 5 Retrolental fibroplasia the incidence retinopathy of prematurity remains prevalent among small premature infants 77 78 About 4 5 of surviving babies weighing less than 1 kg are legally blind with a larger percentage exhibiting significant visual impairment Neurocognitive and developmental abnormalities may also be seen leading to profound disability including the inability to provide self care incontinence motor disabilities and altered social personal skills 76 The discussion of HBOT in the setting of retrolental fibroplasia should include two factors hyperoxia and neovascularization through angiogenesis Oxygen saturations of 88 95 will maintain an arterial pO2 above 45 mmHg and usually less than
220 HEYBOER ET AL 75 80 mmHg Targeting oxygen saturation between 88 and 93 has been shown to result in a significant reduction in retinopathy of prematurity 77 Arterial pO2 is 90 to 110 mmHg at sea level HBOT has been shown to increase the arterial pO2 to well above 2 000 mmHg 57 Such high partial pressures and oxygen saturations could potentially increase the risk of development As discussed previously an abnormal angiogenic process occurs in the retina in response to decreased perfusion and hypoxia HBOT has been shown to increase angiogenesis through upregulation of VEGF production These two benefits of HBOT not only play a central role in other conditions i e wound healing but have also been the focus of discussion and the cornerstone of research for therapeutic options in the setting of retrolental fibroplasias Retrolental fibroplasia remains an unfortunate growing global problem and a devastating complication of premature infants in both industrialized and developing nations When severe visual outcomes are unfavorable even with treatment and it still remains the most common cause of blindness 76 Prevention lies with a focus on research investigating preventative treatments that can modulate angiogenesis for example and sound clinical practice regarding oxygen supplementation and delivery in the premature infant Claustrophobia Claustrophobia is the fear of being enclosed in small spaces with no escape and may be triggered by different stimuli in the daily environment such as elevators tunnels small windowless rooms basements or even tight clothing Symptoms may include sweating palpitations hyperventilation lightheadedness choking chest tightness increased blood pressure trembling anxiety headache confusion or even disorientation Claustrophobia is thought to be caused by classical conditioning a result of past usually childhood experience or a learned behavior from parents or peers Other theories attribute the size of the amygdala to a person experiencing claustrophobia with persons suffering from panic disorders having smaller amygdala 79 Psychological effects of claustrophobia are experienced by some patients when placed in the tubelike cylindrical monoplace chambers or under hoods and face masks in multiplace chambers Between 15 and 37 of people worldwide are affected by claustrophobia with 5 7 affected by severe claustrophobia 80 It appears to be present in about 2 of the general patient population and may cause some degree of confinement anxiety even in a multiplace chamber Incidence of confinement anxiety in monoplace chambers is reported at 8 events per 10 000 treatments 15 Mild confinement anxiety is easily controlled with sedation before treatments such that individuals may continue to receive daily HBOT 15 More severe cases may need referral to a psychiatrist or a psychologist and cognitive behavioral therapy relaxation exercises and or long term drug therapy might be necessary 79 Preventive measures with adequate patient history patient education reassurance and coaching are the most effective means of anticipating episodes of claustrophobia and treating them effectively before HBOT Other side effects of HBOT Blood pressure effects HBOT causes an increase in both systolic and diastolic blood pressure DBP This holds true for both hypertensive and nonhypertensive patients 81 82 Overall the effect on blood pressure is mild One study reported an overall increase in systolic blood pressure SBP of 6 and DBP of 12 81 Another study reported increases in SBP of 7 mmHg DBP of 4 mmHg and MAP of 5 mmHg 82 No patients experienced signs of hypertensive urgency or emergency in these studies 81 82 The effect diminished with each additional treatment protective 82 Calcium channel blockers and beta blockers exacerbated HBOT effect on blood pressure 81 82 Proposed mechanisms include increased systemic vascular resistance through alphareceptor induced vasoconstriction Endothelin 1 is elevated during HBOT and endothelin 1 induced vasoconstriction may be involved 82 84 Pulmonary edema There is a theoretical risk of pulmonary edema in patients with compromised left ventricular function who are undergoing HBOT There are limited published data although the risk is low based off the data available Two studies reported their incidence at 1 in 1 000 0 1 and 1 in 4 500 0 02 83 84 While the etiology is not fully known it appears to be related to hyperbaric oxygen inducing increased systemic vascular resistance and decreased cardiac output 83 85 A recent study evaluating the effects of hyperbaric oxygen at 243 kPa found a reduction in cardiac output due only to a decrease in heart rate with no impact on other cardiac function 86 Other potential mechanisms of hyperbaric induced pulmonary edema include increased pulmonary capillary wedge pressure myocardial damage or consumption of endothelial derived NO by oxygen free radicals or cardiac output imbalance between the right and left heart 84 Noncardiac acute pulmonary edema is not expected in patients with normal
HYPERBARIC OXYGEN SIDE EFFECTS cardiac function treated with HBOT Nonetheless it may occur in those with compromised baseline cardiac function Patients with a history of congestive heart failure should have a baseline echocardiogram before HBOT and caution should be taken in patients with a low ejection fraction EF i e
222 assistance in various studies including quality studies that have been carried out The authors also thank Susan Wojcik PhD and William Grant EDD from the Department of Emergency Medicine SUNY Upstate Medical University for their assistance in study design and statistical analysis AUTHOR DISCLOSURES AND GHOSTWRITING The authors do not have any commercial conflicts of interest The article was written exclusively by the authors HEYBOER ET AL TAKE HOME MESSAGES HBOT remains among the safest therapies used today HBOT is the treatment of patients with 100 oxygen at higher than atmospheric pressure It is both the primary and secondary effects that result in its beneficial effects and side effects One of the most common side effects identified in the peerreviewed literature is MEB It is typically mild and selflimited Patient instruction on middle ear clearing daily monitoring with otoscopic examination and appropriate compression rates are important to its prevention Oxygen toxicity seizure is one of the most feared side effects of HBOT It is important to remember that this is an uncommon and self limiting side effect It is resolved with withdrawal of 100 oxygen and has no long term implications Continued HBOT is permissible and may be done with adjustment to maximum pressure and addition of air breaks Higher occurrence rates have been linked to higher treatment pressures ABOUT THE AUTHORS Marvin Heyboer III MD FACEP FUHM FACCWS is an Associate Professor of Emergency Medicine at SUNY Upstate Medical University He is board certified in Undersea and Hyperbaric Medicine and Emergency Medicine He is the Medical Director of Upstate University Hospital Hyperbaric Medicine and Wound Care Center and the Director of the Fellowship in Undersea and Hyperbaric Medicine He is actively involved in research and has published multiple articles in the areas of hyperbaric medicine and wound care William Santiago MD is an Assistant Professor of Emergency Medicine at SUNY Upstate Medical University He is board certified in Undersea and Hyperbaric Medicine and Emergency Medicine He is a Hyperbaric Medicine and Wound Care physician and an Emergency Medicine physician at Upstate University Hospital Norman McCulloch MD MBA is board certified in Internal Medicine He is fellowship trained in Undersea and Hyperbaric Medicine and board eligible in Undersea and Hyperbaric Medicine with the American Board of Preventive Medicine He is also an NOAA Dive Medical Officer Deepali Sharma MD is a Fellow in Undersea and Hyperbaric Medicine at SUNY Upstate Medical University She is residency trained in Emergency Medicine She is a practicing Emergency Medicine physician at Upstate University Hospital REFERENCES 1 Thom SR Hyperbaric oxygen its mechanism and efficacy Plast Reconstr Surg 2011 127 S1 131S 141S 5 Weaver LK Hyperbaric Oxygen Therapy Indications 13th ed North Palm Beach FL Best Publishing Company 2014 2 Thom SR Bhopale VM Velazquez OC Goldstein LJ Thom LH Buerk DG Stem cell mobilization by hyperbaric oxygen Am J Physiol Heart Circ Physiol 2006 290 1378 1386 6 Thom SR Hyperbaric oxygen therapy J Intensive Care Med 1989 4 58 74 3 Goldstein LJ Gallagher KA Bauer SM et al Endothelial progenitor cell release into circulation is triggered by hyperoxia induced increases in bone marrow nitric oxide Stem Cells 2006 24 2309 2318 4 Liu ZJ Velazquez OC Hyperoxia endothelial progenitor cell mobilization and diabetic wound healing Antioxid Redox Signal 2008 10 1869 1882 7 Heyboer III M Jennings S Grant WD Ojevwe C Byrne J Wojcik SM Seizure incidence by treatment pressure in patients undergoing hyperbaric oxygen therapy UHM 2014 41 380 385 8 Heyboer III M Wojcik S Grant WD Chambers P Jennings S Adcock P Middle ear barotrauma in hyperbaric oxygen therapy UHM 2014 41 359 363 9 Jain KK Textbook of Hyperbaric Medicine 5th ed Cambridge MA Hogrefe Publishing 1999 10 Shupak A Gilbey P Effects of pressure In Neuman TS Thom SR Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia PA Saunders Elsevier 2008 513 526 11 O Neill OJ Weitzner ED The O Neill grading system for evaluation of the tympanic membrane a practical approach for clinical hyperbaric patients UHM 2015 42 265 271 12 Bluestone CD Eustachian Tube Structure Function Role in Otitis Media Hamilton ON BC Decker Inc 2005 13 Beuerlein M Nelson RN Wellin DB Inner and middle ear hyperbaric oxygen induced barotrauma Laryngoscope 1997 107 1350 1356
HYPERBARIC OXYGEN SIDE EFFECTS 14 Bluestone CD Studies in otitis media Children s Hospital of Pittsburgh University of Pittsburgh progress report 2004 Laryngoscope 2004 114 S105 1 26 15 Camporesi EM Side effects of hyperbaric oxygen therapy UHM 2014 41 253 257 16 Vahidova D Sen P Papesch M Zein Snachez M Mueller P Does the slow compression technique of hyperbaric oxygen therapy decrease the incidence of middle ear barotraumas J Laryngol Otol 2006 120 446 449 17 Fitzpatrick D Franck B Mason K Shannon S Risk factors for symptomatic otic and sinus barotrauma in a multiplace hyperbaric chamber Undersea Hyperb Med 2010 37 203 208 18 Clements KS Vrabee JT Mader JT Complications of tympanostomy tubes inserted for facilitation of hyperbaric oxygen therapy Arch Otolaryngol Head Neck Surg 1998 124 278 19 Presswood G Zamboni WA Stephenson LL Santos PM Effect of artificial airway on ear complications from hyperbaric oxygen Laryngoscope 1994 104 1383 1384 20 Bessereau J Tabah A Genotelle N Francais A Coulange M Annane D Middle ear barotraumas after hyperbaric oxygen therapy UHM 2010 37 203 208 21 Skevas T Baumann I Bruckner T Clifton N Plinkert PK Klingmann C Medical and surgical treatment in divers with chronic rhinosinusitis and paranasal sinus barotrauma Eur Arch Otorhinolaryngol 2012 269 853 860 22 Gunn DJ O Hagan S Unilateral optic neuropathy from possible sphenoidal sinus barotrauma after recreational scuba diving a case report UHM 2013 40 81 86 23 Stoetzer M Kuehlhorn C Ruecker M Ziebolz D Gellrich NC von See C Pathophysiology of barodontalgia a case report and review of the literature Case Rep Dent 2012 2012 453415 24 Robichaud R McNally ME Barodontalgia as a differential diagnosis symptoms and findings J Can Dent Assoc 2005 71 39 42 25 Zadik Y Drucker S Diving dentistry a review of the dental implications of scuba diving Australian Dent J 2011 56 265 271 26 Cakmak T Battal B Kara K et al A case of tension pneumothorax during hyperbaric oxygen therapy in an earthquake survivor with crush injury complicated by ARDS adult respiratory distress syndrome Undersea Hyperb Med 2015 42 9 13 27 Unsworth IP Pulmonary barotrauma in a hyperbaric chamber Anesthesia 1973 28 675 678 28 Wolf HK Moon RE Mitchell PR Burger PC Barotrauma and air embolism in hyperbaric oxygen therapy Am J Forensic Med Pathol 1990 11 149 153 29 Rivalland G Mitchell SJ Van Schalkwyk JM Pulmonary barotrauma and cerebral gas embolism during hyperbaric oxygen therapy Aviat Space Environ Med 2010 81 888 890 30 Kellogg RH La pression barometrique paul bert s hypoxia theory and its critics Respir Physiol 1978 34 1 28 31 Bert P La Pression Barome trique Paris Masson et Cie 1878 32 Lambertsen CJ Effects of oxygen at high partial pressure In Fenn WO Rahn H eds Handbook of Physiology Bethesda MD Am Physiol Soc 1965 1027 1046 33 Bitterman N CNS oxygen toxicity UHM 2004 31 63 72 34 Lambertsen CJ Kough RH Cooper DY Emmel GL Loeschcke HH Schmidt CF Oxygen toxicity Effects in man of oxygen inhalation at 1 and 3 5 atmospheres upon blood gas transport cerebral circulation and cerebral metabolism Jr Applied Phys 1953 5 471 486 35 Torbati D Church DF Keller JM Pryor W Free radical generation in the brain precedes hyperbaric oxygn induced convulsions Free Radic Biol Med 1992 13 101 106 36 Clark JM Oxygen toxicity In Neuman TS Thom SR eds Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia PA Saunders Elsevier 2008 527 564 37 Chavko M Auker CR McCarron RM Relationship between protein nitration and oxidation and development of hyperoxic seizures Nitric Oxide 2003 9 18 23 38 Banham NDG Oxygen toxicity seizures 20 years experience from a single hyperbaric unit Diving Hyperb Med 2011 41 202 210 39 Donald KW Oxygen poisoning in man BMJ 1947 1 712 717 40 Davis JC Hyperbaric oxygen therapy J Intensive Care Med 1989 4 55 57 223 47 Hadanny A Meir O Bechor Y Fishlev G Bergan J Efrati S Seizures during hyperbaric oxygen therapy retrospective analysis of 62 614 treatment sessions UHM 2016 43 21 28 48 Clark JM Lambertsen CJ Pulmonary oxygen toxicity a review Pharmacol Rev 1971 23 37 133 49 Clark JM Lambertsen CJ Gelfand R et al Effects of prolonged oxygen exposure at 1 5 2 0 or 2 5 ATA on pulmonary function in men Predictive Studies V J Appl Physiol 1999 86 243 259 50 Comroe JH Dripps RD Dumke PR Deming M The effect of inhalation of high concentrations of oxygen for twenty four hours on normal men at sea level and at a simulated altitude of 18 000 feet JAMA 1945 128 710 717 51 Clark JM Lambertsen CJ Rate of development of pulmonary O2 toxicity in man during O2 breathing at 2 0 atm abs J Appl Physiol 1971 30 739 752 52 Michel EL Langevin RW Gell CF Effect of continuous human exposure to oxygen tension of 418 mmHg for 168 hours Aerosp Med 1960 31 138 144 53 Herlocher JE Quigley DG Behar VS et al Physiologic response to increased oxygen partial pressure I Clinical observations Aerosp Med 1964 35 613 618 54 Thorsen E Aanderud L Aasen TB Effects of a standard hyperbaric oxygen treatment protocol on pulmonary function Eur Respir J 1998 12 1442 1445 55 Butler FK Diving and Hyperbaric ophthalmology Surv Ophthalmol 1995 39 347 396 56 Nichols CW Lambertsen CJ Effects of high oxygen pressures on the eye N Engl J Med 1969 281 25 30 57 McMonnies CW Hyperbaric oxygen therapy and the possibility of ocular complications or contradictions Clin Exp Optom 2015 98 122 125 58 Tibbles PM Edelsberg JS Hyperbaric oxygen therapy N Engl J Med 1996 334 1642 1648 41 Plafki C Peters P Almeling M Welslau W Busch R Complications and side effects of hyperbaric oxygen therapy Aviat Space Environ Med 2000 71 119 124 59 Butler FK Hagan C Ocular complications in hyperbaric oxygen therapy In Neuman TS Thom SR eds Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia PA Saunders Elsevier 2008 565 572 42 Hampson N Atik D Central nervous system oxygen toxicity during routine hyperbaric oxygen therapy UHM 2003 30 147 153 60 Anderson B Farmer JC Hyperoxic myopia Trans Am Ophthalmol Soc 1978 76 116 124 43 Yildiz S Aktas S Cimsit M Ay H Togrol E Seizure incidence in 80 000 patient treatments with hyperbaric oxygen Aviat Space Environ Med 2004 75 992 994 61 Churchill S Deru K Wilson G Cable R Bell JE Weaver LK Rates of visual acuity change in patients receiving hyperbaric oxygen in monoplace and multiplace chambers UHM 2016 43 217 223 44 Welslau W Almeling M Toxicity of hyperbaric oxygen HBO incidence of major CNS intoxications Strahlenther Onkol 1996 172 S2 10 12 62 Evanger K Pierscionek BK Vaagbo G Thorsen E Haugen OH Myopic shift during hyperbaric oxygenation attributed to lens index changes Optom Vis Sci 2015 92 1076 1084 45 Hampson NB Simonson SG Kramer CC Piantadosi CA Central nervous system oxygen toxicity during hyperbaric treatment of patients with carbon monoxide poisoning UHM 1996 23 215 219 46 Sanders RW Katz KD Suyama J et al Seizure during hyperbaric oxygen therapy for carbon monoxide toxicity a case series and five year experience J Emerg Med 2012 42 e69 e72 63 Evanger K Haugen OH Irgens A Aanderud L Thorsen E Ocular refractive changes in patients receiving hyperbaric oxygen administered by oronasal mask or hood Acta Ophthalmol Scand 2004 82 449 453 64 Giblin FJ Padgaonkar VA Leverenz VR et al Nuclear light scattering disulfide formation and
224 membrane damage in lenses of older guinea pigs treated with hyperbaric oxygen Exp Eye Res 1995 60 219 235 65 Palmquist BM Philipson B Barr PO Nuclear cataract and myopia during hyperbaric oxygen therapy B J Ophthalmol 1984 68 113 117 66 Kindwall EP Whelan HT Hyperbaric Medicine Practice 3rd ed Flagstaff AZ Best Publishing Company 2008 67 Solomon R Donnenfeld ED Recent advances and future frontiers in treating age related cataracts JAMA 2003 290 248 251 68 Allen D Vasavada A Cataract and surgery for cataract BMJ 2006 333 128 132 69 Gesell LB Trott A De Novo cataract development following a standard course of Hyperbaric Oxygen Therapy UHM 2007 34 389 392 70 Weikel KA Garber C Baburins A Taylor A Nutritional modulation of cataract Nutr Rev 2014 72 30 47 71 Giblin FJ Glutathione a vital lens antioxidant J Ocul Phamacol Ther 2000 16 121 135 72 Butler FK The eye in the wilderness In Auerbach P eds Wilderness Medicine 5th ed St Louis Mosby 2007 604 624 73 Ashton N Ward B Serpell G Role of oxygen in the genesis of retrolental fibroplasia a preliminary report Br J Ophthalmol 1953 37 513 520 74 Teoh SL Boo NY Ong LC Nyein MK Lye MS Au MK Duration of oxygen therapy and exchange transfusion as risk factors associated with retinopathy of prematurity in very low birth weight infants Eye 1995 9 733 737 75 Patz A The role of oxygen in retrolental fibroplasia Tr Am Ophth Soc 1968 66 940 985 76 Sola A Chow L Rogido M Retinopathy of prematurity and oxygen therapy a changing relationship An Pediatr Barc 2005 62 48 61 HEYBOER ET AL 77 Chow LC Wright KW Sola A Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants Pediatrics 2003 111 339 345 78 Weinberger B Laskin DL Heck DE Laskin JD Oxygen toxicity in premature infants Toxicol Appl Pharmacol 2002 181 60 67 79 Paddock M Claustrophobia causes symptoms and treatments June 25 2015 www medical newstoday com articles 37062 last accessed November 7 2016 80 Davey GC Phobias A Handbook of Theory Research and Treatment 1st ed West Sussex England John Wiley Sons Ltd 1997 81 Al Waili NS Butler GJ Beale J et al Influences of hyperbaric oxygen on blood pressure heart rate and blood glucose levels in patients with diabetes mellitus and hypertension Arch Med Res 2006 37 991 997 82 Heyboer III M Smith G Santiago W Wojcik SM Effect of hyperbaric oxygen therapy on blood pressure UHM Accepted September 27 2016 83 Abel FL Mcnamee JE Cone DL Clarke D Tao J Effects of hyperbaric oxygen on ventricular performance pulmonary blood volume and systemic and pulmonary vascular resistance UHM 2000 27 67 73 84 Weaver LK Churchill S Pulmonary edema associated with hyperbaric oxygen therapy Chest 2001 120 1407 1409 85 Whalen RE Saltzman HA Holloway DH Jr et al Cardiovascular and blood gas response to hyperbaric oxygenation Am J Cardiol 1965 15 638 646 86 Gawthrope IC Playford DA King B Brown K Wilson C McKeown B The cardiac effects of hyperbaric oxygen at 243 kPa using inchamber echocardiography Diving Hyperb Med 2014 44 141 145 87 Stevens SL Narr AJ Claus PL et al The incidence of hypoglycemia during HBO therapy a retrospective review UHM 2015 42 191 196 88 Swaby J Heyboer M Wojcik S Grant W Effects of hyperbaric oxygen therapy on diabetic serum glucose levels an extended study Undersea Hyperb Med J 2015 42 190 89 Hart GB Strauss MB Central nervous system oxygen toxicity in a clinical setting In Bove AA Bachrach AJ Greenbaum LJ eds Undersea and Hyperbaric Physiology IX Proceedings of the Ninth International Symposicum on Underwater and Hyperbaric Physiology Bethesda MD Undersea and Hyperbaric Medical Society 1987 695 699 Abbreviations and Acronyms AGE ATA CNS CO2 COPD DBP EF ET HBOT IGF 1 MEB NO ONOOPaO2 PBT pO2 PTX ROS SBP TM VEGF arterial gas embolism atmospheres absolute central nervous system carbon dioxide chronic obstructive pulmonary disease diastolic blood pressure ejection fraction Eustachian tube hyperbaric oxygen therapy insulin like growth factor middle ear barotrauma nitric oxide peroxynitrite partial pressure of oxygen in arterial blood pulmonary barotrauma partial pressure of oxygen pneumothorax reactive oxygen species systolic blood pressure tympanic membrane vascular endothelial growth factor
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________________________________________________________________________ Supplemental Figure 4 Forest plots and GRADE analysis for Question 1 Non critical outcome of minor amputation HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control ___________________________________________________________________________________________________________________________________________ Supplemental Figure 5 Forest plots and GRADE analysis for Question 1 Non critical outcome of persistent infection HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control 238 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________________________________________________________________________ Supplemental Figure 6 Alternate forest plots and GRADE analysis for Question 2 Comparison of observational studies vs randomized controlled trials HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control E T Huang J Mansouri M H Murad et al 239
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ___________________________________________________________________________________________________________________________________________ Supplemental Figure 7 Alternate forest plots and GRADE analysis for Question 2 Comparison of observational studies vs randomized controlled trials HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control 240 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________________________________________________________________________________________ Supplemental Figure 8 Alternate forest plots for Question 2 HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control ____________________________________________________________________________________________________________________________________________________________ Supplemental Figure 9 Additional GRADE analysis for Question 2 Non critical outcome of minor amputation E T Huang J Mansouri M H Murad et al 241
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________________________________________________________________________________________ Supplemental Figure 10 Alternate forest plots and GRADE analysis for Question 3 Comparison of observational studies vs randomized controlled trials HBO2 Control Peto Odds Ratio Peto Odds Ratio Favors HBO2 Favors Control HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control 242 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________________________________________________________________________________________ Supplemental Figure 11 Alternate forest plots and GRADE analysis for Question 3 Comparison of observational studies vs randomized controlled trials E T Huang J Mansouri M H Murad et al 243
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU ____________________________________________________________________________________________________________________________________________________________ Supplemental Figure 12 Alternate GRADE analysis for Question 3 Comparison of observational studies vs randomized controlled trials ___________________________________________________________________________________________________________________________________________ Supplemental Figure 13 Forest plots and GRADE analysis for Question 4 Non critical outcome of minor amputation HBO2 Control Risk Ratio Risk Ratio Favors HBO2 Favors Control 244 E T Huang J Mansouri M H Murad et al
_________________________________________________________________________________________________________________________________________________________ REFERENCES 1 National diabetes fact sheet national estimates and general information on diabetes and prediabetes in the United States 2011 U S Department of Health and Human Services Centers for Disease Control and Prevention Atlanta GA 2 Cowie Catherine C Diabetes 1996 vital statistics 1996 University of Michigan American Diabetes Association 3 NIH Cancer Fact Sheet 2010 National Institutes of Health 4 Abidia A et al The role of hyperbaric oxygen therapy in ischaemic diabetic lower extremity ulcers a double blind randomised controlled trial Eur J Vasc Endovasc Surg 2003 25 6 513 518 5 Doctor N Pandya S Supe A Hyperbaric oxygen therapy in diabetic foot J Postgrad Med 1992 38 3 112114 111 6 Duzgun AP et al Effect of hyperbaric oxygen therapy on healing of diabetic foot ulcers J Foot Ankle Surg 2008 47 6 515 519 7 Faglia E et al Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer A randomized study Diabetes Care 1996 19 12 1338 1343 8 Kessler L et al Hyperbaric oxygenation accelerates the healing rate of nonischemic chronic diabetic foot ulcers a prospective randomized study Diabetes Care 2003 26 8 2378 2382 9 Lin T Chen S Niu K The vascular effects of hyperbaric oxygen therapy in treatment of early diabetic foot Undersea Hyperb Med 2001 28 Suppl 67 10 Londahl M et al Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes Diabetes Care 2010 33 5 998 1003 11 Ma L et al A prospective randomized controlled study of hyperbaric oxygen therapy effects on healing and oxidative stress of ulcer tissue in patients with a diabetic foot ulcer Ostomy Wound Manage 2013 59 3 18 24 12 Kaur S et al Evaluation of the efficacy of hyperbaric oxygen therapy in the management of chronic nonhealing ulcer and role of periwound transcutaneous oximetry as a predictor of wound healing response A randomized prospective controlled trial J Anaesthesiol Clin Pharmacol 2012 28 1 70 75 13 Baroni G et al Hyperbaric oxygen in diabetic gangrene treatment Diabetes Care 1987 10 1 81 86 14 Bishop AJ Mudge E A retrospective study of diabetic foot ulcers treated with hyperbaric oxygen therapy Int Wound J 2012 9 6 p 665 676 E T Huang J Mansouri M H Murad et al 15 Chen CE et al Treatment of diabetic foot infection with hyperbaric oxygen therapy Foot Ankle Surg 2010 16 2 91 95 16 Cianci P Adjunctive hyperbaric oxygen therapy in the treatment of the diabetic foot J Am Podiatr Med Assoc 1994 84 9 448 455 17 Faglia E et al Change in major amputation rate in a center dedicated to diabetic foot care during the 1980s prognostic determinants for major amputation J Diabetes Complications 1998 12 2 96 102 18 Fife CE et al Factors influencing the outcome of lower extremity diabetic ulcers treated with hyperbaric oxygen therapy Wound Repair Regen 2007 15 3 322 331 19 Fife CE et al The predictive value of transcutaneous oxygen tension measurement in diabetic lower extremity ulcers treated with hyperbaric oxygen therapy a retrospective analysis of 1 144 patients Wound Repair Regen 2002 10 4 198 207 20 Hart GB Strauss M Responses of ischemic ulcerative conditions to OHP Proceedings of the Sixth International Congress on Hyperbaric Medicine 1979 312 314 21 Kalani M et al Hyperbaric oxygen HBO therapy in treatment of diabetic foot ulcers Long term follow up J Diabetes Complications 2002 16 2 153 158 22 Margolis DJ et al Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and the prevention of amputation a cohort study Diabetes Care 2013 36 7 1961 1966 23 Oriani G et al Hyperbaric oxygen therapy in diabetic gangrene Journal of Hyperbaric Medicine 1990 5 3 171175 24 Oriani G et al Diabetic foot and hyperbaric oxygen therapy a ten year experience Journal of Hyperbaric Medicine 1992 7 4 213 221 25 Strauss MB Bryant BJ Hart GB Transcutaneous oxygen measurements under hyperbaric oxygen conditions as a predictor for healing of problem wounds Foot Ankle Int 2002 23 10 933 937 26 Tiaka EK et al The role of hyperbaric oxygen in the treatment of diabetic foot ulcers Angiology 2012 63 4 302 314 27 Unger HD Lucca M The role of hyperbaric oxygen therapy in the treatment of diabetic foot ulcers and refractory osteomyelitis Clin Podiatr Med Surg 1990 7 3 483 492 28 Wattel F et al Hyperbaric oxygen therapy in chronic vascular wound management Angiology 1990 41 1 59 65 245
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU 29 Wattel F et al Hyperbaric oxygen in the treatment of diabetic foot lesions search for predictive healing factors Journal of Hyperbaric Medicine 1991 6 4 p 263 268 45 Stoekenbroek RM et al Hyperbaric oxygen for the treatment of diabetic foot ulcers a systematic review Eur J Vasc Endovasc Surg 2014 47 6 647 655 30 Zamboni WA et al Evaluation of hyperbaric oxygen for diabetic wounds a prospective study Undersea Hyperb Med 1997 24 3 175 179 46 Wang C et al Hyperbaric oxygen for treating wounds a systematic review of the literature Arch Surg 2003 138 3 272 279 discussion 280 31 Tongson L et al Hyperbaric oxygen therapy as adjunctive treatment for diabetic foot ulcers Wounds International 2013 4 4 8 12 47 Roeckl Wiedmann I Bennett M Kranke P Systematic review of hyperbaric oxygen in the management of chronic wounds Br J Surg 2005 92 1 24 32 32 Lyon KC The case for evidence in wound care investigating advanced treatment modalities in healing chronic diabetic lower extremity wounds J Wound Ostomy Continence Nurs 2008 35 6 585 590 48 Wunderlich RP Peters EJ Lavery LA Systemic hyperbaric oxygen therapy lower extremity wound healing and the diabetic foot Diabetes Care 2000 23 10 1551 1555 33 Niinikoski J Hyperbaric oxygen therapy of diabetic foot ulcers transcutaneous oxymetry in clinical decision making Wound Repair Regen 2003 11 6 458 461 34 Kaya A et al Can major amputation rates be decreased in diabetic foot ulcers with hyperbaric oxygen therapy Int Orthop 2009 33 2 441 446 35 Oubre CM et al Retrospective study of factors affecting non healing of wounds during hyperbaric oxygen therapy J Wound Care 2007 16 6 245 250 36 Ong M Hyperbaric oxygen therapy in the management of diabetic lower limb wounds Singapore Med J 2008 49 2 105 109 37 Bishop AJ Mudge E Diabetic foot ulcers treated with hyperbaric oxygen therapy a review of the literature Int Wound J 2014 11 1 28 34 38 Game FL et al A systematic review of interventions to enhance the healing of chronic ulcers of the foot in diabetes Diabetes Metab Res Rev 2012 28 Suppl 1 119 141 39 Goldman RJ Hyperbaric oxygen therapy for wound healing and limb salvage a systematic review PM R 2009 1 5 471 489 40 Kranke P et al Hyperbaric oxygen therapy for chronic wounds Cochrane Database Syst Rev 2004 2 CD004123 41 Kranke P et al Hyperbaric oxygen therapy for chronic wounds Cochrane Database Syst Rev 2012 4 CD004123 42 Liu R et al Systematic review of the effectiveness of hyperbaric oxygenation therapy in the management of chronic diabetic foot ulcers Mayo Clin Proc 2013 88 2 166 175 43 Murad MH et al Using GRADE for evaluating the quality of evidence in hyperbaric oxygen therapy clarifies evidence limitations J Clin Epidemiol 2014 67 1 65 72 44 O Reilly D et al Hyperbaric oxygen therapy for diabetic ulcers systematic review and meta analysis International Journal of Technology Assessment in Health Care 2013 29 3 269 281 246 49 Bakker K et al Practical guidelines on the management and prevention of the diabetic foot 2011 Diabetes Metab Res Rev 2012 28 Suppl 1 225 231 50 Game FL et al Specific guidelines on wound and wound bed management 2011 Diabetes Metab Res Rev 2012 28 Suppl 1 232 233 51 Wagner F The dysvascular foot a system for diagnosis and treatment Foot and Ankle 1981 2 2 p 64 122 52 Armstrong DG The University of Texas Diabetic Foot Classification System Ostomy Wound Manage 1996 42 8 60 61 53 Lavery LA et al Validation of the Infectious Diseases Society of America s diabetic foot infection classification system Clin Infect Dis 2007 44 4 562 565 54 Schaper NC Diabetic foot ulcer classification system for research purposes a progress report on criteria for including patients in research studies Diabetes Metab Res Rev 2004 20 Suppl 1 S90 S95 55 Widatalla AH et al Implementation of diabetic foot ulcer classification system for research purposes to predict lower extremity amputation Int J Diabetes Dev Ctries 2009 29 1 1 5 56 Strauss MB Aksenov IV Evaluation of diabetic wound classifications and a new wound score Clin Orthop Relat Res 2005 439 79 86 57 Mills JL Sr et al The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System risk stratification based on wound ischemia and foot infection WIfI J Vasc Surg 2014 59 1 220 34 e1 2 58 Clinical practice guidelines we can trust Inst of Med of the National Academies Editor 2011 59 Guyatt GH et al GRADE guidelines 1 IntroductionGRADE evidence profiles and summary of findings tables J Clin Epidemiol 2011 64 4 383 394 60 Guyatt GH et al GRADE guidelines 2 Framing the question and deciding on important outcomes J Clin Epidemiol 2011 64 4 395 400 E T Huang J Mansouri M H Murad et al
UHM 2015 Vol 42 No 3 CLINICAL PRACTICE GUIDELINE FOR HBO2 TO TREAT DFU 61 Balshem H et al GRADE guidelines 3 Rating the quality of evidence J Clin Epidemiol 2011 64 4 401 406 62 Guyatt GH et al GRADE guidelines 4 Rating the quality of evidence study limitations risk of bias J Clin Epidemiol 2011 64 4 407 415 63 Guyatt GH et al GRADE guidelines 5 Rating the quality of evidence publication bias J Clin Epidemiol 2011 64 12 1277 1282 64 Guyatt GH et al GRADE guidelines 7 Rating the quality of evidence inconsistency J Clin Epidemiol 2011 64 12 p 1294 302 65 Guyatt GH et al GRADE guidelines 8 Rating the quality of evidence indirectness J Clin Epidemiol 2011 64 12 p 1303 1310 66 Guyatt GH et al GRADE guidelines 9 Rating up the quality of evidence J Clin Epidemiol 2011 64 12 p 13111316 74 Lipsky BA et al 2012 infectious diseases society of america clinical practice guideline for the diagnosis and treatment of diabetic foot infections J Am Podiatr Med Assoc 2013 103 1 2 7 75 Braun L et al What s new in the literature an update of new research since the original WHS diabetic foot ulcer guidelines in 2006 Wound Repair Regen 2014 76 Braun LR et al Diabetic foot ulcer an evidence based treatment update Am J Clin Dermatol 2014 15 3 267 281 77 Steed DL et al Guidelines for the treatment of diabetic ulcers Wound Repair Regen 2006 14 6 680 692 78 Monteiro Soares M et al Classification systems for lower extremity amputation prediction in subjects with active diabetic foot ulcer a systematic review and metaanalysis Diabetes Metab Res Rev 2014 79 Strauss MB The Wagner wound grading system Wound Care Hyperbaric Medicine 2012 3 4 38 45 67 Brunetti M et al GRADE guidelines 10 Considering resource use and rating the quality of economic evidence J Clin Epidemiol 2013 66 2 140 150 80 Fife CE et al Transcutaneous oximetry in clinical practice consensus statements from an expert panel based on evidence Undersea Hyperb Med 2009 36 1 43 53 68 Guyatt GH et al GRADE guidelines 11 Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes J Clin Epidemiol 2013 66 2 p 151 157 81 Berendt AR Counterpoint hyperbaric oxygen for diabetic foot wounds is not effective Clin Infect Dis 2006 43 2 193 198 69 Guyatt GH et al GRADE guidelines 12 Preparing summary of findings tables binary outcomes J Clin Epidemiol 2013 66 2 158 172 70 Guyatt GH et al GRADE guidelines 13 Preparing summary of findings tables and evidence profiles continuous outcomes J Clin Epidemiol 2013 66 2 173 183 71 Andrews JC et al GRADE guidelines 14 Going from evidence to recommendations the significance and presentation of recommendations J Clin Epidemiol 2013 66 7 719 725 72 Andrews JC et al GRADE guidelines 15 Going from evidence to recommendation determinants of a recommendation s direction and strength J Clin Epidemiol 2013 66 7 726 735 73 Guyatt GH et al GRADE guidelines 6 Rating the 82 Thom SR Hyperbaric oxygen its mechanisms and efficacy Plast Reconstr Surg 2011 127 Suppl 1 131S 141S 83 Camporesi EM Side effects In Hyperbaric Oxygen Therapy Indications L K Weaver Editor 2014 Best Publishing North Palm Beach Florida 247 252 84 Cianci P Hunt TK Long term results of aggressive management of diabetic foot ulcers suggest significant cost effectiveness Wound Repair Regen 1997 5 141 146 85 Gomez Castillo JD Bennett MH The cost of hyperbaric therapy at the Prince of Wales Hospital Sydney South Pacific Underwater Medicine Society Journal 2005 35 4 5 86 Chuck AW et al Cost effectiveness and budget impact of adjunctive hyperbaric oxygen therapy for diabetic foot ulcers Int J Technol Assess Health Care 2008 24 2 178 183 quality of evidence imprecision J Clin Epidemiol 2011 64 12 1283 1293 E T Huang J Mansouri M H Murad et al 247
ORIGINAL RESEARCH Clinical Medicine 2021 Vol 21 No 6 e629 32 Hyperbaric oxygen therapy for the treatment of long COVID early evaluation of a highly promising intervention ABSTRACT Authors Tim Robbins A Michael Gonevski B Cain Clark C Sudhanshu Baitule D Kavi Sharma E Angel Magar F Kiran Patel G Sailesh Sankar H Ioannis Kyrou I Asad AliJ and Harpal S RandevaK Background Long COVID is a common occurrence following COVID 19 infection The most common symptom reported is fatigue Limited interventional treatment options exist We report the first evaluation of hyperbaric oxygen therapy HBOT for long COVID treatment Methods A total of 10 consecutive patients received 10 sessions of HBOT to 2 4 atmospheres over 12 days Each treatment session lasted 105 minutes consisting of three 30 minute exposures to 100 oxygen interspersed with 5 minute air breaks Validated fatigue and cognitive scoring assessments were performed at day 1 and 10 Statistical analysis was with Wilcoxon signed rank testing reported alongside effect sizes cognition p 0 0137 d 1 07 large executive function p 0 0039 d 1 06 large attention p 0 0020 d 1 2 very large information processing p 0 0059 d 1 25 very large and verbal function p 0 0098 d 0 92 large Conclusion Long COVID related fatigue can be debilitating and may affect young people who were previously in economic employment The results presented here suggest potential benefits of HBOT with statistically significant results following 10 sessions KEYWORDS long COVID hyperbaric oxygen therapy fatigue DOI 10 7861 clinmed 2021 0462 Results HBOT yielded a statistically significant improvement in the Chalder fatigue scale p 0 0059 d 1 75 very large global Introduction Authors ANIHR clinical lecturer University Hospitals Coventry and Warwickshire NHS Trust Coventry UK Warwick Medical School Coventry UK and Coventry University Coventry UK Bhyperbaric doctor Midlands Diving Chamber Rugby UK Cassistant professor University Hospitals Coventry and Warwickshire NHS Trust Coventry UK and Coventry University Coventry UK Dclinical fellow University Hospitals Coventry and Warwickshire NHS Trust Coventry UK Etrial manager University Hospitals Coventry and Warwickshire NHS Trust Coventry UK Fresearch grant coordinator University Hospitals Coventry and Warwickshire NHS Trust Coventry UK Gchief medical officer deputy chief executive officer and consultant cardiologist University Hospitals Coventry and Warwickshire NHS Trust Coventry UK and Warwick Medical School Coventry UK Hassociate medical director University Hospitals Coventry and Warwickshire NHS Trust Coventry UK and Warwick Medical School Coventry UK Iassociate professor University Hospitals Coventry and Warwickshire NHS Trust Coventry UK Warwick Medical School Coventry UK and Coventry University Coventry UK Jconsultant sleep and respiratory physician University Hospitals Coventry and Warwickshire NHS Trust Coventry UK and Warwick Medical School Coventry UK K director of research and development University Hospitals Coventry and Warwickshire NHS Trust Coventry UK and Warwick Medical School Coventry UK The COVID 19 pandemic has resulted in the need to support large cohorts of patients suffering from long COVID after recovery from acute infection 1 Long COVID is a term used to describe presence of various symptoms even weeks or months after acquiring SARS CoV 2 infection irrespective of the viral status 2 Long COVID is a common condition with estimates identifying that between 10 and 20 of people initially diagnosed with acute COVID 19 will go on to develop symptoms of long COVID 3 There remains some debate about the terminology used in long COVID with the UK National Institute for Health and Care Excellence NICE also using the terminology post COVID 19 syndrome for signs and symptoms that develop during or after an infection consistent with COVID 19 continue for more than 12 weeks and are not explained by an alternative diagnosis and ongoing symptomatic COVID 19 for signs and symptoms of COVID 19 from 4 to 12 weeks 3 However NICE also recognises the umbrella term long COVID Long COVID now poses an emerging public health emergency with multiple challenges for the management of these patients in clinical practice 4 6 The symptoms associated with long COVID are diverse including breathlessness cough fatigue brain fog anxiety and depression 7 One of the most commonly reported symptoms is fatigue present in up to 65 of long COVID patients this is accompanied by a substantial proportion also reporting cognitive and affective deficits described in the literature as brain fog 8 11 The fatigue experienced by these patients can be particularly severe preventing them from performing their usual Royal College of Physicians 2021 All rights reserved e629
Tim Robbins Michael Gonevski Cain Clark et al work and activities while the age group most affected by long COVID tends to be economically active adults 12 Currently specific treatment options for long COVID are limited with even fewer treatment options available for those suffering from fatigue 13 14 Thus there is a growing need to identify effective treatments for these patients 15 Despite distinct differences there are important similarities between long COVID fatigue and chronic fatigue syndrome 9 16 Hyperbaric oxygen therapy HBOT is an intervention where an individual breathes near 100 oxygen intermittently while inside a hyperbaric chamber that is pressurized to greater than sea level pressure 1 atmosphere absolute or ATA 17 18 HBOT is used for both elective eg soft tissue radiation complications and non healing chronic wounds and emergency medical conditions eg carbon monoxide poisoning decompression illness and gas embolism 17 In particular HBOT has been shown to be safe and effective in the treatment of chronic fatigue syndrome 19 20 At University Hospitals Coventry and Warwickshire NHS Trust working in direct partnership with the Midlands Diving Chamber at the Rugby Hospital of St Cross we proposed that HBOT may be of benefit to people suffering from symptoms of long COVID The first patient to receive HBOT for long COVID received this on the 11 January 2021 Currently there is no study to our knowledge which explored the effects of HBOT on long COVID related fatigue Here we present the first evaluation of a HBOT service for the treatment of long COVID symptoms internationally Methods We retrospectively evaluated the response of fatigue symptoms of patients with long COVID related fatigue receiving HBOT at the Midlands Diving Chamber medical facility Hospital of St Cross Rugby This retrospective evaluation was approved by the University Hospitals Coventry and Warwickshire NHS Trust COVID 19 Research Ethics Committee through the GAFREC Process ID 10026 We evaluated 10 consecutive patients undergoing HBOT for long COVID related fatigue at the Midlands Diving Chamber All patients were suffering from new fatigue that developed during or after an infection consistent with COVID 19 and continuing for more than 12 weeks The clinical inclusion and exclusion criteria for these patients are listed in Table 1 All patients received 10 HBOT sessions once daily at 2 4 atmospheres for 1 hour and 45 minutes over 12 days with a 2 day break in the middle for the weekend The responses of these 10 consecutive patients receiving HBOT therapy were evaluated with the primary outcome measure being the change in Chalder fatigue scale between days 1 and 10 of treatment 21 The secondary measure evaluated was the change in the cognitive profile scores of day 1 and day 10 as reported through the NeuroTrax evaluation 22 This scoring included global cognitive score memory executive function attention information processing speed visual spatial verbal function and motor skills Statistical analysis In order investigate differences between day 1 and day 10 undergoing HBOT Wilcoxon signed rank testing was conducted and reported alongside corresponding effect sizes Cohen s d classified as small 0 2 medium 0 5 large 0 8 or very large 1 2 e630 Table 1 Inclusion and exclusion criteria for hyperbaric oxygen therapy Inclusion criteria Exclusion criteria Age above 18 years Previous confirmed COVID 19 infection diagnosed with swab PCR test or positive antibody test Subject willing and able to read understand and sign an informed consent to have hyperbaric oxygen therapy Patient suffering severe longstand ing post COVID 19 syndrome History of traumatic brain injury or any other non COVID brain pathology Active malignancy current solid organ or blood cancer either under active treatment observation or palliative care Substance use at baseline alcohol use in excess of current government guidelines Severe or unstable physical disorders or major cognitive deficits at baseline HBOT for any reason prior to study enrolment Chest pathology incompatible with pressure changes including moderate to severe asthma COPD and history of pneumothorax Epilepsy Ear or sinus pathology incompatible with pressure changes Claustrophobia COPD chronic obstructive pulmonary disease HBOT hyperbaric oxygen therapy and 95 confidence intervals CIs 23 In addition Bayes factors were also calculated to express the probability of a difference given H10 alternate hypothesis relative to H01 null hypothesis that is values larger than 1 are in favour of H10 assuming that H01 and H10 are equally likely and using a default prior 24 Bayes factors were reported as the probability of the data given the alternative relative to the null hypothesis or vice versa classified as anecdotal BF1 3 moderate BF3 10 strong BF10 30 very strong BF30 100 or extreme BF 100 25 27 Bayesian analysis was concurrently utilised because it permits the amalgamation of discipline specific knowledge facilitates direct probability statements to be made pertaining to included parameters ie population level effects allows zero effects to be determined provides estimates of uncertainty around parameter values that are more intuitively interpretable than those from null hypothesis testing alone and supports in the interpretation of p values 28 29 All analyses were conducted using R software 30 Results In the present cohort 60 of the patients were women The mean average age of participants was 47 5 years range 24 74 All patients had been suffering from long COVID symptoms for over 3 months Participant level and overall group data for all collected validated scores between day 1 and day 10 of HBOT are presented in Table 2 Wilcoxon signed rank tests indicated that once daily HBOT for 10 days yielded a statistically significant improvement in Chalder fatigue scale p 0 0059 d 1 75 very large global cognition p 0 0137 d 1 07 large executive function p 0 0039 Royal College of Physicians 2021 All rights reserved
Hyperbaric oxygen for the treatment of long COVID Table 2 Day 1 vs day 10 of hyperbaric oxygen therapy p value a Mean difference 95 CI Cohen s d BF Global cognition 0 0137 8 4 14 55 2 9 1 07 7 626 Memory 0 8457 0 9 10 6 7 0 01 0 3091 a 7 3 12 65 2 2 1 06 7 3286 Attention a 0 0020 7 12 45 2 05 1 2 12 5093 IPS 0 0059a 15 3 29 8 8 2 1 25 15 3199 Visual spatial 0 1056 5 5 11 3 0 65 0 76 2 12 Executive function 0 0039 a Verbal function 0 0098 21 95 44 85 6 15 0 92 4 1335 Motor skills 0 0827 3 9 7 55 2 2 0 52 0 85 18 9 5 26 1 75 98 13 a Chalder fatigue scale a 0 0059 significant difference between time points BF Bayes factor CI confidence interval IPS information processing speed d 1 06 large attention p 0 0020 d 1 2 very large information processing speed p 0 0059 d 1 25 very large and verbal function p 0 0098 d 0 92 large Concomitantly Bayes factors indicated that the evidence favouring the alternative vs the null hypothesis was moderate for global cognition BF7 63 executive function BF7 33 and verbal function BF4 13 strong for attention BF12 51 and information processing speed BF15 32 and very strong for Chalder fatigue index BF98 13 All pairwise comparisons including p values mean differences 95 CIs Cohen s d effect sizes and Bayes Factors are presented in Table 2 and Fig 1 Finally participant level and overall group data for days 1 and 10 are presented in the supplementary material S1 No adverse events were reported in any of these patients receiving HBOT during this treatment or in the immediate posttreatment phase Discussion At University Hospitals Coventry and Warwickshire NHS Trust we have established a dedicated clinician led clinic for patients presenting with long COVID related fatigue The severity of symptoms seen and the impact on quality of life is profound Arbitrary units n 140 A en o n 160 120 100 80 60 40 20 ills n ot or sk c o M un Ve rb a lf sp a a l ed al pe su In fo r m a on Vi pr oc es sin gs y or fu nc o co al u ve Ex ec on i gn sc ue ob Gl er fa g ad Ch M em ale 0 Before A er Fig 1 Scores between day 1 before and day 10 after of hyperbaric oxygen therapy significant difference arbitrary units are construct specific Royal College of Physicians 2021 All rights reserved Many patients are unable to work either in manual or office based roles drive participate in their usual physical activity or at times engage with their family in the manner they would wish The treatment options available for such people with severe symptoms of long COVID are limited with very few interventional options Here to our knowledge we describe the first evaluated use of HBOT to manage long COVID in the UK or internationally We report statistically and clinically significant improvements to both the overall fatigue score and a range of cognitive domains using validated scales The effect size measures calculated are large suggesting a substantial improvement and thus there is a small likelihood these results are due to chance despite the small initial sample size These are important findings suggesting a possible positive effect of HBOT on the common long COVID related symptoms of fatigue and brain fog These results match with the clinical and qualitative observations of patients receiving the therapy many of whom report their lives have been transformed The mechanism of long COVID is still uncertain 1 One possible hypothesis is that the wide variety of changes that characterise long COVID are a result of prolonged tissue hypoxia 6 This is frequently the common denominator for many diseases that are responsive to HBOT 31 Further research is needed to understand the underlying mechanisms of long COVID and positive responses seen in relation to HBOT 1 While these results are important they represent only an initial evaluation Indeed the sample size consists of only 10 patients Furthermore these patients have not been followed up for a prolonged period to assess whether the noted improvements of these long COVID related symptoms were sustained Based on initial informal feedback patients do excellently in the longer term Thus there is a need to assess these effects of HBOT in the context of a randomised placebo controlled prospective study However these initial results suggest that HBOT merits further study as a treatment option for patients presenting with long COVID symptoms such as fatigue Given the scale of the emerging long COVID public health emergency globally and the still ongoing COVID 19 pandemic there is an urgent need for larger scale randomised placebo controlled trials to evaluate the potential impact of HBOT in the context of long COVID In addition creation of a registry of patients receiving HBOT for long COVID symptoms such as fatigue in order to obtain followup data over time is also suggested These are both elements e631
Tim Robbins Michael Gonevski Cain Clark et al of work currently being developed collaboratively between the Midlands Diving Chamber and University Hospitals Coventry and Warwickshire NHS Trust Supplementary material Additional supplementary material may be found in the online version of this article at www rcpjournals org clinmedicine S1 Descriptive participant level and overall group data day 1 vs day 10 References 1 Marshall M The four most urgent questions about long COVID Nature 2021 594 168 70 2 Raveendran A Jayadevan R Sashidharan S Long COVID an overview Diabetes Metab Syndr 2021 15 869 75 3 Venkatesan P NICE guideline on long COVID Lancet Respir Med 2021 9 129 4 Rando HM Bennett TD Byrd JB et al Challenges in defining Long COVID Striking differences across literature Electronic Health Records and patient reported information medRxiv 2021 2021 03 20 21253896 5 Alwan NA Johnson L Defining long COVID Going back to the start Med N Y 2021 2 501 4 6 Nabavi N Long covid How to define it and how to manage it BMJ 2020 370 m3489 7 Mandal S Barnett J Brill SE et al Long COVID a cross sectional study of persisting symptoms biomarker and imaging abnormalities following hospitalisation for COVID 19 Thorax 2021 76 396 8 8 Cabrera Martimbianco AL Pacheco RL Bagattini M Riera R Frequency signs and symptoms and criteria adopted for long COVID a systematic review Int J Clin Pract 2021 75 e14357 9 Wostyn P COVID 19 and chronic fatigue syndrome Is the worst yet to come Med Hypotheses 2021 146 110469 10 Morley JE COVID 19 the long road to recovery J Nutr Health Aging 2020 24 917 9 11 Boldrini M Canoll PD Klein RS How COVID 19 Affects the Brain JAMA Psychiatry 2021 78 682 3 12 Maxwell E Living with Covid19 National Institute for Health Research 2020 13 Shah W Hillman T Playford ED Hishmeh L Managing the long term effects of covid 19 summary of NICE SIGN and RCGP rapid guideline BMJ 2021 372 n136 14 Gaber T Assessment and management of post COVID fatigue Progress in Neurology and Psychiatry 2021 25 36 9 15 Palmer SJ Government funding for research into long COVID British Journal of Cardiac Nursing 2021 16 1 3 e632 16 Wong TL Weitzer DJ Long COVID and Myalgic Encephalomyelitis Chronic Fatigue Syndrome ME CFS A Systemic Review and Comparison of Clinical Presentation and Symptomatology Medicina 2021 57 418 17 Kirby JP Snyder J Schuerer DJ Peters JS Bochicchio GV Essentials of hyperbaric oxygen therapy 2019 review Mo Med 2019 116 176 18 Moon R Hyperbaric oxygen therapy indications Best Publishing Company 2019 19 Akarsu S Tekin L Ay H et al The efficacy of hyperbaric oxygen therapy in the management of chronic fatigue syndrome Undersea Hyperb Med 2013 40 197 200 20 Hoof EV Coomans D Becker PD et al Hyperbaric therapy in chronic fatigue syndrome Journal of Chronic Fatigue Syndrome 2003 11 37 49 21 Jackson C The Chalder fatigue scale CFQ 11 Occup Med Lond 2015 65 86 22 Doniger GM NeuroTraxcomputerized cognitive tests Test descriptions Medina NeuroTrax 2013 1 16 23 Robbins T Keung SNLC Sankar S Randeva H Arvanitis TN Application of standardised effect sizes to hospital discharge outcomes for people with diabetes BMC Medical Informatics and Decision Making 2020 20 1 6 24 Eyre EL Clark CC Tallis J et al The effects of combined movement and storytelling intervention on motor skills in South Asian and White children aged 5 6 years living in the United Kingdom Int J Environ Res Public Health 2020 17 3391 25 Marsman M Wagenmakers E J Bayesian benefits with JASP European Journal of Developmental Psychology 2017 14 545 55 26 Wagenmakers E J Marsman M Jamil T et al Bayesian inference for psychology Part I Theoretical advantages and practical ramifications Psychon Bull Rev 2018 25 35 57 27 Wagenmakers E J Love J Marsman M et al Bayesian inference for psychology Part II Example applications with JASP Psychon Bull Rev 2018 25 58 76 28 Wasserstein RL Lazar NA The ASA statement on p values context process and purpose The American Statistician 2016 70 129 133 29 Amrhein V Greenland S McShane B Scientists rise up against statistical significance Nature 2019 567 305 7 30 R Core Team R A language and environment for statistical computing R 2013 31 Choudhury R Hypoxia and hyperbaric oxygen therapy a review Int J Gen Med 2018 11 431 42 Address for correspondence Dr Timothy Robbins University Hospitals Coventry and Warwickshire NHS Trust Clifford Bridge Road Coventry CV2 2DX UK Email timothy robbins nhs net Royal College of Physicians 2021 All rights reserved
Review Derleme stanbul Med J 2020 21 4 234 41 DO I 10 4274 imj galenos 2020 89725 Current Approach to Hyperbaric Oxygen Therapy Hiperbarik Oksijen Tedavisinde G ncel Yakla m F sun Kocaman r t k i li Florence Nightingale Hospital Hyperbaric Oxygen Therapy Center stanbul Turkey ABSTRACT Z Hyperbaric oxygen HBO therapy is a therapy method based on inhalation of 100 pure oxygen through a mask or endotracheal tube or directly from the environment while subjected to a fully closed pressure chamber with 1 atmosphere It has been successfully used to treat many diseases from different medical specialties This review apart from describing the general features of HBO therapy emphasises on its therapeutic application in different medical specialties This would promote its usage alongside other methods by physicians from different clinical fields Hiperbarik oksijen HBO tedavisi tamamen kapal bir bas n odas i erisinde 1 atmosferden daha y ksek bas n larda ortamdan maskeyle veya endotrekeal t p vas tas yla fas lal olarak 100 saf oksijen solutulmas na dayanan bir tedavi y ntemidir Farkl t p dallar ndan bir ok hastal kta ba ar ile kullan lmaktad r Bu derlemede HBO tedavisinin genel zelliklerinin tan mlanmas d nda farkl olarak bran lara g re kullan m alanlar n n vurgulanmas b ylece farkl kliniklerden hekimlerin bu tedavi y ntemini hastalar i in kullanabilmelerine rehberlik edilmesi ama lanm t r Keywords Hyperbaric oxygen decompression illness carbon monoxide diabetic foot vascular disease osteomyelitis post operative wounds crush grafts flaps filling injection complications radionecrosis sudden deafness sudden blindness Anahtar Kelimeler Hiperbarik oksijen dekompresyon hastal karbonmonoksit diyabetik ayak periferik vask ler hastal k osteomiyelit postoperatif yara ezilme yaralanmas riskli greft flepler dolgu komplikasyonu radyonekroz ani i itme kayb ani g rme kayb Short History Mechanism of Hyperbaric Oxygen Therapy Oxygen was first found in 1772 by Swedish chemist Carl Wilhelm However he himself has not reported this scientifically In 1774 the English chemist Joseph Priestly published and introduced it in the scientific framework 1 Hyperbaric oxygen HBO therapy first started in France in the late 19th and early 20th centuries In 1834 Junod explained the positive effects of high pressure oxygen and in 1876 mobile compartments were put into use Production of hyperbaric chambers began from 1860 Paul Bert considered the father of Hyperbaric Medicine has described the effectiveness of HBO therapy In the same years Haldane reported that carbon monoxide intoxication was effectively treated with HBO therapy 1 4 The two main rules of HBO therapy pressure and 100 oxygen also form Definition can be balanced spontaneously With this effect it is possible to HBO therapy is a therapy based on the inhalation of 100 pure oxygen intermittently in a completely closed pressure chamber at pressures higher than 1 atmosphere from ambient air by mask or by endotrekeal tube Figure 1 3 5 downsizing air bubbles present in the tissue and intravascular area and the basis of the mechanism of effect 1 Effects of pressure 2 Effects of oxygen 1 The effects of pressure According to Boyle Mariotte law gases contract with the effect of pressure applied externally During pressurization also called the compression phase of HBO therapy a contraction occurs in gas containing cavities in the body The air in the middle ear can be narrowed by manoeuvres such as Valsalva Frenzel the air in the lungs can be narrowed by breathing and the air in the sinuses and intestines reduce tissue blood pressure in diseases such as gas gangrene air and gas embolism and decompression sickness The bubble which has lost its spheric form may disappear or be eliminated from the lungs 5 9 Address for Correspondence Yaz ma Adresi F sun Kocaman r t k MD i li Florence Nightingale Hospital Hyperbaric Oxygen Therapy Center stanbul Turkey Phone 90 555 721 66 69 E mail fkocaman yahoo com ORCID ID orcid org 0000 0002 2498 9330 Cite this article as At f Kocaman r t k F Current Approach to Hyperbaric Oxygen Therapy stanbul Med J 2020 21 4 234 41 Received Geli Tarihi 22 05 2020 Accepted Kabul Tarihi 01 06 2020 Copyright 2020 by the University of Health Sciences Turkey stanbul Training and Research Hospital stanbul Medical Journal published by Galenos Publishing House Telif Hakk 2020 Sa l k Bilimleri niversitesi stanbul E itim ve Ara t rma Hastanesi stanbul T p Dergisi Galenos Yay nevi taraf ndan bas lm t r 234
F sun Kocaman r t k Current Approach in Hyperbaric Oxygen Therapy 2 The effects of oxygen According to Henry s law under pressure the solubility of gases in liquids increases In HBO therapy conducted in 2 8 atmospheres the amount of oxygen dissolved in plasma is six times the amount in normobaric conditions The dissolved oxygen carried by the plasma can provide the amount needed for the tissue to survive even if there is no oxygen due to hemoglobin By this mechanism the antimicrobial effect of leukocytes is supported adherence of leukocytes to the capillary wall is reduced physiological vasoconstriction occurs in normal tissues fibroblast growth and collagen construction increase making of superoxide dismutase is triggered adenosine triphosphate the cell membrane present in tissue edema is conserved osteoclastic activity is regulated capillary proliferation increases ocular lens flexibility is reduced surfactant construction is reduced in the lungs separation of carbon monoxide CO gas from hemoglobin and suppressing alpha toxin production in gas gangrene In the case of hyperoxia it is also possible to withdraw the edema at intersellular distance to the intravascular area while vasoconstricting and reduce the distance that dissolved oxygen must exceed to reach the tissue 5 8 Indications for Hyperbaric Oxygen Therapy According to the HBO therapy application list in annex 2D 3 of the Health Implementation Comminique in our country the indication list evaluated under the Social Security Instution of is summarized in Table 2 12 In addition there are diseases that are being investigated and positive results are being reported with extensive research expected Emergency Medicine and Hyperbaric Oxygen Therapy Apart from CO poisoning and sudden vision loss decompression sickness and air gas embolism which lead to the birth of undersea medicine are diseases that emergency physicians may encounter in their emergency clinics Anamnesis of those suffering from decompression disease is most likely a recent history of diving or a history of exposure to high pressure and associated skin and neurological involvement In this disease which develops after diving accompanied by deep and missed safety stops which are not done according to the rules HBO therapy to be applied allows the bubbles to shrink the edema around the bubble to The United States based Undersea and Hyperbaric Medical Society UHMS and the European Committee for Hyperbaric Medicine ECHM have been working extensively on the creation of indications lists for HBO therapy Lists of indications that can be applied according to these commissions are given in Table 1 10 11 Figure 2 Control panel Figure 1 Multiplace pressure chamber Figure 3 Hyperbaric oxygen therapy unit 235
stanbul Med J 2020 21 4 234 41 Table 1 Indications for hyperbaric oxygen therapy Table 2 Social security institution hyperbaric oxygen therapy indication list UHMS indications ECHM indications Air and gas embolism 1 Absolute Indications Air embolism CO poisoning CO poisoning and toxic effect of gases and cyanides Open fractures with crush injury Gas gangrene Prevention of osteoradionecrosis after dental extraction Soft tissue infections fasciitis necrotizing fasciitis Mandible osteoradionecrosis Diabetic foot wounds and infections Soft tissue radionecrosis cystitis proctitis Peripheral vascular disease vascular induced ulcers such as Buerger s disease infections and wounds that develop after thromboembolism Arteriel insufficiencies Carbon monoxide CO poisoning Clostridial myonecrosis Compromised grafts and flaps Acute traumatic ischemia Decompression sickness Radiation injury Idiopathic sudden sensorineural hearing loss Intracranial abscess Necrotizing soft tissue infections Refractory osteomyelitis Decompression illness Gas embolism Anaerobic and mixed bacterial infections Decompresson sickness Crush compression post traumatic Injuries Venous ulcers Chronic ulcers Decubitus ulcers Sudden deafness Postoperative wound infection vascular complications 2 General Indications Spondylodiscitis intervertebral disc infection acute subacute chronic osteomyelitis Prosthetic infection and inflammation Severe anemia Diabetic foot lesions Thermal burns Femoral head avascular necrosis Avascular necrosis Compromised skin grafts and musculocutaneous flaps Late effects of cystitis dermatitis proctitis and other radiation due to RT Central retinal artery occlusion Burns Crush Injury without fracture Frostbite Osteoradionecrosis bones other than mandible Intracranial abscess Soft tissue radionecrosis other than cystitis and proctitis Malign otitis externa Application of preoperative or preimplant protection to radiotherapytreated tissue Ischaemic ulsers After graft and flap operations Anoxic encephalopathy Sudden sensorineural hearing loss Retinal artery occlusions RT Radiotherapy CO Carbon monoxide Refractory chronic osteomyelitis 2nd degree more than 20 body surface area Pneumatosis cystoides intestinalis Neuroblastoma stage IV 3 Relative Indications Selected cases in acute and chronic brain trauma chronic stroke postanoxic encephalopathy Radio induced lesions of larynx Radio induced lesions of the central nervous system Reperfusion syndrome Limb replantation Selected non healing wounds secondary to systemic processes Sickle cell disease Interstitial cystitis UHMS Undersea and Hyperbaric Medical Society ECHM Europen Committee for Hyperbaric Medicine 236 decrease and the inflammation to be reduced The patient s skin and neurological signs are reduced especially when the blisters shrink It should be remembered that the only treatment for decompression disease is the HBO therapy and that it should be seen by an undersea medicine physician even if there is a claim that safe diving is performed in the story 2 8 13 16 Air gas embolism is the condition of gas bubbles in the vascular area This condition may be iatrogenic after some surgical intervention or invasive procedures or may develop after lung barotrauma in diving or other hyperbaric environments This disease can result in Aacute respiratory distress syndrome brain edema lack of brain metabolism and sudden death In non fatal cases air bubbles block circulation it can be seen that hemoconcentration develops when platelets leukocytes fibrinogen and thrombin adhere to the bubble and the clinical picture is rapidly aggravated In the following period the thrombotic process comes to the fore and deterioration occurs in the vessel wall This disease can be an unintended complication of diving surgical practice and undersea medicine practice As soon as the clinical picture is recognized the bubbles in the vascular site of the patient receiving HBO therapy shrink the nitrogen load in the bubble is reduced the activation of the
F sun Kocaman r t k Current Approach in Hyperbaric Oxygen Therapy adhesion cascade decreases hypoxia of ischemic tissue regresses and brain edema decreases HBO therapy can be applied to the patient who needs intensive care support until the clinical picture declines 2 17 20 Internal Medicine and Hyperbaric Oxygen Therapy In our country the incidence of CO poisoning caused by coal and wood stove is high especially in winter CO binds to hemoglobin due to its high affinity as a gas creating hypoxia within the cell at the mitochondrial level It has been proven that this causes ultrastructural changes in myocytes and swells in mitochondria in electron microscopic investigations of the myocardial and this is due to deterioration of the energy use of the myocardial 21 22 HBO therapy speeds up the separation of CO gas from hemoglobin shortening the time it takes to be excreted from the body and correcting intracellular hypoxia In the studies it was determined that damage due to CO intoxication in the myocardium was also improved with HBO therapy 23 24 In patients diagnosed with CO intoxication in the emergency department CO level over 25 CO level over 20 and pregnant Loss of consciousness and or in the presence of pathological neurological signs In the presence of end organ damage such as ischemic findings in electrocardiogram In severe metabolic acidosis HBO therapy should be used to reduce mortality and increase cure rate 24 29 It should be kept in mind that intracellular hypoxia can persist even if the CO level in blood gas decreases and that myocardial damage and clinical signs may be seen even in patients below the levels mentioned above 22 General Surgery and Hyperbaric Oxygen Therapy Surgical interventions for whatever purpose disrupt the integrity of the body and create a controlled and clean wound on the skin In normal wound healing 1st day hemostasis 0 3 day inflammatory phase 3 15th day remodelization phase occurs and the process continues The wound healing stops due to an intrinsic or extrinsic problem occurring in one or more of these processes and the clinical picture of the postoperative wound appears Infection and ischemia are the most common causes of wound healing delay 2 The infection causes an exaggerated response in the inflammatory phase of wound healing resulting in rapid depletion of oxygen in the tissue resulting in insufficient blood flow due to the effect of tissue edema However ischemia occurs because the tissue reaches less oxygen than it needs The wound location is hypoxic hypoglycemic acidotic hyperkalemic hyperlactic and hypercarbic due to these reasons Especially fibroblast proliferation lysine and proline hydroxylation in collagen synthesis angiogenesis and leukocytosis activity are oxygen dependent functions This whole healing process is interrupted by lack of oxygen 2 30 32 Diabetic foof ulcer develops in 2 2 of diabetic patients every year and training for prevention of ulcer provides serious benefits to the national economy 33 Diabetic patients account for a significant proportion of non traumatic amputations and morbidity all over the world In diabetic foot treatment with multidisciplinary approach good regulation of diabetes proper dietary protocol control of infection correction of vascular pathologies adequate and timely debritmans daily optimal wound healing environment reducing pressure on the foot area and HBO therapy should be added to the protocol Educating the patient about diabetic foot and explaining the importance of following medical treatment and diet program will reduce recurrence in amputations of foot ulcers and the addition of HBO therapy will decrease the amputation rate 34 38 Such publications can be seen as an indication that attention needs to be paid to patient selection and the time at which the patient is referred to an HBO therapy clinic The main reason behind all non healing wounds postoperative wounds soft tissue infections and diabetic foot wounds are lack of oxygen and the problem in wound healing processes HBO therapy attempts to restore healthy functioning of this process by providing the oxygen that tissue needs reducing edema controlling infections regulating intracellular metabolism and increasing the effectiveness of antibiotics In recent years the use of perioperative HBO therapy has also started to be suggested by publications 39 40 It is important to recognize the patient at risk during the preoperative period to identify early complications in the wound healing process during the postoperative period and to take the necessary precautions In addition to surgical nephrological and intensive care support HBO therapy can also be applied in severe energy traumas earthquake traffic accident industrial accident crush injuries compartment syndrome risky flap graft and organ replantation The main pathology in all of these diseases is ischemia and tissue edema While the increase of edema causes vicious circle by increasing hypoxia in the tissue reduction of edema supply of needed oxygen to the tissue re provision of microcirculation elimination of hypoxia and breaking of the cycle can be achieved with HBO therapy Unlike normobaric oxygen HBO therapy can enhance tissue viability and reduce the need for amputation by increasing the amount of dissolved oxygen in the plasma reducing the need for operations shortening the duration of hospitalization and preventing the risk of hospital infection 41 44 Plastic Surgery and Hyperbaric Oxygen Therapy In addition to diabetic foot wounds postoperative wounds compromised grafts flaps organ replantation HBO therapy can also be useful in the prevention and relief of complications of medical aesthetic applications 2 40 44 47 In risky grafts and flaps HBO therapy supports preoperative site preparation control of infections reduction of graft flap edema during postoperative period increase of collagen production and reduction of rejection 44 46 237
stanbul Med J 2020 21 4 234 41 Successful HBO therapy practices have been reported following replantations of tissue losses such as ear amputation and penile amputation The replanted tissue continues to be fed with dissolved oxygen from microcirculation and merges with healthy tissue 47 48 After filling applications to replace the tissue loss on the face caused by aging sudden vision loss and tissue necrosis may develop and HBO therapy may be applied to these types of cases HBO therapy reduces edema in the filling area is useful in correcting hypoxia and reduces scar formation 48 49 Orthopedics and Hyperbaric Oxygen Therapy Indications of HBO therapy in orthopedics can be summarized as postoperative wound healing osteomyelitis and avascular necrosis Osteomyelitis is a pyogenic infection of the bone that can be difficult to treat progressive and recurrent Hypoxia ischemia and necrosis develop in the bone due to infection Furthermore the strong structure of the bone causes the infection to be controlled and the effectiveness of the antibiotic therapy to decrease in bone tissue 50 Surgery antibiotics sensitive to bone culture and HBO therapy are applied in the treatment From the point of view of Hyperbaric Medicine whatever the cause this is a kind of closed wound and local oxygen support is important in correcting hypoxia in the tissue controlling the infection and in remission of the disease HBO therapy removes hypoxia by correcting edema and microcirculation increases bactericidal activity of neutrophils with increased oxygen in tissue increases vascularization allows antibiotics to be transported and penetrated to the problem area and accelerates postoperative wound healing 50 52 Etiopathogenesis of avascular necrosis includes corticosteroids alcohol infections dysbaric conditions infiltrating diseases of the bone marrow coagulation defects autoimmune diseases Basically it is a bone disease which is associated with tissue edema due to decreased local blood circulation which leads to necrosis in the bone and creates the need for prosthetics in the later stages 53 55 In addition to bone drill operation HBO therapy also has the effect of reducing existing hypoxia and edema improving metabolism in bone tissue and regulating osteoclastic and blastic activity enabling bone tissue regeneration 54 56 59 In orthopedics HBO therapy can also be used for perioperative and postoperative wound healing 39 40 Vascular Surgery and Hyperbaric Oxygen Therapy Wounds related to peripheral artery disease accompanied or not by diabetes venous ulcers and sternum osteomyelitis following cardiac surgery are groups of patients that vascular surgeons and undersea physicians can follow together In cases where oxygen transport is restricted due to mechanical reasons such as peripheral artery disease and Buerger s disease even if the gold standard treatment is surgical HBO therapy carries oxygen needed for tissue regeneration dissolved in plasma and provides major factors for wound healing In addition reduction of carbon dioxide retention and residual substances will reduce claudication and decrease the limitation of the patient s ability to activity 37 60 63 Because of this effect it is possible to stop the deterioration of the tissue and wound during the preoperative period 238 and to recover faster both the existing wound and the operation wound during the postoperative period In ulcers that develop due to venous insufficiency surgical intervention restriction of patient standing time elastic bandages appropriate varicose veins as well as the application of HBO therapy will accelerate wound healing HBO therapy plays an active role in reducing local edema in the development of granulation tissue in the wound and in accelerating epithelization and provides wound healing 2 31 63 In addition to the treatment of sternal infections and osteomyelitis that develop after cardiothoracic surgery HBO therapy can be used HBO therapy with its effects such as reduction of hypoxia reduction of edema support of immune resistance of the patient increase of antibiotic effectiveness reduces the duration of antibiotic therapy in this disease and reduces relapses 64 67 Radiation Oncology and Hyperbaric Oxygen Therapy While in radiotherapy RT the target is cancerous tissue neighboring normal tissue is also damaged and suffers loss of healthy cells and capillary vessels In tissue that has lost its cells and blood supply fibrosis develops accompanied by hypoxia The tissue in this condition has problems in healing due to a surgical intervention trauma or a spontaneous wound Osteonecrosis of the jaw after RT applied in head and neck cancers radiation cystitis after RT applied in genital region cancers proctitis can be given as an example of these diseases HBO therapy removes hypoxia in the tissue in these diseases speeding up new cell construction collagen production and angiogenesis neovascularization 2 68 72 According to the Marx protocol giving HBO therapy prior to surgery such as tooth extraction especially to the patient who has received RT due to head and neck cancer provides protection from osteoradionecrosis 69 Eye Diseases and Hyperbaric Oxygen Therapy Retinal artery occlusion is one of the emergency indications by both ophthalmologists and undersea physicians It is characterized by sudden blindness that develops immediately following occlusion of the retinal artery and its branches due to reasons such as thrombus embolism vasculitis The aim should be to reduce or dissolve the thrombus embolism to restore circulation and to provide tissue nutrition with the help of collaterals or diffusion until this is achieved Retinal cells are very sensitive to hypoxia Therefore HBO therapy should be administered very quickly in such cases 2 73 74 Otolaryngology and Hyperbaric Oxygen Therapy Sudden hearing loss malignant otitis externa and postoperative wound healing are indications that otolaryngology will be supported by undersea physicians Sudden hearing loss is defined as greater than 30 decibels sensorineural hearing reduction over at least three contiguous frequencies occurring over 3 days or less 75 In etiology vascular causes viral cochleitis autoimmune diseases and acoustic trauma can be considered The common feature of all these causes is hypoxia in the inner ear 75 76 HBO therapy which is added to steroid therapy corrects hypoxia in
F sun Kocaman r t k Current Approach in Hyperbaric Oxygen Therapy the inner ear reduces edema reactivates cells whose metabolism has stopped and restores hearing 2 75 77 Otitis externa is a life threatening progressive infection of the soft tissue of the external ear canal Patients may have diseases such as diabetes immunosuppressive use or cancer HBO therapy when added to appropriate antibiotics regresses edema in the outer ear tract increases the effectiveness of antibiotics strengthens body defense mechanisms provides remission of osteomyelitis in bone tissue HBO therapy should be considered as an adjuvant therapy pathway especially in resistant cases 78 79 Neurosurgery and Hyperbaric Oxygen Therapy Spondylodiscitis and intracranial abscesses are in neurosurgical indications where HBO therapy is used Intracranial abscesses are formed by aerobic and anaerobic agents in the brain tissue HBO therapy reduces edema around the abscess acts bactericidal to anaerobic microorganisms inside the abscess reduces hypoxia increases antibiotic penetration strengthens body defense mechanisms and helps control the infection in the abscess HBO therapy may be useful especially if any of these parameters are present 51 80 81 Multiple abscesses Deep and large abscess Early stage abscess that does not require surgery High risk patient profile Non surgical risky abscess Anaerobic or multiple bacterial isolation Failure to respond to standard treatment As a result HBO therapy is a treatment that has hyperoxic edema reducing infection fighting immune system supporting neovascularization enhancing inflammation reducing wound healingaccelerating effects In the light of scientific studies a new effect is emerging every day and the list of diseases it can treat is expanding With the new data to be added to the literature in the coming years it can be seen that this branch of science is very open to development and progress and in its current form it can take place in the treatment protocols of many diseases from different clinics 4 Kindwall EP Hyperbaric oxygenation general considerations A history of hyperbaric medicine Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 1 16 5 Hardy K The physics of hyperbaric oxygen therapy Neuman TS Thom SR editors Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia Saunders Elsevier 2008 p 57 64 6 Welslau W Physics of hyperbaric pressure Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer 2006 p 15 24 7 Hammarlund C Hyperbaric oxygenation general considerations The physiologic effects of hyperbaric oxygen Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 17 32 8 Welslau W Physiologic effects of increased barometric pressure Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 31 48 9 Ratzenhofer Komenda B Fovory R Welslau W Somlle J ttner FM Mathieu D Physiologic effects of hyperbaric oxygen transport and tissue oxygen pressure Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 49 74 10 UHMS Moon RE editor Hyperbaric Oxygen Therapy Indications 14th Edition Best Publishing Company 2019 11 Mathieu D Marroni A Kot J Consensus Conference Diving and Hyperbaric Medicine 2017 47 24 32 12 Sa l k Uygulama Tebli i 05 07 2018 tarih ve 30469 M kerrer Say l Resmi Gazete Ek 2 D 3 2013 Available from URL https www resmigazete gov tr eskiler 2018 07 20180705M1 1 htm 13 Elliott DH Disorders approved for treatment with hyperbaric oxygen Decompression sickness Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 311 26 14 Moon RE Gorman DF Decompression sickness Neuman TS Thom SR editors Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia Saunders Elsevier 2008 p 283 320 15 Marroni A Cronje FJ Meintjes J Cali Corleo R Dysbaric Illness Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 173 216 16 Vann RD Butler FK Mitchell SJ Moon RE Decompression illness Lancet 2011 377 153 64 17 Hoesen KV Neuman TS Gas embolism venous and arterial gas embolism Neuman TS Thom SR editors Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia Saunders Elsevier 2008 p 257 81 18 Mathieu D Tissier S Boulo ML Gas embolism Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 217 38 Peer review Internally peer reviewed 19 Kindwall EP Disorders approved for treatment with hyperbaric oxygen Gas embolism Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 327 42 Financial Disclosure The author declared that this study received no financial support 20 Malik N Claus PL Illman JE Klingerman SJ Moynagh MR Levin DL et al Air embolism diagnosis and management Future Cardiol 2017 13 365 78 References 21 Tritapepe L Macchiarelli G Rocco M Scopinaro F Schiallaci O Mastuscelli E et al Functional and ultrastructural evidence of myocardial stunning after acute carbon monoxide poisoning Crit Care Med 1998 26 797 801 Ethics 1 Clarke D History of hyperbaric therapy Neuman T Thom S editors Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia Saunders Elsevier 2008 p 3 23 2 im it M Hiperbarik T p stanbul T rkiye Efil Yay nevi 2009 3 Wattel F A history of hyperbaric medicine Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer 2006 p 1 11 22 Song L Bian G Yang W Li HF Variant angina induced by carbon monoxide poisining Medicine Baltimore 2019 98 16 23 Satran D Henry CR Adkinson C Nicholson CI Bracha Y Henry TD Cardiovascular manifestations of moderate to severe carbon monoxide poisining J Am Coll Cardiol 2005 45 1513 6 239
stanbul Med J 2020 21 4 234 41 24 Mathiue D Mathieu Nolf M Linke JC Favory R Wattel F Carbon monoxide poisining Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 239 62 43 Jain KK Hyperbaric oxygenation in traumatology and orthopedics Kain JJ editor Textboof of Hyperbaric Medicine 6th ed Cham Springer International Publishing 2017 p 429 42 25 Weaver LK Carbon monoxide poisoning Crit Care Clin 1999 15 297 317 44 Mesimeris TA Comprimised skin graft and falp Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 329 62 26 Kao LW Na agas KA Carbon monoxide poisoning Emerg Med Clin North Am 2004 22 985 1018 27 Hampson NB Dunford RG Kramer CC Norkool DM Selection criteria utilized for hyperbaric oxygen treatment of carbon monoxide poisoning J Emerg Med 1995 13 227 31 28 Huang CC Ho CH Chen YC Lin HJ Hsu CC Wang JJ et al Hyperbaric oxygen therapy is associated with lower short and long term mortality in patients with carbon monoxide poisoning Chest 2017 152 943 53 29 Eichcorn L Thudium M J ttner B The diagnosis and treatment of carbon monoxide poisining Dtsch Arztebl Int 2018 115 863 70 30 Knighton DR Mechanisms of wound healing Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 119 40 31 Jain KK HBO therapy in wound healing plastic surgery and dermatology Kain JJ editor Textboof of Hyperbaric Medicine Sixth Ed Cham Springer International Publishing 2017 p 183 206 32 Tapias LF Wright CD Lanuti M Muniappan A Deschler D Mathisen DJ Hyperbaric oxygen in the prevention and management of tracheal and oesophageal anastomotic complications Eur J Cardiothorac Surg 2020 57 1203 9 45 Nemiroff PM Disorders approved for treatment with hyperbaric oxygen Hyperbaric oxygen in skin grafts and flaps Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 565 80 46 Zamboni WA Baynosa RC Comprimised grafts and flaps Neuman TS Thom SR editors Physiology and Medicine of Hyperbaric Oxygen Therapy Philadelphia Saunders Elsevier 2008 p 373 96 47 Shapell HW Kislevitz M Reddy G Amirlak B Morey A Successful replantation of amputated penis with adjuvant hyperbaric oxygen therapy Undersea Hyperb Med 2019 46 695 9 48 Mass CS Complications in the cosmetic Office setting Complications in facial plastic surgery Capone RB Sykes JM editors New York Thieme Medical Publishers Inc 2012 p 10 6 49 Hwang K Hyperbaric oxygen therapy to avoid blindless from filler injection J Craniofac Surg 2016 27 2154 5 50 Kemmer A Stein T Heirholzer C Persistent osteomyelitis Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 429 50 33 Ramsey SD Newton K Blough D McCulloch DK Sandhu N Reiber GE et al Incidence outcomes and cost of foot ulcers in patients with diabetes Diabetes Care 1999 22 382 7 51 Britt MW Calhoun J Mader JT Mader JP Disorders approved for treatment with hyperbaric oxygen The use of hyperbaric oxygen in the treatment of osteomyelitis Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 419 28 34 Eleftheriadou I Kokkinos A Liatis S Makrilakis K Tentolouris N Tentolouris A et al Atlas of the Diabetic Foot Third ed New Jersey Wiley Blackwell 2019 52 Kirby JP Hyperbaric oxygen therapy as an elective treatment Mo Med 2019 116 184 7 35 Boulton AJ Armstrong DG Albert SF Frykberg RG Hellman R Kirkman MS et al American Diabetes Association America Association of Clinical Endocrinologists Comprehensive foot examination and risk assessment a report of the task force of the foot care interest group of American Diabetes Association with endorsement by the American Association of Clinical Endocrinologist Diabetes Care 2008 31 1679 85 53 Ditri L Montanari Y Melamed Y Reis D Femoral head necrosis Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 547 52 36 Kaya A Aydin F Altay T Karapinar Levent Ozturk Hasan Karakuzu Cengiz Can major amputation rates be decreased in diabetic foot ulcers with hyperbaric oxygen therapy Int Orthop 2009 33 441 6 37 Goldman RJ Hyperbaric oxygen therapy for wound healing and limb salvage a systematic review PM R 2009 1 471 89 54 Assouline Dayan Y Chang C Greenspan A Shoenfeld Y Gershwin ME Pathogenesis and natural history of osteonecrosis Semin Arthritis Rheum 2002 32 94 124 55 Shier A Abdelrazek M Soliman A De Sanctis V Elsayed A Abdulla M et al Short term outcome and MRI changes in three adult patients with sickle cell disease and aseptic osteonecrosis after treatment with hyperbaric oxygen threrapy a preliminary report Case Rep Oncol 2020 13 365 72 38 Liu R Li L Yang M Boden G Yang G Systematic review of the effectiveness of hyperbaric oxygenation therapy in the management of chronic diabetic foot ulcers Mayo Clin Proc 2013 88 166 75 56 Bosco G Vezzani G Mrakic Sposta S Rizzato A Enten G Abou Samra A et al Hyperbaric oxygen therapy ameliorates osteonecrosis in patients by modulating inflammation and oxidative stress J Enzyme Inhib Med Chem 2018 33 1501 5 39 Boet S Martin L Cheng Boivin O Etherington N Louge P Pignel R et al Can preventive hyperbaric oxygen therapy optimise surgical outcome A systematic review of randomised controlled trials Eur J Anaesthesiol 2020 37 1 13 57 Ververidis AN Paraskevopoulos K Keskinis A Ververidis NA Molla Moustafa R Tilkeridis K Bone marrow edema syndrome transient osteoporosis of the hip joint and management with the utilization of hyperbaric oxygen therapy J Orthop 2020 22 29 32 40 Friedman T Menashe S Landau G Sherf M Wiser I Seligman Y et al Hyperbaric oxygen preconditioning can reduce postabdominoplasty complications a retrospective cohort study Plast Reconstr Surg Glob Open 2019 7 e2417 58 Baig SA Baig MN Osteonecrosis of the femoral head etiology investigations and management Cureus 2018 10 e3171 41 Torp KD Murphy Lavoie HM Acute traumatic ischemia hyperbaric evaluation and treatment In StatPearls Treasure Island FL StatPearls Publishing 2020 42 Garcia Covarrubias L McSwain NE Jr Van Meter K Bell RM Adjuvant hyperbaric oxygen therapy in the management of crush injury and traumatic ischemia an evidence based approach Am Surg 2005 71 144 51 240 59 Li W Ye Z Wang W Wang K Li L Zhao D Clinical effect of hyperbaric oxygen therapy in the treatment of femoral head necrosis a systematic review and meta analysis Orthopade 2017 46 440 6 60 Nakamura H Makiguchi T Atomura D Yamatsu Y Shirabe K Yokoo S Changes in skin perfusion pressure after hyperbaric oxygen therapy following revascularization in patients with critical limb ischemia a preliminary study Int J low Extrem Wounds 2020 19 57 62
F sun Kocaman r t k Current Approach in Hyperbaric Oxygen Therapy 61 Conte MS Bradbury AW Kohl P White JV Dick F Fitridge R et al Global vascular guidelines on the management of chronic limb threatening ischemia Eur J Vasc Endovasc Surg 2019 58 1 109 62 Heyboer M Grant WD Byrne J Pons P Morgan M Igbal B et al Hyperbaric oxygen for the treatment of nonhealing arterial insufficiency ulcers Wound Repair and Regen 2014 22 351 5 63 R oeckl Wiedmann I Bennett M Kranke P Systematic review of hyperbaric oxygen in the management of chronic wounds British Journal of Surgery 2005 92 24 32 64 Yu WK Chen YW Shie HG Lien TC Kao HK Wang JH Hyperbaric oxygen therapy as an adjunctive treatment for sternal infection and osteomyelitis after sternotomy and cardiothoracic surgery J Cardiothorac Surg 2011 6 141 65 Shields RC Nichols FC Buchta WG Claus PL Hyperbaric oxygen therapy for chronic refractory osteomyelitis of the sternum Ann Thorac Surg 2010 89 1661 3 66 Barili F Polvani G Topkara VK Dainese L Cheema FH Roberto M et al Role of hyperbaric oxygen therapy in the treatment of postoperative organ space sternal surgical site infections World J Surg 2007 31 1702 6 67 Mills C Bryson P The role of hyperbaric oxygen in the treatment of sternal wound infection Eur J Cardiothorac Surg 2006 30 153 9 68 Pasquier D Schmutz J Lartigau E Radio induced lesion in normal tissues Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 363 400 69 Marx RE Disorders approved for treatment with hyperbaric oxygen Radiation injury to tissue Kindwall EP editor Hyperbaric Medicine Practice Arizona Best Publishing Company 1995 p 447 504 70 Feldmeier JJ Principles of wound management Poblem wounds the irradiated wound Sheffield PL Smith APS Fife C editors Wound Care Practice Arizona Best Publishing Company 2004 p 369 88 71 Marx RE Johnson RP Kline SN Prevention of osteoradionecrosis a randomized prospective clinical trial of hyperbaric oxygen versus penicillin JADA 1985 111 49 54 72 Junior LHF Limirio PHJO Soares PBF Dechichi P De Souza Castro Filice L Quagliatto PS et al The effect of hyperbaric oxygen therapy on bone macroscopy composition and biomechanical properties after ionizing radiation injury Radiat Oncol 2020 15 95 73 Weinberger A Siekmann U Acute ischemic ophthalmological disorders Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 527 36 74 Beiran I Goldberg I Adir Y Tamir A Shupak A Miller B Early hyperbaric oxygen therapy for retinal artery occlusion Eur J Ophtalmol 2001 11 345 50 75 Bagli BS Clinical efficiancy of hyperbaric oxygen therapy on idiopathic sudden sensorineural hearing loss Undersea Hyperb Med 2020 47 51 6 76 Bayoumy AB De Ru JA The use of hyperbaric oxygen in acute hearing loss a narrative review Eur Arch of Otorhinolaryngol 2019 276 1859 80 77 K rpinar S Alkan Z Yi it O G r AP Toklu AS Cakir B et al Factors influencing the outcome of idiopathic sudden sensorineural hearing loss treated with hyperbaric oxygen therapy Eur Arch Otorhinolaryngol 2011 268 41 7 78 Barthelemy A Rocco M Sudden deafness Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 451 68 79 Amaro CE Espiney R Radu L Guerreiro F Malignant necrotizing externa otitis the experience of a single hyperbaric centre Eur Arch Otorhinolaryngol 2019 276 1881 7 80 Lampl L Frey G Intra cranial abscess Mathieu D editor Handbook on Hyperbaric Medicine Dordrecht Springer International Publishing 2006 p 291 304 81 Kutlay M Colak A Y ld z S Demircan N Ak n ON Stereotactic aspiration and antibiotic treatment combined with hyperbaric oxygen therapy in the management of bacterial brain abscesses Neurosurgery 2008 2 540 6 241
COVID 19 update The evolving use of hyperbaric oxygen therapy during the COVID 19 pandemic Abstract The Sars CoV 2 COVID 19 pandemic has resulted in significant and unprecedented shifts in the delivery of health care services in the United States Although wound care remains an essential service during the COVID 19 pandemic the financial consequences and infectious disease ramifications of the pandemic have resulted in closure or limitation of hours in many outpatient wound and hyperbaric oxygen therapy HBOT centers As HBOT patients often require daily treatment sessions for a period of months it is necessary for facilities providing HBOT services to adjust to the COVID 19 pandemic while still maintaining availability of this important service Modification of HBOT session timing and chamber decontamination procedures utilisation of telehealth services for initial patient evaluations and acceptance of novel patient populations and diagnoses are mechanisms by which HBOT centers can adapt to the evolving model of health care delivery throughout a pandemic While COVID 19 is not a currently accepted indication for HBOT patients may be referred for HBOT consultation due to the post infectious sequelae of the virus and thus HBOT facilities must be aware of the potential uses of this treatment for post viral complications By redefining paradigms for health care delivery during the COVID 19 pandemic HBOT and wound centers can continue to provide highquality and uninterrupted care to vulnerable patient populations Declaration of interest The authors have no conflicts of interest to declare H yperbaric oxygen therapy HBOT is a treatment modality in which patients are enclosed in a hyperbaric chamber that enables inhalation of 100 oxygen at 2 3 times atmospheric pressure 1 HBOT may be performed in a monoplace single person occupancy or multiple multiple person occupancy chamber in the United States most hyperbaric chambers are located within hospital settings HBOT is utilised for a variety of medical conditions and can be especially helpful in the treatment of the complex chronic wound patient 1 Sequential administration of hyperbaric oxygenation can promote neovascularisation of the wounded territory and allow for limb salvage in patients who under other circumstances would face amputation 1 Interruptions in HBOT may have potentially devastating effects with progression to amputation leading to significantly increased risk of morbidity and mortality In the United States the Centers for Medicare and Medicaid Services CMS has advocated for increased delivery of care through telemedicine or in the home environment during the SARS CoV 2 COVID 19 pandemic 2 In wound care these recommendations are difficult to follow as best practices are heavily dependent on in clinic procedures 2 Over the course of the COVID19 pandemic wound care centres have temporarily Areeg A Abu El Hawa 1 BS Karina Charipova 1 BS Jenna C Bekeny 2 BA Kelly K Johnson Arbor 1 2 MD Corresponding author email kkja me com 1 Georgetown University School of Medicine Washington District of Columbia 2 Department of Plastic and Reconstructive Surgery MedStar Georgetown University Hospital Washington District of Columbia S8 closed or restricted their hours in response to directions from the CMS and other governing bodies 3 Wound care centres including HBOT centres are frequently located within hospitals that have implemented containment strategies including restrictions on visitors and the provision of outpatient services due to the COVID 19 pandemic Unfortunately eliminating or significantly reducing the ability to deliver quality care to wounded patients a large proportion of whom have multiple chronic comorbid conditions such as diabetes puts this fragile cohort at even greater risk for medical complications during the pandemic As a result of the COVID 19 pandemic patients with chronic diseases have experienced adverse health effects including missed routine medical appointments and testing 3 In one survey of healthcare professionals worldwide 67 of respondents reported that their patients had experienced moderate or severe effects due to COVID19 related changes in healthcare services diabetes was the most common condition affected by these changes 4 The Alliance of Wound Care Stakeholders the Alliance is a not for profit organisation that promotes advocacy and outreach regarding wound care in the United States In March 2020 the Alliance published a position statement in support of the classification of wound care departments as an essential service 5 In its statement the Alliance argued that even if clinic visits are limited and transitioned to telehealth wound care departments should stay open in order to provide urgent wound care that is infection sparing limbsalvaging and life saving 5 Our HBOT centre fully endorses this position statement and is in agreement with the determination made by the Alliance that by providing appropriate and timely wound care we are 2021 MA Healthcare Ltd coronavirus infections hyperbaric oxygenation infection control pandemic wound wound healing JOURNAL OF WOUND CARE NORTH AMERICAN SUPPLEMENT VOL 30 NO 2 FEBRUARY 2021 Downloaded from magonlinelibrary com by 104 028 029 066 on January 21 2022
COVID 19 update able to unburden other parts of the hospital system by preventing our patient population from needing to seek emergent care 5 The COVID 19 pandemic presents an unprecedented challenge to maintaining patient access to HBOT and has enabled swift yet carefully planned action at our tertiary wound care centre to ensure patient safety and to optimise wound outcomes The aim of this article is to describe our approach to HBOT over the course of the pandemic and to highlight implications for our patient population 2021 MA Healthcare Ltd New approach to HBOT Patient triage Considering restrictions placed on our hospital system because of COVID 19 our HBOT team was faced with the difficult task of balancing both continuity of care and the safety of staff and patients During the earlier months of the pandemic the American College of Surgeons published COVID 19 guidelines for the triage of patients in departments such as vascular surgery however no such guidelines were established specific to HBOT 6 We designed an internal system of triage to assist in the decision making process to determine which patients should be encouraged to continue HBOT pause treatment or initiate treatment during the pandemic One of the hurdles we encountered during initial discussions of triage is a core tenet of HBOT scheduling Successful treatment with HBOT at our center requires both the ability to deliver care every weekday and the willingness of patients to commit to a daily two hour treatment session for up to three months Due to the significant medical comorbidities found in a majority of the HBOT patient population the risks of travel back and forth to the hospital for daily hyperbaric treatments may be significant The medical conditions associated with a higher risk of severe disease or death due to COVID 19 including diabetes hypertension and coronary artery disease are also present in many patients who undergo HBOT 7 At the start of the pandemic we were faced with substantial albeit reasonable hesitation and apprehension on the part of our patients with regards to coming to the hospital on a daily basis for treatment including concerns about the availability of personal protective equipment PPE and the risks of travel in the context of regional stay at home orders To address these patient concerns initial hyperbaric patient evaluations were performed via video assisted telehealth visits whenever possible While telehealth visits were implemented with relative ease in our practice we acknowledge the difficulties associated with the transition to virtual patient care Fortunately we did not encounter significant obstacles to insurance reimbursement patient access to telehealth platforms or other technology related complications for these initial telehealth visits After a stay at home order was issued for the District of Columbia at the end of March 2020 a decision was made to only utilise HBOT for emergent or urgent indications These patients included those whose conditions were deemed to have the potential to significantly worsen if ongoing treatment was paused or new treatment was not initiated Prior to the stay athome order our HBOT centre treated from 8 12 patients daily of both inpatient and outpatient status with a wide variety of hyperbaric indications Upon initiation of the stay at home order our patient census was reduced to individuals with urgent or emergent conditions including acute skin graft or flap necrosis and sudden sensorineural hearing loss As the stay athome order included a temporary moratorium on elective surgical procedures our inpatient HBOT volume which had previously largely involved the perioperative treatment of limb salvage patients was essentially eliminated We established a new core outpatient hyperbaric cohort in which most patients had urgent or emergent indications as delineated above During this initial time of transition we also experienced new patient referrals from outside of our local geographic region since at least one other HBOT centre in our region had closed to outpatient care due to concerns related to infection control in the multiplace hyperbaric environment Clinic redesign Our HBOT suite contains four monoplace hyperbaric chambers and is located within the multidisciplinary wound care center of our institution Prior to the pandemic this location served as a hub for all of the members of the multidisciplinary wound care team including the departments of plastic surgery vascular surgery podiatry and rheumatology This layout enabled centralisation of care for every wounded patient facilitating rapid collaboration for both evaluation and treatment Prior to the COVID 19 pandemic our facility served patients Monday through Friday With this form of scheduling our practice served up to 12 patients on any given day with four hyperbaric chambers running treatments up to three times per day As a result of careful planning our practice was able to maintain its Monday through Friday schedule A decision was made to decrease the number of daily treatment sessions from 3 to 2 to allow for adequate time between patient cohorts to clean the facility Around the time of the initiation of the District of Columbia s stay at home order the hyperbaric technicians began to manually disinfect the interior of each hyperbaric chamber following every use Prior to the COVID 19 pandemic this process had been performed on a weekly basis as part of a routine chamber maintenance schedule Each manual disinfection process which utilised cleaning products and instructions recommended by the chamber manufacturer lasted approximately 10 minutes in duration After chamber disinfection the hyperbaric chamber was pressurised to a standard treatment depth 2 0 atmospheres absolute for an additional 10 minutes JOURNAL OF WOUND CARE NORTH AMERICAN SUPPLEMENT VOL 30 NO 2 FEBRUARY 2021 S9 Downloaded from magonlinelibrary com by 104 028 029 066 on January 21 2022
to fully ventilate the chamber and allow for off gassing of the disinfectant vapors All hard surfaces within the HBOT suite including hyperbaric gurneys countertops and vital sign monitors were disinfected between patient visits Additionally the hyperbaric changing room including lockers and seating surfaces was disinfected between each patient s use of the area These enhanced cleaning measures provided an additional margin of safety for reduction of potential virus transmission in the hyperbaric environment however the additional time required for the disinfecting process necessitated a change in the daily patient scheduling process to allow for increased time intervals between patients New patient population Despite the logistical challenges encountered by our HBOT practice during COVID 19 the pandemic also enabled us to expand our services to benefit a new patient population Our approach to patient triage and the redesign of our clinic space allowed us to provide care to patients who had no other HBOT options due to temporary location closure As a result of these treatment centre closures our facility remained the only HBOT center in the region capable of treating pediatric patients We experienced a significant increase in pediatric referrals for HBOT during the initial months of the pandemic mostly for treatment of acutely compromised skin grafts and flaps Although the local District of Columbia government had restricted the performance of elective procedures in our region the pandemic spread throughout the United States at different rates and thus other jurisdictions did not have the same limitations on outpatient surgical procedures during this time Due to this we received multiple referrals for the hyperbaric treatment of pediatric patients who lived in our region and who were scheduled to undergo or who had already undergone surgical procedures in different areas of the United States These patients were initially evaluated via telehealth platforms hyperbaric education and initial chamber orientation were provided to the children s parents via video conference as well As many of the new paediatric patients experienced daily commutes of an hour or more to reach our facility we attempted to time the HBOT treatments around the childrens naptimes While the hospital had visitor restrictions in place during the pandemic paediatric patients could have a single caregiver accompany them into the facility and remain close to them for the duration of each hyperbaric treatment Due to concerns for infection control and the lack of overall data regarding the use of HBOT as a treatment for COVID 19 our HBOT facility elected to not treat patients who were diagnosed with acute COVID 19 infection Recently published case reports and small single institution studies have proposed that HBOT can be used to improve hypoxemia and prevent transition to mechanical ventilation in COVID 19 patients 8 9 A S10 randomised controlled trial currently underway at the Assaf Harofeh Medical Center in Israel ClinicalTrials gov Identifier NCT04358926 is investigating the efficacy of HBOT in moderate severe COVID 19 patients 10 A similar study is being carried out by the Ochsner Health System in New Orleans Louisiana NCT04343183 11 At NYU School of Medicine in New York HBOT was used to treat 20 patients with respiratory distress due to COVID 19 infection The results of this study indicated that HBOT can be utilised to safely treat patients with COVID 19 infection although the results were limited by a small enrollment size and limited inclusion criteria 12 It is hypothesised that alternate treatment strategies such as HBOT and the delivery of erythropoiesis stimulating agents may therefore have the potential to increase oxygenation of tissue by means other than standard respiratory and ventilator support 13 While these preliminary data are promising when evaluating these findings it is essential to take into consideration the logistics and possible adverse effects of HBOT including the risk of oxygen toxicity the concern for virus aerosolisation in the hyperbaric environment and practical issue of isolation from other necessary medical interventions during this time 14 In August 2020 the Undersea Hyperbaric Medical Society UHMS issued a statement concluding that while well designed clinical trials are necessary to establish a proper clinical foundation for the treatment of COVID 19 the use of HBO on an off protocol basis may be appropriate in some cases 15 While we fully endorse the exploration of ways in which HBOT can be used to treat patients during the ongoing pandemic the use of HBOT for the treatment of acute COVID 19 infection remains experimental at this time While our HBOT centre has not treated patients with acute COVID 19 infection during the pandemic we did experience increased physician initiated referrals for treatment of patients who experienced chronic sequelae which were temporally related to previous COVID 19 infection These referrals included patients with acute peripheral lower extremity ischemia sudden sensorineural hearing loss acute anaemia with inability to receive transfusion due to religious beliefs and anosmia dysgeusia these patients were diagnosed with these conditions during or soon after their diagnosis of COVID 19 was established In addition we received patient initiated referrals from individuals who were interested in receiving HBOT as a treatment for persistent fatigue and malaise after COVID 19 infection fatigue as well as dyspnea are the most commonly reported long term health consequences reported after acute COVID 19 infection 16 As the chronic sequelae of COVID 19 are largely poorly understood at this time it is unclear whether HBOT is a viable treatment for these COVID 19 related conditions Additionally in the United States there are limitations in insurance coverage for the post COVID 19 conditions which do not align with the traditionally accepted indications for HBOT In some cases workers compensation plans may cover the 2021 MA Healthcare Ltd COVID 19 update JOURNAL OF WOUND CARE NORTH AMERICAN SUPPLEMENT VOL 30 NO 2 FEBRUARY 2021 Downloaded from magonlinelibrary com by 104 028 029 066 on January 21 2022
COVID 19 update use of HBOT for patients who contracted COVID 19 due to workplace exposure e g healthcare workers We continue to explore whether HBOT is a potential effective treatment for the chronic sequelae of COVID 19 Impact Despite the challenges associated with the COVID 19 pandemic our HBOT centre was able to remain open during the duration of the District of Columbia s stay athome order in 2020 In doing so we were able to provide continuing care to multiple patients who would otherwise have not been able to receive this treatment due to temporary closures at other HBOT centres in the region Unfortunately even with the modifications our HBOT team made to adapt to the pandemic our practice was unable to function at its full capacity throughout this time There were certain limitations to care during the pandemic some patients were unable to continue care at our facility due to restrictions in non emergency medical transport services and there were occasional difficulties in obtaining insurance prior authorisation for hyperbaric treatments related to communication delays with insurance representatives who were teleworking Even as restrictions in the District of Columbia are being lifted our practice continues to encounter obstacles and redefine our approach in this new era of patient care Our HBOT center began to schedule our routine patient population in the middle of June 2020 Within the first day of adding patients to an expanded treatment schedule it became evident that some patients who had previously received care regularly at our center were unable to continue with the treatment as they were still sheltering in place away from the District of Columbia other patients voiced concerns regarding their safety when returning to the hospital for care and many patients required new insurance prior authorizations for HBOT as their previous authorisations dates of service had expired due to the interruption in treatment For the most part these obstacles have been resolved and as of October 2020 we are experiencing patient volumes which approximate our pre COVID 19 numbers Conclusion The COVID 19 pandemic resulted in significant shifts to the provision of inpatient and outpatient medical services given the sustained increases in cases occurring across the United States the healthcare community will likely be operating under the pandemic model of care for the foreseeable future As wound care has remained an essential service throughout the pandemic it is imperative for physicians and healthcare facilities to define paradigms for care for patients who require treatment with HBOT during this time By understanding the ways in which medical facilities have adapted to provide care to patients during the pandemic HBOT facilities can continue to optimise our delivery of patient care and provide uninterrupted access to hyperbaric medicine services during this challenging time JWC 2021 MA Healthcare Ltd References 1 Benedict Mitnick CD Johnson Arbor K Atypical wounds Hyperbaric oxygen therapy Clin Podiatr Med Surg 2019 3 6 3 525 533 https doi org 10 1016 j cpm 2019 02 008 2 Rogers L How podiatrists can navigate the shifting model of wound care during the COVID 19 pandemic PodiatryToday https www podiatrytoday com blogged how podiatrists can navigate shiftingmodel wound care during covid 19 pandemic accessed June 30 2020 3 Saqib MA Siddiqui S Qasim M et al Effect of COVID 19 lockdown on patients with chronic diseases Diabetes Metab Syndr 2020 14 6 1621 1623 https doi org 10 1016 j dsx 2020 08 028 4 Chudasama YV Gillies CL Zaccardi F et al Impact of COVID 19 on routine care for chronic diseases A global survey of views from healthcare professionals Diabetes Metab Syndr 2020 14 5 965 967 https doi org 10 1016 j dsx 2020 06 042 5 Alliance of Wound Care Stakeholders Wound care is an essential not elective service that prevents hospital admissions and ED visits among a fragile cohort of patients at high risk of COVID 19 https www woundcarestakeholders org images Final2_Statement_ _Wound_Care_ as_Essential pdf accessed June 30 2020 6 American College of Surgeons COVID 19 guidelines for triage of vascular surgery patients Elective case triage guidelines for surgical care https www facs org covid 19 clinical guidance elective case vascular surgery accessed June 30 2020 7 Chow N Fleming Dutra K Gierke R et al CDC COVID 19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 United States February 12 March 28 2020 MMWR Morb Mortal Wkly Rep 2020 69 13 382 386 https doi org 10 15585 mmwr mm6913e2 8 Thibodeaux K Speyrer M Raza A et al Hyperbaric oxygen therapy in preventing mechanical ventilation in COVID 19 patients a retrospective case series J Wound Care 2020 29 Sup5a S4 S8 9 Guo D Pan S Wang M Guo Y Hyperbaric oxygen therapy may be effective to improve hypoxemia in patients with severe COVID 2019 pneumonia two case reports Undersea Hyperb Med 2020 47 2 181 187 https doi org 10 22462 04 06 2020 2 10 Assaf Harofeh Medical Center Hyperbaric oxygen therapy effect in COVID 19 RCT https clinicaltrials gov ct2 show NCT04358926 accessed October 17 2020 11 Undersea Hyperbaric Medical Society Hyperbaric oxygen and COVID 19 clinical trials registered on clinicaltrials gov https www uhms org images Position Statements HBO2_and_COVID_6 11 2020 pdf accessed June 30 2020 12 Gorenstein SA Castellano ML Slone ES et al Hyperbaric oxygen therapy for COVID 19 patients with respiratory distress treated cases versus propensity matched controls Undersea Hyperb Med 2020 Third Quarter 47 3 405 413 13 Geier MR Geier DA Respiratory conditions in coronavirus disease 2019 COVID 19 Important considerations regarding novel treatment strategies to reduce mortality Med Hypotheses 2020 140 109760 https doi org 10 1016 j mehy 2020 109760 14 Moon RE Weaver LK Hyperbaric oxygen as a treatment for COVID 19 infection EDITORIAL COMMENTARY Hyperbaric oxygen as a treatment for COVID 19 infection Undersea Hyperb Med 2020 47 2 177 179 https doi org 10 22462 04 06 2020 1 15 Undersea Hyperbaric Medical Society UHMS Position Statement Hyperbaric Oxygen HBO2 for COVID 19 Patients https www uhms org images Position Statements UHMS_PS_HBO2_for_COVID 19_ Patients_20200822 pdf accessed October 16 2020 16 del Rio C Collins LF Malani P Long term health consequences of COVID 19 JAMA 2020 Nov 324 17 1723 https doi org 10 1001 jama 2020 19719 Epub ahead of print JOURNAL OF WOUND CARE NORTH AMERICAN SUPPLEMENT VOL 30 NO 2 FEBRUARY 2021 S 11 Downloaded from magonlinelibrary com by 104 028 029 066 on January 21 2022
Hyperbaric Oxygen Therapy Can Improve Post Concussion Syndrome Years after Mild Traumatic Brain Injury Randomized Prospective Trial Rahav Boussi Gross1 Haim Golan3 4 Gregori Fishlev1 Yair Bechor1 Olga Volkov3 4 Jacob Bergan1 Mony Friedman1 Dan Hoofien6 7 Nathan Shlamkovitch8 Eshel Ben Jacob2 5 9 10 Shai Efrati1 2 3 10 1 The Institute of Hyperbaric Medicine Assaf Harofeh Medical Center Zerifin Israel 2 Research and Development Unit Assaf Harofeh Medical Center Zerifin Israel 3 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 4 Nuclear Medicine institute Assaf Harofeh Medical Center Zerifin Israel 5 The Raymond and Beverly Sackler Faculty of Exact Sciences School of Physics and Astronomy Tel Aviv University Tel Aviv Israel 6 Department of Psychology The Hebrew University of Jerusalem Jerusalem Israel 7 The National Institute for the Rehabilitation of the Brain Injured Tel Aviv Israel 8 Otolaryngology Head Neck Surgery Assaf Harofeh Medical Center Zerifin Israel 9 Center for Theoretical Biological Physics Rice University Houston Texas United States of America 10 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Abstract Background Traumatic brain injury TBI is the leading cause of death and disability in the US Approximately 70 90 of the TBI cases are classified as mild and up to 25 of them will not recover and suffer chronic neurocognitive impairments The main pathology in these cases involves diffuse brain injuries which are hard to detect by anatomical imaging yet noticeable in metabolic imaging The current study tested the effectiveness of Hyperbaric Oxygen Therapy HBOT in improving brain function and quality of life in mTBI patients suffering chronic neurocognitive impairments Methods and Findings The trial population included 56 mTBI patients 1 5 years after injury with prolonged postconcussion syndrome PCS The HBOT effect was evaluated by means of prospective randomized crossover controlled trial the patients were randomly assigned to treated or crossover groups Patients in the treated group were evaluated at baseline and following 40 HBOT sessions patients in the crossover group were evaluated three times at baseline following a 2 month control period of no treatment and following subsequent 2 months of 40 HBOT sessions The HBOT protocol included 40 treatment sessions 5 days week 60 minutes each with 100 oxygen at 1 5 ATA Mindstreams was used for cognitive evaluations quality of life QOL was evaluated by the EQ 5D and changes in brain activity were assessed by SPECT imaging Significant improvements were demonstrated in cognitive function and QOL in both groups following HBOT but no significant improvement was observed following the control period SPECT imaging revealed elevated brain activity in good agreement with the cognitive improvements Conclusions HBOT can induce neuroplasticity leading to repair of chronically impaired brain functions and improved quality of life in mTBI patients with prolonged PCS at late chronic stage Trial Registration ClinicalTrials gov NCT00715052 Citation Boussi Gross R Golan H Fishlev G Bechor Y Volkov O et al 2013 Hyperbaric Oxygen Therapy Can Improve Post Concussion Syndrome Years after Mild Traumatic Brain Injury Randomized Prospective Trial PLoS ONE 8 11 e79995 doi 10 1371 journal pone 0079995 Editor Jinglu Ai St Michael s Hospital University of Toronto Canada Received August 22 2013 Accepted October 4 2013 Published November 15 2013 Copyright 2013 Boussi Gross et al This is an open access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use distribution and reproduction in any medium provided the original author and source are credited Funding The study was supported by the research fund of Assaf Harofeh medical center by the Tauber Family Foundation and by the Maguy Glass Chair in Physics of Complex Systems at Tel Aviv University None of the supporting bodies had any role in study design data collection and analysis decision to publish or preparation of the manuscript Competing Interests The authors have declared that no competing interests exist E mail efratishai 013 net SE eshel rice edu EB J These authors contributed equally to this work dysfunction Intensive therapy and rehabilitation programs are considered essential for maximizing quality of life but are often just partially successful Clearly new methods for brain repair should be examined in order to provide sustained relief to brain damage patients Recent studies reported that hyperbaric oxygen treatment HBOT can induce neuroplasticity leading to significant neurological improvement in post stroke patients at the convalescent stage and at late chronic stages months to years after the acute event 3 4 Introduction Traumatic brain injury TBI and stroke are the major causes of brain damage Every year close to two million people in the US suffer TBI which is the leading cause of death and disability among the general population Stroke affects almost a million people and is the leading cause of inability to maintain independent life among adults 1 2 There is no effective treatment metabolic intervention in the daily clinical practice for post TBI and stroke patients with chronic neurological PLOS ONE www plosone org 1 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI function in animal models 26 27 28 29 30 The elevated oxygen levels can have a significant effect on the brain metabolism largely regulated by the glial cells see discussion Improved energy management leads to multifaceted repair including activation of angiogenesis and triggering of neuroplasticity reactivation of quiescent neurons creation of new synapses and new axonal connections and might even induce differentiation of neuronal stem cells 22 The idea that HBOT can promote brain repair is reasonable and has gained experimental support yet is still largely dismissed by the medical community as is discussed next Definitions and classifications Traumatic brain injury is defined as damage to the brain resulting from external mechanical force such as rapid acceleration or deceleration impact blast waves or penetration by a projectile Consequently to the injury brain function is temporarily or permanently impaired and structural damage may or may not be detectable with current imaging technology TBI is usually classified based on severity anatomical features of the injury and the cause of the injury The severity is assessed according to the loss of consciousness LOC duration the post traumatic amnesia PTA and the Glasgow coma scale GCS grading of the level of consciousness Approximately 70 90 of the TBI in the US are classified as mild TBI mTBI or concussion LOC duration of 0 30 minutes PTA duration of less than a day and GCS grade of 13 15 Post concussion syndrome PCS is a set of symptoms succeeding mTBI in most patients The PCS symptoms include headache dizziness neuropsychiatric symptoms and cognitive impairments 5 6 In most patients PCS may continue for weeks or months and up to 25 of the patients may experience prolonged PCS PPCS in which the symptoms last for over six months 7 8 9 10 11 12 Such individuals are at high risk for emotional and cognitive dysfunction culminating in inability to carry out ordinary daily activities work responsibilities and standard social relationships 9 10 11 12 The medical community reservations A study of the effect of hyperbaric oxygen treatment of severe brain injured patients has been published already two decades ago Several prospective clinical trials on treatment of mTBI have been published in the last decade 31 32 33 and three studies published in the last two years addressed the effect of HBOT on chronic mild TBI patients 34 35 36 However the reported beneficial effects of the hyperbaric treatment were severely questioned by the medical community and triggered high skepticisms to the extent that TBI and stroke patients in the US are rarely treated by hyperbaric oxygen The HBOT option has been dismissed by the medical community on the grounds of 1 Lack of knowledge about the connection between metabolism and neuroplasticity 2 Lack of randomized clinical trial with standard placebo control 3 Sham control with room air at 1 3Atm yielded significant improvements These issues are clarified and elaborated on in the discussion section Associated brain pathology and function impairments Diffuse axonal injury diffuse shearing of axonal pathways and small blood vessels is one of the most common pathological feature associated with mTBI 13 Another primary pathological feature usually caused by a direct hit to the skull is brain contusions which commonly involve the frontal and anterior temporal lobes 12 Secondary pathologies of mTBI include ischemia mild edema and other bio chemical and inflammatory processes culminating in impaired regenerative healing processes resulted from increasing tissue hypoxia 14 Due to the diffuse nature of injury cognitive impairments are usually the predominant symptoms involving deficiencies in several cognitive functions primarily memory attention processing speed and executive functions all localized in multiple brain areas Their potent functions rely on potent network structure and connectivity between different brain areas 12 15 16 We note that the diffuse nature of the mTBI injury renders the pathological damage hard to be detected by common neuroimaging methods such as CT and MRI so that diagnosis largely relies on subjective reports of the patients as well as cognitive and quality of life tests While diffusion tensor imaging DTI has the potential to detect diffuse axonal injuries this method is still not commonly used for diagnosis of mTBI pathology The placebo dilemma People can sense a pressure increase beyond 1 3Atm hence standard placebo with normal air pressure for HBOT could perhaps be attained by exposing the patients to normal pressure combined with falsifying stimulation e g by increasing and decreasing the pressure which generates a fictitious pressure sensation Since breathing normal air under hyperbaric conditions leads to elevated tissue oxygen e g about 50 for 1 3Atm standard placebo could also be attained by giving the patients compressed air with sub normal oxygen concentration In the discussion section we explain that the first approach can be effective only for some patients and poses logistic difficulties and the second approach involves ethical issues In an attempt to evade the placebo dilemma a recent study of HBOT for mTBI compared the effect of 100 oxygen at 2 4Atm with the effect of room air at 1 3Atm as sham control 36 The study found significant improvements in both groups and with slightly higher efficacy at 1 3Atm Based on these results the authors resented a sweeping conclusion that their study shows that HBOT has no effect on post mTBI brain damage and the observed improvements resulted from placebo associated with spending time in the hyperbaric chamber As is discussed in great details in the discussion section we reason that the authors reached wrong conclusions for two main reasons First room air at 1 3Atm cannot serve as a proper sham control since it is not an ineffectual treatment as is required from placebo since it leads to a significant increase in the level of tissue oxygenation which has been shown to be effective 37 38 Second 100 oxygen at 2 4Atm leads to too high oxygen levels which can cause inhibitory effect or even focal toxicity Rationale for hyperbaric oxygen treatment HBOT The brain receives 15 of the cardiac output consumes 20 of the total body oxygen and utilizes 25 of the total body glucose Still this energy supply is only sufficient to keep about five to ten percent of the neurons active at any given time Thus at standard healthy condition at any given time the brain is utilizing almost all oxygen energy delivered to it The regeneration process after brain injury requires much additional energy This is where hyperbaric oxygen treatment can help the increased oxygen level in the blood and body tissues during treatment 17 18 19 can supply the energy needed for brain repair Indeed several previous studies have demonstrated that elevated levels of dissolved oxygen by HBOT can have several reparative effects on damaged brain tissues 3 19 20 21 22 23 24 25 Other studies revealed the beneficial effect of HBOT on the injured brain and cognitive PLOS ONE www plosone org The crossover approach To overcome the placebo issue a randomized crossover approach was successfully used to test the effect of HBOT in post stroke patients at late chronic stage 3 The advantage of the 2 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI crossover approach is the triple comparison between treatments of two groups between treatment and no treatment of the same group and between treatment and no treatment in different groups Up till now a similar prospective randomized crossover trial to evaluate the brain repair effect of HBOT in mTBI patients at late chronic stage has not been done The aim of our current study was to provide firm evaluation of the HBOT effects on brain activity and cognitive impairments in mTBI patients with prolonged PCS at late chronic stage Evaluation of cognitive state Cognitive Indices The state of the patients cognitive functions was assessed in terms of the following four cognitive indices ordered from the index associated with most fundamental basic functions to that associated with the higher functions 1 Information Processing Speed IPS index This index is associated with the basic ability to process and respond to stimuli at different levels of speed and complexity 2 Attention related index This index is associated primarily with the ability to remain concentrated and respond effectively throughout relatively extended periods of time 3 Memory related index This index is associated with the learning of verbal and visual new stimuli and the immediate and delayed recognition of these learned stimuli 4 Executive Functions EF index This index is associated with cognitive abilities involved in the initiation planning organization and regulation of behavior Each of above cognitive indices was computed as a normalized combined score of 2 3 cognitive tests from the Mindstreams Computerized Cognitive Test Battery Mindstreams NeuroTrax Corp NY Cognitive tests The Mindstreams battery includes several cognitive tests devised to check various aspects of brain capabilities In the current study we evaluated the cognitive indices based on the scores of the 6 cognitive tests listed below which are expected to be relevant for mild TBI For detailed description of all cognitive tests in Mindstreams battery see 39 The tests are 1 Verbal memory Ten pairs of words are presented followed by a recognition test in which the first word of a previously presented pair appears together with a list of four words from which the patients choose the other member of the pair There are four immediate repetitions and one delayed repetition after 10 min 2 Non verbal memory Eight pictures of simple geometric objects are presented followed by a recognition test in which four versions of each object are presented each oriented in a different direction There are four immediate repetitions and one delayed repetition after 10 min 3 Go No Go test In this continuous performance test a colored square red green white or blue appears randomly on the center of the screen The patient in then asked to respond quickly only for red squares by pressing the mouse button and inhibit his reaction to any other colored square 4 Stroop test Timed test of response inhibition modified from the Stroop paper based test In the first phase patients choose a colored square matching the color of a general word for example the word Cat appears in red letters the patient must choose the red square out of two colored squares in the following screen In the next phase termed the Choice Reaction Time test the task is to choose the colored square matching the name of the color presented in white letter color In the final Stroop interference phase patients are asked to choose the colored square matching the color and not the meaning of a former colornaming word presented in an incongruent color for example the word RED appears in green letters the patient is asked to choose the color green and not red a task requiring the ability to inhibit an automatic response to the meaning of the word 5 Staged information processing test Timed test requiring a reaction based on solving simple arithmetic problems pressing right left mouse button if the answer higher lower than 4 respectively with three levels of information processing load single digit two digits addition subtraction and three digits addition subtraction problems each containing three speed levels 3 2 and 1 second for the presentation of the stimuli Methods The study was performed as a prospective randomized controlled two group trial The study was conducted in the hyperbaric institute and the research unit of Assaf Harofeh Medical Center Israel Enrolment of patients started at 2008 and ended at 2012 All patients signed written informed consent The protocol was approved by Assaf Harofeh institutional review board Participants Inclusion The participants were patients of age 18 years or older who suffered mild TBI less than 30 minutes loss of consciousness 1 6 years prior to their inclusion All patients experienced post concussion syndrome PCS and complained of impaired cognitive functions for over a year yet brain damage was below the detection level of MRI or CT brain imaging Only patients who reported no change in cognitive function during one month prior to the beginning of the study were included Exclusions Exclusions were due to chest pathology incompatible with HBOT inner ear disease claustrophobia and inability to sign informed consent Smoking was not allowed during the study Protocol and End Points After signing an informed consent form the patients were invited for baseline evaluation Included patients were randomized into two groups 1 1 randomization a treated group and a crossover group The neuropsychological functions evaluated by Mindstreams testing battery and brain activity as visualized by SPECT Single photon emission computed tomography were the primary endpoints of the study Secondary end point included quality of life evaluation by the EQ 5D questionnaire Evaluations were made by medical and neuropsychological practitioners who were blinded to patients inclusion in the control crossed or the treated groups Patients in the treated group were evaluated twice at baseline and after 2 months of HBOT Patients in the crossover group were evaluated three times baseline after 2 months control period of no treatment and after subsequent 2 months of HBOT Figure 1 The post HBOT neurological evaluations as well as the SPECT scans were performed more than 1 week 1 3 weeks after the end of the HBOT protocol The following HBOT protocol was practiced 40 daily sessions 5 days week 60 minutes each 100 oxygen at 1 5ATA Patients were not involved in any other cognitive or rehabilitation intervention as part of the study protocol The detailed clinical study protocol copy of the informed consent as well as CONSORT 2010 checklist of information are attached as supporting information Protocol S1 Form S1 Checklist S1 We note that information regarding sample size detectable change and power calculation parameters is included and addressed in the statistical considerations section in the SI1 PLOS ONE www plosone org 3 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 1 Flow chart of the patients in the study doi 10 1371 journal pone 0079995 g001 6 Catch game A test of motor planning that requires participants to catch a falling object on a computer screen by moving a paddle horizontally so that it can catch the falling object To assign scores Mindstreams data was uploaded to the NeuroTrax central server Outcome parameters were calculated using custom software blind to diagnosis or testing site To minimize differences related to age and education each outcome parameter was normalized and fit to an IQ like scale mean 100 STD 15 according to patient s age and education We note that the score evaluation was based on normative data from cognitively healthy individuals collected in controlled research studies that were part of more than 10 clinical sites 40 The cognitive indices scores The computation of the cognitive indices based on the scores of the cognitive tests was done as follows 1 Information Processing Speed index was computed as the combined score for the low and medium load stages of the staged information processing test 2 Attention index was calculated as the mean score of reaction time for Go No Go test and choice reaction time of the Stroop test at second phase mean STD of reaction time for Go No Go test mean reaction time for a low load stage of staged information processing test and mean accuracy for a medium load stage of information processing test 3 Memory index was computed as the mean score for total learning score after four repetitions and delayed recognition phase of verbal and non verbal memory tests 4 Executive PLOS ONE www plosone org Functions index was computed based on the scores of the Stroop test and the Go No Go test and the mean weighted accuracy for catch game For more information regarding the validity of the tests and the construction of the cognitive indices see 41 42 5 In addition we defined the individual s General Cognitive Score as the average of the scores of the four cognitive indices for each individual It is important to note that the above cognitive index scores were specifically designed to represent known impaired cognitive domains in mild TBI In addition the fact that each index is referred to more than one test score ensures the index to be associated more with a cognitive domain score and less with a testdependent score We also utilized a computerized testing battery which supports the inclusion of more accurate measures such as reaction time and elimination of the bias effect of tests administration and hand scoring An important aspect of the tests is the inclusion of the cognitive domain of information processing speed known to be impaired in mild TBI patients Quality of life evaluation Quality of life QOL was evaluated by the EQ 5D questionnaire 43 EQ 5D essentially consists of 2 pages the EQ 5D descriptive system and the EQ visual analogue scale EQ VAS The EQ 5D descriptive system covers mobility self care usual activities pain discomfort and anxiety depression The EQ VAS 4 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI records the respondent s self rated health on a vertical visual analogue scale range 0 worst 100 best Results Participants Profiles The study included 90 screened patients aged 18 years or older who signed an informed consent Pre study exclusions Nineteen patients had their consent withdrawn before the beginning of the control treatment period 13 in the crossover group 6 in the treated group In study exclusions Four patients decided to drop out during the treatment protocol 3 due to personal reasons and 1 due to ear problem 1 in crossover group 3 in treatment group Seven patients 5 in crossover group 2 in treatment group were excluded due to technical performance problems in their cognitive tests and 4 patients due to inconsistent use of medications such us methylphenidate during the tests period 2 in crossover group 2 in treated group Accordingly 56 patients 32 in the treated group and 24 in crossover group were included in the final analysis Figure 1 Thirty two 57 patients were females the mean age was 44 years range of 21 66 years and the time elapsed since the acute traumatic event ranged from 1 6 years with 33 months average The most frequent etiology of the TBI was a vehicle accident n 38 with some other less common etiologies falls 7 object hit 6 pedestrian accident 3 assault 2 Baseline patients characteristics are summarized in Table 1 As seen from this table there was no significant difference in the included measures between the groups except for years of education where there was a minor advantage for the treated group Brain Functional Imaging SPECT Brain single photon emission computed tomography SPECT was conducted with 925 1 110 MBq 25 30 mCi of technetium99m methyl cysteinate dimmer Tc 99m ECD at 40 60 min post injection using a dual detector gamma camera ECAM or Symbia T Siemens Medical Systems equipped with high resolution collimators Data was acquired in 3 degree steps and reconstructed iteratively with Chang method m 0 12 cm attenuation correction 44 Visual analysis was conducted by fusing pre and post treatment studies that were normalized to cerebellum brain activity SPECT images were reoriented into Talairach space using NeuroGam Segami Corporation for identification based on visual inspection of Brodmann cortical areas and in order to compute the mean perfusion in each Brodmann area BA In addition volume rendered brain perfusion images normalized to cerebellum maximal activity were reconstructed All SPECT analysis was done while blinded to the laboratory and clinical data Change in perfusion in all Brodmann areas for each subject was determined by calculating the percentage difference between post period and pre baseline period divided by the pre baseline period perfusion An average of these perfusion changes for each Brodmann area was calculated Statistical analysis The statistical analysis was done using SPSS software version 16 0 Continuous data is expressed as means 6 standard deviations and compared by one tailed paired t test for intragroup comparisons and two tailed unpaired t test for inter group comparisons Effect sizes for main comparisons were calculated using Cohen s d Categorical data is expressed in numbers and percentages and compared by x2 test P values 0 05 were considered statistically significant All randomly allocated patients were included in the safety analysis and those with complete postbaseline assessment were included in efficacy analysis The Effect on Cognitive Functions Changes in cognitive indices The effect of the hyperbaric oxygen treatment on the patients cognitive functions as assessed by the four cognitive indices is summarized in Figure 2 and Table 2 The baseline mean cognitive scores of all four indices were close in the two groups within the standard error but with somewhat higher values in the treated group The HBOT treatments of both groups led to statistically significant improvements in the mean scores of all four indices As is apparent in Figure 2 and detailed in Table 2 a significant improvement was observed in the treated group after HBOT in all cognitive measures Information Processing Speed t 31 4 20 p 0 0001 Attention t 31 3 26 p 0 005 Memory t 31 4 13 p 0 0005 and Executive Functions t 31 3 72 p 0 0005 Effect sizes were medium to large the Cohen s d measures 45 were 0 74 0 57 0 73 and 0 66 respectively No significant improvement was noticed in the crossover group during the control period Information Processing Speed t 23 0 53 p 0 298 Attention t 23 0 33 p 0 368 Memory t 23 0 74 p 0 233 and Executive Functions t 23 0 54 p 0 295 However a significant improvement following HBOT was noticed in the crossover group as well Information Processing Speed t 23 1 98 p 0 05 Attention t 23 2 29 p 0 05 Memory t 23 3 21 p 0 005 and Executive Functions t 23 2 26 p 0 05 Effect sizes were medium to large with Cohen s d measures of 0 40 0 47 0 65 and 0 46 respectively Note that t 31 and t 23 correspond to N 1 where N 32 and N 24 are the number of patients in the treated and crossover group respectively Assessment of a general cognitive score The changes in the four cognitive indices presented in Figure 2 and in Table 2 show noticeable variability For example the mean values of the Information Processing Speed and Executive Functions indices decreased during the control period of the crossover group while the corresponding mean values of the Attention and Memory Scatter plot analysis of the clinical scores The analysis aims to better quantify and compare changes in the clinical scores while taking into consideration the high patient topatient variability following Efrati et al 3 The idea was to inspect for each patient at each time stage the scaled relative differences in each of the clinical scores More specifically we calculated for a specific patient j the scaled relative difference SRDj defined as STD SFj SRDj SFj vSFj w SIj vSIj w STD SIj z vSFj SIj w 1 Where SFj is the value of a clinical score at the end of the time stage either treatment or control and SIj is the score at the beginning of the time stage We note that the symbol indicates average over the values of the patients in the group For example SFj means the average of SFj over all patients j that belong to the group The abbreviation STD means the standard deviation between the values of the patients in the group This analysis enables quantitative inspection of the changes in the clinical scores as is further explained in 3 PLOS ONE www plosone org 5 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Table 1 Baseline patients characteristics Treated group n 32 Crossover group n 24 Comparison Age years 42 5612 6 45 7610 9 p 0 32 Gender male 11 34 13 54 p 0 07 Years of education 16 263 9 14 063 1 p 0 05 Time since injury months 34 6616 7 31 7616 3 p 0 51 None 24 75 14 58 30 minutes 8 25 10 42 Loss of consciousness p 0 18 Etiology Vehicle accident 20 63 18 75 Fall 5 16 2 8 Object hit 4 12 2 8 Pedestrian accident 2 6 1 4 Assault 1 3 1 4 Hypertension HTN 5 15 4 16 Diabetes Mellitus DM 2 6 2 8 Hyperlipidemia 4 12 3 12 Ischemic Heart Disease 0 1 4 Epileptic seizure 0 0 Smoking 1 3 0 Aspirin 2 6 3 12 Glucose lowering drugs 2 6 1 4 Anti HTN 4 12 3 12 Background disease Medications Statins 3 9 3 12 Anti depressant 7 22 4 16 doi 10 1371 journal pone 0079995 t001 indices increased Figure 3 shows the mean values of the individual general cognitive scores with standard error for the treated and crossover groups at each evaluation stage baseline and postHBOT for both groups and after the control for the crossover group It can be seen that the cross group had the same general score at baseline and after the control period This value seems higher than the score of the treated group at baseline 88 vs 85 and the post HBOT general cognitive score of the treated group seems higher than that of the crossover group 96 vs 94 While these differences are within the standard error they still give rise to what appears to be significant differences in the level of changes post vs pre HBOT between the crossover and the treated groups 6 points for the crossover group vs 11 for the treated group Examining the relative changes There is a high patient topatient variability in the cognitive indices with scores ranging from 20 to 120 The magnitude of the change in a cognitive score has different implications for patients at low or high base levels Hence we inspect the effect of the HBOT on the relative changes i e the change relative to the base value We calculated for each person the relative change in each of the cognitive indices for each period control and HBOT for the crossover group and HBOT for the treated group In Figure 4A we show the mean relative changes in all four cognitive indices for the crossover group following the control period and following HBOT and for the treated group following HBOT In Figure 4B we show the mean PLOS ONE www plosone org relative changes in the general cognitive score for the same three periods We note that calculating the mean of the relative changes is more informative than calculating the changes in the mean values especially for small groups with high patient to patient variability Looking at the relative changes elucidates the improvements after the HBOT period vs the control period of the crossover group However it also amplifies the differences mentioned earlier between the crossover and treated groups the bigger relative changes in the treated group vs the crossover group reflect the fact that the baseline values of the treated group were lower and the post HBOT values were higher in comparison to the corresponding values of the crossover group Scatter plot analysis of the cognitive indices As mentioned in the methods section the analysis aims to present the mean relative changes in cognitive indices while superimposing information regarding the patient to patient variability For that we calculated for each patient i the normalized relative change NRC i Next we calculated for each group control and HBOT in the crossover group and HBOT in the treated group the locations of the mean departures from baseline Finally we marked the location of each patient i at a distance NRC i from the location of his her group s mean difference see methods section for details Typical results are shown in Figure 5 More specifically we show the scatter plots for Information Processing Speed vs Executive Functions Figure 5A for Attention vs Memory 6 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 2 Assessment of the cognitive indices Each patient in each group was assigned a score at baseline after the control period for patients in the crossover group and after HBOT The figures show the mean scores and standard errors for the two groups at each stage for the four cognitive indices Information Processing Speed A Attention B Memory C and Executive Functions D as defined in the method section doi 10 1371 journal pone 0079995 g002 Attention EF Interestingly the scattering of the individual patients also follows the linear line for the scatter plots of the specific cognitive indices as function of the general cognitive score Figures 5C and 5D These linear dependences demonstrate high consistency between the changes of the different cognitive indices for each patient As such the analysis provides valuable test for the validity of the test performances and the validity of the general cognitive score Figure 5B for Attention vs General cognitive score Figure 5C and for IPS vs General cognitive score Figure 5D The results illustrate the differences between the three cases control and HBOT for the crossover group and HBOT for the treated group which form three distinct clusters Also clear in all the figures is the linear dependence between the changes in the different cognitive indices similar results are also obtained for the other combinations e g Memory IPS Attention IPS Memory EF and Table 2 Summary of results for Mindstreams cognitive indices scores Treated group n 32 Baseline HBOT Crossover group n 24 P1 P2 Baseline Control Pre HBOT Post HBOT P2 P3 P4 Memory 82 43625 15 96 54617 18 0 567 0005 85 90617 80 88 36617 34 95 61615 54 0 233 0 005 0 835 Executive function 88 26614 74 96 96611 69 0 367 0 0005 91 73613 26 90 20615 77 95 13613 84 0 295 0 05 0 595 Attention 85 13620 28 95 30612 90 0 854 0 005 86 10618 42 87 05620 98 92 02618 95 0 368 0 05 0 443 Information processing speed 85 12615 88 95 04613 75 0 324 0 0001 89 74618 81 88 30619 68 92 47618 25 0 298 0 05 0 55 Abbreviations Values are presented as mean 6 STD P1 stands for the p values for baseline comparison of treated and crossover group P2 stands for the p values for comparison of the second measurement to baseline in the same group P3 stands for the p values for comparison of pre and post HBOT in the crossover group P4 stands for the p values for endpoint scores comparison following treatment in both groups The baseline mean cognitive scores of all four indices were close in the two groups with no significant difference The HBOT treatments of both groups led to statistically significant improvements in the mean scores of all four indices as oppose to no significant improvement after control period alone The tables are discussed in details in the results section doi 10 1371 journal pone 0079995 t002 PLOS ONE www plosone org 7 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 3 Assessments of the general cognitive score The figure shows the level of the general cognitive score defined in the text for the crossover group at baseline after the control period and after HBOT and for the treated group at baseline and after HBOT doi 10 1371 journal pone 0079995 g003 evaluation and evaluator the cognitive function tests were done by a computerized validated method and the SPECT analysis was blind to patients participation in treated crossover group Brain SPECT evaluations were completed for 31 patients in the treated group one patient from the treated group did not complete two SPECT scans and for 24 in the crossover group In supporting information Table S1 we present detailed statistics of the SPECT results for all Brodmann areas BA of all the tested patients The results revealed a significant increase in brain activity perfusion following the hyperbaric oxygen treatments in both groups compared to the change during the control period of the crossover group A summary of the results is presented in Figure 7 To construct the figure we calculated for each patient the relative change in the SPECT measured brain activity during each phase of the trial The relative change was defined as the difference in normalized activity relative to the cerebellum activity see SI4 between the end point and the start point divided by the activity at the start We calculated for each BA the average changes over all patients that underwent HBOT both treated and cross groups These results correspond to the red curve in Figure 7 The blue curve represents the results of similar calculations for the control period averaging for each BA over all the results of all patients in the crossover group during the control period The results revealed significant improvement in brain perfusion following HBOT in the frontal and temporal areas including inferior frontal gyrus BA 45 the middle frontal area BA 46 parts of the orbito frontal cortex BA 47 and 11 most of the temporal cortex BA 36 37 38 20 21 22 28 and parts of the Cingulate gyrus BA 24 25 These fronto temporal regions responsible for the cognitive functions are the most affected in The Effect on quality of life The effect on the QOL is summarized in Table 3 The EQ 5D score significantly improved following HBOT in the treated group t 31 7 41 p 0 0001 and in the crossover group after HBOT t 23 6 17 p 0 0001 As expected there was no improvement in the EQ 5D score in the crossover group following the control period During the control period we have noticed some reduction in this group with respect to the patients subjective perception of their quality of life t 23 2 60 p 0 01 Similar results were obtained for the EQ VAS evaluations as summarized in Table 3 More specifically the EQ VAS score significantly improved following HBOT both in the treated group t 31 4 86 p 0 0001 and in the crossover group following treatment t 23 4 79 p 0 0001 while there was no significant improvement following the control period t 23 0 32 p 0 373 Details are presented in Table 3 Examining the relative changes Figure 6 presents the mean relative changes and standard errors in both measurements of quality of life for the treated group following HBOT and for the crossover group after the control period and after HBOT SPECT assessments of brain activity Motivation Since mTBI involves a diffuse structural and or physiologic metabolic derangement 46 47 48 patients with mTBI have more frequent and more extensive areas of brain damage than can be seen by anatomical imaging conventional CT and MRI scans The preferred brain imaging methods are thus functional metabolic SPECT PET CT perfusion and functional MRI In order to achieve greater validity of the results cognitive function and SPECT analysis were done by a blinded PLOS ONE www plosone org 8 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 4 Assessment of the relative changes A The relative changes as defined in the text for the four cognitive indices The changes are shown for the crossover group following the control period green bars and HBOT blue bars and for the treated group following HBOT red bars B Relative changes in the general cognitive score for the same three cases as in A doi 10 1371 journal pone 0079995 g004 Example 2 SPECT analysis of a 46 year old woman from the treated group following mTBI as a result of a car accident 1 year prior to inclusion in the study The patient s main complaints were related to her memory and concentration capabilities as well as dizziness and tinnitus that interfered with her daily functioning Following HBOT the dizziness and tinnitus disappeared in addition to significant improvement in all cognitive domains The patient s cognitive indices demonstrated significant improvements following treatment increase of 1 5 STD in Memory 57 preHBOT to 78 post HBOT 1 STD increase in Attention 88 to 104 1 5 STD increase in Executive Functions 82 to 102 and 0 6 STD increase in Information Processing Speed 85 to 95 SPECT images of the patient at baseline and following HBOT are shown in Figure 9 The percentage of CBF change demonstrated significant improvements after HBOT in parts of the frontal and temporal lobes in agreement with the improvements in neurological functions Example 3 SPECT analysis of a 44 year old man from the cross group suffering from cognitive impairments due to mild TBI as a result of a fall 2 years prior to treatments The patient complained mainly on short and long term memory difficulties attention and concentration problems decline in naming abilities as well as headaches dizziness anxiety and sleep problems Following HBOT the patient experienced significant improvements in most aspects including concentration and memory headaches dizziness mood and sleep The patient s cognitive indices demonstrated significant improvements in Executive Functions after treatment baseline 60 after control 63 and postHBOT 74 SPECT images of the patient after the control period head trauma 12 The temporal lobe plays a significant role in memory and learning skills 49 50 51 the frontal lobe is associated with attention and executive functions 52 53 and the cingulate gyrus plays an important role in emotions and cognitive self regulation 54 55 56 The SPECT results of elevated activity in these Brodmann areas are consistent with the improvement in cognitive indices following HBOT Further below we show specific examples of SPECT results for four patients two from the treated group and two from the crossover group Representative examples Example 1 SPECT analysis of a 51 year old woman from the treated group Figure 8 The patient suffered from cognitive impairments due to mTBI as a result of a fall in a moving bus 2 years prior to inclusion in the study The patient experienced no loss of consciousness and CT imaging did not reveal anatomic damage The patient s main complaints included headaches dizziness memory and concentration problems and random mood swings The patient was a manager in a private business and since the injury was having difficulties following and completing daily activities and routine Following HBOT the patient reported significant improvement in every aspect of daily functioning The patient s cognitive indices demonstrated significant improvements following treatment increase of 3 5 STD in Memory 56 pre HBOT to 108 post HBOT 2 STD increase in Attention 47 to 81 1 5 STD increase in Executive Functions 65 to 85 and a 0 7 STD increase in Information Processing Speed 85 to 95 PLOS ONE www plosone org 9 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 5 Scatter plot analysis of the changes in cognitive indices The scatter plots show the normalized relative changes NRC as defined in the methods section and explained in the text above A Scatter plot for the changes in IPS as function of changes in EF B Scatter plot for changes in Attention as function of Memory The changes in the Attention and in the IPS as function of the General cognitive score are shown in C and D respectively Circles are for the treated group and diamonds are for the crossover group The color code is Red for changes during HBOT and blue for changes during control doi 10 1371 journal pone 0079995 g005 following treatment in comparison to the changes during the control period Executive Functions at baseline after control and post HBOT were 77 71 and 88 respectively and Attention scores were 62 64 and 78 respectively SPECT images of the patient after the control period and following HBOT are shown in Figure 11 At first global look the CBF changes after HBOT seem to be similar to the changes after the control period demonstrating no significant change However a closer inspection of the SPECT images reveal local improved perfusion in the right anterior temporal and right dorso lateral frontal areas This example is shown to demonstrate that even for patients with relatively mild cognitive improvements there is good correspondence between the change in the cognitive tests and the SPECT results and following HBOT are shown in Figure 10 The CBF change was not significant after the control period but substantial improvement after HBOT in most of bilateral frontal and temporal lobes and right parietal lobe Example 4 SPECT analysis of a 39 year old woman from the cross group suffering from cognitive impairments due to mild TBI as a result of a car hit as a pedestrian 2 years prior to treatments The patient s complaints included dizziness nausea fatigue and decrease in memory and concentration abilities The patient also had troubles in performing every day activities such as attaining the grocery store or reading the newspaper The patient was working as a nurse and could not continue to perform her work after the accident due to the impaired abilities The patient s cognitive indices demonstrated significant improvements Table 3 Summary of results of quality of life questionnaire EQ 5D and EQ VAS Treated group n 32 Baseline HBOT Crossover group n 24 P1 P2 Baseline Control Pre HBOT Post HBOT P2 P3 P4 EQ 5D 7 8761 36 6 4861 07 0 615 0 0001 7 7061 11 8 0661 05 6 7561 06 0 01 0 0001 0 362 EQ VAS 5 0362 31 6 6262 45 0 696 0 0001 5 2661 70 5 2161 66 6 3961 80 0 373 0 0001 0 696 Abbreviations Values are presented as mean 6 STD P1 stands for the p values for baseline comparison of treated and crossover group P2 stands for the p values for comparison of the second measurement to baseline in the same group P3 stands for the p values for comparison of pre and post HBOT in the crossover group P4 stands for the p values for endpoint scores comparison following treatment in both groups EQ 5D as well as the EQ VAS scores significantly improved following HBOT both in the treated group and in the crossover group following treatment while there was no significant improvement following the control period doi 10 1371 journal pone 0079995 t003 PLOS ONE www plosone org 10 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 6 Assessments of the mean relative changes and standard errors in quality of life measurements The changes are shown for the crossover group following control period green bars and following HBOT blue bars and for the treated group following HBOT red bars Note that according to the questionnaire structure in the EQ 5D measurement improvement is reflected as score decrease hence the negative values of change doi 10 1371 journal pone 0079995 g006 3 imply that increasing the plasma oxygen concentration with hyperbaric oxygenation is a potent means of delivering to the brain sufficient oxygen for tissue repair HBOT might initiate a cellular and vascular repair mechanism and improve cerebral vascular flow 34 58 59 60 More specifically HBOT induces regeneration of axonal white matter 61 62 63 64 has positive effect upon the myelinization and maturation of injured neural fibers 65 and can stimulate axonal growth and increase the ability of neurons to function and communicate with each other 66 In addition HBOT was found to have a role in initiation and or facilitation of angiogenesis and cell proliferation processes needed for axonal regeneration 67 At the cellular level HBOT can improve cellular metabolism reduce apoptosis alleviate oxidative stress and increase levels of neurotrophins and nitric oxide through enhancement of mitochondrial function in both neurons and glial cells Moreover the effects of HBOT on neurons can be mediated indirectly by glial cells including astrocytes 23 HBOT may promote the neurogenesis of endogenous neural stem cells 24 With regard to secondary injury mechanisms in mTBI HBOT can initiate vascular repair mechanism and improve cerebral vascular flow 58 59 68 69 promote blood brain barrier integrity and reduce inflammatory reactions 28 as well as brain edema 20 21 22 26 34 70 A drawback to the above mentioned findings is that the different effects have been tested at different experimental setups and while utilizing different protocols of HBOT However it is well noticed that there is at least one common denominator to all repair regeneration mechanisms Discussion We presented a prospective randomized and controlled cross over study of the effect of HBOT with 100 oxygen at 1 5Atm on mTBI patients at late chronic stage The results clearly demonstrate that HBOT can induce neuroplasticity and significant brain function improvement in mild TBI patients with prolonged PostConcussion Syndrome at late chronic stage years after brain injury Additional statistical validation using simulated randomizations is available as supporting information Text S1 Linking elevated oxygen metabolism and brain activity to neuroplasticity The changes in SPECT images after treatment indicate that HBOT led to reactivation of neuronal activity in stunned areas that seemed normal under CT and MRI imaging While SPECT imaging has a limited spatial resolution compared for example to fMRI the changes in activity were sufficiently robust to be clearly detected by the SPECT images Recently Kan et al 57 discussed the need for potent interventions such as elevated tissue oxygen capable of repairing microenvironment alterations after mTBI e g impairments in vascular changes in cerebral blood flow and in perfusion leading to reduced oxygen availability followed by reduced metabolism which in turn leads to reduced neuronal activity loss of synapses and tampered neuronal connectivity The observed reactivation of neuronal activity in the stunned areas found here along with similar results in post stroke patients PLOS ONE www plosone org 11 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 7 Distribution of the Brodmann areas relative SPECT CBF changes The change for each BA represents and averaging of the relative changes of all the patients as explained in the text The results show a clear difference between the control and the HBOT periods We note that the higher variations for the control period are associated with the fact that the averaging in this case is over 24 patients the crossover group while for the HBOT period the averaging is over all 55 patients doi 10 1371 journal pone 0079995 g007 mainly to the cognitive dysfunction following the injury are commonly based on behavioral compensation methods such as attention training drills teaching memory planning strategies and usage of external aids 16 76 and have limited patient specific success in repair of mTBI impaired brain function 77 Therefore studies at the late chronic stage allow assessment of the power of the HBOT approach to achieve brain function improvements in addition to rather than instead of the standard rehabilitation programs they are all energy oxygen dependent It might be possible that HBOT enables the metabolic change simply by supplying the missing energy oxygen needed for those regeneration processes Rationale for testing the HBOT effect on patients at late chronic stage As stated in the introduction the crossover approach is adopted in order to avoid the inherent difficulties associated with randomized HBOT trial while practicing standard placebo see Text S1 The placebo dilemma and the rationale for a crossover approach are further discussed below following the rationale to selecting patients at late chronic stage First as explained in 3 applying hyperbaric oxygen in the acute or early phase after brain injury makes it almost impossible to signify and assess the HBOT effects vs the effects of the spontaneous natural repair mechanism that are effective at this stage Moreover in some patients the elevated oxygen can inhibit natural regeneration or even cause toxicity In 3 it was proposed that this might explain the contradictive results in studies using HBOT at early stage after stroke 71 72 73 74 75 One can assume that any added energy during the degenerative stage immediately after brain injury could further increase the unwanted post injury damage On the other hand elevated oxygen supply during the regenerative stage would supply the energy needs for the innate brain repair processes Second as also explained in 3 patients at the chronic late stage demonstrate neurological stability with low probability of spontaneous changes unrelated to treatment Third typically patients at this stage years after injury have already gone through rehabilitation programs These programs which attempt to attend PLOS ONE www plosone org The placebo dilemma and debate There are inherent ethical and logistic difficulties in handling the sham control in HBOT trial according to the standard placebo definition Medically ineffectual treatment for medical conditions intended to deceive the recipient from knowing which treatment is given First the minimal pressure for the patients to sense pressure increase is 1 3Atm Second breathing regular air under hyperbaric conditions of 1 3Atm leads to more than 50 elevation in tissue oxygenation There are many case reports illustrating significant effects due to small increases in air pressure including effects on the brain 38 78 79 80 Moreover even a slight increase in partial pressure such as to 1 05 ATM at altitude 402 m below sea level the Dead Sea can lead to noticeable physiological effects 81 82 83 84 85 Since 50 elevation in tissue oxygen can have significant physiological effects treatment with room air at 1 3Atm is not an ineffectual treatment as is required from a proper sham control Yet a recent randomized controlled trial on mTBI patients by Wolf et al 36 used room air at 1 3Atm as sham control for treatment with 100 oxygen at 2 4Atm Both groups 12 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 8 Volume rendered Brain SPECT perfusion maps of Example 1 a 51 year old woman from the treated group suffering mTBI that had occurred 2 years prior to inclusion in the study Comparison of the baseline activity upper row with the post HBOT activity middle row and the CBF changes bottom row demonstrated significant improvements after HBOT in bilateral orbito frontal and lateral parietal regions and left ventro lateral frontal region correlating to BAs 45 47 and 11 doi 10 1371 journal pone 0079995 g008 test this issue by evaluating the specific dose response in post mTBI patients A potential way to comply with standard placebo could be to expose the patients to normal pressure combined with falsifying stimulations e g by increasing and decreasing the pressure which generates a fictitious pressure sensation This approach poses non trivial logistic difficulties Some patients especially in long term repeated treatments can detect pressure fluctuations Another potential way to avoid the increase in tissue oxygen at 1 3Atm in order to attain a standard placebo is to let the patients breath air with lower than normal oxygen level Obviously this is an unsuitable approach as it involves ethical issues and leaves an open question with regards to the pressure effect Nevertheless Cifu et al 35 conducted a randomized blinded clinical study in which 2 0 ATA with 10 5 oxygen was used as the sham control More specifically the patients were at 2 0 ATA but were randomly assigned to one of three groups breathing either 10 5 75 or 100 oxygen to mimic normal air at 1 0 ATA 100 air at 1 5 ATA and 100 air at 2 0 ATA respectively The authors concluded that This study demonstrated that HBO2 at either 1 5 or 2 0 ATA equivalent had no effect on post concussion symptoms after mild traumatic brain injury when compared with sham revealed significant improvements in cognitive symptoms and in the measure of post traumatic stress disorder PTSD We find these results very important they actually demonstrate that the significantly less expensive and logistically simpler treatment of mTBI patients with mild HBNO2 mild hyperbaric pressure of 1 3Atm and regular air can lead to meaningful improvements Our interpretation is based on previous studies demonstrating that mild HBNO2 conditions can be effectual treatment The authors of that study presented a very different interpretation Overlooking the fact that mild HBNO2 can be an effectual treatment they regarded it as sham control and concluded that the observed improvements must be due to placebo and that HBOT has no therapeutic effect on mTBI patients In other words they implicitly assumed that bringing the patients many times to spend long duration in the hyperbaric chamber can trigger such a powerful placebo effect that it can lead to a significant repair of chronic brain damage due to mTBI Remembering that for mTBI patients with intact macro vascular bed breathing 100 oxygen at 2 4ATA generate very high oxygen levels in tissues which can cause an inhibitory effect or even focal toxicity it is conceivable that HBOT using 2 4 ATA can be less effective than 1 3 ATA or other lower levels of pressure 86 Future studies are needed to PLOS ONE www plosone org 13 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 9 Volume rendered Brain SPECT perfusion maps of Example 2 The results are of a patient in the treated group suffering mTBI that had occurred 1 year prior to inclusion in the study Comparison of the baseline activity upper row with the post HBOT activity middle row and the CBF changes bottom row demonstrated significant improvements after HBOT in bilateral orbito frontal regions the medial aspect of the temporal lobes and the temporal poles that correspond to BAs 11 25 27 28 and 38 doi 10 1371 journal pone 0079995 g009 crossover approach involves two groups a treated group in which the patients went through two months of 40 HBOT sessions and a crossover group in which the patients first went through two month of no treatment followed by two months of HBOT sessions The advantage of the crossover approach is the triple comparison between treatments of two groups between treatment and no treatment of the same group and between treatment and no treatment in different groups see Text S1 For both groups the HBOT sessions induced statistically significant improvement in cognitive functions according to four cognitive indices Information Processing Speed Attention Memory and Executive functions in brain activity according to SPECT imaging and in quality of life according to the EQ 5D and the EQ VAS scores compared to the control period of the crossover group To gain better validity of the results we used the scatter plot analysis of the changes of the cognitive indices in terms of the corresponding scaled relative changes The scatter plots figure 5 show correlations in the improvements of the different indices both for the group means and the individual patients The good correspondence between the improvements in the cognitive indices the quality of life scores and the elevated brain activity as revealed by the SPECT imaging which was done in a compression Unfortunately the HBOT effect in this study was assessed merely based on the self administered Rivermead PostConcussion Symptoms Questionnaire RPQ which is known to display several flaws in implementation and in its ability to accurately reflect test taker experience Moreover interpretation and accuracy of the RPQ can vary widely due to selfadministration and the various confounding variables involved 87 Put aside this weakness the study suffers from a logical flaw The authors mention that their study was motivated by the results of Wolf et al 36 and they accepted the interpretation that any observed improvements should be a reflection of placebo effect and have nothing to do with the HBOT If indeed placebo can be so powerful in mTBI patients one would expect that stress related to the idea of breathing half the normal level of air may trigger powerful negative placebo effect Rationale for the crossover approach In the current study we tested the effect of 1 5 ATA using the crossover approach As stated in the introduction the approach is adopted in order to avoid the inherent difficulties associated with conducting HBOT trial while practicing standard placebo The PLOS ONE www plosone org 14 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 10 Volume rendered Brain SPECT images representing the percentage of CBF change post control period and post HBOT of the cross group patient described in example 3 As can be clearly seen the improvement in perfusion following HBOT was significantly high in most areas of the brain as opposed to insignificant change following the control period The most significant improvements were in both frontal and temporal lobes and right parietal lobe doi 10 1371 journal pone 0079995 g010 how to optimize patient specific protocol is important subject for future research In conclusion this study provides for the first time convincing results based on a crossover study demonstrating that HBOT can induce neuroplasticity and significant brain function improvements in mild TBI patients with prolonged Post Concussion Syndrome at late chronic stage years after injury The results call for better understanding of how to set the optimal HBOT protocol for the specific patients and how to determine which patients benefit the most from this treatment The findings reported here bear the promises that HBOT can be effective in treating other brain impairments like easing PTSD symptoms or repairing radiation damage It is also reasonable to expect that HBOT can help slow down or even reverse metabolic disorders associated neurodegenerative diseases completely blinded fashion further substantiates the clinical findings Implications Combined with previous studies of the HBOT effects on TBI and CVA patients the results presented here show that treatment with hyperbaric oxygen can significantly repair the chronically impaired brain functions and dramatically improve the quality of life of these patients Yet HBOT did not become a common acceptable treatment for TBI and CVA largely because of the debate regarding the placebo issue and the optimal time for administration Additional larger scale clinical studies are required to asses if and to what extent placebo effects might be operative However since the improvements are significant with no significant side effects it seems reasonable to let patients benefit from HBOT now rather than wait until future studies are completed We foresee that the future oxygen pressure dose response studies described in the discussion section will have significant therapeutic implications In particular we expect that HBOT treatment with room air at 1 3ATA will have significant brain repair effects and its effect should be compared with the 1 5ATA protocol used in this study In the current study the HBOT effects were assessed shortly after treatment ended Future follow up studies are needed in order to investigate the durability of the effect It might be that some patients will need more than 40 HBOT sessions The issue of PLOS ONE www plosone org Supporting Information Table S1 SPECT based measurements of changes in brain activity This SI includes data regarding the SPECT imaging for all the patients Table S1 1 S1 3 The data was normalized according to Cerebellum activity and the relative change percentage from baseline was calculated for each subject for each Brodmann area Average and STD of all subjects were then calculated for each BA The data is available for all three groups of subjects control group after waiting period control group after HBOT crossover and treated group after HBOT 15 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 11 Volume rendered Brain SPECT images representing the CBF change in percentage post control period and post HBOT of the cross group patient described in example 4 The overall changes after the control period and the HBOT show normal variations of brain perfusion in the 10 to 10 range from green to orange colors However close inspection reveals localized significant changes white circles in the in the right temporal pole and in the right dorso lateral area These changes in perfusion are in good agreement with the improvements in the cognitive indices as the SPECT detected changes correspond to Brodmann areas 45 46 11 38 and 39 doi 10 1371 journal pone 0079995 g011 use of their software Dr Glen Doniger in particular for his great help in administering the software s data and results and Prof Avraham Schweiger for his contribution to implementing the software in our study We are grateful to Dr Hanna Levi for valuable help with the statistics and data analysis and Dr Yaron Gross for his help with the randomizations analysis We are thankful Dr Alexander Vol and Dr Orna Gribova for enlightening discussions regarding the design of the proper hyperbaric oxygen therapy for TBI patients We thank Dr Nachum Gal and Dr Laura Herzog for their help in initiating this study We thank the following individuals for their important contribution in patients management during this study Alona Esterin Mazi Aski Sela Angela Chanimov Malca Katovski Lea Shkolnic Eyal Malca Vitali Triban Talia levy Doing so ease associating the changes in SPECT measurements of brain activity with the assessed changes in the cognitive indices PDF Protocol S1 Clinical study protocol DOCX Form S1 Informed consent form English translation DOCX Checklist S1 CONSORT 2010 checklist DOCX Text S1 Crossover approach and simulated randomi zation DOC Author Contributions Conceived and designed the experiments RB G HG SE Performed the experiments HG GF YB OV NS Analyzed the data RB G HG JB MF DH EB J SE Contributed reagents materials analysis tools HG OV SE Wrote the paper RB G HG EB J SE Acknowledgments The authors express special thanks to Michal Ben Jacob for her significant help in editing the manuscript We thank NeuroTrax Corporation for the References 5 Bazarian JJ Wong T Harris M Leahey N Mookerjee S et al 1999 Epidemiology and predictors of post concussive syndrome after minor head injury in an emergency population Brain injury BI 13 173 189 6 McCauley SR Boake C Pedroza C Brown SA Levin HS et al 2005 Postconcussional disorder Are the DSM IV criteria an improvement over the ICD 10 The Journal of nervous and mental disease 193 540 550 7 Kashluba S Paniak C Blake T Reynolds S Toller Lobe G et al 2004 A longitudinal controlled study of patient complaints following treated mild traumatic brain injury Archives of clinical neuropsychology the official journal of the National Academy of Neuropsychologists 19 805 816 8 Iverson GL 2005 Outcome from mild traumatic brain injury Current opinion in psychiatry 18 301 317 1 Coronado VG Xu L Basavaraju SV McGuire LC Wald MM et al 2011 Surveillance for traumatic brain injury related deaths United States 1997 2007 Morbidity and mortality weekly report Surveillance summaries 60 1 32 2 Faul M XL Wald MM Coronado VG 2010 Traumatic Brain Injury in the United States Emergency Department Visits Hospitalizations and Deaths 2002 2006 Atlanta GA Centers for Disease Control and Prevention National Center for Injury Prevention and Control 3 Efrati S Fishlev G Bechor Y Volkov O Bergan J et al 2013 Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PloS one 8 e53716 4 Cao H Ju K Zhong L Meng T 2013 Efficacy of hyperbaric oxygen treatment for depression in the convalescent stage following cerebral hemorrhage Experimental and therapeutic medicine 5 1609 1612 PLOS ONE www plosone org 16 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI 9 Bohnen N Jolles J Twijnstra A 1992 Neuropsychological deficits in patients with persistent symptoms six months after mild head injury Neurosurgery 30 692 695 discussion 695 696 10 Binder LM 1997 A review of mild head trauma Part II Clinical implications Journal of clinical and experimental neuropsychology 19 432 457 11 Bazarian JJ McClung J Shah MN Cheng YT Flesher W et al 2005 Mild traumatic brain injury in the United States 1998 2000 Brain injury BI 19 85 91 12 Kushner D 1998 Mild traumatic brain injury toward understanding manifestations and treatment Archives of internal medicine 158 1617 1624 13 Medana IM Esiri MM 2003 Axonal damage a key predictor of outcome in human CNS diseases Brain a journal of neurology 126 515 530 14 Kochanek PM Clark R S B Jenkins L W 2007 TBI Pathobiology In Zasler ND Katz D I Zafonte R D editor Brain injury medicine NY Demos medical publishing pp 81 92 15 Levin HS Mattis S Ruff RM Eisenberg HM Marshall LF et al 1987 Neurobehavioral outcome following minor head injury a three center study Journal of neurosurgery 66 234 243 16 Sohlberg MM Mateer CA 2001 Cognitive Rehabilitation An Integrative Neuropsychological Approach NY The Guilford Press 17 Niklas A Brock D Schober R Schulz A Schneider D 2004 Continuous measurements of cerebral tissue oxygen pressure during hyperbaric oxygenation HBO effects on brain edema and necrosis after severe brain trauma in rabbits J Neurol Sci 219 77 82 18 Reinert M Barth A Rothen HU Schaller B Takala J et al 2003 Effects of cerebral perfusion pressure and increased fraction of inspired oxygen on brain tissue oxygen lactate and glucose in patients with severe head injury Acta Neurochir Wien 145 341 349 discussion 349 35 19 Calvert JW Cahill J Zhang JH 2007 Hyperbaric oxygen and cerebral physiology Neurol Res 29 132 141 20 Neubauer RA James P 1998 Cerebral oxygenation and the recoverable brain Neurol Res 20 Suppl 1 S33 36 21 Golden ZL Neubauer R Golden CJ Greene L Marsh J et al 2002 Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy Int J Neurosci 112 119 131 22 Zhang JH Lo T Mychaskiw G Colohan A 2005 Mechanisms of hyperbaric oxygen and neuroprotection in stroke Pathophysiology 12 63 77 23 Gunther A Kuppers Tiedt L Schneider PM Kunert I Berrouschot J et al 2005 Reduced infarct volume and differential effects on glial cell activation after hyperbaric oxygen treatment in rat permanent focal cerebral ischaemia Eur J Neurosci 21 3189 3194 24 Yang YJ Wang XL Yu XH Wang X Xie M et al 2008 Hyperbaric oxygen induces endogenous neural stem cells to proliferate and differentiate in hypoxicischemic brain damage in neonatal rats Undersea Hyperb Med 35 113 129 25 Rockswold SB Rockswold GL Zaun DA Zhang X Cerra CE et al 2010 A prospective randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism intracranial pressure and oxygen toxicity in severe traumatic brain injury Journal of neurosurgery 112 1080 1094 26 Palzur E Vlodavsky E Mulla H Arieli R Feinsod M et al 2004 Hyperbaric oxygen therapy for reduction of secondary brain damage in head injury an animal model of brain contusion Journal of neurotrauma 21 41 48 27 Harch PG Kriedt C Van Meter KW Sutherland RJ 2007 Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury Brain research 1174 120 129 28 Vlodavsky E Palzur E Soustiel JF 2006 Hyperbaric oxygen therapy reduces neuroinflammation and expression of matrix metalloproteinase 9 in the rat model of traumatic brain injury Neuropathology and applied neurobiology 32 40 50 29 Palzur E Zaaroor M Vlodavsky E Milman F Soustiel JF 2008 Neuroprotective effect of hyperbaric oxygen therapy in brain injury is mediated by preservation of mitochondrial membrane properties Brain research 1221 126 133 30 Daugherty WP Levasseur JE Sun D Rockswold GL Bullock MR 2004 Effects of hyperbaric oxygen therapy on cerebral oxygenation and mitochondrial function following moderate lateral fluid percussion injury in rats Journal of neurosurgery 101 499 504 31 Lin JW Tsai JT Lee LM Lin CM Hung CC et al 2008 Effect of hyperbaric oxygen on patients with traumatic brain injury Acta neurochirurgica Supplement 101 145 149 32 Golden Z Golden CJ Neubauer RA 2006 Improving neuropsychological function after chronic brain injury with hyperbaric oxygen Disability and rehabilitation 28 1379 1386 33 Rockswold GL Ford SE Anderson DC Bergman TA Sherman RE 1992 Results of a prospective randomized trial for treatment of severely brain injured patients with hyperbaric oxygen Journal of neurosurgery 76 929 934 34 Harch PG Andrews SR Fogarty EF Amen D Pezzullo JC et al 2012 A phase I study of low pressure hyperbaric oxygen therapy for blast induced postconcussion syndrome and post traumatic stress disorder Journal of neurotrauma 29 168 185 35 Cifu DX Hart BB West SL Walker W Carne W 2013 The Effect of Hyperbaric Oxygen on Persistent Postconcussion Symptoms The Journal of head trauma rehabilitation PLOS ONE www plosone org 36 Wolf G Cifu D Baugh L Carne W Profenna L 2012 The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury Journal of neurotrauma 29 2606 2612 37 Collet JP Vanasse M Marois P Amar M Goldberg J et al 2001 Hyperbaric oxygen for children with cerebral palsy a randomised multicentre trial HBOCP Research Group Lancet 357 582 586 38 James PB 2001 Hyperbaric oxygenation for cerebral palsy Lancet 357 2052 2053 39 Doniger GM 2007 Mindstreams Computerized Cognitive Tests Test Descriptions Available http www mirror upsite co il uploaded files 1383_ e7d7d3d98c924f036d3123733419149d pdf Accessed 05 July 2013 40 Doniger GM 2012 Guide to MindStreams Normative Data Available http www mirror upsite co il uploaded files 1383_ b44d4786c91058be301cb09a94ba70f4 pdf Accessed 05 July 2013 41 Doniger GM Simon ES 2007 Construct Validity of Mindstreams Comparison with Paper Based Tests Available http www mirror upsite co il uploaded files 1383_b69dcc4f4445c4c986f21b3d307ec9be pdf Accessed 05 July 2013 42 Doniger GM 2007 Mindstreams Validity Reliability Available http www mirror upsite co il uploaded files 1383_2416003ae4c2131649d294df988f2143 pdf Accessed 05 July 2013 43 Rabin R de Charro F 2001 EQ 5D a measure of health status from the EuroQol Group Annals of medicine 33 337 343 44 Jaszczak RJ Chang LT Stein NA Moore FE 1979 Whole body single photon emission computed tomography using dual large field of view scintillation cameras Physics in medicine and biology 24 1123 1143 45 Cohen J 1988 Statistical power analysis for the behavioral sciences Mahwah NJ Lawrence Erlbaum 46 Lin AP Liao HJ Merugumala SK Prabhu SP Meehan WP 3rd et al 2012 Metabolic imaging of mild traumatic brain injury Brain imaging and behavior 6 208 223 47 Hattori N Swan M Stobbe GA Uomoto JM Minoshima S et al 2009 Differential SPECT activation patterns associated with PASAT performance may indicate frontocerebellar functional dissociation in chronic mild traumatic brain injury Journal of nuclear medicine official publication Society of Nuclear Medicine 50 1054 1061 48 Belanger HG Vanderploeg RD Curtiss G Warden DL 2007 Recent neuroimaging techniques in mild traumatic brain injury The Journal of neuropsychiatry and clinical neurosciences 19 5 20 49 Squire LR 2004 Memory systems of the brain a brief history and current perspective Neurobiology of learning and memory 82 171 177 50 Squire LR Zola Morgan S 1991 The medial temporal lobe memory system Science 253 1380 1386 51 Scoville WB Correll RE 1973 Memory and the temporal lobe A review for clinicians Acta neurochirurgica 28 251 258 52 Stuss DT Alexander MP 2000 Executive functions and the frontal lobes a conceptual view Psychological research 63 289 298 53 Stuss DT 2011 Functions of the frontal lobes relation to executive functions Journal of the International Neuropsychological Society JINS 17 759 765 54 Insel TR 2010 Faulty circuits Scientific American 302 44 51 55 Posner MI Rothbart MK Sheese BE Tang Y 2007 The anterior cingulate gyrus and the mechanism of self regulation Cognitive affective behavioral neuroscience 7 391 395 56 Catafau AM Parellada E Lomena F Bernardo M Setoain J et al 1998 Role of the cingulate gyrus during the Wisconsin Card Sorting Test a single photon emission computed tomography study in normal volunteers Psychiatry research 83 67 74 57 Kan EM Ling EA Lu J 2012 Microenvironment changes in mild traumatic brain injury Brain research bulletin 87 359 372 58 Neubauer RA James P 1998 Cerebral oxygenation and the recoverable brain Neurological research 20 Suppl 1 S33 36 59 Golden ZL Neubauer R Golden CJ Greene L Marsh J et al 2002 Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy The International journal of neuroscience 112 119 131 60 Zhang JH Lo T Mychaskiw G Colohan A 2005 Mechanisms of hyperbaric oxygen and neuroprotection in stroke Pathophysiology the official journal of the International Society for Pathophysiology ISP 12 63 77 61 Chang CC Lee YC Chang WN Chen SS Lui CC et al 2009 Damage of white matter tract correlated with neuropsychological deficits in carbon monoxide intoxication after hyperbaric oxygen therapy Journal of neurotrauma 26 1263 1270 62 Lo C Shifteh K Gold T Bello JA Lipton ML 2009 Diffusion tensor imaging abnormalities in patients with mild traumatic brain injury and neurocognitive impairment Journal of computer assisted tomography 33 293 297 63 Lo CP Chen SY Chou MC Wang CY Lee KW et al 2007 Diffusion tensor MR imaging for evaluation of the efficacy of hyperbaric oxygen therapy in patients with delayed neuropsychiatric syndrome caused by carbon monoxide inhalation European journal of neurology the official journal of the European Federation of Neurological Societies 14 777 782 64 Chen Z Ni P Xiao H Chen J Qian G et al 2008 Changes in brain function and anatomical structure following treatment of hyperbaric oxygen for visual pathway abnormalities in 16 cases Neural Regeneration Research 3 117 123 65 Vilela DS Lazarini PR Da Silva CF 2008 Effects of hyperbaric oxygen therapy on facial nerve regeneration Acta oto laryngologica 128 1048 1052 17 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI 66 Neubauer RA Walker M 2000 Hyperbaric Oxygen Therapy Garden City Park NY Avery Publishing Group 67 Kuffler DP 2011 The role of hyperbaric oxygen therapy in enhancing the rate of wound healing with a focus on axon regeneration Puerto Rico health sciences journal 30 35 42 68 Rockswold SB Rockswold GL Defillo A 2007 Hyperbaric oxygen in traumatic brain injury Neurological research 29 162 172 69 Zhou Z Daugherty WP Sun D Levasseur JE Altememi N et al 2007 Protection of mitochondrial function and improvement in cognitive recovery in rats treated with hyperbaric oxygen following lateral fluid percussion injury Journal of neurosurgery 106 687 694 70 Calvert JW Cahill J Zhang JH 2007 Hyperbaric oxygen and cerebral physiology Neurological research 29 132 141 71 Anderson DC Bottini AG Jagiella WM Westphal B Ford S et al 1991 A pilot study of hyperbaric oxygen in the treatment of human stroke Stroke a journal of cerebral circulation 22 1137 1142 72 Nighoghossian N Trouillas P Adeleine P Salord F 1995 Hyperbaric oxygen in the treatment of acute ischemic stroke A double blind pilot study Stroke a journal of cerebral circulation 26 1369 1372 73 Rusyniak DE Kirk MA May JD Kao LW Brizendine EJ et al 2003 Hyperbaric oxygen therapy in acute ischemic stroke results of the Hyperbaric Oxygen in Acute Ischemic Stroke Trial Pilot Study Stroke a journal of cerebral circulation 34 571 574 74 Vila JF Balcarce PE Abiusi GR Dominguez RO Pisarello JB 2005 Improvement in motor and cognitive impairment after hyperbaric oxygen therapy in a selected group of patients with cerebrovascular disease a prospective single blind controlled trial Undersea hyperbaric medicine journal of the Undersea and Hyperbaric Medical Society Inc 32 341 349 75 Imai K Mori T Izumoto H Takabatake N Kunieda T et al 2006 Hyperbaric oxygen combined with intravenous edaravone for treatment of acute embolic stroke a pilot clinical trial Neurologia medico chirurgica 46 373 378 discussion 378 76 Glisky EL 2004 Disorders of memory In Ponsford J editor Cognitive and Behavioral Reabilitation From Neurobiology to Clinical Practice New York The Guilford Press pp 100 129 PLOS ONE www plosone org 77 de Frias CM Dixon RA Backman L 2003 Use of Memory Compensation Strategies Is Related to Psychosocial and Health Indicators The Journals of Gerontology Series B Psychological Sciences and Social Sciences 58 P12 P22 78 Golding FC Griffiths P Hempleman HV Paton WD Walder DN 1960 Decompression sickness during construction of the Dartford Tunnel British journal of industrial medicine 17 167 180 79 Austin D 1998 Gammow bag for acute mountain sickness Lancet 351 1815 80 Mychaskiw G 2nd Stephens PL 2013 Hyperbaric Oxygen Mild Traumatic Brain Injury and Study Design An Elusive Target Journal of neurotrauma 81 Goldbart AD Cohen AD Weitzman D Tal A 2007 Effects of rehabilitation winter camps at the Dead Sea on European cystic fibrosis patients The Israel Medical Association journal IMAJ 9 806 809 82 Kramer MR Springer C Berkman N Glazer M Bublil M et al 1998 Rehabilitation of hypoxemic patients with COPD at low altitude at the Dead Sea the lowest place on earth Chest 113 571 575 83 Falk B Nini A Zigel L Yahav Y Aviram M et al 2006 Effect of low altitude at the Dead Sea on exercise capacity and cardiopulmonary response to exercise in cystic fibrosis patients with moderate to severe lung disease Pediatric pulmonology 41 234 241 84 Abinader EG Sharif D Rauchfleich S Pinzur S Tanchilevitz A 1999 Effect of low altitude Dead Sea location on exercise performance and wall motion in patients with coronary artery disease The American journal of cardiology 83 250 251 A255 85 Gabizon I Shiyovich A Novack V Khalameizer V Yosefy C et al 2011 Impact of descent and stay at a Dead Sea resort low altitude on patients with systolic congestive heart failure and an implantable cardioverter defibrillator The Israel Medical Association journal IMAJ 13 402 407 86 Mychaskiw Ii G Stephens P 2012 Hyperbaric oxygen mild traumatic brain injury and study design an elusive target Journal of neurotrauma 87 Potter S Leigh E Wade D Fleminger S 2006 The Rivermead Post Concussion Symptoms Questionnaire a confirmatory factor analysis Journal of neurology 253 1603 1614 18 November 2013 Volume 8 Issue 11 e79995
1519 INVITED COMMENTARY Hyperbaric Oxygen Therapy for Traumatic Brain Injury Still an Enigma Brent E Masel MD ABSTRACT Masel BE Hyperbaric oxygen therapy for traumatic brain injury still an enigma Arch Phys Med Rehabil 2011 92 1519 21 With their article on the use of HBOT for post TBI dysautonomia Lv and colleagues discuss a novel use for this form of treatment Although HBOT has been a part of our TBI treatment armamentarium for many years its use remains a very controversial issue In this commentary the science and research studies behind HBOT for TBI are reviewed hopefully leaving the reader with an adequate knowledge base to answer a patient or family s inquiries as to the usefulness of HBOT for TBI Key Words Brain injuries traumatic Hyperbaric oxygen therapy Rehabilitation 2011 by the American Congress of Rehabilitation Medicine THEIR ARTICLE in this issue of Archives of Physical InewNMedicine and Rehabilitation Lv et al describe a potential use for hyperbaric oxygen therapy HBOT As so often 1 happens in medicine a research project was spawned by an unexpected response to a treatment The first patient in the study was receiving HBOT as part of a standard course of treatment for traumatic brain injury TBI and also happened to have post TBI dysautonomia also known as paroxysmal sympathetic hyperactivity PSH A study was begun with 5 subsequent subjects with PSH resulting from TBI receiving an HBOT regimen of 100 oxygen at 1 5 atmospheres atm with two 10 day courses separated by a 5 day rest period All patients were refractory to medications commonly used for PSH including propranolol bromocriptine midazolam morphine and gabapentin The paroxysms stopped however in 5 to 10 treatments with no recurrence after medication withdrawal They hypothesized that the response was due to the activation of devitalized neurons and as so often is the frustrating case in TBI research could not completely exclude the possibility that the improvement was due to spontaneous recovery Usually associated with injury to the deep structures of the brain PSH also known as cerebral sympathetic or diencephalic storming is thought to occur in 15 to 33 of survivors of severe TBI is generally believed to be related to a poor outcome and is a difficult problem to treat 2 It is a syndrome of episodic dysfunction of the autonomic nervous system presenting with dramatic paroxysmal changes in blood pressure respiratory and heart rate muscle tone and body From the Transitional Learning Center at Galveston Galveston Texas No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated Correspondence to Brent E Masel MD Transitional Learning Center at Galveston 1528 Postoffice St Galveston Texas 77550 e mail bmasel tlc galveston org Reprints are not available from the author 0003 9993 11 9209 00228 36 00 0 doi 10 1016 j apmr 2011 06 011 temperature It is a diagnosis of exclusion with similar symptoms seen with seizure disorders infections deep vein thrombosis neuroleptic malignant syndrome alcohol and or drug withdrawal and expanding cerebral lesions 3 Published literature on treatment is mostly anecdotal or small case studies Medications used included dantrolene benzodiazepines major tranquilizers and neurotransmitter agonists and antagonists 4 This study suggests another potential use for HBOT however it also highlights many of the reasons that this treatment is so controversial 4 The patients had many different medications on board when treatment was started The amount of dive time 120min was longer than most protocols The storming stopped yet no mention is made of the eventual outcomes Although HBOT for TBI has been used routinely for several decades in the authors center as it is thought to improve the patients recovery from the traumatic coma they make no mention of the number of individuals with PSH who did not improve with HBOT and except for this small study they have not published the outcomes on what must be a vast number of patients with TBI treated with this modality In 1992 Rockswold et al5 published a large prospective randomized HBOT TBI study of 168 patients to evaluate the effect of HBOT on acute severe TBI The mortality rate after 12 months was 17 for the 84 HBOT patients and 32 for the 82 control patients Analysis of the outcome of survivors however showed that the HBOT did not increase the number of patients who had a good recovery and moderate disability In 1976 Artru et al6 published a randomized controlled HBOT study of 60 patients in coma resulting from TBI Average time from injury to treatment was 4 5 days The overall mortality as well as the mean duration of coma was not significantly different in the HBOT or the standard therapy group They did find however a subgroup with a higher rate of recovery of consciousness This group was younger than 30 years and had brainstem contusions without supratentorial mass lesions McDonagh et al7 published an excellent review of HBOT for TBI in July 2004 They found only 7 studies out of 400 citations in the literature 5 observational trials and the 2 randomized controlled studies noted above that met their inclusion criteria Although subject to criticism 8 they concluded that the evidence for HBOT for TBI is insufficient to prove effectiveness or ineffectiveness and more high quality studies are needed The evidence indicates that there is a small chance of a mortality benefit which may depend on subgroup selection 7 p1198 Bennett et al9 in a Cochrane Collaboration review evaluated 5 acute TBI clinical trials involving 442 patients They conList of Abbreviations ATM CMS HBOT PSH TBI atmosphere Centers for Medicare and Medicaid Services hyperbaric oxygen therapy paroxysmal sympathetic hyperactivity traumatic brain injury Arch Phys Med Rehabil Vol 92 September 2011
1520 HYPERBARIC OXYGEN THERAPY FOR TRAUMATIC BRAIN INJURY Masel cluded that the effectiveness of HBOT on recovery is uncertain with the combined results suggesting that HBOT reduces the risk of death however there was no evidence that these survivors had an improved quality of life HBOT refers to the intermittent treatment with 100 oxygen at greater than normal 1atm atmospheric pressure 10 Most oxygen carried in the blood is bound to hemoglobin which in ambient air and at standard pressure is 97 saturated Some oxygen however is carried in solution Under hyperbaric conditions that portion increases as explained by Henry s law 11 As more oxygen is forced into a solution under hyperbaric conditions it can provide for greater tissue oxygenation in the setting of impaired hemoglobin function or concentration and may get to areas where red blood cells might not normally reach resulting in enhanced perfusion Although the number of indications for HBOT may be quite large the theories behind the mechanisms of therapy are few HBOT is believed to 1 enhance perfusion 2 stimulate angiogenesis 3 supersaturate the bloodstream with oxygen and 4 act as a bactericide 12 Rockswold5 commented that as a result of inadequate oxygenation of the traumatized brain aerobic metabolism converts to anaerobic metabolism Because of inadequate energy production by anaerobic metabolism the cells lose their homeostasis with the subsequent formation of damaging free radicals They thought that HBOT in an acute setting might control this cascade of events Relative to more subacute chronic TBI the mechanism behind the use of HBOT is even less clear The most commonly accepted concept the idling neuron theory assumes that after a TBI or stroke there is an ischemic penumbra which represents a border between clearly diseased and clearly healthy tissue The idling neurons reside in a quiescent state within this ischemic penumbra and have the potential for recovery By possibly increasing the oxygenation of these tissues these neurons may be reactivated although clearly cellular recovery is much more complex than merely giving a car engine more gas Obviously the timing of the treatment postinjury is critical as well How long an ischemic penumbra can exist in an individual is unknown and reports of improvement after HBOT in patients with very chronic TBI suggest another mechanism should be considered Although relatively safe HBOT is not a completely benign process It is contraindicated in patients taking certain medications with certain infections and with emphysema HBOT is also thought to possibly lower a patient s seizure threshold Generalized tonic clonic seizure activity caused by central nervous system oxygen toxicity is a rare but well known complication of HBOT Clinicians should be aware that HBOT for TBI is expensive HBOT is recognized for reimbursement by the Centers for Medicare and Medicaid Services CMS for certain conditions but HBOT for TBI is considered an off label use and is not covered by CMS and most insurance policies In 2000 a report by the U S Government Accounting Office estimated that the cost of HBOT non TBI was 405 per session with a mean total treatment cost of 12 000 per patient 13 One of the biggest reasons that TBI HBOT studies are inconclusive is the lack of a definitive treatment regimen ie HBOT dosing as well as consistent subject selection and outcome measures Head to head analysis of the studies in the literature is extremely difficult Typical approaches use 1 5 to 2 5atm 1 5atm appears to be the most common for 30 to 90 minutes while the patient is breathing 100 oxygen These treatments are then repeated multiple times with the time between treatments and the overall number of treatments the Arch Phys Med Rehabil Vol 92 September 2011 reason for terminating treatment outcome measures and costs varying widely from facility to facility The subjects in the Artru study6 received treatments at 2 5atm for 10 days with 4 days off and then 10 more days of treatment repeating until the patients regained consciousness or died The subjects in the Rockswold study5 received treatment at 1 5atm for 1 hour every 8 hours for 2 weeks until the patient was brain dead or could consistently obey simple commands In the Lv study 1 the subjects were treated at 1 5atm but received treatment for 2 hours somewhat longer than what is commonly used They received 10 days of treatment 5 days off and then 10 days of treatment again In none of these 3 studies was there an explanation as to the science behind the choice of the treatment protocol As an example Lv1 did not explain the reasoning behind giving a second course of therapy despite the fact that the paroxysms had stopped in all subjects after the first course of HBOT Well defined and researched clinical studies must be done to resolve these issues In the summary of their review Bennett9 stated Due to the small number of trials with a limited number of participants it is not possible to be confident in the findings further large high quality trials are required to define the true extent of benefit from HBOT 9 p2 Agreement on the most effective research protocols must be reached Until then we will continue to compare apples to oranges to grapes Although charged with a difficult task a consensus group of experts in HBOT as well as experts in brain injury treatment and outcomes must be convened to decide on treatment protocol issues such as HBOT dosing and subject selection as well as primary and secondary outcome measures This group should first focus on acute TBI where the measures are somewhat easier to define The next more difficult step would be to reach consensus on postacute and chronic TBIs where the myriad of confounding variables seems to constantly increase as time passes postinjury Presently Clinical Trials gov www ClinicalTrials gov lists 9 hyperbaric treatment studies 1 is completed 3 are recruiting 2 are active but not recruiting and the status of 3 is unknown Two large studies are being funded by the U S army Treatment protocols differ in terms of length of treatment percentage of oxygen inhaled depth of the dive and outcome measures Unfortunately there are no studies on acute TBI In the complex and frustrating world of TBI research HBOT remains an enigma with a complex array of possible mechanisms of action and an equally complex array of possible uses Until definitive well constructed studies are performed HBOT for TBI will always remain a puzzle and an off label promising therapeutic modality out of reach to all those who do not have the resources to pay for it With the wars in Iraq and Afghanistan and the recent tragedy in Tucson never has public interest in TBI been greater and never has it been so obvious that the medical community has so little to offer for treatment of these devastating injuries Just about anything can be accomplished with enough money Isn t it time for the government to finally provide the resources for the studies that will once and for all answer the question of the effectiveness of HBOT for TBI So how does the harried practitioner respond to a desperate family s request for advice on HBOT for a loved one All we can do is lay out the facts and let the family decide It s expensive and won t be covered by insurance It s a promising therapeutic modality but it s clear that the jury is out and that s just about all we can say definitively The wise family will then ask But doctor what would you do if this were your loved one My answer and it s strictly my personal feeling would be that in an acute or subacute setting I would pay for
HYPERBARIC OXYGEN THERAPY FOR TRAUMATIC BRAIN INJURY Masel 2 to 4 weeks of therapy and would monitor the changes closely however I would point out as tactfully as I could that I have the resources to do so But no I would not put my family into debt to pursue HBOT My personal feeling is that it s worth the gamble but only if one can afford the bet Even after having done and followed HBOT research 14 I remain steadfastly definitively conflicted I just don t know References 1 Lv L Q Hou L J Yu M K Ding X H Qi X Q Lu Y C Hyperbaric oxygen therapy in the management of paroxysmal sympathetic hyperactivity after severe traumatic brain injury a report of 6 cases Arch Phys Med Rehabil 2011 92 1515 8 2 Baguley IJ Nicholls JL Felmingham KL Crooks J Gurka JA Wade LD Dysautonomia after traumatic brain injury a forgotten syndrome Arch Phys Med Rehabil 1999 67 39 43 3 Lemke Denise M Riding out the storm sympathetic storming after traumatic brain injury J Neurosci Nurs 2004 36 4 9 4 Baguley IJ Cameron ID Green AM Slewayounan S Marosszeky JE Gurka JA Pharmacological management of dysautonomia following traumatic brain injury Brain Inj 2004 18 409 17 5 Rockswold GL Ford SE Anderson DC Bergman TA Sherman RE Results of a prospective randomized trial for treatment of severely brain injured patients with hyperbaric oxygen J Neurosurg 1992 76 929 34 1521 6 Artru F Chacornac R Deleuze R Hyperbaric oxygenation for severe head injuries preliminary results of a controlled study Eur J Neurol 1976 14 310 8 7 McDonagh M Helfand M Carson S Russman BS Hyperbaric oxygen therapy for traumatic brain injury a systematic review of the evidence Arch Phys Med Rehabil 2004 85 1198 1204 8 Harch PG Medicine that overlooks the evidence Arch Phys Med Rehabil 2006 87 592 3 9 Bennett MH Trytko B Jonker B Hyperbaric oxygen therapy for the adjunctive treatment of traumatic brain injury Cochrane Database Syst Rev 2004 4 CD004609 10 Hampton NB Hyperbaric oxygen therapy 1999 committee report Kensington Undersea Hyperbaric Medical Society 1999 11 International Union of Pure and Applied Chemistry Quantities units and symbols in physical chemistry 2nd ed Oxford Blackwell Science 1993 12 Tibbles PM Edelsberg JS Hyperbaric oxygen therapy N Engl J Med 1996 334 1642 8 13 Office of Evaluation and Inspections Hyperbaric oxygen therapy its use and appropriateness Dallas Dept of Health and Human Services 2000 Available at http www dhhs gov progorg oei Accessed May 12 2011 14 Barrett K Masel B Patterson J Scheibel RS Corson K Mader J Regional CBF in chronic stable TBI treated with hyperbaric oxygen Undersea Hyperb Med 2004 31 395 406 Arch Phys Med Rehabil Vol 92 September 2011
See discussions stats and author profiles for this publication at https www researchgate net publication 352761689 Hyperbaric oxygen therapy ameliorates the symptoms of post concussion syndrome by inhibiting MMP 9 activity a randomized controlled trial in Indonesia Article in F1000 Research June 2021 DOI 10 12688 f1000research 53289 1 CITATION READS 1 135 10 authors including Maximillian Christian Oley Mendy Hatibie Sam Ratulangi University Sam Ratulangi University 21 PUBLICATIONS 43 CITATIONS 38 PUBLICATIONS 48 CITATIONS SEE PROFILE SEE PROFILE Eko Prasetyo Billy Kepel Sam Ratulangi University Sam Ratulangi University 40 PUBLICATIONS 42 CITATIONS 49 PUBLICATIONS 161 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects 19 View project Herbal medicine View project All content following this page was uploaded by Eko Prasetyo on 30 June 2021 The user has requested enhancement of the downloaded file SEE PROFILE
F1000Research 2021 10 501 Last updated 28 JUN 2021 RESEARCH ARTICLE Hyperbaric oxygen therapy ameliorates the symptoms of post concussion syndrome by inhibiting MMP 9 activity a randomized controlled trial in Indonesia version 1 peer review 1 not approved Maximillian Christian Oley 1 4 Mendy Hatibie Oley3 5 6 Eko Prasetyo 1 2 4 Billy Johnson Kepel7 Mardoni Setiawan8 Andi Asadul Islam9 Mochammad Hatta 10 Deanette Michelle Aling3 Marcella Tirza Tulong3 Muhammad Faruk 11 1Neurosurgery Division Department of Surgery Faculty of Medicine Sam Ratulangi University Manado North Sulawesi 95162 Indonesia 2Neurosurgery Division Department of Surgery R D Kandou Hospital Manado North Sulawesi 95163 Indonesia 3Hyperbaric Centre Siloam Hospital Manado Indonesia North Sulawesi 95111 Indonesia 4Neuroscience Centre Siloam Hospital Manado North Sulawesi 95111 Indonesia 5Plastic Reconstructive and Aesthetic Surgery Division Department of Surgery Faculty of Medicine Sam Ratulangi University Manado North Sulawesi 95162 Indonesia 6Plastic Reconstructive and Aesthetic Surgery Division Department of Surgery R D Kandou Hospital Manado North Sulawesi 95163 Indonesia 7Department of Chemistry Faculty of Medicine Sam Ratulangi University North Sulawesi Manado 95162 Indonesia 8Department of Surgery Lamandau Hospital Lamandau Kalimantan Tengah 74162 Indonesia 9Department of Neurosurgery Faculty of Medicine Hasanuddin University Makassar South Sulawesi 90245 Indonesia 10Clinical Microbiology Program Faculty of Medicine Hasanuddin University Makassar South Sulawesi 90245 Indonesia 11Department of Surgery Faculty of Medicine Hasanuddin University Makassar South Sulawesi 90245 Indonesia v1 First published 25 Jun 2021 10 501 https doi org 10 12688 f1000research 53289 1 Open Peer Review Latest published 25 Jun 2021 10 501 https doi org 10 12688 f1000research 53289 1 Reviewer Status Abstract Introduction Post concussion syndrome is common in young adults and can greatly interfere with the quality of daily life It has a wide range of symptoms that require prompt and well targeted treatment to avoid further brain impairment Hyperbaric oxygen therapy HBOT is a promising regenerative treatment option for these patients to help prevent the progression of post concussion syndrome This study aims to determine whether HBOT accelerates the healing process and reduces symptoms in patients with post concussion syndrome Methods 20 patients with post concussion syndrome participated in this randomized controlled trial study After receiving standard mild traumatic brain injury treatment in accordance with the Advanced Trauma Life Support guidelines the patients were divided into HBOT and control groups Matrix metallopeptidase 9 MMP 9 Invited Reviewers 1 version 1 25 Jun 2021 1 David X Cifu report Virginia Commonwealth University School of Medicine Richmond USA Any reports and responses or comments on the Page 1 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 levels and Rivermead Post Concussion Symptoms Questionnaire RPQ scores were used to compare the two groups before HBOT after 1st 3rd and 5th week Results The study sample was predominantly male 65 with an average age of 60 years old HBOT reduced serum MMP 9 levels by nearly 20 ng mL p 0 001 compared with the control treatment The efficacy of HBOT was also reflected in the RPQ scores which were significantly lower in the HBOT group than the control group before HBOT after 1st 3rd 5th week 3 80 on RPQ 3 p p
F1000Research 2021 10 501 Last updated 28 JUN 2021 Introduction Head injury is the leading cause of death and disability among young adults 1 In Indonesia head injuries account for almost half of all deaths caused by trauma 2 4 The symptoms of head injury range from mild to severe depending on the extent of brain damage 5 Patients with head injuries often experience considerable cognitive behavioral and communication impairment 6 These patients deserve prompt effective treatments that are not only lifesaving but also preserve their brain function Hyperbaric oxygen therapy HBOT involves the inhalation of 100 oxygen at a higher pressure than the atmospheric standard Patients inhale 100 oxygen and pressure increases gradually to 2 3 absolute atmosphere ATA 7 10 HBOT has become popular in the field of neurology because it inhibits apoptosis suppresses inflammation and protects the integrity of the blood brain barrier BBB in addition to stimulating angiogenesis and neurogenesis The neuroprotective effects of HBOT are most effective during the acute phase which is the first 24 hours post head injury 11 The anti neuroinflammatory properties of HBOT are at least partially exerted by suppressing matrix metallopeptidase 9 MMP 9 expression 12 MMP 9 is a Zn dependent endopeptidase enzyme that maintains and remodels the extracellular matrix ECM MMP 9 is produced by microglia neurons oligodendrocytes astrocytes and the vascular endothelium 13 In chronic brain injury HBOT increases cerebral blood flow improves any related neuropsychological disorders and promotes neurophysiological and electrophysiological recovery 14 As such this therapy improves the quality of life in patients with post concussion syndrome and prevents its progression to more advanced stages 15 Taken together these data suggest that HBOT represents a promising therapeutic modality for various forms of head injury The persistence of symptoms associated with mild traumatic brain injury TBI is referred to as post concussion syndrome The majority of patients with post concussion syndrome recover within three to six months 16 In most clinical trials on the survey based patient progress was evaluated by neuropsychological examination such as the Rivermead Post Concussion Symptoms Questionnaire RPQ The RPQ is one of the most commonly used instruments for determining the severity of the symptoms caused by mild to moderate TBI Individual item scores reflect the presence and severity of post concussion symptoms that overlap with a wide range of conditions e g pain fatigue and mental health conditions including depression The RPQ is divided into two groups RPQ 3 and RPQ 13 RPQ 3 consists of three initial symptoms such as headaches feelings of dizziness nausea and or vomiting The RPQ 13 is a progression of these initial symptoms such as noise sensitivity sleep disturbance fatigue feeling irritable feeling depressed or impatient forgetfulness poor concentration taking longer to think blurred vision light sensitivity double vision and restlessness 17 Questionnaires are repeatedly administered to monitor the patient s progress over time and promptly identify changes in the severity of symptoms The recovery process usually requires three to six months of conservative treatment to resolve the symptoms 18 However these conservative treatments are slow and sometimes ineffective leaving patients with life long symptoms ranging from headaches to impaired cognitive function Therefore the present study aims to determine whether and how HBOT accelerates post concussion syndrome recovery by analyzing RPQ scores and MMP 9 levels respectively We hypothesize that HBOT can improve post concussion symptoms by decreasing MMP 9 levels in patients with TBI undergoing HBOT compared with traditional therapeutic approaches Methods Study design This study used a randomized controlled trial design to assess levels of MMP 9 and Rivermead Post Concussion Symptoms Questionnaire RPQ scores at pre treatment baseline and post treatment at weeks one three and five Ethical approval The study was conducted after obtaining approval from the research ethics committee of Prof Dr R D Kandou Hospital Manado Code number 125 EC KEPK KANDOU XII 2020 This study was registered with the Research Registry with a registration number no 6465 on January 17 2021 Written informed consent was obtained from all the participants The work was carried out in line with the Consolidated Standards of Reporting Trials CONSORT guidelines 19 20 Population and sample This study included 20 patients with mild TBI The patients were randomly divided according to treatment into a control group and an experimental group The experimental group received HBOT in addition to the Advanced Trauma Life Support ATLS protocol while the control group only received the latter In accordance with randomized controlled trial Page 3 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 design the patients in the control group were so selected because they refused to receive HBOT The study was carried out at Dr R D Kandou Hospital Manado North Sulawesi Indonesia Procedure All patients received standard mild TBI treatment according to the ATLS protocol including head CT scans using computed tomography SOMATOM Scope Siemens Healthineers AG Erlangen Germany to identify any brain abnormalities The HBOT group also received 60 minute HBOT sessions breathing in 100 oxygen at 2 3 ATA three times during this study at weeks one three and five 21 RPQ score Items in the questionnaires are divided into two groups The first group RPQ 3 consists of three items and the second group RPQ 13 consists of 13 subsequent items 17 18 22 The total score for the RPQ 3 items range from 0 12 and reflect the baseline symptom pool of post concussion symptoms A higher RPQ 3 score requires reassessment and close monitoring 23 MMP 9 measurements Prior to initiating treatment in both groups the RPQ was administered blood samples were collected for serum MMP 9 assays and head CT scans were performed to identify any brain abnormalities such as subarachnoid hemorrhage SAH epidural hematoma EDH subdural hemorrhage SDH and intracerebral hemorrhage ICH MMP 9 levels were measured in the Biomolecular and Immunology Laboratory of the Faculty of Medicine at Sam Ratulangi University in Manado Indonesia after every HBOT session for both the HBOT and control groups At the end of week 1 3 and 5 all patients were reevaluated for serum MMP 9 levels and RPQ scores An enzyme linked immunosorbent assay ELISA was used to quantify MMP 9 levels in ng mL as described in the MMP9 Human ELISA Kit protocol Invitrogen Corporation Carlsbad CA USA catalog number BMS2016 2 9 21 24 Statistical analysis Microsoft Excel was used for data entry and R Statistical Software version 3 6 325 was used for all statistical analyses For the categorical variables frequency tables were used to assess distributions Both center and dispersion values were calculated according to the type of variable as was the normality of the distribution for numeric variables Normally distributed numeric variables are presented as means and standard deviations SD If the distribution is abnormal median values and interquartile ranges IQR are given Differences for each variable according to the treatment group HBOT vs control were analyzed using the t test for numerical variables and the chi square or Fisher s exact test for categorical variables Changes in serum MMP 9 levels in the treatment group according to the time of examination were visually evaluated using graphs and linear mixed model analysis with random intercept these analysis measurements were repeated for each study subject The effects of HBOT on serum MMP 9 levels and RPQ scores were evaluated using linear regression models The modeling results are reported as changes in the outcome value for each unit increase in the independent variable lower and upper limits of the 95 confidence interval CI and p values which were considered statistically significant below 0 05 Results Patient characteristics including age sex and the presence of intracranial bleeding are presented in Table 1 The average patient age was 39 years and this was not significantly different between the HBOT and control groups The male tofemale ratio was approximately 6 5 3 5 Intracranial bleeding was found in over half of the cases and these were equally distributed between the HBOT and control groups No patient dropped out during the 6 week study period Serum MMP 9 levels and RPQ scores Table 2 displays the MMP 9 levels and RPQ scores at different measurement time points The two patient groups had different MMP 9 serum levels even before treatment was initiated however this difference was not statistically significant While both groups experienced decreases in MMP 9 levels during the course of this study the reduction in the HBOT group was significantly greater than in the control group 40 6 ng mL vs 21 7 ng mL p 0 001 Therefore even though the control group had higher MMP 9 levels at baseline this was compensated for by the highly significant endpoint difference the difference between both scores delta after five weeks RPQ scores did not differ between the two study groups at baseline However by the end of week five patients receiving HBOT had marked improvements in their RPQ scores compared with controls mean 3 1 vs 6 5 for RPQ 3 14 2 vs 29 6 for RPQ 13 both p values 0 001 As a result the delta scores from baseline to week five in the HBOT group were higher compared with the control group 8 0 vs 4 2 for RPQ 3 23 4 vs 7 2 for RPQ 13 both p values 0 001 Page 4 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 Table 1 Patient characteristics Characteristics Total N 20 Control n 10 HBOT n 10 Pa Age SD 38 9 15 1 38 0 15 0 39 7 16 0 0 809 Male 13 65 7 30 6 60 1 000 Female 7 35 3 30 4 40 6 30 3 30 3 30 SAH 5 25 2 20 3 30 EDH 3 15 1 10 2 20 Sex Intracranial bleeding Negative 1 000 Positive SDH 1 5 1 10 0 0 ICH 5 25 3 30 2 20 Note Data were successfully collected from twenty mild traumatic brain injury patients who participated in the study The average age of these patients was 40 years but with quite a large variation SD 15 years Table 1 There was no significant difference in the ages of patients in the HBOT group compared to controls The male to female ratio was approximately 6 5 3 5 and the ratio was relatively unchanged when stratified according to the HBOT vs control group Overall patient characteristics in both groups were relatively similar This is important to consider as the allocation of treatments in the study was not completely random The absence of difference between both groups suggests that selection bias related to age sex or location of intracranial hemorrhage might be excluded Another positive thing that supports the fairly even distribution of patients in the two study groups thereby minimizing the possibility of selection bias that might be feared due to the allocation of treatment without randomization is shown in Table 5 2 RPQ scores in the treatment group did not differ from the control group at baseline Abbreviations SD standard deviation HBOT hyperbaric oxygen therapy SAH subarachnoid hemorrhage EDH epidural hematoma SDH subdural hemorrhage ICH intracerebral hemorrhage a t test for numeric variables Fisher s exact test for categorical variables Figure 1 illustrates the changes in serum MMP 9 levels in both groups at four different time points MMP 9 levels in the HBOT group are consistently lower and decline notably after two weeks compared with the control group Figure 2 shows that the patients receiving HBOT had overall lower MMP 9 levels than those in the control group Similarly Figure 3 depicts the declining MMP 9 concentration in both groups over time and highlights that HBOT causes MMP 9 values to plummet within four weeks of initiating post injury treatment compared with controls Regression analysis using a linear mixed model revealed that changes in MMP 9 level depended on the interaction between both groups HBOT vs control and time Figure 4 The p values for the group time and the interaction of both variables were highly statistically significant p 0 001 There was a decrease in MMP 9 concentration in both groups over time however this decline was accelerated in the HBOT group compared with controls Effects of HBOT on serum MMP 9 levels and RPQ scores Table 3 presents the regression analysis of the relationship between the outcome variables MMP 9 concentration and RPQ scores and HBOT administration Scores for the individual variables were marked as delta and represent the difference between the results at week five and baseline Compared with controls the HBOT group exhibited significant declines in MMP 9 concentration 127 91 vs 9 76 p 0 001 RPQ 3 4 78 vs 2 82 p 0 001 and RPQ 13 scores 19 62 vs 12 78 p 0 001 Discussion Based on their timing and different distinctive underlying pathomechanisms head traumas are categorized as primary or secondary brain injury 26 Secondary brain injury occurs in the weeks following and in response to the primary brain injury which occurs at the time of and is directly caused by the trauma itself Patients with secondary brain injury experience biochemical metabolic and cellular changes that are orchestrated by a complex biochemical cascade that causes increased intracranial pressure BBB damage neuroinflammation brain edema brain hypoxia ischemia and neurodegeneration 27 The outcome of TBI is dependent on the secondary brain injury process 28 The starting point of our study is based on this secondary pathomechanism and its reversible dynamic nature The ECM and BBB both play important roles in neuroplasticity 29 An imperative factor in the damage of the BBB is MMP 9 which is produced by microglia the first line of defense against brain injury As the sensors and effectors of the brain s immune system microglial activity is the primary marker of neuroinflammation 30 31 Page 5 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 Table 2 Serum MMP 9 levels and RPQ scores in the HBOT and control groups Total N 20 Control n 10 HBOT n 10 pa Baseline 100 6 17 4 113 1 16 2 88 2 5 9 0 001 Week 1 91 17 9 105 13 77 1 8 8 0 001 Variableb MMP 9 ng mL Week 3 78 2 21 1 96 6 11 5 59 8 7 4 0 001 Week 5 69 5 24 2 91 3 10 2 47 6 8 3 0 001 Delta 31 2 13 5 21 7 8 5 40 6 10 7 0 001 RPQ 3 10 9 0 9 10 7 0 9 11 1 0 9 0 340 RPQ 13 37 2 3 1 36 8 2 8 37 6 3 4 0 574 RPQ Score Baseline Week 5 RPQ 3 4 8 1 9 6 5 1 3 1 0 3 0 001 RPQ 13 21 9 8 1 29 6 2 4 14 2 1 2 0 001 RPQ 3 6 1 2 2 4 2 1 8 0 1 1 0 001 RPQ 13 15 3 9 7 2 3 5 23 4 3 7 0 001 Delta Note Table 2 shows even distribution of RPQ scores from patients in the two study groups since baseline thereby minimizing the possibility of selection bias that might be feared due to the allocation of treatment without randomization Similarly the mean reduction in serum levels in the HBOT group was significantly greater than controls 40 6 ng mL vs 21 7 ng mL p
F1000Research 2021 10 501 Last updated 28 JUN 2021 Figure 2 Changes in MMP 9 levels in the HBOT and control groups Figure 3 MMP 9 concentration over time Enzymes such as occludin and claudin cause the basal degradation of endothelial lamina by targeting laminin fibronectin collagen proteoglycan and tight junction proteins degradation of ZO 1 which are also the two main functional elements of the BBB 32 The downstream outcomes of the enzymatic digestion of these structural proteins include cytoskeletal damage the disruption of cellular homeostasis ischemia inflammation tissue necrosis and apoptosis 33 The stability of the microenvironment surrounding neurons including the ECM is necessary for healthy brain function This stability is sustained by the BBB to maintain brain homeostasis and prevent cell death and dysfunction 32 The integrity of the BBB is the key to the restoration of brain homeostasis after physical injury The BBB plays a pertinent role in this process because its integrity is influenced by MMP 9 activity a major effector in secondary brain injury Therefore MMP 9 represents a reliable relevant biological marker for predicting TBI outcome 34 Page 7 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 Figure 4 Linear mixed model output for MMP 9 serum levels treatment group time of examination and their interaction as fixed effects Table 3 Regression model of the relationship between treatment type MMP 9 serum level and RPQ scores Outcome HBOT vs Control 95 CI P value MMP 9 18 83 27 91 9 76 0 001 RPQ 3 3 80 4 78 2 82 0 001 RPQ 13 16 20 19 62 12 78 0 001 Note CI confidence interval In the present study HBOT was administered to prevent or inhibit MMP 9 production HBOT acts on the neutrophil adhesion mechanism in endothelial cells More specifically HBOT reduces the expression of endothelial adhesion molecules and inhibits neutrophil adhesion molecule clustering thus reducing the number of neutrophils adhered to endothelial cells Decreasing the number of neutrophils activates pro inflammatory processes including the release of pro inflammatory cytokines e g IL1B IL 6 IL8 and TNFa and decreases the expression of MMP 9 35 The results of this study demonstrate HBOT s ability to inhibit the production of MMP 9 Similarly a study in Canada found improved cognitive function quality of life and elevated brain activity in patients with mild TBI and prolonged post concussion syndrome after 40 HBOT sessions over two months 36 In another study 40 rats were subjected to dynamic cortical deformation DCD and then divided into three treatment groups three hours after the initial trauma 20 rats received HBOT with 100 oxygen at 2 8 ATA for 45 minutes 10 received 100 oxygen for 45 minutes under normobaric conditions 1 ATA and 10 were untreated controls Neuroinflammatory markers TIMP 1 and TIMP 2 and MMP 9 levels were measured 96 hours after treatment MMP 9 Page 8 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 levels were found to be significantly lower in the HBOT group relative to controls Inflammatory infiltration around the focus of necrotic brain tissue was prominent in most untreated animals and was composed predominantly of myeloperoxidase positive neutrophils Both normobaric and hyperbaric hyperoxia resulted in a significant decrease of neutrophil infiltration GLM ANOVA main effect of treatment group P 0 0001 This reduction in the neuroinflammatory response was more extended with HBOT in comparison with normobaric hyperoxia Tukey Kramer P 0 05 12 HBOT decreases intracranial pressure ICP reduces cerebrospinal fluid CSF pressure in patients with acute brain injury restores the metabolic activity of the substance grisea in a single photon emission computerized tomography scans of the closed head injury and to restore glucose metabolism after brain injury 37 38 HBOT decreases mortality rates and improves the functional outcome of patients with severe head injuries In such chronic brain injuries HBOT increases cerebral blood flow improves neuropsychological disorders and promotes neurophysiological and electrophysiological recovery 39 Several studies have reported that multiple HBOT sessions can improve neurological deficits and cognitive impairment in both acute and advanced chronic phases of head injury in rats 40 42 The long term therapeutic effects of HBOT are derived from the induction of angiogenesis neuroplasticity and proliferation and differentiation of nerve stem cells When HBOT was administered within three hours post injury in a fluid percussion mouse model of TBI there was a significant increase in the number of endothelial cells neurons and new glial cells four days after the initial injury 40 Ten daily HBOT sessions at 2 5 ATA for 60 minutes enhances neuroplasticity by increasing axonal sprouting and synapse remodeling contributing to the restoration of locomotor function in rats with TBI 42 Harch et al study on the blood vessel density was measured bilaterally in the hippocampus using diaminobenzidine staining and correlated with MWT performance Morris Water Task They found increased vascular density in the bruised hippocampus and improved cognitive function in these rats after consecutive HBOT sessions 7 days week 1 5 ATA 90 minute sessions HBOT over 40 days 43 Several signaling pathways and transcription factors have been implicated in HBOT induced neurogenesis including wingless related integration site hypoxia inducible factors and cAMP response element binding 44 The outcome of this study was evaluated by the RPQ RPQ 13 scores range from zero to 52 with higher scores reflecting more severe post concussion syndrome The RPQ 13 items encompass a group of advanced symptoms while the RPQ 3 symptoms include headaches dizziness and nausea All those symptoms included in RPQ highly impact patient participation in social activities psychosocial functioning and lifestyle 17 During the three to six months typically required to resolve these symptoms patients are advised to gradually resume their routine activities If symptoms do not resolve within this period patients are usually often referred to a specialist for further assessment and treatment services 45 The data collected in the present study showed a notable decrease in the RPQ 3 and RPQ 13 scores There was no significant difference in the baseline RPQs of the groups at the beginning of the study However by the end of the five weeks of treatment the patients receiving HBOT had much better RPQ scores mean 3 1 vs 6 5 for RPQ 3 and 14 2 vs 29 6 for RPQ 13 both p values 0 001 As a result the delta score from baseline to the end of week five in the HBOT group was significantly lower than the control group 8 0 vs 4 2 for RPQ 3 p 0 001 23 4 vs 7 2 for RPQ 13 p 0 001 The decline in RPQ scores over time was significant RPQ 3 3 80 p 0 001 and RPQ 13 16 20 p 0 001 HBOT administration in patients with mild TBI contributed to this improvement RPQ scores Based on the findings described here HBOT confers great benefits by improving the quality of life of patients with mild TBI and likely prevents further brain damage by increasing cerebral blood flow improving neuropsychological disorders and promoting neurophysiological and electrophysiological recovery Given that repeated HBOT sessions restored neurological deficits and cognitive impairment HBOT should be incorporated as a therapeutic modality for the treatment of patients with head injuries Although there are many benefits of HBOT there are also several drawbacks such as seizures oxygen poisoning pneumothorax and middle ear injuries Although this study supports the efficacy of HBOT in treating post concussion syndrome the small sample population and single biomarker are limitations that must be addressed in future studies The kinetics and underlying mechanisms of HBOT also warrant further investigation to maximize the many beneficial effects of HBOT Conclusions HBOT effectively relieves the symptoms associated with post concussion syndrome through a mechanism that involves repressing MMP 9 activity Page 9 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 Consent statement Written informed consent for publication of the patients details was obtained from the patients a guardian of the patient Data availability Underlying data Zenodo Hyperbaric oxygen therapy ameliorates the symptoms of post concussion syndrome by inhibiting MMP 9 activity A Randomized Controlled Trial in Indonesia http doi org 10 5281 zenodo 4785703 46 This project contains the following underlying data Maximilian Data Post Concussion Syndrome 2 docx Patient characteristics Maximilian Data Post Concussion Syndrome xlsx Human Matrix Metalloproteinase 9 MMP 9 VALUE Reporting guidelines This project also contains the following reporting guidelines CONSORT checklist CONSORT flowchart Data are available under the terms of the Creative Commons Attribution 4 0 International license CC BY 4 0 References 1 Jalali R Rezaei M A Comparison of the Glasgow Coma Scale Score with Full Outline of Unresponsiveness Scale to Predict Patients Traumatic Brain Injury Outcomes in Intensive Care Units Crit Care Res Pract 2014 2014 1 4 PubMed Abstract Publisher Full Text Free Full Text 10 Oley MH Oley MC Aling DMR et al Effects of hyperbaric oxygen therapy on the healing of thermal burns and its relationship with ICAM 1 A case control study Ann Med Surg 2021 61 104 109 PubMed Abstract Publisher Full Text Free Full Text 2 Samma L Widodo D A case evaluation of traumatic brain injury in Wahidin Sudirohusodo Hospital Makassar during January 2016 December 2017 Bali Med J 2019 8 542 Publisher Full Text 11 S nchez EC Mechanisms of Action of Hyperbaric Oxygenation in Stroke Crit Care Nurs Q 2013 36 290 298 PubMed Abstract Publisher Full Text 12 3 Wardoyo MS Widodo D Ihwan A et al The relationship between different dosages of mannitol 20 and osmolarity blood sugar serum and coagulation factors in moderate brain injury patients with increased intracranial pressure Med Cl nica Pr ctica 2021 4 100235 Publisher Full Text Vlodavsky E Palzur E Soustiel JF Hyperbaric oxygen therapy reduces neuroinflammation and expression of matrix metalloproteinase 9 in the rat model of traumatic brain injury Neuropathol Appl Neurobiol 2006 32 40 50 PubMed Abstract Publisher Full Text 13 4 Prasetyo E The primary secondary and tertiary brain injury Crit Care Shock 2020 23 4 13 Rempe RG Hartz AM Bauer B Matrix metalloproteinases in the brain and blood brain barrier Versatile breakers and makers J Cereb Blood Flow Metab 2016 36 1481 1507 PubMed Abstract Publisher Full Text Free Full Text 5 NASEM Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans In Veterans Diagnosis Assess Trauma Brain Inj Washington D C National Academies Press 2019 PubMed Abstract Publisher Full Text 14 Wolf G Cifu D Baugh L et al The Effect of Hyperbaric Oxygen on Symptoms after Mild Traumatic Brain Injury J Neurotrauma 2012 29 2606 2612 PubMed Abstract Publisher Full Text 15 6 Sepahvand E Jalali R Mirzaei M et al Glasgow coma scale versus full outline of unresponsiveness scale for prediction of outcomes in patients with traumatic brain injury in intensive care unit Turk Neurosurg 2015 PubMed Abstract Publisher Full Text Cifu DX Hart BB West SL et al The Effect of Hyperbaric Oxygen on Persistent Postconcussion Symptoms J Head Trauma Rehabil 2014 29 11 20 PubMed Abstract Publisher Full Text 16 D Souza M Trivedi R Singh K et al Traumatic brain injury and the post concussion syndrome A diffusion tensor tractography study Indian J Radiol Imaging 2015 25 404 PubMed Abstract Publisher Full Text Free Full Text 17 Potter S Leigh E Wade D et al The Rivermead Post Concussion Symptoms Questionnaire J Neurol 2006 253 1603 1614 Publisher Full Text 18 Asselstine J Kristman VL Armstrong JJ et al The Rivermead PostConcussion Questionnaire score is associated with disability and self reported recovery six months after mild traumatic brain injury in older adults Brain Inj 2020 34 195 202 PubMed Abstract Publisher Full Text 19 Agha RA Borrelli MR Vella Baldacchino M et al The STROCSS statement Strengthening the Reporting of Cohort Studies in 7 Shinomiya N Molecular Mechanisms of Hyperbaric Oxygen Therapy In Hyperb Oxyg Ther Singapore Springer Singapore 2020 3 20 Publisher Full Text 8 Raveenthiraraja T Manoharan S Hyperbaric oxygen therapy A review Int J Pharm Pharm Sci 2013 5 52 54 9 Oley MH Oley MC Tjandra DE et al Hyperbaric oxygen therapy in the healing process of foot ulcers in diabetic type 2 patients marked by interleukin 6 vascular endothelial growth factor and PEDIS score A randomized controlled trial study Int J Surg Open 2020 27 154 161 Publisher Full Text Page 10 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 Surgery Int J Surg 2017 46 198 202 PubMed Abstract Publisher Full Text Free Full Text 20 21 Schulz KF Altman DG Moher D CONSORT 2010 Statement updated guidelines for reporting parallel group randomised trials BMJ 2010 340 c332 c332 PubMed Abstract Publisher Full Text Free Full Text Oley MH Oley MC Islam AA et al Hyperbaric oxygen therapy in managing systemic inflammatory response syndrome caused by ischemia reperfusion injury following hand replantation and long term outcomes A report of two cases Ann Med Surg 2020 60 155 161 PubMed Abstract Publisher Full Text Free Full Text Injury A Paired Microdialysis Study J Neurotrauma 2015 32 1553 1559 PubMed Abstract Publisher Full Text Free Full Text 35 Pekovic S Dacic S Krstic D et al Hyperbaric Oxygen Therapy in Traumatic Brain Injury Cellular and Molecular Mechanisms In Hyperb Oxyg Treat Res Clin Pract Mech Action Focus InTech 2018 Publisher Full Text 36 Boussi Gross R Golan H Fishlev G et al Hyperbaric Oxygen Therapy Can Improve Post Concussion Syndrome Years after Mild Traumatic Brain Injury Randomized Prospective Trial PLoS One 2013 8 e79995 PubMed Abstract Publisher Full Text Free Full Text 22 King NS Crawford S Wenden FJ et al The Rivermead Post Concussion Symptoms Questionnaire a measure of symptoms commonly experienced after head injury and its reliability J Neurol 1995 242 587 592 PubMed Abstract Publisher Full Text 37 Hu Q Manaenko A Xu T et al Hyperbaric oxygen therapy for traumatic brain injury bench to bedside Med Gas Res 2016 6 102 PubMed Abstract Publisher Full Text Free Full Text 38 23 Eyres S Carey A Gilworth G et al Construct validity and reliability of the Rivermead Post Concussion Symptoms Questionnaire Clin Rehabil 2005 19 878 887 PubMed Abstract Publisher Full Text Hayakawa T Kanai N Kuroda R et al Response of cerebrospinal fluid pressure to hyperbaric oxygenation J Neurol Neurosurg Psychiatry 1971 34 580 586 PubMed Abstract Publisher Full Text Free Full Text 39 24 Nasution RA Islam AA Hatta M et al Role of CAPE in reducing oxidative stress in animal models with traumatic brain injury Ann Med Surg 2020 57 118 122 PubMed Abstract Publisher Full Text Free Full Text Golden ZL Neubauer R Golden CJ et al Improvement in Cerebral Metabolism in Chronic Brain Injury after Hyperbaric Oxygen Therapy Int J Neurosci 2002 112 119 131 PubMed Abstract Publisher Full Text 40 25 R Core Team R A Language and Environment for Statistical Computing 2018 Reference Source 26 Werner C Engelhard K Pathophysiology of traumatic brain injury Br J Anaesth 2007 99 4 9 PubMed Abstract Publisher Full Text Lin K C Niu K C Tsai K J et al Attenuating inflammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury J Trauma Acute Care Surg 2012 72 650 659 PubMed Abstract Publisher Full Text 41 Daugherty WP Levasseur JE Sun D et al Effects of hyperbaric oxygen therapy on cerebral oxygenation and mitochondrial function following moderate lateral fluid percussion injury in rats J Neurosurg 2004 101 499 504 PubMed Abstract Publisher Full Text 42 Brkic P Stojiljkovic M Jovanovic T et al Hyperbaric oxygenation improves locomotor ability by enhancing neuroplastic responses after cortical ablation in rats Brain Inj 2012 26 1273 1284 PubMed Abstract Publisher Full Text 43 Harch PG Kriedt C Van Meter KW et al Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury Brain Res 2007 1174 120 129 PubMed Abstract Publisher Full Text 27 Frattalone AR Ling GSF Moderate and Severe Traumatic Brain Injury Neurosurg Clin N Am 2013 24 309 319 PubMed Abstract Publisher Full Text 28 Alves JL Blood brain barrier and traumatic brain injury J Neurosci Res 2014 92 141 147 Publisher Full Text 29 Thomsen MS Routhe LJ Moos T The vascular basement membrane in the healthy and pathological brain J Cereb Blood Flow Metab 2017 37 3300 3317 PubMed Abstract Publisher Full Text Free Full Text 30 Loane DJ Faden AI Neuroprotection for traumatic brain injury translational challenges and emerging therapeutic strategies Trends Pharmacol Sci 2010 31 596 604 PubMed Abstract Publisher Full Text Free Full Text 44 31 Loane DJ Byrnes KR Role of microglia in neurotrauma Neurotherapeutics 2010 7 366 377 PubMed Abstract Publisher Full Text Free Full Text Mu J Krafft PR Zhang JH Hyperbaric oxygen therapy promotes neurogenesis where do we stand Med Gas Res 2011 1 14 PubMed Abstract Publisher Full Text Free Full Text 45 Voormolen DC Haagsma JA Polinder S et al Post Concussion Symptoms in Complicated vs Uncomplicated Mild Traumatic Brain Injury Patients at Three and Six Months Post Injury Results from the CENTER TBI Study J Clin Med 2019 8 1921 PubMed Abstract Publisher Full Text Free Full Text 46 Oley MC Oley MH Prasetyo E et al Hyperbaric Oxygen Therapy Ameliorates the Symptoms of Post Concussion Syndrome by Inhibiting MMP 9 Activity A Randomized Controlled Trial in Indonesia F1000res 2021 Publisher Full Text 32 Daneman R Prat A The Blood Brain Barrier Cold Spring Harb Perspect Biol 2015 7 a020412 PubMed Abstract Publisher Full Text Free Full Text 33 Mittal M Siddiqui MR Tran K et al Reactive Oxygen Species in Inflammation and Tissue Injury Antioxid Redox Signal 2014 20 1126 1167 PubMed Abstract Publisher Full Text Free Full Text 34 Guilfoyle MR Carpenter KLH Helmy A et al Matrix Metalloproteinase Expression in Contusional Traumatic Brain Page 11 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 Open Peer Review Current Peer Review Status Version 1 Reviewer Report 28 June 2021 https doi org 10 5256 f1000research 56656 r88241 2021 Cifu D This is an open access peer review report distributed under the terms of the Creative Commons Attribution License which permits unrestricted use distribution and reproduction in any medium provided the original work is properly cited David X Cifu Department of Physical Medicine Rehabilitation Virginia Commonwealth University School of Medicine Richmond VA USA This is a small n 20 unblinded RCT of low dose HBOT three 60 minute sessions at b n 2 3 ATA over 5 weeks in middle aged mean 39 years old people with what were labeled as mild TBI The researchers identified reductions in serum MMP 9 and symptoms RPQ after 6 weeks Unfortunately this study is significantly underpowered flawed in its diagnosis of mTBI 70 had intracranial bleeding including SDH EDH and IPH the diagnosis of mTBI precludes these conditions does not provide the specific time post injury the dosing of HBOT is atypical for mTBI trials the controls refused to be in the HBOT arm apparently that was by design and thus were negatively biased and there was no HBOT sham so the treatment subjects were positively biased toward improvement Additionally the authors have misquoted the mTBI HBOT literature e g references 14 and 15 do not support the efficacy of HBOT for mTBI and do not seem to be aware of the HBOT literature Of note the abstract records the average age of participants as 60 years old but the results section and tables identify it as 39 years old This study has too significant methodological limitations and inconsistencies to warrant indexing Is the work clearly and accurately presented and does it cite the current literature Partly Is the study design appropriate and is the work technically sound No Are sufficient details of methods and analysis provided to allow replication by others Yes Page 12 of 13
F1000Research 2021 10 501 Last updated 28 JUN 2021 If applicable is the statistical analysis and its interpretation appropriate Yes Are all the source data underlying the results available to ensure full reproducibility Yes Are the conclusions drawn adequately supported by the results No Competing Interests No competing interests were disclosed Reviewer Expertise TBI HBOT mild TBI Rehabilitation I confirm that I have read this submission and believe that I have an appropriate level of expertise to state that I do not consider it to be of an acceptable scientific standard for reasons outlined above The benefits of publishing with F1000Research Your article is published within days with no editorial bias You can publish traditional articles null negative results case reports data notes and more The peer review process is transparent and collaborative Your article is indexed in PubMed after passing peer review Dedicated customer support at every stage For pre submission enquiries contact research f1000 com View publication stats Page 13 of 13
JOURNAL OF NEUROTRAUMA 30 1995 1999 December 1 2013 Mary Ann Liebert Inc DOI 10 1089 neu 2012 2799 Letter to the Editor Hyperbaric Oxygen Therapy for Post Concussion Syndrome Contradictory Conclusions from a Study Mischaracterized as Sham Controlled Paul G Harch Dear Editor The recent study by Wolf and associates1 has affirmed the effectiveness of hyperbaric oxygen therapy in the treatment of patients with mild traumatic brain injury mTBI post concussion syndrome PCS and post traumatic stress disorder PTSD This affirmation emerges from analysis of the study data rather than from the study s stated conclusions Mischaracterized as a shamcontrolled placebo implied design the study errs in concluding that HBO2 at 2 4 ATA pressure had no effect on post concussive symptoms after mild TBI A reconsideration of the science of hyperbaric therapy reveals that the study by Wolf and colleagues1 is neither a sham nor placebo controlled study Rather it is a Phase II study of two composite doses of hyperbaric therapy that demonstrated significant improvements in PCS and PTSD symptoms at the 2 4 atmospheres absolute ATA pure oxygen dose as well as the low pressure 1 3 ATA air oxygen dose Hyperbaric oxygen therapy HBOT is a combination product of increased pressure and increased pressure of oxygen above ambient atmospheric pressure according to scientific principles and current Food and Drug Administration understanding Although traditionally misdefined as a treatment for diseases based on the increased oxygen component alone 1 4 ATA oxygen 2 it is a treatment with hyperbaric pressure and hyperoxia for disease processes2 3 whose primary targets are oxygen and pressure sensitive genes 4 6 Evidence for this dual component nature of hyperbaric therapy is found in the 351 year history of hyperbaric air therapy7 and the recent 60 year history of animal human tissue and human experiments that have documented biological effects of pressure especially in the micropressure range8 9 of the Wolf and coworkers1 sham control group and the control groups of the Department of Defense DoD HBOT TBI studies 10 Examples of this literature are listed in Tables 1 and 2 11 28 Pressures from 1 21 1 26 ATA delivered to human29 31 and 1 0015 1 015 ATA to animal endothelial cells 32 and 1 10 and 1 20 ATA to human platelets33 34 for 15 min or longer have caused the elaboration or suppression of vasoactive substances 29 31 and the elaboration of growth factors 32 inflammatory mediators 33 oxidation products 34 and cell proliferation 32 This literature and biological effects from a 1 min exposure to 1 09 ATA or 3 min at 1 04 ATA17 inform the symptomatic improvements noted in the Wolf and associates1 sham group as do benefits of hyperbaric air on spinal function and PTSD in spinal cord injured veterans during a SCUBA diving training course 28 To meet the definition of a true sham 35 any controlled experiment to test HBOT must omit in its control groups the active ingredients of increased pressure and hyperoxia The Wolf and colleagues1 sham control group does neither rather it includes both The sham control group is exposed to 1 3 1 2 ATA of air which is a 20 30 increase in pressure and 28 43 increase in plasma oxygen36 over sea level plasma oxygen and a slightly greater increase over San Antonio hyperbaric treatment site atmospheric pressure 37 Because pressure and hyperoxia are noninert i e are biologically active the Wolf and coworkers1 sham control group cannot test for placebo effects placebo placebo response is defined as The effect that an inactive or inert substance has on a clinical condition 38 Wolf and associates1 allude to possible bioactivity of the control group but the lack of discussion indicates a lack of appreciation that the presence of hyperoxia and pressure negate Wolf and colleagues1 characterization as a sham control group Restating the design of the Wolf and coworkers1 study it is a Phase II comparative dosing study of two composite doses of hyperbaric therapy four actual doses compressed air low dose increased pressure and increased oxygen and compressed oxygen high dose pressure and high dose oxygen Both doses were efficacious in the treatment of mTBI PCS and PTSD The PTSD data demonstrated 18 and 22 reductions in the PCL M interpolated from the Figure 1 graph in Wolf and colleagues1 in the HBOT and sham groups respectively after 30 2 h treatments These reductions compared favorably with five other therapies six studies for PTSD39 44 that used the PCL M 6 45 reductions The PCS ImPACT data were similarly significantly improved in both groups but it is the disparity in component and pattern change on the ImPACT results for the two groups that underscore the dual dose design of the study and efficacy of these two doses 10 IMPACT scores significantly improved in the low dose group compared with 2 in the high dose group For all 22 items of the ImPACT 20 improved 1 was unchanged and 1 was worse in the Department of Medicine Louisiana State University School of Medicine New Orleans Louisiana 1995
1996 HARCH Table 1 In vitro and In vivo Studies on Hyperbaric Pressure and Oxygen Effects Study 1 2 3 4 5 6 7 8 Cunningham O J Dowell R T 12 Hishikawa K 13 Mattana J 14 Teiger E 15 Kramer M R 16 Kawata Y 17 Macdonald A G review9 9 Agar A 18 11 Year Model In Vivo IV In Vitro IVT Animal human Ambient gas 1900 1929 1978 1994 1995 1996 1998 1998 1999 Multiple medical disorders Aortic constriction IV Vascular smooth muscle cells IVT Mesangial renal cells IVT Aortic constriction IV COPD pulmonary function Mesangial renal cells IVT Wide range of IV and IVT 2000 Neuroblastoma IVT glaucoma model Brain stem neurons IVT Dorsal root ganglion neurons IVT Cerebral palsy IV Subacute hypoxic ischemia brain injury IV Chronic toxic encephalopathy or autism IV Cerebrovascular injury epilepsy migraine IV Acute stroke Fibroblast wound healing IVT Autism Spinal cord injury and PTSD Human Rat neonate and adult Rat Rat Rat Humans Rat Bacteria insect nematode animal human Rat Air Air Helium 95 air 5 CO2 Air Air Air 95 air 100 air helium 95 air 5 CO2 Rat Rat Human children Rat Air helium 95 air 5 CO2 Air 100 oxygen Air 100 oxygen Human adults and children 24 oxygen Human adults 30 40 and 100 oxygen 100 oxygen 94 air 6 CO2 Air 24 oxygen Air Dean J B 19 Heal R D 20 Collet J P 21 Yu H A I 22 2000 2001 2001 2002 14 Heuser G 23 2002 15 Kazantseva N V 24 2002 10 11 12 13 16 17 18 19 Rusyniak D E 25 Stanley A C 26 Rossignol D A 27 Kaplin A 28 2003 2005 2009 2011 Human adults Human neonatal fibroblasts Human children Human veterans COPD chronic obstructive pulmonary disease PTSD post traumatic stress disorder low dose group while 11 improved 3 were unchanged and 8 were worse in the high dose group Table 1 in Wolf and associates1 The pattern of composite ImPACT scores over the course of the study is also different for the two groups Figure 2 in Wolf and coworkers1 Subjects in the low dose group experienced initial deterioration then steady improvement until the end of the study while the high dose group showed improvement then a steady reversal of benefit to near baseline followed by rebound improvement 6 weeks posttreatment This sinusoidal trajectory in the high dose group suggests a differential dosing effect and possibly an overdose response with partial recovery after removal of the high dose and is consistent with the worsening of eight scores in this group It is also consistent with a phenomenon previously described and documented in multiple cases of HBOT treatment of chronic cerebral disorders 45 Since the initial submission of this Letter to the Editor Wolf and colleagues1 have now confirmed this overdosing effect on PCS symptoms in the 2 4 ATA group in a subset analysis presented on June 14 2013 46 This demonstration of low dose effectiveness and progressive high dose overdosing is also evident in other animal and clinical studies 25 47 48 Wolf and associates1 list multiple possibilities for the improvements in PCS and PTSD including placebo Hawthorne effect the natural resolution of symptoms over time exposure to sham control partial pressures of oxygen and nitrogen and change in living environment and daily routine While 30 chamber experiences and change in living environment and daily routine are theoretical placebo contributions the myriad standard clinical pressure hyperoxia2 and micropressure induced biological effects demonstrated in both animal and human studies8 9 and Tables 1 and 2 suggest that placebo is not the majority effect At the same time placebo effects were also present in all six of the aforementioned PTSD PCL M studies Hawthorne effect is also theoretically possible but the foundation proofing of the Hawthorne effect has been undermined by re evaluation of the initial data set 49 Symptoms in veterans with TBI and PTSD in fact do not resolve over time as acknowledged by Wolf and coworkers1 in their conclusion improved more than would be expected greater than 6 months after mTBI and reports on persistent care and even worsening of condition over time in the Veterans Affairs system 50 51 All of the explanations by Wolf and colleagues 1 however do not explain the disparity in component and pattern change in the ImPACT data and transient overdose effect in the high dose oxygen group If placebo Hawthorne effect and other non biological etiologies are causally entertained why wouldn t the component and pattern changes be identical in the two groups The last choice effects of increased partial pressures of oxygen and nitrogen seems most plausible as the dominant etiology for the statistically significant improvements in both groups but it is not necessarily nitrogen pressure but pressure per se that is involved Wolf and associates1 state however it seems very unlikely such a minimal dose of oxygen and nitrogen could influence brain function favorably The preceding argument and studies in Table 1 and 2 suggest the opposite In conclusion the study by Wolf and colleagues1 is a non sham non placebo non controlled Phase II two composite dose study of hyperbaric therapy hyperbaric air and hyperbaric oxygen in U S veterans with PCS from mTBI with or without PTSD The study demonstrated significant net improvements in PCS and PTSD symptoms with both doses of hyperbaric therapy improvements that are similar in magnitude to other therapies for PTSD and greater than would be expected for PTSD and PCS over time without treatment based on the natural history of the diseases and published persistence rates in veterans 50 51 Their results are thus comparatively effective to other existing therapies for PTSD and possibly PCS of mTBI
1997 0 129 0 129 arterial oxygen partial pressure 0 205 0 205 0 23 0 237 not measured for 2nd pressure 0 129 0 129 arterial oxygen partial pressure No controls pre post 0 221 2 4 0 199 0 251 0 222 0 222 0 950 2 352 3 332 0 199 0 599 0 273 1 750 0 250 0 625 2 50 No control 0 312 0 300 0 330 0 480 1 500 1 14 2 50 0 194 0 205 0 213 0 229 0 216 0 312 SCUBA course 8 9 10 11 12 13 14 15 16 17 18 19 1 14 2 50 1 000 1 039 1 079 1 158 1 03 1 30 Likely 3 ATA No control 1 30 1 000 1 100 1 200 1 500 1 000 1 010 1 260 1 000 1 131 1 000 1 000 4 000 1 000 3 000 1 300 1 750 1 000 2 500 Approximately same as 1 same model Pre 0 912 Post 1 0526 1 000 1 039 1 066 1 092 1 118 1 000 1 053 1 066 and 1 066 1 079 1 000 1 053 1 105 1 158 No controls average1 34 2 36 ATA max 3 ATA 1 103 1 163 1 150 1 217 Total pressure ATA Control experimental 1 h day 10 days 15 20m 5 15 20m 4 10 20 m 1 or 4 5 60 m 5 1h 12 18 h 1 h day 40 days Likely 1 h Few sec days 2h 5 15 min 8 min 20 sec 60 minutes d 40 d 60 minday 10 days 1 30 minutes 12 24 48 hours 21 days 1 2 4 7 15 30 days 1 or 7 days 24 and 48 h 2 3 hours up to days Multiple treatments 2 3 4 5 weeks Duration Rxs Effect Enzyme activation w i 1 min 1 092 ATA gene expression proliferation post 12 h and 24 h exposure Wide range of biological effects Increased apoptosis Differential effects of pressure and oxygen on firing rate Suppression of firing rate Both groups Significant improvements in motor and cognition Increased bFGF in hyperbaric air increased bFGF and bFGF mRNA in HBO Improved blood flow on SPECT brain imaging Improvement symptoms EEG blood flow vital signs biochemical params 1 5 ATA Better outcome in the low dose group Delayed wound healing and less proliferating cell nuclear antigen Clinical improvement Improved spinal cord function and PTSD Improved arterial oxygen and exercise capacity Increased cell proliferation and DNA synthesis process begins w i 30s press Decreased cell number and increased matrix collagen MC at 7d Dose response for MC Increased apoptosis of cardiac myocytes by 1 day peak at 4 days Cardiac myocyte and non myocyte proliferation Generally improvement in clinical and laboratory parameters ATA atmospheres absolute bFGF basic fibroblast growth factor HBO hyperbaric oxygen EEG electroencephalography PTSD post traumatic stress disorder 0 270 0 270 7 6 5 3 No controls 0 281 0 496 Oxygen pressure ATA Control experimental 1 Study Table 2 Continuation of Table 1 In vitro and in Vivo Studies on Hyperbaric Pressure and Oxygen Effects
1998 If further evidence for the efficacy of hyperbaric therapy in mTBI PCS and PTSD is deemed necessary as alternatives to the pivotal trial 10 and in light of nearly 1 billion dollars of research and development money already spent by the Department of Defense DoD on research seeking effective treatments for TBI and PTSD this author would suggest two options 1 Abandoning the pursuit of a sham hyperbaric control group and prioritizing the data from the wait list group in the DoD HOPP study10 Wolf and coworkers1 mention a wait list group in their recommendations for future studies This option is based on the physical impossibility of controlling for a chamber experience because of the inability to control for pressure no method to duplicate middle ear pressure changes without placement of pressure equalization tubes and no commercially available mechanisms to duplicate adiabatic heating and cooling on compression and decompression Continued attempts at a sham pressure control group will only further confuse the scientific and lay community and 2 an economical Civilian DoD Veterans Affairs VA off label networked hyperbaric treatment program using a Medicare like Coverage with Evidence Development52 pathway The safety of HBOT 1 5 and even higher doses is not in issue hyperbaric oxygen therapy in mTBI PCS PTSD has satisfied one of the cardinal rules of medicine First Do No Harm The Coverage with Evidence pathway would allow the DoD and VA to immediately begin treating active military and veteran casualties with hyperbaric therapy in both military and civilian clinics hospitals such that this health and quality of life improving therapy can be delivered without further delay to the hundreds of thousands of injured PCS PTSD casualties and veterans now in need Author Disclosure Statement Dr Harch owns a small consulting company Harch Hyperbarics Inc and is president of a non profit corporation The International Hyperbaric Medical Foundation IHMF He derives no income salary or benefits from the IHMF References 1 Wolf G Cifu D Baugh L Carne W and Profenna L 2012 The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury J Neurotrauma 29 2606 2612 2 Gesell L B ed 2009 Hyperbaric Oxygen Therapy Indications 12th ed The Hyperbaric Oxygen Therapy Committee Committee Report Undersea and Hyperbaric Medical Society Durham NC pps 4 5 3 Harch P G and Neubauer R A 1999 Hyperbaric oxygen therapy in global cerebral ischemia anoxia and coma in Chapter 18 Textbook of Hyperbaric Medicine 3rd revised ed K K Jain ed Hogrefe and Huber Publishers Seattle pps 319 345 4 Godman C A Chheda K P Hightower L E Perdrizet G Shin D G and Giardina C 2010 Hyperbaric oxygen induces a cytoprotective and angiogenic response in human microvascular endothelial cells Cell Stress Chaperones 15 431 442 5 Chen Y Nadi N S Chavko M Auker C R and McCarron R M 2009 Microarray analysis of gene expression in rat cortical neurons exposed to hyperbaric air and oxygen Neurochem Res 34 1047 1056 6 Kendall A C Whatmore J L Harries L W Winyard P G Eggleton P and Smerdon G R 2013 Different oxygen treatment pressures alter inflammatory gene expression in human endothelial cells Undersea Hyper Med 40 115 123 7 Jain K K 2004 The history of hyperbaric medicine in Textbook of Hyperbaric Medicine 4th revised and expanded edition K K Jain ed Hogrefe and Huber Publishers Cambridge MA pps 3 8 8 Dean J B Mulkey D K Garcia A J III Putnam R W and Henderson R A III 2003 Neuronal sensitivity to hyperoxia hypercapnia and inert gases at hyperbaric pressures J Appl Physiol 95 883 909 HARCH 9 Macdonald A G and Fraser P J 1999 The transduction of very small hydrostatic pressures Comp Biochem Physiol A Mol Integr Physiol 122 13 36 10 Weaver L K Cifu D Hart B Wolf G and Miller S 2012 Hyperbaric oxygen for post concussion syndrome design of Department of Defense clinical trials Undersea Hyperb Med 39 807 814 11 Trimble V H 1974 The Uncertain Miracle Hyperbaric Oxygenation Doubleday Company Inc Garden City NY 12 Dowell R T and McManus R E III 1978 Pressure induced cardiac enlargement in neonatal and adult rats Left ventricular functional characteristics and evidence of cardiac muscle cell proliferation in the neonate Circ Res 42 303 310 13 Hishikawa K Nakaki T Marumo T Hayashi M Suzuki H Kato R and Saruta T 1994 Pressure promotes DNA synthesis in rat cultured vascular smooth muscle cells J Clin Invest 93 1975 1980 14 Mattana J and Singhal P C 1995 Applied pressure modulates mesangial cell proliferation and matrix synthesis Am J Hypertens 8 1112 1120 15 Teiger E Than V D Richard L Wisnewsky C Tea B S Gaboury L Tremblay J Schwartz K and Hamet P 1996 Apoptosis in pressure overload induced heart hypertrophy in the rat J Clin Invest 97 2891 2897 16 Kramer M R Springer C Berkman N Glazer M Bublil M BarYishay E and Godfrey S 1998 Rehabilitation of hypoxemic patients with COPD at low altitude at the Dead Sea the lowest place on earth Chest 113 571 575 17 Kawata Y Mizukami Y Fujii Z Sakumura T Yoshida K and Matsuzaki M 1998 Applied pressure enhances cell proliferation through mitogen activated protein kinase activation in mesangial cells J Biol Chem 273 16905 16912 18 Agar A Yip S S Hill M A and Coroneo M T 2000 Pressure related apoptosis in neuronal cell lines J Neurosci Res 60 495 503 19 Dean J B and Mulkey D K 2000 Continuous intracellular recording from mammalian neurons exposed to hyperbaric helium oxygen or air J Appl Physiol 89 807 822 20 Heal R D Rogers A T Lunt G G Pointer S A and Parsons A T 2001 Development of a neuronal pressure sensor Biosens Bioelectron 16 905 909 21 Collet J P Vanasse M Marois P Amar M Goldberg J Lambert J Lassonde M Hardy P Fortin J Tremblay S D Montgomery D Lacroix J Robinson A and Majnemer A HBO CP Research Group 2001 Hyperbaric oxygen for children with cerebral palsy a randomized multicentre trial Lancet 357 582 586 22 Yu H A I Tian R L Pan X W Luan Z and Song L W 2002 Effects of hyperbaric oxygen on brain bFGF and bFGF mRNA expression of neonatal rats after hypoxia ischemia injury in The Proceedings of the 2nd International Symposium on Hyperbaric Oxygenation for Cerebral Palsy and the Brain Injured Child J T Joiner ed Best Publishing Co Flagstaff pps 57 66 23 Heuser G Heuser S A Rodelander D Aguilera O and Uszler M 2002 Treatment of neurologically impaired adults and children with mild hyperbaric oxygen 1 3ATA and 24 oxygen in The Proceedings of the 2nd International Symposium on Hyperbaric Oxygenation for Cerebral Palsy and the Brain Injured Child J T Joiner ed Best Publishing Co Flagstaff pps 109 116 24 Kazantseva N V 2002 Mechanisms of curative effect of minimized hyperbaric treatment in cerebral ischemia in The Proceedings of the 2nd International Symposium on Hyperbaric Oxygenation for Cerebral Palsy and the Brain Injured Child J T Joiner ed Best Publishing Co Flagstaff pps 199 212 25 Rusyniak D E Kirk M A May J D Kao L W Brizendine E J Welch J L Cordell W H and Alonso R J 2003 Hyperbaric oxygen therapy in acute ischemic stroke results of the Hyperbaric Oxygen in Acute Ischemic Stroke Trial Pilot Study Stroke 34 571 574 26 Stanley A C Lounsbury K M Corrow K Callas P W Zhar R Howe A K and Ricci M A 2005 Pressure elevation slows the fibroblast response to wound healing J Vasc Surg 42 546 551 27 Rossignol D A Rossignol L W Smith S Schneider C Logerquist S Usman A Neubrander J Madren E M Hintz G Grushkin B and Mumper E A 2009 Hyperbaric treatment for children with autism a multicenter randomized double blind controlled trial BMC Pediatr 13 9 21
International Journal of Athletic Therapy and Training 2021 26 140 144 https doi org 10 1123 ijatt 2019 0135 2021 Human Kinetics Inc CLINICAL CASE REPORT Hyperbaric Oxygen Therapy to Treat Acute Sport Related Traumatic Brain Injuries A Case Series Patricia R Roby PhD ATC 1 Robert C Lynall PhD ATC 2 Michael J Cools MD 1 Stephen W Marshall PhD 1 Janna C Fonseca MEd ATC 3 James R Stevens MD 3 and Jason P Mihalik PhD CAT C ATC FACSM FNATA1 1 The University of North Carolina at Chapel Hill 2University of Georgia 3Carolina Family Practice Sports Medicine We report on hyperbaric oxygen HBO2 therapy used to improve postinjury outcomes in eight acutely concussed high school student athletes 5 males 3 females mean age 16 0 1 2 years Patients were randomly assigned into one of three intervention groups a HBO2 therapy b hyperbaric therapy with compressed medical grade air HBA or c normobaric 100 O2 therapy All patients completed ve 1 hr treatments within the rst 10 days following his or her concussion Main outcome measures included mental status examination symptom burden and the number of days from injury until the physician permitted the student athlete to return to activity Patients receiving HBO2 treatment experienced the greatest absolute symptom reduction over the ve treatment sessions No meaningful differences were found in mental status examination All participants returned to activity in a similar timeframe HBO2 therapy may be an effective option for the acute treatment of postconcussion symptoms particularly in young athletes presenting with a high symptom burden Keywords adolescent concussion symptoms Student athletes typically experience de cits in neurocognitive function motor control and an array of clinical symptoms following concussion 1 Insult to the neural tissue causes changes in cellular and physiological function resulting in a loss of energy stores coupled with decreased cerebral blood ow 2 The resulting mismatch between KEY POINTS supply and demand results in a potentially damaging energy Consensus statements have crisis which has been associrecently moved away from strict rest ated with migraine like sympfollowing concussion toms headaches dizziness photophobia phonophobia Treatments aimed at reducing initial symptom burden may reduce and nausea 2 Elevated symprecovery times tom endorsement3 and greater symptom severity4 at the time Hyperbaric oxygen therapy may be of injury i e symptom buran effective treatment in high school den have been associated athletes with prolonged recovery following concussion Clinicians could plausibly improve recovery times by addressing this initial symptom burden Consensus statements have only recently deviated from longtime recommendations encouraging rest until Roby and Mihalik are with the Department of Exercise and Sport Science Matthew Gfeller Sport Related Traumatic Brain Injury Research Center The University of North Carolina at Chapel Hill Chapel Hill NC USA and Human Movement Science Curriculum Department of Allied Health Sciences The University of North Carolina at Chapel Hill Chapel Hill NC USA Lynall is with UGA Concussion Research Laboratory Department of Kinesiology University of Georgia Athens GA USA Cools and Mihalik are with the Department of Neurosurgery The University of North Carolina at Chapel Hill Chapel Hill NC USA Marshall is with the Injury Prevention Research Center The University of North Carolina at Chapel Hill Chapel Hill NC USA Fonseca and Stevens are with Carolina Family Practice Sports Medicine Raleigh NC USA Mihalik jmihalik email unc edu is corresponding author symptom resolution Thus there are limited data demonstrating the concussion treatments that will bene t young athletes the most Using hyperbaric oxygen HBO2 therapy as a medical treatment to support and accelerate the body s own healing mechanisms to speed recovery from injury surgery or chronic illness has been well established 5 9 Using HBO2 therapy has demonstrated bene ts in animal studies 10 as well as those suffering from moderate to severe traumatic brain injury 11 Unfortunately it has not been adequately studied as an acute concussion treatment Giza and Hovda2 previously described the neurometabolic cascade resulting from concussion During the days immediately following head trauma cerebral blood ow which carries oxygen required by tissues to survive and repair may be reduced to 50 of normal 12 13 Using HBO2 therapy may mitigate the reduced cerebral blood ow observed following concussion by supersaturating the tissues with oxygen In this case series we describe the effect of HBO2 therapy on reducing initial symptom burden in acutely concussed high school student athletes compared to two different placebo treatments a 100 O2 normobaric therapy and b hyperbaric therapy with medical grade air Case Series Patients This case series presents eight cases three randomly assigned to hyperbaric therapy with 100 oxygen HBO2 three randomly assigned to hyperbaric therapy with medical grade air HBA and two randomly assigned to 100 O2 normobaric therapy The patients 140 Unauthenticated Downloaded 01 21 22 10 41 PM UTC
Hyperbarics and Concussion A Novel Approach included in this case series were referred to a community based family practice facility by his or her school s athletic trainer if they experienced signs and symptoms consistent with concussion Once referred a systematic and protocolled concussion evaluation was performed Every physician rendering a concussion diagnosis was board certi ed in family medicine and had completed a sports medicine fellowship They were all experienced in evaluating and managing sport related concussion Once a student athlete was diagnosed with concussion the study protocol and objectives were discussed with the patient and their legal guardian After eligibility was con rmed see Table 1 for exclusion criteria legal guardians provided informed consent and participants provided minor assent on forms approved by the Of ce of Human Research Ethics at the University of North Carolina at Chapel Hill Examination We employed the Postconcussion Symptom Scale PCSS and Standardized Assessment of Concussion SAC to measure symptoms and mental status respectively The PCSS checklist is a selfreported symptom assessment that measures the presence and severity of 22 symptoms Symptoms are scored on a 7 point Likert scale ranging from 0 no symptom to 6 severe symptom Table 2 14 15 The SAC was designed to be a brief sideline concussion assessment and is sensitive and speci c to even the mildest concussion in the absence of observable injury signs 16 20 These outcomes were measured at initial visit and each follow up visit during the recovery process until such time that the physician permitted the student athlete to return to activity Our main outcomes also included the number of days from injury until cleared for activity which was de ned as the day a physician cleared an athlete to return to team workouts and regularly scheduled team practices We selected return to activity as the endpoint because this represents a readily documented clinical decision and we were concerned that day of return to full contact may be harder to document in our community sports teams Intervention Following consent participants were randomly assigned and blinded to a treatment group Cards with random treatment group assignments were created and participants were sequentially assigned as they enrolled in the study Group assignment was not shared with the participants or his her treating physicians Additionally our participants did not obtain nor were they prescribed any concurrent treatments during the initial 10 days of their injury management The three treatment groups were as follows Table 1 141 a HBO2 therapy treatment at 1 5 atmospheres 100 O2 at pressure equal to 15 ft below sea level b hyperbaric therapy with medical grade air HBA treatment at 1 5 atmospheres medical grade air and c 100 O2 therapy with negligible pressure Due to the same relative pressures for HBO2 and HBA participants were unable to tell the difference and thus blinded to the treatment arm they were randomly assigned Negligible pressure in the O2 therapy group was provided by increasing the pressure inside the chamber until the participant reported feeling their ears pop those pressures were not high enough to affect oxygen diffusion The participant received the feeling of pressure being applied and thus was blinded to the treatment arm The intervention was administered in a facility independent of the primary care clinic All participants and all members of the medical care teams were blinded to treatment group All patients received ve 1 hr sessions within 10 days of sustaining his or her concussion with no more than 1 day between any two treatments regardless of treatment arm Prior to each treatment session all participants completed the PCSS Participants completed the SAC and repeated the PCSS immediately after each treatment session Regardless of treatment arm patients were placed in a SIGMA 40 Monoplace Hyperbaric System Perry Baromedical Corporation Riviera Beach FL equipped with a safety interlock system and monitored by a Certi ed Hyperbaric Technician The monoplace chamber for all patients is pressurized with 100 oxygen All patients wore a non rebreather mask which allowed air to be delivered directly to the patient while Table 2 Postconcussion Symptom Scale PCSS Symptoms Symptoms Headache Nausea Emesis Balance problems Dizziness Fatigue Trouble falling asleep Sleeping more than usual Sleeping less than usual Drowsiness Irritability Sensitivity to light Sensitivity to noise Increased sadness Nervousness Feeling more emotional Numbness or tingling Feeling slowed down Sensation of being in a fog Dif culty with concentration Dif culty with memory Visual problems Exclusion Criteria Criteria Loss of consciousness for 20 min at time of injury Glasgow Coma Scale 13 at time of injury Evidence of drug use Concurrent injury e g fractures sprains etc Current hospitalization History of nitrogen dioxide poisoning emphysema shock lung disease disorder and pneumothorax History of attention de cit disorders and learning disabilities Claustrophobia These exclusion criteria were speci c to employing the hyperbaric oxygen chambers IJATT Vol 26 No 3 2021 Unauthenticated Downloaded 01 21 22 10 41 PM UTC
142 Roby et al preventing the patient from breathing the air gases used to pressurize the monoplace chamber The monoplace chamber was compressed with 100 oxygen to a pressure of 1 5 atmospheres at a rate of 1 psi min Treatments lasted 60 min at 1 5 atmospheres followed by decompression of the chamber at a rate of 1 psi min Comparative Outcomes Eight patients 3 females 5 males mean age 16 0 1 2 years and their legal guardians consented to participate in this study Table 3 No adverse events were noted for any patient The most common sport played was soccer 4 8 with the remaining athletes sustaining a concussion while competing in baseball cheer lacrosse or volleyball We computed clinically relevant descriptive data and present them in our case series results and the associated tables and gures Given we present a case series without the sample size expected of a traditional scienti c study we were unable to perform formal statistical comparisons between the treatment arms Total SAC score remained consistent throughout the ve testing sessions for all treatments Figure 1 HBO2 Therapy Overall the participants receiving HBO2 therapy returned to activity in an average of 13 7 5 1 days median 15 days range 8 18 days Following ve 1 hr treatment Table 3 HBA Therapy Average time to return to activity for the participants receiving HBA therapy was 13 0 5 7 days median 13 days range 9 17 days Following ve 1 hr treatment sessions patient 2 experienced a 14 point reduction in total symptom score initial score 16 nal score 2 87 5 reduction and patient 5 experienced a 30 point reduction in total symptom score initial score 37 nal score 7 81 1 reduction O2 Therapy Patients receiving O2 therapy returned to activity in an average of 19 0 16 5 days median 11 days range 8 38 days Following ve 1 hr treatment sessions patient 1 experienced a 20 point reduction in total symptom score initial score 24 nal score 4 83 3 reduction and patient 8 experienced a 22 point reduction in total symptom score initial score 23 nal score 1 95 7 reduction Patient 4 did not report for their nal treatment session but experienced a 41 point reduction in total symptom score following four 1 hr Demographic Information and Patient Histories Patient Groupa 1 2 3 4 5 6 7 8 sessions patient 3 experienced a total symptom score reduction of 37 points initial score 41 nal score 4 90 2 reduction patient 6 experienced a total symptom score reduction of 7 points initial score 9 nal score 2 77 8 reduction and patient 7 experience a total symptom score reduction of 72 initial score 77 nal score 5 93 5 reduction O2 HBA HBO2 O2 HBA HBO2 HBO2 O2 Age years Sex 17 15 17 18 15 16 15 15 F F M M M M M F Sport of Previous Concussions Days Between Injury and First Treatment Days Until Cleared for Activity Symptom Score Reductionb Soccer Volleyball Lacrosse Soccer Soccer Soccer Baseball Cheer 4 0 1 0 0 1 0 0 3 3 3 3 4 2 4 4 11 17 15 8 9 8 18 38 20 14 37 41c 30 7 72 22 a Group assignment identi ed as follows a O2 treatment group received 100 oxygen at normobaric pressure b HBA treatment group received medical grade air at 1 5 atmospheric pressure and c HBO2 treatment group received 100 oxygen at 1 5 atmospheric pressure bSymptom score reduction represents the improvement positive values represent decreased burden measured after completing the fth therapy session relative to their initial score cPatient 4 did not report for their nal treatment session reduction follows four treatment sessions Figure 1 Change in clinical outcomes Total symptom score A and total Standardized Assessment of Concussion SAC score B for each patient following ve treatment sessions HBO2 hyperbaric oxygen therapy HBA 1 5 atmospheres of pressure with medical grade air O2 100 oxygen IJATT Vol 26 No 3 2021 Unauthenticated Downloaded 01 21 22 10 41 PM UTC
Hyperbarics and Concussion A Novel Approach treatment sessions initial score 44 nal score 3 93 1 reduction Discussion We performed this study to determine if HBO2 therapy could be an effective treatment for acute concussion in high school studentathletes Though all patients experienced similar reductions in total symptom severity score patients receiving HBO2 experienced the greatest absolute change in total symptom score following ve 1 hr treatments Additionally some but not all patients receiving HBO2 therapy also saw the greatest pre to posttreatment improvements in symptom scores within each therapy session Our results suggest that HBO2 therapy may be an effective treatment to address initial symptom burden for high school student athletes suffering from concussion Of those receiving HBO2 treatment patient 7 initial symptom score 77 was markedly more symptomatic at the beginning of the trial relative to those receiving HBA or O2 yet recovered to the same degree as the other patients by the fth treatment Patient 3 reported a greater initial total symptom score than average21 and recovered in a similar time to participants receiving other treatment Initial symptom burden has been associated with prolonged or complex recoveries following concussion 3 4 22 McCrea et al 3 found athletes reporting total symptom severity scores 20 from baseline on immediate testing 2 3 hr postinjury and 1 day postinjury had 2 56 2 89 and 4 14 times greater risk of prolonged recovery respectively By actively addressing initial symptom burden HBO2 therapy may be effective in reducing the risk of prolonged or complicated recovery Additionally we found no meaningful changes in SAC total scores The average score for each patient at initial evaluation was similar to normative values suggesting either that the participants did not report postinjury de cits in mental status or that the participants mental status had recovered by the time SAC was administered From initial evaluation to the fth treatment session SAC total scores remained within 1 standard deviation of normative values for this age group 23 suggesting hyperbaric or normobaric oxygen therapy does not negatively affect mental status as measured by the SAC We caution that our data supporting HBO2 therapy as an acute concussion treatment require substantial follow up studies to support ef cacy Off label HBO2 treatments may cost as much as 300 400 for a 90 min treatment 24 Determining the optimum protocol for treating concussions will require studying considerably more patients employing the randomized controlled trial designs we propose in this case series investigation Clinical Bottom Line The standard of care for athletes suffering from sport related concussion had long consisted of both physical and cognitive rest until their self reported symptoms resolved and objective clinical measures of concussion show signs of recovery This standard of care provides little to no active treatment options beyond a passive wait and see approach for which clinicians have very little evidence based understanding More recent guidelines25 have softened this stance to permit symptom limited activity during the rst stage of the patient s return to sport strategy Our understanding of innovative acute treatment options will continue to evolve with emerging science addressing these clinical 143 challenges This case series presents formative data suggesting that HBO2 therapy may be effective in reducing initial symptom burden in the acute stages following sport related concussion in adolescent athletes Future research should continue investigating acute interventions such as HBO2 therapy targeted at minimizing the risks of developing persistent complications related to concussion in young athletes Acknowledgments This case series was funded by the National Operating Committee on Standards for Athletic Equipment NOCSAE The results of this case series do not constitute endorsement by the NOCSAE The results of the case series are presented clearly honestly and without fabrication falsi cation or inappropriate data manipulation The authors have no con icts of interests to disclose related to this case series References 1 Broglio SP Cantu RC Gioia GA et al National Athletic Trainers Association position statement management of sport concussion J Athl Train 2014 49 2 245 265 PubMed ID 24601910 doi 10 4085 1062 6050 49 1 07 2 Giza CC Hovda DA The new neurometabolic cascade of concussion Neurosurgery 2014 75 suppl S24 S33 doi 10 1227 NEU 0000000000000505 3 McCrea M Guskiewicz K Randolph C et al Incidence clinical course and predictors of prolonged recovery time following sportrelated concussion in high school and college athletes J Int Neuropsychol Soc 2013 19 1 22 33 PubMed ID 23058235 doi 10 1017 S1355617712000872 4 Meehan WP Mannix RC Stracciolini A Elbin RJ Collins MW Symptom severity predicts prolonged recovery after sport related concussion but age and amnesia do not J Pediatr 2013 163 3 721 725 PubMed ID 23628374 doi 10 1016 j jpeds 2013 03 012 5 Hargens AR Schmidt DA Evans KL et al Quantitation in a model of skeletal compartment necrosis syndrome J Bone Joint Surg 1981 63 4 631 636 PubMed ID 7217130 doi 10 2106 00004623198163040 00014 6 Pierce AK Assisted respiration Annu Rev Med 1969 20 1 431 448 PubMed ID 4893408 doi 10 1146 annurev me 20 020169 002243 7 Bird AD Telfer ABM Effect of hyperbaric oxygen on limb circulation Lancet 1965 285 7381 355 356 doi 10 1016 S01406736 65 91783 6 8 Nylander G Nordstrtim H Eriksson E Effects of hyperbaric oxygen on oedema formation after a scald burn Burns 1984 10 3 193 196 http ac els cdn com 0305417984900263 1 s2 0 0305417984900263main pdf _tid ea6c6098 7d1c 11e7 88cf 00000aacb360 acdnat 150 2295060_8e322e278c41c998b522f5af014eae31 Accessed August 8 2017 doi 10 1016 0305 4179 84 90026 3 9 Sukoff M Ragatz RE Hyperbaric oxygenation for the treatment of acute cerebral edema Neurosurgery 1982 10 1 29 38 PubMed ID 7057975 10 Huang L Obenaus A Hamer M Zhang JH Neuroprotective effect of hyperbaric oxygen therapy in a juvenile rat model of repetitive mild traumatic brain injury Med Gas Res 2016 6 4 187 193 PubMed ID 28217290 doi 10 4103 2045 9912 196900 11 Wang F Wang Y Sun T Yu H L Hyperbaric oxygen therapy for the treatment of traumatic brain injury a meta analysis Neurol Sci 2016 37 5 693 701 PubMed ID 26746238 doi 10 1007 s10072015 2460 2 IJATT Vol 26 No 3 2021 Unauthenticated Downloaded 01 21 22 10 41 PM UTC
144 Roby et al 12 Yamakami I McIntosh TK Effects of traumatic brain injury on regional cerebral blood ow in rats as measured with radiolabeled microspheres J Cereb Blood Flow Metab 1989 9 1 117 124 PubMed ID 2910893 doi 10 1038 jcbfm 1989 16 13 Yuan XQ Prough DS Smith TL Dewitt DS The effects of traumatic brain injury on regional cerebral blood ow in rats J Neurotrauma 1988 5 4 289 301 PubMed ID 3249308 doi 10 1089 neu 1988 5 289 14 Broglio SP Macciocchi SN Ferrara MS Sensitivity of the concussion assessment battery Neurosurgery 2007 60 6 1050 1058 PubMed ID 17538379 doi 10 1227 01 NEU 0000255479 90999 C0 15 Patel AV Mihalik JP Notebaert AJ Guskiewicz KM Prentice WE Neuropsychological performance postural stability and symptoms after dehydration J Athl Train 2007 42 1 66 75 PubMed ID 17597946 16 McCrea M Standardized mental status assessment of sports concussion Clin J Sport Med 2001 11 3 176 181 PubMed ID 11495322 doi 10 1097 00042752 200107000 00008 17 McCrea M Kelly JP Randolph C Cisler R Berger L Immediate neurocognitive effects of concussion Neurosurgery 2002 50 5 1032 1040 PubMed ID 11950406 doi 10 1097 00006123 20020 5000 00017 18 McCrea M Kelly JP Randolph C et al Standardized assessment of concussion SAC on site mental status evaluation of the athlete J Head Trauma Rehabil 1998 13 2 27 35 PubMed ID 9575254 doi 10 1097 00001199 199804000 00005 19 McCrea M Kelly JP Kluge J Ackley B Randolph C Standardized assessment of concussion in football players Neurology 20 21 22 23 24 25 1997 48 3 586 588 PubMed ID 9065531 doi 10 1212 WNL 48 3 586 Barr WB McCrea M Sensitivity and speci city of standardized neurocognitive testing immediately following sports concussion J Int Neuropsychol Soc 2001 7 6 693 702 PubMed ID 11575591 doi 10 1017 S1355617701766052 Meehan WP Mannix R Monuteaux MC Stein CJ Bachur RG Early symptom burden predicts recovery after sport related concussion Neurology 2014 83 24 2204 2210 PubMed ID 25381296 doi 10 1212 WNL 0000000000001073 Lau B Lovell MR Collins MW Pardini J Neurocognitive and symptom predictors of recovery in high school athletes Clin J Sport Med 2009 19 3 216 221 PubMed ID 19423974 doi 10 1097 JSM 0b013e31819d6edb Valovich McLeod TC Bay RC Lam KC Chhabra A Representative baseline values on the Sport Concussion Assessment Tool 2 SCAT2 in adolescent athletes vary by gender grade and concussion history Am J Sports Med 2012 40 4 927 933 doi 10 1177 03635465114 31573 Tibbles PM Edelsberg JS Hyperbaric oxygen therapy N Engl J Med 1996 334 25 1642 1648 PubMed ID 8628361 doi 10 1056 NEJM199606203342506 McCrory P Meeuwisse W Dvo k J et al Consensus statement on concussion in sport the 5th international conference on concussion in sport held in Berlin October 2016 Br J Sports Med 2017 51 11 838 847 PubMed ID 28446457 doi 10 1136 bjsports2017 097699 IJATT Vol 26 No 3 2021 Unauthenticated Downloaded 01 21 22 10 41 PM UTC
Research Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of posttraumatic brain injury patients retrospective analysis Amir Hadanny 1 2 3 4 Stefanie Abbott 2 Gil Suzin 2 Yair Bechor 2 Shai Efrati2 4 5 6 To cite Hadanny A Abbott S Suzin G et al Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post traumatic brain injury patients retrospective analysis BMJ Open 2018 8 e023387 doi 10 1136 bmjopen 2018 023387 Prepublication history for this paper is available online To view these files please visit the journal online http dx doi org 10 1136 bmjopen 2018 023387 EUBS 2017 EANS 2017 Received 5 April 2018 Revised 27 June 2018 Accepted 24 July 2018 Author s or their employer s 2018 Re use permitted under CC BY NC No commercial re use See rights and permissions Published by BMJ 1 Neurosurgery Department Galilee Medical Center Nahariya Israel 2 Sagol Center for Hyperbaric Medicine and Research Assaf Harofeh Medical Center Zerifin Israel 3 Galilee Faculty of Medicine Bar Ilan University Ramat Gan Israel 4 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 5 Research and Development Unit Assaf Harfoeh Medical Center Zerifin Israel 6 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Correspondence to Dr Amir Hadanny amir had gmail com Abstract Objectives The aim of the study is to evaluate the effect of hyperbaric oxygen therapy HBOT in participants suffering from chronic neurological deficits due to traumatic brain injury TBI of all severities in the largest cohort evaluated so far with objective cognitive function tests and metabolic brain imaging Methods A retrospective analysis was conducted of 154 patients suffering from chronic neurocognitive damage due to TBI who had undergone computerised cognitive evaluations pre HBOT and post HBOT treatment Results The average age was 42 7 14 6 years and 58 4 were men All patients had documented TBI 0 3 33 years mean 4 6 5 8 median 2 75 years prior to HBOT HBOT was associated with significant improvement in all of the cognitive domains with a mean change in global cognitive scores of 4 6 8 5 p
multiple brain areas 9 10 cognitive impairments are usually the predominant symptoms Global brain hypoperfusion and its related tissue ischaemia detected in patients suffering from TBI serves as a rate limiting factor for any regenerative process 11 13 By increasing the oxygen level in blood and body tissues HBOT can augment the repair mechanisms 5 Various models have strongly suggested that HBOT can induce angiogenesis improve brain plasticity enhance neurogenesis and synaptogenesis and foster functional recovery 14 15 Conflicting clinical HBOT data and objective measurements in PCS Some of the previous studies which evaluated the effect of HBOT on chronic neurological and cognitive impairments due to TBI mainly used self assessment questionnaires as their primary endpoints 16 18 Such endpoints have several inherent disadvantages First they lack an objective evaluation that is not biased by the patients perspectives Second self administrated questionnaires are exposed to various confounding variables such as litigation and compensation 19 Unlike the questionnaires standardised cognitive tests with high test retest reliability can and should be used as objective evaluations of neurocognitive impairments 20 In addition novel brain imaging techniques such as single photon emission computed tomography SPECT and perfusion sequences in MRI which evaluate cerebral blood flow and brain metabolism can shed new light in PCS diagnosis and in evaluating therapeutic interventions 20 In clinical studies which used objective cognitive assessments HBOT was found to induce significant improvements in patients suffering from PCS due to mild TBI 5 6 15 21 However to the best of our knowledge the objective effect of HBOT on chronic neurocognitive impairments stemming from moderate to severe TBI in addition to mild has not been investigated In addition to objective evaluations there are inherent ethical and logistic difficulties in handling the sham control in HBOT trials 4 5 20 22 HBOT includes two active ingredients pressure and oxygen Pressure is needed to increase plasma oxygen but the pressure change alone may also have significant cellular effects 5 Additionally the greatest effect of pressure is in human tissues that are under tight autoregulation pressure control such as the brain where the intracranial pressure is normally 0 0092 0 0197 atm 23 24 To generate a pressure sensation the chamber pressure must be 1 2 ATA or higher However such a change in environmental pressure from 1 ATA to 1 2 ATA and subsequent tissue oxygenation with an increase of tissue oxygenation by at least 50 has a significant biological effect 25 26 Thus sham therapy in previous studies using 1 2 ATA on 21 inhaled oxygen ie air cannot be regarded as an inert or sham control but rather as a lower dose of the active ingredient 4 20 In regards to a possible effect of vasoconstriction of the large blood vessels induced by hyperbaric oxygen it has been 2 well established that the tissues are saturated by hyperoxia and do not suffer from hypoxia as the vasoconstriction effect is compensated by increased plasma oxygen content and microvascular blood flow 27 Any increase in pressure even with reduced oxygen percentage cannot serve as a true placebo but rather as a low dosage of the active ingredient further supporting the need for objective data gathered from large cohorts of patients suffering from PCS and treated by HBOT The aim of the current study was to evaluate the objective effects of HBOT on patients with TBI suffering from chronic neurological deficits stemming from mild moderate and severe TBI in the largest cohort evaluated until now Since all the patients had metabolic brain imaging and a computerised neurocognitive test battery before and after HBOT correlations between specific cognitive indexes and their related brain regions activity were also evaluated Materials and methods Participants A retrospective analysis was conducted on patients suffering from TBI related chronic neurocognitive damage more than 3 months from injury treated by HBOT between January 2008 and January 2017 at the Sagol Center for Hyperbaric Medicine and Research Assaf Harofeh Medical Center Israel Patients were included if they had pre HBOT and post HBOT computerised cognitive evaluations Patients with a history of potential additional brain insults such as spontaneous subarachnoid haemorrhage anoxic brain injury or history of prior cognitive impairment were excluded figure 1 Patients and public involvement Patients and public weren t involved in the study due to its retrospective nature Figure 1 Patients flowchart TBI traumatic brain injury HBOT hyperbaric oxygen therapy Hadanny A et al BMJ Open 2018 8 e023387 doi 10 1136 bmjopen 2018 023387 BMJ Open first published as 10 1136 bmjopen 2018 023387 on 28 September 2018 Downloaded from http bmjopen bmj com on January 21 2022 by guest Protected by copyright Open access
TBI severity TBI severities were rated according to the TBI admission documents Mild TBI was defined as loss of consciousness LOC with duration of 0 30 min post traumatic amnesia PTA with duration of less than a day and a Glasgow Coma Scale GCS grade of 13 15 28 Moderate TBI was defined as LOC with duration of more than 30 min and up to 24 hours PTA with duration of 1 7 days and GCS grade of 9 12 Severe TBI was defined as LOC with duration of more than 24 hours PTA with duration of more than 7 days and GCS less than 9 In addition if there was imaging evidence of an injury such as a haematoma contusion or haemorrhage then the TBI was classified as moderate to severe 28 Hyperbaric oxygen treatment Patients were treated with 40 70 daily hyperbaric sessions 5 days a week Each session consisted of 60 90 minutes of exposure to 100 oxygen at 1 5 2 ATA Cognitive assessment The patients cognitive functions were assessed by NeuroTrax computerised cognitive tests NeuroTrax 29 The NeuroTrax tests evaluate various aspects of brain functions and include verbal memory immediate and delayed recognition non verbal memory immediate and delayed recognition go no go response inhibition problem solving Stroop interference finger tapping catch game staged information processing speed single digit two digit and three digit arithmetic verbal function and visual spatial processing Cognitive index scores were computed from the normalised outcome parameters for memory executive function attention information processing speed visual spatial verbal function and motor skills domains 30 A global cognitive score was computed as the average of all index scores for each individual After administration the NeuroTrax data were uploaded to the NeuroTrax central server and outcome parameters were automatically calculated using software blind to diagnosis or testing site To account for the wellknown effects of age and education on cognitive performance each outcome parameter was normalised and fit to an IQ like scale mean 100 SD 15 according to the patient s age and education The normative data used by NeuroTrax consist of test data from cognitively healthy individuals in controlled research studies at more than 10 sites 31 Specifically the patients were given two different versions of the NeuroTrax test battery before and after HBOT to allow repeated administrations with minimal learning effects Test retest reliability for these versions was evaluated and found to be high with no significant learning effect 32 33 Regarding the current study cohort in a previous randomised controlled trial in patients suffering from TBI the NeuroTrax scores were found to be stable in the retest of the control group 21 Hadanny A et al BMJ Open 2018 8 e023387 doi 10 1136 bmjopen 2018 023387 Brain SPECT imaging Brain activity was assessed using SPECT 1 2 weeks prior to and after the HBOT period The SPECT method was selected for evaluation due to its known normal range and test retest established validity The imaging was conducted using 925 1110 MBq 25 30 mCi of a technetium 99 methyl cysteinate dimmer Tc 99m ECD at 40 60 min postinjection using a dual detector gamma camera ECAM or Symbia T Siemens Medical Systems equipped with high resolution collimators Data were acquired in three degree steps and reconstructed iteratively using the Chang method of attenuation correction 0 12 cm 34 Both pretreatment and post treatment SPECT images were normalised to the median maximal brain activity in the entire brain and were then reoriented into Talairach space using NeuroGam software Segami to identify Brodmann cortical areas and to compute the mean perfusion in each Brodmann area BA In addition volume rendered brain perfusion images were reconstructed and normalised to the entire brain median maximal activity All SPECT analyses were done by study team members who were blinded to the laboratory and clinical data SPECT scans were performed late morning to midday On the day of the SPECT scan patients were treated with only their chronic medications and were instructed not to smoke Changes in perfusion in all Brodmann areas for each subject were determined by calculating the percentage of the difference of the normalised activity values between post treatment and pretreatment divided by the pretreatment value Statistical analysis Continuous data were expressed as means SDs The normal distribution for all variables was tested using the Kolmogorov Smirnov test The mean differences between cognitive index scores before and after HBOT were analysed using one way analysis of variance ANOVA with post hoc Bonferroni tests Multiple linear regression models and multivariate logistic regression models were performed to control for potential confounders and to determine independent predictors for clinical outcome The alpha level was set to 0 05 Data were statistically analysed using SPSS software V 22 0 Results Patient profiles Of the 242 patients suffering from neurocognitive impairment due to TBI treated by HBOT between January 2008 and January 2017 25 patients had potential additional brain insults and 63 did not have repeat computerised neurocognitive evaluations Therefore 154 patients were included in the final analysis of whom 100 patients completed pre HBOT and post HBOT SPECT imaging figure 1 The patients baseline characteristics are summarised in table 1 The average age was 42 7 14 6 years and 58 4 3 BMJ Open first published as 10 1136 bmjopen 2018 023387 on 28 September 2018 Downloaded from http bmjopen bmj com on January 21 2022 by guest Protected by copyright Open access
Table 1 Baseline patient characteristics Characteristics Total Mild TBI Moderate TBI Severe TBI Significance Patients n Age years 154 100 42 7 14 6 69 44 8 48 8 12 0 24 15 6 41 7 12 7 61 39 6 36 2 15 3
Table 2 Cognitive indices pre HBOT and post HBOT of the entire study cohort Baseline PostHBOT Mean change P values General Memory 88 3 15 2 81 7 23 2 92 9 14 2 89 9 21 9 4 6 8 5 8 1 16 9
Figure 4 Mean changes of post HBOT compared with pre HBOT across the different TBI severities Both patients who suffered mild and severe TBI groups had improvements in general memory attention information processing speed and motor skills scores whereas patients who suffered moderate TBI had significant improvement in memory P10 change in cognitive indices proportions across traumatic brain injury TBI groups General Memory Total Mild TBI 36 23 4 64 41 6 15 21 7 28 40 6 Moderate TBI Severe TBI P values 7 29 2 9 37 5 14 23 0 27 44 3 0 756 0 830 Executive functions 51 33 1 23 33 3 7 29 2 21 34 9 0 897 Attention Information processing speed 62 40 3 48 31 2 27 39 1 23 33 3 8 33 3 12 50 27 44 3 13 21 3 0 631 0 032 6 Hadanny A et al BMJ Open 2018 8 e023387 doi 10 1136 bmjopen 2018 023387 BMJ Open first published as 10 1136 bmjopen 2018 023387 on 28 September 2018 Downloaded from http bmjopen bmj com on January 21 2022 by guest Protected by copyright Open access
Figure 5 The mean relative change in Broadmann areas posthyperbaric oxygen therapy for the entire study cohort This study has several limitations The major one relates to its retrospective methodology This limitation is diminished when considering that this large cohort of patients was treated at late chronic stages The findings presented here are in agreement and reinforce the findings from previous prospective controlled trials in which the neuroplasticity effects of HBOT were demonstrated in chronic stages of different types of brain injuries 15 21 42 43 Moreover the correlation between the changes in cognitive function and the metabolic brain imaging gives further strength to the results Another important limitation relates to the HBOT protocol which was inconsistent across the cohort Although significant neurotherapeutic effects were seen with 60 min of 1 5 ATA the optimal protocol needed to induce maximal neuroplasticity for the specific individual with minimal side effects has not been investigated The strengths of the study are worth mentioning First objective cognitive assessments using computerised tests were performed on each patient both pretreatment and post treatment Objective measures are significantly superior to PCS questionnaires which are inaccurate variable and contain various confounders rather than reflect the true PCS state 44 Second most of the patients in the study underwent an objective ancillary brain SPECT to confirm PCS diagnosis prior to HBOT This practice is crucial when considering the differential diagnosis following TBI PTSD depression etc Moreover post treatment brain SPECTs revealed an anatomical functional correlation in regards to HBOT s Figure 6 Cognitive functions correlated with Brodmann areas Each of the traumatic brain injury TBI groups mild moderate and severe had perfusion metabolism increase in specific Brodmann areas correlated with improved cognitive function Hadanny A et al BMJ Open 2018 8 e023387 doi 10 1136 bmjopen 2018 023387 7 BMJ Open first published as 10 1136 bmjopen 2018 023387 on 28 September 2018 Downloaded from http bmjopen bmj com on January 21 2022 by guest Protected by copyright Open access
effect in brain neuroplasticity Third the study cohort consisted of a civilian population that does not have any potential secondary gain such as financial compensation by reporting sick Previous studies included patients with PCS who suffered mild TBI injury Considering its strengths and limitations the current study implies that the cognitive function of patients with post TBI can be improved significantly irrespectively of whether the primary brain injury was classified as mild moderate or severe Although long term data are still lacking considering the high safety profile of the treatment these results are promising and should encourage rehabilitation centres to consider HBOT for patients with chronic neurocognitive deficits following TBI Future studies should monitor these patients in the long term 6 months 12 months as well as their return to activities of daily living Conclusions HBOT was associated with significant cognitive improvements in patients who suffer from chronic neurocognitive deficits due to mild moderate and severe TBI Improvement in memory correlated with activation of the perirhinal cortex improvement of executive functions correlated with activation of the inferior frontal gyrus and improvement in attention correlated with activation of the anterior cingulate gyrus Contributors AH concept data collection data analysis manuscript draft and manuscript review SA data collection and data analysis GS YB data collection and manuscript review SE concept data analysis manuscript draft and manuscript review Funding This research received no specific grant from any funding agency in the public commercial or not for profit sectors Competing interests None declared Patient consent Data collected retrospectively were anonymised Ethics approval The study was approved by the institutional review board of Assaf Harfoeh Medical Center Israel Provenance and peer review Not commissioned externally peer reviewed Data sharing statement Extra data are available by emailing amir had gmail com Open access This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial CC BY NC 4 0 license which permits others to distribute remix adapt build upon this work non commercially and license their derivative works on different terms provided the original work is properly cited appropriate credit is given any changes made indicated and the use is non commercial See http creativecommons org licenses by nc 4 0 References 1 Coronado VG Xu L Basavaraju SV et al Surveillance for traumatic brain injury related deaths United States 1997 2007 MMWR Surveill Summ 2011 60 1 32 2 Bazarian JJ Wong T Harris M et al Epidemiology and predictors of post concussive syndrome after minor head injury in an emergency population Brain Inj 1999 13 173 89 3 Kashluba S Paniak C Blake T et al A longitudinal controlled study of patient complaints following treated mild traumatic brain injury Arch Clin Neuropsychol 2004 19 805 16 4 Figueroa XA Wright JK Hyperbaric oxygen B level evidence in mild traumatic brain injury clinical trials Neurology 2016 87 1400 6 8 5 Efrati S Ben Jacob E Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Rev Neurother 2014 14 233 6 6 Tal S Hadanny A Sasson E et al Hyperbaric oxygen therapy can induce angiogenesis and regeneration of nerve fibers in traumatic brain injury patients Front Hum Neurosci 2017 11 508 7 Medana IM Esiri MM Axonal damage a key predictor of outcome in human CNS diseases Brain 2003 126 Pt 3 515 30 8 Kochanek PM Clark RSB Jenkins LW TBI pathobiology In Zasler ND Katz DI Zafonte RD eds Brain injury medicine New York Demos medical publishing 2007 81 92 9 Kushner D Mild traumatic brain injury toward understanding manifestations and treatment Arch Intern Med 1998 158 1617 24 10 Sohlberg MM Mateer CA Cognitive rehabilitation an integrative neuropsychological approach New York The Guilford Press 2001 11 Kim J Whyte J Patel S et al Resting cerebral blood flow alterations in chronic traumatic brain injury an arterial spin labeling perfusion FMRI study J Neurotrauma 2010 27 1399 411 12 stergaard L Engedal TS Aamand R et al Capillary transit time heterogeneity and flow metabolism coupling after traumatic brain injury J Cereb Blood Flow Metab 2014 34 1585 98 13 Stein SC Graham DI Chen XH et al Association between intravascular microthrombosis and cerebral ischemia in traumatic brain injury Neurosurgery 2004 54 687 91 discussion 91 14 Jiang Q Zhang ZG Ding GL et al Investigation of neural progenitor cell induced angiogenesis after embolic stroke in rat using MRI Neuroimage 2005 28 698 707 15 Tal S Hadanny A Berkovitz N et al Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 2015 33 943 51 16 Wolf G Cifu D Baugh L et al The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury J Neurotrauma 2012 29 2606 12 17 Cifu DX Hoke KW Wetzel PA et al Effects of hyperbaric oxygen on eye tracking abnormalities in males after mild traumatic brain injury J Rehabil Res Dev 2014 51 1047 56 18 Miller RS Weaver LK Bahraini N et al Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms a randomized clinical trial JAMA Intern Med 2015 175 43 52 19 Smith Seemiller L Fow NR Kant R et al Presence of postconcussion syndrome symptoms in patients with chronic pain vs mild traumatic brain injury Brain Inj 2003 17 199 206 20 Hadanny A Efrati S Treatment of persistent post concussion syndrome due to mild traumatic brain injury current status and future directions Expert Rev Neurother 2016 16 875 87 21 Boussi Gross R Golan H Fishlev G et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 2013 8 e79995 22 Efrati S Ben Jacob E How and why hyperbaric oxygen therapy can bring new hope for children suffering from cerebral palsy an editorial perspective Undersea Hyperb Med 2014 41 71 6 23 Etzion Y Grossman Y Pressure induced depression of synaptic transmission in the cerebellar parallel fibre synapse involves suppression of presynaptic N type Ca2 channels Eur J Neurosci 2000 12 4007 16 24 Berman S Abu Hamad R Efrati S Mesangial cells are responsible for orchestrating the renal podocytes injury in the context of malignant hypertension Nephrology 2013 18 292 8 25 Fujita N Ono M Tomioka T et al Effects of hyperbaric oxygen at 1 25 atmospheres absolute with normal air on macrophage number and infiltration during rat skeletal muscle regeneration PLoS One 2014 9 e115685 26 Takemura A Ishihara A Mild hyperbaric oxygen inhibits growthrelated decrease in muscle oxidative capacity of rats with metabolic syndrome J Atheroscler Thromb 2017 24 26 38 27 Bhutani S Vishwanath G Hyperbaric oxygen and wound healing Indian J Plast Surg 2012 45 316 24 28 Malec JF Brown AW Leibson CL et al The mayo classification system for traumatic brain injury severity J Neurotrauma 2007 24 1417 24 29 Dwolatzky T Whitehead V Doniger GM et al Validity of a novel computerized cognitive battery for mild cognitive impairment BMC Geriatr 2003 3 4 30 Zur D Naftaliev E Kesler A Evidence of multidomain mild cognitive impairment in idiopathic intracranial hypertension J Neuroophthalmol 2015 35 26 30 31 Doniger GM Guide to normative data 2014 http www1 neurotrax com docs norms_ guide pdf Hadanny A et al BMJ Open 2018 8 e023387 doi 10 1136 bmjopen 2018 023387 BMJ Open first published as 10 1136 bmjopen 2018 023387 on 28 September 2018 Downloaded from http bmjopen bmj com on January 21 2022 by guest Protected by copyright Open access
32 Melton JL Psychometric evaluation of the Mindstreams neuropsychological screening tool Panama City Navy Experimental Diving Unit US 2005 33 Schweiger GMD A Dwolatzky T D Jaffe E S Simon reliability of a novel computerized neuropsychological battery for mild cognitive impairment Acta Neuropsychologica 2003 1 407 13 34 Jaszczak RJ Chang LT Stein NA et al Whole body single photon emission computed tomography using dual large field of view scintillation cameras Phys Med Biol 1979 24 1123 43 35 Hadanny A Golan H Fishlev G et al Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restor Neurol Neurosci 2015 33 471 86 36 Efrati S Fishlev G Bechor Y et al Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS One 2013 8 e53716 37 Chen J Zhang ZG Li Y et al Intravenous administration of human bone marrow stromal cells induces angiogenesis in the ischemic boundary zone after stroke in rats Circ Res 2003 92 692 9 Hadanny A et al BMJ Open 2018 8 e023387 doi 10 1136 bmjopen 2018 023387 38 Brown MW Aggleton JP Recognition memory what are the roles of the perirhinal cortex and hippocampus Nat Rev Neurosci 2001 2 51 61 39 Aron AR Robbins TW Poldrack RA Inhibition and the right inferior frontal cortex Trends Cogn Sci 2004 8 170 7 40 Miller EK Cohen JD An integrative theory of prefrontal cortex function Annu Rev Neurosci 2001 24 167 202 41 Bush G Luu P Posner MI Cognitive and emotional influences in anterior cingulate cortex Trends Cogn Sci 2000 4 215 22 42 Harch PG Hyperbaric oxygen in chronic traumatic brain injury oxygen pressure and gene therapy Med Gas Res 2015 5 9 43 Harch PG Andrews SR Fogarty EF et al A phase I study of low pressure hyperbaric oxygen therapy for blast induced postconcussion syndrome and post traumatic stress disorder J Neurotrauma 2012 29 168 85 44 Potter S Leigh E Wade D et al The rivermead post concussion symptoms questionnaire a confirmatory factor analysis J Neurol 2006 253 1603 14 9 BMJ Open first published as 10 1136 bmjopen 2018 023387 on 28 September 2018 Downloaded from http bmjopen bmj com on January 21 2022 by guest Protected by copyright Open access
Retrospective Clinical Research Report Hyperbaric oxygen for severe traumatic brain injury a randomized trial Journal of International Medical Research 48 7 1 12 The Author s 2020 Article reuse guidelines sagepub com journals permissions DOI 10 1177 0300060520939824 journals sagepub com home imr Xianliang Zhong1 Aijun Shan1 Jianzhong Xu1 Jian Liang2 Ying Long3 and Bo Du1 Abstract Objective The present study aimed to explore the effects of hyperbaric oxygen therapy on the prognosis and neurological function of patients with severe traumatic brain injury Methods A prospective study was carried out in 88 patients diagnosed with severe brain injury at our hospital and they were enrolled as research participants and randomly assigned to control and experimental groups n 44 per group using a random number table method Both groups underwent routine treatment Patients in the experimental group were administered hyperbaric oxygen therapy approximately 1 week after admission when their vital signs had stabilized Results No significant intergroup differences were observed in the Glasgow Coma Scale GCS and U S National Institutes of Health Stroke Scale NIHSS scores before treatment However after oxygen treatment compared with the control group the experimental group showed higher GCS and lower NIHSS scores The GCS score at admission tracheotomy status and first hyperbaric oxygen therapy duration were independent prognostic factors in patients with severe traumatic brain injury Conclusion Hyperbaric oxygen therapy may promote recovery of neurological function and improve the cognitive function and prognosis of patients with severe traumatic brain injury 3 1 Department of Emergency Shenzhen People s Hospital The Second Clinical Medical College of Jinan University The First Affiliated Hospital of Southern University of Science and Technology Shenzhen Guangdong China 2 Department of Neurosurgery Shenzhen People s Hospital The Second Clinical Medical College of Jinan University The First Affiliated Hospital of Southern University of Science and Technology Shenzhen Guangdong China Department of Hyperbaric Oxygen Shenzhen People s Hospital The Second Clinical Medical College of Jinan University The First Affiliated Hospital of Southern University of Science and Technology Shenzhen Guangdong China Corresponding author Bo Du Department of Emergency Shenzhen People s Hospital The Second Clinical Medical College of Jinan University The First Affiliated Hospital of Southern University of Science and Technology No 1017 Dongmen North Road Luohu District Shenzhen Guangdong 518020 China Email bodoyx 163 com Creative Commons Non Commercial CC BY NC This article is distributed under the terms of the Creative Commons Attribution NonCommercial 4 0 License https creativecommons org licenses by nc 4 0 which permits non commercial use reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages https us sagepub com en us nam open access at sage
2 Journal of International Medical Research Keywords Hyperbaric oxygen therapy brain injury recovery randomized trial neurological function cognitive function Date received 12 August 2019 accepted 15 June 2020 Introduction Brain injury is commonly associated with systemic trauma This type of injury accounts for approximately 20 of the overall trauma incidence in the entire body and is the most common form of disability 1 2 According to its severity brain injury can be categorized as mild moderate or severe The latter category includes extensive brain contusion and or skull fracture brainstem injury diffuse axonal injury and intracranial hematoma 3 4 Because severe brain injury is characterized by severe symptoms rapid progression sequelae and high disability and mortality rates it seriously threatens the survival and quality of life of affected patients 5 Accordingly severe brain injury is a focus of neurosurgical treatment 6 Most patients with mild moderate or severe brain injury mainly receive nonoperative treatments including mild hypothermia therapy and dehydration therapy 7 8 Hyperbaric oxygen therapy has previously been used to treat some types of brain injury 9 This therapy can rapidly correct and relieve brain anoxia and craniocerebral edema reduce intracranial pressure and improve the neurological function prognosis and quality of life of patients 10 11 However few reports have discussed the efficacy of hyperbaric oxygen therapy in patients with severe brain injury and its effects on their neurological function Therefore the present study primarily investigated and analyzed the efficacy of hyperbaric oxygen therapy for patients with severe brain injury by comparing its clinical efficacy with that of routine treatment and comprehensively analyzing the factors affecting the efficacy of hyperbaric oxygen therapy These findings provide an experiential reference regarding the application of hyperbaric oxygen therapy for severe brain injury Materials and methods Participants A prospective study was carried out in 88 patients diagnosed with severe brain injury at our hospital from May 2016 to December 2018 and they were enrolled as research participants and were divided into control and experimental groups n 44 per group using a random number table method Patients in both groups underwent routine treatment Patients in the experimental group received hyperbaric oxygen therapy approximately 1 week after admission when their vital signs had stabilized The patients enrolled comprised 47 males and 41 females aged between 18 and 60 years mean age 45 19 7 71 years The following inclusion criteria were applied a diagnosis of severe brain injury and Glasgow Coma Scale GCS score measured when admitted to the hospital and when the patient was treated with hyperbaric oxygen for 2 weeks between 3 and 8 points stable vital signs observed within 1 week after surgery during hospitalization with no active cranial bleeding as indicated by a computed tomography CT examination and the provision of signed informed consent by the participant or their family This study was approved by the Ethics Committee of Shenzhen People s Hospital
Zhong et al The Second Clinical Medical College of Jinan University approval number ChiCTR1800015678 approval date December 2018 The following exclusion criteria were applied a history of cerebral hemorrhage cerebral infarction and or brain injury concurrent organ diseases such as heart liver and kidney disease or combined tumor acute infection diabetes severe organ failure mental disease or physical disability death within 2 weeks after the trauma event transfer to another hospital and pregnancy 3 chamber pressure of 0 20 to 0 25 MPa was chosen followed by pressurization for 20 minutes oxygen inhalation with constant pressure for 80 minutes and decompression for 20 minutes Both groups of patients were treated once a day for 2 weeks During hyperbaric oxygen therapy professional nurses closely monitored the patients and immediately suspended treatment if a serious adverse reaction or an event reflecting intolerance of hyperbaric oxygen therapy occurred Observation indices Treatment methods Both groups were intensively and continuously monitored during the early postadmission period All patients underwent decompressive craniectomy The care administered to the control group included electrocardiographic intracranial pressure cerebral blood flow and oxygen saturation monitoring When necessary patients in the control group received oxygen via positive pressure delivery sputum aspiration reinforced dehydration preventive hemostasis digestive system protection antibiotics for pathogen infection prevention and other supportive or drug treatments such as neural nutrition to maintain brain cell activity or complementary energy and fluid supplementation 11 Patients in the control group who required tracheotomy underwent this procedure within 4 days after surgery Patients whose disease status remained stable at 1 week after surgery underwent treatment with thromboembolism prophylaxis after a repeat CT examination confirmed the absence of active cranial bleeding In addition to the abovementioned treatments patients in the experimental group received 30 treatments in a hyperbaric oxygen chamber Yantai Moon Oxygen Chamber Co Ltd starting at approximately 1 week after admission when their vital signs had stabilized A Primary endpoints The systolic peak flow velocity Vs mean velocity Vm pulsatility index PI and intracranial pressure of the cerebral middle artery were measured in patients of both groups using a transcranial Doppler analyzer KJ 2V6M Nanjing KeyGen Biotech Co Ltd Nanjing China moreover blood oxygen saturation SaO2 blood oxygen pressure PaO2 and blood hemoglobin Hb were detected using blood samples that were simultaneously collected Thereafter the brain oxygen uptake rate was calculated using the Fick equation which is based on the SaO2 PaO2 and Hb values Secondary endpoints The GCS and U S National Institutes of Health Stroke Scale NIHSS scores of each patient were determined at admission and 2 weeks after hyperbaric oxygen therapy GCS scores ranged from 0 to 15 points 15 points indicated clear consciousness 12 to 14 points indicated mild disturbance of consciousness 9 to 11 points indicated moderate disturbance of consciousness and 8 points indicated coma Accordingly a lower score indicated a more severe disturbance of consciousness whereas a higher score indicated less severe coma NIHSS scores included assessments of consciousness staring facial paralysis upper extremity strength lower limb muscular strength ataxia aphasia dysarthria
4 sensation visual field negligence and distal limb function and ranged from 0 to 42 points A higher NIHSS12 score indicated a more severe absence of neurological function and more severe neurological deficit At 3 months after brain oxygen treatment patients were scored using the Glasgow Outcome Scale GOS 13 A GOS value of 5 points indicated that the patient had recovered well and returned to a normal state despite mild defects 4 points indicated that the patient had mild disability but could to live independently and work with precautions 3 points indicated that the patient was conscious and had severe disability requiring care in daily life 2 points indicated that the patient was in a vegetative state with minimal reaction e g eye opening with the sleep wakefulness cycle and 1 point indicated death Statistical analysis The statistical analysis was performed using SPSS 22 0 SPSS IBM Corp Armonk NY USA Enumerated data are expressed in terms of n Comparisons of enumerated data between groups were analyzed using the v2 test Measurement data are expressed as means standard deviation Data with a normal distribution were analyzed using an independent samples t test whereas those without a normal distribution were analyzed using the Mann Whitney U test Comparisons within groups of values before and after treatment were assessed using a paired t test A logistic regression test was used for multivariate analysis A value of P 0 05 indicated statistical significance Results General characteristics of the control and experimental groups The control and experimental groups did not significantly differ in terms of general Journal of International Medical Research characteristics including sex age height weight tracheotomy status cerebral hernia status at admission GCS score at admission and before hyperbaric oxygen therapy GCS1 injury cause and postoperative diagnosis Table 1 Comparison of prognoses between the control and experimental groups In the control group the analysis revealed a good prognosis mild disability severe disability vegetative state and death in 6 14 6 14 11 25 8 18 and 13 29 patients respectively In the experimental group the analysis revealed a good prognosis mild disability severe disability vegetative state and death in 15 34 9 20 9 20 5 11 and 6 14 patients respectively Patients in the experimental group showed a significantly better prognosis than those in the control group P 0 05 Table 2 Comparison of cerebral metabolism and cerebral blood flow indices before and after treatment in the control and experimental groups Before treatment the control and experimental groups did not exhibit significant differences in the Vs Vm PI intracranial pressure and brain oxygen uptake rate After treatment both groups exhibited significant increases in the Vs Vm and brain oxygen uptake rate all P 0 05 and significant decreases in the PI and intracranial pressure both P 0 05 However an intergroup comparison after treatment revealed a significantly higher Vs Vm and brain oxygen uptake rate and a significantly lower PI and intracranial pressure in the experimental group compared with those in the control group all P 0 05 Table 3 and Figure 1
Zhong et al 5 Table 1 General characteristics of the control and experimental groups Category Gender Male Female Age Height cm Weight kg Tracheotomy GCS score at admission GCS1 Medical history Hypertension Diabetes Hyperlipidemia PLT Injury cause Falling injury Vehicle accident injury Blunt injury Postoperative diagnosis Laceration injury subdural hematoma Laceration injury epidural hematoma Laceration injury intracerebral hematoma Subdural hematoma Epidural hematoma Complex hematoma Control group n 44 Experimental group n 44 22 50 22 50 45 7 165 7 61 8 35 80 6 1 8 2 3 7 2 5 4 9 3 7 16 2 25 56 19 43 45 8 165 7 62 7 37 84 6 1 7 1 2 5 1 2 3 7 2 5 17 3 5 11 37 84 2 5 7 16 34 77 3 7 22 50 7 16 4 9 4 9 1 2 6 14 19 43 8 18 4 9 2 5 3 72 8 18 t v2 P 0 411 0 5 0 312 0 339 0 433 0 306 1 116 1 289 0 079 0 8 0 7 0 7 0 6 0 3 0 2 0 9 0 7 0 660 0 5 0 7 2 239 0 8 n or mean standard deviation PLT platelets Table 2 Comparison of prognosis between the control and experimental groups n Group n Good Mild disability Severe disability Vegetative state Death Control group Experimental group z P 44 44 2 769 0 006 6 14 15 34 09 6 14 9 20 45 11 25 9 20 45 8 18 5 11 37 13 29 6 13 64 Comparison of GCS and NIHSS scores before and after treatment in the control and experimental groups Before treatment the control and experimental groups did not significantly differ in terms of GCS and NIHSS scores After treatment both groups exhibited significant increases in GCS scores P 0 05 and significant decreases in NIHSS scores P 0 05 However after treatment an intergroup comparison revealed
6 Journal of International Medical Research Table 3 Comparison of cerebral metabolism and cerebral blood flow indices before and after brain oxygen treatment between the control and experimental groups means standard deviation Brain oxygen uptake rate Group n Time Vs cm s Vm cm s PI Intracranial pressure mmHg Control group 44 Before brain oxygen treatment After brain oxygen treatment 80 94 9 79 46 19 5 11 0 68 0 15 15 94 3 46 25 51 4 41 85 48 8 86 50 43 4 76 0 61 0 11 13 73 3 68 30 49 4 72 2 281 0 025 81 46 9 65 4 027
Zhong et al 7 Figure 1 Comparison of cerebral metabolism and cerebral blood flow indices before and after treatment between the control and experimental groups a Comparisons of systolic peak flow velocity Vs before and after treatment revealed no significant intergroup difference before treatment significant increases in both groups after treatment P 0 05 and a higher Vs in the experimental group than in the control group after treatment P 0 05 b Comparisons of the mean velocity Vm before and after treatment revealed no significant intergroup difference before treatment significant increases in both groups after treatment P 0 05 and a higher Vm in the experimental group than the control group after treatment P 0 05 c Comparisons of the pulsatility index PI before and after treatment revealed no significant intergroup difference before treatment significant decreases in both groups after treatment P 0 05 and a lower PI in the experimental group than in the control group after treatment P 0 05 d Comparisons of the intracranial pressure before and after treatment revealed no significant intergroup difference before treatment significant decreases in both groups after treatment P 0 05 and a lower intracranial pressure in the experimental group than in the control group after treatment P 0 05 e Comparisons of the brain oxygen uptake rate before and after treatment revealed no significant intergroup difference before treatment significant increases in both groups after treatment P 0 05 and a higher brain oxygen uptake rate in the experimental group than in the control group after treatment P 0 05 Note indicates a comparison with the before treatment condition P 0 05 indicates a comparison with the control group after treatment P 0 05 Discussion Severe brain injury a common form of clinical traumatic disease is a critical condition 14 Brain injury has high disability and mortality rates and may cause respiratory tract obstruction central apnea pulmonary infection epilepsy hydrocephalus post traumatic syndrome cognition and language disorders and other sequelae that decrease the quality of life of patients 8 15 Therefore it is crucial to select effective and suitable treatment methods to improve the quality of life and survival prognosis of patients with severe brain injury 16 17
8 Journal of International Medical Research Table 4 Comparison in GCS and NIHSS scores before and after treatment between the control and experimental groups means standard deviation GCS score NIHSS score Group n Before treatment After treatment Before treatment After treatment Control group Experimental group t P 44 44 6 49 1 15 6 18 1 44 1 116 0 268 9 16 2 84 12 06 2 76 4 857 0 001 19 46 2 64 19 61 2 19 0 290 0 773 14 61 2 33 8 46 2 37 12 270 0 001 GCS Glasgow Coma Scale NIHSS U S National Institutes of Health Stroke Scale Figure 2 Comparison of Glasgow Coma Scale GCS and U S National Institutes of Health Stroke Scale NIHSS scores before and after treatment between the control and experimental groups a Comparisons of GCS scores before and after treatment revealed no significant intergroup difference before treatment significant increases in both groups after treatment P 0 05 and a significantly higher GCS score in the experimental group than in the control group after treatment P 0 05 b Comparisons of the NIHSS scores before and after treatment revealed no significant intergroup difference before treatment significant increases in both groups after treatment P 0 05 and a significantly higher NIHSS score in the experimental group than in the control group after treatment P 0 05 Note indicates a comparison with the before treatment condition P 0 05 indicates a comparison with the control group after treatment P 0 05 Several recent studies have explored the efficacy of hyperbaric oxygen therapy For example Mozayeni et al 18 examined the safety and practicability of hyperbaric oxygen therapy for the treatment of patients with concussion following a chronic mild traumatic brain injury and reported that this therapy is clinically feasible considering its safety and cost effectiveness Benincasa et al 19 found that hyperbaric oxygen therapy could reduce the tumor necrosis factor a mediated inflammatory responses of endothelial cells thereby promoting vascular recovery following injury Our study revealed that the experimental group showed a better prognosis than the control group moreover the experimental group showed a higher GCS score and lower NIHSS score after treatment than before treatment and performed better in both aspects relative to the control group In addition some studies have reported
Zhong et al 9 Table 5 Univariate analysis of factors affecting the prognosis of patients n or means standard deviation Factors Sex Male Female Age years 50 50 Injury cause Falling injury Vehicle accident injury Blunt injury Glasgow Coma Scale score at admission Tracheotomy status Yes No First hyperbaric oxygen therapy duration d Number of hyperbaric oxygen therapy courses Poor prognosis group n 20 Good prognosis group n 24 12 60 00 8 40 00 13 54 17 11 45 83 7 35 00 13 65 00 8 33 33 16 66 67 4 20 00 15 75 00 1 5 00 5 16 1 45 3 12 50 19 79 17 2 8 33 7 62 1 68 14 70 00 6 30 00 8 16 1 78 3 14 0 49 t v2 P 0 151 0 697 0 013 0 908 0 588 0 745 5 142 5 442
10 that hyperbaric oxygen therapy could improve the oxygen supply to injured brain tissues by promoting vasoconstriction and vascular regeneration and preventing secondary brain injury demonstrating a good ability to promote the recovery of bodily and cognitive functions of patients 20 22 Patients with severe brain injury often present with different degrees of hypoxia and ischemia as well as increases in intracranial pressure which damage the brain microcirculation and induce a vicious circle Therefore the additional resolution of these features using hyperbaric oxygen therapy can significantly improve treatment efficacy 8 The present study revealed that after treatment both the control and experimental groups had an increased Vs Vm and brain oxygen uptake rate and a decreased PI and intracranial pressure although the experimental group exhibited more significant improvements in these aspects all P 0 05 Using a constructed rat model Yang et al 23 demonstrated that hyperbaric oxygen therapy could promote the proliferation of neural stem cells by activating vascular endothelial growth factor One study by Lim et al 24 revealed that hyperbaric oxygen therapy could improve traumatic brain injury induced depressionlike behavior in rats by reducing neural inflammation In addition s study by Harch et al 25 revealed that hyperbaric oxygen therapy is significantly effective for the treatment of patients with mild and moderate traumatic brain injury Hadanny et al 26 showed that hyperbaric oxygen therapy is safe and beneficial for patients with mild to moderate traumatic brain injury Hyperbaric oxygen can induce neuroplasticity and improve cognitive function of patients with hypoxic brain damage These findings suggest that hyperbaric oxygen can effectively promote the recovery of neurological function and is a feasible and effective solution for the treatment of severe brain injury Regarding the underlying Journal of International Medical Research mechanism we suspect that hyperbaric oxygen can promote brain cell metabolism accelerate the decomposition and absorption of damaged brain tissue promote the establishment of collateral circulation and restore the oxygen supply to neurons Furthermore the oxygen supply is associated with neuronal regeneration improved local microcirculation and reduced free radical levels In the present study the univariate analysis of the good and poor prognosis groups revealed significant intergroup differences in the GCS score at admission tracheotomy status first hyperbaric oxygen therapy duration and number of hyperbaric oxygen therapy courses whereas the multivariate analysis confirmed that all of these factors except the number of hyperbaric oxygen therapy courses were independent prognostic factors Therefore hyperbaric oxygen therapy may play an important role in improving the prognosis of patients with severe brain injury A study by Xu et al 27 compared hyperbaric oxygen therapy with routine therapy for the treatment of severe brain injury and found that brain contusion coronary heart disease hydrocephalus and tracheotomy affected the prognosis of patients with severe brain injury In addition that study reported that hyperbaric oxygen therapy could improve the indices of patients with severe brain injury thereby significantly improving their prognosis These findings are consistent with those of our study and indicate that hyperbaric oxygen therapy can effectively improve the prognosis of patients with severe brain injury The present study confirmed that hyperbaric oxygen therapy was an effective treatment for patients with severe brain injury however the underlying mechanism was not further explored The optimal hyperbaric oxygen therapy duration in a clinical setting remains unknown This study did not conduct a long term follow up examination of patients with severe brain injury and therefore the
Zhong et al long term performance remains unclear Furthermore this study was not blinded or sham controlled These shortcomings of our study should be addressed in future studies to further verify our conclusions In conclusion hyperbaric oxygen therapy can effectively promote the recovery of neurological function as well as improve the cognitive function and prognosis of patients with severe traumatic brain injury Declaration of conflicting interest The authors declare that there is no conflict of interest Funding This study was funded by Guangdong Natural Science Foundation No 2020A1515010289 Clinical Research Project of Shenzhen Health and Family Planning Commission No SZLY2018007 Shenzhen People s Hospital Young and Middle aged Research Funds Cultivation Fund No SYKYPY201923 and Shenzhen Key Medical Discipline Construction Fund Shenzhen Key Medical Discipline 20202024 ORCID iD Bo Du https orcid org 0000 0003 2794 5816 References 1 Cao Y Qiu J Wang B et al The analysis on risk factors and clinical treatment of brain injury concurrent with acute kidney injury Cell Biochem Biophys 2015 71 199 204 2 Zhang W Li S Visocchi M et al Clinical analysis of hyponatremia in acute brain injury J Emerg Med 2010 39 151 157 3 Tu XH He ZY Fu X et al Brain arousal dysfunction in severe brain injury treated with acupuncture Zhongguo Zhen Jiu 2010 30 974 976 4 Zweckberger K Sakowitz OW Unterberg AW et al Classification and therapy of brain injury CCI Laryngorhinootologie 2008 87 121 132 quiz 33 6 11 5 Wang L Li M Wang YQ et al Clinical study of value of transcranial Doppler ultrasonography in diagnosing brain death in severe brain injury Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2012 24 670 673 6 Huang Q Xu H and Xiao QS Clinical research of different analgesia methods on perianesthetic pain of patients with moderate and severe brain injury who have emergency operation Eur Rev Med Pharmacol Sci 2017 21 88 92 7 Rockswold GL Ford SE Anderson DC et al Results of a prospective randomized trial for treatment of severely brain injured patients with hyperbaric oxygen J Neurosurg 1992 76 929 934 8 Rockswold SB Rockswold GL Zaun DA et al A prospective randomized Phase II clinical trial to evaluate the effect of combined hyperbaric and normobaric hyperoxia on cerebral metabolism intracranial pressure oxygen toxicity and clinical outcome in severe traumatic brain injury J Neurosurg 2013 118 1317 1328 9 Wang F Wang Y Sun T et al Hyperbaric oxygen therapy for the treatment of traumatic brain injury a meta analysis Neurol Sci 2016 37 693 701 10 Shandley S Wolf EG Schubert Kappan CM et al Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy Undersea Hyperb Med 2017 44 257 269 11 Geng F Ma Y Xing T et al Effects of hyperbaric oxygen therapy on inflammasome signaling after traumatic brain injury Neuroimmunomodulation 2016 23 122 129 12 Naess H Kurtz M Thomassen L et al Serial NIHSS scores in patients with acute cerebral infarction Acta Neurol Scand 2016 133 415 420 13 McMillan T Wilson L Ponsford J et al The Glasgow Outcome Scale 40 years of application and refinement Nat Rev Neurol 2016 12 477 14 Huang QB Zhang Y Su YH et al Prognostic correlation of intracranial pressure monitoring in patients with severe brain injury Zhonghua Yi Xue Za Zhi 2013 93 1788 1790
12 15 Chinda JY Abubakar AM Umaru H et al Epidemiology and management of head injury in paediatric age group in NorthEastern Nigeria Afr J Paediatr Surg 2014 10 358 361 16 Tan M Lu XL Duan JW et al Effects of probiotics on blood glucose levels and clinical outcomes in patients with severe craniocerebral trauma Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2013 25 627 630 17 Eshete A and Taye F Magnitude of severe head injury and its associated factors among head injury patients in Gedeo Zone Southern Ethiopia a two year retrospective Study Ethiop J Health Sci 2018 28 323 330 18 Mcdonagh M Helfand M Carson S et al Hyperbaric oxygen therapy for traumatic brain injury a systematic review of the evidence Arch Phys Med Rehabil 2011 92 1519 1521 19 Benincasa JC De Freitas Filho LH Carneiro GD et al Hyperbaric oxygen affects endothelial progenitor cells proliferation in vitro Cell Biol Int 2019 43 136 146 20 Daly MC Faul J and Steinberg JS Hyperbaric oxygen therapy as an adjunctive treatment for diabetic foot wounds a comprehensive review with case studies Wounds 2010 22 1 11 21 Montecorboli U Annese T Marinaccio C et al Angiogenesis and hyperbaric oxygen in the chick embryo chorioallantoic membrane Int J Dev Biol 2015 59 461 464 Journal of International Medical Research 22 Tal S Hadanny A Sasson E et al Hyperbaric oxygen therapy can induce angiogenesis and regeneration of nerve fibers in traumatic brain injury patients Front Hum Neurosci 2017 11 508 23 Yang Y Wei H Zhou X et al Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor extracellular signal regulated kinase signaling after traumatic brain injury Neuroreport 2017 28 1232 1238 24 Lim SW Sung KC Shiue YL et al Hyperbaric oxygen effects on depression like behavior and neuroinflammation in traumatic brain injury rats World Neurosurg 2017 100 128 137 25 Harch PG Andrews SR Fogarty EF et al Case control study hyperbaric oxygen treatment of mild traumatic brain injury persistent post concussion syndrome and posttraumatic stress disorder Med Gas Res 2017 7 156 174 26 Hadanny A Golan H Fishlev G et al Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restor Neurol Neurosci 2015 33 471 486 27 Xu L Li B Yang C et al Clinical research on postoperative efficacy and related factors of early simulation hyperbaric oxygen therapy for severe brain injury Pak J Pharm Sci 2016 29 273 280
Received 27 August 2020 DOI 10 1002 ccr3 3658 Accepted 10 November 2020 CASE REPORT Late application of hyperbaric oxygen therapy during the rehabilitation of a patient with severe cognitive impairment after a traumatic brain injury Ma gorzata Skiba MD1 Anna R kas Dudziak PhD2 W odzimierz P otek PhD MD2 1 Stefan Cardinal Wyszy ski District Specialist Hospital Lublin Poland 2 Gynaecological Obstetric Clinical Hospital of the Pozna University of Medical Sciences Pozna Poland Correspondence Anna R kas Dudziak Clinic of Anaesthesiology in Obstetrics and Gynaecology Gynaecological Obstetric Clinical Hospital of the Pozna University of Medical Sciences ul Polna 33 60 535 Pozna Poland Artur Beka a MD2 Abstract The hyperbaric therapy resulted in the patient s quick recovery and significantly accelerated the recovery after the brain injury KEYWORDS cognitive functioning hyperbaric oxygen therapy traumatic brain injury IN TRO D U C T ION 1 Traumatic brain injuries TBIs are one of the main causes of death TBI treatment is multidirectional but proper brain oxygenation is one of the most important factors affecting the final result of treatment Little is known about the possible influence of hyperbaric oxygen therapy on the function of the central nervous system CNS during rehabilitation after a traumatic brain injury 1 2 The aim of the study was to analyze the case of a patient treated in a hyperbaric chamber during rehabilitation after a severe TBI The research assumption was that exposure to an elevated pressure of oxygen may increase its availability in the CNS structures and accelerate recovery The hyperbaric therapy resulted in the patient s quick recovery and significantly accelerated the recovery of his memory and verbal functions Hyperbaric oxygen therapy HBOT is a non invasive method of treating patients in a specially designed hyperbaric chamber where they breathe 100 oxygen administered at a pressure higher than local atmospheric pressure 3 The use of hyperbaric oxygen in patient therapy dates back to the 17th century when C Henshaw a British physician and physiologist designed the first hyperbaric chamber 4 I Boerema a Dutch surgeon is considered the father of modern oxygen hyperbaric oxygen therapy It is the most effective method of supplying oxygen to all body cells even those around which the blood supply has been disordered During therapy the conditions inside the hyperbaric chamber cause the blood oxygen partial pressure to increase due to a significant increase in its solubility in the plasma Hyperbaric oxygen therapy can be successfully applied to patients with hard to heal wounds in the course of diabetic foot syndrome after injuries and radiotherapy chronic osteomyelitis bacterial tissue infection carbon monoxide poisoning and extensive burns second and third degree burns covering over 20 of the body surface area For therapeutic purposes the pressure inside the chamber should exceed 1 4 atmosphere absolute ATA to increase the amount of oxygen supplied to cells in the body During treatments a pressure of 2 5 ATA is usually applied 4 5 Thanks to hyperbaric oxygen therapy This is an open access article under the terms of the Creative Commons Attribution License which permits use distribution and reproduction in any medium provided the original work is properly cited 2020 The Authors Clinical Case Reports published by John Wiley Sons Ltd 960 wileyonlinelibrary com journal ccr3 Clin Case Rep 2021 9 960 965
SKIBA et al 2 0 2 8 ATA oxygen concentration in healthy tissues can be increased to as much as 1 000 mmHg whereas in wounds and hypoxic areas it can be increased up to 250 mmHg 6 Oxygen therapy is considered to be a safe and non invasive method However there is a risk of respiratory toxicity Lorrain Smith effect chest tightness or pain cough irritation or inflammation of the trachea and bronchi apnea and reduced vital capacity damage to the alveolar epithelium and capillary endothelium pulmonary edema atelectasis with hypoxia Paul Bert effect which may occur during HBOT is described as a set of CNS symptoms nausea dizziness hiccups eyelid and facial tremor vision and hearing disorders hallucinations breathing difficulty fatigue anxiety loss of consciousness and tonic clonic seizures The most common contraindications for HBOT are as follows pneumothorax emphysema with CO2 retention some drugs eg bleomycin the presence of a pacemaker epilepsy fever viral infections spherocytosis 7 In recent years this method of treatment has become more available and the list of indications where it has proved to be effective is longer As early as 1976 there were reports on the possibility to use HBOT in CNS pathologies It was then that Tishchenko noted that hyperbaric oxygen improved the cognitive functions and reduced the number of neurological complications in 20 patients treated in a hyperbaric chamber 8 Hyperbaric oxygen therapy increases the metabolism of nerve cells reduces intracranial pressure and improves the cognitive function and quality of life 9 10 At the moment the possibility of using HBOT in the late period after TBI as a method supporting rehabilitation is an issue of interest The aim of the study was to analyze the case of a patient after a traumatic brain injury treated with HBOT during the rehabilitation period This type of therapy is not widely used in Poland and any case of its use may be an interesting scientific report 2 CA S E ST U DY Here is a case study of a 34 year old patient an academic PhD degree employed at a Polish university The patient is a professional laboratory diagnostician with excellent knowledge of several foreign languages In September 2017 he suffered a severe multiorgan injury after his motorcycle had collided with a lorry He suffered a traumatic brain injury with accompanying epidural hematoma of the left frontal region with numerous fractures of cranial bones including calvarial basilar skull and viscerocranium fractures preliminary Glasgow Coma Scale rating 4 points severe TBI After the accident computed tomography imaging also revealed numerous bilateral rib fractures and spleen rupture Immediately after the injury the patient was qualified for 961 surgery to remove the epidural hematoma and spleen After the surgery he was admitted to the Intensive Care Unit ICU where artificial ventilation was continued under analgosedation and hyperosmotic and neuroprotective therapy was implemented On the first day after the injury a CT scan of the patient s head revealed significant enlargement of the area of contusion of the frontal lobes of both cerebral hemispheres There were numerous foci of intracerebral bleeding and subarachnoid bleeding The patient s condition improved after the therapy After 23 days of the therapy contact with the patient was established but he was still suffering from sensory aphasia and significant muscle weakness As a result of injury the patient lost vision in his left eye The patient stayed in the ICU for 5 months Then he underwent rehabilitation which continued until August 2018 During the rehabilitation before HBOT the patient underwent an initial neuropsychological examination which revealed deep cognitive impairment He could remember events only from one day or the previous 6 9 hours His mood was changeable and that is why he refused to take part in planned psychological tests Attempts to conduct the Mini Mental State Examination ended with a few initial tasks Frontal lobe syndrome was diagnosed As the patient s clinical condition was improving he was qualified for active rehabilitation including psychiatric rehabilitation As there was a chance to improve the patient s cognitive function after optimizing the supply of oxygen to the CNS he was qualified for treatment in a hyperbaric chamber Within 5 months the patient underwent a series of 42 hyperbaric oxygen therapy sessions each of which lasted 90 minutes During the first 3 weeks there were sessions five times a week Next they were held three times a week for the next 4 weeks The therapy was discontinued for 48 days because the patient needed to have his calvaria augmented After the break sessions were held three times a week for another 5 weeks After the therapy the patient s nervous and mental functions as well as his motor skills and coordination improved His memory also improved significantly which resulted in better communication During the therapy his cognitive processes memory and concentration improved His excessive sleepiness passed away His motor skills and vision in his left eye improved He answered questions in full sentences In the neuropsychologist s opinion the patient s condition improved significantly after the hyperbaric therapy His emotional lability disappeared and the overall level of his cognitive functions improved His everyday communication and performance of minor chores also improved The therapy reduced the symptoms of the frontal lobe syndrome which was diagnosed by the neuropsychologist during the first examination Detailed neuropsychological assessment was possible after full HBOT The patient maintained verbal contact but
962 with reduced orientation to time and place He scored low in tasks testing the course of cognitive processes His attention and stimulus selection were disordered He exhibited hemispatial neglect skipped the left side of space and visual spatial deficits Unfortunately his working memory was disordered which resulted in a low auditory verbal learning level However the patient s direct auditory memory functioned well The analysis of executive functions revealed organization and planning disorders dissociation between the patient s knowledge and ability to use it and frontal amnesia The patient s social behavior was disordered He exhibited verbal disinhibition confabulation anosognosia reduced insight and criticism As far as other cognitive spheres are concerned the patient s abstract thinking ability was reduced and he made delusional interpretations The patient was characterized by high fatigability and despite his awareness of behavioral disorders he was not able to correct them While staying at the rehabilitation center the patient s state changed dynamically His emotional lability disappeared whereas his general level of cognitive functions and compliance with behavioral standards improved slightly The clinical picture was dominated by visual spatial disorders disorientation and behavioral disorders which pointed to frontal lobe syndrome The patient s willingness to cooperate varied depending on his mood He required permanent care After rehabilitation with the HBOT his short term memory improved and now he can remember the topics of conversations about 3 4 days back 3 D IS C U S S ION The injury the patient suffered in the accident damaged numerous nerve structures in his body The primary damage which had been caused by mechanical force stretched and disrupted his nerve cells This condition is known as diffuse axonal injury Cells affected by primary injury trigger inflammatory reactions which lead to cerebral edema and increased intracranial pressure In addition the resulting hematomas and inflammation which accompanied blood extravasation caused swelling of the adjacent tissue and aggravated dysfunction of the nervous tissue The lesions resulting from the injury intensified the increase in the intracranial pressure which subsequently caused a decrease in the cerebral perfusion pressure The intracranial lesions caused the compression of undamaged vessels and reduced the flow in them Secondary injury disordered the cerebral blood supply and resulted in the hypoxia of more distant and peripherally located parts of the brain In the region where the perfusion of tissues is reduced nerve cells receive too little oxygen to function properly Therefore their metabolism slows down and they become dormant to prevent apoptosis This ischemic SKIBA et al damage is potentially reversible and it can be treated by HBOT Although indications for the HBOT in CNS disorders are optional rather than basic this treatment method is approved by experts 6 Due to the increased blood oxygen content which is maintained for a long period of time the availability of oxygen increases and nerve cells are better oxygenated When breathing air at atmospheric pressure the blood oxygen tension in arterial blood is about 100 mmHg whereas the oxygen pressure in tissues is about 55 mmHg The increase in atmospheric pressure triples the availability of oxygen to the cells of the central nervous system When the pressure is three times higher than atmospheric pressure and the patient is breathing pure oxygen the blood oxygen tension increases to 2 000 mmHg whereas the tissue oxygen tension rises up to 500 mmHg 11 This effect improves the oxygenation of all tissues and thus the ischemic area is reduced This change increases cellular metabolism which restores cellular functions disturbed during the trauma 12 Apart from that hyperbaric oxygen therapy has been proved to limit post ischemic reduction in ATP production and to reduce the accumulation of lactates in ischemic tissues 13 The disruption of the mechanism that increases damage to nerve cells has a neuroprotective effect on the rest of the brain and reduces the extent of permanent damage Another mechanism that may significantly affect the treatment is the influence of hyperbaric oxygen therapy on vasoconstriction and vasodilatation of cerebral vessels After exposure to hyperbaric oxygen the cerebral blood flow is reduced due to lower concentration of nitric oxide An experiment on rats exposed to pressures of 3 and 4 ATA for 30 minutes showed that their regional cerebral flow decreased respectively by 26 39 and 37 43 and this effect lasted up to 75 min The effect persisted longer in the group of the animals which had received nitric oxide N omega nitroL arginine methyl ester prior to the exposure In the same experiment the nitric oxide concentration increased during further exposure and caused a secondary increase in the regional blood flow in the brains of all rats 14 Harch et al subjected rats to HBOT 31 33 days after experimental cerebral contusion The animals had 80 sessions at a pressure of 1 5 ATA Improvement in behavioral and neurobiological outcomes was assessed in the study The animals blood vessel density was measured bilaterally in the hippocampus by means of diaminobenzidine staining and correlated with the results of behavioral tests Vascular density in the damaged hippocampus increased significantly In consequence spatial movement in the group subjected to HBOT increased significantly as compared with the control groups 15 Repeated exposure stimulates the growth of blood vessels by increasing the secretion of the vascular endothelial growth factor VEGF by macrophages Experimental studies showed that the HBOT brought significantly better results
SKIBA et al in mice after brain injury both in the cognitive and motor range 16 The production of oxygen free radicals stimulates anti inflammatory mechanisms which later reduce cerebral edema and thus compensate for the re expansion of blood vessels A study conducted on mice with induced brain injury showed that the interleukin 10 level increased whereas cerebral edema decreased as early as 3 hours after hyperbaric oxygen therapy at a pressure of 2 ATA 17 Three exposures to hyperbaric conditions at a pressure of 2 ATA reduced the inflammatory markers and increased the number of new endothelial and glial cells Lin et al 2012 Another study showed that after HBOT the caspase 3 and interleukin 8 levels as well as the tumor necrosis factor alpha level TNF decreased 18 The intensity of free radical production and lipid peroxidation was investigated in an experiment on rabbits with total brain ischemia induced for 10 minutes by infusion of artificial cerebrospinal fluid into the subarachnoid space Next immediately after reperfusion the test group was placed in a hyperbaric chamber at a pressure of 2 8 ATA for 75 minutes Meanwhile the control group breathed atmospheric air The concentrations of oxidized and free glutathione and malondialdehyde were measured in the experiment The neurophysiological symptoms of brain damage were assessed by analyzing the cortical somatosensory evoked potentials The production of oxygen free radicals increased in the test group exposed to the hyperbaric environment because there was a higher ratio of oxidized to reduced glutathione Lipid peroxidation was comparable in both groups as evidenced by the malondialdehyde level The somatosensory evoked potentials were as much as 50 higher in the group of rabbits subjected to hyperbaric oxygen therapy 19 The publications discussed above described laboratory tests on animals and the period directly related to the moment of TBI It is extremely difficult to use HBOT in humans in the immediate period after TBI The problem of HBOT efficacy in people in the late period following damage to the central nervous system CNS should be carefully evaluated because to date there have been few studies describing the problem Efrata et al described the beneficial effects of HBOT applied in the neurological rehabilitation of 74 patients after stroke They had 40 HBOT sessions at a pressure of 2 ATM for 2 months The hyperbaric treatment improved the patients neurological functions including speech more than the standard treatment applied to other patients 20 The patient described in our case study had TBI rather than acute CNS ischemia but in TBI pathogenesis massive blood supply disorders are an important link in the CNS pathology chain so the possible positive effect of HBOT in TBI can also be broadly taken into consideration In our case the patient had a similar number of HBOT sessions The following areas are particularly vulnerable in TBI the frontal area the subfrontal white matter the deeper midline 963 structures including the basal ganglia and diencephalon the rostral brain stem and the temporal lobes including the hippocampi In the course of TBI the catecholaminergic and cholinergic relay systems which are involved in the regulation of arousal cognition reward behavior and mood are particularly vulnerable Damage to the dorsolateral prefrontal cortex impairs executive functions The orbitofrontal cortex is responsible for intuitive social behaviors The third important system is the neuronal system related to the anterior cingulate cortex which is involved in reward related behaviors 21 Imaging tests conducted on our patient revealed structural damage to similar regions which was reflected by his cognitive status During the HBOT the patient s cognitive functions and behavior improved significantly Golden et al made a statistical analysis of 50 patients after TBI who underwent SPECT before during and after hyperbaric oxygen therapy The results of this analysis confirmed the hypothesis that HBOT improved blood supply in the cortex while the therapy had no effect on the region of the pons and cerebellum The blood supply was better in younger patients but the improvement in functions was comparable in both groups 22 In the context of the research conducted by Golden et al it was justified to apply HBOT to our patient due to his young age and the fact that traumatic lesions were mostly located in his cerebral cortex Boussi Gross observed that treatment in a hyperbaric chamber improved the quality of life of patients after TBI The researcher suggested that neuroplasticity played a role in improvement of chronically impaired brain functions 23 Hadanny et al described the use of HBOT in a distant time after brain damage The study was conducted on patients who had suffered brain injury 3 months to 33 years before A team of scientists observed significant improvement in cognitive functions in correlation with an increase in the neurological activity in individual parts of the brain After the HBOT the patients memory and attention usually improved 24 In our case the patient was qualified for HBOT due to the persistence of severe cognitive deficit He was qualified for the treatment with due caution The patient did not develop epilepsy which might have disqualified him from therapy The potential pathogenic effect of the concomitant chest injury was also taken into consideration However the patient did not develop pneumothorax despite numerous rib fractures As the time interval between the injury and HBOT allowed full recovery from respiratory pathologies there was low risk of lung damage during the HBOT The case described in this article documents the effectiveness of using HBOT to treat the patient after a severe TBI injury complicated by significant sensory aphasia Significant neurological complications can be expected after such a severe injury because there is a linear correlation between the GCS score and the occurrence of severe neurological disorders within a GCS range of 3 9 25
964 It is disputable whether the observed neurological improvement resulted from the natural course of the disease or it was accelerated by the HBOT 26 According to reference publications the language disorder tends to disappear naturally within 1 3 months 27 As our patient had severe cognitive impairment after 5 months of ITU treatment we can assume that the changes regressed extremely slowly and the risk of chronic cognitive impairment was high In the context of the aforementioned reports we can hypothesize that the HBOT had beneficial effect on our patient According to recent reports treatment in a hyperbaric chamber is safe and beneficial to patients after a traumatic brain injury and those with symptoms of post traumatic stress disorder and post concussion syndrome 28 Another aspect to be taken into consideration is the patient s higher cognitive level before the TBI According to the cognitive reserve theory patients with initially higher IQ and higher level of education function cognitively better after TBI Kesler et al compared the total intracranial volume TICV and ventricle to brain ratio VBR by means of high resolution magnetic resonance imaging 29 30 They also analyzed the level of education and used standardized tests to compare the cognitive outcome of 25 patients before and after TBI The results of this study suggest that a larger premorbid brain volume and a higher level of education may decrease vulnerability to cognitive deficits following TBI which is consistent with the cognitive reserve concept 31 There was an analogous situation in our study because HBOT was applied to the patient with a high initial level of education patient s IQ before TBI unknown Therefore the patient s high cognitive reserve may have influenced the positive outcome of HBOT Currently there are only 12 hyperbaric oxygen therapy centers in Poland which are mostly located in large medical centers Therefore there are limited possibilities to apply this therapy in common TBI cases Additional experience in optional HBOT uses may be a source of important information broadening our knowledge and the scope of therapy applied to our patients As the awareness of healthcare workers concerning this therapeutic option in TBI is increasing the application of HBOT may extend and result in secondary assessment of its effectiveness in patients with CNS pathology In the future studies comparing the results of rehabilitation with various HBOT schemes may be the basis for modification and extension of the current treatment scheme for patients with TBI 4 CO NC LU S ION The use of HBOT in the course of rehabilitation was safe for the patient after TBI and it may have shortened the recovery of neurological functions Further research is necessary to SKIBA et al precisely determine the influence of HBOT on the recovery process CONFLICT OF INTEREST In behalf of My and Co authors I certify that there is no actual or potential conflict of interest in relation to this article AUTHOR CONTRIBUTIONS ARD MS AB and WP contributed to the design and implementation of the case report to the analysis of the results and to the writing of the manuscript CONSENT FOR PUBLICATION The consent to the publication of the data was issued by the Bioethics Committee at the Medical University of Lublin based on the written and oral consent of the patient to the publication of data on 10 11 2019 DATA AVAILABILIT Y STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request ORCID Anna R kas Dudziak https orcid org 0000 0003 4438 6083 R E F E R E NC E S 1 Adamides AA Winter CD Lewis PM Cooper DJ Kossmann T Current controversies in the management of patients with severe traumatic brain injury ANZ J Surg 2006 76 163 174 2 Boerema I Meyne N Brum Melkamp W Life without blood a study of the influence of high atmospheric pressure and hypothermia on dilution of the blood J Cardiovasc Surg 1960 1 133 146 3 Naro ny W Siebert J Mo liwo ci i ograniczenia stosowania hiperbarii tlenowej w medycynie The Possibilities and Limitations to the Use of Hyperbaric Oxygen Therapy in Medicine Forum Medycyny Rodzinnej 2007 1 368 375 4 Jain KK Textbook of hyperbaric medicine 4th edn G ttingen Hogrefe Huber Publishers 2004 5 Mathieu D Handbook on hyperbaric medicine Dordecht Springer 2006 6 Knefel G Podstawy hiperbarycznej terapii tlenowej The Essentials of Hyperbaric Oxygen Therapy Leczenie Ran 2006 3 83 93 7 Szyma ska B Kawecki M Knefel G Kliniczne aspekty hiperbarii tlenowej Clinical Aspects of Hyperbaric Oxygen Therapy Wiadomo ci Lekarskie LIX 2006 59 1 2 105 109 8 Tishchenko AT Hyperbaric oxygen therapy in the clinical treatment of mental disorders accompanying severe cranio cerebral trauma Zh Nevropatol Psikhiatr Im S S Korsakova 1976 76 262 268 9 Deng Z Chen W Jin J Zhao J Xu H The neuroprotection effect of oxygen therapy a systematic review and meta analysis Nigerian J Clin Pract 2018 21 401 416 10 Rockswold SB Rockswold GL Zaun DA et al A prospective randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism intracranial pressure
SKIBA et al and oxygen toxicity in severe traumatic brain injury J Neurosurg 2010 112 1080 1094 11 Tibbles PM Edelsberg JS Hyperbaric oxygen therapy N Engl J Med 1996 334 1642 1648 12 Daugherty WP Levasseur JE Sun D Rocksworld GL Bullock MR Effects of hyperbolic oxygen therapy on cerebral oxygenation and mitochondrial function following moderate lateral fluid percussion injury in rats J Neurosurg 2004 101 499 504 13 Stewart RJ Yamaguchi KT Mason SW Roshdieh BB Dabassi NI Ness NT Tissue ATP levels in burn injured skin treated with hyperbaric oxygenation Undersea Biomed Res 1989 16 Suppl 53 14 Demchenko IT Boso AE O Neill TJ Bennett PB Piantadosi CA Nitric oxide and cerebral blood flow responses to hyperbaric oxygen J Appl Physiol 2000 88 1381 1389 15 Harch PG Kredit C Van Meter KW Sutherland RJ Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury Brain Res 2007 1174 120 129 16 Beratz Goldstein R Toussia Cohen S Elpaz A Rubovitch V Pick CG Immediate and delated hyperbaric oxygen therapy as a neuroprotective treatment for traumatic brain injury in mice Mol Cell Neurosci 2017 83 74 82 17 Chen X Duan XS Xu LJ Zhao JJ She ZF Interleukin 10 mediates the neuroprotection of hyperbaric oxygen therapy against traumatic brain injury in mice Neuroscience 2014 266 235 243 18 Zhang Y Yang Y Tang H et al Hyperbaric oxygen therapy ameliorates local brain metabolism brain edema and inflammatory response in a blast induced traumatic brain injury model in rabbits Neurochem Res 2014 39 950 960 19 Mink RB Dudka AJ Hyperbaric oxygen after global cerebral ischemia in rabbits does not promote lipid per oxidation Crit Care Med 1995 23 1398 1404 20 Efrati S Fishlev G Bechor Y Volkov O Bergan J Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS ONE 2013 8 1 e53716 21 McAllister TW Neurobiological consequences of traumatic brain injury Dialogues Clin Neurosci 2011 13 287 300 22 Golden ZL Neubauer R Golden CJ Greene L Marsh J Melko A Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy J Neurosci 2009 112 119 131 23 Boussi Gross R Golan H Fishlev G Bechor Y Volkov O Hyperbaric oxygen therapy can improve post concussion syndrome 965 years after mild traumatic brain injury randomized prospective trial PLoS ONE 2013 8 11 e79995 https doi org 10 1371 journ al pone 0079995 24 Hadanny A Abbott S Suzin G Bechor Y Efrati S Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post traumatic brain injury patients retrospective analysis BMJ Open 2018 8 9 e023387 25 Hukkelhoven CW Rampen AJ Maas AI Farace E Habbema JD Some prognostic models for traumatic brain injury were not valid J Clin Epidemiol 2006 59 2 132 143 26 Wang GH Zhang XG Jiang ZL et al Neuroprotective effects of hyperbaric oxygen treatment on traumatic brain injury in the rat J Neurotrauma 2010 27 1733 1743 27 Wood RL Neurobehavioral sequelae of traumatic brain injury Taylor Francis 1990 98 28 Harch PG Andrews SR Forgarty EF Lucarini J Van Meter KW Case control study hyperbaric oxygen treatment of mild traumatic brain injury persistent post concussion syndrome and post traumatic stress disorder Medical Gas Res 2017 7 156 174 29 Cihan YB Uzun G Yildiz S D nmez H Hyperbaric oxygen therapy for radiation induced brain necrosis in a patient with primary central nervous system lymphoma J Surgical Oncology 2009 100 732 735 30 Feldmeier JJ Hyperbaric oxygen for delayed radiation injuries Undersea Hyperb Med 2004 31 133 145 31 Kesler SR Adams HF Blasey CM Bigler ED Premorbid intellectual functioning education and brain size in traumatic brain injury an investigation of the cognitive reserve hypothesis Appl Neuropsychol 2003 10 153 162 How to cite this article Skiba M R kas Dudziak A Beka a A P otek W Late application of hyperbaric oxygen therapy during the rehabilitation of a patient with severe cognitive impairment after a traumatic brain injury Clin Case Rep 2021 9 960 965 https doi org 10 1002 ccr3 3658
Can Hyperbaric Oxygen Improve Post Concussion Syndrome PCS Presenter Nadia Colavecchio SRT July 22 6 30 PM Eastern Session Abstract INTRODUCTION Brain injuries are a leading cause of death and disability worldwide for individuals under the age of 40 In fact one in three Canadians is directly impacted by brain injuries Currently there is no effective intervention treatment in clinical practice for post mild traumatic brain injury mTBI patients experiencing neurological dysfunction Although there are intensive rehabilitation programs these are only partially successful as every patient s journey with mTBI is both unique and complex Recent studies show that hyperbaric oxygen therapy HBOT may induce angiogenesis and neuroplasticity in this population leading to a neurological improvement reversal of symptoms and improved quality of life OBJECTIVE To determine the effectiveness of Hyperbaric Oxygen Therapy HBOT in improving brain function and quality of life in patients suffering from prolonged post concussion syndrome PCS as a result of a mTBI METHODOLOGY A literature search was performed using PubMed IOS Press BioMedCentral and ResearchGate databases Randomized control trials RCT case studies and retrospective analyses were included in this review RESULTS One RCT found that patients receiving a HBOT protocol demonstrated significant improvements in cognitive function brain activity and quality of life A retrospective analysis conducted by Tal Hadanny Berkovitz Ben Jacob and Efrati 2015 showed those who underwent HBOT had significant increase blood flow and cerebral blood volume as well as improvement in global cognitive scores p 0 007 Research by Harch Fogarty Staab and Van Meter 2009 found that the administration of low pressure HBOT caused a reduction in signs and symptoms of chronic mTBI Single photon emission computerized tomography SPECT imaging done pre and post HBOT shows an increase in blood flow to multiple lobes of the brain and an overall normalization of blood flow following intervention CONCLUSION HBOT may induce cerebral angiogenesis and neuroplasticity which not only improves perfusion to damaged brain tissue but repairs chronically impaired brain function in mTBI patients with prolonged PCS Session Objectives 1 To determine the effectiveness of Hyperbaric Oxygen Therapy HBOT in improving brain function and quality of life in patients suffering from prolonged post concussion syndrome PCS as a result of a mTBI Speaker Biography Nadia is a Respiratory Therapy student at Conestoga College She has always had a passion for healthcare and the intricate workings of the human body Prior to life as an SRT she completed a bachelor s degree in Kinesiology at McMaster University There she fulfilled many placements in a variety of settings and was fortunate to work with diverse populations acquiring a growing interest in concussion management She completed certification as a concussion management practitioner allowing her to administer baseline tests assessments and exertional return to play protocols When she is not in class or studying you can find her in the clinic working with these patients CSRT 2020 E Conference Series www csrt com conference
biomolecules Review Hyperbaric Oxygen Treatment From Mechanisms to Cognitive Improvement Irit Gottfried 1 Nofar Schottlender 1 2 and Uri Ashery 1 2 1 2 Citation Gottfried I Schottlender N Ashery U Hyperbaric Oxygen School of Neurobiology Biochemistry and Biophysics Life Sciences Faculty Tel Aviv University Tel Aviv 6997801 Israel iritgo tauex tau ac il I G schottlender mail tau ac il N S Sagol School of Neuroscience Tel Aviv University Tel Aviv 6997801 Israel Correspondence uria tauex tau ac il Tel 972 3 6409827 Abstract Hyperbaric oxygen treatment HBOT the medical use of oxygen at environmental pressure greater than one atmosphere absolute is a very effective therapy for several approved clinical situations such as carbon monoxide intoxication incurable diabetes or radiation injury wounds and smoke inhalation In recent years it has also been used to improve cognition neurowellness and quality of life following brain trauma and stroke This opens new avenues for the elderly including the treatment of neurological and neurodegenerative diseases and improvement of cognition and brain metabolism in cases of mild cognitive impairment Alongside its integration into clinics basic research studies have elucidated HBOT s mechanisms of action and its effects on cellular processes transcription factors mitochondrial function oxidative stress and inflammation Therefore HBOT is becoming a major player in 21st century research and clinical treatments The following review will discuss the basic mechanisms of HBOT and its effects on cellular processes cognition and brain disorders Keywords hyperbaric oxygen treatment HBOT cognition brain disorders neuroprotection neuroinflammation Alzheimer s disease Treatment From Mechanisms to Cognitive Improvement Biomolecules 2021 11 1520 https doi org 10 3390 biom11101520 Academic Editor Vladimir N Uversky Received 14 September 2021 Accepted 13 October 2021 Published 15 October 2021 Publisher s Note MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations Copyright 2021 by the authors Licensee MDPI Basel Switzerland This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution CC BY license https creativecommons org licenses by 4 0 1 Hyperbaric Oxygen Treatment HBOT The Concept HBOT the medical administration of 100 oxygen at environmental pressure greater than one atmosphere absolute ATA is used clinically for a wide range of medical conditions One of HBOT s main mechanisms of action is elevation of the partial pressure of oxygen in the blood and tissues as compared to simple oxygen supplementation 1 2 This allows five to ten times more oxygen to enter the blood plasma and to reach tissues suffering from low oxygen supply following e g brain injury stroke or vascular dysfunction Therefore it is not surprising that HBOT has been used for over 50 years for wounds nonhealing diabetic foot ulcers air embolisms or decompression sickness burned tissue repair carbon monoxide intoxication peripheral arterial occlusive disease smoke inhalation radiation injury and promoting recovery from serious illness 3 10 Nevertheless today there are only 13 FDA approved HBOTs 11 however in parallel there are a growing number of off label uses which have not been cleared by the FDA such as treatment for stroke patients or patients suffering from Alzheimer s disease AD 12 13 and even treatment of COVID 19 patients which have shown very promising results 14 19 Further clinical trials that are currently in progress and additional basic scientific studies aimed at understanding HBOT s mechanisms of action will most probably expand the use of HBOT to other areas 2 Cognitive Improvement 2 1 Cognitive Improvement Following Brain Injuries Although the use of HBOT in cases of brain related disorders is pending FDA approval there are numerous studies showing improved cognitive assessment following Biomolecules 2021 11 1520 https doi org 10 3390 biom11101520 https www mdpi com journal biomolecules
Biomolecules 2021 11 1520 2 of 11 treatment for several brain injuries 20 For example post stroke patients suffer from reduced cognitive performance and in particular memory difficulties HBOT for stroke patients at late chronic stages has shown significant improvements in all memory measures These clinical improvements are well correlated with improvements in brain metabolism mainly in temporal areas High oxygen 92 alone was also shown to positively affect the working memory of individuals with intellectual and developmental disabilities at least in the short term 21 Similar improvement was seen in a large cohort of post stroke patients who underwent 40 HBOT sessions 2 ATA leading to significant neurological and cognitive improvements even at the late chronic phase after stroke 22 23 Mechanistically in preclinical studies HBOT has been suggested to reduce oxidative stress inflammation and neural apoptosis thereby improving functional recovery from stroke 24 It was also suggested that HBOT in rats suffering from ischemic stroke stimulates the expression of trophic factor and neurogenesis and the mobilization of bone marrow stem cells to the ischemic area which can enhance cell repair 25 In addition HBOT elevates cerebral blood flow CBF associated with restoration of physical abilities and cognitive functions 26 27 The improvement in cognition and executive functions as well as in physical abilities gait sleep and quality of life in these stroke patients continued for up to three months after the last treatment which was the follow up period in that study 27 These encouraging results suggest the occurrence of long term changes lasting the order of months Similarly in patients with mild traumatic brain injury TBI HBOT improved hippocampal CBF 28 and facilitated recovery during the rehabilitation phase 29 Moreover growing evidence suggests that HBOT can induce neuroplasticity and improve cognitive function in patients suffering from chronic neurocognitive impairment due to TBI stroke and anoxic brain damage 22 23 30 32 These changes were associated with the induction of cerebral angiogenesis increased CBF and volume and improved cerebral white and gray microstructures 33 Other teams have investigated whether HBOT can improve brain function and cognition in neurodegenerative diseases such as AD and vascular dementia VD and if HBOT can also affect healthy people or improve cognitive decline in the elderly who are suffering from cognitive impairments 2 2 Cognitive Improvement Following HBOT in AD and VD Recent human studies have shown that HBOT can improve cognitive functions in patients with mild cognitive impairment MCI AD and VD 13 20 34 38 and ameliorate the reduced brain metabolism in MCI and AD 34 35 Similarly cerebrovascular disease patients showed improvement in motor and cognitive performance compared to a control group following HBOT 38 Interestingly improvements in cognitive function assessed by Mini Mental State Exam MMSE and Mini Cog test were reported in AD patients even one month after the end of the last HBOT and for up to three months in amnestic MCI patients In addition HBOT ameliorated the reduced brain glucose metabolism in some of the AD and amnestic MCI patients 34 These are very promising results because they suggest that even with severe cognitive deterioration in progressive neurodegenerative brain disorders relatively short duration HBOT 40 min once a day for 20 days can improve conditions for one to three months In a more severe case of AD a longer treatment of eight weeks 1 15 ATA reversed the patient s symptomatic decline and PET scan showed an increase in brain metabolism 35 Nevertheless the current belief is that HBOT cannot revert severe cases with major neuron loss and therefore should be considered mainly at early disease stages when only minimal cognitive deficiency is detected It should be noted that the elevation of pressure by itself was also suggested to regulate AD 39 However further research in this direction should explore the exact effect A larger group of VD patients who received 12 weeks of HBOT 2 ATA showed improvement in MMSE scores and elevated serum humanin levels 36 Humanin is a unique human mitochondrion derived peptide that has neuroprotective effects 40 42 and together with findings of increased brain metabolism this suggests an important role for improving
Biomolecules 2021 11 1520 39 However further research in this direction should explore the exact effect A larger group of VD patients who received 12 weeks of HBOT 2 ATA showed improvement in 3 of 11 MMSE scores and elevated serum humanin levels 36 Humanin is a unique human mitochondrion derived peptide that has neuroprotective effects 40 42 and together with findings of increased brain metabolism this suggests an important role for improving mitochondrial function as as part of of HBOT s mechanism of of action AsAs HBOT use inin the clinic is mitochondrial function part HBOT s mechanism action HBOT use the clinic considered to be safesafe andand well tolerated it should be considered and recommended as an is considered to be well tolerated it should be considered and recommended alternative therapeutic approach for AD well in early stagesstages of MCI as an alternative therapeutic approach forand ADVD and 37 VDas 37 asas well as in early of Hence HBOTHBOT improves several aspects of brain including an improvement in cerMCI Hence improves several aspects of activity brain activity including an improvement ebral blood blood flow brain and brain and this and leadsthis to improvein cerebral flow metabolism brain metabolism andmicrostructure brain microstructure leads to ment in cognitive functions and physical functions sleep and gait leading to an improvement in cognitive functions and physical functions sleep and gait leadingoverall to an improved performance Figure 1 Nevertheless it is also it clear thatclear although the effectsthe of overall improved performance Figure 1 Nevertheless is also that although effects of HBOT last studies in some several months when treating patients with HBOT last in some forstudies several for months when treating patients with progressive progressive neurodegenerative diseases as AD maintenance HBOwill treatments neurodegenerative diseases such as AD such maintenance HBO treatments probablywill be probably needed be needed Figure HBOT has has been been shown shown to to improve improve cerebral cerebral blood blood flow flow Figure 1 1 HBOT HBOT improves improves brain brain function function HBOT brain metabolism metabolism and andbrain brain microstructure leading to improved cognitive functions physical microstructure leading to improved cognitive functions physical funcfunctions sleep tions sleep and and gait gait 2 3 Cognitive Improvement in Healthy Individuals 2 3 Cognitive Improvement in Healthy Individuals Over the last few decades several studies have examined the possible contribution Over the last few decades several studies have examined the possible contribution of HBOT to cognitive performance in both young and elderly populations In one of the of HBOT to cognitive performance in both young and elderly populations In one of the first studies examining the effects of HBOT on the elderly 43 it was found to improve first studies examining the effects of HBOT on the elderly 43 it was found to improve cognitive function in elderly patients with cognitive deficits In a more recent study with a cognitive function in elderly patients with cognitive deficits In a more recent study with cohort of healthy young adults HBOT increased spatial working memory and memory a cohort of healthy young adults HBOT increased spatial working memory and memory quotient and this was correlated with changes in regional homogeneity as measured by quotient andfunctional this was correlated with changes in regional homogeneity as measured by resting state MRI 44 In another prospective study double blind randomized resting state functional MRI 44 In another prospective study double blind randomized healthy volunteers were asked to perform a cognitive task a motor task and a simultanehealthy volunteers were to performwhile a cognitive task a motor and a Compared simultaneous cognitive motor taskasked multitasking in a functional HBO task chamber ous cognitive motor task multitasking while in a functional HBO chamber Compared to the performance under normobaric conditions single cognitive and motor task and to the performance under scores normobaric conditions single cognitive motor task and multitasking performance were significantly enhanced by theand HBO environment supporting the hypothesis that oxygen is a rate limiting factor for brain activity 45 These results were further validated by two recent studies that examined the effects of HBOT on healthy young 46 and old 47 adults In these studies HBOT resulted in an improved learning curve and higher resilience to interference of episodic memory in the healthy young adults 46 and induced cognitive enhancements in healthy aging adults which
multitasking performance scores were significantly enhanced by the HBO environment supporting the hypothesis that oxygen is a rate limiting factor for brain activity 45 These results were further validated by two recent studies that examined the effects of HBOT on healthy young 46 and old 47 adults In these studies HBOT resulted in an improved curve and higher resilience to interference of episodic memory in the healthy Biomolecules learning 2021 11 1520 4 of 11 young adults 46 and induced cognitive enhancements in healthy aging adults which were associated with regional improvement in CBF 47 Similarly in a recent paper a group of elderly patients with memory loss atimprovement baseline to HBOT improved were associated with regional in CBFshowed 47 Similarly in a cogrecent paper a nitive performances following 60 daily HBOT sessions 2 ATA and this was associated group of elderly patients with memory loss at baseline to HBOT showed improved cogwith an increase innitive CBF 48 Interestingly when was applied short time performances following 60HBOT daily HBOT sessionsfor 2 a ATA and this only was associated withthere an increase in CBF 48 Interestingly when HBOT was applied forelderly a short time only 15 consecutive days was no improvement in cognitive impairment in the 15 consecutive days there was no improvement in cognitive impairment in the elderly 49 49 suggesting that a longer treatment is necessary Indeed current protocols are extendsuggesting that months a longer 40 60 treatment is necessary current protocols are extending ing the treatment to two to three daily sessions 5Indeed days per week 2 3 ATA the treatment to two to three months 40 60 daily sessions 5 days per week 2 3 ATA and and promise to yield more significant and long lasting effects 12 promise to yield more significant and long lasting effects 12 In summary it is clear that the HBO environment in and of itself improves cognitive In summary it is clear that the HBO environment in and of itself improves cognitive performance and performance that this canand be that attributed to the elevated this can directly be attributed directly to theoxygen elevatedlevels oxygensuglevels suggestgesting that oxygen a rate limiting factor for brain However repeated ex exposure ingisthat oxygen is a rate limiting factor activity for brain 45 activity 45 However repeated posure to HBOT for longerfor periods time is to achieve long lasting effects thatthat lead to to HBOT longer of periods of needed time is needed to achieve long lasting effects in neuronal vascular neuronal and cellular activity as detailed in Figure 2 12 lead to changes in changes vascular and cellular activity as detailed in Figure 2 12 Figure 2 HBOT affects multiple cellular and molecular pathways HBOT affectsHBOT severalaffects molecular and molecular cellular pathways Figure 2 HBOT affects multiple cellular and molecular pathways several that are important for cellular and neuronal recovery including neuroprotection via SIRT1 oxidative stress via SIRT1 and and cellular pathways that are important for cellular and neuronal recovery including neuroprotecNrf 2 tion apoptosis via SIRT1 neurogenesis via Wnt3 Green frames represent proteins and processes that are upregulated via SIRT1 oxidative stress via SIRT1 and Nrf 2 apoptosis via SIRT1 neurogenesis via Wnt3 red frames proteins and processes are downregulated Abbreviations nuclearrepresent factor erythroid 2 related Greenrepresent frames represent proteins andthat processes that are upregulated red frames proteins factorand 2 Nrf 2 nuclear factor B NF B Hypoxia Inducible Factor factor 1 alphaerythroid HIF1a heme oxygenase processes that are kappa downregulated Abbreviations nuclear 2 related factor12 HO 1 superoxide dismutase 1 SOD1 malondialdehyde MDA B cell lymphoma 2 Bcl2 HIF1a Bcl 2 associated X protein Bax Nrf 2 nuclear factor kappa B NF B Hypoxia Inducible Factor 1 alpha heme oxygenase vascular endothelial growth factor VEGF A Glutathione S transferases GST Glutathione Peroxidase GPx 1 HO 1 superoxide dismutase 1 SOD1 malondialdehyde MDA B cell lymphoma 2 Bcl2 Bcl tumor necrosis factor alpha TNFa Wnt Family Member 3 Wnt3 2 associated X protein Bax vascular endothelial growth factor VEGF A Glutathione S transfer ases GST Glutathione Peroxidase GPx tumor necrosis factor alpha TNFa Wnt Family Member 3 Mechanistic Explanation for the Effects of HBOT on Cognition 3 Wnt3 What are the cellular and molecular pathways that contribute to the long term neuron function and cognition enhancing effects of HBOT A series of studies using animal models for brain injuries and brain diseases showed an improvement in the animals cognitive performance and provided a mechanistic understanding of some of HBOT s
Biomolecules 2021 11 1520 5 of 11 effects Not surprisingly these effects are not mediated by a single pathway but were found to be mediated by several pathways including inhibition of apoptosis improvement of mitochondrial function stem cell proliferation enhancement of antioxidant defense activity reduction in neuroinflammation and neuroprotection Figure 2 The normobaric oxygen paradox or hyperoxic hypoxic paradox has been suggested to play a key role in HBOT s effects 12 50 52 It is based on the fact that during HBOT sessions oxygen level is increased from 21 to 100 or less in some cases and at the end of each treatment oxygen level is reduced back to 21 Such fluctuations activate several factors elevation of oxygen can activate nuclear factor erythroid 2 related factor 2 Nrf 2 while the reduction to 21 can be interpreted as a hypoxic signal and activate Hypoxia Inducible Factor 1 alpha HIF1a 50 51 HIF1a belongs to a family of proteins that are involved in angiogenesis and vascular remodeling erythropoiesis glycolysis iron transport and survival 53 55 Nrf2 is involved in several cellular defense mechanisms and it mediates the repair and degradation of damaged proteins 51 55 56 and activates the antioxidant pathways and the detoxification of endogenous and exogenous products 57 Under high hyperoxia nuclear factor kappa B NF B which is usually activated under oxidative stress and inflammation is also activated 51 and mediates inflammatory and immune responses NF B is also involved in synaptic plasticity and in the antiapoptotic pathway by activating Bcl 2 58 Some of these effects are discussed below It should be noted that the optimal conditions for achieving best results from the Hyperoxic Hypoxic Paradox require additional research in the coming years 3 1 Mitochondrial Function Mitochondria consume roughly 85 to 90 of the oxygen that we breathe and are the major source of ATP production It is therefore likely that the main molecular target of HBOT is the mitochondrion As already noted humanin a neuroprotective mitochondrionderived peptide in humans was elevated in VD patients following HBOT 36 suggesting a major role for mitochondrial activity in HBOT s mechanisms of action Recent studies have suggested the therapy s direct effects on neurons were mediated by mitochondrial transfer from cell to cell HBOT was shown to facilitate the transfer of mitochondria from astrocytes to neuronal cells making the latter more resilient to neuroinflammation 59 This neuroglial crosstalk may facilitate recovery and explain some of the mechanisms induced by HBOT 50 In TBI rats HBOT for 4 h 1 5 ATA led to an increase in ATP levels and neuron survival both of which were associated with improved cognitive recovery 60 Furthermore in a rat model for AD HBOT reduced mitochondria mediated apoptosis signaling by increasing Bcl 2 which is anti apoptotic and decreasing Bcl 2 associated X protein Bax which is pro apoptotic 61 3 2 Neurogenesis and Angiogenesis An additional avenue for cognitive improvement might be stem cell proliferation Stem cell proliferation has been documented on various occasions following HBOT 62 64 and evidence for neuronal cell proliferation has emerged in the last two decades In an early study HBOT for hypoxic ischemic neonatal rats promoted neurogenesis of endogenous neuronal stem cells as measured by an increase in both 5 bromo 20 deoxyuridine BrdU and doublecortin in the subventricular zone SVZ and the hippocampal dentate gyrus DG an area involved in spatial navigation 65 Accordingly HBOT improved spatial learning and memory abilities in rats with TBI 66 This was associated with an increase in hippocampal neuronal activity These results were further supported by another study in which HBOT induced neuronal cell proliferation as revealed by an increase in nestin and BrdU in the hippocampal DG area 67 and elevation of Wnt 3 and nestin in the SVZ 68 In a study aimed at examining the mechanistic contribution of HBOT to recovery from TBI it was found that HBOT increases neuronal stem cell proliferation and migration to the lesion area as well as the levels of vascular endothelial growth factor VEGF and its receptor VEGFR 2 Raf 1
Biomolecules 2021 11 1520 6 of 11 Mitogen activated protein kinase MEK1 2 and phospho extracellular signal regulated kinase ERK 1 2 protein 69 Accordingly it was suggested that HBOT promotes neuronal stem cell proliferation and possibly angiogenesis through VEGF ERK signaling 69 Moreover in a rat model for VD HBOT also stimulated neurogenesis in the piriform cortex and improved blood supply 70 HBOT was also shown to enhance mobilization of bone marrow stem cells to an ischemic area and the release of trophic factors that can promote brain and neuronal recovery and enhance neurogenesis 25 Interestingly in patients with delayed encephalopathy after acute carbon monoxide poisoning HBOT mobilized circulating stem cells in the peripheral blood which was associated with improved cognition 71 In a TBI rat model HBOT stimulated angiogenesis as evidenced by a higher number of BrdU and VEGF positive cells and an increase in the number of BrdU and NeuNpositive cells suggesting enhanced neurogenesis 72 These findings provide support for improvement of human brain cognition associated with changes in cerebral angiogenesis and neuronal growth and proliferation improving CBF and brain activity 33 Indeed a recent study showed that HBOT improves blood flow in an AD mouse model by mitigating the blood vessel constriction that occurs in these AD mice under the regular course of the disease but without HBOT This was associated with an improved performance of the AD mice 48 Moreover in elderly patients with significant memory loss at baseline HBOT increased CBF and improved cognitive performance 48 It would be interesting to examine whether HBOT also restores neurogenesis in neurodegenerative diseases such as AD and whether it will affect neurogenesis and angiogenesis 73 in wild type mice and healthy humans 3 3 Neuroinflammation Another important effect of HBOT in several brain dysfunctions is reduced neuroinflammation TBI is usually associated with increased inflammation apoptosis and gliosis neuronal cell death and cognitive and motor dysfunction In a TBI rat model HBOT was shown to reduce neuroinflammation and increase levels of the anti inflammatory cytokine interleukin IL 10 these changes were associated with improvements in cognitive deficit 72 In an AD mouse model HBOT reversed hypoxia and ameliorated brain pathology and improved the animals behavioral performance 74 75 This improvement was also associated with a reduction in proinflammatory cytokines such as IL 1b IL 6 and tumor necrosis factor alpha TNF and an increase in anti inflammatory cytokines such as IL 4 and IL 10 leading to reduced neuroinflammation HBOT also significantly improved recovery from sepsis following cecal ligation and puncture the treatment was associated with a reduction in the inflammatory response including decreased expression of TNF IL 6 and IL 10 17 76 Changes in cytokines following exposure to oxygen have also been reported in humans A low intensity exercise program in combination with exposure to mild hyperoxia 30 elevates the proinflammatory IL 6 that contributes to host defense during infection and tissue while at both mild 30 oxygen and high hyperoxic state 100 oxygen the anti inflammatory cytokine IL 10 was elevated significantly 52 In a rat model for MCI HBOT had a protective effect on early cognitive dysfunction that was mediated by ERK These animals performed better in the Morris water maze and showed less apoptosis and better hippocampal cell morphology 77 In a rat model for AD that was induced by injections of amyloid peptide into the hippocampus HBOT improved animal behavior and reduced neuronal damage astrocyte activation and dendritic spine loss This was associated with a reduction in hippocampal p38 mitogen activated protein kinase MAPK phosphorylation 78 which occurs in the early stage of the disease and is associated with increased neuroinflammation cytoskeletal remodeling and tau phosphorylation 79 80 These papers suggest that the MAPK ERK pathways which are involved in cell proliferation and plasticity are also a target for HBOT
Biomolecules 2021 11 1520 7 of 11 3 4 Neuroprotective Antioxidant and Antiapoptotic Activities HBO preconditioning induced tolerance to cerebral ischemia 81 This was mediated by an increase in SIRT1 a class III histone deacetylase which has been suggested to be involved in neuroprotection 82 The neuroprotective effect of preconditioning HBOT was associated with a reduction in lactate dehydrogenase and was attenuated by a reduction in SIRT1 activity or expression by either the SIRT1 inhibitor EX527 or SIRT1 knockdown Interestingly the neuroprotective effect was mimicked by resveratrol a SIRT1 activator Changes in SIRT1 level were also associated with elevation in B cell lymphoma 2 Bcl 2 expression and a decrease in cleaved caspase 3 level suggesting that some of the effects might be mediated via inhibition of apoptosis 82 Moreover expression of SIRT1 in the brain was associated with increased expression of the nuclear factor erythroid 2 related factor 2 Nrf 2 heme oxygenase 1 HO 1 and superoxide dismutase 1 SOD1 whereas the level of malondialdehyde MDA decreased supporting the notion that HBOT enhances the antioxidant defense pathway thereby assisting in neuroprotection 83 Indeed HBO preconditioning increased the expression of SIRT1 Nrf 2 and HO 1 and ameliorated memory dysfunction in additional models of cognitive decline 84 and SIRT1 was also shown to play a role in recovery after middle cerebral artery occlusion in rats Therefore this might serve as the mechanism for HBOT s effects in cases of acute ischemic stroke 85 A combination of HBOT and Ginkgo biloba extract following induction of toxicity with amyloid A fragments demonstrated enhanced SOD and glutathione levels while levels of MDA and Bax and activity of caspases 9 and 3 were reduced in rat hippocampal tissue suggesting both antioxidant and antiapoptotic activity 61 86 In a mouse model for mild TBI HBOT improved learning abilities and prevented astrocyte activation and neuronal loss suggesting a neuroprotective effect 87 Additional involvement in apoptotic pathways was demonstrated in an AD rat model that showed improved cognitive and memory abilities following HBOT which were associated with NF B pathway activation and reduced hippocampal neuron loss 88 Further animal model studies may reveal additional mechanisms underlying the effects of HBOT thus facilitating the development of more efficient HBOT protocols Taken together HBOT has a multifaceted neuroprotective effect on the brain that involves the immune neuronal and vascular systems leading to enhancement and recovery of cognitive performance 4 HBOT The Next Leap HBOT has been used for centuries to treat a variety of symptoms and syndromes and in recent years it has been shown to improve many brain disorders Nevertheless it is still not fully established clinically and additional basic research and clinical trials are necessary Notably in recent years numerous such clinical trials have been supported by the NIH Over 230 clinical trials examining HBOT have been reported https clinicaltrials gov accessed on 4 September 2021 Of these 50 clinical trials are examining the effects of HBOT on brain related injuries and disorders Current and future clinical trials will provide additional validated information for a wider range of disorders while basic research will expand our mechanistic understanding and help optimize treatment conditions by allowing for more accurate determinations of treatment length frequency of treatments and the exact protocol This will reduce cost time and complications Overall HBOT is becoming a central player in the 21st century healthcare system with the ability to improve both personal performance and cognition Author Contributions All authors were involved in writing original draft preparation review and editing All authors have read and agreed to the published version of the manuscript Funding N S is supported by a Scholarship from the Tel Aviv University Center for Combatting Pandemics U A was supported by The Aufzien Family Center for the Prevention and Treatment of Parkinson s Disease at Tel Aviv University Conflicts of Interest The authors declare no conflict of interest
Biomolecules 2021 11 1520 8 of 11 References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 Calvert J W Cahill J Zhang J H Hyperbaric oxygen and cerebral physiology Neurol Res 2007 29 132 141 CrossRef Jones M W Brett K Han N Wyatt H A Hyperbaric Physics StatPearls Publishing Treasure Island FL USA 2019 Glik J Cholewka A Stanek A Englisz B Sieron K Miku s Zag rska K Knefel G Nowak M Kawecki M Thermal imaging and planimetry evaluation of the results of chronic wounds treatment with hyperbaric oxygen therapy Adv Clin Exp Med 2019 28 229 236 CrossRef Kasprzyk Kucewicz T Cholewka A Englisz Jurgielewicz B Mucha R Relich M Kawecki M Sieron K Onak P Stanek A Thermal effects of topical hyperbaric oxygen therapy in hard to heal wounds A pilot study Int J Environ Res Public Health 2021 18 6737 CrossRef Stanek A Gebala Prajsnar K Pasek J Prajsnar G Berszakiewicz A Sieron A Cholewka A Zabrze I Selected physical medicine interventions in the treatment of diabetic foot syndrome Acta Angiol 2015 21 140 145 CrossRef Lin P Y Sung P H Chung S Y Hsu S L Chung W J Sheu J J Hsueh S K Chen K H Wu R W Yip H K Clinical Medicine Hyperbaric Oxygen Therapy Enhanced Circulating Levels of Endothelial Progenitor Cells and Angiogenesis Biomarkers Blood Flow in Ischemic Areas in Patients with Peripheral Arterial Occlusive Disease J Clin Med 2018 7 548 CrossRef Carturan D Boussuges A Vanuxem P Bar Hen A Burnet H Gardette B Ascent rate age maximal oxygen uptake adiposity and circulating venous bubbles after diving J Appl Physiol 2002 93 1349 1356 CrossRef Edwards M Singh M Selesny S Cooper J S Hyperbaric Treatment of Thermal Burns StatPearls Publishing Treasure Island FL USA 2021 Cooper J S Hanley M E Hyperbaric Treatment of Radiation Proctitis StatPearls Publishing Treasure Island FL USA 2021 Hanley M E Manna B Hyperbaric Treatment of Diabetic Foot Ulcer StatPearls Publishing Treasure Island FL USA 2021 Hyperbaric Oxygen Therapy Get the Facts FDA Available online https www fda gov consumers consumer updates hyperbaric oxygen therapy get facts accessed on 6 October 2021 Kamat S M Mendelsohn A R Larrick J W Rejuvenation through Oxygen More or Less Rejuvenation Res 2021 24 158 163 CrossRef Somaa F A Review of the Application of Hyperbaric Oxygen Therapy in Alzheimer s Disease J Alzheimer s Dis 2021 81 1361 1367 CrossRef PubMed Thibodeaux K Speyrer M Raza A Yaakov R Serena T E Hyperbaric oxygen therapy in preventing mechanical ventilation in COVID 19 patients A retrospective case series J Wound Care 2020 29 S4 S8 CrossRef PubMed Abu El Hawa A A Charipova K Bekeny J C Johnson Arbor K K The evolving use of hyperbaric oxygen therapy during the COVID 19 pandemic J Wound Care 2021 30 S8 S11 CrossRef PubMed Paganini M Bosco G Perozzo F A G Kohlscheen E Sonda R Bassetto F Garetto G Camporesi E M Thom S R The Role of Hyperbaric Oxygen Treatment for COVID 19 A Review In Advances in Experimental Medicine and Biology Springer Cham Switzerland 2021 Volume 1289 pp 27 35 De Maio A Hightower L E COVID 19 acute respiratory distress syndrome ARDS and hyperbaric oxygen therapy HBOT What is the link Cell Stress Chaperones 2020 25 717 720 CrossRef Guo D Pan S Wang M M Guo Y Hyperbaric oxygen therapy may be effective to improve hypoxemia in patients with severe COVID 2019 pneumonia Two case reports Undersea Hyperb Med 2020 47 181 187 CrossRef PubMed Boet S Etherington C Djaiani G Tricco A C Sikora L Katznelson R Efficacy and safety of hyperbaric oxygen treatment in SARS CoV 2 COVID 19 pneumonia A systematic review Diving Hyperb Med 2021 51 271 281 CrossRef PubMed Marcinkowska A B Mankowska N D Kot J Winklewski P J Impact of Hyperbaric Oxygen Therapy on Cognitive Functions A Systematic Review Neuropsychol Rev 2021 CrossRef Kim H S Choi M H Baek J H Park S J Lee J C Jeong U H Kim S P Kim H J Choi Y Lim D W et al Effects of 92 oxygen administration on cognitive performance and physiological changes of intellectually and developmentally disabled people J Physiol Anthropol 2015 34 3 CrossRef PubMed Hadanny A Rittblat M Bitterman M May Raz I Suzin G Boussi Gross R Zemel Y Bechor Y Catalogna M Efrati S Hyperbaric oxygen therapy improves neurocognitive functions of post stroke patients a retrospective analysis Restor Neurol Neurosci 2020 38 93 107 CrossRef PubMed Efrati S Fishlev G Bechor Y Volkov O Bergan J Kliakhandler K Kamiager I Gal N Friedman M Ben Jacob E et al Hyperbaric oxygen induces late neuroplasticity in post stroke patients Randomized prospective trial PLoS ONE 2013 8 e53716 CrossRef PubMed Cozene B Sadanandan N Gonzales Portillo B Saft M Cho J Park Y J Borlongan C V An extra breath of fresh air Hyperbaric oxygenation as a stroke therapeutic Biomolecules 2020 10 1279 CrossRef Lee Y S Chio C C Chang C P Wang L C Chiang P M Niu K C Tsai K J Long course hyperbaric oxygen stimulates neurogenesis and attenuates inflammation after ischemic stroke Mediat Inflamm 2013 2013 512978 CrossRef PubMed Chen L Li F Gu D Hyperbaric oxygen therapy for cerebral blood flow and electroencephalogram in patients with acute cerebral infarction Choice for therapeutic occasion Neural Regen Res 2007 2 171 174 CrossRef Rosario E R Kaplan S E Khonsari S Vazquez G Solanki N Lane M Brownell H Rosenberg S S The Effect of Hyperbaric Oxygen Therapy on Functional Impairments Caused by Ischemic Stroke Neurol Res Int 2018 2018 3172679 CrossRef PubMed
Biomolecules 2021 11 1520 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 9 of 11 Ma J Hong G Ha E Hong H Kim J Joo Y Yoon S Lyoo I K Kim J Hippocampal cerebral blood flow increased following low pressure hyperbaric oxygenation in firefighters with mild traumatic brain injury and emotional distress Neurol Sci 2021 42 4131 4138 CrossRef PubMed Skiba M R ekas Dudziak A Beka a A P otek W Late application of hyperbaric oxygen therapy during the rehabilitation of a patient with severe cognitive impairment after a traumatic brain injury Clin Case Rep 2021 9 960 965 CrossRef PubMed Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E Efrati S Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 2015 33 943 951 CrossRef PubMed Boussi Gross R Golan H Fishlev G Bechor Y Volkov O Bergan J Friedman M Hoofien D Shlamkovitch N Ben Jacob E et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury Randomized prospective trial PLoS ONE 2013 8 e79995 CrossRef Harch P Andrews S Rowe C Lischka J Townsend M Yu Q Mercante D Hyperbaric oxygen therapy for mild traumatic brain injury persistent postconcussion syndrome A randomized controlled trial Med Gas Res 2020 10 8 20 CrossRef PubMed Tal S Hadanny A Sasson E Suzin G Efrati S Hyperbaric Oxygen Therapy Can Induce Angiogenesis and Regeneration of Nerve Fibers in Traumatic Brain Injury Patients Front Hum Neurosci 2017 11 508 CrossRef PubMed Chen J Zhang F Zhao L Cheng C Zhong R Dong C Le W Hyperbaric oxygen ameliorates cognitive impairment in patients with Alzheimer s disease and amnestic mild cognitive impairment Alzheimer s Dement 2020 6 e12030 CrossRef Harch P G Fogarty E F Hyperbaric oxygen therapy for Alzheimer s dementia with positron emission tomography imaging A case report Med Gas Res 2018 8 181 184 CrossRef Xu Y Wang Q Qu Z Yang J Zhang X Zhao Y Protective Effect of Hyperbaric Oxygen Therapy on Cognitive Function in Patients with Vascular Dementia Cell Transpl 2019 28 1071 1075 CrossRef You Q Li L Xiong S Q Yan Y F Li D Yan N N Chen H P Liu Y P Meta Analysis on the Efficacy and Safety of Hyperbaric Oxygen as Adjunctive Therapy for Vascular Dementia Front Aging Neurosci 2019 11 86 CrossRef Vila J F Balcarce P E Abiusi G R Dom nguez R O Pisarello J B Improvement in motor and cognitive impairment after hyperbaric oxygen therapy in a selected group of patients with cerebrovascular disease A prospective single blind controlled trial Undersea Hyperb Med 2005 32 341 349 Denis P A Alzheimer s disease A gas model The NADPH oxidase Nitric Oxide system as an antibubble biomachinery Med Hypotheses 2013 81 976 987 CrossRef Z rate S C Traetta M E Codagnone M G Seilicovich A Rein s A G Humanin a mitochondrial derived peptide released by astrocytes prevents synapse loss in hippocampal neurons Front Aging Neurosci 2019 11 123 CrossRef PubMed Hazafa A Batool A Ahmad S Amjad M Chaudhry S N Asad J Ghuman H F Khan H M Naeem M Ghani U Humanin A mitochondrial derived peptide in the treatment of apoptosis related diseases Life Sci 2021 264 118679 CrossRef Hashimoto Y Ito Y Niikura T Shao Z Hata M Oyama F Nishimoto I Mechanisms of neuroprotection by a novel rescue factor humanin from swedish mutant amyloid precursor protein Biochem Biophys Res Commun 2001 283 460 468 CrossRef PubMed Jacobs E A Winter P M Alvis H J Small S M Hyperoxygenation Effect on Cognitive Functioning in the Aged N Engl J Med 1969 281 753 757 CrossRef Yu R Wang B Li S Wang J Zhou F Chu S He X Wen X Ni X Liu L et al Cognitive enhancement of healthy young adults with hyperbaric oxygen A preliminary resting state fMRI study Clin Neurophysiol 2015 126 2058 2067 CrossRef PubMed Vadas D Kalichman L Hadanny A Efrati S Hyperbaric Oxygen Environment Can Enhance Brain Activity and Multitasking Performance Front Integr Neurosci 2017 11 25 CrossRef Suzin G Frolinger T H Yogev D Hadanny A Catalogna M Rassovsky Y Efrati S Oxygen The rate limiting factor for episodic memory performance even in healthy young individuals Biomolecules 2020 10 1328 CrossRef Hadanny A Malka D K Gil S Rahav B G Merav C Kobi D Yafit H Ramzia A H Efrat S Gregory F et al Cognitive enhancement of healthy older adults using hyperbaric oxygen A randomized controlled trial Aging 2020 12 13740 13761 CrossRef Shapira R Gdalyahu A Gottfried I Sasson E Hadanny A Efrati S Blinder P Ashery U Hyperbaric oxygen therapy alleviates vascular dysfunction and amyloid burden in an Alzheimer s disease mouse model and in elderly patients Aging 2021 13 20935 20961 CrossRef Raskin A Gershon S Crook T H Sathananthan G Ferris S The effects of hyperbaric and normobaric oxygen on cognitive impairment in the elderly Arch Gen Psychiatry 1978 35 50 56 CrossRef PubMed Hadanny A Efrati S The hyperoxic hypoxic paradox Biomolecules 2020 10 958 CrossRef PubMed Fratantonio D Virgili F Zucchi A Lambrechts K Latronico T Laf re P Germonpr P Balestra C Increasing oxygen partial pressures induce a distinct transcriptional response in human pbmc A pilot study on the normobaric oxygen paradox Int J Mol Sci 2021 22 458 CrossRef PubMed
Biomolecules 2021 11 1520 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 10 of 11 Balestra C Lambrechts K Mrakic Sposta S Vezzoli A Levenez M Germonpr P Virgili F Bosco G Laf re P Hypoxic and Hyperoxic Breathing as a Complement to Low Intensity Physical Exercise Programs A Proof of Principle Study Int J Mol Sci 2021 22 9600 CrossRef PubMed Van Vliet T Casciaro F Demaria M To breathe or not to breathe Understanding how oxygen sensing contributes to age related phenotypes Ageing Res Rev 2021 67 101267 CrossRef PubMed Greer S N Metcalf J L Wang Y Ohh M The updated biology of hypoxia inducible factor EMBO J 2012 31 2448 2460 CrossRef PubMed Fratantonio D Cimino F Speciale A Virgili F Need more than two to Tango Multiple tools to adapt to changes in oxygen availability BioFactors 2018 44 207 218 CrossRef Cimino F Speciale A Anwar S Canali R Ricciardi E Virgili F Trombetta D Saija A Anthocyanins protect human endothelial cells from mild hyperoxia damage through modulation of Nrf2 pathway Genes Nutr 2013 8 391 399 CrossRef Tonelli C Chio I I C Tuveson D A Transcriptional Regulation by Nrf2 Antioxid Redox Signal 2018 29 1727 1745 CrossRef Mattson M P Meffert M K Roles for NF B in nerve cell survival plasticity and disease Cell Death Differ 2006 13 852 860 CrossRef PubMed Lippert T Borlongan C V Prophylactic treatment of hyperbaric oxygen treatment mitigates inflammatory response via mitochondria transfer CNS Neurosci Ther 2019 25 815 823 CrossRef PubMed Zhou Z Daugherty W P Sun D Levasseur J E Altememi N Hamm R J Rockswold G L Bullock M R Protection of mitochondrial function and improvement in cognitive recovery in rats treated with hyperbaric oxygen following lateral fluid percussion injury J Neurosurg 2007 106 687 694 CrossRef PubMed Tian X Zhang L Wang J Dai J Shen S Yang L Huang P The protective effect of hyperbaric oxygen and Ginkgo biloba extract on A 25 35 induced oxidative stress and neuronal apoptosis in rats Behav Brain Res 2013 242 1 8 CrossRef Thom S R Milovanova T N Yang M Bhopale V M Sorokina E M Uzun G Malay D S Troiano M A Hardy K R Lambert D S et al Vasculogenic stem cell mobilization and wound recruitment in diabetic patients Increased cell number and intracellular regulatory protein content associated with hyperbaric oxygen therapy Wound Repair Regen 2011 19 149 161 CrossRef Goldstein L J Gallagher K A Bauer S M Bauer R J Baireddy V Liu Z J Buerk D G Thom S R Velazquez O C Endothelial Progenitor Cell Release into Circulation Is Triggered by Hyperoxia Induced Increases in Bone Marrow Nitric Oxide Stem Cells 2006 24 2309 2318 CrossRef Milovanova T N Bhopale V M Sorokina E M Moore J S Hunt T K Hauer Jensen M Velazquez O C Thom S R Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo J Appl Physiol 2009 106 711 728 CrossRef Yang Y J Wang X L Yu X H Wang X Xie M Liu C T Hyperbaric oxygen induces endogenous neural stem cells to proliferate and differentiate in hypoxic ischemic brain damage in neonatal rats Undersea Hyperb Med 2008 35 113 129 Liu S Shen G Deng S Wang X Wu Q Guo A Hyperbaric oxygen therapy improves cognitive functioning after brain injury Neural Regen Res 2013 8 3334 3343 CrossRef Wei L Wang J Cao Y Ren Q Zhao L Li X Wang J Hyperbaric oxygenation promotes neural stem cell proliferation and protects the learning and memory ability in neonatal hypoxic ischemic brain damage Int J Clin Exp Pathol 2015 8 1752 1759 Wang X L Yang Y J Xie M Yu X H Liu C T Wang X Proliferation of neural stem cells correlates with Wnt 3 protein in hypoxic ischemic neonate rats after hyperbaric oxygen therapy Neuroreport 2007 18 1753 1756 CrossRef Yang Y Wei H Zhou X Zhang F Wang C Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor extracellular signal regulated kinase signaling after traumatic brain injury Neuroreport 2017 28 1232 1238 CrossRef PubMed Zhang T Yang Q W W Wang S N N Wang J Z Z Wang Q Wang Y Luo Y J J Hyperbaric oxygen therapy improves neurogenesis and brain blood supply in piriform cortex in rats with vascular dementia Brain Inj 2010 24 1350 1357 CrossRef PubMed Zhang L Sun Q Xin Q Qin J Zhang L Wu D Gao G Xia Y Hyperbaric oxygen therapy mobilized circulating stem cells and improved delayed encephalopathy after acute carbon monoxide poisoning with up regulation of brain derived neurotrophic factor Am J Emerg Med 2021 42 95 100 CrossRef PubMed Lin K C C Niu K C C Tsai K J J Kuo J R R Wang L C C Chio C C C Chang C P P Attenuating inflammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury J Trauma Acute Care Surg 2012 72 650 659 CrossRef PubMed Buckley C J Cooper J S Hyperbaric Affects on Angiogenesis StatPearls Publishing Treasure Island FL USA 2021 Shapira R Solomon B Efrati S Frenkel D Ashery U Hyperbaric oxygen therapy ameliorates pathophysiology of 3xTg AD mouse model by attenuating neuroinflammation Neurobiol Aging 2018 62 105 119 CrossRef Shapira R Efrati S Ashery U Hyperbaric oxygen therapy as a new treatment approach for Alzheimer s disease Neural Regen Res 2018 13 CrossRef Halbach J L Prieto J M Wang A W Hawisher D Cauvi D M Reyes T Okerblom J Ramirez Sanchez I Villarreal F Patel H H et al Early hyperbaric oxygen therapy improves survival in a model of severe sepsis Am J Physiol Regul Integr Comp Physiol 2019 317 R160 R168 CrossRef
Biomolecules 2021 11 1520 77 78 79 80 81 82 83 84 85 86 87 88 11 of 11 Lin Y Lin X Zheng X Liu F Ye C Huang L Zhou Q Chen T Lin L Hyperbaric oxygen therapy cognitive function in a rat model of mild cognitive impairment via ERK signaling Ann Cardiothorac Surg 2020 9 3472 3480 CrossRef Zhao B Pan Y Wang Z Xu H Song X Hyperbaric oxygen pretreatment improves cognition and reduces hippocampal damage via p38 mitogen activated protein kinase in a rat model Yonsei Med J 2017 58 131 138 CrossRef Corr a S A L Eales K L The Role of p38 MAPK and Its Substrates in Neuronal Plasticity and Neurodegenerative Disease J Signal Transduct 2012 2012 1 12 CrossRef Sun A Liu M Nguyen X V Bing G p38 MAP kinase is activated at early stages in Alzheimer s disease brain Exp Neurol 2003 183 394 405 CrossRef Gamdzyk M Ma ek M Bratek E Koks A Kaminski K Ziembowicz A Salinska E Hyperbaric oxygen and hyperbaric air preconditioning induces ischemic tolerance to transient forebrain ischemia in the gerbil Brain Res 2016 1648 257 265 CrossRef Yan W Fang Z Yang Q Dong H Lu Y Lei C Xiong L SirT1 mediates hyperbaric oxygen preconditioning induced ischemic tolerance in rat brain J Cereb Blood Flow Metab 2013 33 396 406 CrossRef PubMed Xue F Huang J W Ding P Y Zang H G Kou Z J Li T Fan J Peng Z W Yan W J Nrf2 antioxidant defense pathway is involved in the neuroprotective effects of Sirt1 against focal cerebral ischemia in rats after hyperbaric oxygen preconditioning Behav Brain Res 2016 309 1 8 CrossRef PubMed Hong qiang H Mang qiao S Fen X Shan shan L Hui juan C Wu gang H Wen jun Y Zheng wu P Sirt1 mediates improvement of isoflurane induced memory impairment following hyperbaric oxygen preconditioning in middle aged mice Physiol Behav 2018 195 1 8 CrossRef Hu Q Manaenko A Bian H Guo Z Huang J L Guo Z N Yang P Tang J Zhang J H Hyperbaric Oxygen Reduces Infarction Volume and Hemorrhagic Transformation Through ATP NAD Sirt1 Pathway in Hyperglycemic Middle Cerebral Artery Occlusion Rats Stroke 2017 48 1655 1664 CrossRef Tian X Wang J Dai J Yang L Zhang L Shen S Huang P Hyperbaric Oxygen and Ginkgo Biloba Extract Inhibit A 25 35 induced Toxicity and Oxidative Stress in vivo A Potential Role in Alzheimer s Disease Int J Neurosci 2012 122 563 569 CrossRef Baratz Goldstein R Toussia Cohen S Elpaz A Rubovitch V Pick C G Immediate and delayed hyperbaric oxygen therapy as a neuroprotective treatment for traumatic brain injury in mice Mol Cell Neurosci 2017 83 74 82 CrossRef PubMed Zhang L D Ma L Zhang L Dai J G Chang L G Huang P L Tian X Q Hyperbaric oxygen and ginkgo biloba extract ameliorate cognitive and memory impairment via nuclear factor Kappa B pathway in rat model of alzheimer s disease Chin Med J 2015 128 3088 3093 CrossRef PubMed
MILITARY MEDICINE 187 1 2 e40 2022 Alternative Uses of Hyperbaric Oxygen Therapy in Military Medicine Current Positions and Future Directions Adam T Biggs PhD Lanny F Littlejohn MD Hugh M Dainer PhD MD Materials and Methods There were no inclusion or exclusion criteria for articles addressing currently approved HBOT uses as covered under the military health system These references were provided for comparison and illustration as needed For alternative HBOT uses the review focuses explicitly upon three alternative uses in PTSD mTBI and TBI The review addresses any piece of case study evidence observational data quasi experimental design or randomized controlled trial that explored any or a combination of these issues within an active duty population a veteran population or a civilian population Results The existing medical evidence does not support a consensus viewpoint for these alternative uses of HBOT Based on the literature review there are four competing positions to explain the lack of consistency among the empirical results These possibilities are described in no particular order First an explanation suggests that the results are because of placebo effects The combination of participant expectations and subjective symptom reporting creates the potential that reported improvements are because of placebo rather than casual mechanisms Second another position suggests that experiments have utilized sham conditions which induced therapeutic benefits If sham conditions have actually been weakened active treatment conditions rather than placebo controls it could explain the lack of observed significant differences in randomized clinical trials Third there has been a substantial amount of heterogeneity both in the symptoms treated and the treatments applied This heterogeneity could explain the inconsistency of the data and the difficulty in reaching a consensus viewpoint Fourth the HBOT treatments may actively treat some tangential medical issue the patient is having The treatment would thus promote an environment of healing without directly treating either PTSD mTBI or TBI and the reduction in orthogonal medical issues facilitates a pathway to recovery by reducing tangential medical problems Conclusions The mixed empirical evidence does not support recommending HBOT as a primary treatment for PTSD mTBI or TBI If applied under the supervision of a licensed military medical professional the consistently safe track record of HBOT should allow it to be considered as an alternative treatment for PTSD mTBI or TBI once primary treatment methods have failed to produce a benefit However the evidence does warrant further clinical investigation with particular emphasis on randomized clinical trials better placebo controls and a need to develop a consistent treatment protocol Naval Special Warfare Command Medical Department Coronado CA 92155 USA Naval Special Warfare Group FOUR Medical Department Virginia Beach VA 23521 USA The views expressed in this article reflect the results of research conducted by the author and do not necessarily reflect the official policy or position of the Department of the Navy the DoD or the U S Government The authors are military service members or federal contracted employees of the U S Government This work was prepared as part of their official duties Title 17 U S C 105 provides that copyright protection under this title is not available for any work of the U S Government Title 17 U S C 101 defines a U S Government work as work prepared by a military service member or employee of the U S Government as part of that person s official duties doi https doi org 10 1093 milmed usab022 e40 INTRODUCTION Hyperbaric oxygen therapy HBOT describes a technique wherein patients breathe air with above average oxygen concentration in a pressurized environment usually a tube or chamber The intent is to increase blood oxygen levels as a means to facilitate healing This technique is already well established and there are currently 13 FDA cleared uses for hyperbaric chambers including treatment of air or gas Published by Oxford University Press on behalf of the Association of Military Surgeons of the United States 2021 This work is written by a US Government employee s and is in the public domain in the US MILITARY MEDICINE Vol 187 January February 2022 Downloaded from https academic oup com milmed article 187 1 2 e40 6132032 by guest on 21 January 2022 ABSTRACT Introduction Hyperbaric oxygen therapy HBOT is a commonly used treatment for a variety of medical issues including more than a dozen currently approved uses However there are alternative proposed uses that have significant implications among an active duty military or veteran population as treatments for PTSD mild traumatic brain injury mTBI and traumatic brain injury TBI These applications have seen a recent groundswell of support from the operator and veteran communities raising the visibility of using HBOT for alternative applications The current review will cover the existing evidence regarding alternative uses of HBOT in military medicine and provide several possibilities to explain the potential conflicting evidence from empirical results
Alternative Uses of Hyperbaric Oxygen Therapy in Military Medicine embolism carbon monoxide poisoning decompression sickness and radiation necrosis 1 Although there are HBOT uses supported by the FDA there are also claims by various organizations and individuals which extend beyond these established uses Examples of more controversial treatments include the potential for HBOT treatments of cancer mild traumatic brain injury mTBI and Alzheimer s disease The goal of this review is to consider the available evidence regarding HBOT to include case studies and randomized placebocontrolled studies when evaluating the possible alternative uses of HBOT in military patients MILITARY MEDICINE Vol 187 January February 2022 FIGURE 1 Dissolved oxygen concentration in blood across different inspired oxygen levels and pressures Top line indicates result under 100 inspired oxygen level middle line indicates result under 75 inspired oxygen level and bottom line indicates result under 21 inspired oxygen level solution This state produces greater oxygenation because oxygen in solution can reach obstructed areas through which red blood cells could not pass as well as enabling oxygenation under conditions with impaired oxygen transportation via hemoglobin such as carbon monoxide poisoning 6 To describe with greater precision patients breathing normobaric air typically have arterial oxygen tensions of 100 mmHg and tissue oxygen tension of 55 mmHg whereas the combination of 100 oxygen at 2 0 3 0 ATA can produce arterial oxygen tension in excess of 2 000 mmHg and oxygen tension within tissues of almost 400 mmHg 7 These levels have numerous cellular and physiological benefits to a recovering patient Wound healing becomes expedited through angiogenesis facilitating the migration of macrophages and speeding epithelialization 8 These factors ultimately maintain tissue viability while reducing the possibility of infection and potentiating more beneficial recovery conditions However despite these multiple mechanisms of action which might enhance patient recovery therapeutic benefits are rarely attained from a single visit with some conditions requiring between 20 and 40 treatments 9 Modern HBOT is usually a safe procedure with protocols written to avoid the physical danger of combustion in an oxygen rich environment and physiological danger of toxic exposures Even so there are some potential side effects the patient may experience Common effects include middle ear barotrauma because of the pressure changes which can cause ear pain general discomfort and difficulty with ear equalization 10 These middle ear effects are typically mild and can be mitigated or avoided with proper ear clearing and appropriate compression rates The closeness of the space could conceivably induce claustrophobia which is dependent more on the combination of the specific chamber and individual than anything generalizable to HBOT at large Some more extreme side effects can occur such as central nervous system oxygen toxicity seizure pulmonary oxygen toxicity tracheobronchitis edema and fibrosis and ocular toxicity decreased e41 Downloaded from https academic oup com milmed article 187 1 2 e40 6132032 by guest on 21 January 2022 HOW DOES HBOT AFFECT THE PATIENT The direct biological impact of HBOT is to increase the amount of oxygen carried within the blood and into body tissues Under normal pressure at the sea level defined as 1 atmosphere 1 ATA the proportion of oxygen in the blood is most heavily dependent on saturated or oxygenladed hemoglobin as a result of the partial pressure to which the blood is exposed Partial pressure of the oxygen is typically high in the lungs and readily causes oxygen to bind to any available hemoglobin but in other tissues lower partial pressures causes the oxygen to be released from hemoglobin directly into the bloodstream and allows oxygenation of body tissues This relationship produces a sigmoid plot where there is a non linear relationship between hemoglobin saturation and the partial pressure of oxygen Many other factors besides the partial pressure of oxygen can affect this relationship including carbon monoxide2 and temperature 3 although pressure and oxygen concentration are considered the critical factors Hyperbaric oxygen therapy combines these factors by both increasing oxygen concentration of the air and increasing relative pressure which in turn maximizes the ability of hemoglobin to saturate with oxygen Moreover the increased pressure of HBOT is important because simply breathing gas with higher than normal oxygen levels normobaric oxygen therapy is less effective in increasing the oxygen capacity of the blood 4 This effect is because of higher levels of oxygen that dissolve directly in blood serum at pressures greater than 1 ATA See Fig 1 The end product is that HBOT causes higher levels of oxygen to reach tissues throughout the body not only through oxyhemoglobin but also because of oxygen dissolved directly in the serum In clinical practice patients enter a hyperbaric tube or environment that could be designed for a single user monoplace chamber or for multiple individuals multiplace chamber to use simultaneously Patients then breathe gas with increased oxygen concentration anywhere up to 100 compared to the 21 oxygen concentration of normal air while experiencing an environment with increased pressure For HBOT common pressures include up to 3 0 ATA although the precise value used during treatment varies significantly by treatment regimen device and conditions being treated 5 Increased pressure allows among other things more oxygen to be carried in
Alternative Uses of Hyperbaric Oxygen Therapy in Military Medicine though typically temporary visual acuity but these issues are rare with modern treatment protocols 10 e42 MILITARY MEDICINE Vol 187 January February 2022 Downloaded from https academic oup com milmed article 187 1 2 e40 6132032 by guest on 21 January 2022 EVIDENCE CONCERNING HYPERBARIC OXYGEN THERAPY APPROVED USES Even though HBOT has previously been demonstrated as a safe and reliable method to increase oxygenation and facilitate healing the controversial issues arise when discussing the evidence for and against some of its potential uses The best evidence supporting HBOT comes in established medical uses that have already received various approval or cleared uses by governing bodies such as the FDA or professional medical organizations There are currently 13 FDA cleared uses for HBOT chambers air or gas embolism carbon monoxide poisoning clostridal myositis crush injury or other acute traumatic ischemias decompression sickness bends enhancement of healing in select wounds exceptional blood loss severe anemia intracranial abscess necrotizing soft tissue infections osteomyelitis delayed radiation injury skin grafts and flaps and thermal burns 11 Within these FDA cleared options there remain numerous questions about the most efficacious usage of HBOT For example there are questions as to the duration of benefits and which treatment time window is best administered for optimal impact Some evidence attained from patients with diabetic foot ulcers suggested more benefits of HBOT in short term usage compared to long term issues 12 which aligns with research that HBOT has neuroprotective effects when administered within the acute phase of trauma 13 Despite the FDA cleared uses and evidence supporting them individual treatment regimens differ in pressure applied time of treatment number of treatments and overall benefit to be anticipated from HBOT The latter point is particularly important as it will impact choices among treatment options and associated costs The empirical literature suggests that some benefit should be conferred yet the scope and scale of such facilitated healing continue to be a subject of debate One study observed a reduction in ulcer area between 33 and 62 when treating diabetic foot ulcer across a variety of protocols 12 although even in these uses the authors concluded that further research was necessary to address experimental shortcomings It is possible to selectively choose from various studies and observe comparable benefits in diseases ranging from cardiac ischemia to neonatal hypoxia 14 yet moderate improvement is a reasonable expectation within the same repeated caveat Specifically improvements are regularly observed following HBOT in the various FDA cleared uses for the treatment with the understanding that anticipated benefits vary substantially Ultimately an important interpretation is that many of the current HBOT uses counter some state in which the patient suffers from oxygen deficiencies or would otherwise benefit from the body s response to increased oxygenation EVIDENCE CONCERNING HYPERBARIC OXYGEN THERAPY PTSD MTBI AND TBI Discussion and research continue regarding uses not currently on the FDA cleared list The most significant discussion appears to be regarding the evidence for and against using HBOT as a treatment for PTSD traumatic brain injury TBI or mild traumatic brain injury TBI There are additional ongoing clinical investigations regarding autism and cerebral palsy with a robust literature that likewise includes widely variable results However the remainder of this discussion will focus on PTSD and mTBI TBI as the more relevant treatment needs for military medicine and literature concerning other disorders such as autism and cerebral palsy will not be reviewed here The website https clinicaltrials gov offers a searchable database of ongoing publicly funded and privately funded clinical trials To explore current clinical trials involving HBOT beyond mTBI TBI and PTSD we recommend searching this website The evidence for HBOT in PTSD mTBI TBI is controversial because the results are so mixed in the empirical literature and strong proponents exist both for and against the method Preliminary evidence supporting the use of HBOT for these conditions comes from case studies with anywhere between 1 and 6 patients as a part of the treatment These examples demonstrate improvements in neuropsychological functioning for mTBI 15 chronic TBI 16 17 and improvements in PTSD symptoms 18 19 Alternatively some case studies could caution medical professionals about rare complications such as tension pneumocephalus because of unrepaired skull fractures 20 However this evidence should be interpreted with caution for several reasons The primary reason is that causal factors are much more difficult to isolate in case studies compared to randomized placebo controlled studies which limits the conclusions that can be made from these observations Additionally case studies are inherently prone to publication bias 21 The point being that suggestive or exciting results tend to be published whereas the failures and less surprising outcomes tend to be withheld Substantial improvements and rare complications both fall into the more evocative category and increase the visibility of these cases through a publication bias Even so case study evidence should be considered alongside the greater contextual evidence supporting or refuting HBOT for these more controversial conditions but this evidence should be considered alongside the results of more carefully controlled clinical investigations in humans Several clinical trials primarily dealing with postconcussion syndrome have demonstrated significant improvements in cognitive testing and quality of life assessments following HBOT treatments 22 23 Patients undergoing HBOT or even a combined hyperbaric hyperoxia and normobaric hyperoxia treatment24 have exhibited reduced mortality rates and numerous beneficial conditions to include increased cerebral blood flow 25 There are also some pieces of empirical
Alternative Uses of Hyperbaric Oxygen Therapy in Military Medicine WHY SO MUCH CONTRADICTING EVIDENCE FOR HBOT IN PTSD MTBI AND TBI The evidence thus far provides very disparate findings when HBOT is specifically evaluated in the context of PTSD or as a therapy following a post concussive event either of which have significant implications for military medicine Unfortunately there are multiple discrepancies between studies that prevent simple comparisons between conditions For example some studies utilize a normal treatment course without pressurized chamber intervention as well a sham condition whereas other studies utilize equivalent pressure conditions with different inspired oxygen levels The majority of studies follow a treatment regimen of 40 sessions across 6 8 weeks although there are exceptions to this too as some studies MILITARY MEDICINE Vol 187 January February 2022 will utilize fewer sessions Differences across treatment types and sham conditions substantially complicate any consensus across these incongruent results However there are currently four primary positions which could be offered as possibilities to explain the current findings 1 placebo effects 2 active sham treatments 3 treatment heterogeneity and 4 the facilitation argument Each position will be discussed in turn for its relevance to the wider conversation Placebo Effects One position argues against the effectiveness of HBOT treatments by suggesting the observed improvements are largely if not solely because of placebo effects This evidence is supported by the failure of HBOT to produce greater than sham benefits across multiple randomized clinical trials when the procedure is compared to a sham intervention 29 33 A sham condition is essential in these randomized clinical trials for several reasons Foremost simple observation over time could be masked by natural healing during the same period and a control condition provides an important comparison against the intervention technique Second any intervention is regularly anticipated to produce improvement because of the expectations of the individual patient This improvement could be in the form of a placebo effect where a patient s belief in the treatment facilitates improvement under the treatment regimen or a Hawthorne effect where the patient is reacting differently because of the presence of an observer during the evaluation 34 Each factor could be impacting the results in a different way For example patients can readily feel the pressure change and therefore predict when they are undergoing the treatment condition which is why a pressure of at least 1 2 ATA is recommended to mask the pressurization process 35 The Hawthorne effect is particularly important for clinical evaluations assessing symptomology because an individual patient may report fewer symptoms simply because of their awareness of the evaluation or an attempt conscious or unconscious to align with what they believe to be the desired result These combined possibilities could produce seeming improvements in cognitive or symptomatic reports following HBOT despite no reliable causal change in the individual that would support prolonged benefits of treatment Sham or control comparisons are the best way to prevent reduce or categorize the scope of placebo effects and when an active HBOT condition fails to outperform the sham pressure condition in a double blind placebocontrolled study a logical conclusion is that any observed benefits are because of some form of placebo effect and not because of a true clinical improvement in the patient s condition Active Sham Treatments The counterargument to the placebo effects position is that many of the sham conditions used in randomized clinical trials are not actually sham conditions they are inadvertently e43 Downloaded from https academic oup com milmed article 187 1 2 e40 6132032 by guest on 21 January 2022 evidence to support underlying mechanisms that might provide causal factors to explain these improvements Notably HBOT can induce neuroplasticity through angiogenesis and nerve fiber regeneration in patients who have suffered TBI while potentially reducing inflammatory responses 26 Retrospective studies have likewise reviewed patient records and concluded that there are significant benefits to the use of HBOT for TBI patients and others suffering from postconcussive symptoms 27 These studies also identify several unknowns about the treatment such as the duration of these benefits One study demonstrated significant improvements in post concussive and PTSD symptoms yet these benefits lasted less than 6 months 28 This issue will in turn inherently affect the required duration of any treatment regimen and the expected impact on long term quality of life The primary counterevidence to these claims comes from randomized clinical trials that attempt to use sham conditions to address the possibility of placebo effects Essentially case studies and some empirical studies typically provide an active condition for HBOT with increased inspired oxygen concentration under increased atmospheric pressure Randomized clinical trials also tend to provide a corresponding sham or placebo condition that administers a variant of the active condition to make any improvements because of patient anticipation These control conditions vary but each approach tends to provide one of the following a sham control with pressured but non hyperbaric environment inspired oxygen rates lower than room air both partial pressure and lower oxygen rates or some combination thereof to create a condition intended to simulate normal breathing or at least watered down hyperbaric conditions Hyperbaric oxygen therapy treatments have failed to produce greater benefits than sham treatments across several randomized clinical trials for those trials that included more rigorous control conditions 29 33 Although both HBOT and sham treatments typically produced improved performance on cognitive or symptomatic evaluations the clinical trials ultimately concluded that the benefits of HBOT were not significantly better than a sham treatment Some researchers and clinicians may therefore conclude that HBOT is equivalent to sham treatment
Alternative Uses of Hyperbaric Oxygen Therapy in Military Medicine Treatment Heterogeneity Some authors suggest that the heterogeneity of human TBI and issues with multiple factors such as delayed treatment timeline and subjective methods in outcome measurement could produce a misinterpretation of the results 37 This argument could explain both the mixed findings of the previous literature and why an otherwise effective treatment regimen might not generate reliable improvements during patient recovery TBI and mTBI research inherently have variability in observed symptoms because concussive events rarely produce the exact same symptomology or the same severity The variance is ultimately addressed through multiple studies and replication or failure to replicate which should overcome the issue of variance in symptomology HBOT research does not have sufficient volume of empirical evidence to make conclusive statements across symptom severity Similarly there are issues in the heterogeneity of the treatments themselves with varying pressurized levels between 1 5 and 3 0 ATA in the HBOT condition as well as differences in both the number of sessions and length of individual sessions The empirical literature is still addressing potential efficacy of HBOT in general and treatment heterogeneity contributes to further confusion among the results In short the treatment heterogeneity argument suggests that there is not sufficient evidence to come to a definitive conclusion regarding HBOT efficacy because the HBOT treatments have not been applied consistently Facilitation Argument There is empirical and mechanistic evidence available that HBOT can produce neurologically significant benefits to a patient 15 17 These benefits are well evidenced through e44 FDA cleared uses of the treatment regimen7 and through studies demonstrating neuroplasticity or other neurological benefits at a cellular level 13 26 As such there is one possibility that HBOT intervention will produce some therapeutic effect by improving the health of an individual following a traumatic event that caused either general physiological impairments or psychological distress If the individual experiences cognitive and general mental functioning improvements or physiological improvements following HBOT treatment these improvements could facilitate recovery by removing obstacles in their daily lives By this position there are no direct mechanistic relationships to PTSD or psychological impairments but the treatment may address tangential cognitive or psychological issues from which the patient is suffering In turn the absence of additional neurological challenges facilitates and smooths a pathway to recovery This position would explain why there is some mechanistic evidence for neurological improvement while still producing mixed results in clinical trials when orthogonal or comorbid issues are not fully addressed However we should note that this position is only speculative The facilitation argument ostensibly calls for more latent variable analyses to address indirect effects in HBOT studies and discount alternative explanations SUMMARY AND CONCLUSIONS Hyperbaric oxygen therapy is recognized as a safe commonly used medical procedure However there is an ongoing debate among the medical literature regarding the efficacy of HBOT as a potential treatment for PTSD mTBI and TBI Reviews and opinions cover both sides of the argument with individuals claiming both sufficient support to pursue HBOT as a treatment for these issues36 and highly critical opinions challenging HBOT intervention as a waste of time waste of money and providing false hope to impaired servicemembers 38 At present multiple DoD reviews from the Government Accountability Office39 and the Department of Veteran s Affairs11 have considered the evidence and concluded that the robust treatment benefits observed in individual case studies have not been evident in controlled randomized clinical trials thereby failing to reach a sufficient level of scientific evidence mandating or supporting this treatment for medically prescribed applications as far as PTSD mTBI and TBI are concerned The strongest evidence supporting HBOT has been produced by case studies and animal models that help support mechanisms by which HBOT could impact neurological functioning Unfortunately these findings have failed to transition well into human clinical trials instead producing highly mixed results regarding the efficacy of the treatment The current most reliable conclusion is that HBOT can be safely used for its FDA cleared applications and while its minimal risks make it a potential adjunct treatment regimen for other issues to include PTSD mTBI and TBI there is not sufficient clinical evidence at the present time to support its use as a MILITARY MEDICINE Vol 187 January February 2022 Downloaded from https academic oup com milmed article 187 1 2 e40 6132032 by guest on 21 January 2022 active conditions that likewise produce a therapeutic benefit 36 This argument is sometimes referred to colloquially as the sham is not a sham position Under this premise active conditions are not outperforming sham conditions because the sham conditions are actually producing a reliable albeit smaller treatment effect contributing to greater difficulty in achieving a statistically significant difference between conditions This argument could be a factor in combined conditions of higher pressure and inspired oxygen levels greater than room air Pressurizing air between 1 2 and 1 3 ATA produces between a 33 and 49 increase in dissolved oxygen in the bloodstream Combined with the lack of guidelines for oxygen and pressure combinations among this alternative treatment supposedly sham conditions could increase dissolved oxygen content in the bloodstream e g because of increased pressure intended to simulate full treatment pressurization and induce similar therapeutic conditions to the actual active treatment If studies are not suitably powered to detect statistical differences between two active treatment conditions of varying effect size then the result would be a non statistically significant difference for a real effect
Alternative Uses of Hyperbaric Oxygen Therapy in Military Medicine primary treatment method for post concussive issues following military deployment or blast exposure That said given the thorough track record of safety for HBOT when overseen by a licensed military professional consideration for HBOT as an alternative treatment is reasonable on a case by case basis particularly where standard treatments have failed to produce significant improvements understanding that these treatments may not be covered financially by the military health system FUNDING No external funding was received for this work CONFLICT OF INTEREST STATEMENT The authors declare no financial or non financial conflicts of interest SOURCE OF SUPPORT None declared HUMAN RESEARCH No human subjects research was involved in this review REFERENCES 1 Food and Drug Administration Consumer Update Hyperbaric oxygen therapy don t be misled 2013 Available at https www fda gov cons umers consumer updates hyperbaric oxygen therapy dont be misled August 23 accessed September 12 2019 2 Barker SJ Tremper KK The effect of carbon monoxide inhalation on pulse oximetry and transcutaneous PO2 Anesthesiology 1987 66 5 677 9 3 Knowles TP Mullin RA Hunter JA Douce HF Effects of syringe material sample storage time and temperature on blood gases and oxygen saturation in arterialized human blood samples Respir Care 2006 51 7 732 6 4 Eve DJ Steele MR Sanberg PR Borlongan CV Hyperbaric oxygen therapy as a potential treatment for post traumatic stress disorder associated with traumatic brain injury Neuropsychiatr Dis Treat 2016 12 2016 2689 MILITARY MEDICINE Vol 187 January February 2022 e45 Downloaded from https academic oup com milmed article 187 1 2 e40 6132032 by guest on 21 January 2022 SEARCH PROCESS AND INCLUSION CRITERIA Preliminary searches began with published reviews of the HBOT literature with specific emphasis on three alternative uses mTBI TBI and PTSD Hyperbaric oxygen therapy was entered into multiple databases such as PubMed and Google Scholar along with the additional terms of mild traumatic brain injury traumatic brain injury or post traumatic stress disorder This review had no limitations based upon case study evidence observational data quasi experimental design or randomized controlled trial that explored any or a combination of these issues within an active duty population a veteran population or a civilian population There were no inclusion or exclusion criteria for articles addressing currently approved HBOT uses as covered under the military health system Each reference was included to support of an illustrative point of existing uses or to describe the process of administering hyperbaric oxygen References were constrained only by the maximum permissible amount under this journal format 5 Mathieu D Neviere R Pellerin P Patenotre P Wattel F Pedicle musculocutaneous flap transplantation prediction of final outcome by transcutaneous oxygen measurements in hyperbaric oxygen Plast Reconstr Surg 1993 91 2 329 34 PMID 8430149 6 Gill AL Bell CN Hyperbaric oxygen its uses mechanisms of action and outcomes QJM 2004 97 7 385 95 7 Tibbles PM Edelsberg JS Hyperbaric oxygen therapy N Engl J Med 1996 334 25 1642 8 8 Kindwall EP Gottlieb LJ Larson DL Hyperbaric oxygen therapy in plastic surgery a review article Plast Reconstr Surg 1991 88 5 898 908 9 Mayo Clinic Hyberbaric oxygen therapy Available at https www mayoclinic org tests procedures hyperbaric oxygen therapy about pa c 20394380 January 12 2018 accessed September 13 2019 10 Plafki C Peters P Almeling M Welslau W Busch R Complications and side effects of hyperbaric oxygen therapy Aviat Space Environ Med 2000 71 2 119 24 11 Peterson K Bourne D Anderson J Boundy E Helfand M Evidence brief Hyperbaric Oxygen Therapy HBOT for traumatic brain injury and or post traumatic stress disorder In VA Evidence Synthesis Program Evidence Briefs Internet Department of Veterans Affairs 2018 Available from https www ncbi nlm nih gov books NBK499535 accessed February 02 2021 12 Kranke P Bennett MH Martyn St James M Schnabel A Debus SE Weibel S Hyperbaric oxygen therapy for chronic wounds Cochrane Database Syst Rev 2015 6 13 Lin KC Niu KC Tsai KJ et al Attenuating inflammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury J Trauma Acute Care Surg 2012 72 3 650 9 14 Shahriari A Khooshideh M Heidari M Diseases treated with hyperbaric oxygen therapy a literature review Med Hypothesis Discovery Innovation Interdiscip Sci J 2014 1 2 15 Wright CJK Zant E Groom K Schlegel RE Gilliland K Case report treatment of mild traumatic brain injury with hyperbaric oxygen Undersea Hyperbaric Med 2009 36 6 391 99 16 Hardy P Johnston KM De Beaumont L et al Pilot case study of the therapeutic potential of hyperbaric oxygen therapy on chronic brain injury J Neurol Sci 2007 253 1 2 94 105 17 Stoller KP Hyperbaric oxygen therapy 1 5 ATA in treating sports related TBI CTE two case reports Med Gas Res 2011 1 1 17 18 Improvement of PCS and PTSD following SPECT and HBOT Harch PG Fogarty PG Staab PK Van Meter K Low pressure hyperbaric oxygen therapy and SPECT brain imaging in the treatment of blastinduced chronic traumatic brain injury post concussion syndrome and post traumatic stress disorder a case report Cases J 2009 2 1 6538 19 Improvement in PTSD symptoms Eovaldi B Zanetti C Hyperbaric oxygen ameliorates worsening signs and symptoms of post traumatic stress disorder Neuropsychiatr Dis Treat 2010 6 1 785 20 Lee LC Lieu FK Chen YH Hung TH Chen SF Tension pneumocephalus as a complication of hyperbaric oxygen therapy in a patient with chronic traumatic brain injury Am J Phys Med Rehabil 2012 91 6 528 32 21 Easterbrook PJ Gopalan R Berlin JA Matthews DR Publication bias in clinical research Lancet 1991 337 8746 867 72 22 Boussi Gross R Golan H Fishlev G et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 2013 8 11 e79995 23 Harch PG Andrews SR Fogarty EF et al A phase I study of lowpressure hyperbaric oxygen therapy for blast induced post concussion syndrome and post traumatic stress disorder J Neurotrauma 2012 29 1 168 85
Alternative Uses of Hyperbaric Oxygen Therapy in Military Medicine e46 31 Wares JR Cifu DX Hoke KW Wetzel PA Gitchel G Carne W Effects of hyperbaric oxygen on eye tracking abnormalities in males after mild traumatic brain injury J Rehabil Res Dev 2014 51 7 1047 56 32 Cifu DX Walker WC West SL et al Hyperbaric oxygen for blastrelated postconcussion syndrome three month outcomes Ann Neurol 2014 75 2 277 86 33 Miller RS Weaver LK Bahraini N et al Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms a randomized clinical trial JAMA Intern Med 2015 175 1 43 52 34 Adair JG The Hawthorne effect a reconsideration of the methodological artifact J Appl Psychol 1984 69 2 334 45 35 Weaver LK Bell J Deru K A blinded trial to investigate whether pressure familiar individuals can determine chamber pressure Undersea Hyperbaric Med 2012 39 4 801 5 36 Figueroa XA Wright JK Hyperbaric oxygen B level evidence in mild traumatic brain injury clinical trials Neurology 2016 87 13 1400 6 37 Hu Q Manaenko A Xu T Guo Z Tang J Zhang JH Hyperbaric oxygen therapy for traumatic brain injury bench to bedside Med Gas Res 2016 6 2 102 10 38 Bennett MH Evidence brief Hyperbaric Oxygen Therapy HBOT for traumatic brain injury and or post traumatic stress disorder Diving Hyperb Med 2018 48 2 115 39 Government Accountability Office Research on hyperbaric oxygen therapy to treat traumatic brain injury and post traumatic stress disorder Available at https www gao gov assets 680 674334 pdf December 2015 accessed September 16 2019 MILITARY MEDICINE Vol 187 January February 2022 Downloaded from https academic oup com milmed article 187 1 2 e40 6132032 by guest on 21 January 2022 24 Rockswold SB Rockswold GL Zaun DA Liu J A prospective randomized Phase II clinical trial to evaluate the effect of combined hyperbaric and normobaric hyperoxia on cerebral metabolism intracranial pressure oxygen toxicity and clinical outcome in severe traumatic brain injury J Neurosurg 2013 118 6 1317 28 25 Rockswold SB Rockswold GL Zaun DA et al A prospective randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism intracranial pressure and oxygen toxicity in severe traumatic brain injury J Neurosurg 2010 112 5 1080 94 26 Tal S Hadanny A Sasson E Suzin G Efrati S Hyperbaric oxygen therapy can induce angiogenesis and regeneration of nerve fibers in traumatic brain injury patients Front Hum Neurosci 2017 19 11 508 27 Hadanny A Abbott S Suzin G Bechor Y Efrati S Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post traumatic brain injury patients retrospective analysis BMJ Open 2018 8 9 e023387 28 Weaver LK Wilson SH Lindblad AS et al Hyperbaric oxygen for post concussive symptoms in United States military service members a randomized clinical trial Undersea Hyperbaric Med 2018 45 2 129 56 29 Wolf G Cifu D Baugh L Carne W Profenna L The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury J Neurotrauma 2012 29 17 2606 12 30 Cifu DX Hart BB West SL Walker W Carne W The effect of hyperbaric oxygen on persistent postconcussion symptoms J Head Trauma Rehabil 2014 29 1 11 20
Hyperbaric Oxygen Therapy Can Improve Post Concussion Syndrome Years after Mild Traumatic Brain Injury Randomized Prospective Trial Rahav Boussi Gross1 Haim Golan3 4 Gregori Fishlev1 Yair Bechor1 Olga Volkov3 4 Jacob Bergan1 Mony Friedman1 Dan Hoofien6 7 Nathan Shlamkovitch8 Eshel Ben Jacob2 5 9 10 Shai Efrati1 2 3 10 1 The Institute of Hyperbaric Medicine Assaf Harofeh Medical Center Zerifin Israel 2 Research and Development Unit Assaf Harofeh Medical Center Zerifin Israel 3 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 4 Nuclear Medicine institute Assaf Harofeh Medical Center Zerifin Israel 5 The Raymond and Beverly Sackler Faculty of Exact Sciences School of Physics and Astronomy Tel Aviv University Tel Aviv Israel 6 Department of Psychology The Hebrew University of Jerusalem Jerusalem Israel 7 The National Institute for the Rehabilitation of the Brain Injured Tel Aviv Israel 8 Otolaryngology Head Neck Surgery Assaf Harofeh Medical Center Zerifin Israel 9 Center for Theoretical Biological Physics Rice University Houston Texas United States of America 10 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Abstract Background Traumatic brain injury TBI is the leading cause of death and disability in the US Approximately 70 90 of the TBI cases are classified as mild and up to 25 of them will not recover and suffer chronic neurocognitive impairments The main pathology in these cases involves diffuse brain injuries which are hard to detect by anatomical imaging yet noticeable in metabolic imaging The current study tested the effectiveness of Hyperbaric Oxygen Therapy HBOT in improving brain function and quality of life in mTBI patients suffering chronic neurocognitive impairments Methods and Findings The trial population included 56 mTBI patients 1 5 years after injury with prolonged postconcussion syndrome PCS The HBOT effect was evaluated by means of prospective randomized crossover controlled trial the patients were randomly assigned to treated or crossover groups Patients in the treated group were evaluated at baseline and following 40 HBOT sessions patients in the crossover group were evaluated three times at baseline following a 2 month control period of no treatment and following subsequent 2 months of 40 HBOT sessions The HBOT protocol included 40 treatment sessions 5 days week 60 minutes each with 100 oxygen at 1 5 ATA Mindstreams was used for cognitive evaluations quality of life QOL was evaluated by the EQ 5D and changes in brain activity were assessed by SPECT imaging Significant improvements were demonstrated in cognitive function and QOL in both groups following HBOT but no significant improvement was observed following the control period SPECT imaging revealed elevated brain activity in good agreement with the cognitive improvements Conclusions HBOT can induce neuroplasticity leading to repair of chronically impaired brain functions and improved quality of life in mTBI patients with prolonged PCS at late chronic stage Trial Registration ClinicalTrials gov NCT00715052 Citation Boussi Gross R Golan H Fishlev G Bechor Y Volkov O et al 2013 Hyperbaric Oxygen Therapy Can Improve Post Concussion Syndrome Years after Mild Traumatic Brain Injury Randomized Prospective Trial PLoS ONE 8 11 e79995 doi 10 1371 journal pone 0079995 Editor Jinglu Ai St Michael s Hospital University of Toronto Canada Received August 22 2013 Accepted October 4 2013 Published November 15 2013 Copyright 2013 Boussi Gross et al This is an open access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use distribution and reproduction in any medium provided the original author and source are credited Funding The study was supported by the research fund of Assaf Harofeh medical center by the Tauber Family Foundation and by the Maguy Glass Chair in Physics of Complex Systems at Tel Aviv University None of the supporting bodies had any role in study design data collection and analysis decision to publish or preparation of the manuscript Competing Interests The authors have declared that no competing interests exist E mail efratishai 013 net SE eshel rice edu EB J These authors contributed equally to this work dysfunction Intensive therapy and rehabilitation programs are considered essential for maximizing quality of life but are often just partially successful Clearly new methods for brain repair should be examined in order to provide sustained relief to brain damage patients Recent studies reported that hyperbaric oxygen treatment HBOT can induce neuroplasticity leading to significant neurological improvement in post stroke patients at the convalescent stage and at late chronic stages months to years after the acute event 3 4 Introduction Traumatic brain injury TBI and stroke are the major causes of brain damage Every year close to two million people in the US suffer TBI which is the leading cause of death and disability among the general population Stroke affects almost a million people and is the leading cause of inability to maintain independent life among adults 1 2 There is no effective treatment metabolic intervention in the daily clinical practice for post TBI and stroke patients with chronic neurological PLOS ONE www plosone org 1 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI function in animal models 26 27 28 29 30 The elevated oxygen levels can have a significant effect on the brain metabolism largely regulated by the glial cells see discussion Improved energy management leads to multifaceted repair including activation of angiogenesis and triggering of neuroplasticity reactivation of quiescent neurons creation of new synapses and new axonal connections and might even induce differentiation of neuronal stem cells 22 The idea that HBOT can promote brain repair is reasonable and has gained experimental support yet is still largely dismissed by the medical community as is discussed next Definitions and classifications Traumatic brain injury is defined as damage to the brain resulting from external mechanical force such as rapid acceleration or deceleration impact blast waves or penetration by a projectile Consequently to the injury brain function is temporarily or permanently impaired and structural damage may or may not be detectable with current imaging technology TBI is usually classified based on severity anatomical features of the injury and the cause of the injury The severity is assessed according to the loss of consciousness LOC duration the post traumatic amnesia PTA and the Glasgow coma scale GCS grading of the level of consciousness Approximately 70 90 of the TBI in the US are classified as mild TBI mTBI or concussion LOC duration of 0 30 minutes PTA duration of less than a day and GCS grade of 13 15 Post concussion syndrome PCS is a set of symptoms succeeding mTBI in most patients The PCS symptoms include headache dizziness neuropsychiatric symptoms and cognitive impairments 5 6 In most patients PCS may continue for weeks or months and up to 25 of the patients may experience prolonged PCS PPCS in which the symptoms last for over six months 7 8 9 10 11 12 Such individuals are at high risk for emotional and cognitive dysfunction culminating in inability to carry out ordinary daily activities work responsibilities and standard social relationships 9 10 11 12 The medical community reservations A study of the effect of hyperbaric oxygen treatment of severe brain injured patients has been published already two decades ago Several prospective clinical trials on treatment of mTBI have been published in the last decade 31 32 33 and three studies published in the last two years addressed the effect of HBOT on chronic mild TBI patients 34 35 36 However the reported beneficial effects of the hyperbaric treatment were severely questioned by the medical community and triggered high skepticisms to the extent that TBI and stroke patients in the US are rarely treated by hyperbaric oxygen The HBOT option has been dismissed by the medical community on the grounds of 1 Lack of knowledge about the connection between metabolism and neuroplasticity 2 Lack of randomized clinical trial with standard placebo control 3 Sham control with room air at 1 3Atm yielded significant improvements These issues are clarified and elaborated on in the discussion section Associated brain pathology and function impairments Diffuse axonal injury diffuse shearing of axonal pathways and small blood vessels is one of the most common pathological feature associated with mTBI 13 Another primary pathological feature usually caused by a direct hit to the skull is brain contusions which commonly involve the frontal and anterior temporal lobes 12 Secondary pathologies of mTBI include ischemia mild edema and other bio chemical and inflammatory processes culminating in impaired regenerative healing processes resulted from increasing tissue hypoxia 14 Due to the diffuse nature of injury cognitive impairments are usually the predominant symptoms involving deficiencies in several cognitive functions primarily memory attention processing speed and executive functions all localized in multiple brain areas Their potent functions rely on potent network structure and connectivity between different brain areas 12 15 16 We note that the diffuse nature of the mTBI injury renders the pathological damage hard to be detected by common neuroimaging methods such as CT and MRI so that diagnosis largely relies on subjective reports of the patients as well as cognitive and quality of life tests While diffusion tensor imaging DTI has the potential to detect diffuse axonal injuries this method is still not commonly used for diagnosis of mTBI pathology The placebo dilemma People can sense a pressure increase beyond 1 3Atm hence standard placebo with normal air pressure for HBOT could perhaps be attained by exposing the patients to normal pressure combined with falsifying stimulation e g by increasing and decreasing the pressure which generates a fictitious pressure sensation Since breathing normal air under hyperbaric conditions leads to elevated tissue oxygen e g about 50 for 1 3Atm standard placebo could also be attained by giving the patients compressed air with sub normal oxygen concentration In the discussion section we explain that the first approach can be effective only for some patients and poses logistic difficulties and the second approach involves ethical issues In an attempt to evade the placebo dilemma a recent study of HBOT for mTBI compared the effect of 100 oxygen at 2 4Atm with the effect of room air at 1 3Atm as sham control 36 The study found significant improvements in both groups and with slightly higher efficacy at 1 3Atm Based on these results the authors resented a sweeping conclusion that their study shows that HBOT has no effect on post mTBI brain damage and the observed improvements resulted from placebo associated with spending time in the hyperbaric chamber As is discussed in great details in the discussion section we reason that the authors reached wrong conclusions for two main reasons First room air at 1 3Atm cannot serve as a proper sham control since it is not an ineffectual treatment as is required from placebo since it leads to a significant increase in the level of tissue oxygenation which has been shown to be effective 37 38 Second 100 oxygen at 2 4Atm leads to too high oxygen levels which can cause inhibitory effect or even focal toxicity Rationale for hyperbaric oxygen treatment HBOT The brain receives 15 of the cardiac output consumes 20 of the total body oxygen and utilizes 25 of the total body glucose Still this energy supply is only sufficient to keep about five to ten percent of the neurons active at any given time Thus at standard healthy condition at any given time the brain is utilizing almost all oxygen energy delivered to it The regeneration process after brain injury requires much additional energy This is where hyperbaric oxygen treatment can help the increased oxygen level in the blood and body tissues during treatment 17 18 19 can supply the energy needed for brain repair Indeed several previous studies have demonstrated that elevated levels of dissolved oxygen by HBOT can have several reparative effects on damaged brain tissues 3 19 20 21 22 23 24 25 Other studies revealed the beneficial effect of HBOT on the injured brain and cognitive PLOS ONE www plosone org The crossover approach To overcome the placebo issue a randomized crossover approach was successfully used to test the effect of HBOT in post stroke patients at late chronic stage 3 The advantage of the 2 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI crossover approach is the triple comparison between treatments of two groups between treatment and no treatment of the same group and between treatment and no treatment in different groups Up till now a similar prospective randomized crossover trial to evaluate the brain repair effect of HBOT in mTBI patients at late chronic stage has not been done The aim of our current study was to provide firm evaluation of the HBOT effects on brain activity and cognitive impairments in mTBI patients with prolonged PCS at late chronic stage Evaluation of cognitive state Cognitive Indices The state of the patients cognitive functions was assessed in terms of the following four cognitive indices ordered from the index associated with most fundamental basic functions to that associated with the higher functions 1 Information Processing Speed IPS index This index is associated with the basic ability to process and respond to stimuli at different levels of speed and complexity 2 Attention related index This index is associated primarily with the ability to remain concentrated and respond effectively throughout relatively extended periods of time 3 Memory related index This index is associated with the learning of verbal and visual new stimuli and the immediate and delayed recognition of these learned stimuli 4 Executive Functions EF index This index is associated with cognitive abilities involved in the initiation planning organization and regulation of behavior Each of above cognitive indices was computed as a normalized combined score of 2 3 cognitive tests from the Mindstreams Computerized Cognitive Test Battery Mindstreams NeuroTrax Corp NY Cognitive tests The Mindstreams battery includes several cognitive tests devised to check various aspects of brain capabilities In the current study we evaluated the cognitive indices based on the scores of the 6 cognitive tests listed below which are expected to be relevant for mild TBI For detailed description of all cognitive tests in Mindstreams battery see 39 The tests are 1 Verbal memory Ten pairs of words are presented followed by a recognition test in which the first word of a previously presented pair appears together with a list of four words from which the patients choose the other member of the pair There are four immediate repetitions and one delayed repetition after 10 min 2 Non verbal memory Eight pictures of simple geometric objects are presented followed by a recognition test in which four versions of each object are presented each oriented in a different direction There are four immediate repetitions and one delayed repetition after 10 min 3 Go No Go test In this continuous performance test a colored square red green white or blue appears randomly on the center of the screen The patient in then asked to respond quickly only for red squares by pressing the mouse button and inhibit his reaction to any other colored square 4 Stroop test Timed test of response inhibition modified from the Stroop paper based test In the first phase patients choose a colored square matching the color of a general word for example the word Cat appears in red letters the patient must choose the red square out of two colored squares in the following screen In the next phase termed the Choice Reaction Time test the task is to choose the colored square matching the name of the color presented in white letter color In the final Stroop interference phase patients are asked to choose the colored square matching the color and not the meaning of a former colornaming word presented in an incongruent color for example the word RED appears in green letters the patient is asked to choose the color green and not red a task requiring the ability to inhibit an automatic response to the meaning of the word 5 Staged information processing test Timed test requiring a reaction based on solving simple arithmetic problems pressing right left mouse button if the answer higher lower than 4 respectively with three levels of information processing load single digit two digits addition subtraction and three digits addition subtraction problems each containing three speed levels 3 2 and 1 second for the presentation of the stimuli Methods The study was performed as a prospective randomized controlled two group trial The study was conducted in the hyperbaric institute and the research unit of Assaf Harofeh Medical Center Israel Enrolment of patients started at 2008 and ended at 2012 All patients signed written informed consent The protocol was approved by Assaf Harofeh institutional review board Participants Inclusion The participants were patients of age 18 years or older who suffered mild TBI less than 30 minutes loss of consciousness 1 6 years prior to their inclusion All patients experienced post concussion syndrome PCS and complained of impaired cognitive functions for over a year yet brain damage was below the detection level of MRI or CT brain imaging Only patients who reported no change in cognitive function during one month prior to the beginning of the study were included Exclusions Exclusions were due to chest pathology incompatible with HBOT inner ear disease claustrophobia and inability to sign informed consent Smoking was not allowed during the study Protocol and End Points After signing an informed consent form the patients were invited for baseline evaluation Included patients were randomized into two groups 1 1 randomization a treated group and a crossover group The neuropsychological functions evaluated by Mindstreams testing battery and brain activity as visualized by SPECT Single photon emission computed tomography were the primary endpoints of the study Secondary end point included quality of life evaluation by the EQ 5D questionnaire Evaluations were made by medical and neuropsychological practitioners who were blinded to patients inclusion in the control crossed or the treated groups Patients in the treated group were evaluated twice at baseline and after 2 months of HBOT Patients in the crossover group were evaluated three times baseline after 2 months control period of no treatment and after subsequent 2 months of HBOT Figure 1 The post HBOT neurological evaluations as well as the SPECT scans were performed more than 1 week 1 3 weeks after the end of the HBOT protocol The following HBOT protocol was practiced 40 daily sessions 5 days week 60 minutes each 100 oxygen at 1 5ATA Patients were not involved in any other cognitive or rehabilitation intervention as part of the study protocol The detailed clinical study protocol copy of the informed consent as well as CONSORT 2010 checklist of information are attached as supporting information Protocol S1 Form S1 Checklist S1 We note that information regarding sample size detectable change and power calculation parameters is included and addressed in the statistical considerations section in the SI1 PLOS ONE www plosone org 3 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 1 Flow chart of the patients in the study doi 10 1371 journal pone 0079995 g001 6 Catch game A test of motor planning that requires participants to catch a falling object on a computer screen by moving a paddle horizontally so that it can catch the falling object To assign scores Mindstreams data was uploaded to the NeuroTrax central server Outcome parameters were calculated using custom software blind to diagnosis or testing site To minimize differences related to age and education each outcome parameter was normalized and fit to an IQ like scale mean 100 STD 15 according to patient s age and education We note that the score evaluation was based on normative data from cognitively healthy individuals collected in controlled research studies that were part of more than 10 clinical sites 40 The cognitive indices scores The computation of the cognitive indices based on the scores of the cognitive tests was done as follows 1 Information Processing Speed index was computed as the combined score for the low and medium load stages of the staged information processing test 2 Attention index was calculated as the mean score of reaction time for Go No Go test and choice reaction time of the Stroop test at second phase mean STD of reaction time for Go No Go test mean reaction time for a low load stage of staged information processing test and mean accuracy for a medium load stage of information processing test 3 Memory index was computed as the mean score for total learning score after four repetitions and delayed recognition phase of verbal and non verbal memory tests 4 Executive PLOS ONE www plosone org Functions index was computed based on the scores of the Stroop test and the Go No Go test and the mean weighted accuracy for catch game For more information regarding the validity of the tests and the construction of the cognitive indices see 41 42 5 In addition we defined the individual s General Cognitive Score as the average of the scores of the four cognitive indices for each individual It is important to note that the above cognitive index scores were specifically designed to represent known impaired cognitive domains in mild TBI In addition the fact that each index is referred to more than one test score ensures the index to be associated more with a cognitive domain score and less with a testdependent score We also utilized a computerized testing battery which supports the inclusion of more accurate measures such as reaction time and elimination of the bias effect of tests administration and hand scoring An important aspect of the tests is the inclusion of the cognitive domain of information processing speed known to be impaired in mild TBI patients Quality of life evaluation Quality of life QOL was evaluated by the EQ 5D questionnaire 43 EQ 5D essentially consists of 2 pages the EQ 5D descriptive system and the EQ visual analogue scale EQ VAS The EQ 5D descriptive system covers mobility self care usual activities pain discomfort and anxiety depression The EQ VAS 4 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI records the respondent s self rated health on a vertical visual analogue scale range 0 worst 100 best Results Participants Profiles The study included 90 screened patients aged 18 years or older who signed an informed consent Pre study exclusions Nineteen patients had their consent withdrawn before the beginning of the control treatment period 13 in the crossover group 6 in the treated group In study exclusions Four patients decided to drop out during the treatment protocol 3 due to personal reasons and 1 due to ear problem 1 in crossover group 3 in treatment group Seven patients 5 in crossover group 2 in treatment group were excluded due to technical performance problems in their cognitive tests and 4 patients due to inconsistent use of medications such us methylphenidate during the tests period 2 in crossover group 2 in treated group Accordingly 56 patients 32 in the treated group and 24 in crossover group were included in the final analysis Figure 1 Thirty two 57 patients were females the mean age was 44 years range of 21 66 years and the time elapsed since the acute traumatic event ranged from 1 6 years with 33 months average The most frequent etiology of the TBI was a vehicle accident n 38 with some other less common etiologies falls 7 object hit 6 pedestrian accident 3 assault 2 Baseline patients characteristics are summarized in Table 1 As seen from this table there was no significant difference in the included measures between the groups except for years of education where there was a minor advantage for the treated group Brain Functional Imaging SPECT Brain single photon emission computed tomography SPECT was conducted with 925 1 110 MBq 25 30 mCi of technetium99m methyl cysteinate dimmer Tc 99m ECD at 40 60 min post injection using a dual detector gamma camera ECAM or Symbia T Siemens Medical Systems equipped with high resolution collimators Data was acquired in 3 degree steps and reconstructed iteratively with Chang method m 0 12 cm attenuation correction 44 Visual analysis was conducted by fusing pre and post treatment studies that were normalized to cerebellum brain activity SPECT images were reoriented into Talairach space using NeuroGam Segami Corporation for identification based on visual inspection of Brodmann cortical areas and in order to compute the mean perfusion in each Brodmann area BA In addition volume rendered brain perfusion images normalized to cerebellum maximal activity were reconstructed All SPECT analysis was done while blinded to the laboratory and clinical data Change in perfusion in all Brodmann areas for each subject was determined by calculating the percentage difference between post period and pre baseline period divided by the pre baseline period perfusion An average of these perfusion changes for each Brodmann area was calculated Statistical analysis The statistical analysis was done using SPSS software version 16 0 Continuous data is expressed as means 6 standard deviations and compared by one tailed paired t test for intragroup comparisons and two tailed unpaired t test for inter group comparisons Effect sizes for main comparisons were calculated using Cohen s d Categorical data is expressed in numbers and percentages and compared by x2 test P values 0 05 were considered statistically significant All randomly allocated patients were included in the safety analysis and those with complete postbaseline assessment were included in efficacy analysis The Effect on Cognitive Functions Changes in cognitive indices The effect of the hyperbaric oxygen treatment on the patients cognitive functions as assessed by the four cognitive indices is summarized in Figure 2 and Table 2 The baseline mean cognitive scores of all four indices were close in the two groups within the standard error but with somewhat higher values in the treated group The HBOT treatments of both groups led to statistically significant improvements in the mean scores of all four indices As is apparent in Figure 2 and detailed in Table 2 a significant improvement was observed in the treated group after HBOT in all cognitive measures Information Processing Speed t 31 4 20 p 0 0001 Attention t 31 3 26 p 0 005 Memory t 31 4 13 p 0 0005 and Executive Functions t 31 3 72 p 0 0005 Effect sizes were medium to large the Cohen s d measures 45 were 0 74 0 57 0 73 and 0 66 respectively No significant improvement was noticed in the crossover group during the control period Information Processing Speed t 23 0 53 p 0 298 Attention t 23 0 33 p 0 368 Memory t 23 0 74 p 0 233 and Executive Functions t 23 0 54 p 0 295 However a significant improvement following HBOT was noticed in the crossover group as well Information Processing Speed t 23 1 98 p 0 05 Attention t 23 2 29 p 0 05 Memory t 23 3 21 p 0 005 and Executive Functions t 23 2 26 p 0 05 Effect sizes were medium to large with Cohen s d measures of 0 40 0 47 0 65 and 0 46 respectively Note that t 31 and t 23 correspond to N 1 where N 32 and N 24 are the number of patients in the treated and crossover group respectively Assessment of a general cognitive score The changes in the four cognitive indices presented in Figure 2 and in Table 2 show noticeable variability For example the mean values of the Information Processing Speed and Executive Functions indices decreased during the control period of the crossover group while the corresponding mean values of the Attention and Memory Scatter plot analysis of the clinical scores The analysis aims to better quantify and compare changes in the clinical scores while taking into consideration the high patient topatient variability following Efrati et al 3 The idea was to inspect for each patient at each time stage the scaled relative differences in each of the clinical scores More specifically we calculated for a specific patient j the scaled relative difference SRDj defined as STD SFj SRDj SFj vSFj w SIj vSIj w STD SIj z vSFj SIj w 1 Where SFj is the value of a clinical score at the end of the time stage either treatment or control and SIj is the score at the beginning of the time stage We note that the symbol indicates average over the values of the patients in the group For example SFj means the average of SFj over all patients j that belong to the group The abbreviation STD means the standard deviation between the values of the patients in the group This analysis enables quantitative inspection of the changes in the clinical scores as is further explained in 3 PLOS ONE www plosone org 5 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Table 1 Baseline patients characteristics Treated group n 32 Crossover group n 24 Comparison Age years 42 5612 6 45 7610 9 p 0 32 Gender male 11 34 13 54 p 0 07 Years of education 16 263 9 14 063 1 p 0 05 Time since injury months 34 6616 7 31 7616 3 p 0 51 None 24 75 14 58 30 minutes 8 25 10 42 Loss of consciousness p 0 18 Etiology Vehicle accident 20 63 18 75 Fall 5 16 2 8 Object hit 4 12 2 8 Pedestrian accident 2 6 1 4 Assault 1 3 1 4 Hypertension HTN 5 15 4 16 Diabetes Mellitus DM 2 6 2 8 Hyperlipidemia 4 12 3 12 Ischemic Heart Disease 0 1 4 Epileptic seizure 0 0 Smoking 1 3 0 Aspirin 2 6 3 12 Glucose lowering drugs 2 6 1 4 Anti HTN 4 12 3 12 Background disease Medications Statins 3 9 3 12 Anti depressant 7 22 4 16 doi 10 1371 journal pone 0079995 t001 indices increased Figure 3 shows the mean values of the individual general cognitive scores with standard error for the treated and crossover groups at each evaluation stage baseline and postHBOT for both groups and after the control for the crossover group It can be seen that the cross group had the same general score at baseline and after the control period This value seems higher than the score of the treated group at baseline 88 vs 85 and the post HBOT general cognitive score of the treated group seems higher than that of the crossover group 96 vs 94 While these differences are within the standard error they still give rise to what appears to be significant differences in the level of changes post vs pre HBOT between the crossover and the treated groups 6 points for the crossover group vs 11 for the treated group Examining the relative changes There is a high patient topatient variability in the cognitive indices with scores ranging from 20 to 120 The magnitude of the change in a cognitive score has different implications for patients at low or high base levels Hence we inspect the effect of the HBOT on the relative changes i e the change relative to the base value We calculated for each person the relative change in each of the cognitive indices for each period control and HBOT for the crossover group and HBOT for the treated group In Figure 4A we show the mean relative changes in all four cognitive indices for the crossover group following the control period and following HBOT and for the treated group following HBOT In Figure 4B we show the mean PLOS ONE www plosone org relative changes in the general cognitive score for the same three periods We note that calculating the mean of the relative changes is more informative than calculating the changes in the mean values especially for small groups with high patient to patient variability Looking at the relative changes elucidates the improvements after the HBOT period vs the control period of the crossover group However it also amplifies the differences mentioned earlier between the crossover and treated groups the bigger relative changes in the treated group vs the crossover group reflect the fact that the baseline values of the treated group were lower and the post HBOT values were higher in comparison to the corresponding values of the crossover group Scatter plot analysis of the cognitive indices As mentioned in the methods section the analysis aims to present the mean relative changes in cognitive indices while superimposing information regarding the patient to patient variability For that we calculated for each patient i the normalized relative change NRC i Next we calculated for each group control and HBOT in the crossover group and HBOT in the treated group the locations of the mean departures from baseline Finally we marked the location of each patient i at a distance NRC i from the location of his her group s mean difference see methods section for details Typical results are shown in Figure 5 More specifically we show the scatter plots for Information Processing Speed vs Executive Functions Figure 5A for Attention vs Memory 6 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 2 Assessment of the cognitive indices Each patient in each group was assigned a score at baseline after the control period for patients in the crossover group and after HBOT The figures show the mean scores and standard errors for the two groups at each stage for the four cognitive indices Information Processing Speed A Attention B Memory C and Executive Functions D as defined in the method section doi 10 1371 journal pone 0079995 g002 Attention EF Interestingly the scattering of the individual patients also follows the linear line for the scatter plots of the specific cognitive indices as function of the general cognitive score Figures 5C and 5D These linear dependences demonstrate high consistency between the changes of the different cognitive indices for each patient As such the analysis provides valuable test for the validity of the test performances and the validity of the general cognitive score Figure 5B for Attention vs General cognitive score Figure 5C and for IPS vs General cognitive score Figure 5D The results illustrate the differences between the three cases control and HBOT for the crossover group and HBOT for the treated group which form three distinct clusters Also clear in all the figures is the linear dependence between the changes in the different cognitive indices similar results are also obtained for the other combinations e g Memory IPS Attention IPS Memory EF and Table 2 Summary of results for Mindstreams cognitive indices scores Treated group n 32 Baseline HBOT Crossover group n 24 P1 P2 Baseline Control Pre HBOT Post HBOT P2 P3 P4 Memory 82 43625 15 96 54617 18 0 567 0005 85 90617 80 88 36617 34 95 61615 54 0 233 0 005 0 835 Executive function 88 26614 74 96 96611 69 0 367 0 0005 91 73613 26 90 20615 77 95 13613 84 0 295 0 05 0 595 Attention 85 13620 28 95 30612 90 0 854 0 005 86 10618 42 87 05620 98 92 02618 95 0 368 0 05 0 443 Information processing speed 85 12615 88 95 04613 75 0 324 0 0001 89 74618 81 88 30619 68 92 47618 25 0 298 0 05 0 55 Abbreviations Values are presented as mean 6 STD P1 stands for the p values for baseline comparison of treated and crossover group P2 stands for the p values for comparison of the second measurement to baseline in the same group P3 stands for the p values for comparison of pre and post HBOT in the crossover group P4 stands for the p values for endpoint scores comparison following treatment in both groups The baseline mean cognitive scores of all four indices were close in the two groups with no significant difference The HBOT treatments of both groups led to statistically significant improvements in the mean scores of all four indices as oppose to no significant improvement after control period alone The tables are discussed in details in the results section doi 10 1371 journal pone 0079995 t002 PLOS ONE www plosone org 7 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 3 Assessments of the general cognitive score The figure shows the level of the general cognitive score defined in the text for the crossover group at baseline after the control period and after HBOT and for the treated group at baseline and after HBOT doi 10 1371 journal pone 0079995 g003 evaluation and evaluator the cognitive function tests were done by a computerized validated method and the SPECT analysis was blind to patients participation in treated crossover group Brain SPECT evaluations were completed for 31 patients in the treated group one patient from the treated group did not complete two SPECT scans and for 24 in the crossover group In supporting information Table S1 we present detailed statistics of the SPECT results for all Brodmann areas BA of all the tested patients The results revealed a significant increase in brain activity perfusion following the hyperbaric oxygen treatments in both groups compared to the change during the control period of the crossover group A summary of the results is presented in Figure 7 To construct the figure we calculated for each patient the relative change in the SPECT measured brain activity during each phase of the trial The relative change was defined as the difference in normalized activity relative to the cerebellum activity see SI4 between the end point and the start point divided by the activity at the start We calculated for each BA the average changes over all patients that underwent HBOT both treated and cross groups These results correspond to the red curve in Figure 7 The blue curve represents the results of similar calculations for the control period averaging for each BA over all the results of all patients in the crossover group during the control period The results revealed significant improvement in brain perfusion following HBOT in the frontal and temporal areas including inferior frontal gyrus BA 45 the middle frontal area BA 46 parts of the orbito frontal cortex BA 47 and 11 most of the temporal cortex BA 36 37 38 20 21 22 28 and parts of the Cingulate gyrus BA 24 25 These fronto temporal regions responsible for the cognitive functions are the most affected in The Effect on quality of life The effect on the QOL is summarized in Table 3 The EQ 5D score significantly improved following HBOT in the treated group t 31 7 41 p 0 0001 and in the crossover group after HBOT t 23 6 17 p 0 0001 As expected there was no improvement in the EQ 5D score in the crossover group following the control period During the control period we have noticed some reduction in this group with respect to the patients subjective perception of their quality of life t 23 2 60 p 0 01 Similar results were obtained for the EQ VAS evaluations as summarized in Table 3 More specifically the EQ VAS score significantly improved following HBOT both in the treated group t 31 4 86 p 0 0001 and in the crossover group following treatment t 23 4 79 p 0 0001 while there was no significant improvement following the control period t 23 0 32 p 0 373 Details are presented in Table 3 Examining the relative changes Figure 6 presents the mean relative changes and standard errors in both measurements of quality of life for the treated group following HBOT and for the crossover group after the control period and after HBOT SPECT assessments of brain activity Motivation Since mTBI involves a diffuse structural and or physiologic metabolic derangement 46 47 48 patients with mTBI have more frequent and more extensive areas of brain damage than can be seen by anatomical imaging conventional CT and MRI scans The preferred brain imaging methods are thus functional metabolic SPECT PET CT perfusion and functional MRI In order to achieve greater validity of the results cognitive function and SPECT analysis were done by a blinded PLOS ONE www plosone org 8 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 4 Assessment of the relative changes A The relative changes as defined in the text for the four cognitive indices The changes are shown for the crossover group following the control period green bars and HBOT blue bars and for the treated group following HBOT red bars B Relative changes in the general cognitive score for the same three cases as in A doi 10 1371 journal pone 0079995 g004 Example 2 SPECT analysis of a 46 year old woman from the treated group following mTBI as a result of a car accident 1 year prior to inclusion in the study The patient s main complaints were related to her memory and concentration capabilities as well as dizziness and tinnitus that interfered with her daily functioning Following HBOT the dizziness and tinnitus disappeared in addition to significant improvement in all cognitive domains The patient s cognitive indices demonstrated significant improvements following treatment increase of 1 5 STD in Memory 57 preHBOT to 78 post HBOT 1 STD increase in Attention 88 to 104 1 5 STD increase in Executive Functions 82 to 102 and 0 6 STD increase in Information Processing Speed 85 to 95 SPECT images of the patient at baseline and following HBOT are shown in Figure 9 The percentage of CBF change demonstrated significant improvements after HBOT in parts of the frontal and temporal lobes in agreement with the improvements in neurological functions Example 3 SPECT analysis of a 44 year old man from the cross group suffering from cognitive impairments due to mild TBI as a result of a fall 2 years prior to treatments The patient complained mainly on short and long term memory difficulties attention and concentration problems decline in naming abilities as well as headaches dizziness anxiety and sleep problems Following HBOT the patient experienced significant improvements in most aspects including concentration and memory headaches dizziness mood and sleep The patient s cognitive indices demonstrated significant improvements in Executive Functions after treatment baseline 60 after control 63 and postHBOT 74 SPECT images of the patient after the control period head trauma 12 The temporal lobe plays a significant role in memory and learning skills 49 50 51 the frontal lobe is associated with attention and executive functions 52 53 and the cingulate gyrus plays an important role in emotions and cognitive self regulation 54 55 56 The SPECT results of elevated activity in these Brodmann areas are consistent with the improvement in cognitive indices following HBOT Further below we show specific examples of SPECT results for four patients two from the treated group and two from the crossover group Representative examples Example 1 SPECT analysis of a 51 year old woman from the treated group Figure 8 The patient suffered from cognitive impairments due to mTBI as a result of a fall in a moving bus 2 years prior to inclusion in the study The patient experienced no loss of consciousness and CT imaging did not reveal anatomic damage The patient s main complaints included headaches dizziness memory and concentration problems and random mood swings The patient was a manager in a private business and since the injury was having difficulties following and completing daily activities and routine Following HBOT the patient reported significant improvement in every aspect of daily functioning The patient s cognitive indices demonstrated significant improvements following treatment increase of 3 5 STD in Memory 56 pre HBOT to 108 post HBOT 2 STD increase in Attention 47 to 81 1 5 STD increase in Executive Functions 65 to 85 and a 0 7 STD increase in Information Processing Speed 85 to 95 PLOS ONE www plosone org 9 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 5 Scatter plot analysis of the changes in cognitive indices The scatter plots show the normalized relative changes NRC as defined in the methods section and explained in the text above A Scatter plot for the changes in IPS as function of changes in EF B Scatter plot for changes in Attention as function of Memory The changes in the Attention and in the IPS as function of the General cognitive score are shown in C and D respectively Circles are for the treated group and diamonds are for the crossover group The color code is Red for changes during HBOT and blue for changes during control doi 10 1371 journal pone 0079995 g005 following treatment in comparison to the changes during the control period Executive Functions at baseline after control and post HBOT were 77 71 and 88 respectively and Attention scores were 62 64 and 78 respectively SPECT images of the patient after the control period and following HBOT are shown in Figure 11 At first global look the CBF changes after HBOT seem to be similar to the changes after the control period demonstrating no significant change However a closer inspection of the SPECT images reveal local improved perfusion in the right anterior temporal and right dorso lateral frontal areas This example is shown to demonstrate that even for patients with relatively mild cognitive improvements there is good correspondence between the change in the cognitive tests and the SPECT results and following HBOT are shown in Figure 10 The CBF change was not significant after the control period but substantial improvement after HBOT in most of bilateral frontal and temporal lobes and right parietal lobe Example 4 SPECT analysis of a 39 year old woman from the cross group suffering from cognitive impairments due to mild TBI as a result of a car hit as a pedestrian 2 years prior to treatments The patient s complaints included dizziness nausea fatigue and decrease in memory and concentration abilities The patient also had troubles in performing every day activities such as attaining the grocery store or reading the newspaper The patient was working as a nurse and could not continue to perform her work after the accident due to the impaired abilities The patient s cognitive indices demonstrated significant improvements Table 3 Summary of results of quality of life questionnaire EQ 5D and EQ VAS Treated group n 32 Baseline HBOT Crossover group n 24 P1 P2 Baseline Control Pre HBOT Post HBOT P2 P3 P4 EQ 5D 7 8761 36 6 4861 07 0 615 0 0001 7 7061 11 8 0661 05 6 7561 06 0 01 0 0001 0 362 EQ VAS 5 0362 31 6 6262 45 0 696 0 0001 5 2661 70 5 2161 66 6 3961 80 0 373 0 0001 0 696 Abbreviations Values are presented as mean 6 STD P1 stands for the p values for baseline comparison of treated and crossover group P2 stands for the p values for comparison of the second measurement to baseline in the same group P3 stands for the p values for comparison of pre and post HBOT in the crossover group P4 stands for the p values for endpoint scores comparison following treatment in both groups EQ 5D as well as the EQ VAS scores significantly improved following HBOT both in the treated group and in the crossover group following treatment while there was no significant improvement following the control period doi 10 1371 journal pone 0079995 t003 PLOS ONE www plosone org 10 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 6 Assessments of the mean relative changes and standard errors in quality of life measurements The changes are shown for the crossover group following control period green bars and following HBOT blue bars and for the treated group following HBOT red bars Note that according to the questionnaire structure in the EQ 5D measurement improvement is reflected as score decrease hence the negative values of change doi 10 1371 journal pone 0079995 g006 3 imply that increasing the plasma oxygen concentration with hyperbaric oxygenation is a potent means of delivering to the brain sufficient oxygen for tissue repair HBOT might initiate a cellular and vascular repair mechanism and improve cerebral vascular flow 34 58 59 60 More specifically HBOT induces regeneration of axonal white matter 61 62 63 64 has positive effect upon the myelinization and maturation of injured neural fibers 65 and can stimulate axonal growth and increase the ability of neurons to function and communicate with each other 66 In addition HBOT was found to have a role in initiation and or facilitation of angiogenesis and cell proliferation processes needed for axonal regeneration 67 At the cellular level HBOT can improve cellular metabolism reduce apoptosis alleviate oxidative stress and increase levels of neurotrophins and nitric oxide through enhancement of mitochondrial function in both neurons and glial cells Moreover the effects of HBOT on neurons can be mediated indirectly by glial cells including astrocytes 23 HBOT may promote the neurogenesis of endogenous neural stem cells 24 With regard to secondary injury mechanisms in mTBI HBOT can initiate vascular repair mechanism and improve cerebral vascular flow 58 59 68 69 promote blood brain barrier integrity and reduce inflammatory reactions 28 as well as brain edema 20 21 22 26 34 70 A drawback to the above mentioned findings is that the different effects have been tested at different experimental setups and while utilizing different protocols of HBOT However it is well noticed that there is at least one common denominator to all repair regeneration mechanisms Discussion We presented a prospective randomized and controlled cross over study of the effect of HBOT with 100 oxygen at 1 5Atm on mTBI patients at late chronic stage The results clearly demonstrate that HBOT can induce neuroplasticity and significant brain function improvement in mild TBI patients with prolonged PostConcussion Syndrome at late chronic stage years after brain injury Additional statistical validation using simulated randomizations is available as supporting information Text S1 Linking elevated oxygen metabolism and brain activity to neuroplasticity The changes in SPECT images after treatment indicate that HBOT led to reactivation of neuronal activity in stunned areas that seemed normal under CT and MRI imaging While SPECT imaging has a limited spatial resolution compared for example to fMRI the changes in activity were sufficiently robust to be clearly detected by the SPECT images Recently Kan et al 57 discussed the need for potent interventions such as elevated tissue oxygen capable of repairing microenvironment alterations after mTBI e g impairments in vascular changes in cerebral blood flow and in perfusion leading to reduced oxygen availability followed by reduced metabolism which in turn leads to reduced neuronal activity loss of synapses and tampered neuronal connectivity The observed reactivation of neuronal activity in the stunned areas found here along with similar results in post stroke patients PLOS ONE www plosone org 11 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 7 Distribution of the Brodmann areas relative SPECT CBF changes The change for each BA represents and averaging of the relative changes of all the patients as explained in the text The results show a clear difference between the control and the HBOT periods We note that the higher variations for the control period are associated with the fact that the averaging in this case is over 24 patients the crossover group while for the HBOT period the averaging is over all 55 patients doi 10 1371 journal pone 0079995 g007 mainly to the cognitive dysfunction following the injury are commonly based on behavioral compensation methods such as attention training drills teaching memory planning strategies and usage of external aids 16 76 and have limited patient specific success in repair of mTBI impaired brain function 77 Therefore studies at the late chronic stage allow assessment of the power of the HBOT approach to achieve brain function improvements in addition to rather than instead of the standard rehabilitation programs they are all energy oxygen dependent It might be possible that HBOT enables the metabolic change simply by supplying the missing energy oxygen needed for those regeneration processes Rationale for testing the HBOT effect on patients at late chronic stage As stated in the introduction the crossover approach is adopted in order to avoid the inherent difficulties associated with randomized HBOT trial while practicing standard placebo see Text S1 The placebo dilemma and the rationale for a crossover approach are further discussed below following the rationale to selecting patients at late chronic stage First as explained in 3 applying hyperbaric oxygen in the acute or early phase after brain injury makes it almost impossible to signify and assess the HBOT effects vs the effects of the spontaneous natural repair mechanism that are effective at this stage Moreover in some patients the elevated oxygen can inhibit natural regeneration or even cause toxicity In 3 it was proposed that this might explain the contradictive results in studies using HBOT at early stage after stroke 71 72 73 74 75 One can assume that any added energy during the degenerative stage immediately after brain injury could further increase the unwanted post injury damage On the other hand elevated oxygen supply during the regenerative stage would supply the energy needs for the innate brain repair processes Second as also explained in 3 patients at the chronic late stage demonstrate neurological stability with low probability of spontaneous changes unrelated to treatment Third typically patients at this stage years after injury have already gone through rehabilitation programs These programs which attempt to attend PLOS ONE www plosone org The placebo dilemma and debate There are inherent ethical and logistic difficulties in handling the sham control in HBOT trial according to the standard placebo definition Medically ineffectual treatment for medical conditions intended to deceive the recipient from knowing which treatment is given First the minimal pressure for the patients to sense pressure increase is 1 3Atm Second breathing regular air under hyperbaric conditions of 1 3Atm leads to more than 50 elevation in tissue oxygenation There are many case reports illustrating significant effects due to small increases in air pressure including effects on the brain 38 78 79 80 Moreover even a slight increase in partial pressure such as to 1 05 ATM at altitude 402 m below sea level the Dead Sea can lead to noticeable physiological effects 81 82 83 84 85 Since 50 elevation in tissue oxygen can have significant physiological effects treatment with room air at 1 3Atm is not an ineffectual treatment as is required from a proper sham control Yet a recent randomized controlled trial on mTBI patients by Wolf et al 36 used room air at 1 3Atm as sham control for treatment with 100 oxygen at 2 4Atm Both groups 12 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 8 Volume rendered Brain SPECT perfusion maps of Example 1 a 51 year old woman from the treated group suffering mTBI that had occurred 2 years prior to inclusion in the study Comparison of the baseline activity upper row with the post HBOT activity middle row and the CBF changes bottom row demonstrated significant improvements after HBOT in bilateral orbito frontal and lateral parietal regions and left ventro lateral frontal region correlating to BAs 45 47 and 11 doi 10 1371 journal pone 0079995 g008 test this issue by evaluating the specific dose response in post mTBI patients A potential way to comply with standard placebo could be to expose the patients to normal pressure combined with falsifying stimulations e g by increasing and decreasing the pressure which generates a fictitious pressure sensation This approach poses non trivial logistic difficulties Some patients especially in long term repeated treatments can detect pressure fluctuations Another potential way to avoid the increase in tissue oxygen at 1 3Atm in order to attain a standard placebo is to let the patients breath air with lower than normal oxygen level Obviously this is an unsuitable approach as it involves ethical issues and leaves an open question with regards to the pressure effect Nevertheless Cifu et al 35 conducted a randomized blinded clinical study in which 2 0 ATA with 10 5 oxygen was used as the sham control More specifically the patients were at 2 0 ATA but were randomly assigned to one of three groups breathing either 10 5 75 or 100 oxygen to mimic normal air at 1 0 ATA 100 air at 1 5 ATA and 100 air at 2 0 ATA respectively The authors concluded that This study demonstrated that HBO2 at either 1 5 or 2 0 ATA equivalent had no effect on post concussion symptoms after mild traumatic brain injury when compared with sham revealed significant improvements in cognitive symptoms and in the measure of post traumatic stress disorder PTSD We find these results very important they actually demonstrate that the significantly less expensive and logistically simpler treatment of mTBI patients with mild HBNO2 mild hyperbaric pressure of 1 3Atm and regular air can lead to meaningful improvements Our interpretation is based on previous studies demonstrating that mild HBNO2 conditions can be effectual treatment The authors of that study presented a very different interpretation Overlooking the fact that mild HBNO2 can be an effectual treatment they regarded it as sham control and concluded that the observed improvements must be due to placebo and that HBOT has no therapeutic effect on mTBI patients In other words they implicitly assumed that bringing the patients many times to spend long duration in the hyperbaric chamber can trigger such a powerful placebo effect that it can lead to a significant repair of chronic brain damage due to mTBI Remembering that for mTBI patients with intact macro vascular bed breathing 100 oxygen at 2 4ATA generate very high oxygen levels in tissues which can cause an inhibitory effect or even focal toxicity it is conceivable that HBOT using 2 4 ATA can be less effective than 1 3 ATA or other lower levels of pressure 86 Future studies are needed to PLOS ONE www plosone org 13 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 9 Volume rendered Brain SPECT perfusion maps of Example 2 The results are of a patient in the treated group suffering mTBI that had occurred 1 year prior to inclusion in the study Comparison of the baseline activity upper row with the post HBOT activity middle row and the CBF changes bottom row demonstrated significant improvements after HBOT in bilateral orbito frontal regions the medial aspect of the temporal lobes and the temporal poles that correspond to BAs 11 25 27 28 and 38 doi 10 1371 journal pone 0079995 g009 crossover approach involves two groups a treated group in which the patients went through two months of 40 HBOT sessions and a crossover group in which the patients first went through two month of no treatment followed by two months of HBOT sessions The advantage of the crossover approach is the triple comparison between treatments of two groups between treatment and no treatment of the same group and between treatment and no treatment in different groups see Text S1 For both groups the HBOT sessions induced statistically significant improvement in cognitive functions according to four cognitive indices Information Processing Speed Attention Memory and Executive functions in brain activity according to SPECT imaging and in quality of life according to the EQ 5D and the EQ VAS scores compared to the control period of the crossover group To gain better validity of the results we used the scatter plot analysis of the changes of the cognitive indices in terms of the corresponding scaled relative changes The scatter plots figure 5 show correlations in the improvements of the different indices both for the group means and the individual patients The good correspondence between the improvements in the cognitive indices the quality of life scores and the elevated brain activity as revealed by the SPECT imaging which was done in a compression Unfortunately the HBOT effect in this study was assessed merely based on the self administered Rivermead PostConcussion Symptoms Questionnaire RPQ which is known to display several flaws in implementation and in its ability to accurately reflect test taker experience Moreover interpretation and accuracy of the RPQ can vary widely due to selfadministration and the various confounding variables involved 87 Put aside this weakness the study suffers from a logical flaw The authors mention that their study was motivated by the results of Wolf et al 36 and they accepted the interpretation that any observed improvements should be a reflection of placebo effect and have nothing to do with the HBOT If indeed placebo can be so powerful in mTBI patients one would expect that stress related to the idea of breathing half the normal level of air may trigger powerful negative placebo effect Rationale for the crossover approach In the current study we tested the effect of 1 5 ATA using the crossover approach As stated in the introduction the approach is adopted in order to avoid the inherent difficulties associated with conducting HBOT trial while practicing standard placebo The PLOS ONE www plosone org 14 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 10 Volume rendered Brain SPECT images representing the percentage of CBF change post control period and post HBOT of the cross group patient described in example 3 As can be clearly seen the improvement in perfusion following HBOT was significantly high in most areas of the brain as opposed to insignificant change following the control period The most significant improvements were in both frontal and temporal lobes and right parietal lobe doi 10 1371 journal pone 0079995 g010 how to optimize patient specific protocol is important subject for future research In conclusion this study provides for the first time convincing results based on a crossover study demonstrating that HBOT can induce neuroplasticity and significant brain function improvements in mild TBI patients with prolonged Post Concussion Syndrome at late chronic stage years after injury The results call for better understanding of how to set the optimal HBOT protocol for the specific patients and how to determine which patients benefit the most from this treatment The findings reported here bear the promises that HBOT can be effective in treating other brain impairments like easing PTSD symptoms or repairing radiation damage It is also reasonable to expect that HBOT can help slow down or even reverse metabolic disorders associated neurodegenerative diseases completely blinded fashion further substantiates the clinical findings Implications Combined with previous studies of the HBOT effects on TBI and CVA patients the results presented here show that treatment with hyperbaric oxygen can significantly repair the chronically impaired brain functions and dramatically improve the quality of life of these patients Yet HBOT did not become a common acceptable treatment for TBI and CVA largely because of the debate regarding the placebo issue and the optimal time for administration Additional larger scale clinical studies are required to asses if and to what extent placebo effects might be operative However since the improvements are significant with no significant side effects it seems reasonable to let patients benefit from HBOT now rather than wait until future studies are completed We foresee that the future oxygen pressure dose response studies described in the discussion section will have significant therapeutic implications In particular we expect that HBOT treatment with room air at 1 3ATA will have significant brain repair effects and its effect should be compared with the 1 5ATA protocol used in this study In the current study the HBOT effects were assessed shortly after treatment ended Future follow up studies are needed in order to investigate the durability of the effect It might be that some patients will need more than 40 HBOT sessions The issue of PLOS ONE www plosone org Supporting Information Table S1 SPECT based measurements of changes in brain activity This SI includes data regarding the SPECT imaging for all the patients Table S1 1 S1 3 The data was normalized according to Cerebellum activity and the relative change percentage from baseline was calculated for each subject for each Brodmann area Average and STD of all subjects were then calculated for each BA The data is available for all three groups of subjects control group after waiting period control group after HBOT crossover and treated group after HBOT 15 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI Figure 11 Volume rendered Brain SPECT images representing the CBF change in percentage post control period and post HBOT of the cross group patient described in example 4 The overall changes after the control period and the HBOT show normal variations of brain perfusion in the 10 to 10 range from green to orange colors However close inspection reveals localized significant changes white circles in the in the right temporal pole and in the right dorso lateral area These changes in perfusion are in good agreement with the improvements in the cognitive indices as the SPECT detected changes correspond to Brodmann areas 45 46 11 38 and 39 doi 10 1371 journal pone 0079995 g011 use of their software Dr Glen Doniger in particular for his great help in administering the software s data and results and Prof Avraham Schweiger for his contribution to implementing the software in our study We are grateful to Dr Hanna Levi for valuable help with the statistics and data analysis and Dr Yaron Gross for his help with the randomizations analysis We are thankful Dr Alexander Vol and Dr Orna Gribova for enlightening discussions regarding the design of the proper hyperbaric oxygen therapy for TBI patients We thank Dr Nachum Gal and Dr Laura Herzog for their help in initiating this study We thank the following individuals for their important contribution in patients management during this study Alona Esterin Mazi Aski Sela Angela Chanimov Malca Katovski Lea Shkolnic Eyal Malca Vitali Triban Talia levy Doing so ease associating the changes in SPECT measurements of brain activity with the assessed changes in the cognitive indices PDF Protocol S1 Clinical study protocol DOCX Form S1 Informed consent form English translation DOCX Checklist S1 CONSORT 2010 checklist DOCX Text S1 Crossover approach and simulated randomi zation DOC Author Contributions Conceived and designed the experiments RB G HG SE Performed the experiments HG GF YB OV NS Analyzed the data RB G HG JB MF DH EB J SE Contributed reagents materials analysis tools HG OV SE Wrote the paper RB G HG EB J SE Acknowledgments The authors express special thanks to Michal Ben Jacob for her significant help in editing the manuscript We thank NeuroTrax Corporation for the References 5 Bazarian JJ Wong T Harris M Leahey N Mookerjee S et al 1999 Epidemiology and predictors of post concussive syndrome after minor head injury in an emergency population Brain injury BI 13 173 189 6 McCauley SR Boake C Pedroza C Brown SA Levin HS et al 2005 Postconcussional disorder Are the DSM IV criteria an improvement over the ICD 10 The Journal of nervous and mental disease 193 540 550 7 Kashluba S Paniak C Blake T Reynolds S Toller Lobe G et al 2004 A longitudinal controlled study of patient complaints following treated mild traumatic brain injury Archives of clinical neuropsychology the official journal of the National Academy of Neuropsychologists 19 805 816 8 Iverson GL 2005 Outcome from mild traumatic brain injury Current opinion in psychiatry 18 301 317 1 Coronado VG Xu L Basavaraju SV McGuire LC Wald MM et al 2011 Surveillance for traumatic brain injury related deaths United States 1997 2007 Morbidity and mortality weekly report Surveillance summaries 60 1 32 2 Faul M XL Wald MM Coronado VG 2010 Traumatic Brain Injury in the United States Emergency Department Visits Hospitalizations and Deaths 2002 2006 Atlanta GA Centers for Disease Control and Prevention National Center for Injury Prevention and Control 3 Efrati S Fishlev G Bechor Y Volkov O Bergan J et al 2013 Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PloS one 8 e53716 4 Cao H Ju K Zhong L Meng T 2013 Efficacy of hyperbaric oxygen treatment for depression in the convalescent stage following cerebral hemorrhage Experimental and therapeutic medicine 5 1609 1612 PLOS ONE www plosone org 16 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI 9 Bohnen N Jolles J Twijnstra A 1992 Neuropsychological deficits in patients with persistent symptoms six months after mild head injury Neurosurgery 30 692 695 discussion 695 696 10 Binder LM 1997 A review of mild head trauma Part II Clinical implications Journal of clinical and experimental neuropsychology 19 432 457 11 Bazarian JJ McClung J Shah MN Cheng YT Flesher W et al 2005 Mild traumatic brain injury in the United States 1998 2000 Brain injury BI 19 85 91 12 Kushner D 1998 Mild traumatic brain injury toward understanding manifestations and treatment Archives of internal medicine 158 1617 1624 13 Medana IM Esiri MM 2003 Axonal damage a key predictor of outcome in human CNS diseases Brain a journal of neurology 126 515 530 14 Kochanek PM Clark R S B Jenkins L W 2007 TBI Pathobiology In Zasler ND Katz D I Zafonte R D editor Brain injury medicine NY Demos medical publishing pp 81 92 15 Levin HS Mattis S Ruff RM Eisenberg HM Marshall LF et al 1987 Neurobehavioral outcome following minor head injury a three center study Journal of neurosurgery 66 234 243 16 Sohlberg MM Mateer CA 2001 Cognitive Rehabilitation An Integrative Neuropsychological Approach NY The Guilford Press 17 Niklas A Brock D Schober R Schulz A Schneider D 2004 Continuous measurements of cerebral tissue oxygen pressure during hyperbaric oxygenation HBO effects on brain edema and necrosis after severe brain trauma in rabbits J Neurol Sci 219 77 82 18 Reinert M Barth A Rothen HU Schaller B Takala J et al 2003 Effects of cerebral perfusion pressure and increased fraction of inspired oxygen on brain tissue oxygen lactate and glucose in patients with severe head injury Acta Neurochir Wien 145 341 349 discussion 349 35 19 Calvert JW Cahill J Zhang JH 2007 Hyperbaric oxygen and cerebral physiology Neurol Res 29 132 141 20 Neubauer RA James P 1998 Cerebral oxygenation and the recoverable brain Neurol Res 20 Suppl 1 S33 36 21 Golden ZL Neubauer R Golden CJ Greene L Marsh J et al 2002 Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy Int J Neurosci 112 119 131 22 Zhang JH Lo T Mychaskiw G Colohan A 2005 Mechanisms of hyperbaric oxygen and neuroprotection in stroke Pathophysiology 12 63 77 23 Gunther A Kuppers Tiedt L Schneider PM Kunert I Berrouschot J et al 2005 Reduced infarct volume and differential effects on glial cell activation after hyperbaric oxygen treatment in rat permanent focal cerebral ischaemia Eur J Neurosci 21 3189 3194 24 Yang YJ Wang XL Yu XH Wang X Xie M et al 2008 Hyperbaric oxygen induces endogenous neural stem cells to proliferate and differentiate in hypoxicischemic brain damage in neonatal rats Undersea Hyperb Med 35 113 129 25 Rockswold SB Rockswold GL Zaun DA Zhang X Cerra CE et al 2010 A prospective randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism intracranial pressure and oxygen toxicity in severe traumatic brain injury Journal of neurosurgery 112 1080 1094 26 Palzur E Vlodavsky E Mulla H Arieli R Feinsod M et al 2004 Hyperbaric oxygen therapy for reduction of secondary brain damage in head injury an animal model of brain contusion Journal of neurotrauma 21 41 48 27 Harch PG Kriedt C Van Meter KW Sutherland RJ 2007 Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury Brain research 1174 120 129 28 Vlodavsky E Palzur E Soustiel JF 2006 Hyperbaric oxygen therapy reduces neuroinflammation and expression of matrix metalloproteinase 9 in the rat model of traumatic brain injury Neuropathology and applied neurobiology 32 40 50 29 Palzur E Zaaroor M Vlodavsky E Milman F Soustiel JF 2008 Neuroprotective effect of hyperbaric oxygen therapy in brain injury is mediated by preservation of mitochondrial membrane properties Brain research 1221 126 133 30 Daugherty WP Levasseur JE Sun D Rockswold GL Bullock MR 2004 Effects of hyperbaric oxygen therapy on cerebral oxygenation and mitochondrial function following moderate lateral fluid percussion injury in rats Journal of neurosurgery 101 499 504 31 Lin JW Tsai JT Lee LM Lin CM Hung CC et al 2008 Effect of hyperbaric oxygen on patients with traumatic brain injury Acta neurochirurgica Supplement 101 145 149 32 Golden Z Golden CJ Neubauer RA 2006 Improving neuropsychological function after chronic brain injury with hyperbaric oxygen Disability and rehabilitation 28 1379 1386 33 Rockswold GL Ford SE Anderson DC Bergman TA Sherman RE 1992 Results of a prospective randomized trial for treatment of severely brain injured patients with hyperbaric oxygen Journal of neurosurgery 76 929 934 34 Harch PG Andrews SR Fogarty EF Amen D Pezzullo JC et al 2012 A phase I study of low pressure hyperbaric oxygen therapy for blast induced postconcussion syndrome and post traumatic stress disorder Journal of neurotrauma 29 168 185 35 Cifu DX Hart BB West SL Walker W Carne W 2013 The Effect of Hyperbaric Oxygen on Persistent Postconcussion Symptoms The Journal of head trauma rehabilitation PLOS ONE www plosone org 36 Wolf G Cifu D Baugh L Carne W Profenna L 2012 The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury Journal of neurotrauma 29 2606 2612 37 Collet JP Vanasse M Marois P Amar M Goldberg J et al 2001 Hyperbaric oxygen for children with cerebral palsy a randomised multicentre trial HBOCP Research Group Lancet 357 582 586 38 James PB 2001 Hyperbaric oxygenation for cerebral palsy Lancet 357 2052 2053 39 Doniger GM 2007 Mindstreams Computerized Cognitive Tests Test Descriptions Available http www mirror upsite co il uploaded files 1383_ e7d7d3d98c924f036d3123733419149d pdf Accessed 05 July 2013 40 Doniger GM 2012 Guide to MindStreams Normative Data Available http www mirror upsite co il uploaded files 1383_ b44d4786c91058be301cb09a94ba70f4 pdf Accessed 05 July 2013 41 Doniger GM Simon ES 2007 Construct Validity of Mindstreams Comparison with Paper Based Tests Available http www mirror upsite co il uploaded files 1383_b69dcc4f4445c4c986f21b3d307ec9be pdf Accessed 05 July 2013 42 Doniger GM 2007 Mindstreams Validity Reliability Available http www mirror upsite co il uploaded files 1383_2416003ae4c2131649d294df988f2143 pdf Accessed 05 July 2013 43 Rabin R de Charro F 2001 EQ 5D a measure of health status from the EuroQol Group Annals of medicine 33 337 343 44 Jaszczak RJ Chang LT Stein NA Moore FE 1979 Whole body single photon emission computed tomography using dual large field of view scintillation cameras Physics in medicine and biology 24 1123 1143 45 Cohen J 1988 Statistical power analysis for the behavioral sciences Mahwah NJ Lawrence Erlbaum 46 Lin AP Liao HJ Merugumala SK Prabhu SP Meehan WP 3rd et al 2012 Metabolic imaging of mild traumatic brain injury Brain imaging and behavior 6 208 223 47 Hattori N Swan M Stobbe GA Uomoto JM Minoshima S et al 2009 Differential SPECT activation patterns associated with PASAT performance may indicate frontocerebellar functional dissociation in chronic mild traumatic brain injury Journal of nuclear medicine official publication Society of Nuclear Medicine 50 1054 1061 48 Belanger HG Vanderploeg RD Curtiss G Warden DL 2007 Recent neuroimaging techniques in mild traumatic brain injury The Journal of neuropsychiatry and clinical neurosciences 19 5 20 49 Squire LR 2004 Memory systems of the brain a brief history and current perspective Neurobiology of learning and memory 82 171 177 50 Squire LR Zola Morgan S 1991 The medial temporal lobe memory system Science 253 1380 1386 51 Scoville WB Correll RE 1973 Memory and the temporal lobe A review for clinicians Acta neurochirurgica 28 251 258 52 Stuss DT Alexander MP 2000 Executive functions and the frontal lobes a conceptual view Psychological research 63 289 298 53 Stuss DT 2011 Functions of the frontal lobes relation to executive functions Journal of the International Neuropsychological Society JINS 17 759 765 54 Insel TR 2010 Faulty circuits Scientific American 302 44 51 55 Posner MI Rothbart MK Sheese BE Tang Y 2007 The anterior cingulate gyrus and the mechanism of self regulation Cognitive affective behavioral neuroscience 7 391 395 56 Catafau AM Parellada E Lomena F Bernardo M Setoain J et al 1998 Role of the cingulate gyrus during the Wisconsin Card Sorting Test a single photon emission computed tomography study in normal volunteers Psychiatry research 83 67 74 57 Kan EM Ling EA Lu J 2012 Microenvironment changes in mild traumatic brain injury Brain research bulletin 87 359 372 58 Neubauer RA James P 1998 Cerebral oxygenation and the recoverable brain Neurological research 20 Suppl 1 S33 36 59 Golden ZL Neubauer R Golden CJ Greene L Marsh J et al 2002 Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy The International journal of neuroscience 112 119 131 60 Zhang JH Lo T Mychaskiw G Colohan A 2005 Mechanisms of hyperbaric oxygen and neuroprotection in stroke Pathophysiology the official journal of the International Society for Pathophysiology ISP 12 63 77 61 Chang CC Lee YC Chang WN Chen SS Lui CC et al 2009 Damage of white matter tract correlated with neuropsychological deficits in carbon monoxide intoxication after hyperbaric oxygen therapy Journal of neurotrauma 26 1263 1270 62 Lo C Shifteh K Gold T Bello JA Lipton ML 2009 Diffusion tensor imaging abnormalities in patients with mild traumatic brain injury and neurocognitive impairment Journal of computer assisted tomography 33 293 297 63 Lo CP Chen SY Chou MC Wang CY Lee KW et al 2007 Diffusion tensor MR imaging for evaluation of the efficacy of hyperbaric oxygen therapy in patients with delayed neuropsychiatric syndrome caused by carbon monoxide inhalation European journal of neurology the official journal of the European Federation of Neurological Societies 14 777 782 64 Chen Z Ni P Xiao H Chen J Qian G et al 2008 Changes in brain function and anatomical structure following treatment of hyperbaric oxygen for visual pathway abnormalities in 16 cases Neural Regeneration Research 3 117 123 65 Vilela DS Lazarini PR Da Silva CF 2008 Effects of hyperbaric oxygen therapy on facial nerve regeneration Acta oto laryngologica 128 1048 1052 17 November 2013 Volume 8 Issue 11 e79995
Hyperbaric Oxygen Therapy for TBI 66 Neubauer RA Walker M 2000 Hyperbaric Oxygen Therapy Garden City Park NY Avery Publishing Group 67 Kuffler DP 2011 The role of hyperbaric oxygen therapy in enhancing the rate of wound healing with a focus on axon regeneration Puerto Rico health sciences journal 30 35 42 68 Rockswold SB Rockswold GL Defillo A 2007 Hyperbaric oxygen in traumatic brain injury Neurological research 29 162 172 69 Zhou Z Daugherty WP Sun D Levasseur JE Altememi N et al 2007 Protection of mitochondrial function and improvement in cognitive recovery in rats treated with hyperbaric oxygen following lateral fluid percussion injury Journal of neurosurgery 106 687 694 70 Calvert JW Cahill J Zhang JH 2007 Hyperbaric oxygen and cerebral physiology Neurological research 29 132 141 71 Anderson DC Bottini AG Jagiella WM Westphal B Ford S et al 1991 A pilot study of hyperbaric oxygen in the treatment of human stroke Stroke a journal of cerebral circulation 22 1137 1142 72 Nighoghossian N Trouillas P Adeleine P Salord F 1995 Hyperbaric oxygen in the treatment of acute ischemic stroke A double blind pilot study Stroke a journal of cerebral circulation 26 1369 1372 73 Rusyniak DE Kirk MA May JD Kao LW Brizendine EJ et al 2003 Hyperbaric oxygen therapy in acute ischemic stroke results of the Hyperbaric Oxygen in Acute Ischemic Stroke Trial Pilot Study Stroke a journal of cerebral circulation 34 571 574 74 Vila JF Balcarce PE Abiusi GR Dominguez RO Pisarello JB 2005 Improvement in motor and cognitive impairment after hyperbaric oxygen therapy in a selected group of patients with cerebrovascular disease a prospective single blind controlled trial Undersea hyperbaric medicine journal of the Undersea and Hyperbaric Medical Society Inc 32 341 349 75 Imai K Mori T Izumoto H Takabatake N Kunieda T et al 2006 Hyperbaric oxygen combined with intravenous edaravone for treatment of acute embolic stroke a pilot clinical trial Neurologia medico chirurgica 46 373 378 discussion 378 76 Glisky EL 2004 Disorders of memory In Ponsford J editor Cognitive and Behavioral Reabilitation From Neurobiology to Clinical Practice New York The Guilford Press pp 100 129 PLOS ONE www plosone org 77 de Frias CM Dixon RA Backman L 2003 Use of Memory Compensation Strategies Is Related to Psychosocial and Health Indicators The Journals of Gerontology Series B Psychological Sciences and Social Sciences 58 P12 P22 78 Golding FC Griffiths P Hempleman HV Paton WD Walder DN 1960 Decompression sickness during construction of the Dartford Tunnel British journal of industrial medicine 17 167 180 79 Austin D 1998 Gammow bag for acute mountain sickness Lancet 351 1815 80 Mychaskiw G 2nd Stephens PL 2013 Hyperbaric Oxygen Mild Traumatic Brain Injury and Study Design An Elusive Target Journal of neurotrauma 81 Goldbart AD Cohen AD Weitzman D Tal A 2007 Effects of rehabilitation winter camps at the Dead Sea on European cystic fibrosis patients The Israel Medical Association journal IMAJ 9 806 809 82 Kramer MR Springer C Berkman N Glazer M Bublil M et al 1998 Rehabilitation of hypoxemic patients with COPD at low altitude at the Dead Sea the lowest place on earth Chest 113 571 575 83 Falk B Nini A Zigel L Yahav Y Aviram M et al 2006 Effect of low altitude at the Dead Sea on exercise capacity and cardiopulmonary response to exercise in cystic fibrosis patients with moderate to severe lung disease Pediatric pulmonology 41 234 241 84 Abinader EG Sharif D Rauchfleich S Pinzur S Tanchilevitz A 1999 Effect of low altitude Dead Sea location on exercise performance and wall motion in patients with coronary artery disease The American journal of cardiology 83 250 251 A255 85 Gabizon I Shiyovich A Novack V Khalameizer V Yosefy C et al 2011 Impact of descent and stay at a Dead Sea resort low altitude on patients with systolic congestive heart failure and an implantable cardioverter defibrillator The Israel Medical Association journal IMAJ 13 402 407 86 Mychaskiw Ii G Stephens P 2012 Hyperbaric oxygen mild traumatic brain injury and study design an elusive target Journal of neurotrauma 87 Potter S Leigh E Wade D Fleminger S 2006 The Rivermead Post Concussion Symptoms Questionnaire a confirmatory factor analysis Journal of neurology 253 1603 1614 18 November 2013 Volume 8 Issue 11 e79995
Neuropsychology Review https doi org 10 1007 s11065 021 09500 9 REVIEW Impact of Hyperbaric Oxygen Therapy on Cognitive Functions a Systematic Review Anna B Marcinkowska1 2 Natalia D Mankowska1 Jacek Kot3 Pawel J Winklewski1 2 Received 17 May 2020 Accepted 7 March 2021 The Author s 2021 Abstract Hyperbaric oxygen therapy HBOT is a modality of treatment in which patients inhale 100 oxygen inside a hyperbaric chamber pressurised to greater than 1 atmosphere The aim of this review is to discuss neuropsychological findings in various neurological disorders treated with HBOT and to open new perspectives for therapeutic improvement A literature search was conducted in the MEDLINE via PubMed database from the inception up 10 May 2020 Eligibility criteria included original articles published in English Case studies were excluded Full text articles were obtained from the selected studies and were reviewed on the following inclusion criteria 1 performed cognitive processes assessment 2 performed HBOT with described protocol Two neuropsychologists independently reviewed titles abstracts full texts and extracted data The initial search retrieved 1024 articles and a total of 42 studies were finally included after applying inclusion and exclusion criteria The search yielded controversial results with regard to the efficiency of HBOT in various neurological conditions with cognitive disturbance outcome To the best of our knowledge this is the first state of the art systematic review in the field More objective and precise neuropsychological assessment methods are needed to exact evaluation of the efficacy of HBOT for neuropsychological deficits Future studies should widen the assessment of HBOT effects on different cognitive domains because most of the existing studies have focussed on a single process Finally there is a need for further longitudinal studies Keywords Neuropsychology Cognition Hyperbaric oxygen therapy Introduction Key Points Enhanced oxygen supply and increased pressure result in a variety of pathophysiological mechanisms A more aggressive approach to carbon monoxide poisoning is needed to ameliorate cognitive consequences A post concussion syndrome trials should include standardised neuropsychological methods Hyperbaric oxygen therapy could be considered in stroke patients after thrombolysis or thrombectomy Hyperbaric oxygen therapy for treating dementia should be further investigated Anna B Marcinkowska anna marcinkowska gumed edu pl 1 Applied Cognitive Neuroscience Lab Department of Human Physiology Medical University of Gda sk Tuwima Str 15 80 210 Gda sk Poland 2 2nd Department of Radiology Medical University of Gda sk Gda sk Poland 3 National Centre for Hyperbaric Medicine Institute of Maritime and Tropical Medicine in Gdynia Medical University of Gdansk Gda sk Poland Hyperbaric oxygen therapy HBOT is a modality of treatment in which patients inhale 100 oxygen through a head tent mask or endotracheal tube inside a hyperbaric chamber that has been pressurised to greater than 1 absolute atmosphere ATA HBOT is typically administered at more than one and less than three ATA and induces a state of increased pressure and hyperoxia that cause mechanical and physiologic effects HBOT has been recommended for various conditions for more than 40 years Grim 1990 Leach et al 1998 Initially it was used to treat decompression sickness in divers However over the years its far reaching potential has been recognised and it has been approved for a variety of purposes including carbon monoxide CO poisoning decompression sickness and gas embolism problematic wound healing delayed radiation injuries sudden deafness and other conditions as indicated by evidence based medicine Mathieu et al 2017 Moon 2019 Although controlled clinical trials are limited the rational basis of HBOT as well 13 Vol 0123456789
as good clinical results have gradually increased the use of HBOT for neurological disorders linked with cognitive disturbances Neurological disorders as well as conditions related to central nervous system CNS damage may present with a variety of neuropsychological symptoms such as impairment of memory and learning processes attention and visuo spatial functions language processes and executive dysfunctions The neuroprotective and therapeutic effects of neuropsychological deficits provided by HBOT have been established in experimental animal and human models although they remain controversial In this review we will summarise the existing results of HBOT usage in several neurological states its current understanding and opinions for future studies To the best of our knowledge this is the first state of the art systematic review in this topic To understand the role of HBOT in neurological disorders a basic knowledge of cerebral metabolism cerebral blood flow and the neurophysiology of the brain is essential The physiological basis of HBOT is the gas laws While breathing air at atmospheric pressure most of the oxygen is bound to haemoglobin In this situation blood haemoglobin is saturated with oxygen at approximately 97 and working at near maximum capacity with a small amount of oxygen dissolved in the blood plasma compartment If the percent of inhaled oxygen or the pressure at which oxygen is breathed is increased more oxygen will dissolve into the blood plasma In HBOT conditions the fraction of inspired oxygen and partial pressure of oxygen increases supersaturating the blood with oxygen Inhaling 100 oxygen at 3 ATA increases mean arterial oxygen tension from approximately 100 mmHg in normobaric conditions to 2000 mmHg and the amount of oxygen delivery to the tissues from 3 to 60 mL of oxygen per litre of blood Jain 2017 Supersaturation of the blood to this degree supports resting tissue oxygen requirements without a necessary contribution from haemoglobin carriage Hence HBOT is useful in diseases in which haemoglobin function is limited such as CO poisoning or ischaemia Mathieu 2006a The excess oxygen is carried in solution and it can diffuse to areas where red blood cells cannot reach This elevation in the partial pressure of oxygen in tissue mediates the therapeutic benefits of HBOT Enhanced oxygen supply and increased pressure result in a wide variety of pathophysiological mechanisms Thus HBOT is believed to diminish neuroinflammatory responses blood brain barrier permeability and apoptosis while positively impacting neurogenesis neuronal and axonal integrity and synaptogenesis reviewed by Daly et al 2018 Fischer et al 2010 All of these effects may potentially influence patients cognitive functioning Nevertheless direct links are very difficult to establish Recent advances in radiology and medical imaging in particular diffusion tensor imaging DTI and advanced perfusion models could potentially fill 13 Neuropsychology Review the gap and provide better understanding of the interdependence among white matter structure cerebral blood flow and cognition Chen et al 2010 Tal et al 2017 Brain metabolism generates large amounts of reactive forms of oxygen There is an excessive literature demonstrating that augmented oxygen reactivity is associated with deteriorated performance in cognitive tasks Bhatt et al 2020 Kandlur et al 2020 At the same time however reactive oxygen species may also play a role in functional and structural modifications indispensable for synaptic plasticity Massaad Klann 2011 In particular reactive forms of oxygen seem to be involved in regulation of N methyl d aspartate NMDA receptors Betzen et al 2009 calcium Ca2 channels Huddleston et al 2008 potassium channels Gong et al 2000 and Ca2 calmodulin kinase II Shetty et al 2008 functioning Hydrogen peroxide promotes ryanodine receptor redox modifications in hippocampal neurons Kemmerling et al 2007 Consequently although oxygen reactive forms seem to be necessary for long term potentiation the cellular substrate for memory they are also implicated with deficient long term potentiation during aging Hu et al 2007 and in mouse models of Alzheimer Disease AD Cai et al 2008 HBOT schemes differ from study to study what may result in various exposures to oxidative stress Therefore it is difficult to predict whether beneficial or detrimental effects of reactive oxygen forms on cognition in particular study prevails The diversity and strength of innate repair mechanisms activated by HBOT are associated both with the elevated level of dissolved oxygen and the elevated pressure Efrati Ben Jacob 2014b However it remains unclear how oxygen and pressure relate to each other For instance it has been proposed that HBOT may act as a transducer to improve oxidative metabolism while subsequent normobaric oxygen therapy 100 oxygen 1 ATA may further enhance this effect Rockswold et al 2010 2013 Exposure of rat brain slices to high pressures 5 3 ATA typically shows an augmentation in the synaptic NMDA receptors response usually followed by post synaptic excitability modifications Bliznyuk et al 2020 Mor Grossman 2010 Mor Grossman 2007 HBOT and normobaric reoxygenation augment excitability and activate oxygen induced potentiation in CA1 hippocampal neurons Garcia et al 2010b Moreover oxygen induced neural plasticity does not need modifications in excitatory synaptic transmission Garcia et al 2010a When referring to experiments performed with the use of brain slices it should be kept in mind that it remains unclear whether the reported hyperexcitability and which forms of increased neuronal excitability are a part of the learning process or actually represent cellular manifestation of neuronal oxygen poisoning The only experiments performed by our team on humans exposed to 1 4
Neuropsychology Review ATA and 2 8 ATA HBO may suggest that actually oxygen related mechanisms affecting cognition and poisoning might be interrelated Kot et al 2015 The study was however performed on young males from the elite military Special Forces unit and therefore might not be representative for wider population Traditional view is that hyperoxia below 2 8 ATA diminishes brain perfusion Di Piero et al 2002 Kety Schmidt 1948 Omae et al 1998 due to cerebral vasoconstriction caused by an interruption in nitric oxide mediated basal relaxation of cerebral vessels Bitterman Bitterman 1998 Oury et al 1992 The topic has been extensively reviewed by our team Winklewski et al 2013 The existing dogma has been challenged by Micarelli et al 2013 Authors investigated 7 healthy volunteers during acute exposure to HBO at 2 5 ATA thus mimicking a possible therapeutic condition The authors reported augmented brain perfusion in the left hemisphere with a relative cerebral blood flow increase in the neural networks encompassing dorsal and ventral attention pathways Nevertheless the links between changes in brain perfusion and cognition are complex and not fully understood Quite insightful are data coming from the investigations of the impact of physical training on perfusion and cognition It is generally believed that active lifestyle slowdown cerebral prefusion and cognitive decline associated with age Boraxbekk et al 2016 Jackson et al 2016 Szalewska et al 2017 However Guiney et al 2019 demonstrated that improvements in higher order cognitive functioning in healthy older adults associated with habitual physical activity were not related to improved cerebrovascular functioning Hyperoxia and in particular HBOT exposure results in increased parasympathetic nervous system activity bradycardia and dissociation between heart rate and broader cardiovascular system responses Lodato Jubran 1993 Parkinson Registrar 1871 Walter et al 1962 The neurovisceral integration model proposes a bi directional cortical influences on autonomic functioning and integrates central nervous and autonomic systems Smith et al 2017 Thayer Lane 2000 The main affector and effector of the parasympathetic nervous system is the vagal nerve Electrical vagal nerve stimulation seems to improve cognitive functioning in particular memory consolidation and recognition Clark et al 1999 Ghacibeh et al 2006 Vonck et al 2014 Interestingly also behavioural interventions such as slow breathing associated with vagal nerve increased activity are able to modulate cortical alpha rhythm Hsu et al 2020 Maric et al 2020 Cardiovascular desynchronization in turn may have detrimental impact on cognition Ogoh Tarumi 2019 Evidence for cognitive improvements after HBOT in different neurological disorders accumulates Boussi Gross et al 2015 Hardy et al 2002 Rossignol et al 2007 Tapeantong Poungvarin 2009 Nevertheless there is still an ongoing debate regarding the efficacy of HBOT in individuals with traumatic brain injury TBI stroke or other neurological conditions Although it is widely agreed and confirmed by the majority of studies that HBOT leads to significant improvements in cognition the debate is mostly related to a control group issue and minimal effective dosages the minimal pressure that does not have any physiological effect on the CNS Churchill et al 2013 Efrati Ben Jacob 2014a b Golden et al 2006 Harch et al 2007 Wolf et al 2012 There are several neurological conditions where HBOT has been reported to be useful that is CO poisoning TBI and post concussion syndrome PCS stroke and neurodegenerative disorders Existing intensive functional therapy and neuropsychological rehabilitation programmes are considered essential to minimise cognitive and physical sequelae associated with brain damage in various neurological states Neuropsychological rehabilitation refers to helping cognitively impaired individuals to totally or partially restore normal functioning compensate cognitive emotional psychosocial and behavioural deficits and improve the quality of life However considering the heterogeneity of physical cognitive behavioural and psychosocial symptoms in various neurological states these programmes are often only partially successful Those programs should be improved and modified in accordance with the better understanding of cognitive processes and brain structures via newest neuroimaging techniques and medical development It is well known that neuroplasticity and synaptic reorganization have a decisive role in neuropsychological rehabilitation effects Sohlberg Mateer 2001 Some of the mechanisms involved in both processes have essential implications for rehabilitation such as diaschisis functional reorganization or modification of synaptic connectivity among others Sohlberg Mateer 2001 Thus alternative approaches dedicated to the metabolic recovery of cerebral tissues that stimulates synaptic and functional plasticity such as HBOT need to be further explored in order to improve the neuropsychological outcome of a patient Finally there are some adverse events and risks associated with HBOT They are related to changes in atmospheric pressure hyperbaric oxygen exposure and psychological factors i e confinement anxiety Middle ear barotrauma is the most common HBOT related complication with incidence rates ranging between authors from 2 to 82 In one of the largest retrospective study of HBOT safety the incident risk of middle era barotrauma was 9 2 of patients which gives 410 events per 100 000 sessions The safety of hyperbaric oxygen treatment was assessed in 2 334 patients Hadanny et al 2016b To minimise this risk patients are provided with instructions describing ear clearing techniques like swallowing chewing and modified Valsalva manoeuvre In intubated and unconscious patients 13
myringotomy is the procedure of choice before the HBOT Oxygen itself is a drug and there is always a risk of adverse effects based on biochemical reactions CNS oxygen toxicity presented with the temporarily loss of consciousness and general seizures is quite infrequent event It occurs with a rate of only 1 59 events per 100 000 sessions mostly at pressures 2 4 ATA and above Hadanny et al 2016a Seizures during hyperbaric oxygen therapy were assessed in retrospective analysis of 62 614 treatment sessions This is one of the reasons why in case of using HBOT in emergency indications i e diving accidents CO intoxication compartment syndrome etc when high partial pressure of oxygen is used use of multiplace chambers with direct supervision of medical attendant inside the chamber is preferred If such event occurs the internal attendant immediately removes the oxygen mask from the patient and switches him or her to air breathing Lungs oxygen toxicity is cumulative but can be avoided by using minimum inspired fractions of oxygen between HBOT sessions In some patients with pre existing cardiac problems there is a risk of hypotension after HBOT due to hypovolemia evoked by vanishing vasoconstrictive effect Hypovolemia risk can be mitigated by careful volume assessment and if needed volume loading before the end of oxygen exposure Eyes oxygen toxicity manifesting as myopia may occur in patients receiving HBOT over several weeks Myopia is usually spontaneously reversible within a short period of time Gas embolism and pulmonary barotrauma a well known phenomena in divers during decompression in hyperbaric chambers are very rare Mathieu 2006b Oriani et al 1996 In conclusion of the adverse effects the HBOT is generally considered as a low risk medical procedure when conducted by the well trained hyperbaric personnel in carefully assessed patients Methodology PRISMA guidelines were used for the reporting of this systematic review Moher et al 2009 Data Sources Electronic database Pubmed was searched from 1946 to 2020 for relevant studies last search was performed on 10 May 2020 The reference lists of included studies were handsearched for additional references Separate search for four medical indications for HBOT CO intoxication post concussion syndrome stroke ageing and neurodegenerative diseases was made The following search terms were used 13 Neuropsychology Review a CO intoxication Search hyperbaric oxygen therapy AND carbon monoxide AND cognition hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND carbon monoxide MeSH Terms OR carbon All Fields AND monoxide All Fields OR carbon monoxide All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cognitives All Fields b Traumatic brain injury Search hyperbaric oxygen therapy AND concussion AND cognition Sort by Most Recent hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND brain concussion MeSH Ter ms OR brain All Fields AND concussion All Fields OR brain concussion All Fields OR concussion All Fields OR concussions All Fields OR concussed All Fields OR concussive All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cognitives All Fields and Search hyperbaric oxygen therapy AND traumatic brain injury AND cognition hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND brain injuries traumatic MeSH Terms OR brain All Fields AND injuries All Fields AND traumatic All Fields OR traumatic brain injuries All Fields OR traumatic All Fields AND brain All Fields AND injury All Fields OR traumatic brain injury All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cognitives All Fields c Stroke Search hyperbaric oxygen therapy AND stroke AND cognition hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND
Neuropsychology Review stroke MeSH Terms OR stroke All Fields OR strokes All Fields OR stroke s All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cognitives All Fields and Search hyperbaric oxygen therapy AND cognition AND ischemia hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cognitives All Fields AND ischaemia All Fields OR ischemia MeSH Terms OR ischemia All Fields OR ischaemias All Fields OR ischemias All Fields d Ageing and neurodegenerative disorders Search hyperbaric oxygen therapy AND neurodegenerative disease AND cognition hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND neurodegenerative diseases MeSH Terms OR neurodegenerative All Fields AND diseases All Fields OR neurodegenerative diseases All Fields OR neurodegenerative All Fields AND disease All Fields OR neurodegenerative disease All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cogni tives All Fields and Search hyperbaric oxygen therapy AND alzheimer disease hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND alzheimer disease MeSH Terms OR alzheimer All Fields AND disease All Fields OR alzheimer disease All Fields and Search hyperbaric oxygen therapy AND neurodegeneration AND cognition Sort by Most Recent hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND nerve degeneration MeSH Terms OR nerve All Fields AND degeneration All Fields OR nerve degeneration All Fields OR neurodegeneration All Fields OR neurodegenerating All Fields OR neurodegenerations All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cognitives All Fields and Search hyperbaric oxygen therapy AND ageing AND cognition Sort by Most Recent hyperbaric oxygenation MeSH Terms OR hyperbaric All Fields AND oxygenation All Fields OR hyperbaric oxygenation All Fields OR hyperbaric All Fields AND oxygen All Fields AND therapy All Fields OR hyperbaric oxygen therapy All Fields AND aging MeSH Terms OR aging All Fields OR ageing All Fields AND cognition MeSH Terms OR cognition All Fields OR cognitions All Fields OR cognitive All Fields OR cognitively All Fields OR cognitives All Fields Study Selection and Eligibility Criteria A two step approach was used to select articles Firstly titles and abstracts of all search results were screened for the following characteristics 1 original article published in English 2 case studies were excluded Secondly full text articles were obtained from the selected studies and were reviewed on the following inclusion criteria 1 performed cognitive processes assessment 2 performed HBO therapy with described HBOT protocol Two neuropsychologists independently reviewed titles abstracts full texts and extracted data The review process is summarized in Figs 1 2 3 and 4 Results from the systematic literature search are provided separately in each indication section of the manuscript Results and Discussion HBOT and Cognitive Dysfunctions After CO Intoxication Exposure to CO which excludes oxygen from tissues through the formation of a stable complex carboxyhaemoglobin COHb can damage various body systems including the CNS The acute symptoms reported by patients are headache weakness or lethargy dizziness nausea shortness of breath chest pain visual changes and muscle cramping Moreover up to 45 have cognitive problems with memory attention and concentration Weaver et al 2002 Patients in more severe states with a loss of consciousness or with COHb levels greater than 13
Neuropsychology Review Fig 1 PRISMA Flow Diagram for Included Studies for HBOT usage in cognitive dysfunction after CO intoxication 25 frequently show cognitive dysfunction lasting 1 month or longer Goldstein 2008 Weaver et al 2002 Multiple mechanisms are involved in both acute and delayed CO toxicity including neuroinflammation apoptosis and brain lipid peroxidation All of them are ameliorated by HBOT reviewed by Mannaioni et al 2006 Most patients with CO poisoning can recover from the acute phase However around 1 30 of patients develop delayed neuropsychological sequelae 2 6 weeks after recovery from the acute phase Choi 1983 Weaver 2009 Weaver et al 2007 Therefore treatment for CO poisoning during the acute phase aims to address immediate threats to life as well as prevent delayed and sometimes permanent neuropsychological morbidity Liao et al 2019 Mathieu et al 1985 Gale and Hopkins 2004 recruited 20 patients with CO poisoning and assessed neuropsychological functioning 13 They showed a correlation between impairment of verbal memory and visual memory and reduced hippocampal volume in patients Cognitive disturbances were present even 6 months or longer after CO poisoning Chang et al 2010 described similar findings about persistent neuropsychological deficits verbal episodic memory visual memory and visual spatial ability in 9 patients with CO exposure these issues were still present after 3 and 10 months Moreover T2 weighted brain magnetic resonance imaging of patients with delayed neuropsychiatric sequelae after CO poisoning shows damage to the hippocampus Bruno et al 1993 Henke et al 1999 and white matter lesion in the frontal lobe and periventricular area Mundy et al 2013 Park Kim 2014 Those regions are involved in reference memory and working memory respectively Burges et al 2002 Prior et al 1997
Records identified through database searching n 61 Eligibility Included Identification Screening Eligibility Included Records screened n 54 Records excluded n 25 Full text articles assessed for eligibility n 29 Full text articles excluded with reasons n 10 Studies included in qualitative synthesis n 19 The standard treatment for CO poisoning includes administration of 100 oxygen and general supportive care Administration of supplemental oxygen increases the Fig 3 PRISMA Flow Diagram for Included Studies for HBOT usage in postroke cognitive disturbances Additional records identified through other sources n 13 Records after duplicates removed n 54 Screening Fig 2 PRISMA Flow Diagram for Included Studies for usage of HBOT in TBI related cognition disorders Identification Neuropsychology Review dissolved oxygen content hastens the elimination of COHb in the blood and decreases cerebral oedema Goldstein 2008 HBOT is often recommended for patients with acute Records identified through database searching n 41 Additional records identified through other sources n 13 Records after duplicates removed n 34 Records screened n 34 Records excluded n 19 Full text articles assessed for eligibility n 15 Full text articles excluded with reasons n 9 Studies included in qualitative synthesis n 6 13
Neuropsychology Review Records identified through database searching n 78 Additional records identified through other sources n 2 Records after duplicates removed n 54 Records screened n 54 Records excluded n 45 Full text articles assessed for eligibility n 14 Full text articles excluded with reasons n 6 Included Eligibility Screening Fig 4 PRISMA Flow Diagram for Included Studies for HBOT in cognitive ageing and neurodegenerative disorders Identification Studies included in qualitative synthesis n 8 CO poisoning especially if they have lost consciousness or have severe poisoning symptoms Mathieu et al 2017 Stoller 2007 There are also few animal studies in this field Liu et al 2016 sought whether neurogenesis is the target for HBOT to abrogate the delayed neuropsychological sequelae after CO poisoning HBOT 2 5 ATA with 100 oxygen for 60 min was conducted on rats during the first 7 days after CO poisoning Their animal research suggests that early HBOT may ameliorate delayed neuropsychological disturbances after acute CO poisoning by promoting neurogenesis through upregulating Brain Derived Neurotrophic Factor BDNF in the hippocampus Furthermore the same group of authors conducted study with HBO therapy combined with N butylphthalide on 80 rats HBOT was conducted on the same conditions as in previous study Rats performed Morris Water Maze Task Last part of the study included hippocampus microstructure assessment Authors concluded that combined therapy can improve cognitive functioning through maintaining ultrastructural integrity of hippocampus and thus may play a neuroprotective role in brain tissue in rats with CO poisoning Animal studies examining effect of HBOT on cognition after carbon monoxide intoxication are presented in Table 1 Several studies have investigated the effect of HBOT with multiple neuropsychological methods Scheinkestel et al 1999 conducted a double blind randomised clinical trial to investigate the effects of HBOT by measuring cognitive functioning immediately after the therapy daily treatments with 100 oxygen in a hyperbaric chamber 60 min at 2 8 ATA for the HBOT group and at 1 0 ATA for the normobaric oxygen group for three days and 1 month later They found no improvement in the patients states and they reported a worse outcome in learning tests Table 1 Effect of HBOT in carbon monoxide poisoning on cognition in animals Authors Studied group Liu et al 2016 10 rats after acute carbon monoxide poisoning Bi et al 2017 80 rats after CO intoxication divided in two groups HBOT and HBOT N butylphthalide HBOT protocol 7 sessions for 60 min at 2 5 ATA Eight arm maze test Results Improvement in memory 7 sessions for 60 min at 2 5 ATA Morris Water Maze Task Improvement in memory ATA absolute atmosphere CO carbon monoxide HBOT hyperbaric oxygen therapy 13 Cognitive measures
Neuropsychology Review A similar methodology was used by Weaver et al 2002 they examined 152 patients with CO poisoning with various neuropsychological tests after the first and third session and at 2 and 6 weeks 6 months and 12 months after HBOT All subjects underwent three protocol directed sessions in monoplace hyperbaric chambers at intervals of 6 to 12 h The first oxygen treatment session was initiated within 24 h after the end of the exposure to CO During both hyperbaric oxygen and normobaric oxygen sessions all intubated patients were mechanically ventilated with 100 oxygen The patients in the HBOT group were exposed to 100 oxygen at 3 ATA and then 2 ATA during the first chamber session and then to 100 oxygen at 2 ATA during sessions 2 and 3 Subjects in the normobaric oxygen group were exposed to air at 1 ATA for all three chamber sessions After three sessions there were improvement in a few neuropsychological tests Digit Span Trail Making Digit Symbol Block Design and Story Recall demonstrating increased attention visuo spatial and memory processes as well as processing speed This avoided two of the limitations of the study by Scheinkestel et al 1999 i e loss to follow up and cluster rather than patient level randomisation for group exposures Thus it was the first study that was not plagued with or accused of having methodological flaws From this study 44 individuals were subsequently enrolled to ancillary prospective APOE genotyping study The authors found that HBOT reduced cognitive deficits after CO poisoning in the absence of the e4 allele and concluded that HBOT is a useful treatment for preventing cognitive sequalae after CO poisoning Hopkins et al 2007 Delayed neuropsychiatric sequel is estimated to occur in 10 30 of victims of carbon monoxide poisoning but the reported incidence varies widely S nmez et al 2018 Its various symptoms mainly comprise cognitive impairment parkinsonism urinary and faecal incontinence dementia and psychosis Choi 1983 Tapeantong Poungvarin 2009 Emergent HBOT within 24 h reduces the risk of cognitive sequelae after acute CO poisoning Weaver et al 2002 Yeh et al 2014 indicated that patients with delayed neuropsychiatric sequel after CO intoxication had poorer performance on general cognitive functioning language skills psychomotor speed visual spatial processes logical and working memory and executive function compared to those with acute CO poisoning at 1 month Compared with the acute neuropsychological sequel group the group with delayed symptoms had more significant progress at 6 month follow up after HBOT with regard to general cognitive function psychomotor speed and visuo spatial skills However the follow up progress on language processes logical memory and executive function tasks did not differ between the groups These results support previous brain image findings that patients with delayed neuropsychiatric sequel had abnormal deep white matter and frontal lobe regions Ernst Zibrak 1998 Zagami et al 1993 The authors suggested that future research should employ standardised and comprehensive neuropsychological tasks as well as larger samples and matching brain imaging investigations Lo et al 2007 performed magnetic resonance diffusion tensor imaging and Mini Mental State Examination MMSE examination in 6 patients with delayed neuropsychiatric sequel immediately before and 3 months after HBOT subjects underwent from 8 to 40 consecutive sessions depending on the clinical response with a pressure of 2 5 ATA for 120 min in each session to obtain fractional anisotropy values and assess neuropsychological functioning There was a significantly higher mean fractional anisotropy value in the control group compared with the patients both before and 3 months after HBOT Notably in the individuals with delayed symptoms of CO poisoning the mean fractional anisotropy value 3 months after HBOT was also significantly higher than before HBOT All of the patients regained full scores in the MMSE 3 months after the hyperbaric oxygen therapy Chang et al 2010 examined 9 patients with symptoms of delayed neuropsychiatric sequel who received HBOT at 2 5 ATA for 120 min five days per week during hospitalisation 8 40 sessions For all patients cognitive symptoms significantly improved after the therapy with significantly higher MMSE scores However white matter changes remained evident in the brain magnetic resonance scans Although HBOT has been applied clinically for the treatment of both acute and delayed phase of CO poisoning and HBOT reduces the neurological sequelae caused by the poison the clinical benefits and the underlying mechanisms are still controversial Annane et al 2011 Birmingham Hoffman 2011 Camporesi 2014 Hampson et al 2013 Weaver et al 2007 Nevertheless growing evidence has indicated that HBOT can promote proliferation of endogenous neural stem cells and stimulate neurogenesis in the injured brain Lee et al 2013 Mu et al 2011 Z dori et al 2011 Delayed encephalopathy after acute CO poisoning DEACMP is a very serious complications Goldstein 2008 DEACMP is a common cause of clinical neurological complications and may result in memory impairment unresponsiveness visceral autonomic nervous system dysfunction Parkinson s disease cognitive dysfunction and behavioural disorders in patients Currently the pathogenesis of DEACMP remains elusive Given that the CNS is the tissue that is most sensitive to oxygen some researchers have sought primary factors that induce DEACMP in hypoxia caused by CO poisoning Lee et al 1988 Prockop Chichkova 2007 This theory does not explain all clinical manifestations and pathological changes present in DEACMP especially the variety of symptoms that occur after the recovery of the carbonyl haemoglobin level Other researchers have reported that delayed CO poisoning neuropathology is associated with 13
an adaptive immunological response to chemically modified myelin basic protein Thom et al 2004 Xiang et al 2017a b in their double blind randomised study involving 215 DEACMP patients MMSE score 24 indicative of cognitive delay found that both HBOT and the combined application of N butylphthalide and HBOT with 2 5 ATA for 80 min per day significantly increased cognitive functioning measured with MMSE after short term treatment The efficacy of the combined treatment was greater than HBOT alone After 8 weeks of treatment almost half of the experimental group achieved significantly higher results compared to the control group The researchers concluded that HBOT may increase the blood oxygen level to alleviate the hypoxic state in the brain of CO poisoned patients This phenomenon is beneficial to the functional recovery of damaged brain cells Moreover the combined application of N butylphthalide and HBOT may be a potential effective therapy in treating cognitive dysfunction for patients with DEACMP Furthermore the same authors conducted study on 120 DEACMP patients divided in two groups HBOT alone and HBOT plus dexamethasone Each patients received 20 hyperbaric oxygen therapy sessions at 2 5 ATA for 80 min per day MMSE performed before and after 4 weeks of treatment showed cognitive improvement in both groups Although authors concluded that the combined application of dexamethasone and HBO therapy should be considered as it yields better efficacy for patients with DEACMP Xiang et al 2017a b Efficacy of N butylphthalide and dexamethasone combined with HBOT in patients with DEACMP was also studied in recent study by Zhang et al 2020 Authors examined 171 DEACMP patients and divided in two groups combined therapy and HBO alone Cognitive state was assessed with MMSE and Montreal Cognitive Assessment MoCA scale before and 1 and 3 months and 1 year after the treatment Their results indicate that combined therapy can significantly improve cognitive and motor functions of patients with DEACMP Human studies examining effect of HBOT on cognition after carbon monoxide intoxication are presented in Table 2 Current studies examining CO intoxication effects mostly agree that HBOT is promising therapy for improving patients cognition Although research paradigm varies e g therapy range from 3 to 40 HBOT sessions thus comparing results should be made with caution Furthermore detailed neuropsychological assessment is rarely done Cognitive screening methods i e MMSE MoCA are not reliable and sensitive enough to detect subtle changes in cognitive functioning Future studies should be designed to determine optimal combinations of the dose and timing of HBOT and planned subgroup analyses should attempt to define which patients could benefit most from hospital transfer These studies will hopefully provide the evidence needed 13 Neuropsychology Review to eliminate the remaining doubt about the effectiveness of HBOT More aggressive and appropriate treatment options than are used today are needed The correct diagnosis of the cognitive consequences of CO poisoning often occur quite a bit after the exposure Thus appropriate and timely treatment is even more problematic HBOT and TBI Related Cognition Disorders TBI can be caused by several factors An external physical force rapid acceleration or deceleration of the head bleeding within or around the brain lack of sufficient oxygen to the brain or toxic substances passing through the blood brain barrier The damage caused by TBI can be focal confined to one area of the brain or diffuse involving more than one area of the brain Zhang et al 2014 Symptoms of a TBI vary from mild and moderate to severe depending on the extent of the damage to the brain TBI can result in temporary or permanent impairment of cognitive emotional or physical functioning state Thus it has become a significant concern in civilian and military populations Chiu LaPorte 1993 TBI is linked with several pathological mechanisms that is diffuse shearing of axonal pathways and small blood vessels which is also known as diffuse axonal injury Medana Esiri 2003 ischaemia mild oedema and other biochemical and inflammatory processes that culminate in impaired regenerative or healing processes resulting from increasing tissue hypoxia Zasler et al 2007 Furthermore TBI can lead to PCS a complex of symptoms such as headaches dizziness imbalance vertigo fatigue changes in sleep pattern neuropsychiatric symptoms e g behavioural and mood changes confusion and cognitive impairments in memory attention concentration and executive functions McCauley et al 2000 Due to multiple pathological mechanisms cognitive impairments are usually the predominant symptoms localised in multiple brain areas Kushner 1998 Levin 1990 Sohlberg Mateer 2001a b The use of HBOT for brain injury is based on the hypothesis that injured or inactive neurons would benefit from increased blood flow and oxygen delivery which would act to metabolically or electrically reactivate the cells Deng 2018 Francis Baynosa 2017 Neubauer James 1998 In recent years animal models Chen et al 2010 Efrati Ben Jacob 2014a b Lin et al 2012 Neubauer James 1998 and human studies Barrett et al 2004 Boussi Gross et al 2013 Golden et al 2006 Harch et al 2012 Shi et al 2003 Tal et al 2015 Wright et al 2009 have shown that HBOT can improve PCS by targeting basic pathological processes Hadanny Efrati 2016 The evidence about the effectiveness of HBOT for TBI is conflicting and the case series and time series studies of HBOT for TBI patients had serious flaws One of the most concerning issues is the
Patients referred to acute CO poisoning 104 subjects received HBO therapy Symptomatic acute carbon monoxide poisoning 76 subjects 6 patients with delayed neuropsychiatric sequel caused by CO intoxication 9 patients with delayed neuropsychiatric sequel after CO intoxication 215 DEACMP patients divided in two groups HBOT and HBOT N butylphthalide 120 patients with DEACMP divided in two groups HBOT and HBOT dexamethasone 171 DEACMP patients divided in two groups HBOT and HBOT N butylphthalide dexamethasone Scheinkestel et al 1999 Weaver et al 2002 Lo et al 2007 Cognitive improvement higher MMSE scores Cognitive improvement in both groups Cognitive improvement in both groups Cognitive improvement in both groups MMSE performed before and after treatment MMSE and MoCA scale performed before and 1 and 3 months and 1 year after HBOT 8 40 sessions at 2 5 ATA for 120 min five days per week 40 sessions at 2 5 ATA for 80 min per day 5 sessions per week for 8 weeks 20 HBOT sessions 5 sessions per week at 2 5ATA for 80 min per day 20 HBOT sessions 5 sessions per week at 2 5ATA for 80 min per day 8 40 HBOT sessions for 120 min at 2 5 ATA 3 chamber sessions within 24 h 3 HBO sessions 1 day of HBOT performed at 3 then 2 ATA day 2 and 3 at 2 ATA Cognitive improvement patients regained full scores in the MMSE Increased attention visuo spatial memory processes and processing speed No improvement worsening in memory tests Neuropsychological assessment performed after treatment Simple reaction time Choice reaction time Digit span forward and backward Rey Auditory Verbal Learning MMSE Neuropsychological tests were administered immediately after 2 and 6 weeks 6 and 12 months after HBO Digit Span Trail Making Test Digit Symbol Block Design and Story Recall MMSE performed immediately before and 3 months after the HBOT MMSE performed before and after HBOT MMSE performed before and after HBOT 3 6 days 1 session per day HBOT for 60 min at 2 8 ATA Results Cognitive measures HBOT protocol ATA absolute atmosphere CO carbon monoxide HBOT hyperbaric oxygen therapy MMSE Mini Mental State Examination MoCA Montreal Cognitive Assessment DEACMP delayed encephalopathy after acute CO poisoning Zhang et al 2020 Xiang et al 2017a Xiang et al 2017b Chang et al 2010a b Studied group Authors Table 2 Effect of HBOT in carbon monoxide poisoning on cognition in human Neuropsychology Review 13
Neuropsychology Review optimal time window for HBOT a factor that can determine its efficacy in TBI Animal model studies have demonstrated that HBOT has a positive effect on cognitive outcome Kraitsy et al 2014 Lin et al 2012 Zhou et al 2007 found that rats with brain injury treated with HBO 1 h at 1 5 ATA 3hour normobaric oxygen had significant improvement in cognitive recovery HBO research using sham NBO and HBO was used by Harch et al 2007 Authors proved that 80 HBOT sessions performed twice a day for 90 min at 1 5 ATA can significantly improve spatial learning in TBI rats They confirmed their results with showing increase in hippocampus vascular density after hyperbaric oxygen therapy Wang et al investigated the prolonged therapeutic time window of HBOT in animal models Their study involved HBOT administration within 6 h after TBI Their results showed decreased neuronal apoptosis and improved cognitive ability Furthermore they described that multiple HBOT sessions 3 ATA hourly for 3 or 5 days could extend the therapeutic time window up to 48 h post TBI Wang et al 2010 The authors also reported that a treatment initiated within 12 h after injury improved neurologic outcomes compared with a longer window of 24 h They concluded that 72 h after injury there is no significant improvement after single a HBOT session However if the first HBOT starts at 24 h after concussion and continues for 3 or 5 consecutive days there are significant improvements in cognitive deficits Their results suggest that the optimal HBOT paradigm for human studies may be a single treatment initiated within 24 h after the injury followed by treatments for 5 consecutive days Liu et al 2013 investigated the effect and mechanism of HBOT on cognitive functioning in rats Authors suggest that hyperbaric oxygen therapy significantly improves spatial learning and memory skills at rats with traumatic brain injury and the potential mechanism behind those improvements is mediated by metabolic changes and nerve cell restoration in the hippocampus Another research proving neuroprotective effect of HBOT after TBI was conducted by Baratz Goldstein et al 2017 They investigated impact of 4 consecutive days hyperbaric oxygen treatment on mice with traumatic brain injury 2 different time lines 3 h after injury and 7 days post injury They found that mice treated with hyperbaric oxygen showed significant improvement in learning abilities Their results suggest neuroprotective effect of HBOT in TBI with short and long therapeutic window Similar results memory improvement were described by Chen et al 2014 Moreover they described therapeutic effect of hyperbaric oxygen on neuroinflammation apoptosis and oedema after TBI The data from these pre clinic and clinic studies indicate that HBOT is beneficial when it is applied early after an insult or injury Application of HBOT within a therapeutic time window established in preclinical study is an important requirement to ensure treatment efficiency Studies examining effect of HBOT on cognition in animal models of TBI are presented in Table 3 Cifu et al 2014 conducted a randomised blinded clinical study on subjects with persistent post concussion symptoms In their study a randomised controlled trial including 50 military service members suffering mild TBI between 3 and 71 months before HBOT HBOT was assessed at 2 0 ATA All Table 3 Effect of HBOT in traumatic brain injury on cognition in animals Authors Studied group HBOT protocol Cognitive measures Results Zhou et al 2007 23 TBI rats HBO for 1 h at 1 5 ATA Improvements in cognition Harch et al 2007 19 TBI rats Wang et al 2010 6 rats with TBI 80 HBOT twice a day 7 days week 1 5 ATA for 90 min 3 ATA hourly for 3 or 5 days HBOT for 60 min daily at 2 ATA for 1 and 2 weeks Morris water maze post injury days 11 to 15 Morris water maze Liu et al 2013 Baratz Goldstein et al 2017 Chen et al 2014 Zhou et al 2007 Beam balancing test Prehensile traction test 20 rats with TBI Morris water maze test immediately after TBI 1 and 2 weeks of HBOT 15 mice with TBI HBOT session for 4 days for 7 and 30 days after TBI 60 min at 2 ATA Elevated plus maze Y maze Novel object recognition test 9 TBI mice in each test HBOT performed 3 h after Morris water maze postinjury days 14 15 16 and injury for 60 min at 2 17 beam walk task 1 3 7 ATA for 5 days and 14 days post injury 23 TBI rats HBO for 1 h at 1 5 ATA Morris water maze post injury days 11 to 15 ATA absolute atmosphere HBOT hyperbaric oxygen therapy TBI Traumatic Brain Injury 13 Improvement in spatial learning Improved cognitive ability Improvement in spatial learning and memory Improvement in learning abilities Improved motor skills and spatial learning Improvements in cognition
Neuropsychology Review subjects were randomly assigned to one of three groups breathing 10 5 75 or 100 oxygen to mimic normal air at 1 0 ATA 100 oxygen at 1 5 ATA or 100 oxygen at 2 0 ATA respectively HBOT at either 1 5 or 2 0 ATA equivalent had no effect on post concussion symptoms after mild TBI when compared with sham compression However the HBOT effect on cognitive functions was assessed with the self administered Rivermead Post Concussion Symptoms Questionnaire RPQ which is known to display several flaws in implementation and in its ability to accurately reflect test taker experience Moreover interpretation and accuracy of the RPQ can vary widely due to self administration and the various confounding variables involved Indeed it is sensitive to subjective patient memory social desirability stress and other covariates such as personality factors and willingness to reveal problems as are the two other methods Relying completely on the self administration assessments is a weakness of this study Potter et al 2006 Furthermore Walker et al 2014 conducted a randomised double blind and sham control feasibility trial comparing pretreatment and posttreatment conducted in 60 male active duty marines with combat related mild TBI Subjects with PCS that had persisted for 3 to 36 months were randomised to one of three groups receiving preassigned oxygen fractions 10 5 75 or 100 at 2 0 ATA This design led to groups with an oxygen exposure equivalent to breathing surface air 100 oxygen at 1 5 ATA and 100 oxygen at 2 0 ATA respectively Each subject received 40 hyperbaric chamber sessions of 60 min each for 10 weeks Multiple neuropsychological tests of cognitive performance were collected preintervention and 1 week postintervention There were no significant changes in cognitive functioning between groups and pre and post HBOT The authors concluded that HBOT is not useful to treat cognitive balance or fine motor deficits associated with mild TBI and PCS Harch et al 2012 performed an uncontrolled HBOT trial of 16 participants with PCS after blast exposure during military service There was an improvement in both cognitive and psychomotor characteristics The authors reported significant improvement one week after HBOT 40 at 1 5 ATA 5 days per week for 60 min each session in full scale intelligence quotient IQ delayed and working memory executive functions and attention In a randomised trial Wolf et al 2012 studied participants with chronic PCS Their results demonstrated no efficacy in cognitive impairment treatment with HBOT at an exposure pressure of 2 4 ATA for 90 min given once daily for 30 treatments compared to 1 3 ATA air exposure However both groups the control group received treatment with room air at 1 3 ATA improved beyond what would be expected more than 6 months after mild TBI In subsequent study they received similar results no significant difference was observed between air 1 3 ATA and HBO 2 4 ATA although both groups shoved improvement in cognition without statistical significance The Wolf et al 2012 studies were widely criticised for using 1 3 ATA in control group Mychaskiw Stephens 2013 Weaver et al 2013 Actually it should be recognized that 1 3 ATA air and 2 4 ATA oxygen may represent low and high edges of the oxygen dose response curve Hyperbaric physiology indicates that relatively subtle changes in tissue partial oxygen pressure may exert a significant therapeutic effect Mychaskiw Stephens 2013 Weaver et al 2013 Boussi Gross et al 2013 presented a prospective randomised and controlled crossover study of the effect of HBOT with 100 oxygen at 1 5 ATA 5 days per week 60 min each on mild TBI patients at late chronic stage The authors randomly divided the subjects into treated or crossover groups The patients in the treated group were evaluated before and after 40 HBOT sessions Subjects in the control group were evaluated at three times baseline and after 2 and 4 months Neuropsychological examination included assessment of information processing attention memory and executive functions All subjects underwent single photon emission computed tomography examination HBOT induced neuroplasticity and significant brain function improvement in mild TBI patients with prolonged PCS at a late chronic stage years after brain injury There was also improvement in all assessed cognitive functions Moreover changes in single photon emission computed tomography images after treatment indicate that HBOT reactivates neuronal activity in stunned areas that seem normal under computed tomography and magnetic resonance imaging Tal et al 2015 in their study using perfusion magnetic resonance imaging proved that HBOT can significantly increase cerebral blood flow and cerebral blood volume following 50 70 daily hyperbaric sessions 5 days a week each session consisted of 60 min of exposure to 100 oxygen at 1 5 ATA There was also significant cognitive improvement in patients post TBI The mean time from the acute injury was 10 3 3 2 years The most prominent improvements were seen in information processing speed visual spatial processing and motor skills indices The increased perfusion to the dysfunctional tissue and the significant cognitive improvement suggest that impaired tissue perfusion may serve as a rate limiting factor for regeneration and neuroplasticity even years after the acute injury The authors concluded that that appropriate biological trigger can induce neuroplasticity months to years after the acute injury In a subsequent study Tal et al 2017 evaluated diffusion tensor imaging changes before and after HBOT of prolonged PCS HBOT was initiated 6 months to 27 years 10 3 3 2 years from injury for 60 daily hyperbaric sessions 5 days per week with sessions consisting of 90 min of exposure to 100 oxygen at 2 ATA The authors found an increase in fractional anisotropy and a decrease in mean diffusivity after HBOT together with cognitive function improvement of patients in the late chronic stage of TBI 13
Their results suggest that HBOT can induce brain microstructure recovery with significant improvement in memory executive functions and information processing speed They concluded that HBOT can improve the integrity of brain fibres a phenomenon that correlates with improved cognitive functioning It should be kept in mind however that quantitative validation of diffusion tensor imaging pathologic metrics remains very limited Winklewski et al 2018 Churchill et al Churchill et al 2016 examined effect of HBOT on information processing speed after mTBI In their study investigators measured speed of processing at baseline 6 and 13 weeks in military personnel with mTBI Subjects were randomized to 40 sessions of air 1 2 ATA or HBOT 1 5 ATA They found no significant changes in reaction time between HBO or air Furthermore Shandley and colleagues found that HBOT 90 min at 2 4 ATA correlates with stem cell mobilization as well as increased neuropsychological performance comparing to 90 min air at 1 3 ATA Authors suggest that stem cell mobilization may be required for cognitive improvement in TBI population Hadanny et al 2018 demonstrated the neurotherapeutic effects of HBOT for chronic TBI The study included 154 subjects 42 7 14 6 years with documented TBI 0 3 33 years mean 4 6 5 8 median 2 75 years prior to HBOT The HBOT protocol comprised 40 70 daily hyperbaric sessions 5 days a week Each session involved exposure to 100 oxygen at 1 5 2 ATA The authors confirmed that HBOT induced significant improvement in memory executive functions information processing speed and global cognitive scores Weaver et al 2012 proposed the design of randomised study to evaluate the efficacy and utility of HBOT for American combatants with PCS Based on this design authors conducted clinical trial They examined executive functions processing speed memory and learning of 71 military service members with mTBI 35 with PTSD who were randomly administered to HBO or air 40 HBO sessions at 1 5 ATA vs air at 1 2 ATA for 60 min Authors found that after 13 weeks HBOT improved post concussive and PTSD symptoms cognitive processing speed sleep quality and balance function especially in individuals with PTSD Although changes did not persist beyond six months Weaver et al 2018 Research on effect of HBOT on cognition in traumatic brain disorders in humans are presented in Table 4 Currently the results of HBOT in clinical TBI trials are controversial and the efficiency of HBOT in TBI has not been well established First the optimal time window for HBOT administration must be determined to ensure its efficacy in treating TBI Second objective and precise neuropsychological assessment methods are another challenge in the evaluation of the efficacy of HBOT in TBI patients Third heterogeneity in patients and HBOT paradigms pressure frequency 13 Neuropsychology Review length of treatment course partly affect or determine the outcome There have been variations in patients age and in the severity and nature of the injury in the studies Future trials of HBOT for PCS should consider measuring outcomes with standardised neuropsychological methods and at longer intervals postintervention or in combination with rehabilitation therapy to determine potential delayed or priming effects HBOT and Poststroke Cognitive Disturbances Stroke is a result of a blocked artery or a ruptured blood vessel It leads to an interruption in cell homeostasis and symptoms such as loss of speech and loss of motor function It is a major cause of disability and mortality among adults with long term impairments in the physical emotional and cognitive state of survivors Robinson 2006 Neuropsychological disturbances after stroke are very common they involve multiple cognitive deficits that lead to a decline in everyday functioning and in social functioning Godefroy Bogousslavsky 2007 The main therapeutic targets are the regions surrounding the focal site of injury where the tissue is at high risk of disruption but not irreparably damaged thus there is still the potential to salvage these neurons Baron 2001 Lo et al 2003 Singhal 2007 Cell death and reduced neuronal activity caused by an ischaemic event can lead to excitotoxicity oxidative stress inflammation and apoptosis all of which are pathways where hypoxia plays a key role Lo et al 2003 Therefore increased oxygenation has been considered as a potential treatment for stroke this treatment may lead to tissue repair and the generation of new synaptic connections Golden et al 2002 Neubauer James 1998 Therapy and neuropsychological rehabilitation programmes are valuable for improving cognition at early stages but they usually provide only partial recovery from symptoms To date there is no efficient neuropsychological rehabilitation programs available for late chronic stages Rajeswaran 2013 Ricker Callahan 2000 Current concepts of the pathophysiology of stroke provide a rationale for using HBOT in its management Conventional methods of stroke treatment and their functional consequences are not satisfactory and the outcomes remain controversial There are only a few experimental animal studies and uncontrolled human trials that have shown the effectiveness and safety of HBOT after stroke Clinical observations and basic research data suggest that HBOT may be a useful and effective treatment option in the management of acute stroke but more studies are needed to clarify its clinical utility S nchez 2013 The use of HBOT as a treatment following stroke was first raised 50 60 years ago Hart Strauss 2003 Hart Thompson 1971 Despite decades of interest studies that have investigated the effects of HBOT following a stroke have produced mixed results Bennett et al 2014 Freiberger et al 2016 Helms et al
25 TBI patients Wolf et al 2015 56 male TBI patients with PCS 25 TBI patients Wolf et al 2012 Boussi Gross et al 2013 16 male TBI patients Harch et al 2012 Walker et al 2014 Results Significant improvement in all cognitive measures No effect of HBOT No effect of HBOT Improvement in delayed memory working memory Stroop test Rivermead Post Concussion Questionnaire 16 No significant changes Rivermead Post Concussion Question No significant changes naire 16 Cognitive measures Wechsler Test of Adult Reading Conners Continuous Performance Test II Paced Auditory Serial Addition Test Halsted Reitan Trail Making Test A B Stroop test California Verbal Learning Test II Wechsler Adult Intelligence Scale III select items digit symbol coding digit span letter number sequencing symbol search and arithmetic Delis Kaplan Executive Function Systems version of the Controlled Oral Word Association Test single letter and category items Benton Visual Memory Test Revised Test of Memory Malingering 40 sessions of HBOT at 1 5 Green Word Memory Test Effort ATA 60 min in twice a day 30 days Wechsler Test of Adult Reading Rivermead Post Concussion Symptom Questionnaire Wechsler Adult Intelligence Scale IV Test of Variables of Attention Stroop Test Finger Tapping Test Grooved Pegboard Wechsler Memory Scale IV Rivermead Paragraph Memory 30 HBOT at 2 4 ATA and 1 3 ATA air Immediate Post Concussion Assesssessions for 90 min ment and Cognitive Testing Post Traumatic Disorder Check List 30 HBOT at 2 4 ATA and 1 3 ATA air Immediate Post Concussion Assesssessions for 90 min ment and Cognitive Testing Post Traumatic Disorder Check List 40 HBOT sessions 5 days week Mindstreams Verbal memory Non60 min with 100 oxygen at 1 5 ATA vernal memory Go No Go test Stroop test Staged information processing test Catch game 61 male Marines with mTBI and PCS 40 HBOT sessions 1 daily sham or 100 oxygen at 1 5 ATA or 100 oxygen at 2 ATA 40 male Marines with mTBI 40 HBOT for 60 min at 1 5ATA or 2ATA Cifu et al 2014 HBOT protocol Studied group Authors Table 4 Effect of HBOT in traumatic brain injury on cognition in human Neuropsychology Review 13
13 10 TBI patients 15 TBI patients 23 TBI patients 15 TBI patients Tal et al 2015 Tal et al 2017 Churchill et al 2016 Shandley et al 2017 Amir Hadanny et al 2018 154 TBI patients Studied group Authors Table 4 continued Cognitive measures 60 HBOT sessions 5 week at 1 5 ATA NeuroTrax Verbal for 60 min Memory Non Verbal Memory Go No Go Problem Solving Stroop test Finger Tapping Catch Game Staged Information Processing Speed Verbal Function and Visual Spatial Processing 60 daily HBOT sessions 5 week for NeuroTrax Verbal 90 min at 2 ATA Memory Non Verbal Memory Go No Go Problem Solving Stroop test Finger Tapping Catch Game Staged Information Processing Speed Verbal Function and Visual Spatial Processing Automated Neuropsychological 40 HBOT sessions at 1 5 ATA for 60 min Assessment Metrics Simple Reaction Time and Procedural Reaction Time subtests Immediate Post Concussion Assess30 HBOT sessions at 2 4 ATA for 90 min ment and Cognitive Testing BrainCheckers 40 70 daily HBOT sessions NeuroTrax Verbal 5 week for 60 90 min at 1 5 2 ATA Memory Non Verbal Memory Go No Go Problem Solving Stroop test Finger Tapping Catch Game Staged Information Processing Speed Verbal Function and Visual Spatial Processing HBOT protocol Improvement in memory and attention Increased cognitive performance No significant changes Improvement in the memory executive functions information processing speed and global cognitive scores Improvement in information processing speed visual spatial processing and motor skills Results Neuropsychology Review
ATA absolute atmosphere HBOT hyperbaric oxygen therapy PCS Post Concussion Syndrome Improvement in post concussive Automated Neuropsychological and PTSD symptoms cognitive processAssessment Metrics ing speed sleep quality California Verbal Learning Test II Brief Visuospatial Memory Test Revised Test of Memory Malingering Wechsler Adult Intelligence Scale IV digit span and processing speed Wechsler Test of Adult Reading Stroop color and word test Controlled oral word association test Trail making test parts A and B Grooved pegboard Trait Anger Expression Inventory 36 TBI patients Weaver et al 2018 40 HBO sessions at 1 5 ATA for 60 min Studied group Authors Table 4 continued HBOT protocol Cognitive measures Results Neuropsychology Review 2005 Rehabilitation of stroke patients is one aspect that should be planned during the first few months following stroke Thus long term follow up studies are required to determine whether such measures would reduce the chronic disability attached to impaired cognition in stroke in stroke patients First clinical researches in this field were made by Sarno and Sarno Sarno et al 1972a b Authors investigated the effect of HBOT on language skills disrupted after stroke First study included 16 left hemisphere stroke patients second 32 stroke patients 16 with left sided damage Patients underwent neuropsychological examination with detailed assessment of various verbal processes before chamber treatment and after every session Each patient participated in two double blinded conditions HBOT performed at 2 ATA of 100 oxygen or sham 10 5 oxygen both for 90 min with random order Authors found no significant changes in neuropsychological tests results after exposure to oxygen Boussi Gross et al 2015 presented a retrospective analysis of the effects of HBOT on memory impairments in poststroke patients during the late chronic unremitting stage The HBOT protocol consisted of 40 to 60 daily sessions 5 days per week 90 min each 100 oxygen at 2 ATA Their data showed statistically significant improvements in memory functions in the majority of patients These neuropsychological findings were in good agreement with metabolic brain changes assessed by single photon emission computed tomography brain imaging Imaging analysis identified the brain regions associated with the memory impairments and improvements perirhinal cortex and its activation correlated with clinical improvement in the delayed memory measures improvement in verbal and nonverbal delayed memory abilities with the change in activation in the left and right perirhinal cortex respectively These results are consistent with previous reports that HBOT induces neuroplasticity effects at late chronic stage although these studies lacked a control group Nevertheless these and previous studies have provided convincing evidence that HBOT can induce neuroplasticity at chronic poststroke stages in areas with metabolic dysfunction which if relevant to memory function in the brain can improve after HBOT Boussi Gross et al 2013 Efrati et al 2013 Hadanny et al 2015 firstly examined effect of HBOT on patients suffering from anoxic brain damage caused by cardiac arrest Patients received 60 daily HBOT sessions of 100 oxygen at 1 5 ATA for 60 min Neuropsychological measures were compared with single photon emission computed tomography results Authors found significant improvement in memory attention and executive functions Those changes correlated with increased brain activity in relevant brain areas assessed by single photon emission computed tomography imaging Their further retrospective research 13
focus was put on 162 stroke patients 87 in left hemisphere 121 ischemic They found that HBOT 40 60 sessions 90 min of 100 oxygen at 2 ATA had significant effect on all cognitive domains Authors concluded that hyperbaric oxygen therapy can be successful treatment even in late chronic stage of post stroke patients Hadanny et al 2020 In one of the most recent studies Rosario et al 2018 measured the impact of HBOT across a number of cognitive domains including speech language skills general cognition memory and emotional behavioural impairments The authors assessed functional abilities over a 3 month period for 6 subjects who underwent two 4 week periods of HBOT commenced over 6 months after a stroke HBOT comprised 20 total treatments of 100 at 2 0 ATA for 60 min for 4 weeks on weekdays There were significant improvements in memory and executive function after oxygen therapy Despite a small sample size the authors concluded that their findings support the idea of HBOT as a potential intervention following stroke Researches on effect of HBOT on cognition after ischemia stroke are presented in Table 5 Clearly additional larger prospective randomised trials on the effect of HBOT on cognitive impairment during acute and delayed poststroke periods should be conducted Moreover future studies should widen the assessment of the HBOT effects on different cognitive functions because most of the existing studies focus on memory abilities Additional study limitations relate to the HBOT protocol Even though they have shown similar significant beneficial effect studies that have evaluated HBOT in stroke management have used different treatment protocols The exact HBOT protocol that will induce maximal neuroplasticity with minimal side effects must be determined Bennet et al 2014 reported that when taken together the existing literature does not indicate that HBOT is an effective intervention in the acute phase following an ischaemic stroke Nevertheless the failure of some clinical stroke trials that have utilised HBOT is probably linked to factors such as delayed time to therapy inadequate sample size and the use of excessive chamber pressures Singhal 2007 Further research could focus on investigating HBOT effects on cognitive functions on stroke patients receiving thrombolysis or thrombectomy treatment before oxygen therapy HBOT Usage for Cognitive Ageing and Neurodegenerative Disorders Dementia is a condition characterised by increasing several cognitive deficits such as loss of memory problems with speech and understanding and visuo spatial disruption According to the 2003 World Health Organization WHO World Health Report dementia causes 11 2 more years lived with disability than cardio and cerebrovascular diseases and all forms of cancer in people aged 60 years and older There are currently around 36 million dementia 13 Neuropsychology Review patients worldwide It is anticipated that the number of dementia cases will increase in the subsequent years and will reach 81 1 million by the year 2040 Ferri et al 2005 Research on HBOT for dementia has mainly focussed on animal experiments Table 6 The first investigation of HBOT in the elderly population was performed by Jacobs et al 1969 They reported improved cognitive functioning in 13 elderly patients with chronic organic brain syndrome after exposure to hyperbaric oxygen 30 sessions twice a day with 100 oxygen at 2 5 ATA Five control subjects exposed to a neutral air mixture failed to show improvement Over the next six years five other research reports were published Three confirmed Jacobs original observation Edwards Hart 1974 Jacobs et al 1972 Raskin et al 1978 while two did not Goldfarb et al 1972 Thompson et al 1976 The study by Goldfarb et al 1972 was performed on 10 patients mean age 74 years with cognitive decline All subjects underwent 40 to 58 h of exposure to 100 oxygen at 2 5 ATA in two sessions per day 90 min each Compression and decompression time of each individual chamber session was about 110 min Neuropsychological examination was performed before and after 15 days of treatment There were no significant improvements in cognitive outcome of subjects Moreover Thompson et al 1976 included 21 subjects with dementia 50 80 years old 13 with diagnosis of cortical atrophy 8 cerebrovascular disease and 4 control subjects HBOT consisted of the same procedure as Jacobs et al 1969 There were no significant differences between the experimental and control subjects Jacobs et al 1972 although the severity of dementia in subjects in both studies was different The patients in the Jacobs study had less cognitive deterioration The interest in treating dementia with HBOT has grown in recent years Alzheimer disease is the most common form of dementia It is characterised by progressive cognitive impairment and psychobehavioural disturbances In a rodent model of Alzheimer disease Shapira et al 2018 found that HBOT can improve cognitive function by reducing neuroinflammation The authors conducted their study with 6 mice 3 HBO treated 3 nontreated For animals in the treated group HBOT was administered as 100 oxygen at a pressure of 2 ATA for 60 min daily for 14 consecutive days The effects of HBOT on cognitive functions memory and behaviour in mice were evaluated using a series of behavioural tests Cognitive tests were performed during the 7 days preceding sacrifice with a 24 h delay after the last HBOT or control treatment and a 48 h delay after the last task to reduce stress The authors concluded that HBOT can ameliorate Alzheimer disease pathology and behavioural deficits in a transgenic mouse model of Alzheimer disease Furthermore in another rodent model of Alzheimer disease Zhao et al 2017 proved that HBOT can reduce hippocampal neuronal
16 left hemisphere stroke patients 32 stroke patients 16 left sided damage Sarno et al 1972b Sarno et al 1972a 7 stroke patients 162 stroke patients 87 in left hemisphere 121 ischemic Rosario et al 2018 Hadanny et al 2020 Cognitive measures 1 session of HBO for 90 min at 2 ATA Token Test Functional Communication Profile 1 session of HBO for 90 min at 2 ATA Visual Cancellation Letters Auditory Digit Span Block Design Purdue Pegboard Two Point Tactile Thresholds Motor Impersistence Token Test Functional Communication Profile 40 60 daily HBOT sessions 5 week NeuroTrax immediate verbal memory for 90 min at 2 ATA Delayed verbal memory Immediate nonverbal memory Delayed nonverbal memory Total memory index 60 HBOT sessions 5 per week for NeuroTrax Verbal Memory 60 min at 1 5 ATA Non Verbal Memory Go No Go task Stroop test Finger Tapping Catch Game Staged Information Processing Speed Verbal Function and Visual Spatial Processing 20 HBOT sessions for 60 min at 2 ATA Boston Naming Test Reading Comprehension Battery for Aphasia Porch Index of Communication Ability MMSE California Verbal Learning Test Grooved Pegboard Test Trial Making Test A B Controlled Oral Word Association Test Wechsler Abbreviated Scale of Intelligence block design Weschler Memory Scale Delis Kaplan Executive Function System 40 60 HBOT sessions for 90 min of NeuroTrax 100 oxygen at 2 ATA memory executive function visuospatial skills verbal function attention information processing speed and motor skills HBOT protocol ATA absolute atmosphere HBOT hyperbaric oxygen therapy MMSE Mini Mental State Examination 11 patients with anoxic brain dame after cardiac arrest Hadanny et al 2015 Boussi Gross et al 2015 91 stroke patients Studied group Authors Table 5 Effect of HBOT on cognition after stroke Improvement in all cognitive domains Improvement in speech language memory processing speed and executive functions Improvement in memory attention and executive functions Improvement in all memory measures No improvement No improvement Results Neuropsychology Review 13
Neuropsychology Review Table 6 Effect of HBOT on cognition in animal models of neurodegenerative disease Authors Studied group Shapira et al 2018 14 old triple transgenic mice and 14 non transgenic Zhao et al 2017 8 rats with AD Zhang et al 2010 10 VaD rats HBOT protocol Cognitive measures Results HBOT 100 oxygen at 2 ATA for 60 min daily for 14 consecutive days 5 HBO sessions at 2 ATA for 60 min 10 HBOT sessions for 90 min at 2 ATA Y maze Open field test Novel object recognition test Morris water maze task Improvement in cognition and behaviour measures Improvement in learning and memory The one way avoidance test Improvement of learning and memory AD Alzheimer Disease VaD Vascular Dementia ATA absolute atmosphere HBOT hyperbaric oxygen therapy apoptosis and thus improve cognitive function The authors examined 24 rats 3 groups 8 normal 8 Alzheimer disease 8 Alzheimer disease HBO that underwent the experimental procedure The Alzheimer disease HBOT group received six HBOT sessions 2 ATA for 60 min while the normal and Alzheimer disease groups were placed in hyperbaric chambers without compression or decompression treatment The authors concluded that hyperbaric treatment improves learning and memory skills by inhibiting dendritic spine loss and reducing neuronal apoptosis astrocyte activation and tumour necrosis factor TNF production in the hippocampus of rats with Alzheimer disease The second most common form of dementia is vascular dementia accounting for approximately 30 of all cases of dementia Kalaria et al 2008 Vascular dementia is group of syndromes based on varying vascular mechanisms such as multiple infarcts small vessel ischaemic disease strategically placed infarcts hypoperfusion and haemorrhage Alzheimer disease with cerebrovascular disease hereditary vascular dementia or cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy Brien et al 2003 To date no effective treatments have been approved for established vascular dementia Current treatment methods focus mainly on the reduction of risk factors and slowing the progression of the clinical outcome Erkinjuntti et al 2004 Moorhouse Rockwood 2008 Sorrentino et al 2008 A study on animal models of vascular dementia demonstrated that HBOT 2 ATA for 120 min pressure boost for 15 min steady pressure for 90 min decompression for 15 min once a day for 10 continuous days improves the blood supply and promotes neurogenesis in the piriform cortex Zhang et al 2010 These observations suggest possible benefits of HBOT for vascular dementia in humans Cerebrovascular disease includes a variety of conditions that affect the brain and the cerebral circulation which can lead to vascular dementia Ku ma et al 2018 Vila et al 2005 examined possible reversible effect of HBOT on cognitive decline in cerebrovascular disease Their study included 26 subjects with mild to moderate leukoaraiosis 13 18 received 10 sessions of HBOT for 45 min at 2 5 ATA 8 air sessions at 1 1 ATA After treatment subjects receiving hyperbaric oxygen showed significant improvement in motor and cognitive scales compared to control group Wang and colleagues Wang et al 2009 examined 64 vascular dementia patients 32 HBOT 32 control subjects who underwent 12 weeks of HBOT sessions 97 oxygen administered at 2 0 ATA for 60 min a day for 24 consecutive days a session six days of rest in between sessions as an adjuvant treatment to donepezil Patients who received oxygen treatment showed better cognitive function compared to the control group treated with donepezil alone measured either by the MMSE or by Hasegawa s Dementia Rating Scale Similar methodology was used by Xu et al 2019 Authors prospectively analysed 158 vascular dementia patients who were randomized in two groups HBO treatment 12 weeks of HBOT sessions administered at 2 ATA for 60 min and control group both treated with donepezil hydrochloride Authors concluded that HBO therapy can improve cognitive functions in patients with vascular dementia In one of the most recent reviews in this field You et al 2019 described HBOT as effective and safe complementary therapy for the treatment of vascular dementia However more research is needed because the exact mechanism of this treatment modality remains unclear Given that HBOT has shown usefulness in treating a variety of conditions the possible efficacy for treating Alzheimer disease and vascular dementia should be considered in experimental and preliminary clinical studies Effect of hyperbaric oxygen therapy on dementia is presented in Table 7 Future research should consider more detailed cognitive assessment The current methodology is based mostly on brief neuropsychological batteries and tests for example the MMSE and MoCA Furthermore research must find the most effective HBOT protocol and include more subject and control groups Moreover multimodal assessment of positron emission tomography and magnetic resonance imaging networks could provide additional information on the impact of HBOT on neurodegenerative diseases
32 VaD patients 79 VaD patients Wang et al 2009 Xu et al 2019 12 weeks of HBOT sessions 97 of oxygen at 2 ATA for 60 min 12 weeks of HBOT sessions 5 week 100 of oxygen at 2 ATA for 60 min 10 HBOT sessions for 45 min at 2 5 ATA Wechsler Memory Scale BenderGestalt Memory Ohase Tien s Organic Integrity Test Wechsler Memory Scale BenderGestalt Memory Phase Tien s Organic Integrity Test Wechsler Memory Scale Benton Visual Retention Test Ravesn s Progressive Matrices Hooper Visual Organization Test Tien s Organic Tntegrity Test Word Naming Test Finger Tapping MMSE Gait and Equilibrium Scale Unified Parkinson s Disease Rating Scale Barthel Scale MMSE or Hasegawa s Dementia Rating Score MMSE Cognitive measures Improvement in cognition MMSE score Improvement in cognition Improvement in all scales motor and cognition No significant improvement No significant improvement Improvement in cognition Results ATA absolute atmosphere HBOT hyperbaric oxygen therapy VaD Vascular Dementia CVD Cerebrovascular Disease MMSE MiniMental State Examination 18 CVD patients Vila et al 2005 Thompson et al 1976 21 subjects with dementia 13 with cortical atrophy 8 cerebrovascular disease 10 patients with cognitive decline Goldfarb et al 1972 40 to 58 h HBOT with 100 oxygen at 2 5 ATA in two sessions per day 90 min each 30 HBOT sessions twice a day with 100 oxygen at 2 5 ATA 13 elderly patients with chronic organic 30 HBOT sessions twice a day with brain syndrome 100 oxygen at 2 5 ATA Jacobs et al 1969 HBOT protocol Studied group Authors Table 7 Effect of HBOT on dementia Neuropsychology Review 13
Conclusions To the best of our knowledge this review provides the first state of the art systematic summary of research focused on the use of HBOT in various neurological conditions Existing clinical data can be conflicting due to several inherent procedural issues such as the use of non objective endpoints the lack of appropriate brain imaging as part of the inclusion criteria inappropriate placebo of a hyperbaric environment as well as the inclusion of patients and lack of control groups Clearly larger randomised trials that evaluate the effect of HBOT on cognitive impairment should be conducted Current HBOT studies have reported controversial results with regard to the efficiency of HBOT in various neurological conditions with cognitive disturbance outcome Some study limitations relate to HBOT itself There is still no agreement about an HBOT protocol specifically the appropriate air pressure and the time and repetition of treatment sessions The exact HBOT protocol for each neurological state which will induce maximal neuroplasticity and functional improvement with minimal side effects must be determined Future studies should widen the assessment of HBOT effects on different cognitive functions because most of the existing investigations have focussed on single processes Furthermore more objective and precise neuropsychological assessment methods are needed to evaluate the efficacy of HBOT for neuropsychological deficits To reach an agreement about the effectiveness of HBOT for neuropsychological disorders research needs to focus more on homogeneity of the included subjects The current studies were conducted using heterogeneous groups of patients with wide variations in age severity and nature of the brain damage Thus there is a need for longitudinal studies to verify whether the administration of a more extensive series of HBOT sessions will lead to longer lasting improvements in cognitive functioning Assuming that the methodological issues described in this review can be properly addressed and evaluated HBOT may have potential for the treatment of neuropsychological deficits in a wide range of neurological states Funding The study was supported by Medical University of Gda sk Declarations Conflict of Interest The authors declare that they have no conflict of Interest Open Access This article is licensed under a Creative Commons Attribution 4 0 International License which permits use sharing adaptation distribution and reproduction in any medium or format as long as you give appropriate credit to the original author s and the source provide a link to the Creative Commons licence and indicate if changes were made The images or other third party material in this article are 13 Neuropsychology Review included in the article s Creative Commons licence unless indicated otherwise in a credit line to the material If material is not included in the article s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use you will need to obtain permission directly from the copyright holder To view a copy of this licence visit http creat iveco mmons org licen ses by 4 0 References Annane D Chadda K Gajdos P Jars Guincestre M C Chevret S Raphael J C 2011 Hyperbaric oxygen therapy for acute domestic carbon monoxide poisoning Two randomized controlled trials Intensive Care Medicine 37 3 486 492 https doi org 10 1007 s00134 010 2093 0 Baratz Goldstein R Toussia Cohen S Elpaz A Rubovitch V Pick C G 2017 Immediate and delayed hyperbaric oxygen therapy as a neuroprotective treatment for traumatic brain injury in mice Molecular and Cellular Neuroscience 83 74 82 https doi org 10 1016 j mcn 2017 06 004 Baron J C 2001 Perfusion thresholds in human cerebral ischemia Historical perspective and therapeutic implications Cerebrovascular Diseases 11 SUPPL 1 2 8 https doi org 10 1159 00004 9119 Barrett K F Masel B Patterson J Scheibel R S Corson K P Mader J T 2004 Regional CBF in chronic stable TBI treated with hyperbaric oxygen Undersea Hyperbaric Medicine Journal of the Undersea and Hyperbaric Medical Society Inc 31 4 395 406 http w ww n cbi n lm n ih g ov pubmed 15686 271 Bennett M H Weibel S Wasiak J Schnabel A French C Kranke P 2014 Hyperbaric oxygen therapy for acute ischaemic stroke In Cochrane Database of Systematic Reviews Vol 2014 Issue 11 John Wiley and Sons Ltd https doi org 10 1002 14651 858 CD004 954 pub3 Betzen C White R Zehendner C M Pietrowski E Bender B Luhmann H J Kuhlmann C R W 2009 Oxidative stress upregulates the NMDA receptor on cerebrovascular endothelium Free Radical Biology and Medicine 47 8 1212 1220 https doi org 10 1016 j freer adbio med 2009 07 034 Bhatt S Puli L Patil C R 2020 Role of reactive oxygen species in the progression of Alzheimer s disease Drug Discovery Today 00 00 https doi org 10 1016 j drudis 2020 12 004 Bi M J Sun X N Zou Y Ding X Y Liu B Zhang Y H Guo D D Li Q 2017 N Butylphthalide improves cognitive function in rats after carbon monoxide poisoning Frontiers in Pharmacology 8 FEB 1 12 https doi org 10 3389 fphar 2017 00064 Birmingham C M Hoffman R S 2011 Hyperbaric oxygen therapy for acute domestic carbon monoxide poisoning two randomized controlled trials Intensive Care Medicine 37 7 1218 1218 https doi org 10 1007 s00134 011 2195 3 Bitterman N Bitterman H 1998 L arginine NO pathway and CNS oxygen toxicity Journal of Applied Physiology 84 5 1633 1638 https doi org 10 1152 jappl 1998 84 5 1633 Bliznyuk A Hollmann M Grossman Y 2020 The Mechanism of NMDA Receptor Hyperexcitation in High Pressure Helium and Hyperbaric Oxygen Frontiers in Physiology 11 August 1 8 https doi org 10 3389 fphys 2020 01057 Boraxbekk C J Salami A W hlin A Nyberg L 2016 Physical activity over a decade modifies age related decline in perfusion gray matter volume and functional connectivity of the posterior default mode network A multimodal approach NeuroImage 131 133 141 https doi org 10 1016 j neuro image 2015 12 010 Boussi Gross R Golan H Fishlev G Bechor Y Volkov O Bergan J Friedman M Hoofien D Shlamkovitch N
Neuropsychology Review Ben Jacob E Efrati S 2013 Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury Randomized prospective trial PLoS One 8 11 https doi org 10 1371 journ al pone 00799 95 Boussi Gross R Golan H Volkov O Bechor Y Hoofien D Beeri M S Ben Jacob E Efrati S 2015 Improvement of memory impairments in poststroke patients by hyperbaric oxygen therapy Neuropsychology 29 4 610 621 https doi org 10 1037 neu00 00149 Brien J T O Erkinjuntti T Reisberg B Roman G Sawada T Pantoni L Bowler J V Ballard C Decarli C Gorelick P B Rockwood K Burns A Gauthier S Dekosky S T 2003 Vascular cognitive impairment Lancet Neurol 2 2 89 98 https d oi o rg 1 0 1 016 s 1474 4 422 03 00305 3PMID 12849265 Bruno A Wagner W Orrison W W 1993 Clinical outcome and brain MRI four years after carbon monoxide intoxication Acta Neurologica Scandinavica 87 3 205 209 https doi org 10 1111 j 1600 0404 1993 tb041 02 x Burgess N Maguire E A O Keefe J 2002 The human hippocampus and spatial and episodic memory In Neuron Vol 35 Issue 4 pp 625 641 Cell Press https doi org 10 1016 S0896 6273 02 00830 9 Cai F Wang F Lin F K Liu C Ma L Q Liu J Wu W N Wang W Wang J H Chen J G 2008 Redox modulation of long term potentiation in the hippocampus via regulation of the glycogen synthase kinase 3 pathway Free Radical Biology and Medicine 45 7 964 970 https d oi org 10 1016 j freer adbio med 2008 06 014 Camporesi E M 2014 Side effects of hyperbaric oxygen therapy Undersea and Hyperbaric Medicine 41 3 253 257 Chang C C Chang W N Lui C C Wang J J Chen C F Lee Y C Chen S S Lin Y T Huang C W Chen C C C Chang M P Chang W Chen S 2010a Longitudinal study of carbon monoxide intoxication by diffusion tensor imaging with neurospsychiatric correlation Journal of Psychiatry Neuroscience 35 2 https doi org 10 1503 jpn 090057 Chang D C Lee J T Lo C P Fan Y M Huang K L Kang B H Hsieh H L Chen S Y 2010b Hyperbaric oxygen ameliorates delayed neuropsychiatric syndrome of carbon monoxide poisoning Undersea Hyperbaric Medicine 37 1 23 33 http www ncbi nlm nih gov pubmed 20369 650 Chen X Duan X S Xu L J Zhao J J She Z F Chen W W Zheng Z J Jiang G D 2014 Interleukin 10 mediates the neuroprotection of hyperbaric oxygen therapy against traumatic brain injury in mice Neuroscience 266 235 243 https doi org 10 1016 j neuro scien ce 2013 11 036 Chen Z Ni P Lin Y Xiao H Chen J Qian G Ye Y Xu S Wang J Yang X 2010 Visual pathway lesion and its development during hyperbaric oxygen treatment A bold fMRI and DTI study Journal of Magnetic Resonance Imaging 31 5 1054 1060 https doi org 10 1002 jmri 22142 Chiu W T LaPorte R E 1993 Global Spine and Head Injury Prevention SHIP Project The Journal of Trauma 35 6 969 970 http www ncbi nlm nih gov pubmed 82640 06 Choi S 1983 Delayed Neurologic Sequelae in Carbon Monoxide Intoxication Archives of Neurology 40 7 433 435 https doi org 10 1001 archn eur 1983 04050 07006 3016 Churchill S Scott Miller R Deru K Wilson S H Weaver L K 2016 Simple and procedural reaction time for mild traumatic brain injury in a hyperbaric oxygen clinical trial Military Medicine 181 5 40 44 https doi org 10 7205 MILMED D 15 00148 Churchill S Weaver L K Deru K Russo A A Handrahan D Orrison W W Foley J F Elwell H A 2013 A prospective trial of hyperbaric oxygen for chronic sequelae after brain injury HYBOBI Undersea and Hyperbaric Medicine 40 2 165 193 Cifu D X Hart B B West S L Walker W Carne W 2014 The effect of hyperbaric oxygen on persistent postconcussion symptoms Journal of Head Trauma Rehabilitation 29 1 11 20 https doi org 10 1097 HTR 0b013 e3182 a6aaf0 Clark K B Naritoku D K Smith D C Browning R A Jensen R A 1999 Enhanced recognition memory following vagus nerve stimulation in human subjects Nature Neuroscience 2 1 94 98 https doi org 10 1038 4600 Ferri C P Prince M Brayne C Brodaty H Fratiglioni L Ganguli M Hall K Hasegawa K Hendrie H Huang Y Jorm A Mathers C Menezes P R Rimmer E Scazufca M 2005 Global prevalence of dementia a Delphi consensus study Lancet 366 2112 2117 Daly S Thorpe M Rockswold S Hubbard M Bergman T Samadani U Rockswold G 2018 Hyperbaric Oxygen Therapy in the Treatment of Acute Severe Traumatic Brain Injury A Systematic Review In Journal of Neurotrauma Vol 35 Issue 4 pp 623 629 Mary Ann Liebert Inc https doi org 10 1089 neu 2017 5225 Deng Z Chen W Jin J Zhao J Xu H 2018 The neuroprotection effect of oxygen therapy A systematic review and meta analysis In Nigerian Journal of Clinical Practice Vol 21 Issue 4 pp 401 416 Medknow Publications https doi org 10 4103 njcp njcp_ 315_ 16 Di Piero V Cappagli M Pastena L Faralli F Mainardi G Di Stani F Bruti G Coli A Lenzi G L Gagliardi R 2002 Cerebral effects of hyperbaric oxygen breathing A CBF SPECT study on professional divers European Journal of Neurology 9 4 419 421 https doi org 10 1046 j 1468 1331 2002 00436 x Edwards A E Hart G M 1974 Hyperbaric Oxygenation and the Cognitive Functioning of the Aged Journal of the American Geriatrics Society 22 8 376 379 https d oi org 10 1111 j 1532 5415 1974 tb048 45 x Efrati S Ben Jacob E 2014a Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Review of Neurotherapeutics 14 3 233 236 https doi org 10 1586 14737 175 2014 884928 Efrati S Ben Jacob E 2014b Reflections on the neurotherapeutic effects of hyperbaric oxygen In Expert Review of Neurotherapeutics Vol 14 Issue 3 pp 233 236 https d oi org 10 1586 14737 175 2014 884928 Efrati S Fishlev G Bechor Y Volkov O Bergan J Kliakhandler K Kamiager I Gal N Friedman M Ben Jacob E Golan H 2013 Hyperbaric Oxygen Induces Late Neuroplasticity in Post Stroke Patients Randomized Prospective Trial PLoS One 8 1 https doi org 10 1371 journ al pone 00537 16 Erkinjuntti T Rom n G Gauthier S Feldman H Rockwood K 2004 Emerging Therapies for Vascular Dementia and Vascular Cognitive Impairment Stroke 35 4 1010 1017 https doi org 10 1161 01 STR 00001 20731 88236 33 Ernst A Zibrak J D 1998 Carbon Monoxide Poisoning New England Journal of Medicine 339 22 1603 1608 https doi org 10 1056 NEJM1 99811 26339 2206 Fischer B Palkovic S Holling M Wolfer J Wassmann H 2010 Rationale of Hyperbaric Oxygenation in Cerebral Vascular Insult Current Vascular Pharmacology 8 1 35 43 https doi org 10 2174 15701 61107 90226 598 Francis A Baynosa R 2017 Ischaemia reperfusion injury and hyperbaric oxygen pathways A review of cellular mechanisms In Diving and Hyperbaric Medicine Vol 47 Issue 2 pp 110 117 South Pacific Medicine Underwater Society and the European Underwater and Baromedical Society https doi org 10 28920 dhm47 2 110 117 Freiberger J J Derrick B J Natoli M J Akushevich I Schinazi E A Parker C Stolp B W Bennett P B Vann R D Dunworth S A S Moon R E 2016 Assessment of the interaction of hyperbaric N2 CO2 and O2 on psychomotor performance in 13
divers Journal of Applied Physiology 121 4 953 964 https doi org 10 1152 jappl physi ol 00534 2016 Gale S D Hopkins R O 2004 Effects of hypoxia on the rain Neuroimaging and neuropsychological findings following carbon monoxide poisoning and obstructive sleep apnea Journal of the International Neuropsychological Society 10 1 60 71 https doi org 10 1017 S1355 61770 41010 82 Garcia A J Putnam R W Dean J B 2010a Hyperbaric hyperoxia and normobaric reoxygenation increase excitability and activate oxygen induced potentiation in CA1 hippocampal neurons Journal of Applied Physiology 109 3 804 819 https doi org 10 1152 jappl physi ol 91429 2008 Garcia A J Putnam R W Dean J B 2010b Hyperoxic stimulation of synchronous orthodromic activity and induction of neural plasticity does not require changes in excitatory synaptic transmission Journal of Applied Physiology 109 3 820 829 https doi org 10 1152 jappl physi ol 91430 2008 Ghacibeh G A Shenker J I Shenal B Uthman B M Heilman K M 2006 The influence of vagus nerve stimulation on memory Cognitive and Behavioral Neurology 19 3 119 122 https doi org 10 1097 01 wnn 00002 13908 34278 7d Godefroy O Bogousslavsky J 2007 The behavioral and cognitive neurology of stroke The Behavioral and Cognitive Neurology of Stroke https doi org 10 1017 CBO97 80511 544880 Golden Z Golden C J Neubauer R A 2006 Improving neuropsychological function after chronic brain injury with hyperbaric oxygen Disability and Rehabilitation 28 22 1379 1386 https doi org 10 1080 09638 28060 06383 64 Golden Z L Neubauer R Golden C J Greene L Marsh J Mleko A 2002 Improvement in cerebral metabolism in chronic brain injury after Hyperbaric Oxygen Therapy International Journal of Neuroscience 112 2 119 131 https doi org 10 1080 00207 45021 2027 Goldfarb A I Hochstadt N J Jacobson J H Weinstein E A 1972 Hyperbaric oxygen treatment of organic mental syndrome in aged persons Journal of Gerontology 27 2 212 217 https doi org 10 1093 geronj 27 2 212 Goldstein M 2008 Carbon Monoxide Poisoning Journal of Emergency Nursing 34 6 538 542 https doi org 10 1016 j jen 2007 11 014 Gong L W Gao T M Huang H Tong Z 2000 Redox modulation of large conductance calcium activated potassium channels in CA1 pyramidal neurons from adult rat hippocampus Neuroscience Letters 286 3 191 194 https doi org 1 0 1 016 S 0304 3 940 00 0 1121 6 Grim P S 1990 Hyperbaric Oxygen Therapy JAMA The Journal of the American Medical Association 263 16 2216 https doi org 10 1001 jama 1990 03440 16007 8042 Guiney H Lucas S J E Cotter J D Machado L 2019 Investigating links between habitual physical activity cerebrovascular function and cognitive control in healthy older adults Neuropsychologia 125 July 2018 62 69 https doi org 10 1016 j neuro psych ologia 2019 01 011 Hadanny A Golan H Fishlev G Bechor Y Volkov O Suzin G Ben Jacob E Efrati S 2015 Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restorative Neurology and Neuroscience 33 4 471 486 https doi org 10 3233 RNN 150517 Hadanny A Meir O Bechor Y Fishlev G Bergan J Efrati S 2016 Seizures during hyperbaric oxygen therapy Retrospective analysis of 62 614 treatment sessions Undersea and Hyperbaric Medicine 43 1 21 28 Hadanny A Meir O Bechor Y Fishlev G Bergan J Efrati S 2016 The safety of hyperbaric oxygen treatment 13 Neuropsychology Review Retrospective analysis in 2 334 patients Undersea and Hyperbaric Medicine 43 2 113 122 Hadanny A Abbott S Suzin G Bechor Y Efrati S 2018 Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of posttraumatic brain injury patients Retrospective analysis British Medical Journal Open 8 9 1 9 https doi org 10 1136 bmjop en 2018 023387 Hadanny A Efrati S 2016 The efficacy and safety of hyperbaric oxygen therapy in traumatic brain injury In Expert Review of Neurotherapeutics Vol 16 Issue 4 pp 359 360 Taylor and Francis Ltd https doi org 10 1586 14737 175 2016 11570 18 Hadanny A Rittblat M Bitterman M May Raz I Suzin G Boussi Gross R Zemel Y Bechor Y Catalogna M Efrati S 2020 Hyperbaric oxygen therapy improves neurocognitive functions of post stroke patients a retrospective analysis Restorative Neurology and Neuroscience 38 1 93 107 https doi org 10 3233 RNN 190959 Hampson N B Piantadosi C A Thom S R Weaver L K 2013 Practice recommendations in the diagnosis management and prevention of carbon monoxide poisoning Diving and Hyperbaric Medicine 43 3 172 https doi org 10 1164 rccm 201207 1284CI Harch P G Andrews S R Fogarty E F Amen D Pezzullo J C Lucarini J Aubrey C Taylor D V Staab P K Van Meter K W 2012 A phase i study of low pressure hyperbaric oxygen therapy for blast induced post concussion syndrome and post traumatic stress disorder Journal of Neurotrauma 29 1 168 185 https doi org 10 1089 neu 2011 1895 Harch P G Kriedt C Van Meter K W Sutherland R J 2007 Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury Brain Research 1174 1 120 129 https doi org 10 1016 j brain res 2007 0 6 1 05 Hardy P Collet J P Goldberg J Vanasse M Lambert J Marois P Amar M Montgomery D L Lecomte J M Johnston K M Lassonde M 2002 Neuropsychological effects of hyperbaric oxygen therapy in cerebral palsy Developmental Medicine and Child Neurology 44 7 436 446 https doi org 10 1017 S0012 16220 10023 41 Hart G B Strauss M B 2003 Hyperbaric Oxygen Therapy Stroke 34 9 https doi org 10 1161 01 STR 00000 87115 91721 6E Hart G B Thompson R E 1971 The treatment of cerebral ischemia with H perbaric Oxygen OHP Stroke 2 3 247 250 https doi org 10 1161 01 STR 2 3 247 Helms A K Whelan H T Torbey M T 2005 Hyperbaric Oxygen Therapy of Cerebral Ischemia Cerebrovascular Diseases 20 6 417 426 https doi org 10 1159 00008 8979 Henke K Kroll N E Behniea H Amaral D G Miller M B Rafal R Gazzaniga M S 1999 Memory lost and regained following bilateral hippocampal damage Journal of Cognitive Neuroscience 11 6 682 697 http www ncbi nlm nih gov pubmed 10601 749 Hopkins R O Weaver L K Valentine K J Mower C Churchill S Carlquist J 2007 Apolipoprotein E genotype and response of carbon monoxide poisoning to hyperbaric oxygen treatment American Journal of Respiratory and Critical Care Medicine 176 10 1001 1006 https doi org 10 1164 rccm 200702 290OC Hsu S M Tseng C H Hsieh C H Hsieh C W 2020 Slowpaced inspiration regularizes alpha phase dynamics in the human brain Journal of Neurophysiology 123 1 289 299 https doi org 10 1152 JN 00624 2019 Hu D Klann E Thiels E 2007 Superoxide dismutase and hippocampal function Age and isozyme matter In Antioxidants and Redox Signaling Vol 9 Issue 2 pp 201 210 Antioxid Redox Signal https doi org 10 1089 ars 2007 9 201 Huddleston A T Tang W Takeshima H Hamilton S L Klann E 2008 Superoxide induced potentiation in the hippocampus
Neuropsychology Review requires activation of ryanodine receptor type 3 and ERK Journal of Neurophysiology 99 3 1565 1571 https doi org 10 1152 jn 00659 2007 Jackson P A Pialoux V Corbett D Drogos L Erickson K I Eskes G A Poulin M J 2016 Promoting brain health through exercise and diet in older adults a physiological perspective Journal of Physiology 594 16 4485 4498 https d oi o rg 10 1113 JP271 270 Jacobs E A Alvis H J Small S M 1972 Hyperoxygenation a central nervous system activator Journal of Geriatric Psychiatry 5 2 107 136 http www ncbi nlm nih gov pubmed 45840 68 Jacobs E A Winter P M Alvis H J Small S M 1969 Hyperoxygenation effect on cognitive functioning in the aged The New England Journal of Medicine 281 14 753 757 https d oi o rg 10 1056 NEJM1 96910 02281 1402 Jain K K 2017 Textbook of Hyperbaric Medicine https doi org 10 1007 978 3 319 47140 2 Kalaria R N Maestre G E Arizaga R Friedland R P Galasko D Hall K Luchsinger J A Ogunniyi A Perry E K Potocnik F Prince M Stewart R Wimo A Zhang Z X Antuono P 2008 Alzheimer s disease and vascular dementia in developing countries prevalence management and risk factors In The Lancet Neurology Vol 7 Issue 9 pp 812 826 Lancet Publishing Group https doi org 10 1016 S1474 4422 08 70169 8 Kandlur A Satyamoorthy K Gangadharan G 2020 Oxidative Stress in Cognitive and Epigenetic Aging A Retrospective Glance Frontiers in Molecular Neuroscience 13 March https doi org 10 3389 fnmol 2020 00041 Kemmerling U Mu oz P M ller M S nchez G Aylwin M L Klann E Carrasco M A Hidalgo C 2007 Calcium release by ryanodine receptors mediates hydrogen peroxideinduced activation of ERK and CREB phosphorylation in N2a cells and hippocampal neurons Cell Calcium 41 5 491 502 https doi org 10 1016 j ceca 2006 10 001 Kety S S Schmidt C F 1948 the Effects of Altered Arterial Tensions of Carbon Dioxide and Oxygen on Cerebral Blood Flow and Cerebral Oxygen Consumption of Normal Young Men The Journal of Clinical Investigation 27 4 484 492 https doi org 10 1172 JCI10 1995 Kot J Winklewski P J Sicko Z Tkachenko Y 2015 Effect of oxygen on neuronal excitability measured by critical flicker fusion frequency is dose dependent Journal of Clinical and Experimental Neuropsychology 37 3 276 284 https doi org 10 1080 13803 395 2015 10071 18 Kraitsy K Uecal M Grossauer S Bruckmann L Pfleger F Ropele S Fazekas F Gruenbacher G Patz S Absenger M Porubsky C Smolle Juettner F Tezer I Molcanyi M Fasching U Schaefer U 2014 Repetitive long term Hyperbaric Oxygen Treatment HBOT administered after experimental traumatic brain injury in rats induces significant remyelination and a recovery of sensorimotor function PLoS One 9 5 https doi org 10 1371 journ al pone 00977 50 Kushner D 1998 Mild traumatic brain injury Toward understanding manifestations and treatment In Archives of Internal Medicine Vol 158 Issue 15 pp 1617 1624 https doi org 10 1001 archi nte 158 15 1617 Ku ma E Lourida I Moore S F Levine D A Ukoumunne O C Llewellyn D J 2018 Stroke and dementia risk A systematic review and meta analysis Alzheimer s and Dementia 14 11 1416 1426 https doi org 10 1016 j jalz 2018 06 3061 Leach R M Rees P J Wilmshurst P 1998 ABC of oxygen Hyperbaric oxygen therapy In British Medical Journal Vol 317 Issue 7166 pp 1140 1143 https doi org 10 1136 bmj 317 7166 1140 Lee M S Kim J S Chung T S Suh J H 1988 Measurements of cerebral blood flow in delayed carbon monoxide sequelae using xenon inhalation CT scan Yonsei Medical Journal 29 2 185 192 https doi org 10 3349 ymj 1988 29 2 185 Lee Y S Chio C C Chang C P Wang L C Chiang P M Niu K C Tsai K J 2013 Long course hyperbaric oxygen stimulates neurogenesis and attenuates inflammation after ischemic stroke Mediators of Inflammation 2013 512978 https doi org 10 1155 2013 512978 Levin H S 1990 Memory deficit after closed head injury Journal of Clinical and Experimental Neuropsychology 12 1 129 153 https doi org 10 1080 01688 63900 84009 60 Liao S C Mao Y C Yang K J Wang K C Wu L Y Yang C C 2019 Targeting optimal time for hyperbaric oxygen therapy following carbon monoxide poisoning for prevention of delayed neuropsychiatric sequelae A retrospective study Journal of the Neurological Sciences 396 187 192 https doi org 10 1016 j jns 2018 11 025 Lin K C Niu K C Tsai K J Kuo J R Wang L C Chio C C Chang C P 2012 Attenuating inflammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury Journal of Trauma and Acute Care Surgery 72 3 650 659 https doi org 10 1097 TA 0b013 e3182 3c575f Liu S Shen G Y Deng S K Wang X B Wu Q F Guo A S 2013 Hyperbaric oxygen therapy improves cognitive functioning after brain injury Neural Regeneration Research 8 35 3334 3343 https doi org 10 3969 j issn 1673 5374 2013 35 008 Liu W C Yang S N Wu C W J Chen L W Chan J Y H 2016 Hyperbaric oxygen therapy alleviates carbon monoxide poisoning induced delayed memory impairment by preserving brain derived neurotrophic factor dependent hippocampal neurogenesis Critical Care Medicine 44 1 e25 e39 https doi org 10 1097 CCM 00000 00000 001299 Lo C P Chen S Y Chou M C Wang C Y Lee K W Hsueh C J Chen C Y Huang K L Huang G S 2007 Diffusion tensor MR imaging for evaluation of the efficacy of hyperbaric oxygen therapy in patients with delayed neuropsychiatric syndrome caused by carbon monoxide inhalation European Journal of Neurology 14 7 777 782 https doi org 10 1111 j 1468 1331 2007 01854 x Lo E H Dalkara T Moskowitz M A 2003 Neurological diseases Mechanisms challenges and opportunities in stroke Nature Reviews Neuroscience 4 5 399 414 https d oi org 10 1038 nrn11 06 Lodato R F Jubran A 1993 Response time autonomic mediation and reversibility of hyperoxic bradycardia in conscious dogs Journal of Applied Physiology 74 2 634 642 https doi org 10 1152 jappl 1993 74 2 634 Mannaioni P F Vannacci A Masini E 2006 Carbon monoxide The bad and the good side of the coin from neuronal death to anti inflammatory activity In Inflammation Research Vol 55 Issue 7 pp 261 273 Inflamm Res https doi org 10 1007 s00011 006 0084 y Maric V Ramanathan D Mishra J 2020 Respiratory regulation interactions with neuro cognitive circuitry Neuroscience and Biobehavioral Reviews 112 February 2019 95 106 https d oi org 10 1016 j neubi orev 2020 02 001 Massaad C A Klann E 2011 Reactive oxygen species in the regulation of synaptic plasticity and memory Antioxidants and Redox Signaling 14 10 2013 2054 https doi org 10 1089 ars 2010 3208 Mathieu D Nolf M Durocher A Saulnier F Frimat P Furon D Wattel F 1985 Acute carbon monoxide poisoning risk of late sequelae and treatment by hyperbaric oxygen Clinical Toxicology 23 4 6 315 324 https doi org 10 3109 15563 65850 89906 39 Mathieu D 2006a Handbook on hyperbaric medicine Springer 13
Mathieu D Ed 2006b Handbook on Hyperbaric Medicine Springer Netherlands https doi org 10 1007 1 4020 4448 8 Mathieu D Marroni A Kot J 2017 Tenth european consensus conference on hyperbaric medicine Recommendations for accepted and non accepted clinical indications and practice of hyperbaric oxygen treatment Diving and Hyperbaric Medicine 47 1 24 31 https doi org 10 28920 dhm47 1 24 32 McCauley R D Fewtrell J Duncan A J Jenner C Jenner M N Penrose J D et al 2000 Marineseismic surveys a study of environmental implications The APPEA Journal 40 1 692 https doi org 10 1071 aj990 48 Medana I M Esiri M M 2003 Axonal damage A key predictor of outcome in human CNS diseases In Brain Vol 126 Issue 3 pp 515 530 https doi org 10 1093 brain awg061 Micarelli A Jacobsson H Larsson S A Jonsson C Pagani M 2013 Neurobiological insight into hyperbaric hyperoxia Acta Physiologica 209 1 69 76 https d oi o rg 1 0 1 111 a pha 1 2116 Moher D Liberati A Tetzlaff J Altman D G Altman D Antes G Atkins D Barbour V Barrowman N Berlin J A Clark J Clarke M Cook D D Amico R Deeks J J Devereaux P J Dickersin K Egger M Ernst E Tugwell P 2009 Preferred reporting items for systematic reviews and meta analyses The PRISMA statement In PLoS Medicine Vol 6 Issue 7 PLoS Med https doi org 10 1371 journ al pmed 10000 97 Moon R E 2019 Hyperbaric Oxygen Therapy INDICATIONS 14 TH EDITION Moorhouse P Rockwood K 2008 Vascular cognitive impairment current concepts and clinical developments In The Lancet Neurology Vol 7 Issue 3 pp 246 255 https d oi o rg 1 0 1 016 S1474 4422 08 70040 1 Mor A Grossman Y 2010 The efficacy of physiological and pharmacological N methyl d aspartate receptor block is greatly reduced under hyperbaric conditions Neuroscience 169 1 1 7 https doi org 10 1016 j neuro scien ce 2010 05 009 Mor A Grossman Y 2007 High pressure modulation of NMDA receptor dependent excitability European Journal of Neuroscience 25 7 2045 2052 https doi org 10 1111 j 1460 9568 2007 05479 x Mu J Krafft P R Zhang J H 2011 Hyperbaric oxygen therapy promotes neurogenesis Where do we stand In Medical Gas Research Vol 1 Issue 1 BioMed Central Ltd https doi org 10 1186 2045 9912 1 14 Mundy M E Downing P E Dwyer D M Honey R C Graham K S 2013 A critical role for the hippocampus and perirhinal cortex in perceptual learning of scenes and faces Complementary findings from amnesia and fMRI Journal of Neuroscience 33 25 10490 10502 https doi org 10 1523 JNEUR OSCI 2958 12 2013 Mychaskiw G Stephens P L 2013 Hyperbaric Oxygen Mild Traumatic Brain Injury and Study Design An Elusive Target Journal of Neurotrauma 30 19 1681 1682 https doi org 10 1089 neu 2012 2805 Neubauer R A James P 1998 Cerebral oxygenation and the recoverable brain Neurological Research 20 SUPPL 1 https doi org 10 1080 01616 412 1998 11740 606 Ogoh S Tarumi T 2019 Cerebral blood flow regulation and cognitive function a role of arterial baroreflex function Journal of Physiological Sciences 69 6 813 823 https d oi o rg 1 0 1 007 s12576 019 00704 6 Omae T Ibayashi S Kusuda K Nakamura H Yagi H Fujishima M 1998 Effects of high atmospheric pressure and oxygen on middle cerebral blood flow velocity in humans measured by transcranial Doppler Stroke 29 1 94 97 https doi org 10 1161 01 STR 29 1 94 Oriani G Marroni A Wattel F 1996 Handbook on Hyperbaric Medicine Springer Oury T D Ho Y S Piantadosi C A Crapo J D 1992 Extracellular superoxide dismutase nitric oxide and central nervous 13 Neuropsychology Review system O2 toxicity Proceedings of the National Academy of Sciences of the United States of America 89 20 9715 9719 https doi org 10 1073 pnas 89 20 9715 Park Y M Kim Y S 2014 Secondary mania in a patient with delayed anoxic encephalopathy after carbon monoxide intoxication caused by a suicide attempt General Hospital Psychiatry 36 1 125 e3 125 e4 https doi org 10 1016 j genho sppsy ch 2013 07 003 Parkinson J Registrar M 1871 the Rate of the Pulse in Health By Potter S Leigh E Wade D Fleminger S 2006 The Rivermead Post Concussion Symptoms Questionnaire A confirmatory factor analysis Journal of Neurology 253 12 1603 1614 https doi org 10 1007 s00415 006 0275 z Prior H Schwegler H D cker G 1997 Dissociation of spatial reference memory spatial working memory and hippocampal mossy fiber distribution in two rat strains differing in emotionality Behavioural Brain Research 87 2 183 194 https d oi o rg 10 1016 S0166 4328 97 02282 1 Prockop L D Chichkova R I 2007 Carbon monoxide intoxication An updated review Journal of the Neurological Sciences 262 1 2 122 130 https doi org 10 1016 j jns 2007 06 037 Rajeswaran J 2013 Neuropsychological Rehabilitation Principles and Applications Edited Journal of Chemical Information and Modeling https doi org 10 1017 CBO97 81107 415324 004 Raskin A Gershon S Crook T H Sathananthan G Ferris S 1978 The Effects of Hyperbaric and Normobaric Oxygen on Cognitive Impairment in the Elderly Archives of General Psychiatry 35 1 50 56 https doi org 10 1001 archp syc 1978 01770 25005 2005 Ricker J H Callahan C D 2000 International Handbook of Neuropsychological Rehabilitation In Journal of Head Trauma Rehabilitation Vol 15 Issue 3 https doi org 10 1097 00001 199 20000 6000 00012 Robinson R G 2006 The clinical neuropsychiatry of stroke Second edition In The Clinical Neuropsychiatry of Stroke https doi org 10 1017 CBO97 80511 544231 Rockswold S B Rockswold G L Zaun D A Liu J 2013 A prospective randomized Phase II clinical trial to evaluate the effect of combined hyperbaric and normobaric hyperoxia on cerebral metabolism intracranial pressure oxygen toxicity and clinical outcome in severe traumatic brain injury Journal of Neurosurgery 118 6 1317 1328 https d oi org 10 3171 2013 2 JNS12 1468 Rockswold S B Rockswold G L Zaun D A Zhang X Cerra C E Bergman T A Liu J 2010 A prospective randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism intracranial pressure and oxygen toxicity in severe traumatic brain injury Clinical article Journal of Neurosurgery 112 5 1080 1094 https doi org 10 3171 2009 7 JNS09 363 Rosario E R Kaplan S E Khonsari S Vazquez G Solanki N Lane M Brownell H Rosenberg S S 2018 The Effect of Hyperbaric Oxygen Therapy on Functional Impairments Caused by Ischemic Stroke Neurology Research International 2018 12 15 https doi org 10 1155 2018 31726 79 Rossignol D A Rossignol L W Jill S J Melnyk S Mumper E 2007 The effects of hyperbaric oxygen therapy on oxidative stress inflammation and symptoms in children with autism An open label pilot study BMC Pediatrics 7 1 13 https doi org 10 1186 1471 2431 7 36 S nchez E C 2013 Mechanisms of action of hyperbaric oxygenation in stroke A review In Critical Care Nursing Quarterly Vol 36 Issue 3 pp 290 298 https doi org 10 1097 CNQ 0b013 e3182 94e9e3 Sarno J E Rusk H A Diller L Sarno M T 1972a The effect of hyperbaric oxygen on the mental and verbal ability of stroke patients Stroke 3 1 10 15 https doi org 10 1161 01 STR 3 1 10
Neuropsychology Review Sarno M T Sarno J E Diller L 1972b The effect of hyperbaric oxygen on communication function in adults with aphasia secondary to stroke Journal of Speech and Hearing Research 15 1 42 48 https doi org 10 1044 jshr 1501 42 Scheinkestel C D Bailey M Myles P S Jones K Cooper D J Millar I L Tuxen D V 1999 Hyperbaric or normobaric oxygen for acute carbon monoxide poisoning a randomised controlled clinical trial The Medical Journal of Australia 170 5 203 210 http www ncbi nlm nih gov pubmed 10092 916 Shandley S Wolf E G Schubert Kabban C M Baugh L M Richards M F Prye J Arizpe H M Kalns J 2017 Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy Undersea and Hyperbaric Medicine 44 3 257 269 https doi org 10 22462 5 6 2017 6 Shapira R Solomon B Efrati S Frenkel D Ashery U 2018 Hyperbaric oxygen therapy ameliorates pathophysiology of 3xTg AD mouse model by attenuating neuroinflammation Neurobiology of Aging 62 105 119 https doi org 10 1016 j neuro biola ging 2017 10 007 Shetty P K Huang F L Huang K P 2008 Ischemia elicited oxidative modulation of Ca2 calmodulin dependent protein kinase II Journal of Biological Chemistry 283 9 5389 5401 https doi org 10 1074 jbc M7084 79200 Shi X Tang Z Xiong B Bao J Sun D Zhang Y Yao Y 2003 Cerebral perfusion SPECT imaging for assessment of the effect of hyperbaric oxygen therapy on patients with postbrain injury neural status Chinese Journal of Traumatology Zhonghua Chuang Shang Za Zhi 6 6 346 349 http www ncbi nlm nih gov pubmed 14642 054 Singhal A B 2007 A review of oxygen therapy in ischemic stroke In Neurological Research Vol 29 Issue 2 pp 173 183 https doi org 10 1179 01616 4107X 181815 Smith R Thayer J F Khalsa S S Lane R D 2017 The hierarchical basis of neurovisceral integration Neuroscience and Biobehavioral Reviews 75 274 296 https doi org 10 1016 j neubi orev 2017 02 003 Sohlberg M M Mateer C A 2001 Cognitive rehabilitation An integrative neuropsychological approach PsycNET G Press Ed https psycn et apa org record 2001 01866 000 Sohlberg M M Mateer C A 2001 Improving attention and managing attentional problems Adapting rehabilitation techniques to adults with ADD Annals of the New York Academy of Sciences 931 359 375 https doi org 10 1111 j 1749 6632 2001 tb057 90 x S nmez B M canl M D Parlak S Do an Y Ulubay H G Temel E 2018 Delayed neurologic sequelae of carbon monoxide intoxication Turkish Journal of Emergency Medicine 18 4 167 169 https doi org 10 1016 j tjem 2018 04 002 Sorrentino G Migliaccio R Bonavita V 2008 Treatment of vascular dementia The route of prevention In European Neurology Vol 60 Issue 5 pp 217 223 https doi org 10 1159 00015 1696 Stoller K P 2007 Hyperbaric oxygen and carbon monoxide poisoning a critical review Neurological Research 29 2 146 155 https doi org 10 1179 01616 4107X 181770 Szalewska D Radkowski M Demkow U Winklewski P J 2017 Exercise strategies to counteract brain aging effects Advances in Experimental Medicine and Biology 1020 69 79 https doi org 10 1007 5584_ 2017_3 Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E Efrati S 2015 Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restorative Neurology and Neuroscience 33 6 943 951 https doi org 10 3233 RNN 150585 Tal S Hadanny A Sasson E Suzin G Efrati S 2017 Hyperbaric oxygen therapy can induce angiogenesis and regeneration of nerve fibers in traumatic brain injury patients Frontiers in Human Neuroscience 11 https doi org 10 3389 fnhum 2017 00508 Tapeantong T Poungvarin N 2009 Delayed encephalopathy and cognitive sequelae after acute carbon monoxide poisoning Report of a case and review of the literature Journal of the Medical Association of Thailand 92 10 1374 1379 Thayer J F Lane R D 2000 A model of neurovisceral integration in emotion regulation and dysregulation Journal of Affective Disorders 61 3 201 216 https doi org 10 1016 S0165 0327 00 00338 4 Thom S R Bhopale V M Fisher D Zhang J Gimotty P 2004 Delayed neuropathology after carbon monoxide poisoning is immune mediated Proceedings of the National Academy of Sciences of the United States of America 101 37 13660 13665 https doi org 10 1073 pnas 04056 42101 Thompson L W Davis G C Obrist W D Heyman A 1976 Effects of hyperbaric oxygen on behavioral and physiological measures in elderly demented patients Journals of Gerontology 31 1 23 28 https doi org 10 1093 geronj 31 1 23 Vila J F Balcarce P E Abiusi G R Dom nguez R O Pisarello J B 2005 Improvement in motor and cognitive impairment after hyperbaric oxygen therapy in a selected group of patients with cerebrovascular disease A prospective singleblind controlled trial Undersea and Hyperbaric Medicine 32 5 341 349 Vonck K Raedt R Naulaerts J De Vogelaere F Thiery E Van Roost D Aldenkamp B Miatton M Boon P 2014 Vagus nerve stimulation 25 years later What do we know about the effects on cognition Neuroscience and Biobehavioral Reviews 45 63 71 https doi org 10 1016 j neubi orev 2014 05 005 Walker W C Franke L M Cifu D X Hart B B 2014 Randomized sham controlled feasibility trial of hyperbaric oxygen for service members with postconcussion syndrome Cognitive and psychomotor outcomes 1 week postintervention Neurorehabilitation and Neural Repair 28 5 420 432 https doi org 10 1177 15459 68313 516869 Walter B Daly J Bondurant S 1962 Effects of oxygen breathing on the heart rate blood pressure and cardiac index of normal men resting with reactive hyperemia and after atropine oxygen breathing has been used extensively to treat a wide variety of clinical disorders An underst Journal of Clinical Investigation 41 1 126 132 Wang G H Zhang X G Jiang Z L Li X Peng L L Li Y C Wang Y 2010 Neuroprotective effects of hyperbaric oxygen treatment on traumatic brain injury in the rat Journal of Neurotrauma 27 9 1733 1743 https doi org 10 1089 neu 2009 1175 Wang S Tao Z Ding S Cheng J BS Y Wang Y 2009 Hyperbaric oxygen combined with donepezil in the treatment of vascular dementia Chinese Journal of Physical Medicine and Rehabilitation 31 7 478 480 Weaver L K 2009 Clinical practice Carbon monoxide poisoning The New England Journal of Medicine 360 12 1217 1225 https doi org 10 1056 NEJMc p0808 891 Weaver L K Cifu D Hart B Wolf G Scott Miller R 2012 Hyperbaric oxygen for post concussion syndrome Design of Department of Defense clinical trials Undersea and Hyperbaric Medicine 39 4 807 814 Weaver L K Cifu D Hart B Wolf G Scott Miller R 2013 Reply Department of Defense trials for hyperbaric oxygen and TBI Issues of study design and questionable conclusions Undersea and Hyperbaric Medicine 40 5 471 472 Weaver L K Hopkins R O Chan K J Churchill S Elliott C G Clemmer T P Orme J F J Thomas F O Morris A H 2002 Hyperbaric oxygen for acute carbon monoxide poisoning New England Journal of Medicine 347 14 1057 1067 https doi org 10 1056 NEJMo a0131 21 LK http r ug on 13
world cat org atozt itles link sid EMBAS E issn 00284 793 id d oi 1 0 1 056 2 FNEJ M oa01 3 121 a title H yper b aric oxygen for a cute c arbon m onox i de p oiso n ing stitle New E ngl J M ed t itle N ew E ngla n d J ourn a l of Medic ine volume 347 issue 14 spage 1057 epage 1067 a ulast Weave r a ufir s t L inde l l K a uinit L K aufull Weaver L K coden NEJMA isbn pages 1057 1067 date 2002 auini t1 L auini tm K Weaver L K Valentine K J Hopkins R O 2007 Carbon monoxide poisoning Risk factors for cognitive sequelae and the role of hyperbaric oxygen American Journal of Respiratory and Critical Care Medicine 176 5 491 497 https doi org 10 1164 rccm 200701 026OC Weaver L K Wilson S H Lindblad A S Churchill S Deru K Price R C Williams C S Orrison W W Walker J M Meehan A Mirow S 2018 Hyperbaric oxygen for postconcussive symptoms in United States military service members A randomized clinical trial Undersea and Hyperbaric Medicine 45 2 129 156 https doi org 10 22462 03 04 2018 1 Winklewski P J Kot J Frydrychowski A F Nuckowska M K Tkachenko Y 2013 Effects of diving and oxygen on autonomic nervous system and cerebral blood flow Diving and Hyperbaric Medicine 43 3 148 156 Winklewski P J Sabisz A Naumczyk P Jodzio K Szurowska E Szarmach A 2018 Understanding the physiopathology behind axial and radial diffusivity changes what do we Know In Frontiers in Neurology Vol 9 Issue FEB Frontiers Media S A https doi org 10 3389 fneur 2018 00092 Wolf E G Baugh L M Schubert Kabban C M Richards M F Prye J 2015 Cognitive function in a traumatic brain injury hyperbaric oxygen randomized trial Undersea and Hyperbaric Medicine 42 4 313 332 Wolf G Cifu D Baugh L Carne W Profenna L 2012 The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury Journal of Neurotrauma 29 17 2606 2612 https doi org 10 1089 neu 2012 2549 Wright J K Zant E Groom K Schlegel R E Gilliland K 2009 Case report Treatment of mild traumatic brain injury with hyperbaric oxygen Undersea Hyperbaric Medicine Journal of the Undersea and Hyperbaric Medical Society Inc 36 6 391 399 http w ww n cbi n lm n ih g ov p ubmed 2 01125 30 Xiang W Xue H Wang B Li Y Zhang J Jiang C et al 2017a Combined application of dexamethasone and hyperbaric oxygen therapy yields better efficacy for patients with delayed encephalopathy after acute carbon monoxide poisoning Drug Design Development and Therapy 11 513 519 https doi org 10 2147 DDDT S1265 69 Xiang W Xue H Wang B Li Y Zhang J Jiang C Pang J 2017b Efficacy of N Butylphthalide and Hyperbaric Oxygen Therapy on Cognitive Dysfunction in Patients with Delayed Encephalopathy After Acute Carbon Monoxide Poisoning In Medical science monitor Vol 23 pp 1501 1506 http onlin e libr a ry w iley c om o c ochr a ne c lcen t ral a rtic l es 2 19 CN 01368 219 frame html Xu Y Wang Q Qu Z Yang J Zhang X Zhao Y 2019 Protective Effect of Hyperbaric Oxygen Therapy on Cognitive Function 13 Neuropsychology Review in Patients with Vascular Dementia Cell Transplantation 28 8 1071 1075 https doi org 10 1177 09636 89719 853540 Yeh Z T Tsai C F Yip P K Lo C Y Peng S M Chen S Y Kung L Y 2014 Neuropsychological performance in patients with carbon monoxide poisoning Applied Neuropsychology Adult 21 4 278 287 https doi org 10 1080 23279 095 2013 811670 You Q Li L Xiong S Q Yan Y F Li D Yan N N Chen H P Liu Y P 2019 Meta analysis on the efficacy and safety of hyperbaric oxygen as adjunctive therapy for vascular dementia In Frontiers in Aging Neuroscience Vol 11 Issue APR Frontiers Media S A https doi org 10 3389 fnagi 2019 00086 Z dori A goston V A Demeter K H dinger N V rady L Koh di T Gobl A Nagy Z Madar sz E 2011 Survival and differentiation of neuroectodermal cells with stem cell properties at different oxygen levels Experimental Neurology 227 1 136 148 https doi org 10 1016 j expne urol 2010 10 004 Zagami A S Lethlean A K Mellick R 1993 Delayed neurological deterioration following carbon monoxide poisoning MRI findings Journal of Neurology 240 2 113 116 https doi org 10 1007 bf008 58727 Zasler N D Katz D I Zafonte R D 2007 Brain Injury Medicine Principles and Practice Demos Zhang J Guo Y Li W Li G Chen Y 2020 The efficacy of N butylphthalide and dexamethasone combined with hyperbaric oxygen on delayed encephalopathy after acute carbon monoxide poisoning Drug Design Development and Therapy 14 1333 1339 https doi org 10 2147 DDDT S2170 10 Zhang T Yang Q W Wang S N Wang J Z Wang Q Wang Y Luo Y J 2010 Hyperbaric oxygen therapy improves neurogenesis and brain blood supply in piriform cortex in rats with vascular dementia Brain Injury 24 11 1350 1357 https doi org 10 3109 02699 052 2010 504525 Zhang Y P Cai J Shields L B E Liu N Xu X M Shields C B 2014 Traumatic Brain Injury Using Mouse Models In Translational Stroke Research Vol 5 Issue 4 pp 454 471 Springer US https doi org 10 1007 s12975 014 0327 0 Zhao B Pan Y Wang Z Xu H Song X 2017 Hyperbaric oxygen pretreatment improves cognition and reduces hippocampal damage via p38 mitogen activated protein kinase in a rat model Yonsei Medical Journal 58 1 131 138 https doi org 10 3349 ymj 2017 58 1 131 Zhou Z Daugherty W P Sun D Levasseur J E Altememi N Hamm R J Rockswold G L Bullock M R 2007 Protection of mitochondrial function and improvement in cognitive recovery in rats treated with hyperbaric oxygen following lateral fluid percussion injury Journal of Neurosurgery 106 4 687 694 https doi org 10 3171 jns 2007 106 4 687 Publisher s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
We are IntechOpen the world s leading publisher of Open Access books Built by scientists for scientists 5 600 138 000 175M Open access books available International authors and editors Downloads Our authors are among the 154 TOP 1 12 2 Countries delivered to most cited scientists Contributors from top 500 universities Selection of our books indexed in the Book Citation Index in Web of Science Core Collection BKCI Interested in publishing with us Contact book department intechopen com Numbers displayed above are based on latest data collected For more information visit www intechopen com
Chapter Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury Robert Louis Beckman Abstract Hyperbaric Oxygen Therapy can help heal brain wounds TBI PTSD Concussion Peer reviewed positive scientific and clinical evidence in over 7500 cases demonstrates that HBOT helps heal wounded brains and returns patients to a life denied them by DOD VA Army that will not talk about or even use or pay for HBOT treatment for TBI PTSD PCS Concussion Successful treatment with HBOT 40 one hour sessions virtually eliminates suicidal ideation an effective suicide prevention method Patients also reduce their drug intake to nearly zero and experience 50 reduction in pain and time to withdrawal The history of HBOT for TBI is littered with bad science but evidence based and clinical medicine data show the safety efficacy and cost effectiveness of HBOT as a standard of care that should be put on label and insured Keywords hyperbaric oxygen TBI PTSD concussion The truth goes through three stages first it is ridiculed then it is violently opposed and then it is accepted as self evident Arthur Schopenhauer First they ignore you then they laugh at you then they fight you then you win Mahatma Gandhi 1 Introduction Though neither of these quotes is quite true they lead this introduction because those who are working to heal broken brains and stop the suicide epidemic are closer to winning than when they started There are no guarantees that collective successes will overcome medical resistance to accepting the obvious what they are doing does not work to heal brain wounds and they ignore and denigrate a safe and effective treatment that does Yet those trying to get urgent help to suicidal brain wounded service members see victory on the near horizon for the varieties of truths told in the research and worldwide clinical medicine As with many advances an anecdote helps elucidate the main point changing minds and medicine even with science data and facts is not easy work Two renegade Australian MDs Barry Marshall and J Robin Warren in 1981 knew there was a simple treatment for gastritis and peptic ulcers an antibiotic to kill Heliobacter pylori bacteria Now Helicobacter pylori may be the most successful pathogen in human history While not as deadly as the bacteria that cause tuberculosis 1
Advancement and New Understanding in Brain Injury cholera and the plague it infects more people than all the others combined Yet conventional medicine already knew that ulcers were caused by stress An entire set of industries grew up around healing stress and its aftermath antacids stomach surgery for bleeding ulcers gastritis stomach cancer depression To gastroenterologists the concept of a germ causing ulcers was like saying that the Earth is flat 1 To them the cause of all the illness and death was psychosomatic all in the head Marshall went so far to prove his point that he gave himself ulcers by drinking a broth of H pylori and curing himself And still not recognition Cut to the chase For their relentless persistence and science on H pylori in 2005 Marshall and Warren won the Nobel Prize Treatment with an antibiotic is standard medicine for stomach cancer 2 Twenty four years to go from goats to Nobel laureates Along the way the men were ridiculed and denounced by learned councils around the world And then the truth As you read these pages we expect that you will be whipsawed by the truths exposed as authors and readers wonder about the answer to the Obvious Question Since this works why are they opposed to it As you will see there are no complete answers but the data and the peer reviewed research do provide compelling and overwhelming evidence of the safety efficacy and cost effectiveness of this treatment Over 7500 successes cannot be entirely wrong 2 Background On August 30 2002 Medicare announced its intention to issue a national coverage determination NCD for Hyperbaric Oxygen Therapy HBOT in the treatment of diabetic wounds of the lower extremities The arguments that led to that determination 3 established that oxygen under pressure was safe and effective for this fourteenth indication or disease state The evolution in thinking and the subsequent research was enabled by the 1999 refinement and restatement of the drug definition of HBOT as the use of greater than atmospheric pressure oxygen as a drug to treat basic pathophysiologic processes and their diseases 4 The UHMS defines hyperbaric oxygen HBO2 as an intervention in which an individual breathes near 100 oxygen intermittently while inside a hyperbaric chamber that is pressurized to greater than sea level pressure 1 atmosphere absolute or ATA 5 With that definition the totality of on label indications could be understood as cohesive sets of diagnoses connected by HBOT effects on the acute and or chronic underlying pathophysiology common to the diseases Doctors noticed that the definition necessarily could be applied to the use of HBOT for additional diseases that shared this pathology Of the 14 15 indications accepted by the FDA CMS at least five are non healing wounds and therefore closely related to brain wounding from blast falls impact stroke Improvised explosive devices and concussion Those indications are Crush injury compartment syndrome and other acute traumatic ischemias Arterial Insufficiency entailing enhancement of healing in selected problem wounds includes uses like Diabetic Foot Wounds Hypoxic Wounds Radiation tissue damage soft tissue and bony necrosis Skin grafts and flaps compromised and Air or gas embolism resulting from rapid decompression and blast injury 6 The accurate drug definition of HBOT and its implications for the findings and data in research into traumatic brain injury is used in this paper to argue for HBOT safety and effectiveness in the treatment of Traumatic Brain Injury The argument is constructed by identifying the underlying pathophysiology in traumatic brain injury Evidence for the beneficial effects of HBOT on TBI is presented Benefits to patients with TBI is discussed Evidence for HBOT for TBI risk benefit and cost are discussed The conclusion is simple coverage of HBOT for TBI 2
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 3 Traumatic brain injury basics Research over the last two decades has revealed the complex microcosms of multiple pathophysiological processes resulting from insults to the brain including traumatic brain injury 7 The three essential components determining the outcome of head injuries are brain blood flow the pressure in the skull leading to swelling and hypoxia the lack of oxygen 8 According to the Centers for Disease Control and Prevention CDC traumatic brain injury TBI is caused by a bump blow or jolt to the head or a penetrating head injury that disrupts the normal function of the brain TBI severity ranges from mild i e a brief change in mental status or consciousness to severe i e an extended period of unconsciousness or amnesia after the injury 9 The CDC keeps current statistics on TBI death and disability Traumatic brain injury TBI is a major cause of death and disability in the United States Those who survive a TBI can face effects that last a few days or the rest of their lives Among TBI related ED visits and hospitalizations in 2014 statistics notable for the CDC include Hospitalization rates were highest among persons 75 years of age and older The highest rates of ED visits included persons 75 years of age and older For adults 55 years of age and older falls were the leading cause of hospitalizations and ED visits Among TBI related deaths in 2014 rates were highest for persons 75 years of age and older In 2014 an average of 155 people in the United States died each day from injuries that include a TBI Between 2001 and 2010 the estimated average annual numbers of TBI in the US equaled TBI contributed to the deaths of 56 800 people 282 000 hospitalizations and 2 5 M ER visits Accidental traumatic brain injuries contributed to more deaths than suicides and homicides together 10 Approximately 5 3 M people in the US live with a permanent TBI 11 The lifetime economic cost of TBI including direct and indirect medical costs was estimated to be approximately 76 5 billion in 2010 dollars 12 Current estimates put the yearly costs of TBI among veterans at 48 billion 13 UCLA researchers citing animal and human studies speak of a neurometabolic cascade of events that involves bioenergetic challenges cytoskeletal and axonal alterations impairments in neurotransmission and vulnerability to delayed cell death and chronic dysfunction linking the neurometabolic cascade to clinical characteristics as well as on new connections being made between acute postconcussion pathophysiology long term biological changes and chronic sequelae 14 Further The etiology of postconcussive syndrome is debated but may be caused by diffuse axonal injury or persistent metabolic alterations resulting in neuronal dysfunction and develops in 38 80 of patients with TBI 15 3
Advancement and New Understanding in Brain Injury Advanced neuroimaging reveals the basic neurobiology of concussion mild TBI in animal models which is increasingly corroborated in human studies These images of the brain with such techniques as diffusion tensor imaging DTI validate the wounding from the brain injury Since HBOT has been studied as a science for over 84 years 16 a wealth of evidence exists with or without brain imaging or functional imaging such as SPECT scans that points to the wounding of the brain as an underlying cause of TBI and in many cases the cooccurrence of Post traumatic stress disorder PTSD Controversy continues to wage over proper diagnoses of TBI and PTSD The author is aware for over a decade of clinical medicine and the accumulation of anecdotal evidence in over 7500 successful uses of HBOT to help treat and heal TBI that those combat veterans presenting with PTSD only diagnoses from the VA are overwhelmingly afflicted with undiagnosed TBI Researchers have not yet fully understood how TBI commonly affects the neurological and clinical presentation of PTSD 17 Despite this high prevalence the pathogenesis of TBI PTSD and TBI PTSD remains largely unknown hindering prevention and treatment efforts 18 No matter how acquired TBI in a veteran or a civilian is an injury to the brain tissue Damage is physiological behavioral and emotional Symptoms can include altered consciousness headaches structural damage to brain matter and blood vessels and nerves loss of neurological function that can lead to loss of motor sensory coordination balance vision hearing and other abilities inability to multi task slowed reaction time decreased attention and concentration inability to think fast and frequent incapacity to work sleep relax think or discern what is normal When wounded the brain like all body organs responds with the inflammatory process which proceeds to form scars scar tissue and chronic wounds When the brain injury is compounded by post traumatic stress disorder PTSD the victim is subjected to hyperarousal avoidance behaviors trauma re experiencing increased mental vigilance difficulty falling asleep nightmares constant anxiety resulting from progressive sleep deprivation and elevation of injurious stress hormones Behaviors and emotions are magnified intensifying the patient s negative responses relationship problems domestic violence substance abuse depression criminal activity unemployment incarceration homelessness and too frequently suicide Where the degenerative cycle can be arrested with drugs or psychological interventions the result may be a lifetime of degraded quality of life on welfare not only for the patient but typically for the caregiver as well In 2016 researchers at the Uniformed Services University of the Health Sciences in Bethesda Md found evidence of tissue damage caused by blasts alone not by concussions or other injuries 19 According to the New York Times this could be the medical explanation for shell shock and the sequalae of psychological problems called PTSD 20 The implications are clear IEDs breeching enemy and or friendly fire from personal weapons can lead directly to physical brain damage and the accompanying effects many of which are diagnosed as only PTSD Not to be overlooked are the complex interactions among brain injury trauma and physical emotional behavior mental health Psychiatrist Bessel van der Kolk in The Body Keeps the Score 21 explains how trauma and its resulting stress harms us through physiological changes to body and brain and that those harms can persist throughout life Stress trauma depression mental and physical health are so intertwined that it is hard to know the seat of the disease The author argues that trauma is one of the West s most urgent public health issues The list of its effects is long on mental and physical health employment education crime relationships domestic or family abuse alcoholism drug addiction As with PTSD and TBI whether a brain insult precedes mental health problems it is certain that the brain and the body will suffer in time 4
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 Several studies have looked at this downward cycle in untreated brain injuries 22 and noted a correspondence between the symptoms resulting from that brain injury and the HBOT Mechanisms of Action that work to arrest and heal the traumatic brain injury 4 Hyperbaric oxygenation mechanisms of action Medical studies have shown that Hyperbaric Oxygen Therapy is medicine s best way to provide oxygen to all parts of the body in the shortest period of time Among many effects HBOT has been shown to be effective in Reducing local swelling edema and reperfusion injury Promoting wound healing Improving and repairing injury by increasing oxygen delivery to damaged tissues Improving infection control Releasing nitric oxide with migration to point of injury Increasing the production of collagen Releasing stem cells with migration to area of injury Improving blood flow to the affected area of the brain Restarting stunned cellular metabolism and stunned mitochondria Generating blood vessel growth angiogenesis Activating stem cells 8x normal to repair neural pathways neurogenesis Decreasing markers of inflammation in the body and brain 23 While it is uncommon to hear HBOT talked about in terms of healing wounds to the brain the facts are now obvious a major organ of the body is damaged Treatments in the DoD and Veterans Administration for a brain wounded population of at least 414 000 post 9 11 veterans typically resolve to rest and a mix of cognitive physical speech and occupational therapy along with medication to control specific symptoms such as headaches or anxiety 24 Virtually the last time TBI is referred to as a wound is when speaking of the Invisible Wounds of War Brain wound healing demands that the body grow new tissue blood vessels connective tissue new brain tissue Cells have to grow and divide to form new tissue necessitating stimulation of cells to divide and multiply DNA must be stimulated 25 By 2008 DNA analysts found that a single hyperbaric treatment turns on as many as 8101 genes in the 24 hours following HBOT treatment 26 In short the turned on genes are those genes that code for growth and repair hormones and the anti inflammatory genes 27 As already noted HBOT is already approved for several on label indications collectively similar as wound healing It is worth noting that HBOT chambers are present in 1158 of a total of 3342 hospitals in the US 28 5
Advancement and New Understanding in Brain Injury Those chambers are primarily used for Wound Healing For a variety of reasons those chambers are not put to use on off label uses of HBOT Nevertheless the bulk of science on animal and human patients with TBI has been collected in both hospital based and private clinics Dr Paul Harch prepared voluminous evidence on HBOT for wound healing in his arguments for recognition of DFW in 2002 29 More specific to TBI Dr Philip James in Head Injuries the Curse of Life in the Fast Lane 30 traces the development of HBOT for TBI research as far back as 1972 31 The study found that tissue oxygen levels that fight hypoxia rise with the increase in either the oxygen concentration or pressure hyperbaric oxygenation James writes that this one study answers all the questions and objections raised about using hyperbaric oxygen treatment for patients with head injury 32 Oddo in 2011 identified hypoxia as a culprit Brain hypoxia is associated with poor short term outcome after severe traumatic brain injury independently of elevated ICP low CPP and injury severity Reduced brain oxygen Pbto 2 may be an important therapeutic target after severe traumatic brain injury 33 Dr Daphne Denham the nation s premier expert on HBOT treatment of acute concussion reported that 98 of her patients in her Fargo ND clinic 348 out of 350 treated within ten days of suffering a concussion completely resolved their symptoms in five treatments or less average of 2 4 treatments 34 The only difference in her patients and the thousands of concussed athletes in North Dakota who linger with symptoms for weeks and months using standard of care medicine AKA the tincture of time was HBOT NOTE Maroon and Bost in 2011 write that nonpharmaceutical alternatives dietary supplements and hyperbaric oxygen may be a better first line choice for the treatment of PCS which has generally been underreported by both athletes and the military 35 Of note for the CMS population is the work of Dr Anne McKee on the connections between concussion and Chronic Traumatic Encephalopathy CTE 36 CTE is a progressive neurodegeneration clinically associated with memory disturbances behavioral and personality change Parkinsonism and speech and gait abnormalities traumatic injury may interact additively with Alzheimer s Disease to produce a mixed pathology with greater clinical impact or synergistically by promoting pathological cascades that result in either AD or CTE Of no small importance is groundbreaking research from Washington State University Researchers found that HBOT can halve the pain and symptoms of opiate withdrawal detox 37 And in current investigations of the use of HBOT to arrest and reverse the effects of COVID 19 preliminary evidence from China 38 five cases strongly suggests that based on the immutable science of HBOT and recent clinical application to deteriorating severely hypoxemic COVID 19 pneumonia patients HBOT has significant potential to impact the COVID 19 pandemic Fifty eight patients as of this writing have been positively affected Further clinicians in at least five independent studies in the US using HBOT are raising the PO2 levels in patients in ICUs to the point where they avoid being put on ventilators and in many cases are being sent home after as few as five treatments 39 5 Decades of science studying HBOT to treat TBI A review of the scientific evidence produced in both animal and human HBOT trials over the past twenty years demonstrates conclusively that Hyperbaric Oxygenation of TBI is safe and effective 40 As early as 1977 Holbach and Wasserman demonstrated that HBOT at 1 5ata puts the most oxygen into the brains 6
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 of chronic stroke patients 41 The overriding principle of wound healing of course is that the wound must have energy and oxygen to heal Hypoxia is the most pervasive result of brain insults of all kinds occasioned by inflammation that leads to reduced oxygen delivery to all body organs Following a Consensus Conference in 2008 at which it was declared that HBOT was safe 42 DoD Army VA researchers commenced a series of studies to discern whether HBOT was effective in treating TBI Those studies over nearly eight years consumed over 126Million Other studies in the private sector costing orders of magnitude fewer dollars were also conducted To date there have been at least seventeen peer reviewed studies that have produced data and findings 43 U S and Israelis clinical trials have provided well structured controlled studies demonstrating HBOT medicinal properties in mild TBI and persistent postconcussive symptoms 44 Positive symptom scores for TBI and PTSD symptom scores for the two government sponsored studies 45 the Army sponsored study of Miller et al 46 a civilian sponsored study of Harch et al 47 and an Israeli civilian study 48 show statistically significant improvements over baseline after HBOT treatments The studies involved patients with TBI who also suffered from Persistent PostConcussive Syndrome PPCS for at least two years It was highly unlikely that spontaneous recovery would occur Five studies provide useful cross study comparable measures The U S studies used the Immediate Post Concussion Assessment Cognitive Testing Rivermead Post Concussion Questionnaire and PTSD Checklist Military PCL M as the primary and secondary endpoint measures Even though the Army VA DoD sponsored studies claim to be sham controlled they are really dosing and pressure varying trials Clinical improvements in the studies were significant and consistent Looking at dose response profiles shows that lower oxygen levels 100 O2 and lower pressures 2 0 ATA are probably better for PTST mTBI and PPCS symptom recovery Government sponsored study authors assumed incorrectly that their control groups received inactive treatment Yet they write We recognize that a sham is not inert and we cannot completely discount the physiological effects of minimal increases in nitrogen or oxygen from pressurized room air However we believe it is biologically implausible that air at 1 2 ATA equivalent to 2 m of seawater pressure has a beneficial effect on healing the damaged brain remotely after mTBI 49 It is worth noting that the comment bears on relationship to the established science about the medicinal effects of low levels of either oxygen or pressure 50 Positive improvements from pretreatment baseline measures are observed in all the DoD VA Army and civilian studies The measured responses to both HBO and HBA treatment groups are therapeutic but a minimal effective dose of O2 at 1ata pressure has not been established in the hyperbaric medical literature Thus the use of a sham is problematic and confounding for study interpretation Deng and his team in a metanalysis evaluated nine studies comparing the efficacy between hyperbaric oxygen treatment and controls in traumatic brain injury patients 51 Brain metabolism cognitive function and outcome were taken into consideration Results showed that HBO treatment significantly improved the Glasgow outcome scale GOS score and reduced overall mortality in patients with severe TBI compared with controls In patients with mild TBI HBO showed function alleviating the cognitive disorder after trauma including memory executive function attention and information processing speed In patients with TBI HBO showed significant improvement of Glasgow outcome scale score and reduction of overall mortality while NBO may play a favorable role in improving brain metabolism 7
Advancement and New Understanding in Brain Injury 6 Implications of the science For over four years clinical and evidence based medicine continue to show that HBOT is safe and effective in treating brain injuries Objective analysis of the data from all the pivotal RCTs and crossover studies show in over 700 patients that positive improvements result from HBOT treatment protocols And objective analyses of the studies and data reinforce the findings and the clinical evidence 52 Dr Wolf is a principle co author of the first Army study This recent USAF paper reanalyzing the data in the cornerstone DOD VA Army study concludes This pilot study demonstrated no obvious harm and both groups showed improvement in scores and thus a benefit Subgroup analysis of cognitive changes and PCL M results regarding PTSD demonstrated a relative risk of improvement There is a potential gain and no potential loss The VA Clinical Practice Guidelines define a B evidence rating as a recommendation that clinicians provide the service to eligible patients At least fair evidence was found that the intervention improves health outcomes and concludes that benefits outweigh harm Hyperbaric oxygen therapy for mild traumatic brain injury and PTSD should be considered a legitimate adjunct therapy if future studies demonstrate similar findings or show comparable improvement to standard of care or research related treatment modalities 53 Subsequent studies meet those criteria The Journal of Hyperbaric Medicine is the most prestigious journal on Hyperbaric Medicine in the world In 2012 its editor wrote While we applaud good science there comes a point of stagnation as the standard of evidence required for the blessing of organized medicine exceeds reality where most of us live I feel as do many of my colleagues that there is sufficient clinical and research evidence to justify the use of HBOT as a standard of care treatment for TBI that should be reimbursed by CMS and Tricare I have no doubt that over the next several years HBOT will be proven beyond a reasonable doubt to be one of the most effective treatments for TBI There is a preponderance of evidence now to justify the use and funding for the treatment 54 Wang et al concur Compelling evidence suggests the advantage of hyperbaric oxygen therapy HBOT in traumatic brain injury Patients undergoing hyperbaric therapy achieved significant improvement with a lower overall mortality suggesting its utility as a standard intensive care regimen in traumatic brain injury 55 The Samueli Institute wrote of DoD studies Results showed that both the HBO and sham procedures were associated with significant improvements in post concussion symptoms and secondary outcomes including PTSD which most participants had depression sleep quality satisfaction with life and physical cognitive and mental health functioning these results are consistent with 2 other sham controlled clinical trials among service members and veterans involving a range of HBOT doses The most remarkable lesson of this study was the difference in clinical outcomes between the 2 chamber procedures HBO 1 5 ATA and sham air 1 3 ATA and routine post concussion care These findings reinforce the argument that effective interventions i e the current standard of care practiced by military medicine do not yet exist within the present structure of care or that routine post concussion interventions within the DOD or VHA may even have iatrogenic effects that contribute to symptom persistence the equivalent of a negative placebo nocebo effect 56 While this research has been going on the VA has been quietly conducting a controlled demonstration project to monitor the effects of HBOT for PTSDonly veterans For nearly three years first two and now five sites around the US are using HBOT to treat PTSD and TBI patients Tulsa OK Travis AFB Joint Base Sam Houston Tampa and Fargo ND While the numbers are small the results are 8
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 extremely positive 30 out of 30 patients have all shown positive medical improvement 57 Significantly numerous of the participants are diagnosed with TBI by the VA or have been found to have undiagnosed TBI Either way the overwhelming number of patients have improved significantly These results are significant for reasons related to previous attempts to treat PTSD The National Academies writing in 2014 stated DoD and VA are spending substantial time money and effort on the management of PTSD in service members and veterans 9 3Billion through 2014 yet neither department knows with certainty whether those many programs and services are actually successful in reducing the prevalence of PTSD in service members or veterans and in improving their lives 58 A Summary of the positive findings in the studies sponsored by DoD VA Army is instructive They find that HBOT offered statistical and in some measures clinically significant improvement over local routine TBI care They even note the improvements in all groups when measured against the no treatment group Even their expert consultants wrote that HBOT heals brain injuries The Army s premier researcher Dr Scott Miller despite seeming to be looking for the final nail in the coffin of HBOT says on the Veterans Affairs web site People did get better and we can t ignore those results 59 7 NOTE BENE the sham and placebo controversies in HBOT Expert commentary on the issues surrounding the HBOT sham revealed the fundamental flaws in the DoD VA Army research 60 In a sham treatment the researcher goes through the motions without actually performing the treatment The intent is to have an inert or medically inactive procedure or substance used to compare results with active substances A placebo is often used with half the people in a drug trial to help show whether the drug being studied is more effective than an inactive sugar pill The results of each group are compared NOTE Debate continues on whether it is possible under the circumstances of HBOT treatment to construct a true sham controlled study The placebo effect is very difficult if not impossible to prove in HBOT studies on patients suffering from PPCS that accompanies TBI Further studies cannot ignore a placebo but the overwhelmingly positive effects in so many and so widely different studies make the likelihood of a placebo unusual NOTE when physiologic changes such as both structural and functional increases in brain mass and activity are noted as they were not in DoD VA Army studies since they refuse to perform such objective science it is impossible to ascribe the changes to the placebo effect In numerous of the non government published peer reviewed studies on the use of HBOT for TBI however such positive transformations have been noted in the treated patients Objective evidence of changes are shown in peerreviewed research using such methods as SPECT scans RightEye qEEG etc Those changes can only be the effect of exposure to HBOT 61 A worldwide surge of challenges arose when the DoD Army VA studies purported to use a sham in their studies and reported that HBOT does not work 62 International researchers and authorities could read that both the data and the discussion in all the purported randomized controlled studies said virtually the same thing Both intervention groups sham and treated demonstrated improved outcomes compared with PCS care alone 63 Dr Pierre Marois spoke for many By definition sham is something false or empty Hyperbaric treatments at 1 2 ATA substantially increase the amount of dissolved oxygen in the blood and simultaneously induce cascades of metabolic changes and genes activation Therefore the supposedly sham treatment of Miller s study is not close to being a placebo 64 9
Advancement and New Understanding in Brain Injury The clearest example to date that demonstrates that these gas pressure combinations have a therapeutic effect on brain injury models is the article by Malek et al 65 They demonstrated that HBO 100 O2 and HBA 21 O2 79 N2 were equivalent in protecting neurons after transient forebrain ischemia in the gerbil using 2 5 ATA The role of a potential placebo effect was ruled out in this study and demonstrates the activity of HBO and HBA in a neurologic injury model The certainty that hyperbaric medicine begins with any increase in oxygen concentration and or pressure is further substantiated by on going work at the University of Wisconsin 66 Animal studies already show a significant increase in mobilized stem progenitor cells and decrease in Inflammatory cytokines when HBOT and HBAT room air are applied at pressures as low as 1 2ata Together these findings support the likelihood of biologic activity consubstantial with HBOT being activated at much lower dose of hyperoxia than previously postulated Those results coupled with decades of experiments by the US Navy and US Air Force 67 demonstrate that the Army s and UHMS s claims that hyperbaric medicine only occurs at pressures higher than 1 4ata are fallacious Any increase in oxygen concentration and or pressure is a medical intervention The USAF TBI study used the Agency for Healthcare Quality and Research recommendations for future HBOT research for TBI One pertinent comment was the following Whether placebo controlled trials are necessary to evaluate HBOT has received a great deal of attention in discussions about HBOT Participants on all sides of this debate make the assumption that an evidence based approach implies devotion to double blind placebo controlled trials without regard to practical or ethical considerations This assumption is false Double blind placebo controlled trials are the gold standard for government regulators overseeing the approval of new pharmaceuticals but not for clinical decision making or insurance coverage decisions Evidence based clinical decisions rely more heavily on comparisons of one treatment to other potentially effective therapies not to placebos 68 8 The economic argument in favor of coverage In what will be a ground breaking analysis released on Veterans Day November 11 2020 The TreatNOW Coalition building on the seminal work done in 2011 69 will update and expand the true cost of ownership to the American taxpayer of untreated brain injuries Most studies attempting to estimate costs typically pay attention to the obvious cost categories drugs yearly health care costs ER visits hospitalizations psychiatric care home health care long term care lost wages and sometimes even the impact on the family TreatNOW has gone much further in examining the ripple effect through the family and into society The Study looks at impact on the family in categories such as physical and mental damage to immediate family members including children and care givers social services for children affected by turmoil and spousal suicides occasioned by violence and abuse Divorce homelessness drug abuse incarceration death bycop and the estimated 135 people seemingly affected with every suicide 70 A major cost to society beyond the medical expenditures are the tax implications of taking a brain wounded citizen out of the work force In too many cases that actually equates to two lost incomes and taxes because a care giver is typically a full time aide to the wounded Brain Injury Facts about veterans are hard to pin down accurately since there are so much missing data For example the VA estimates that 70 of veterans are not part of the VA system The VA also estimates TBIs alone for the period of 2000 2017 is over 414 000 RAND estimates that about one third of all returning vets reported 10
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 symptoms of some mental health or cognitive condition More recent estimates range up to 800 000 for post 9 11 and an equal number of living veterans from service in the 20th century Civilian casualties are estimated by the CDC as 2 5 million per year with more than 5 million American effectively unemployable and unable to perform activities of daily living To summarize a much more robust analytical picture untreated brain injuries cost billions of dollars each year when many of them could be reversed by application of HBOT to help heal the underlying and frequently ignored or misdiagnosed brain injury It costs somewhere between 40 000 and 60 000 per year for each brain injured patient HBOT treatment has shown an 85 probability of making a significant contribution to the health and welfare of treated patients at a cost of approximately 20 000 Thus for less than 2 of the costs of sustaining the brain wounded on welfare those brain injuries could be treated The possibility of returning Quality of life and independence to a significant fraction of those wounded is high 9 Coverage with evidence Should further research be required before HBOT for TBI receives an indication the Center for Medicare and Medicaid CMS issued Guidance for the Public Industry and CMS Staff Coverage with Evidence Development November 20 2014 71 CMS and AHRQ declared that the principal purpose of the study would be to test whether the item or service HBOT for TBI meaningfully improves health outcomes of affected beneficiaries who are represented by the enrolled subjects Unsurprisingly the data and the demographics support immediate use of HBOT 10 Conclusion It has been the experience of independent scientists over the last decade that peer reviewed evidence from around the world attests to the safety and efficacy of HBOT in treating and helping to heal TBI and other neurological disorders Yet the bulk of research on brain diseases and injury focuses on description and causes rather than treatments Research into treatments is by design focused on treating symptoms Clinical Practice Guidelines from the VA DoD for example specifically focus on the management of concussion mild traumatic brain injury 72 Their CPG is a compendium of best practices for dealing with symptoms not with healing or curing No mention is made in the document of the wound to the brain nor to healing that wound And none of the treatments listed as standard of practice are approved by the FDA for treating TBI 73 Unsurprisingly huge sums are being poured into worldwide research some coordinated most in a competitive surge to devise better ways to understand the structure function aberrations and diseases and treatments for the brain The US the Brain Initiative Europe Human Brain Project Japan Brain MINDS Project China Brain Project Israel Australia and Canada have funded major projects 74 Groups like One Mind and Paul Allen s Brain Institute are exploring how the brain works and what causes neurological disorders While the projects vary slightly in their aims the thrust is on knowledge rather than clinical medicine and healing Longer term goals of course include medicine to the patient Yet precious little in all the efforts is being done to find immediate use methods to intervene in areas of wide and profound importance to human mental health 11
Advancement and New Understanding in Brain Injury On a more mundane basis federal state local public and private efforts continue year after year to address in conferences and papers and legislation the perennial interrelated issues of suicide mental health brain injury addiction and neurocognitive and neurological decline It is hardly surprising that the expenditures promise phenomenal rewards for breakthroughs Meanwhile billions are expended treating symptoms of underlying brain damage that the science demonstrates is both treatable and potentially reversible not later but now Wright and Figueroa summarize for the majority of researchers on the use of HBOT to treat and help heal TBI There is sufficient evidence for the safety and preliminary efficacy data from clinical studies to support the use of HBOT in mild traumatic brain injury persistent post concussive syndrome mTBI PPCS The reported positive outcomes and the durability of those outcomes has been demonstrated at 6 months post HBOT treatment Given the current policy by Tricare and the VA to allow physicians to prescribe drugs or therapies in an off label manner for mTBI PPCS management and reimburse for the treatment it is past time that HBOT be given the same opportunity This is now an issue of policy modification and reimbursement not an issue of scientific proof or preliminary clinical efficacy 75 It is time to recognize the worldwide body of data reduce healthcare costs improve the lives of millions of brain wounded and their families and avoid lifetimes of lost earnings and the social impact of avoidable suffering HBOT should be endorsed for the treatment of Traumatic Brain Injury This can be achieved by extending CMS coverage to this diagnosis Author details Robert Louis Beckman Foundation for the Study of Inflammatory Disease TreatNow org North Bethesda USA Address all correspondence to heal treatnow org 2020 The Author s Licensee IntechOpen This chapter is distributed under the terms of the Creative Commons Attribution License http creativecommons org licenses by 3 0 which permits unrestricted use distribution and reproduction in any medium provided the original work is properly cited 12
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 References 1 DISCOVER The Dr Who Drank Infectious Broth Gave Himself an Ulcer and Solved a Medical Mystery http discovermagazine com 2010 mar 07dr drank broth gave ulcer solvedmedical mystery 2 See Germs Are Us Exploring the Human Microbiome Michael Specter The New Yorker October 22 2012 http www newyorker com reporting 2012 10 22 121022fa_fact_ specter Casualty Evaluation for Head Injury and Arterial Air Embolis Definitive Therapy in Hyperbaric Chamber Also it was reiterated again in 2006 that combat casualty care for traumatic brain injury was HBOT Zajtohuk R Ed in Chief Textbook of Military Medicine Series on Combat Casualty Care Part 1 Vol 6 p 313 7 Giza C C and Hovda D A The New for Medicare Medicaid Coverage of Hyperbaric Oxygen Therapy Treatment of Diabetic Foot Wounds June 2001 Neurometabolic Cascade of Concussion Neurosurgery October 2014 75 0 4 S24 S33 James P B Philip B James MD Oxygen and the Brain the Journey of Our Lifetime North Palm Beach FL Best Publishing Co 2014 Chap 19 Head Injuries the curse of life in the fast lane 4 Harch PG Neubauer RA Hyperbaric 8 James p 333 3 Harch Paul G M D Argument oxygen therapy in global cerebral ischemia anoxia and coma Chapter 18 In Jain KK ed Textbook of Hyperbaric Medicine 3rd Revised Edition Seattle WA USA Hogrefe and Huber Publishers 1999 319 345 9 Centers for Disease Control and hbo indications html Prevention 2019 Surveillance Report of Traumatic Brain Injuryrelated Emergency Department Visits Hospitalizations and Deaths United States 2014 Centers for Disease Control and Prevention U S Department of Health and Human Services 6 A growing body of literature related 10 https www usnews com to blast injury and TBI PTSD attests to the damage attributable to combat Various names have been used to describe the damage done by blasts Shell Shock Soldier s heart Battle fatigue Anxiety disorder Railway spine Stress syndrome Nostalgia Combat stress reaction Traumatic war neurosis Invisible wounds Post traumatic stress disorder and Traumatic brain injury For a full bibliography on a decades long body of research and data see https treatnow org knowledgebase 3 blast biography and https treatnow org knowledgebase_ category 2020 Bibliography Importantly the United States Army Textbook of Military Medicine 1991 Neurological Abnormalities of the Blast news healthiest communities articles 2019 11 21 suicide is topcause of deaths tied to traumaticbrain injury 5 https www uhms org resources 13 11 https www brainandspinalcord org brain injury statistics 12 https www cdc gov traumaticbraininjury severe html 13 See https treatnow org knowledgebase untreated braininjuries_costs to society 14 Giza and Hovda S24 S33 15 Leila H Eadie editorial New technology and potential for
Advancement and New Understanding in Brain Injury telemedicine in battlefield brain injury diagnostics Concussion 2016 1 4 CNC22 16 Behnke A R et al The circulatory and respiratory disturbances of acute compressed air illness and the administration of oxygen as a therapeutic measure American Journal of Physiology 114 3 526 533 http ajplegacy physiology org cgi content citation 114 3 526 January 31 1936 17 Management of Post Traumatic Stress Working Group VA DoD Clinical Practice Guidelines for Management of Post Traumatic Stress Washington D C Department of Veteans Affairs and Department of Defense Oct 2010 Available at www healthquality va gov PTSD FULL 2010c pdf 18 Controversy continues to wage over proper diagnoses of TBI and PTSD The authors are aware from over a decade of clinical medicine and the accumulation of anecdotal evidence in over 7 200 successful uses of HBOT to help treat and heal TBI that those veterans presenting with PTSD only diagnoses from the VA are overwhelmingly afflicted with undiagnosed TBI Further although populations at high risk for PTSD e g military populations have a high incidence of exposure to traumatic brain injury TBI additional work is needed to fully characterize the ways in which TBI can affect the clinical and neurological presentation of PTSD Spadoni A D Huang M Simmons A N 2018 Emerging approaches to neurocircuits inPTSD and TBI imaging the interplay of neural and emotional trauma Curr Top Behav Neurosci 38 163 192 Tanev K S Pentel K Z Kredlow M A Charney M E 2014 PTSD and TBI co morbidity scope clinical presentation and treatment options Brain Inj 28 261 270 https doi org 10 3109 02699052 2013 873821 and Vasterling J J Verfaellie M Sullivan K D 2009 Mild traumatic brain injury 14 and posttraumatic stress disorder in returning veterans perspectives from cognitive neuroscience Clin Psychol Rev Posttraumatic Stress Disorder Wars Afghanistan Iraq 29 674 684 https doi org 10 1016 j cpr 2009 08 004 19 Baughman Shively S Iren Horkayne Szakaly Robert V Jones James P Kelly Regina C Armstrong Daniel P Perl Characterisation of interface astroglial scarring in the human brain after blast exposure a post mortem case series The Lancet Neurology June 2016 DOI http dx doi org 10 1016 S1474 4422 16 30057 6 20 Worth RF What if PTSD Is More Physical Than Psychological A new study supports what a small group of military researchers has suspected for decades that modern warfare destroys the brain New York Times JUNE 10 2016 http nyti ms 1TYYp6U 21 van der Kolk B The Body Keeps the Score Brain mind and body in the healing of trauma London Penguin Publishing Group 2014 22 Amir Hadanny Shai Efrati 2016 Treatment of persistent post concussion syndrome due to mild traumatic brain injury current status and future directions Expert Review of Neurotherapeutics DOI 10 1080 14737175 2016 1205487 Harch PG Hyperbaric oxygen in chronic traumatic brain injury oxygen pressure and gene therapy Med Gas Res 2015 5 9 Harch PG The genetically modulated healing effects of hyperbaric oxygen therapy Altern Ther Health Med 2015 21 46 55 and Figueroa XA Wright JK Clinical results in brain injury trials using HBO2 therapy another perspective Undersea Hyperb Med J 2015 42 19 23 Extensive bibliographies on the use of HBOT for brain wounds and other injuries can be found in Jain KK The
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 Textbook of Hyperbaric Medicine Fifth edition Cambridge MA Hogrefe Huber Publishers 2009 Philip B James MD Oxygen and the Brain the Journey of Our Lifetime North Palm Beach FL Best Publishing Co 2014 and Paul G Harch MD and Virginia McCullough The Oxygen Revolution Third Edition Hyperbaric Oxygen Therapy The Definitive Treatment of Traumatic Brain Injury TBI Other Disorders Hatherleigh Press 2016 24 https www research va gov topics tbi cfm 33 Oddo M Levine JM Mackenzie L et al Brain hypoxia is associated with short term outcome after severe head injury independently of intracranial hypertension and low cerebral perfusion pressure Neurosurgery 2011 69 1037 1045 34 https tinyurl com ybldktqn 35 Maroon J C and Bost J Concussion management at the NFL College High School and Youth Sports Levels Chap 7 in textbook Clinical Neurosurgery Vol 58 The Congress of Neurological Surgeons 2011 p51 25 Stephen R Thom Hyperbaric oxygen its mechanisms and efficacy Plast Reconstr Surg 2011 Jan 127 Suppl 1 131S 141S 26 Godman C A et al Hyperbaric oxygen treatment induces antioxidant gene expression ANNALS OF THE NEW YORK ACADEMY OF SCIENCES 02 June 2010 https doi org 10 1111 j 1749 6632 2009 05393 x rd 27 Harch and McCullough 3 Edition 36 McKee A C et al Chronic Traumatic Encephalopathy in Athletes Progressive Tauopathy following Repetitive Head Injur J Neuropathol Exp Neurol 2009 Jul 68 7 709 735 37 Daniel Nicoara Raymond M Quock et al Hyperbaric oxygen treatment suppresses withdrawal signs in morphine dependent mice Brain Research 2016 1648 434 DOI 10 1016 j brainres 2016 08 017 Chapter 1 38 Harch PG Hyperbaric oxygen 28 American Hospital Directory www ahd com 29 Harch Paul G M D Argument for Medicare Medicaid Coverage of Hyperbaric Oxygen Therapy Treatment of Diabetic Foot Wounds June 2001 The 129 references accompanying that document have been incorporated into the References accompanying this Application 30 James Oxygen and the Brain Chapter 19 31 Kelly Jr DL et al Effects of hyperbaric oxygenation and tissue oxygen studies in experimental paraplegia JNS Journal of Neurosurgery 1972 36 425 429 32 Oxygen and the Brain p 339 15 treatment of novel coronavirus COVID 19 respiratory failure Med Gas Res Epub ahead of print Apr 24 2020 http www medgasres com preprintarticle asp id 282177 Through Henry s Law HBOT enhances multiple stages in respiratory failure by increasing 1 the dissolving of oxygen in the alveolar and inflammatory barrier 2 the diffusion rate of oxygen 3 the diffusion distance of oxygen 4 the dissolution of oxygen in blood plasma 5 the oxygen saturation of hemoglobin in red blood cells and 6 the delivery of oxygen to the microcirculation and tissue The net result is a reversal of the downward spiral of COVID 19 patients note HBOT affects similar processes in the degenerative concussion cascade after TBI The elevation of systemic levels of oxygen with HBOT has been
Advancement and New Understanding in Brain Injury traditionally misunderstood in terms of respiratory metabolite effects with a transient hyperoxemia that dissipates once the patient leaves the chamber However for 358 years and especially in the modern era 1960 to present permanent and later trophic effects of HBOT have been documented with both single and repetitive HBOT 3 One of the mechanisms of action was recently elucidated as epigenetic modulation through direct effects of hydrostatic pressure and hyperoxia of gene expression suppression of over 40 of the protein coding genes in the human genome The largest clusters of upregulated genes are the growth repair cell signaling and antiinflammatory genes and the largest clusters of down regulated genes are the pro inflammatory genes and those that control programmed cell death A single HBOT has been shown in multiple studies to have dramatic persisting effects on disease pathophysiology especially inflammation its ubiquitous acute form reperfusion injury e g carbon monoxide poisoning necrotizing infection resuscitation and others and extreme forms of acute respiratory distress syndrome ARDS and on reversing the lethal oxygen debt from cardiac arrest In the Chinese COVID19 patients HBOT was likely treating pulmonary and systemic hypoxia inflammation other pulmonary pathophysiologic targets reversing oxygen debt and modulating gene expression both acutely and durably as evidenced by the patient s sustained improvement with each daily HBOT These are similar processes experienced in use of HBOT to treat TBI yet another substantiation of HBOT Mechanisms of Action Ironically the Chinese physicians replicated an historical experience with HBOT in a near identical pulmonary viral pandemic the Spanish flu pandemic of 1918 Dr Orval Cunningham of Kansas City USA applied hyperbaric oxygen therapy pressure and oxygen to a moribund cyanotic Spanish flu patient with agonal 16 breathing who experienced the same dramatic reversal of his disease that the Chinese physicians witnessed See Zhong X Tao X Tang Y Chen R The outcomes of hyperbaric oxygen therapy to retrieve hypoxemia of severe novel coronavirus pneumonia first case report Zhonghua Hanghai Yixue yu Gaoqiya Yixue Zazhi 2020 doi 10 3760 cma j issn 1009 6906 2020 0001 Zhong XL Niu XQ Tao XL Chen RY Liang Y Tang YC The first case of HBOT in critically ill endotracheal intubation patient with COVID 19 Beijing China Novel Coronavirus Pneumonia Research Network Sharing Platform of China Association for Science and Technology 2020 Jain KK Textbook of Hyperbaric Medicine 6th ed Cham Switzerland Springer 2017 Rogatsky GG Shifrin EG Mayevsky A Acute respiratory distress syndrome in patients after blunt thoracic trauma the influence of hyperbaric oxygen therapy Adv Exp Med Biol 2003 540 7785 Sellers LM The fallibility of the forrestian principle semper primus pervenio maxima cum VI Laryngoscope 1964 74 613 633 39 Thibodeaux K Speyrer M Raza A Yaakov R Serena TE Hyperbaric oxygen therapy in preventing mechanical ventilation in COVID 19 patients a retrospective case series J Wound Care 2020 May 1 29 Sup5a S4 S8 40 Figueroa HBOT Clinical Studies 2020 available at https treatnow org knowledgebase hbot significantresearch showing the safety andefficacy of hbot for tbi ptsd This spread sheet contains seventeen peerreviewed scientific papers on the use of HBOT for TBI 41 Holbach KH Caroli A Wassmann H Cerebral energy metabolism in patients with brain lesions of normo and hyperbaric oxygen pressures J Neurol 1977 217 17 30
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 42 DoD HBOT for TBI Consensus Conference White Paper 28 October 2008 randomized prospective trial PLoS One 2013 8 e79995 49 Miller RS Weaver LK Bahraini N 43 Figueroa HBOT Clinical Studies 2020 see note 31 44 Xavier A Figueroa PhD and James K Wright MD Col Ret USAF Hyperbaric Oxygen B Level Evidence in Mild Traumatic Brain Injury Clinical Trials Neurology 2016 87 1 7 et al Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms a randomized clinical trial JAMA Intern Med 2015 175 43 52 50 James MacLaughlin Thom Marois etc 45 Cifu DX Walker WC West SL et al 51 Deng Z Chen W Jin J Zhao J Xu H Hyperbaric oxygen for blast related postconcussion syndrome three month outcomes Ann Neurol 2014 75 277 286 Cifu DX Hart BB West SL Walker W Carne W The effect of hyperbaric oxygen on persistent postconcussion symptoms J Head Trauma Rehabil 2014 29 11 20 Wolf G Cifu D Baugh L Carne W Profenna L The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury J Neurotrauma 2012 29 2606 2612 Weaver LK Wilson SH Lindblad AS et al Hyperbaric oxygen for postconcussive symptoms in United States military service members a randomized clinical trial Undersea Hyperb Med 2018 45 129 156 The neuroprotection effect of oxygen therapy A systematic review and meta analysis Niger J Clin Pract 2018 Apr 21 4 401 416 46 Miller RS Weaver LK Bahraini N et al Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms a randomized clinical trial JAMA Intern Med 2015 175 43 52 52 Wang F et al Hyperbaric oxygen therapy for the treatment of traumatic brain injury a meta analysis Neurol Sci 2016 Jan 8 PubMed PMID 26746238 and Deng Z Chen W Jin J Zhao J Xu H The neuroprotection effect of oxygen therapy A systematic review and meta analysis Niger J Clin Pract 2018 Apr 21 4 401 416 53 E G Wolf L M Baugh C M S Kabban et al Cognitive function in a traumatic brain injury hyperbaric oxygen randomized trial UHM 2015 Vol 42 No 4 2015 http bit ly 2faBldN 54 UHM 2012 Vol 39 No 4 et al A phase I study of low pressure hyperbaric oxygen therapy for blastinduced post concussion syndrome and post traumatic stress disorder J Neurotrauma 2012 29 168 185 How many deaths will it take AN EDITORIAL PERSPECTIVE Undersea Hyperbaric Medical Society Inc How many deaths will it take till they know Monkeys madmen and the standard of evidence George Mychaskiw II DO FAAP FACOP Editor in Chief Chair Department of Anesthesiology Nemours Children s Hospital Orlando Florida USA 48 Boussi Gross R Golan H Fishlev G 55 Wang F et al Hyperbaric oxygen et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury therapy for the treatment of traumatic brain injury a meta analysis Neurol Sci 2016 Jan 8 PubMed PMID 26746238 47 Harch PG Andrews SR Fogarty EF 17
Advancement and New Understanding in Brain Injury 56 Samueli Institute Is Hyperbaric Oxygen Therapy Effective for Traumatic Brain Injury Preliminary Report Prepared for the Hyperbaric Oxygen Research Program USAMRMC USAMMDA February 18 2015 57 Center for Compassionate Innovation VHA Office of Community Engagement 10P10 Room 786 VA Central Office Washington DC 20420 202 461 6969 Email to communityengagement va gov 58 Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations Final Assessment The National Academies The Institute of Medicine Washington DC The National Academies Press 2014 https bit ly 2oYJ17l 59 https www research va gov currents winter2015 winter2015 9 cfm November 17 2014 doi 10 1001 jamainternmed 2014 5479 64 Pierre Marois MD FRCP c Physiatrist Dept of Pediatrics and Dept of Rehabilitation Ste Justine University Hospital Montreal Canada Letter to the Editor JAMA 10 20 2016 65 Malek M Duszczyk M Zyszkowski M Ziembowicz A Salinska E Hyperbaric oxygen and hyperbaric air treatment result in comparable neuronal death reduction and improved behavioral outcome after transient forebrain ischemia in the gerbil Exp Brain Res 2013 224 1 14 66 MacLaughlin KJ Barton GP Braun RK Eldridge MW Effect of intermittent hyperoxia on stem cell mobilization and cytokine expression Med Gas Res 2019 Jul Sep 9 3 139 144 PhD research will recommence after COVID 19 shutdown 60 Ibid and http brainjury org blog 2014 07 03 what the bleep iswrong with the dodva hbot studies 67 Oxygen and the Brain pp 352 354 68 McDonagh MS Carson S Ash JS 61 Hadanny A Abbott S Suzin G et al Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post traumatic brain injury patients retrospective analysis BMJ Open 2018 8 e023387 https bit ly 2RBOQSd et al Hyperbaric oxygen therapy for brain injury cerebral palsy and stroke Rockville MD Agency for Healthcare Research and Quality 2003 Sep AHRQ Publication No 03 E050 69 Doering N et al Untreated Brain 62 Hoge C W and Jonas W B The Ritual of Hyperbaric Oxygen and lessons for the Treatment of Persistent Postconcussion Symptoms in Military Personnel invited commentary in JAMA American Medical Association November 17 2014 p E 1 Injury Scope Costs and a Promising New Treatment Unpublished Research Report Reimers Systems Inc 2012 70 Editorial How many people are affected by one suicide Centre for Suicide Prevention Feb 24 2019 63 R Scott Miller M D COL US 71 https www cms gov Army Director Hyperbaric Oxygen Research Program US Army Medical Materiel Development Activity Ft Detrick MD Effects of Hyperbaric Oxygen on Symptoms and Quality of Life Among Service Members With Persistent Postconcussion Symptoms JAMA Intern Med Published online medicare coverage database details medicare coverage document details aspx MCDId 27 18 72 Grammar G G DeGrabe T J and Picon L M VA DoD CLINICAL PRACTICE GUIDELINE FOR THE MANAGEMENT OF
Hyperbaric Oxygenation in the Treatment of Traumatic Brain Injury DOI http dx doi org 10 5772 intechopen 94401 CONCUSSION MILD TRAUMATIC BRAIN INJURY VHA VA HSR D Cyberseminars 2016 Update 73 See https treatnow org knowledgebase va_dod interventionsand responses to invisible wounds 74 See for example https www newscientist com article dn27318megabucks pouring into global brainscience projects ixzz6O7t8RSuc 75 Ibid 19
ORIGINAL RESEARCH published 19 October 2017 doi 10 3389 fnhum 2017 00508 Hyperbaric Oxygen Therapy Can Induce Angiogenesis and Regeneration of Nerve Fibers in Traumatic Brain Injury Patients Sigal Tal 1 2 Amir Hadanny 1 3 4 Efrat Sasson 5 Gil Suzin 3 and Shai Efrati 1 3 6 7 1 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 2 Radiology Department Assaf Harofeh Medical Center Zerifin Israel 3 Sagol Center for Hyperbaric Medicine and Research Assaf Harofeh Medical Center Zerifin Israel 4 Faculty of Medicine Bar Ilan University Ramat Gan Israel 5 WiseImage Hod Hasharon Israel 6 Research and Development Unit Assaf Harofeh Medical Center Zerifin Israel 7 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Background Recent clinical studies in stroke and traumatic brain injury TBI victims suffering chronic neurological injury present evidence that hyperbaric oxygen therapy HBOT can induce neuroplasticity Objective To assess the neurotherapeutic effect of HBOT on prolonged post concussion syndrome PPCS due to TBI using brain microstructure imaging Edited by Manousos A Klados Aston University Birmingham United Kingdom Reviewed by Baris Saylam Ankara Numune Training Hospital Turkey Jacek Kot Medical University Poland Gdansk Correspondence Amir Hadanny amir had gmail com Shai Efrati efratishai 013 net These authors have contributed equally to this work Received 30 March 2017 Accepted 06 October 2017 Published 19 October 2017 Citation Tal S Hadanny A Sasson E Suzin G and Efrati S 2017 Hyperbaric Oxygen Therapy Can Induce Angiogenesis and Regeneration of Nerve Fibers in Traumatic Brain Injury Patients Front Hum Neurosci 11 508 doi 10 3389 fnhum 2017 00508 Methods Fifteen patients afflicted with PPCS were treated with 60 daily HBOT sessions Imaging evaluation was performed using Dynamic Susceptibility Contrast Enhanced DSC and Diffusion Tensor Imaging DTI MR sequences Cognitive evaluation was performed by an objective computerized battery NeuroTrax Results HBOT was initiated 6 months to 27 years 10 3 3 2 years from injury After HBOT DTI analysis showed significantly increased fractional anisotropy values and decreased mean diffusivity in both white and gray matter structures In addition the cerebral blood flow and volume were increased significantly Clinically HBOT induced significant improvement in the memory executive functions information processing speed and global cognitive scores Conclusions The mechanisms by which HBOT induces brain neuroplasticity can be demonstrated by highly sensitive MRI techniques of DSC and DTI HBOT can induce cerebral angiogenesis and improve both white and gray microstructures indicating regeneration of nerve fibers The micro structural changes correlate with the neurocognitive improvements Keywords hyperbaric oxygen DTI tractography angiogenesis MRI perfusion TBI post concussion INTRODUCTION Traumatic brain injury TBI is a significant public health concern in military and civilian populations Chiu and LaPorte 1993 The estimated number of TBI cases occurring each year is 10 million globally and 1 7 3 8 million in the United States alone 75 90 of those are defined as mild TBI mTBI Selassie et al 2013 Marin et al 2014 Frontiers in Human Neuroscience www frontiersin org 1 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI The post concussion syndrome PCS is a complex of symptoms consisting of headaches dizziness imbalance vertigo fatigue changes in sleep pattern neuropsychiatric symptoms e g behavioral and mood changes confusion and cognitive impairments in memory attention concentration and executive functions McCauley et al 2005 PCS is most often described in the setting of mTBI but may also occur after moderate and severe TBI In Eight to Ninty percent of mTBI cases the symptoms fade away in 7 10 days McCrory et al 2005 Hadanny and Efrati 2016 Still in 10 20 percent PCS may persist for weeks or months due to structural and or metabolic brain damage Twenty five to thirty three percent of those retain a permanent brain injury and experience persistent PCS the symptoms turn chronic and endure more than 6 months Kashluba et al 2004 Bazarian et al 2005 Iverson 2005 Sterr et al 2006 King and Kirwilliam 2011 The sensitivity of classic anatomical brain imaging techniques such as Computed Tomography CT and Magnetic Resonance Imaging MRI is generally not sufficient for detection of the pathophysiologic effects of mTBI New techniques are increasingly utilized for objective evaluation of brain damage Diffuse Tensor Imaging DTI can reveal the combination of axonal injury and secondary gliosis with local microvascular injury Niogi and Mukherjee 2010 Dynamic susceptibility contrast MR perfusion can demonstrate reduced cerebral blood flow CBF global and regional as well as cerebral blood volume CBV Tal et al 2015 The existing pharmacologic and non pharmacologic treatments have mostly failed to elicit efficacious results in both the clinical symptoms and the pathophysiologic cascade leading to permanent brain injury Hadanny and Efrati 2016 In recent years both basic animal models Neubauer and James 1998 Zhang et al 2005 Vlodavsky et al 2006 Chen et al 2010 Huang and Obenaus 2011 Lin et al 2012 Efrati and Ben Jacob 2014 and clinical studies Shi et al 2003 2006 Barrett et al 2004 Golden et al 2006 Wright et al 2009 Harch et al 2012 Boussi Gross et al 2013 Tal et al 2015 have shown that hyperbaric oxygen therapy HBOT can improve PCS by targeting the basic pathological processes responsible for post concussion symptoms Hadanny and Efrati 2016 In our previous study it was evident that HBOT can induce brain angiogenesis demonstrated by perfusion MRI with significant increase in CBF and CBV following HBOT along with significant cognitive improvement in patients post TBI Tal et al 2015 The current study was aimed at evaluating the effects of HBOT on brain microstructure in chronic neurological deficiencies stemming from TBI This has not been studied in humans so far the hospital 0030 15 ASF and registered in the US National Institute of Health Clinical Trials registry NCT02452619 Inclusion criteria Patients with chronic neurocognitive impairment started only after TBI persisting over 6 months who underwent two MRI brain imaging including DTI and DSC sequences and two neurocognitive tests pre and posthyperbaric oxygen therapy HBOT All patients applied for HBOT of their own volition Patients with other neurological conditions were excluded from the study s cohort The classification of TBI was based on the American Congress of Rehabilitation Medicine ACRM and the Centers of Disease Control CDC where mTBI is defined as altered brain function engendered by external forces with one or more of the following loss of consciousness with duration of 0 30 min post traumatic amnesia with duration of less than 24 h and Glasgow Coma Scale grade of 13 15 Malec et al 2007 GCS score of 3 8 or posttraumatic amnesia of more than 7 days or loss of consciousness for more than 24 h is classified as severe TBI GCS score of 9 12 or post traumatic amnesia of 1 7 days or loss of consciousness between 30 min and 24 h is classified as moderate TBI Malec et al 2007 METHODS Images were corrected for motion using SPM software version 12 UCL London UK DSC analysis was performed as described in previous studies stergaard et al 1996a b part I and II using in house software written in Matlab R2011 Mathworks Natick MA Detailed description is found in the Supplementary Material SI 1 In short MR signal intensity was converted to Gd concentration fitted to the gamma variate function and deconvolved on a voxel by voxel basis to calculate the CBF CBV and MTT Mean Transient Time maps Smoothing of 8 mm full Hyperbaric Oxygen Treatment Patients were treated in a multiplace hyperbaric chamber HAUX Life Support GmbH for 60 daily hyperbaric sessions 5 days a week Each session consisted of 90 min of exposure to 100 oxygen at 2 ATA Acceptable compression and decompression rates of 0 8 meter per minute were employed Oxygen was delivered by tight masks MRI Scan Protocol All patients had MRI scans 1 2 weeks before and after HBOT Imaging was done with a 3 Tesla system 20 channels MAGNETOM Skyra Siemens Medical Solutions with a multichannel head coil as a receiver coil The MRI protocol included the following sequences T2 weighted T1 weighted FLAIR susceptibility weighted imaging SWI dynamic susceptibility contrast enhancement DSC and diffusion tensor imaging DTI The MRI DTI and DSC sequences parameters are detailed in the supplementary material SI 1 The injected gadolinium 0 5 mmol ml dosage was 0 2 ml kg patient MRI Analysis MRI analysis was performed by WiseImage Hod Hasharon Israel http www wise image com DSC Analysis A retrospective analysis of patients suffering from chronic neurocognitive impairment due to TBI treated at Sagol Center for Hyperbaric Medicine and Research at Assaf Harofeh Medical Center Israel between September 2013 and December 2015 The study was approved by the Institutional Review Board of Abbreviations CBF cerebral blood flow CBV cerebral blood volume Frontiers in Human Neuroscience www frontiersin org 2 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI Schweiger et al 2003 Melton 2005 Each cognitive domain score was calculated out of 3 5 different tests It had 3 different forms of each test out of which we used one for pre exam and another for the post test This is a strong feature of these tests as it reduces the learning effect with a good test retest validity The fact that each index is referred to more than one test score ensures that the index is associated with a cognitive domain score rather than with a test dependent score width at half maxima FWHM was performed on the perfusion maps using the SPM software DTI Analysis Motion and Echo planar imaging EPI correction and regularization of the DWI volumes as well as calculation of DTI maps MD mean diffusivity FA fractional anisotropy AD axial diffusivity RD radial diffusivity maps were done using ExploreDTI software Leemans et al 2009 Two analysis types were performed voxel based analysis and fiber tracking Detailed description is found in the Supplementary Material SI 1 In short paired t test was performed using voxelbased analysis generating statistical parametric maps Fiber tracking was applied using Explore DTI software in order to plot 8 fiber tracts for each patient Uncinate fasciculus UF Cingulum inferior longitudinal fasciculus ILF and Inferior fronto occipital fasciculus IFOF in both hemispheres After the tracking procedure a mask was created from the tracts matrices of all subjects in order to create a tract mask Overall 8 masks were created for each subject four fiber tracts UF fornix cingulum ILF in both hemispheres The tract masks of the different patients were registered to a tract mask of one patient Statistical Analysis In addition to the MRI analysis described above continuous data were expressed as means standard errors The normal distribution for all variables was tested by means of the Kolmogorov Smirnov test The mean differences between cognitive index scores before and after HBOT were analyzed using two tailed paired t tests or a Wilcoxon signed rank test The alpha level was set to 0 05 Data were statistically analyzed using SPSS software version 22 0 RESULTS Cognitive Assessment Patients The assessment of cognitive functions was done by NeuroTrax computerized cognitive tests NeuroTrax Corp TX Dwolatzky et al 2003 The neurocognitive battery by Neurotrax is a validated computerized cognitive evaluation which was specifically designed to TBI patients These tests evaluate various aspects of brain function and incorporate Verbal Memory immediate and delayed recognition Non Verbal Memory immediate and delayed recognition Go No Go Response Inhibition Problem Solving Stroop Interference Finger Tapping Catch Game Staged Information Processing Speed single digit two digit and three digit arithmetic Verbal Function and Visual Spatial Processing Cognitive index scores were computed from the normalized outcome parameters for the following domains executive function memory attention speed of information processing visual spatial verbal function and motor skills Thaler et al 2012 Achiron et al 2013 Zur et al 2015 The verbal domain score was excluded because only 8 patients 53 had reliable calculated verbal domains A global cognitive score was computed as the average of all index scores for each individual The NeuroTrax data were uploaded to the NeuroTrax central server and outcome parameters were automatically calculated using a software blind to diagnosis or testing site To account for the effects of age and education on cognitive performance each outcome parameter was normalized and fit to an IQ like scale mean 100 S D 5 according to age and education The normative data used by NeuroTrax consist of test data from cognitively healthy individuals in controlled research studies at more than 10 sites Doniger 2014 Specifically the patients received two different versions of the NeuroTrax test battery before and after HBOT so as to produce minimal learning effects upon repeated administration Test retest reliability for those versions was found to be high Frontiers in Human Neuroscience www frontiersin org Fifteen patients with chronic cognitive impairment due to TBI who were treated at the Sagol Center for Hyperbaric Medicine and Research between September 2013 and December 2015 fulfilled the inclusion criteria The mean age was 35 8 3 5 years 21 70 and 53 8 15 were males All patients had documented traumatic brain injury 6 months to 27 years mean 6 7 2 1 years prior to HBOT Seven patients 46 7 suffered from moderate to severe TBI and 8 53 3 suffered from PCS after mTBI See patients baseline characteristics in Table 1 Baseline standard MRI findings for each of the patients are summarized in SI 2 TABLE 1 Patients baseline characteristic Age years 35 8 3 5 Sex Males 8 53 3 Females 7 46 7 Time from trauma years 6 7 2 1 Severity of trauma Mild 8 53 3 Moderate 2 13 3 Severe 5 33 4 MVA 13 86 7 Trauma type Fall 1 6 7 Assault 1 6 7 Medications 3 SSRI 3 20 Benzodiazepines 1 6 7 Opiates 2 13 3 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI Neurocognitive Function Decrease in MD was found in the frontal lobe anterior cingulate gyrus posterior orbital gyrus Precuneus superior frontal gyrus Uncinate fasciculus and frontal lobe white matter left middle frontal gyrus precentral gyrus Graphs of MD in significant clusters are presented in Figures 4C D HBOT induced a considerable improvement in the global cognitive score with a mean change of 8 1 1 5 and a relative change of 9 6 1 9 p 0 0001 Memory executive functions and information processing speed showed the most striking improvements 15 relative change with mean changes of 10 5 2 4 p 0 001 11 3 2 7 p 0 0001 and 13 1 2 7 p 0 0001 respectively Attention increased by 16 1 6 3 post HBOT but did not reach statistical significance p 0 06 There were no differences in neurocognitive scores mean and relative changes of patients taking SSRI Opiates Benzodiazpeines drugs compared to patients without them p 0 2 The effect of HBOT on the patients cognitive functions is summarized in Figure 1 and Table 2 White Matter Tracts Integrity Fiber tracking analysis revealed a statistically significant increase in number of fibers in the left cingulum p 0 03 Figure 5 and in the right ILF following HBOT p 0 029 and in the right Uncinate fasciculus p 0 04 Figure 5 Increased Brain Perfusion Voxel based DSC analysis was compared before and after HBOT using paired t test Average CBV and CBF and delta whole brain maps are depicted in Figure 5 and show the increase in both CBF and CBV post HBOT Brain Microstructure Integrity Changes Voxel based DTI analysis was compared before and after HBOT using paired t test FA and MD whole brain maps are depicted in Figures 2 3 and show the statistically significant increase in FA yellow in Figure 2 and decrease in MD blue in Figure 3 average values TABLE 2 Cognitive indices at baseline and after Hyperbaric Oxygen Therapy HBOT Baseline Regional Changes in Brain Microstructure Integrity Statistically significant increase in FA was found in regions related to motor function internal capsule midbrain association fiber tracts inferior fronto occipial fasciculus IFOF inferior longitudinal fasciculus ILF superior longitudinal fasciculus SLF Cingulum and in the genu of the Corpus Callosum Decrease in FA was found in areas related to the visual system superior colliculi calcarine sulcus and other cognitive areas thalamus and posterior cingulate gyrus Graphs of FA in significant clusters are presented in Figures 4A B Post HBOT Mean change Sig Sig with time as covariate 0 0004 Global 88 2 2 5 96 4 2 5 8 2 1 5 0 0001 Memory 82 2 5 3 92 7 4 7 10 5 2 4 0 001 0 008 Executive Functions 83 9 3 8 95 2 3 4 11 3 2 7 0 001 0 002 Attention 88 1 3 5 96 3 2 9 IPS 84 3 3 3 97 4 3 8 13 1 2 7 VSP 96 6 4 0 105 3 3 1 8 7 3 0 Motor skills 92 3 4 1 98 2 3 8 5 8 2 0 0 0009 W 8 2 4 0 0 062 0 105 0 0001 0 001 0 01 0 04 Data are expressed as means standard errors IPS Information processing speed VSP Visual spatial processing W Wilcoxon signed rank test Bold values indicated statistically significant p 0 05 FIGURE 1 Cognitive indices relative changes post HBOT Relative change in the corresponding cognitive indices after HBOT Relative change was calculated by post HBOT pre HBOT Pre HBOT IPS Information processing speed p 0 05 Frontiers in Human Neuroscience www frontiersin org 4 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI FIGURE 2 Average DTI normalized delta change in FA maps Yellow and red areas show a statistically significant increase in FA p 0 05 Regional Changes in Brain Perfusion DISCUSSION Statically significant increases in CBF involved frontal white matter including corpus callosum association fibers SLF IFOF motor function related structures corona radiata midbrain and cerebellum and structures related to memory function temporal GM and fornix Statistically significant increase in CBV was found in frontal white matter including Uncinate fasiculus and Corpus Callosum frontal gray matter anterior cingulate regions related to sensory motor function and executive functions including the thalamus and midbrain association fiber tracts SLF ILF and cingulum and regions related to memory function hippocampus and fornix Figures 6 7 Most of the anatomic structures that presented a significant increase in CBF also exhibited an increase in CBV Figure 6 The current study shows for the first time in humans that HBOT can induce brain microstructure recovery in TBI patients Brain recovery encompassed gray and white matter areas white matter tracts and angiogenesis Post HBOT FA increased and MD decreased in the DTI sequence CBV and CBF increased in the DSC perfusion sequence along with improved cognitive functions Recovery was induced in the late chronic stage of TBI 6 7 2 1 years post injury Previous studies using DTI have reported that patients suffering from TBI may still have microstructural damage months to years after the initial injury Kraus et al 2007 Yuan et al 2007 Lipton et al 2008 Sugiyama et al 2009 Hartikainen et al 2010 Niogi and Mukherjee 2010 Murugavel et al 2014 Perez et al 2014 Li et al 2016 DTI characterizes the diffusion of water in the tissues thus it indicates microstructural density Frontiers in Human Neuroscience www frontiersin org 5 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI FIGURE 3 Average DTI normalized delta change in MD maps Blue areas mark statistically significant decrease in MD p 0 05 values may reflect the barriers to axoplasmic transport the local accumulation of apoptosis in organelles and secondary Wallerian degeneration in the white matter while the increased MD values may be the result of vasogenic cerebral edema Significant injury foci were reported in dedicated pathways involved in the transmission of efferent and afferent information such as the corpus callosum internal capsule SLF ILF SFO superior frontal gyrus insula and fornix Yuan et al 2007 Caeyenberghs et al 2010 Importantly the microstructure injuries depicted by the DTI imaging markers FA and MD correlated with objective measures of general and cognitive functioning Benson et al 2007 Assaf and Pasternak 2008 Sugiyama et al 2009 Caeyenberghs et al 2010 Hartikainen et al 2010 Alexander et al 2011 Sagi et al 2012 Wada et al 2012 Arenth et al 2014 Haberg et al 2015 Sepehrband et al 2015 Li et al 2016 Disorders in reaction time executive functions information processing speed attention and memory were correlated with axonal lesions in different areas Moreover in two recent longitudinal studies FA values increased in patients with favorable outcome within 6 12 months while no DTI spacing and orientational organization of cell membranes including myelin Assaf and Pasternak 2008 Alexander et al 2011 Animal studies of brain plasticity revealed that decrease in MD and increase in FA correlates with synaptophysin a marker of synaptic vesicles glial fibrillary acidic protein GFAP a marker of astrocyte activation and brain derived neurotrophic factor BDNF a marker of neuronal growth that facilitates learning Sagi et al 2012 With regards to white matter it was found that myelin density estimated by DTI can accurately predict the actual myelin density seen measured by electron microscopy Sepehrband et al 2015 The injury can be demonstrated by increased water diffusion as measured by MD and reduced directionality of diffusion as measured by FA suggesting that either axonal injury or disruption of myelination could have altered brain connectivity Kraus et al 2007 Yuan et al 2007 Lipton et al 2008 Sugiyama et al 2009 Hartikainen et al 2010 Niogi and Mukherjee 2010 Murugavel et al 2014 Perez et al 2014 Li et al 2016 Moreover FA changes appear to correlate with the severity of the clinical presentation Benson et al 2007 Yuan et al 2007 The observed decrease in FA Frontiers in Human Neuroscience www frontiersin org 6 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI FIGURE 4 Graphs of FA and MD averages and standard error in statistically significant clusters A Averages of FA before and after HBOT B Normalized delta of FA maps C Averages of MD before and after HBOT D Normalized delta of MD maps FIGURE 5 White matter tractography change in a single patient A Fibers number increase in the right ILF tract B Fibers number increase in the left IFOF tract C Fibers increase in the right Uncinate tract increase in FA and decrease in MD post HBOT together with cognitive function improvement of patients in the late chronic stage of TBI suggest that brain microstructure recovery can be induced by HBOT changes registered in patients with unfavorable outcome Sidaros et al 2008 Hartikainen et al 2010 In the current study for the first time in humans DTI changes of chronic TBI were evaluated before and after HBOT The Frontiers in Human Neuroscience www frontiersin org 7 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI FIGURE 6 Graphs of CBF and CBV averages and standard error in statistically significant clusters A Averages of CBF before and after HBOT B Averages of CBV before and after HBOT DTI values FA and MD were found in our study to correlate with the improvements in cognitive functions in concordance with previous studies Sugiyama et al 2009 Wada et al 2012 Arenth et al 2014 Haberg et al 2015 Memory executive function and information processing speed were all significantly improved In correlation with these cognitive improvements MD decreased in most of the frontal lobe white matter such as the prefrontal cortex that enables executive control Miller and Cohen 2001 and the anterior cingulate gyrus involved in error detection especially in a Stroop task Bush et al 2000 Also FA increased in most of the long association fibers critical for proper cognitive function role in visual memory Bauer and Trobe 1984 Shinoura et al 2007 In correlation with those changes there was a significant improvement in the memory index which includes a visual memory task i e Memory 10 5 2 4 p 0 001 Cingulum A cluster of white matter fibers projecting from the cingulate gyrus in the frontal lobe to the entorhinal cortex in the temporal lobe The cingulum has been tightly associated with memory disorders Charlton et al 2006 Sepulcre et al 2009 The memory correlates also with the changes in the cingulum Genu of the Corpus Callosum The largest white matter structure in the brain It connects the left and right cerebral hemispheres and facilitates interhemispheric communication Integrity of the corpus callosum is linked to information processing speed and episodic memory Bucur et al 2008 Lockhart and DeCarli 2014 The improvement in information processing speed and memory indices may also correlate with the improvement in the genu of the corpus callosum SLF Bi directional connection of the hemispheric frontal parietal temporal and occipital lobes The SLF plays an important role in high brain functions particularly language reflected in information processing speed and executive function tasks Heilman et al 1970 Rocha et al 2005 Sasson et al 2013 In correlation with those changes there was a significant improvement in neurocognitive test results in both information processing speed IPS and executive functions EF i e IPS 13 1 2 7 p 0 0001 EF 11 3 2 7 p 0 001 ILF Connection between the temporal and occipital lobes on the same hemisphere The ILF is known to play an important Frontiers in Human Neuroscience www frontiersin org Mechanisms of neuroplasticity and cellular repair by HBOT have been suggested in many animal studies Hadanny and Efrati 2016 These include enhanced mitochondrial function and cellular metabolism improved blood brain barrier and inflammatory reactions reduced apoptosis alleviation of 8 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI FIGURE 7 Changes in brain perfusion CBF and CBV post HBOT A Average DSC maps pre and post HBOT and DSC normalized delta maps Top row CBF and CBV pre HBOT Middle row CBF and CBV maps post HBOT Bottom row normalized delta maps showing diffuse increases in CBF and CBV post HBOT B Significant CBF and CBV normalized delta changes post HBOT Areas of maximal statistically significant increase in perfusion Frontiers in Human Neuroscience www frontiersin org 9 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI oxidative stress increased levels of neurotrophins and nitric oxide and up regulation of axonal guidance agents Efrati et al 2013 Efrati and Ben Jacob 2014 Moreover the effects of HBOT on neurons may be mediated indirectly by glial cells HBOT may also promote neurogenesis of endogenous neural stem cells Efrati et al 2013 Efrati and Ben Jacob 2014 HBOT may enable the metabolic change simply by supplying the missing oxygen energy needed for these regeneration processes Efrati et al 2013 Efrati and Ben Jacob 2014 The ability of HBOT to induce angiogenesis was demonstrated in several different preclinical studies Mu et al 2011 Lin et al 2012 Lee et al 2013 Hu et al 2014 Hu et al have demonstrated that HBOT induced neurogenesis is mediated by ROS HIF 1 catenin pathway Hu et al 2014 In the current study it is demonstrated that HBOT can induce neuroplasticity in humans even years after the acute insult Along with the structural changes HBOT induces angiogenesis as shown by the increase of CBF and CBV in this study as well as in our previous study Tal et al 2015 The injured areas in the brains post TBI experience hypoxia and hypoperfusion which serve as a rate limiting factor for any regenerative process Graham and Adams 1971 Graham et al 1978 Stein et al 2004 Kim et al 2010 Ostergaard et al 2014 HBOT induced angiogenesis has been amply confirmed in pre clinical models and can be deduced from brain SPECTs of patients post stroke and post TBI even years after the acute insult Lin et al 2012 Boussi Gross et al 2013 Efrati et al 2013 Peng et al 2014 Duan et al 2015 The generation of new microvessels renders the local environment non hypoxic thus able to induce brain plasticity enhance neurogenesis and synaptogenesis and foster functional recovery Chen et al 2003 Jiang et al 2005 Unsurprisingly CBV and CBF increased in the long association fiber tracts discussed above including corpus callosum association fibers SLF IFOF and cingulum Angiogenesis and increased perfusion to the malfunctioning tissue seen in DSC serve as infrastructure for the regenerative process and the preservation of newly generated metabolic functioning of the axonal microstructure seen in DTI Our study has several limitations The major one is related to lack of control group However one can hardly expect any significant changes in DSC and DTI values or neurocognitive improvement to occur spontaneously years after the acute insult The cognitive improvement seen here is in line with our earlier randomized controlled trial on patients suffering from mild TBI In our previous randomized control study it was clearly demonstrated that the control group had no neurocognitive improvement same cognitive tests used in the current study or significant change of in brain perfusion measured by SPECT 1 5 years after the acute insult Boussi Gross et al 2013 Nevertheless one can hardly expect any significant changes in DSC and DTI values or neurocognitive improvement occurring spontaneously years after the acute insult In addition a previous randomized controlled trial with a control group showed neurocognitive effects and brain perfusion improvement using SPECT Boussi Gross et al 2013 CONCLUSION HBOT can induce cerebral angiogenesis and recovery of brain microstructure in patients with chronic cognitive impairments due to TBI months to years after the acute injury The increased integrity of brain fibers correlates with the functional cognitive improvement The mechanism by which HBOT can induce brain neuroplasticity can be demonstrated by highly sensitive perfusion MRI and DTI Further studies using DTI MRI are needed in order to gain better understanding of the neuroplasticity effect of HBOT in a larger cohort of patients with different types of brain injuries ETHICS STATEMENT This study was carried out in accordance with the recommendations of Assaf Harfoeh Medical Center Institutional Review Board 0030 15 ASF with written informed consent from all subjects All subjects gave written informed consent in accordance with the Declaration of Helsinki The protocol was approved by the Assaf Harfoeh Medical Center Institutional Review Board 0030 15 ASF AUTHOR CONTRIBUTIONS Conceived and designed the experiments AH ST and SE Performed the experiments AH ST GS and SE Analyzed the data AH ES and SE Contributed analysis tools AH ST ES and SE Wrote the paper AH ST GS ES and SE ACKNOWLEDGMENTS Special thanks to Ms Michal Ben Jacob and Mr Raz Tuval for reviewing and proofing the manuscript SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at https www frontiersin org articles 10 3389 fnhum 2017 00508 full supplementary material REFERENCES imaging stains Brain Connect 1 423 446 doi 10 1089 brain 2011 0071 Arenth P M Russell K C Scanlon J M Kessler L J and Ricker J H 2014 Corpus callosum integrity and neuropsychological performance after traumatic brain injury a diffusion tensor imaging study J Head Trauma Rehabil 29 E1 E10 doi 10 1097 HTR 0b013e318289ede5 Assaf Y and Pasternak O 2008 Diffusion tensor imaging DTI based white matter mapping in brain research a review J Mol Neurosci 34 51 61 doi 10 1007 s12031 007 0029 0 Achiron A Chapman J Magalashvili D Dolev M Lavie M Bercovich E et al 2013 Modeling of cognitive impairment by disease duration in multiple sclerosis a cross sectional study PLoS ONE 8 e71058 doi 10 1371 journal pone 0071058 Alexander A L Hurley S A Samsonov A A Adluru N Hosseinbor A P Mossahebi P et al 2011 Characterization of cerebral white matter properties using quantitative magnetic resonance Frontiers in Human Neuroscience www frontiersin org 10 October 2017 Volume 11 Article 508
Tal et al HBOT Induces Regeneration in mTBI and associations with outcome measures J Neurosci Res 93 1109 1126 doi 10 1002 jnr 23534 Hadanny A and Efrati S 2016 Treatment of persistent postconcussion syndrome due to mild traumatic brain injury current status and future directions Expert Rev Neurother 16 875 887 doi 10 1080 14737175 2016 1205487 Harch P G Andrews S R Fogarty E F Amen D Pezzullo J C Lucarini J et al 2012 A phase I study of low pressure hyperbaric oxygen therapy for blast induced post concussion syndrome and post traumatic stress disorder J Neurotrauma 29 168 185 doi 10 1089 neu 2011 1895 Hartikainen K M Waljas M Isoviita T Dastidar P Liimatainen S Solbakk A K et al 2010 Persistent symptoms in mild to moderate traumatic brain injury associated with executive dysfunction J Clin Exp Neuropsychol 32 767 774 doi 10 1080 13803390903521000 Heilman K M Pandya D N and Geschwind N 1970 Trimodal inattention following parietal lobe ablations Trans Am Neurol Assoc 95 259 261 Hu Q Liang X Chen D Chen Y Doycheva D Tang J et al 2014 Delayed hyperbaric oxygen therapy promotes neurogenesis through reactive oxygen species hypoxia inducible factor 1alpha beta catenin pathway in middle cerebral artery occlusion rats Stroke 45 1807 1814 doi 10 1161 STROKEAHA 114 005116 Huang L and Obenaus A 2011 Hyperbaric oxygen therapy for traumatic brain injury Med Gas Res 1 21 doi 10 1186 2045 9912 1 21 Iverson G L 2005 Outcome from mild traumatic brain injury Curr Opin Psychiatry 18 301 317 doi 10 1097 01 yco 0000165601 29047 ae Jiang Q Zhang Z G Ding G L Zhang L Ewing J R Wang L et al 2005 Investigation of neural progenitor cell induced angiogenesis after embolic stroke in rat using MRI Neuroimage 28 698 707 doi 10 1016 j neuroimage 2005 06 063 Kashluba S Paniak C Blake T Reynolds S Toller Lobe G and Nagy J 2004 A longitudinal controlled study of patient complaints following treated mild traumatic brain injury Arch Clin Neuropsychol 19 805 816 doi 10 1016 j acn 2003 09 005 Kim J Whyte J Patel S Avants B Europa E Wang J et al 2010 Resting cerebral blood flow alterations in chronic traumatic brain injury an arterial spin labeling perfusion FMRI study J Neurotrauma 27 1399 1411 doi 10 1089 neu 2009 1215 King N S and Kirwilliam S 2011 Permanent post concussion symptoms after mild head injury Brain Inj 25 462 470 doi 10 3109 02699052 2011 558042 Kraus M F Susmaras T Caughlin B P Walker C J Sweeney J A and Little D M 2007 White matter integrity and cognition in chronic traumatic brain injury a diffusion tensor imaging study Brain 130 2508 2519 doi 10 1093 brain awm216 Lee Y S Chio C C Chang C P Wang L C Chiang P M Niu K C et al 2013 Long course hyperbaric oxygen stimulates neurogenesis and attenuates inflammation after ischemic stroke Mediators Inflamm 2013 512978 doi 10 1155 2013 512978 Leemans A Jeurissen B Sijbers J and Jones D K 2009 ExploreDTI a graphical toolbox for processing analyzing and visualizing diffusion MR data in Proceedings of the 17th Annual Meeting of the International Society for Magnetic Resonance in Medicine Hawaii 3537 Available online at http www exploredti com ref ExploreDTI_ISMRM_2009 pdf Li L Sun G Liu K Li M Li B Qian S W et al 2016 White matter changes in posttraumatic stress disorder following mild traumatic brain injury a prospective longitudinal diffusion tensor imaging study Chin Med J 129 1091 1099 doi 10 4103 0366 6999 180518 Lin K C Niu K C Tsai K J Kuo J R Wang L C Chio C C et al 2012 Attenuating inflammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury J Trauma Acute Care Surg 72 650 659 doi 10 1097 TA 0b013e31823c575f Lipton M L Gellella E Lo C Gold T Ardekani B A Shifteh K et al 2008 Multifocal white matter ultrastructural abnormalities in mild traumatic brain injury with cognitive disability a voxel wise analysis of diffusion tensor imaging J Neurotrauma 25 1335 1342 doi 10 1089 neu 2008 0547 Lockhart S N and DeCarli C 2014 Structural imaging measures of brain aging Neuropsychol Rev 24 271 289 doi 10 1007 s11065 014 9268 3 Malec J F Brown A W Leibson C L Flaada J T Mandrekar J N Diehl N N et al 2007 The mayo classification system for traumatic brain injury severity J Neurotrauma 24 1417 1424 doi 10 1089 neu 2006 0245 Barrett K F Masel B Patterson J Scheibel R S Corson K P and Mader J T 2004 Regional CBF in chronic stable TBI treated with hyperbaric oxygen Undersea Hyperb Med 31 395 406 Bauer R M and Trobe J D 1984 Visual memory and perceptual impairments in prosopagnosia J Clin Neuroophthalmol 4 39 46 Bazarian J J McClung J Shah M N Cheng Y T Flesher W and Kraus J 2005 Mild traumatic brain injury in the United States 1998 2000 Brain Inj 19 85 91 Benson R R Meda S A Vasudevan S Kou Z Govindarajan K A Hanks R A et al 2007 Global white matter analysis of diffusion tensor images is predictive of injury severity in traumatic brain injury J Neurotrauma 24 446 459 doi 10 1089 neu 2006 0153 Boussi Gross R Golan H Fishlev G Bechor Y Volkov O Bergan J et al 2013 Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS ONE 8 e79995 doi 10 1371 journal pone 0079995 Bucur B Madden D J Spaniol J Provenzale J M Cabeza R White L E et al 2008 Age related slowing of memory retrieval contributions of perceptual speed and cerebral white matter integrity Neurobiol Aging 29 1070 1079 doi 10 1016 j neurobiolaging 2007 02 008 Bush G Luu P and Posner M I 2000 Cognitive and emotional influences in anterior cingulate cortex Trends Cogn Sci 4 215 222 doi 10 1016 S1364 6613 00 01483 2 Caeyenberghs K Leemans A Geurts M Taymans T Vander Linden C SmitsEngelsman B C et al 2010 Brain behavior relationships in young traumatic brain injury patients fractional anisotropy measures are highly correlated with dynamic visuomotor tracking performance Neuropsychologia 48 1472 1482 doi 10 1016 j neuropsychologia 2010 01 017 Charlton R A Barrick T R McIntyre D J Shen Y O Sullivan M Howe F A et al 2006 White matter damage on diffusion tensor imaging correlates with age related cognitive decline Neurology 66 217 222 doi 10 1212 01 wnl 0000194256 15247 83 Chen J Zhang Z G Li Y Wang L Xu Y X Gautam S C et al 2003 Intravenous administration of human bone marrow stromal cells induces angiogenesis in the ischemic boundary zone after stroke in rats Circ Res 92 692 699 doi 10 1161 01 RES 0000063425 51108 8D Chen Z Ni P Lin Y Xiao H Chen J Qian G et al 2010 Visual pathway lesion and its development during hyperbaric oxygen treatment a bold fMRI and DTI study J Magn Reson Imaging 31 1054 1060 doi 10 1002 jmri 22142 Chiu W T and LaPorte R E 1993 Global spine and head injury prevention SHIP project J Trauma 35 969 970 doi 10 1097 00005373 199312000 00034 Doniger G M 2014 Guide to Normative Data NeuroTrax Corporation Duan S Shao G Yu L and Ren C 2015 Angiogenesis contributes to the neuroprotection induced by hyperbaric oxygen preconditioning against focal cerebral ischemia in rats Int J Neurosci 125 625 634 doi 10 3109 00207454 2014 956101 Dwolatzky T Whitehead V Doniger G M Simon E S Schweiger A Jaffe D et al 2003 Validity of a novel computerized cognitive battery for mild cognitive impairment BMC Geriatr 3 4 doi 10 1186 1471 2318 3 4 Efrati S and Ben Jacob E 2014 Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Rev Neurother 14 233 236 doi 10 1586 14737175 2014 884928 Efrati S Fishlev G Bechor Y Volkov O Bergan J Kliakhandler K et al 2013 Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS ONE 8 e53716 doi 10 1371 journal pone 0053716 Golden Z Golden C J and Neubauer R A 2006 Improving neuropsychological function after chronic brain injury with hyperbaric oxygen Disabil Rehabil 28 1379 1386 doi 10 1080 09638280600638364 Graham D I Adams J H and Doyle D 1978 Ischaemic brain damage in fatal non missile head injuries J Neurol Sci 39 213 234 doi 10 1016 0022 510X 78 90124 7 Graham D I and Adams J H 1971 Ischaemic brain damage in fatal head injuries Lancet 1 265 266 doi 10 1016 S0140 6736 71 91003 8 Haberg A K Olsen A Moen K G Schirmer Mikalsen K Visser E Finnanger T G et al 2015 White matter microstructure in chronic moderate tosevere traumatic brain injury impact of acute phase injury related variables Frontiers in Human Neuroscience www frontiersin org 11 October 2017 Volume 11 Article 508
RESEARCH ARTICLE The National Brain Injury Rescue and Rehabilitation Study a multicenter observational study of hyperbaric oxygen for mild traumatic brain injury with post concussive symptoms B Robert Mozayeni1 William Duncan2 Eddie Zant3 Tommy L Love4 Robert L Beckman1 Kenneth P Stoller5 1 Foundation for the Study of Inflammatory Disease Bethesda MD USA 2 Patriot Clinics Oklahoma City OK USA 3 Hyperbaric Medicine Inc of Florida Destin FL USA 4 Concentra Medical Center Salt Lake City UT USA 5 Hyperbaric Oxygen Therapy San Francisco American College of Hyperbaric Medicine San Francisco CA USA Correspondence to B Robert Mozayeni MD nbirr01 nbirr org Abstract The National Brain Injury Rescue and Rehabilitation Project was established as a preliminary study to test the safety and practicality of multi center hyperbaric oxygen administration for the post concussive symptoms of chronic mild traumatic brain injury as a precursor to a pivotal independent multi center controlled clinical trial This report presents the results for 32 subjects who completed a preliminary trial of hyperbaric oxygen several years before the passage of the 21st Century Cures Act This study anticipated the Act and its reassessment of clinical research Subjects received 40 82 one hour treatments at 1 5 atmospheres absolute 100 oxygen Outcome measures included repeated self assessment measures and automated neurocognitive tests The subjects demonstrated improvement in 21 of 25 neurocognitive test measures observed The objective neurocognitive test components showed improvement in 13 of 17 measures Earlier administration of hyperbaric oxygen post injury younger age at the time of injury and hyperbaric oxygen administration military status and increased number of hyperbaric oxygen administrations were characteristics associated with improved outcomes There were no adverse events Hyperbaric oxygen was found to be safe inexpensive and worthy of clinical application in the 21st Century model of facile data collection provided by recent research regulatory shifts in medicine The study was approved by the ethics review committee of the Western Institutional Review Board WIRB Protocol 20090761 Key words hyperbaric oxygen traumatic brain injury post concussion syndrome post traumatic stress disorder 21st Century Cures Act HBOT mTBI PTSD concussion doi 10 4103 2045 9912 254636 How to cite this article Mozayeni BR Duncan W Zant E Love TL Beckman RL Stoller KP The National Brain Injury Rescue and Rehabilitation Study a multicenter observational study of hyperbaric oxygen for mild traumatic brain injury with post concussive symptoms Med Gas Res 2019 9 1 1 12 Funding The study was funded through pro bono clinical care provided by the investigators and involved clinics augmented by philanthropic resources of the International Hyperbaric Medical Foundation and multiple community hyperbaric clinics INTRODUCTION Untreated brain insult is among the most expensive public health problems in the world An argument can be made that untreated brain insults are the most expensive public health problem in the world when you take into account brain injuries from war falls strokes accidents violence blasts sports injuries near drownings and a myriad of other wounds to the brain brought on by substance abuse etc The systematic use of hyperbaric oxygen therapy HBOT for brain injury predates World War II 1 Neurological injury is the first indication ever approved for HBOT and today the approved indications include repair of five acute chronic neurological injuries and three chronic non healing wounds 2 Non healing wounds in the brain are a logical progression as demonstrated by research conducted since 1976 1 Thousands of patients in hundreds of locations have been successfully treated since that date An estimated 2000 HBOT treatments for these neurological conditions occur on any one day across the United States 3 The difficulty has been that while significant off label treatment happens across all medical disciplines there has been no sys tematic way to gather and collate those data to scientifically present the findings to effect third party reimbursement A collaboration between William Duncan and John Eisenberg founder and first Director of the Agency for Healthcare Research and Quality AHRQ initiated a track that led to the National Brian Injury Rescue Rehabilitation NBIRR 01 observational study methodology to validate orphaned therapies Though HBOT is far less expensive to society than the cost of living with the human tragedy of untreated brain insults there has been no commercial pathway to development and thus there was no corporate sponsor because the treatment cannot be protected by patents A few peer reviewed scientific articles have reported on studies that document beneficial effects from hyperbaric oxygen HBO2 in subjects with chronic residual effects of moderate to severe traumatic brain injury TBI 4 7 And within the last half decade a sizeable literature has developed that explores the safety and effectiveness of HBO2 with subjects diagnosed with TBI post traumatic stress disorder PTSD post concussion syndrome PCS and and or persistent post concussion syndrome PPCS 8 Based on 2019 Medical Gas Research Published by Wolters Kluwer Medknow 1
Mozayeni et al Med Gas Res the mounting evidence that service member suicides were increasing along with the toll extracted on service members by improvised explosive devices and blast injuries the NBIRR was started to study the safety and practicality of a multicenter study of HBO2 administration at 1 5 atmospheres absolute ATA 1 atm 1 105 Pa for post concussive symptoms from mild TBI mTBI with or without co existing PTSD and PTSD without TBI Study sites were the Oklahoma State University Center for Aerospace Hyperbaric Medicine Tulsa OK USA San Francisco Institute for Hyperbaric Medicine San Francisco CA USA Hyperbaric Medicine Inc Fort Walton Beach FL USA Restorix Health Issaquah WA USA and Life Force Therapies Minneapolis MN USA The study was designed to enroll 1000 subjects over a multi year period in the expectation that improvement of symptoms could be offered to a large number of subjects many of whom may have been injured in the Global War on Terror The non DoD VA medical community particularly National Institutes of Health NIH and the Food and Drug Administration FDA have not been immune to the need for faster responses to life threatening emergencies that have become epidemics In December 2016 the 21st Century Cures Act the Act was signed 9 A major component of the law is an effort to expedite approval of breakthrough medical technologies for patients with life threatening illnesses and limited treatment options Without specifically focusing on brain injuries the Act called out several requirements that were already enabled in NBIRR namely 1 recording the effect of a current therapeutic option on brain injury 2 capturing and assessing patient reported outcomes i e a measurement based on a report from a patient regarding the status of the patient s health condition without amendment or interpretation of the patient s report by a clinician or any other person 3 accumulating data regarding the usage or the potential benefits or risks of a drug derived from an observational study 4 capturing data in a repository and making it freely available to participants via the Cloud 5 subjecting clinical experience data collected nationwide to Bayesian analysis anticipating adaptive trial designs in follow on studies using other alternative therapies 6 tying results data to economic consequences based on the separate or aggregated clinical consequences of the represented health outcomes 7 developing reporting and making available for future use the patient experience data necessary for enhanced structured risk benefit assessment One of the purposes of NBIRR was to evaluate the safety of the HBO2 1 5 ATA protocol for mTBI post concussive symptoms and PTSD While HBO2 is generally accepted as safe potential adverse effects resulting from HBO2 administration in brain injured patients include seizures and worsening of psychiatric conditions The decades long use of HBO2 1 5 ATA in hundreds of patients with multiple sclerosis in millions of sessions in the United Kingdom has established fully the safety of HBO2 1 5 ATA for neurologic conditions yet at the time this study was designed the safety of HBO2 in mTBI 2 www medgasres com subjects was being actively questioned 10 11 Further in August 2013 the FDA issued a Consumer Update12 that was widely interpreted by some wrongly as a warning about the safety of HBO2 The Update was an FDA advisory to consumers not to believe excessive marketing material on the Web about the use of HBO2 for such things as Autism Cancer and several other diseases Our research into the use of HBO2 in treating TBI was never in question The Study Director took the opportunity to terminate this pro bono study due to lack of funding The study had met its primary objectives to ascertain in a large multicenter cohort if there was a long term benefit for a new use of a known safe treatment to provide nationwide access to a safe treatment for a new indication of an FDA cleared Medical device for mild moderate chronic TBI and or PTSD while ascertaining broader efficacy under controlled conditions and to ascertain the optimal number of treatments in the range from 40 80 HBOT sessions HBO2 has been used to treat a variety of brain injuries for decades It was described as a treatment for carbon monoxide poisoning in 1960 13 and it was soon recognized that hyperbaric oxygen had effects impacting brain healing separate from the action to remove carbon monoxide from hemoglobin molecules 14 Since the adoption of oxygen treatment tables in 1967 the brain injuries of decompression sickness and arterial gas embolism have been effectively treated by HBO2 15 In 1969 clinical improvement from stroke was demonstrated with HBO2 administered three months after the stroke 16 Late hypoxic injury to the brain had also been treated successfully with HBO2 17 Significant changes in cerebral blood flow with simultaneous symptomatic physical quality of life and cognitive improvements have recently been demonstrated after HBO2 in a population of blast induced mild moderate TBI military veterans with PCS and PTSD That experience replicated the findings in a controlled animal model of chronic traumatic brain injury incorporating an earlier version of the 1 5 ATA protocol where persistent changes in brain vasculature as well as spatial learning and memory were observed 18 The lack of high quality controlled clinical trials demonstrating the efficacy of HBO2 in brain injury had been a valid criticism for a decade 19 At the end of 2008 that began to change after a DoD sponsored Consensus Conference on the use of HBO2 for brain injury Over a dozen studies and analyses have been conducted since then The data and worldwide analyses point to the safety and efficacy of HBOT when used to help treat brain injury 7 NBIRR IN CONTEXT CONFRONTING THE ALLEGED BIAS IN STUDIES USING AN HBO2 SHAM NBIRR was designed and carried out as an observational study Throughout the research other more extensive and expensive studies were conducted As with all science disagreements occurred about outcomes and interpretations of data Where there was little disagreement however was the dire need to do a better job of making treatments available that actually did something to relieve the suffering of those with brain injuries Beginning in 2008 suspicions arose about the futility of much of the research into treatments for what was then thought of as PTSD Congressional doubts led to an Institute of Medicine review that found the expenditure Medical Gas Research March Volume 9 Issue 1
Mozayeni et al Med Gas Res of 9 3 billion to treat PTSD from 2010 through 2012 could not tell whether this staggering sum resulted in effective or adequate care 20 Despite those findings research continued into a multitude of potential interventions Despite the efforts and the large sums of dollars expended senior analysts could say years later that no new treatments for persistent blast or impact related post concussion symptoms have been identified despite the extensive investment to date The evidence remains weak and inconsistent for both pharmacological and nonpharmacological interventions e g cognitive psychotherapy Concerns have been raised that current screening approaches combined with a specialty driven structure of concussion care in the Veterans Health Administration VHA and DoD may inadvertently promote negative rather than positive recovery expectations 21 The NBIRR study came into being for precisely that need to help overcome the paucity of effective and safe treatments that appeared to be affecting the health safety wellbeing and even the lives of the brain injured and their families Researchers into brain injuries can certainly disagree about many aspects of science but the validity of the basic laws of physics and mathematics should not be flexible Since NBIRR was intended to inform the design of further research studies to investigate the use of HBO2 in brain injured service members and others it is important to dwell on a worldwide controversy about the validity of the findings and conclusions in the DoD VA Army research Though it did not affect the NBIRR study serious disagreements were raised very early and continue to exist about what Army studies characterize as the sham employed in their so called randomized controlled trials The first Army study was a single center double blind randomized shamcontrolled prospective trial at the US Air Force School of Aerospace Medicine where the effects of 2 4 ATA HBO2 on post concussion symptoms in 50 military service members with at least 1 combat related mild traumatic brain injury were examined Each subject received 30 sessions of either a sham compression room air at 1 3 ATA or HBO2 treatments at 2 4 ATA over an 8 week period 22 The challenges from around the world came quickly the claimed sham in this DoD VA Army study and others that followed were not without medicinal properties 30 higher pO2 than in air at sea level and therefore had to be considered a treatment and could not be considered a sham The DoD VA Army studies should accurately be characterized as dose response studies not sham controlled RCTs In a Letter to the Editor in JAMA by noted Canadian Dr Pierre Marois he explains We have much more knowledge about the physiology of hyperbaric therapy in neurological conditions ref and this should help us understand and accept the impact of small increases of pressure on brain function By definition sham is something false or empty Hyperbaric treatments at 1 2 ATA substantially increase the amount of dissolved oxygen in the blood and simultaneously induce cascades of metabolic changes and genes activation Therefore the claimed sham treatment of Miller s study and its predecessors is not close to being a placebo An increase of just 0 2 ATA is an effective treatment and is used to save lives in patients with mountain Medical Gas Research March Volume 9 Issue 1 www medgasres com sickness It has to be considered as a treatment arm Always If there were no preconceived ideas on the amount of pressure needed to induce a positive response on post concussion patients the only scientific conclusion we could draw from the significant results described in Miller s controlled study is that even at small pressures HBOT seems to be effective This could have a significant impact on the quality of life of thousands of military personnel 23 Army researchers have not sufficiently explained their reasoning and the science behind justifying a sham of air at 1 3 ATA despite it being a contradiction in terms Their lack of transparency around their sham plagues on going and proposed research A worldwide outpouring of challenges arose when the Wolf Cifu study was published Not all of the commentary saw its way into print 24 but the gist of challenges can be summarized the claimed DoD VA Army definition of sham and even hyperbaric gas are both wrong Continuing the canard that their sham is legitimate are peer reviewers who do not challenge the fallacy Extensive exposition of the laws of physics bio chemistry and physiology was delivered by Prof Philip James 25 Dr Paul Harch summarizes the science A reconsideration of the science of hyperbaric therapy reveals that the study by Wolf and colleagues is neither a sham nor placebo controlled study Rather it is a Phase II study of two composite doses of hyperbaric therapy that demonstrated significant improvements in PCS and PTSD symptoms at the 2 4 atmospheres absolute ATA pure oxygen dose as well as the low pressure 1 3 ATA air oxygen dose 26 Other significant research published during NBIRR includes findings of an army team investigating blast injury 31 Enormous resources have been expended seeing to differentiate between PTSD and TBI Extreme confusion about diagnoses have resulted due to the difficulty in understanding invisible wounds and the lack of definitive diagnostics We can say from our own experience in this study that most subjects who had been diagnosed with only PTSD upon careful historytaking could be assumed to have been subjected to blasts and probably had incurred mild to moderate TBIs From the clinical standpoint NBIRR did not differentiate between PTSD and TBI diagnoses all subjects received the same treatment under the protocol Yet the research on Blast is instructive for anyone seeking to conduct research on invisible wounds particularly using HBO2 The Perl Team from Walter Reed explains Our findings suggest for the first time that there might be a predictable pattern of physical damage to human brain after blast exposure Additionally the neuroanatomical locations of the interface astroglial scarring seen in our study support the concept that persistent symptoms of blast exposed individuals may correlate with damage to particular structures with potential interference or alteration of their functions We anticipate reconsideration about pathophysiology underlying the neuropsychiatric sequelae that follow blast exposure and also innovative approaches to diagnosis and treatment 27 These neuropsychiatric sequelae are further linked to PTSD since recent data suggest an association between combat blast TBI and PTSD 28 These findings about blast are relevant for this study and further research into TBI PTSD PCS PPCS since we are dealing with a complex of injuries and symptoms that currently do not have definitive diagnoses and markers 3
Mozayeni et al Med Gas Res Current on label and off label interventions without the use of HBO2 tend to compartmentalize each symptom and work on any number of symptoms in isolation Evidence that the VA is aiming at symptom identification and resolution on a symptom by symptom basis as opposed to wholistic integrated patient centered precision medicine can be found in the latest update to VA and DoD Clinical Practice Guideline for the Management of Concussion Mild Traumatic Brain Injury 29 Evolving treatment protocols are turning toward isolating individual symptoms and treating those symptoms of brain injury as opposed to a focus on the cause the underlying brain injury 30 SUBJECTS AND METHODS NBIRR was a multi center trial conducted under the auspices of the International Hyperbaric Medical Foundation HBO2 administration was performed on a voluntary basis by each treating center The protocol at each participating center was approved by the Western Institutional Review Board WIRB Protocol 20090761 each site had its own Principal Investigator and all subjects provided written informed consent No effort was made to exclude subjects based on the etiology of injury A control non treatment group was not included in this initial observational study however all participants in this report had mTBI with post concussive symptoms and a history of at least 3 months of clinical non improvement or deterioration at the time of enrollment Male and female subjects 18 to 65 years of age were eligible if they had a diagnosis of mTBI with post concussive symptoms and or PTSD Inclusion criteria for subjects in this report were any 18 65 year old subject with a history of mild TBI a with post concussive symptoms or PTSD b a diagnosis of mild TBI with post concussive symptoms and or PTSD made by a neurologist or neuropsychologist c negative pregnancy test in females and d current symptoms or functional impairment attributable to TBI and or PTSD Exclusion criteria were a pulmonary disease that precludes HBO2 administration b unstable medical conditions that are contraindicated in HBO2 administration c severe confinement anxiety d pregnancy d a neurological diagnoses other than TBI or PCS e participation in another experimental trial with active intervention f high probability of inability to complete the experimental protocol g insufficient mental or physical capacity to complete the required tests h pre or post TBI history of systemic illness with impact on central nervous system i pre existing mental illness and j any pre existing chronic infection not related to battlefield injuries or government service A new online data entry system CareVectorTM was created to deploy study Case Report Forms to a network of clinics participating in clinical research The CareVectorTM Platform CVPTM is the repository for all data collected on individual patients in NBIRR It compiled a web enabled electronic research record from multiple data sources available from HBO2 sessions tests laboratory tests and clinician patient interactions The platform also allowed for oversight with a built in auditor role to supports analysis and data and safety monitoring functions Security procedures are a built in aspect 4 www medgasres com of the CVP with multi role and multi site access controls To avoid any conflict or bias of analysis the CVP did not process or analyze any data All collected data were analyzed independently by the biostatistician The self assessment measures were a percent back to normal assessment the PHQ 15 Patient Health Questionnaire 15 a measure of somatic symptoms associated with mental disorders the PHQ 9 Patient Health Questionnaire 9 a measure of depression symptoms a quality of life assessment and the Rivermead Post concussion Symptoms Questionnaire 31 Subjects who met the inclusion criteria underwent a battery of pre HBO2 administration evaluations and testing including medical history neurological examination Automated Neuropsychological Assessment Metrics ANAM4TM Central Nervous System Vital Signs CNSVS and a variety of self assessment tests The neurocognitive test results form the basis of this report No imaging studies were included in this protocol A flow diagram of subject participation and inclusion in this report is shown in Figure 1 Figure 1 Flow diagram of study participants included in this report Note mTBI Mild traumatic brain injury PCS post concussion syndrome ANAM4TM is a library of more than thirty computer based test modules designed for a wide variety of clinical and research applications and is the direct outgrowth of more than twenty years of computer based test development across all service branches within the Department of Defense 32 It is a neurocognitive assessment tool that can be used to identify changes in a service member s cognitive function and mood state as a result of some debilitating event The ANAM4TM test battery used in this study has been tailored to provide an instrument that is sensitive to cognitive changes that often accompany mTBI 33 34 The ANAM4TM tests included the mood Medical Gas Research March Volume 9 Issue 1
Mozayeni et al Med Gas Res scores of sleepiness vigor restlessness depression anger happiness fatigue and anxiety The ANAM4TM neurocognitive measures were simple reaction time code substitution learning procedural reaction time mathematical processing matching to sample code substitution delayed and simple reaction time R a measure of basic neural processing speed and efficiency In order to minimize the effect of test retest improvement the ANAM4TM test system automatically detects when an individual has been previously assessed and will iterate to a new stimulus set 35 CNSVSTM is a battery that evaluates verbal and visual memory psychomotor speed complex attention reaction time and cognitive flexibility through application of the verbal and visual memory test finger tapping test symbol digit coding the Stroop test the shifting attention test and the continuous performance test 36 CNSVSTM was added as a secondary objective neuropsychological assessment tool and has been validated as a repetitive assessment measure for brain injury 37 The NBIRR study was designed at a time when ANAMTM and CNSVSTM were relatively non controversial test instruments for capturing data about symptoms and monitoring progress toward end points They had the added advantage that they could be administered via computer over the worldwide web and they were made available to the project for a reduced rate Because this study was self funded we were without funds to perform brain imaging though that would have been preferable In addition to the subjective questionnaires and the scientifically validated instruments of ANAMTM and CNSVSTM objective brain scans are becoming standard instruments in civilian research 38 It would be useful in any further research that brain scans functional MRI or Diffusion Tensor Imaging show great promise though are expensive are part of the protocol to avoid any misunderstandings about how HBO2 as the control is helping or hurting improvement in the health and well being of subjects HBO2 was delivered according to the 1 5 ATA protocol developed by Harch Gottlieb and Van Meter in the early 1990s based on the 1 5 ATA dose used by Neubauer in chronic brain injury 39 All subjects received 100 oxygen at 1 5 ATA in monoplace or multiplace chambers Monoplace chambers were Sechrist 2500 Sechrist 3200 or Perry Sigma 40 monoplace chambers and 100 oxygen was delivered in the chamber ambient environment The multiplace chamber was a 12 person Gulf Coast Hyperbarics chamber with oxygen delivered via hood or aviation non rebreather mask Pressurization time was 3 7 minutes and decompression time was 3 7 minutes The time at 1 5 ATA was 45 minutes for monoplace chambers and 50 minutes for the multiplace chamber This difference was planned in order to give some equivalence to the amount of oxygen delivered in the two types of chambers since descent and ascent were conducted with 100 oxygen in the monoplace chambers and air in the multiplace chamber After initial testing the subjects were to receive 40 HBO2 and were tested again If in the opinion of the subject and the site principal investigator maximum benefit was received evidenced by the initial improvement and then stabilization of symptoms without continued improvement HBO2 administration was stopped at 40 HBO2 sessions All subjects receiving 40 HBO2 sessions reported they had benefitted from the HBO2 administration If possible further Medical Gas Research March Volume 9 Issue 1 www medgasres com benefit was anticipated another 20 or 40 HBO2 sessions were administered and testing performed again when the HBO2 sessions were complete Statistical analysis was performed using R Version 2 15 1 http www R project org And post HBO2 administration changes in ANAM Mood Scores ANAM Cognitive Scores and CNSVSTM Cognitive Scores were compared using Paired t test or Wilcoxon signed rank test for not normally distributed scores Mean and standard deviation of the differences between the scores and its corresponding 95 confidence interval and P value were reported Differences in the neurocognitive scores between the groups were compared by independent ttest or Mann Whitney U test for not normally distributed data Average improvement in each subject s neurocognitive test scores were compared to number of HBO2 sessions received by correlation and regression analysis Slopes correlation coefficients r and r2 and P values were reported Significance level was set at 0 05 and no adjustment for multiple endpoints was applied RESULTS A total of 48 subjects with mTBI with post concussive symptoms with or without PTSD were enrolled in the NBIRR study at 5 centers 32 eventually completed the study Twenty nine subjects were males and three were females Of the 32 subjects in this report seven subjects 22 were active duty military at the time of participation 12 37 were veterans and 13 41 had no military service Fifteen 47 received their injury because of a blast and 17 53 were injured because of a blow Table 1 The delay from injury to protocol enrollment for the subject population was distributed from 0 37 to 46 years after injury Two subjects could not remember their injury well enough to establish a clear date of injury Figure 2 There were 25 potential outcome measures per subject at each time of measurement pre HBO2 and post HBO2 calculated for this report For each participant the measures were compared pre and post HBO2 administration Table 2 The results of the ANAMTM mood scores are expressed as subjective scales 0 100 and the objective neurocognitive screening measures are expressed as percentile placement compared to the peer populations Figures 3 and 4 The changes in subjects on active duty veterans or civilian status no history of military service were compared to each other as groups active duty veteran civilian In general the active duty group showed more improvement than the veteran and civilian groups and the civilian group showed the least improvement Table 3 In comparing subjects with blast injury n 15 to those receiving injury from a blow n 17 4 measures showed post HBO2 administration differences between the two groups with the individuals with blast injury demonstrating more improvement The measures showing significance were ANAM4TM Fatigue Mean 23 8 percentile change 25 1 23 8 25 1 CI confidence interval 32 9 to 14 7 P 0 034 ANAM4TM Code Substitution Learning 21 2 27 2 CI 11 2 31 2 P 0 006 ANAM4TM Procedural reaction Time 30 38 CI 16 44 P 0 001 and ANAM4TM simple reaction time R 8 36 CI 6 to 22 P 0 025 5
Mozayeni et al Med Gas Res Table 1 Study population characteristics Population characteristics Value Military status n Active duty Veteran Civilian Etiology of injury n Blast Blow Total Age at injury years Mean SD Median Range Delay from injury to HBO2 Start years Mean SD Median range Duration of HBO2 days Mean SD Median range No of HBO2 Mean SD Median range Diagnosis n mTBI only mTBI PTSD 7 22 12 37 13 41 15 47 17 53 32 100 30 5 12 0 28 5 7 60 9 5 12 7 3 99 0 36 45 6 114 63 116 26 304 55 8 18 5 41 35 82 25 78 7 22 Number of subjects Note n 32 HBO2 Hyperbaric oxygen mTBI mild traumatic brain injurt PTSD post traumatic stress disorder 0 1 37 0 2 1 3 2 3 4 4 5 10 5 0 0 0 0 Number of years from inhury to protocol enrollment r be 2 0 3 0 4 0 5 2 3 4 10 em t r n Ca em Figure 2 Distribution of subject population time from injury to protocol enrollment Table 2 Outcome measures Measure TM ANAM4 mood scores ANAM4TM neurocognitive tests CNSVS neurocognitive tests Total number of measures Number of outcomes 8 7 10 25 Note CNSVS Central Nervous System Vital Signs ANAM4TM Automated Neuropsychological Assessment Metrics 6 www medgasres com Age at the time of injury impacted improvement in CNSVSTM processing speed slope 0 642 P 0 043 r 0 445 r2 0 198 with earlier age at the time of injury resulting in greater test improvement after HBO2 administration Age at the start of HBO2 administration affected improvement in ANAM4TM code substitution learning slope 0 815 P 0 017 r 0 427 r2 0 182 and ANAM4TM procedural reaction time slope 1 567 P 0 001 r 0 584 r2 0 341 with earlier age at the start of HBO2 administration resulting in greater test improvement after HBO2 Figure 5 A delay in initiation of HBO2 from the time of injury affected four neurocognitive percentile scores ANAM4TM code substitution learning slope 0 0201 P 0 008 r 0 486 r2 0 286 ANAM4TM procedural reaction Time slope 0 02984 P 0 004 r 0 518 r2 0 269 ANAM4TM mathematical processing slope 0 01487 P 0 037 r 0 389 r2 0 152 ANAM4TM R slope 0 02398 P 0 022 r 0 455 r2 0 207 and CNSVS processing speed slope 0 01271 P 0 019 r 0 506 r2 0 256 A delay in HBO2 administration from the time of injury resulted in reduced improvement in test scores Figure 5 The trend toward improved neurocognitive test scores relative to number of HBO2 sessions received is reflected in Figure 6 The average neurocognitive scores improved approximately with each HBO2 received slope 0 554 P 0 038 r 0 368 r2 0 136 The number of HBO2 received was associated with improvement in the percentile performance scores in 4 neurocognitive measures ANAM4TM mathematical processing slope 0 782 P 0 001 r 0 562 r2 0 316 CNSVS psychomotor speed slope 0 509 P 0 044 r 0 424 r2 0 18 CNSVS reaction time slope 0 447 P 0 048 r 0 417 r2 0 174 and CNS vs Executive Function slope 0 612 P 0 03 r 0 453 r2 0 206 In each case a larger number of HBO2 received resulted in improved scores Seven subjects 22 had a diagnosis of PTSD in addition to mTBI with post concussive symptoms The subjects with a diagnosis of PTSD had more improvement in the ANAM4TM fatigue mood scale mean change 23 8 25 1 CI 32 9 to 14 7 P 0 012 and the ANAM4TM Matching to Sample neurocognitive test mean change 13 31 CI 2 25 P 0 028 A diagnosis of PTSD did not adversely affect any of the outcome measures No adverse effects or complications were reported in any of the subjects enrolled in the NBIRR study and the administration of HBO2 at 1 5 AIAin this population of brain injury subjects was safe DISCUSSION When the NBIRR observational study was initiated it was thought that it would be a means to gather evidence that could provide justification for and inform a much larger pivotal clinical trial An observational study while not the highest grade of evidence is typically the first step in understanding a treatment when it is already in use using FDA approved devices Such a study provides clinical evidence that can establish the potential for and inform the design of a deeper and more expensive scientific investigation NBIRR was begun with no outside funding Throughout the course of the study small donations and the patriotism of individual clinicians allowed the study to continue The hope was that the network of clinMedical Gas Research March Volume 9 Issue 1
Mozayeni et al Med Gas Res ANAM percentile scores P 0 001 P 0 002 P 0 001 P 0 001 P 0 031 P 0 001 P 0 001 P 0 001 P 0 001 www medgasres com P 0 001 P 0 001 P 0 003 P 0 023 P 0 282 P 0 003 Pre HBO measures Post HBO measures Figure 3 ANAM4TM Mood left Neurocognitive right Test Scores Note Average values from test subjects are displayed Prior to each ANAM4 TM assessment subjects were asked to rate eight mood areas left before undertaking a battery of neurocognitive test right nonparametric SRT Simple reaction time CS L code substitutionl e a r n i n g P RT p r o c e d u r a l reaction time MP mathematical processing MtS matching to sample CS D code substitutiondelayed SRT R simple reaction time R ANAM4TM Automated Neuropsychological Assessment Metrics Table 3 Changes in ANAM4TM test values from start to end of HBOT within each Military Status active duty veteran civilian and for all subjects combined Active duty n 7 Veteran n 12 Civilian n 13 Total n 32 P value ANOVA 1 86 1 46 P 0 040 CI 3 21 to 0 50 32 7 15 2 P 0 001 CI 18 7 to 46 7 1 18 1 25 P 0 022 CI 2 02 to 0 34 27 4 23 9 P 0 002 CI 12 2 to 42 6 1 13 1 34 P 0 001 CI 1 62 to 0 64 20 8 24 2 P 0 001 CI 12 1 to 29 5 0 156 27 0 19 4 P 0 016 CI 44 9 to 9 1 13 7 17 4 P 0 058 CI 29 8 to 2 4 25 4 21 3 P 0 058 CI 45 1 to 5 8 25 0 25 7 P 0 042 CI 1 2 to 48 8 18 3 27 0 P 0 029 CI 35 5 to 1 2 18 7 27 6 P 0 025 CI 36 2 to 1 1 9 3 27 4 P 0 398 CI 26 7 to 8 2 27 6 21 5 P 0 001 CI 13 9 to 41 3 15 2 21 9 P 0 001 CI 23 1 to 7 3 12 5 21 5 P 0 002 CI 20 2 to 4 7 9 8 21 7 P 0 031 CI 17 7 to 2 0 19 3 23 2 P 0 001 CI 10 9 to 27 6 0 066 35 9 19 1 P 0 003 CI 53 5 to 18 2 Anxiety 16 7 17 8 P 0 059 CI 33 2 to 0 2 Simple 64 30 P 0 001 reaction time CI 36 to 92 Code substitution 40 7 29 5 P 0 011 learning CI 13 4 to 68 0 Procedural 67 18 P 0 001 reaction time CI 50 to 84 Mathematical 37 3 31 8 P 0 021 processing CI 7 8 to 66 7 Matching to 33 28 P 0 021 sample CI 7 to 58 Code substitution 34 32 P 0 029 delayed CI 5 to 63 Simple 73 14 4 P 0 098 reaction time R CI 51 to 95 34 1 26 0 P 0 001 CI 50 6 to 17 5 12 6 24 6 P 0 052 CI 28 2 to 3 0 17 30 P 0 068 CI 2 to 36 16 8 27 4 P 0 057 CI 0 6 to 34 3 29 41 P 0 033 CI 3 to 55 17 4 26 0 P 0 041 CI 0 9 to 33 9 6 31 P 0 539 CI 14 to 25 17 29 P 0 069 CI 2 to 35 10 29 P 0 540 CI 29 to 10 0 69 1 25 P 0 089 CI 1 45 to 0 06 8 3 24 0 P 0 236 CI 6 2 to 22 8 6 0 14 4 P 0 182 CI 14 7 to 2 7 6 1 16 1 P 0 184 CI 15 8 to 3 7 2 0 9 6 P 0 720 CI 7 8 to 3 8 8 5 20 5 P 0 158 CI 3 8 to 20 9 7 8 19 1 P 0 164 CI 19 4 to 3 7 5 4 17 8 P 0 294 CI 16 1 to 5 4 13 19 P 0 027 CI 2 to 25 14 2 21 9 P 0 047 CI 0 2 to 28 1 10 30 P 0 267 CI 9 to 29 21 5 20 5 P 0 004 CI 8 5 to 34 5 10 31 P 0 296 CI 10 to 29 15 40 P 0 220 CI 10 to 41 3 18 P 0 755 23 8 25 1 P 0 001 CI 32 9 to 14 7 10 6 20 5 P 0 003 CI 17 9 to 3 2 26 32 P 0 001 CI 14 to 38 21 2 27 2 P 0 001 CI 11 2 to 31 2 30 38 P 0 001 CI 16 to 44 23 5 25 8 P 0 001 CI 14 0 to 33 0 13 31 P 0 023 CI 2 to 25 20 34 P 0 003 CI 8 to 33 8 36 27 P 0 282 0 008 CI 9 to 14 CI 6 to 22 Sleepiness Vigor Restlessness Depression Anger Happiness Fatigue 0 043 0 512 0 109 0 089 0 342 0 001 0 092 0 004 0 262 0 167 0 474 0 007 Note Final column indicates the significance of differences in ANAM4 changes between the three groups Values are expressed as mean change standard deviation of changes confidence interval CI indicates the 95 CI around the mean change P indicates the P value from a paired test for a significant mean withingroup change ANAM4TM Automated Neuropsychological Assessment Metrics HBOT hyperbaric oxygen therapy Medical Gas Research March Volume 9 Issue 1 7
Mozayeni et al Med Gas Res P 0 001 P 0 096 P 0 006 P 0 001 P 0 001 P 0 001 ANAM percentile scores P 0 0937 P 0 319 per HBO2 measures P 0 001 P 0 003 post HBO2 measures Average percentile improvement in neurocognitive test scores Figure 4 CNSVS Neurocognitive test scores Note Average values from test subjects are displayed above denotes nonparametric NCI Neurocognitive index CM composite memory VerbM verbal memory VisM visual memory PsySp psychomotor speed RT reaction time CxA complex attention CF cognitive flexibility PS processing speed ExFn executive functioning HBO2 hyperhabic oxygen CNSVS Central Nervous System Vital Signs ANAM Automated Neuropsychological Assessment Metrics 50 0 45 0 40 0 35 0 30 0 25 0 20 0 15 0 10 0 5 0 0 Age years Delay in HBO2 years Figure 5 Effect of younger age at time of protocol enrollment and delay in HBO2 administration from time of injury on neurocognitive test score improvement Note Neurocognitive scores are expressed as the sum of average improvement in tests administered HBO2 Hyperbaric oxygen Average percentile improvement in neurocognitive scores 100 80 60 40 20 0 20 40 Number of HBO2 received each point represents one subject Figure 6 Average improvement in each subject s neurocognitive test scores bases on number of HBO2 sessions received Note Each point in the graph represents one subject The line through the points is a best fit linear regression y 0 5539x 1 1863 of individual subjects who have undergone 35 and up to 82 hyperbaric oxygen treatments The trend line slope is 0 55 r 0 3685 P 0 038 HBO2 Hyperbaric oxygen 8 www medgasres com ics could treat some of the large number of active duty and veterans returning from war with post concussive symptoms from mTBI when funding became available The bulk of the study was done pro bono or at dramatically reduced costs by private HBO2 clinics As the study progressed funding was insufficient to continue Additionally to obtain an FDA study indication for HBO2 treatment newly regulated as a drug by the FDA for post concussive symptoms a redesigned study with appropriate controls would be required The preliminary results of the NBIRR study are potentially useful in designing an FDA sanctioned study seeking a new indication and they are presented here in an effort to speed the effort for interested researchers This summary is a report on the 32 subjects with post concussive symptoms who completed the protocol At the time of the current data analysis the long term follow up was not available and is not part of this report No adverse effects since conclusion of NBIRR have been reported This report is offered in the expectation that the information learned can be put to use in an independent well designed controlled clinical trial The DoD VA Army response to the need for effective treatments has been less than rapid After several years ramping up for a study and after expenditure of many millions of dollars without start to a study the US Government commenced their own studies Contemporaneously the sense of urgency that NBIRR participants brought to the research was grounded in the nation s awakening to what even DoD called a suicide epidemic among service members The rules for dealing with an epidemic are fairly straightforward early detection early response In just the last few years the US has confronted three potentially catastrophic epidemics meningitis Ebola and Zika Over one billion dollars was spent on research treatments and interventions that may or may not have contributed to the small number of infections and deaths Yet the suicide epidemic and hundreds of thousands of veterans and active duty suffering from brain injuries coupled with a suicide rate of 20 per day for a total estimated at over 48 000 nearly five combat divisions has caused no sense of urgency and immediate use of alternative therapies that satisfy the criteria set by Doctors Without Borders during the last Ebola epidemic scare Even if the sample size is quite small and more research and analysis is needed the enormity of the public health emergency should lead us to continue using this vaccine right now Replication of a targeted approach focusing on those most at risk of infection should therefore happen immediately and we urge governments in affected countries to start using this vaccine as soon as they can within the framework of the existing trial The NBIRR study demonstrated that a protocol of 40 80 treatments once a day 5 days per week of 1 5 ATA 60 minute HBO2 sessions treatments was safe in this cohort of subjects with mild blast and non blast TBI with post concussive symptoms with or without PTSD The lack of complications in the study is consistent with traditional applications of HBO2 40 The once a day 5 days per week schedule was well tolerated at least to 80 sessions in this study When the NBIRR study was designed the researchers postulated that mTBI with post concussive symptoms and PTSD were dynamic conditions capable of improvement years after diagnosis For this reason no upper limit on the number of Medical Gas Research March Volume 9 Issue 1
Mozayeni et al Med Gas Res years since injury was imposed on subjects The results of the study demonstrated that improvement was possible years after injury though not as great as for subjects who were treated sooner after injury The study also tested the new online data collection system and the research capabilities of a network of hyperbaric clinics The online data entry system the CareVectorTM Platform developed to support multicenter clinical observational studies was successful in capturing patient HBO2 administration computer generated tests and case report data from multiple centers Clinics and the brain injured and cognitively impaired subjects were able to successfully manage the computer based systems necessary to conduct this trial This portends well for future larger studies of this type as well as other pilot trials with different brain injured populations Even though many of the mTBI subjects had lives in disarray it was remarkable that they were able to commit such a large block of their time and resources to complete the study It is also notable that each center paid all of their own administrative costs and Institutional Review Board fees as well as generally treating the subjects pro bono demonstrating that small pilot HBO trials can be successfully conducted without outside funding The Hawthorne effect is a change in the outcome of an experiment affected through the inclusion in the experiment and thought to be influenced by the increased attention given to subjects and the knowledge among subjects that they are being studied 41 In any uncontrolled study placebo and Hawthorne effects cannot be excluded as the source of observed effects Changes in outcome might be attributed at least in part to a placebo effect The placebo effect in this type of study is a psychobiological phenomenon capable of altering the subject s brain and producing subjective improvement The increased attention and schedule of appointments for subjects have the capability of altering subject perceptions of one s self and the added structure to personal schedules and commitment to study participation can be perceived as having therapeutic value 42 Placebo effects have the capability to change the brain and in neurobiology can be considered a form of treatment in some circumstances 43 Without proper controls it is impossible to determine the cause of the improvement seen in the subjects whether it be from the Hawthorne effect placebo effect or hyperbaric oxygen or some combination of the three When TBI patients have stabilized symptoms and have shown no improvement for several months or years the likelihood of spontaneous improvement is low A recent study at the University of Oklahoma Veterans Hospital in veterans of Operation Enduring Freedom Operation Iraqi Freedom OEF OIF screening positive for chronic TBI indicated that for all of the parameters measured there was no difference in occurrence or intensity of symptoms between the subjects who were within 2 years of the TBI and those who suffered the TBI 3 8 years earlier 44 The Congressional Budget Office report on the Veterans Health Administration treatment of PTSD and TBI in recent combat veterans released in February 2012 showed that the health care costs of veterans with all types of TBI remained relatively constant and 67 of TBI patients 76 of PTSD patients and 96 of TBI PTSD patients continued to use VA health care services after four years of treatment 45 Prior to enrollment in the study the NBIRR subjects had failed Medical Gas Research March Volume 9 Issue 1 www medgasres com to improve sometimes for decades and only improved after inclusion in the protocol The Samueli Institute was hired by the Army to provide an independent objective and transparent analysis of the research conducted to date on HBO2 for TBI 46 They concluded based on the DoD VA Army research invalidated by their sham that HBOT does not work but also stated that HBOT is a healing environment They also noted in Summary Conclusions that improvements in outcomes cannot be ignored HBO may be of value and could benefit these patients moderate severe TBI as a relatively safe adjunctive therapy if feasible Army and Samueli Institute researchers noted in an invited commentary that attention had to be paid to what they termed the ritual of hyperbarics 47 They went so far as to remind readers that routine post concussion care may have negative effects that contribute to symptom persistence 48 We are aware of no other treatment demonstrating the degree of improvement for stable or deteriorating mTBI with post concussive symptoms as seen in HBO2 studies conducted independent of DoD VA Army 49 The magnitude of these effects would have to rely on well considered controls in a clinical study Future studies should be designed to separate the possible Hawthorne and placebo effects from that experienced through administration of hyperbaric oxygen One could argue that in the meantime HBO2 should be considered as the safe and effective treatment that it is and as an intervention to help overcome iatrogenic effects that contribute to symptom persistence in over 800 000 brain injured service members A diagnosis of PTSD did not appear to have a negative effect on outcomes and appeared to contribute to better cognitive improvement For simplicity it would have been useful to exclude subjects with the diagnosis of only PTSD and evaluate these subjects in a separate study Army research looking at the use of HBO2 for subjects with only PTSD is reportedly in pre publication Preliminary reporting on outcomes is that HBO2 is safe and efficacious A significant study was published in 2016 that throws a new light on the difficulty of differentiating between brain injuries caused by either PTSD or TBI 50 In what is being called a breakthrough study Dr Daniel P Perl and his team at the Uniformed Services University of the Health Sciences in Bethesda MO USA the medical school run by the Department of Defense have found evidence of tissue damage caused by blasts alone not by concussions or other injuries The New York Times calls it the medical explanation for shell shock preliminary proof of what medicine has been saying without proof for nearly 100 years blasts cause physical damage and this physical damage leads to psychological problems i e PTSD 51 The importance of this admission cannot be overstated this is a DoD discovery with documented evidence that blast injury improvised explosive devices breeching whether in training or combat enemy and or friendly fire can lead directly to physical brain damage and the accompanying effects many of which have been heretofore diagnosed as only PTSD We now know that TBI PTSD is a type of nonhealing wound And it should be noted that HBOT is already approved for all other forms of non healing wounds It is hoped that these results will prove useful in planning 9
Mozayeni et al Med Gas Res future randomized controlled studies of HBO2 for traumatic brain injury with post concussive symptoms and post traumatic stress disorder Future randomized controlled studies should include imaging objective neurocognitive tests as well as objective self assessment measures Objective measures of functionality in daily living would be useful these might include employment status earnings reports education status grade point averages changes in marital status medication records and changes as well as medical visits and hospitalization for mTBI associated conditions To allow time for subjects to demonstrate these results and to establish the durability of HBO2 associated improvement future studies should incorporate long term follow up Based on clinical observations and multi year experience a few other suggestions should be made about the protocol for any further studies 1 The study population should include only subjects who have proven neuroimaging abnormalities 2 To the extent practicable subjects should not live at or be treated at elevations that complicate analysis of the effects of HBO2 3 Service members who participate should have guarantees that their compensation will not be reduced or their service records used negatively if their medical condition is improved with the treatment Too many arguments have been raised for years about the negative inducements voiced to subjects in prior government studies 4 All drugs being ingested by subjects as well as any and all additional therapies and interventions should be carefully recorded throughout the entire study 5 Funding should be provided for expanded end points Brain perfusion MRI DTI brain SPECT and or PET CT along with agreed on computerized neuro cognitive tests 6 Additional end points should be considered cost effectiveness quality of life as reported by subjects families and care givers and documented sustainability of HBO2 treatment at six twelve and twenty four months SUMMARY The HBO2 1 5 ATA protocol for mTBI with post concussive symptoms with or without PTSD was safe and could be used in multiple centers The neurocognitive test scores for subjects improved in 21 of 25 measures Earlier HBO2 post injury younger age at time of injury and HBO2 administration and 80 rather than 40 administrations of HBO2 were associated with greater improvement in neurocognitive scores Similarly active duty or veteran military status was associated with improved outcomes Inclusion in the protocol with HBO2 administration was accompanied by reductions in symptoms and improvement in neurocognitive test scores even several years after sustaining mTBI These results are consistent with the findings in other recent much more well funded peer reviewed research which finds HBO2 both safe and effective Figueroa and Wright summarize what many others have written over the last half52 decade sufficient scientific evidence exists to approve HBOT use in mTBI and PTSD 10 www medgasres com Note on the methodology and funding for this observational study This study can be viewed as a citizen response in 2008 to the lack of urgency in DoD VA Army medical circles about treatments for the invisible wounds of war It is a tribute to the clinics and researchers and volunteers who participated in this boot strapped effort that the effort was successfully concluded with quality data and no adverse events The results add to the evidence based record speaking to the safety and efficacy of HBO2 for brain injuries The participants take some pride in the fact that research funding has materialized and that data from this and government funded studies as opposed to editorial conclusions demonstrate that all subjects receiving HBO2 improved Further research The Act explicitly calls for the use of real world evidence instead of just hard clinical trial evidence when weighing the approval of existing drugs for new uses Oxygen certainly qualifies Due to the Act for example the FDA now must consider patient experience and anecdotal data in its review process The FDA must also expand its programs for expedited approval of breakthrough medical technologies for patients with lifethreatening diseases that have limited treatment options TBI certainly qualifies Further the Act in general calls for priority review for breakthrough devices that provide for more effective treatment of life threatening or irreversibly debilitating human diseases or conditions TBI and the suicide epidemic certainly qualify for both research and expedited review of the data from a device like the combination drug device HBOT The Government is required to establish a program to provide priority review of research and data for devices that represent breakthrough technologies for which no approved alternatives exist offer significant advantages over existing approved or cleared alternatives including the potential to compared to existing approved or cleared alternatives reduce or eliminate the need for hospitalization improve patient quality of life facilitate patients ability to manage their own care or establish long term clinical efficiencies or when the availability of which is in the best interest of patients The Act requires that steps are taken to ensure that the design of clinical trials is as efficient as practicable such as through adoption of shorter or smaller clinical trials application of surrogate endpoints and use of adaptive trial designs and Bayesian statistics to the extent scientifically appropriate HBOT under NBIRR and the contemplated follow on use of alternative therapies in combination with HBOT certainly fall within the ambit of research and treatment contemplated in the Act Acknowledgements The contributions of Drs Paul Harch and James Wright MD along with Steve Reimers MS are gratefully acknowledged Karen Lawson MD ABIHM NBC HWC Paul Rock PhD DO Latisha Smith MD Julie Stapleton MD Enrico Versace MD Ladonna Lacey BS Lisa Terry MS Gayle Link RN Ryan Fulmer CHT Eddie Gomez CHT Michelle Potpan CHT Brian Wolfe CHT Shayne Harmsen BS Franklin Brightwater CHT and Dr Xavier Figueroa were instrumental in operations treatments and data collection Special mention Medical Gas Research March Volume 9 Issue 1
Mozayeni et al Med Gas Res belongs to John C Pezzullo PhD Georgetown University Medical Center who died before publication He was instrumental in statistical analysis of data Author contributions Writing the manuscript BRM and WD revision EZ drafting TLL KPS RLB All authors read and approved the final version of the paper for publication Conflicts of interest Drs Beckman and Mozayeni have an interest in CareVector LLC the developer of the case report form data collection software used to support this study provided pro bono to support the study The other authors declare no conflict of interest Financial support The study was funded through pro bono clinical care provided by the investigators and involved clinics augmented by philanthropic resources of the International Hyperbaric Medical Foundation and multiple community hyperbaric clinics Pro bono clinical research has an important role in orphaned conditions such as mild traumatic brain injury where no grant money is available and no pharmaceuticals or devices are commercially labeled for treatment Institutional review board statement The study was approved by the ethics review committee of the Western Institutional Review Board WIRB Protocol 20090761 Declaration of patient consent The authors certify that they have obtained patient consent forms In the form patients have given their consent for their images and other clinical information to be reported in the journal The patients understand that their names and initials not be published and due efforts will be made to conceal their identity but anonymity cannot be guaranteed Reporting statement This study follows the Consolidated Standards of Reporting Trials CONSORT guidelines Biostatistics statement The statistical methods of this study were reviewed by the biostatistician of Oklahoma State University Center for Aerospace Hyperbaric Medicine Tulsa OK USA Copyright license agreement The Copyright License Agreement has been signed by all authors before publication Data sharing statement Individual participant data that underlie the results reported in this article after deidentification text tables figures and appendices Study protocol and informed consent form will be available immediately following publication without end date Results will be disseminated through presentations at scientific meetings and or by publication in a peer reviewed journal Anonymized trial data will be available indefinitely at www figshare com Plagiarism check Checked twice by iThenticate Peer review Externally peer reviewed Open access statement This is an open access journal and articles are distributed under the terms of the Creative Commons Attribution NonCommercialShareAlike 4 0 License which allows others to remix tweak and build upon the work non commercially as long as appropriate credit is given and the new creations are licensed under the identical terms References 1 James Philip B Oxygen and the Brain The Journey of Our Lifetime North Palm Beach FL Best Publishing Co 2014 2 Weaver LK Hyperbaric Oxygen Therapy Indications 13th edition Durham NC Undersea and Hyperbaric Medical Society 2014 Carbon Monoxide poisoning Neurological Decompression Sickness Navy Dive Table 6A Intercranial Abscess Acute Hearing Loss Radiation Necrosis of the Brain compromised flaps and graphs and arterial insufficiency 3 Jain KK The Textbook of Hyperbaric Medicine Fifth edition Cambridge MA Hogrefe Huber Publishers 2009 p X Medical Gas Research March Volume 9 Issue 1 www medgasres com 4 Golden ZL Neubauer R Golden CJ Greene L Marsh J Mleko A Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy Int J Neurosci 2002 112 119 131 5 Hardy P Johnston KM De Beaumont L et al Pilot case study of the therapeutic potential of hyperbaric oxygen therapy on chronic brain injury J Neurol Sci 2007 253 94 105 6 Neubauer RA Gottlieb SF Pevsner NH Hyperbaric oxygen for treatment of closed head injury South Med J 1994 87 933 936 Neubauer RA Gottlieb SF Hyperbaric oxygen for brain injury J Neurosurg 1993 78 687 688 7 Golden Z Golden CJ Neubauer RA Improving neuropsychological function after chronic brain injury with hyperbaric oxygen Disabil Rehabil 2006 28 1379 1386 8 Wright JK Zant E Groom K Schlegel RE Gilliland K Case report treatment of mild traumatic brain injury with hyperbaric oxygen Undersea Hyperb Med 2009 36 391 399 9 H R 6 114th Congress 1st Session To accelerate the discovery development and delivery of 21st century cures and for other purposes The 21st Century Cures Act Signed into law December 13 2016 Washington DC Government Printing Office 2016 10 Perrins DJ James PB Hyperbaric oxygen therapy and multiple sclerosis Undersea Hyperb Med 2002 29 236 238 11 Adamides AA Winter CD Lewis PM Cooper DJ Kossmann T Rosenfeld JV Current controversies in the management of patients with severe traumatic brain injury ANZ J Surg 2006 76 163 174 12 Hyperbaric Oxygen Therapy Don t Be Misled Washington DC FDA Consumer Health Information U S Food and Drug Administration August 2013 13 Smith G Sharp GR Treatment of carbon monoxide poisoning with oxygen under pressure Lancet 1960 2 905 14 Sluiter ME The treatment of carbon monoxide poisoning by the administration of oxygen at high atmospheric pressure Proc R Soc Med 1963 56 1002 1008 15 Duff JH Shibata HR Vanschaik L Usher R Wigmore RA MacLean LD Hyperbaric oxygen a review of treatment in eightythree patients Can Med Assoc J 1967 97 510 515 16 Hart GB Thompson RE The treatment of cerebral ischemia with hyperbaric oxygen OHP Stroke 1971 2 247 250 17 Neubauer RA James P Cerebral oxygenation and the recoverable brain Neurol Res 1998 20 S33 S36 18 Harch PG Kriedt C Van Meter KW Sutherland RJ Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury Brain Res 2007 1174 120 129 19 Paris JJ Schreiber MD Reardon FE Hyperbaric oxygen therapy for a neurologically devastated child whose decision is it J Perinatol 2003 23 250 253 20 Golden Z Golden CJ Neubauer RA Improving neuropsychological function after chronic brain injury with hyperbaric oxygen Disabil Rehabil 2006 28 1379 1386 21 Institute of Medicine of the National Academies Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations Final Assessment Washington DC Institute of Medicine June 2014 22 Hoge CW Jonas WB The ritual of hyperbaric oxygen and lessons for the treatment of persistent postconcussion v symptoms in military personnel JAMA Intern Med 2014 175 53 54 23 Wolf G Cifu D Baugh L Carne W Profenna L The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury J Neurotrauma 2012 29 2606 2612 24 Collet JP Vanasse M Marois P et al Hyperbaric oxygen for children with cerebral palsy a randomised multicentre trial Lancet 2001 357 582 586 11
Mozayeni et al Med Gas Res 25 Harch PG Hyperbaric oxygen therapy for post concussion syndrome contradictory conclusions from a study mischaracterized as sham controlled J Neurotrauma 2013 30 1995 1999 26 Collet JP Vanasse M Marois P et al Hyperbaric oxygen for children with cerebral palsy a randomised multicentre trial Lancet 2001 357 582 586 27 Harch PG Letters to the Editor Journal of Neurotrauma Hyperbaric Oxygen Therapy for Post Concussion Syndrome Contradictory Conclusions From a Study Mischaracterized as Sham Controlled J Neurotrauma 2013 30 1995 1999 28 Shively SB Horkayne Szakaly I Jones RV Kelly JP Armstrong RC Perl DP Characterisation of interface astroglial scarring in the human brain after blast exposure a post mortem case series Lancet Neurol 2016 15 944 953 29 Rosenfeld JV McFarlane AC Bragge P Armonda RA Grimes JB Ling GS Blast related traumatic brain injury Lancet Neurol 2013 12 882 893 30 Grammer GG DeGraba TJ Picon LM va dod clinical practice guideline for the management of concussion mild traumatic brain injury 2016 update VA HSR D Cyberseminars September 29 2016 31 Kroenke K Spitzer RL Williams JB The PHQ 9 validity of a brief depression severity measure J Gen Intern Med 2001 16 606613 32 King NS Crawford S Wenden FJ Moss NE Wade DT The Rivermead Post Concussion Symptoms Questionnaire a measure of symptoms commonly experienced after head injury and its reliability J Neurol 1995 242 587 592 33 Vincent AS Bleiberg J Yan S et al Reference data from the Automated Neuropsychological Assessment Metrics for use in traumatic brain injury in an active duty military sample Mil Med 2008 173 836 852 34 Cernich A Reeves D Sun W Bleiberg J Automated Neuropsychological Assessment Metrics Sports Medicine Battery Arch Clin Neuropsychol 2007 22 S101 114 35 Segalowitz SJ Mahaney P Santesso DL MacGregor L Dywan J Willer B Retest reliability in adolescents of a computerized neuropsychological battery used to assess recovery from concussion Neuro Rehabilitation 2007 22 243 251 36 Johnson DR Vincent AS Johnson AE Gilliland K Schlegel RE Reliability and construct validity of the Automated Neuropsychological Assessment Metrics ANAM mood scale Arch Clin Neuropsychol 2008 23 73 85 37 Gualtieri CT Johnson LG A computerized test battery sensitive to mild and severe brain injury Medscape J Med 2008 10 90 38 Gualtieri CT Johnson LG Reliability and validity of a computerized neurocognitive test battery CNS Vital Signs Arch Clin Neuropsychol 2006 21 623 643 12 www medgasres com 39 Neubauer RA Gottlieb SF Kagan RL Enhancing idling neurons Lancet 1990 35 542 40 Clark J Side Effects In Gesell LB ed Hyperbaric Oxygen Therapy Indications 12th ed Durham NC Undersea and Hyperbaric Medical Society 2009 215 220 41 Parsons HM What Happened at Hawthorne New evidence suggests the Hawthorne effect resulted from operant reinforcement contingencies Science 1974 183 922 932 42 Miller FG Colloca L Kaptchuk TJ The placebo effect illness and interpersonal healing Perspect Biol Med 2009 52 518 539 43 Benedetti F Carlino E Pollo A How placebos change the patient s brain Neuropsychopharmacology 2011 36 339 354 44 Couch JR Stewart KE Wisdom PJ Persistence of symptoms of post concussion syndrome PCSS for up to 8 years in veterans of OEF OIF campaigns of the wars in Iraq and Afghanistan Headache 2012 52 907 45 The Veterans Health Administration s Treatment of PTSD and Traumatic Brain Injury Among Recent Combat Veterans Washington DC Congressional Budget Office Pub No 4097 2012 46 Samueli Institute Is Hyperbaric Oxygen Therapy Effective for Traumatic Brain Injury Preliminary Report Prepared for the Hyperbaric Oxygen Research Program USAMRMC USAMMDA February 18 2015 47 Miller RS Weaver LK Bahraini N et al Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms a randomized clinical trial JAMA Intern Med 2015 175 43 52 48 Hoge CW Jonas WB The ritual of hyperbaric oxygen and lessons for the treatment of persistent postconcussion symptoms in military personnel JAMA Intern Med 2014 175 53 54 49 Harch PG Andrews SR Fogarty EF Lucarini J Van Meter KW Case control study hyperbaric oxygen treatment of mild traumatic brain injury persistent post concussion syndrome and post traumatic stress disorder Med Gas Res 2017 7 156 174 50 Shively SB Horkayne Szakaly I Jones RV2 Kelly JP Armstrong RC Perl DP Characterisation of interface astroglial scarring in the human brain after blast exposure a post mortem case series Lancet Neurol 2016 15 944 953 51 Robert F Worth What if PTSD is More Physical Than Psychological The New York Times Magazine June 10 2016 http nyti ms 1TYYp6U 52 Figueroa XA Wright JK Hyperbaric oxygen B level evidence in mild traumatic brain injury clinical trials Neurology 2016 87 1400 1406 Received October 30 2018 Accepted February 27 2019 Medical Gas Research March Volume 9 Issue 1
Tal et al HBOT Induces Regeneration in mTBI Sepulcre J Masdeu J C Pastor M A Goni J Barbosa C Bejarano B et al 2009 Brain pathways of verbal working memory a lesion function correlation study Neuroimage 47 773 778 doi 10 1016 j neuroimage 2009 04 054 Shi X Y Tang Z Q Sun D and He X J 2006 Evaluation of hyperbaric oxygen treatment of neuropsychiatric disorders following traumatic brain injury Chin Med J 119 1978 1982 Shi X Y Tang Z Q Xiong B Bao J X Sun D Zhang Y Q et al 2003 Cerebral perfusion SPECT imaging for assessment of the effect of hyperbaric oxygen therapy on patients with postbrain injury neural status Chin J Traumatol 6 346 349 Shinoura N Suzuki Y Tsukada M Katsuki S Yamada R Tabei Y et al 2007 Impairment of inferior longitudinal fasciculus plays a role in visual memory disturbance Neurocase 13 127 130 doi 10 1080 13554790701399254 Sidaros A Engberg A W Sidaros K Liptrot M G Herning M Petersen P et al 2008 Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome a longitudinal study Brain 131 559 572 doi 10 1093 brain awm294 Stein S C Graham D I Chen X H and Smith D H 2004 Association between intravascular microthrombosis and cerebral ischemia in traumatic brain injury Neurosurgery 54 687 691 discussion 691 doi 10 1227 01 NEU 0000108641 98845 88 Sterr A Herron K A Hayward C and Montaldi D 2006 Are mild head injuries as mild as we think Neurobehavioral concomitants of chronic postconcussion syndrome BMC Neurol 6 7 doi 10 1186 1471 2377 6 7 Sugiyama K Kondo T Oouchida Y Suzukamo Y Higano S Endo M et al 2009 Clinical utility of diffusion tensor imaging for evaluating patients with diffuse axonal injury and cognitive disorders in the chronic stage J Neurotrauma 26 1879 1890 doi 10 1089 neu 2008 0839 Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E and Efrati S 2015 Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 33 943 951 doi 10 3233 RNN 150585 Thaler A Mirelman A Gurevich T Simon E Orr Urtreger A Marder K et al onsortium A J 2012 Lower cognitive performance in healthy G2019S LRRK2 mutation carriers Neurology 79 1027 1032 doi 10 1212 WNL 0b013e3182684646 Vlodavsky E Palzur E and Soustiel J F 2006 Hyperbaric oxygen therapy reduces neuroinflammation and expression of matrix metalloproteinase 9 in the rat model of traumatic brain injury Neuropathol Appl Neurobiol 32 40 50 doi 10 1111 j 1365 2990 2005 00698 x Wada T Asano Y and Shinoda J 2012 Decreased fractional anisotropy evaluated using tract based spatial statistics and correlated with cognitive dysfunction in patients with mild traumatic brain injury in the chronic stage AJNR Am J Neuroradiol 33 2117 2122 doi 10 3174 ajnr A3141 Wright J K Zant E Groom K Schlegel R E and Gilliland K 2009 Case report treatment of mild traumatic brain injury with hyperbaric oxygen Undersea Hyperb Med 36 391 399 Yuan W Holland S K Schmithorst V J Walz N C Cecil K M Jones B V et al 2007 Diffusion tensor MR imaging reveals persistent white matter alteration after traumatic brain injury experienced during early childhood AJNR Am J Neuroradiol 28 1919 1925 doi 10 3174 ajnr A0698 Zhang J H Lo T Mychaskiw G and Colohan A 2005 Mechanisms of hyperbaric oxygen and neuroprotection in stroke Pathophysiology 12 63 77 doi 10 1016 j pathophys 2005 01 003 Zur D Naftaliev E and Kesler A 2015 Evidence of multidomain mild cognitive impairment in idiopathic intracranial hypertension J Neuroophthalmol 35 26 30 doi 10 1097 WNO 0000000000000199 Marin J R Weaver M D Yealy D M and Mannix R C 2014 Trends in visits for traumatic brain injury to emergency departments in the United States JAMA 311 1917 1919 doi 10 1001 jama 2014 3979 McCauley S R Boake C Pedroza C Brown S A Levin H S Goodman H S et al 2005 Postconcussional disorder are the DSM IV criteria an improvement over the ICD 10 J Nerv Ment Dis 193 540 550 doi 10 1097 01 nmd 0000172592 05801 71 McCrory P Johnston K Meeuwisse W Aubry M Cantu R Dvorak J et al 2005 Summary and agreement statement of the 2nd International Conference on Concussion in Sport Prague 2004 Br J Sports Med 39 196 204 doi 10 1136 bjsm 2005 018614 Melton J L 2005 Psychometric Evaluation of the Mindstreams Neuropsychological Screening Tool Panama City FL Navy Experimental Diving Unit US Miller E K and Cohen J D 2001 An integrative theory of prefrontal cortex function Annu Rev Neurosci 24 167 202 doi 10 1146 annurev neuro 24 1 167 Mu J Krafft P R and Zhang J H 2011 Hyperbaric oxygen therapy promotes neurogenesis where do we stand Med Gas Res 1 14 doi 10 1186 2045 9912 1 14 Murugavel M Cubon V Putukian M Echemendia R Cabrera J Osherson D et al 2014 A longitudinal diffusion tensor imaging study assessing white matter fiber tracts after sports related concussion J Neurotrauma 31 1860 1871 doi 10 1089 neu 2014 3368 Neubauer R A and James P 1998 Cerebral oxygenation and the recoverable brain Neurol Res 20 Suppl 1 S33 S36 doi 10 1080 01616412 1998 11740606 Niogi S N and Mukherjee P 2010 Diffusion tensor imaging of mild traumatic brain injury J Head Trauma Rehabil 25 241 255 doi 10 1097 HTR 0b013e3181e52c2a Ostergaard L Engedal T S Aamand R Mikkelsen R Iversen N K Anzabi M et al 2014 Capillary transit time heterogeneity and flowmetabolism coupling after traumatic brain injury J Cereb Blood Flow Metab 34 1585 1598 doi 10 1038 jcbfm 2014 131 stergaard L Sorensen A G Kwong K K Weisskoff R M Gyldensted C and Rosen B R 1996a High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part II experimental comparison and preliminary results Magn Reson Med 36 726 736 stergaard L Weisskoff R M Chesler D A Gyldensted C and Rosen B R 1996b High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part I mathematical approach and statistical analysis Magn Reson Med 36 715 725 Peng Z R Yang A L and Yang Q D 2014 The effect of hyperbaric oxygen on intracephalic angiogenesis in rats with intracerebral hemorrhage J Neurol Sci 342 114 123 doi 10 1016 j jns 2014 04 037 Perez A M Adler J Kulkarni N Strain J F Womack K B Diaz Arrastia R 2014 Longitudinal white matter changes after traumatic axonal injury J Neurotrauma 31 1478 1485 doi 10 1089 neu 2013 3216 Rocha F T Rocha A F Massad E and Menezes R 2005 Brain mappings of the arithmetic processing in children and adults Brain Res Cogn Brain Res 22 359 372 doi 10 1016 j cogbrainres 2004 09 008 Sagi Y Tavor I Hofstetter S Tzur Moryosef S Blumenfeld Katzir T and Assaf Y 2012 Learning in the fast lane new insights into neuroplasticity Neuron 73 1195 1203 doi 10 1016 j neuron 2012 01 025 Sasson E Doniger G M Pasternak O Tarrasch R and Assaf Y 2013 White matter correlates of cognitive domains in normal aging with diffusion tensor imaging Front Neurosci 7 32 doi 10 3389 fnins 2013 00032 Schweiger A Doniger G M Dwolatzky T Jaffe D and Simon E S 2003 Reliability of a novel computerized neuropsychological battery for mild cognitive impairment Acta Neuropsychol 1 407 413 Selassie A W Wilson D A Pickelsimer E E Voronca D C Williams N R and Edwards J C 2013 Incidence of sport related traumatic brain injury and risk factors of severity a population based epidemiologic study Ann Epidemiol 23 750 756 doi 10 1016 j annepidem 2013 07 022 Sepehrband F Clark K A Ullmann J F Kurniawan N D Leanage G Reutens D C et al 2015 Brain tissue compartment density estimated using diffusion weighted MRI yields tissue parameters consistent with histology Hum Brain Mapp 36 3687 3702 doi 10 1002 hbm 22872 Frontiers in Human Neuroscience www frontiersin org Conflict of Interest Statement The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest Copyright 2017 Tal Hadanny Sasson Suzin and Efrati This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY The use distribution or reproduction in other forums is permitted provided the original author s or licensor are credited and that the original publication in this journal is cited in accordance with accepted academic practice No use distribution or reproduction is permitted which does not comply with these terms 12 October 2017 Volume 11 Article 508
Expert Review of Neurotherapeutics ISSN 1473 7175 Print 1744 8360 Online Journal homepage https www tandfonline com loi iern20 Reflections on the neurotherapeutic effects of hyperbaric oxygen Shai Efrati Eshel Ben Jacob To cite this article Shai Efrati Eshel Ben Jacob 2014 Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Review of Neurotherapeutics 14 3 233 236 DOI 10 1586 14737175 2014 884928 To link to this article https doi org 10 1586 14737175 2014 884928 Published online 29 Jan 2014 Submit your article to this journal Article views 6302 View related articles View Crossmark data Citing articles 13 View citing articles Full Terms Conditions of access and use can be found at https www tandfonline com action journalInformation journalCode iern20
Editorial Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Rev Neurother 14 3 233 236 2014 Shai Efrati Author for correspondence The Institute of Hyperbaric Medicine Assaf Harofeh Medical Center Zerifin Israel and Research and Development Unit Assaf Harofeh Medical Center Zerifin Israel and Sackler School of Medicine Tel Aviv University Tel Aviv Israel and Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Tel 972 089 779 3935 Fax 972 089 204 989 efratishai 013 net Eshel Ben Jacob Author for correspondence The Institute of Hyperbaric Medicine Assaf Harofeh Medical Center Zerifin Israel and Research and Development Unit Assaf Harofeh Medical Center Zerifin Israel and Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel and The Raymond and Beverly Sackler Faculty of Exact Sciences School of Physics and Astronomy Tel Aviv University Tel Aviv Israel and Center for Theoretical Biological Physics Rice University Houston TX USA Tel 972 036 407 845 Fax 001 713 247 8162 eshel rice edu Traumatic brain injury TBI and stroke are the major causes of brain damage and chronic neurological impairments There is no agreed upon effective metabolic intervention for TBI and stroke patients with chronic neurological dysfunction Clinical studies published this year present convincing evidence that hyperbaric oxygen therapy HBOT might be the coveted neurotherapeutic method for brain repair Here we discuss the multi faceted role of HBOT in neurotherapeutics in light of recent persuasive evidence for HBOT efficacy in brain repair and the new understanding of brain energy management and response to damage We discuss optimal timing of treatment dosage suitable candidates and promising future directions The challenge Traumatic brain injury TBI stroke and age related metabolic brain disorders are the major causes of brain damage and chronic neurological impairments Today there is no agreed upon effective metabolic treatment intervention in the routine clinical practice for TBI and stroke patients with chronic neurological dysfunction Intensive therapy and rehabilitation programs are valuable for improving quality of life right after brain injury but often provide only partial relief and leave the patients chronically disabled With the aging of the population the severity of the problem posed by stroke TBI mainly due to home accidents and metabolic disorders which can lead to dementia and Alzheimer s disease is expected to increase Experts agree that novel neurotherapeutic methods to repair and protect the brain from damage caused by these insults are needed more than ever before New hope Clinical studies published this year present convincing evidence that hyperbaric oxygen therapy HBOT might be the coveted neurotherapeutic method for brain repair 1 2 HBOT is a treatment in which oxygen enriched air up to 100 is administrated to patients in a chamber where the pressure is elevated above one atmosphere absolute 1ATA which is the ambient atmospheric pressure It is becoming widely acknowledged that the combined action of hyperoxia and hyperbaric pressure leads to significant improvement in tissue oxygenation while targeting both oxygenand pressure sensitive genes 3 6 resulting in improved mitochondrial metabolism with anti apoptotic and anti inflammatory effects 7 12 Here we reflect on the multifaceted role of HBOT in neurotherapeutics in light of recent persuasive evidence for HBOT efficacy in brain repair and of new understanding of brain energy management and response to damage We discuss the optimal timing of treatment optimal dose response curve oxygenpressure levels suitable candidates and promising future directions A generation of debate The idea that HBOT can provide a valuable tool for brain repair was first proposed almost half a century ago and has been considered anecdotal ever since Interest was renewed in the mid 90s 8 13 but the results were either ignored or seriously questioned by the medical KEYWORDS hyperbaric oxygen neuroplasticity neurotherapeutic stroke traumatic brain injury informahealthcare com 10 1586 14737175 2014 884928 2014 Informa UK Ltd ISSN 1473 7175 233
Editorial Efrati Ben Jacob community Huang and Obenaus in their 2011 review presented an objective summary of the clinical trials and associated debate till 2011 and a thoughtful description of the animal trials and their implications 8 They reasoned that the HBOTinduced neuroprotection in animal model is due to the observed improved tissue oxidation improved mitochondrial redox preservation of mitochondria integrity hindering of mitochondria associated apoptotic pathways as well as antiinflammatory effects 8 Until 2011 all human HBOT studies involved severe TBI patients While mortality was decreased in those studies there was no significant change in the quality of life This combined with knowledge from a wealth of animal studies indicated that the time of treatment and dose response curve should be reassessed Most importantly it led to the understanding that HBOT should be practiced on mild tomoderate TBI patients who are more apt to achieve clinically meaningful recovery Pre and post treatment SPECT imaging showed that HBOT led to restoration of neuronal activity in stunned areas A second randomized prospective trial published earlier this year used a similar crossover approach and presented equally persuasive evidence that HBOT can also revitalize chronically impaired brain function and significantly improve the quality of life of post stroke patients even years after the event 1 The participants in this study suffered a stroke 6 36 months prior to the trial They were also randomly divided into treated and control group went through brain function and quality evaluations These stroke patients were also treated with 40 HBOT daily sessions However while the mTBI patients were treated at a lower pressure of 1 5ATA since they all had an intact macrovascular bed the stroke patients were given 90 min sessions at 2 0ATA and 100 oxygen The results of SPECT imaging were well correlated with clinical improvements and revealed restored activity mostly in stunned areas in the surroundings of necrotic foci Persuasive new evidence Convincing evidence that HBOT can revitalize chronically impaired brain functions and significantly improve the quality of life of mild TBI mTBI patients with prolonged postconcussion syndrome at late chronic stage even years after injury are presented in a new randomized prospective trial published this year 2 A crossover approach was adopted in order to overcome the HBOT inherent sham control constraint discussed further below The participants who had suffered mTBI 1 5 years prior to the trial were randomly divided into two groups trial and control The trial group patients received 2 months of HBOT while the control group went without treatment in those 2 months The latter were given the same treatment as the trial group 2 months later The advantage of the crossover approach is the opportunity for a triple comparison between treatments of two groups between treatment and no treatment periods of the same group and between treatment and no treatment in different groups It also overcomes the problem posed by the impossibility of making people believe they are exposed to high pressure when they are actually not The treatment consisted of 40 daily sessions lasting 1 h at pressure of 1 5ATA and breathing 100 oxygen The patients cognitive functions and quality of life were assessed by detailed computerized evaluations and compared for all patients with single photon emission computed tomography SPECT scans HBOT sessions led to similar significant improvements in tests of cognitive function and quality of life in both groups No significant improvements occurred by the end of the nontreatment period in the control group Analysis of brain imaging showed significantly increased neuronal activity after a 2 month period of HBOT compared with the control period What makes the results particularly persuasive is the remarkable agreement between the cognitive function restoration and the changes in brain functionality as detected by the SPECT scans The diffuse nature of the mTBI injury renders the pathological damage hard to detect by common neuroimaging methods such as computed tomography and MRI 234 HBOT can activate cerebral plasticity revitalize chronically impaired brain functions The new trials provide convincing evidence that HBOT can induce cerebral plasticity leading to repair of chronically impaired brain functions and improved quality of life in poststroke patients and mTBI patients with prolonged postconcussion syndrome even years after the brain insult 1 2 The term cerebral plasticity is used here as an umbrella term that encompasses both neuroplasticity as commonly used in neuroscience and beyond synaptic changes such as myelinization regeneration of axonal white matter angiogenesis and changes in the glial fabric The observed restoration of neuronal activity in the metabolically dysfunctional stunned areas indicate HBOT as a potent means of delivering to the brain sufficient oxygen needed for activation of neuroplasticty and restoration of impaired functions These are entailed via assortment of intricate mechanisms some of which are mentioned below Underlying repair mechanisms Brain insults may result in a variety of brain injuries including impairment of microvascular integrity and cerebral perfusion These lead to reduced metabolism and neuronal activity which in turn lead to loss of synapses and tampered neuronal connectivity 2 8 9 The stunned areas mentioned earlier are characterized by anaerobic metabolism and ATP depletion culminating in stagnation and shortage of energy for the healing processes and they may persist like this dysfunctional but alive for years after injury 2 8 9 The decreased oxygen level not only causes reduction in neuronal activity but also prevents the generation of new synaptic connections and angiogenesis HBOT can initiate vascular repair and improve cerebral vascular flow induce regeneration of axonal white matter stimulate axonal growth promote blood brain barrier integrity and reduce inflammatory reactions as well as brain edema 7 12 At the cellular level HBOT can improve cellular metabolism reduce apoptosis alleviate oxidative stress and increase Expert Rev Neurother 14 3 2014
Reflections on the neurotherapeutic effects of hyperbaric oxygen levels of neurotrophins and nitric oxide through enhancement of mitochondrial function in both neurons and glial cells and may even promote neurogenesis of endogenous neural stem cells 7 12 14 Regarding mitochondria it is important to note that stroke and TBI engender depolarization of the mitochondria membrane and induction of mitochondrial permeability transition pore which reduces the efficiency of energy production and elevate the level of reactive oxygen species 15 HBOT can inhibit mitochondrial permeability transition pore and thus has the potential to reverse this abnormality 8 However it must be applied carefully to ascertain that the increased tissue oxygen does not cause cellular toxicity due to overly high reactive oxygen species levels Time of treatment Many innate repair mechanisms each with a different characteristic time are activated following the onset of acute brain injury and some may be negatively affected by premature application of HBOT HBOT procedure can begin either at the degenerative or at the regenerative stage At the degenerative stage it must be administered with great care to avoid toxicity On the other hand elevated oxygen levels during the regenerative stage would supply the energy needs for the innate brain repair processes While it is not possible to mark a clear line between the regenerative and the degenerative phases 16 it is quite clear that more than 1 month after the acute event in a stable patient the degenerative process has ended The differences in initiation times and protocols of HBOT may explain contradictive results in previous studies where HBOT timing was not taken into consideration 1 2 17 21 Dose response curve treatment duration The minimal effective dosages of the active ingredients in HBOT pressure and oxygen concentration are still unknown and future studies are needed to test this issue by evaluating the optimal case specific dose response curves For example in the previously described trials 2 0ATA was used for post stroke patients and 1 5ATA was used for mTBI 1 2 There are many case reports illustrating significant effects with even small increases in air pressure including effects on the brain 22 The dose response curve is related to the inherent difficulties in handling the sham control and is a source of misinterpretation of clinical studies the minimal elevated pressure a patient can sense is 1 3 atmosphere which can induce more than 50 elevation in tissue oxygenation Since such oxygenation can have significant physiological effects 1 2 treatment with room air at 1 3ATA is not an ineffectual treatment as is required from a proper sham control At the same time over oxygenation in response to pressure above 2 0ATA can have an inhibitory effect or even focal toxicity It is conceivable that HBOT above two atmospheres can be less effective than 1 3ATA explaining the unexpected improvements in control groups when 1 3ATA was used for sham control informahealthcare com Editorial The duration of treatment is also an unresolved issue It is quite clear that weeks to months would be necessary for brain tissue regeneration and angiogenesis but the upper time limit from which no further improvement is expected is still unknown More studies are needed to determine the minimal effective dosage and the duration for a specific brain injury Non invasive in chamber measurements are currently being developed specifically EEG and diffusion tensor imaging and may shed some light on this important question Clearly there is an urgent need for additional larger scale multi center clinical studies to further confirm the findings and determine the most effective and personalized treatment protocols To guarantee effective and well designed clinical studies wide scale biomedical research is required Such research will also provide validation of the clinical findings crucial aid in interpretation of the results and important clues to additional applications of HBOT Optimal candidates for HBOT Since hyperbaric oxygen therapy is the only treatment proven to significantly benefit post stroke and mTBI patients without limiting side effects it is reasonable to allow the millions of these patients to benefit from it right away and not wait for rigorous studies The classical candidate for HBOT is a patient with unrecovered brain injury where tissue hypoxia is the limiting factor for the regeneration possesses In this patient HBOT may induce neuroplasticity in the stunned regions where there is a brain anatomy physiology e g SPECT computed tomography mismatch 1 2 The anatomical physiological imaging should serve as part of the basic evaluation of every HBOT candidate just like transcutaneous oximetry at the ulcer bed serves as a basic evaluation for patients suffering from peripheral non healing wounds 23 24 Looking ahead Based on the aforementioned rationale one can surmise that HBOT could also be effective in early stages of vascular dementia Alzheimer s disease and other conditions where the clinical presentation could not be fully explained by anatomical imaging However this will require novel basic biomedical research to understand the HBOT effect on the recently discovered mitochondria associated cellular response to hypoxia 7 12 which is a common denominator of stroke TBI dementia and aging 25 26 Financial competing interests disclosure The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript This includes employment consultancies honoraria stock ownership or options expert testimony grants or patents received or pending or royalties No writing assistance was utilized in the production of this manuscript 235
Editorial Efrati Ben Jacob References 1 Efrati S Fishlev G Bechor Y et al Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS One 2013 8 1 e53716 2 Boussi Gross R Golan H Fishlev G et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 2013 8 11 e79995 3 Harch PG Hyperbaric oxygen therapy for post concussion syndrome contradictory conclusions from a study mischaracterized as sham controlled J Neurotrauma 2013 30 23 1995 9 4 5 6 7 8 9 Godman CA Chheda KP Hightower LE et al Hyperbaric oxygen induces a cytoprotective and angiogenic response in human microvascular endothelial cells Cell Stress Chaperones 2010 15 4 431 42 10 Vlodavsky E Palzur E Soustiel JF Hyperbaric oxygen therapy reduces neuroinflammation and expression of matrix metalloproteinase 9 in the rat model of traumatic brain injury Neuropathol Appl Neurobiol 2006 32 1 40 50 11 Lin KC Niu KC Tsai KJ et al Attenuating inflammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury J Trauma Acute Care Surg 2012 72 3 650 9 12 Zhang JH Lo T Mychaskiw G et al Mechanisms of hyperbaric oxygen and neuroprotection in stroke Pathophysiology 2005 12 1 63 77 13 Rockswold GL Ford SE Anderson DC et al Results of a prospective randomized trial for treatment of severely brain injured patients with hyperbaric oxygen J Neurosurg 1992 76 6 929 34 14 Chen Y Nadi NS Chavko M et al Microarray analysis of gene expression in rat cortical neurons exposed to hyperbaric air and oxygen Neurochemical Res 2009 34 6 1047 56 Kendall AC Whatmore JL Harries LW et al Different oxygen treatment pressures alter inflammatory gene expression in human endothelial cells Undersea Hyperbaric Medicine 2013 40 2 115 23 Chen Z Ni P Lin Y et al Visual pathway lesion and its development during hyperbaric oxygen treatment a bold fMRI and DTI study JMRI 2010 31 5 1054 60 Huang L Obenaus A Hyperbaric oxygen therapy for traumatic brain injury Medical Gas Research 2011 1 1 21 Neubauer RA James P Cerebral oxygenation and the recoverable brain Neurol Res 1998 20 Suppl 1 S33 6 236 Gu nther A Ku ppers Tiedt L Schneider PM et al Reduced infarct volume and differential effects on glial cell activation after hyperbaric oxygen treatment in rat permanent focal cerebral ischaemia Eur J Neurosci 2005 21 11 3189 94 15 Wang W Fang H Groom L et al Superoxide flashes in single mitochondria Cell 2008 134 2 279 90 16 Lo EH A new penumbra transitioning from injury into repair after stroke Nat Med 2008 14 5 497 500 17 Anderson DC Bottini AG Jagiella WM et al A pilot study of hyperbaric oxygen in the treatment of human stroke Stroke 1991 22 9 1137 42 18 Nighoghossian N Trouillas P Adeleine P et al Hyperbaric oxygen in the treatment of acute ischemic stroke A double blind pilot study Stroke 1995 26 8 1369 72 19 Rusyniak DE Kirk MA May JD et al Hyperbaric oxygen therapy in acute ischemic stroke results of the Hyperbaric Oxygen in Acute Ischemic Stroke Trial Pilot Study Stroke 2003 34 2 571 4 20 Vila JF Balcarce PE Abiusi GR et al Improvement in motor and cognitive impairment after hyperbaric oxygen therapy in a selected group of patients with cerebrovascular disease a prospective single blind controlled trial Undersea Hyperbaric Medicine 2005 32 5 341 9 21 Imai K Mori T Izumoto H et al Hyperbaric oxygen combined with intravenous edaravone for treatment of acute embolic stroke a pilot clinical trial Neurol Med Chir 2006 46 8 373 8 discussion 378 22 James PB Hyperbaric oxygenation for cerebral palsy Lancet 2001 357 9273 2052 3 23 Niinikoski JH Clinical hyperbaric oxygen therapy wound perfusion and transcutaneous oximetry World Journal Surg 2004 28 3 307 11 24 Efrati S Galli N Bergan J et al Hyperbaric oxygen oxidative stress NO bioavailability and ulcer oxygenation in diabetic patients Undersea Hyperbaric Medicine 2009 36 1 1 12 25 Small GW Kepe V Siddarth P et al PET scanning of brain tau in retired national football league players preliminary findings Am J Geriatr Psychiat 2013 21 2 138 44 26 Gomes AP Price NL Ying AJY et al Declining NAD induces a pseudohypoxic state disrupting nuclear mitochondrial communication during aging Cell 2013 155 7 1624 38 Expert Rev Neurother 14 3 2014
HYPERBARIC OXYGEN THERAPY FACT SHEET 2012 Quotes Hyperbaric Oxygen Treatment can provide an important weapon in the fight against numerous disorders Dr Richard Neubauer1 Giving more oxygen is not alternative medicine it is sound science and common sense There is no substitute for oxygen Professor Philip B James MB ChB PhD DIH FFOM2 Hyperbaric medicine has been operating in Russia since 1965 They have used it widely and have had very dramatic results they ve got figures showing they can detox people in half the time that it takes conventionally Peter McCann Chairman HBOT Trust3 Summary This fact sheet provides a general introduction to the benefits of Hyperbaric Oxygen Therapy HBOT and is aimed at people who are interested in finding out more detail about this remarkable treatment Considering how few people know about the benefits of HBOT even among the medical community this fact sheet should be of interest to doctors and health professionals who are interested in finding new and cost effective forms of treatment Introduction Hyperbaric Oxygen Treatment HBOT was first reported in The Lancet in 1887 and is best known for the treatment of deep sea divers suffering from the bends decompression sickness 4 HBOT can be used in the treatment of Diabetes 5 Cancer 6 Cardiovascular disease 7 Liver disease 8 1
Brain injury 9 Cerebral palsy 10 Alcohol and drug addiction11 Anecdotal evidence also shows that HBOT helps to improve the appetite and those who have had difficulty sleeping It is also useful in the treatment of damaged livers and brains of recovering alcoholics and drug addicts What is HBOT Every time you go up in an aeroplane you are sitting in a hyperbaric chamber explains Professor Philip B James a leading British expert Hyperbaric is simply a term describing an increase in ambient pressure In an aeroplane the pressure has to increase to compensate for the reduced pressure at altitude so our bodies can breathe enough oxygen HBOT Hyperbaric Oxygen Therapy is the medical use of oxygen at a level higher than atmospheric pressure Patients go into a pressurised chamber for an hour and breathe pure oxygen through a mask The result is a big increase in oxygen in the bloodstream the generation of new stem cells and the natural repair of damaged organs and tissues The treatment benefits a wide range of ailments and it also helps to reduce swellings inflammations and wounds that have not healed Dr Harch12 one of the leading American experts on hyperbaric medicine describes HBOT as a biological therapy in other words the increase of oxygen in the blood enables the body to repair itself Dr Harch points out that most ordinary drugs only treat the symptoms of ailments whereas HBOT enables the natural repair of damaged body tissues releases stem cells and is a DNA signaling drug that spike of oxygen is turning on the DNA These factors collectively form a very powerful treatment process Professor Philip James13 a leading British expert on hyperbaric medicine and consultant to Castle Craig Hospital explains why a pressurised chamber is needed To significantly increase the level of oxygen carried in the blood needs a pressure chamber Giving a high level of oxygen for just one hour a day may promote the repair of tissues when all other medical interventions have failed In other words giving more oxygen extends the envelope of natural recovery Many people wonder why standard oxygen therapy the application of 2
oxygen through a facemask as commonly used in ambulances and hospitals does not have the same effect as HBOT The experts point out that in order to benefit from an increase of oxygen in the blood the air pressure in the surrounding atmosphere must be higher than normal air pressure i e the patient needs to go into a pressurised container and then breathe additional oxygen Standard oxygen therapy helps improve breathing but it lacks the therapeutic properties of HBOT How Does Oxygen Help the Body Oxygen plays a key role in the healing and repairing of damaged cells in our bodies but often the flow of oxygen is blocked and the healing process takes much longer All cells benefit from exposure to oxygen for example a cut on the knee will heal more rapidly if the air is allowed onto it Does it Help the Brain Years of alcohol tobacco and drug abuse can result in brain damage and a prematurely aged brain Initial evidence suggests that HBOT may have a role in rejuvenating and rebuilding patients brains and hence their lives A hyperbaric chamber can supply pure oxygen to the brain stimulating the production of new blood vessels New research shows that increased oxygen flow in the blood can result in the awakening of dormant cells in the brain and the creation of new ones neurogenesis How Does it Work Here is a technical explanation of how it works Oxygen is dissolved in the blood and transported in combination with haemoglobin in the red blood cells throughout the body This dissolved oxygen passes into the tissues Breathing high levels of oxygen under hyperbaric conditions causes greater uptake of oxygen by the bodily fluids and so more can reach areas where the circulation is diminished or blocked and therefore improve recovery The extra oxygen greatly enhances the ability of white blood cells to kill bacteria It also reduces swelling and allows new blood vessels to grow more rapidly into the affected areas Source HBOT Trust14 What is an HBOT Chamber The typical hyperbaric chamber is a hard shelled structure rather like a section of a big metal pipe They are similar to the hyperbaric chambers which are used for divers with decompression sickness the bends Such chambers can be run at absolute pressures of up to 6 bars but the usual 3
pressure is just 2 bars Is it Safe To be in a hyperbaric chamber is to be in the safest place in a hospital as breathing such a high concentration of oxygen a patient cannot suffer a stroke or heart attack It would be difficult to find a patient killed by oxygen in a year but of course there are plenty of deaths from lack of it Professor Philip James former Emiretus Professor of Medicine at the University of Dundee The type of pressure chamber used by the Hyperbaric Oxygen Treatment Trust HBOTT is considered so safe that its use was deregulated by an Act of Parliament in 200815 At the HBOTT s chamber in Scotland each session is monitored by several trained technicians Visual communication is ensured by video cameras at either end of the chamber and audio communication is provided by a microphone speaker setup Over 2 4 million treatment sessions for neurological problems and other conditions have been carried out in the UK since 1982 at 64 non profit centres run by volunteers and patients in the UK These treatments have been carried out without a single serious accident Contra Indications There are some rare contra indications for HBO treatment such as sinus pain claustrophobia and myopia16 However the medical textbook Hyperbaric Medicine Practice states Of all the medical treatments carried out in hospitals hyperbaric oxygen treatment is one of the most benign when it comes to side effects 17 What are the Benefits of HBOT As mentioned above HBOT can be used as treatment for a wide range of diseases such as diabetes multiple sclerosis cancer and lyme disease To see more details about these treatments please visit the research section of the HBOTT website The various benefits of HBOT are still being discovered by medical researchers Evidence shows that HBOT curbs infection and promotes the growth of new capillaries and blood vessels to areas of poor circulation particularly useful for those with diabetes It also boosts collagen formation 4
and is very good for the complexion in the USA HBOT is used as a beauty treatment HBOT helps clear the body of toxins and can be a useful component of drug and alcohol detoxification Oxygen is the natural antibiotic of the body Oxygen controls over 300 genes and increases stem cells It helps the damaged bodies of drug and alcohol addicts to recover by speeding up the healing process Creating Stem Cells The most exciting development in recent years was the discovery by medical researchers at Pennsylvania University in the USA that HBOT can help the body increase the production of stem cells New stem cells can help repair damaged organs skin bones and ligaments and are instrumental in the healing process 18 How can HBOT Help People with Alcohol and Drug Addiction Alcohol and drug abuse can result in the buildup of aldehydes and acids in the brain Increasing the absorption of oxygen can reduce the time these toxic substances remain in the brain Thus detoxification of the body is speeded up Evidence in Scotland where HBOT is used to treat addicts in residential treatment shows that HBOT helps to Stimulate the appetite many addicts suffer from eating disorders and improved eating is an important part of addiction treatment Improve sleep patterns many addicts have not slept properly in years and many find sleeping during detox difficult Helps damaged livers and brains by supplying these organs with a higher dosage of oxygen new blood vessels are built and the damage can be repaired What s the Location of our Chamber Hyperbaric oxygen treatment involves sitting in a pressurised chamber and breathing oxygen through a face mask for a period of one hour A typical number of treatment sessions may be 20 one a day for a period of four weeks but some ailments may require more or less sessions as each 5
individual requires different levels of treatment Our chamber is located in a purpose built building in the extensive 50 acre 20 hectare grounds of Castle Craig Hospital located one hour south of Edinbugh With 18 seats it is the biggest hyperbaric oxygen chamber in Scotland and the only one in UK that is dedicated to the treatment of alcoholics and drug addicts Inside patients can relax read write or watch films on one of the two flat panel screens that are placed at either end of the chamber The increase in air pressure can be felt in the ears which pop and patients are given water to drink to help with this The experience is similar to ascending in a plane What Does the Medical Profession Say About HBOT Despite the fact that there is a wealth of HBOT experience from the diving aviation and military sectors the medical establishment in Britain remains uninformed about HBOT In addition oxygen medicine is not taught at medical school and as a result most GPs are unaware of its benefits The official NHS line is that HBOT is a safe treatment but more research is needed The Lancet medical journal does not comment on HBOT as a treatment but it has listed a number of articles in various medical journals 19 While the NHS recognises the value of standard oxygen therapy it only recommends HBOT for the treatment of carbon monoxide poisoning Unfortunately the NHS does not recommend HBOT as a treatment for all the other ailments it can help with but neither does it oppose the treatment by private clinics What s the View of the HBOT Pioneers Professor Philip James Emeritus Professor of Medicine at the University of Dundee frequently challenges the establishment position on HBOT Giving more oxygen is not alternative medicine it is sound science and commonsense There is no substitute for oxygen and hyperbaric medicine must be included in the core curriculum of our medical schools It is necessary to have distrust of the miraculous in medicine especially 6
when for example claims are made for drugs whose pharmacology and benefit have not been scientifically established Although oxygen hardly falls into this category as no one seriously denies its importance to life it is surprising that using a simple enclosure to allow the delivery of high level of oxygen to relieve an acute deficiency is still regarded by some physicians as quackery Professor James goes on to address the other arguments against the establishment view of oxygen therapy They commonly argue that as blood is virtually saturated with oxygen breathing air no more can be carried but the saturation referred to is of haemoglobin not plasma and the haemoglobin value can be 100 when the brain is dying from hypoxia In fact there is actually no limit to the amount of oxygen which can be carried in plasma and at three times atmospheric pressure sufficient can be dissolved to support life without the presence of haemoglobin The arguments against oxygen treatment must be met toxicity is easily dealt with because the dose time limits of hyperbaric oxygen treatment are very well established and include data from millions of man hours of pure oxygen breathing in military diving So are the minor barometric problems such as clearing the middle ear For those interested in learning more from Professor James we suggest you visit YouTube where you can find a series of 6 lectures by him Contact Details Please contact us if you would like more information about HBOT Manager of the HBOT unit Max Volino PhD Contact phone number 44 0 75 012 54918 and 44 0 1721 722 763 Fax 44 0 1721 752662 Email info hyperbaricoxygentherapy org uk Website http www hyperbaricoxygentherapy org uk index php We would particularly recommend that you look at the Hyperbaric Oxygen Treatment Trust website www hyperbaricoxygentherapy org uk one of the most comprehensive information sources online 7
References 1 www oceanhbo com 2 http www ihausa org docs james html 3 http www inexcess tv p 9948 v 1 4https docs google com viewer url http www hyperbaricoxygentherapy org uk resources docs RCT_Li _The_monoplace_hyperbaric_chamber_and_managem ent_of_decompression_illness pdf 5 http www ncbi nlm nih gov pubmed 8941460 6https docs google com viewer url http www hyperbaricoxygentherapy org uk resources docs Hyperoxia_increases_the_uptake_of_5fluorouracil_in_mammary__tumors_independently_of_changes_in_interstitial_flui d_pressure_and__tumor_stroma_ pdf 7 http www hyperbaricoxygentherapy org uk article hyperbaric oxygen andyour heart 73 8 http cat inist fr aModele afficheN cpsidt 17359188 9https docs google com viewer url http www hyperbaricoxygentherapy org uk resources docs Harch__Post_Traumatic_Brain_Disorder_and_hyperbaric_oxygen_treatment pdf 10 http www ncbi nlm nih gov pubmed 11558483 11 http www hyperbaricoxygentherapy org uk article research and guidance4 Alcohol 20and 20Drug 20Addiction 12 http www hbot com about practice 13 http www ihausa org docs james html 14 http www hyperbaricoxygentherapy org uk article faqs 5 3 15http webarchive nationalarchives gov uk www dh gov uk en Consultations Liveconsultations DH_083519 16 http www hyperbaricoxygentherapy org uk article faqs 5 8 17http www hyperbaricmedicine com productcart pc viewPrd asp idproduct 8 3 idcategory 2 18 http www hyperbaricoxygentherapy org uk article stem cell mobilizationby hyperbaric oxygen 57 19http www thelancet com search results searchTerm HBOT fieldName AllFi elds op searchterm2 fieldname2 year volume page jrnl artypes journalFromWhichSearchStarted lancet sort date order desc collectionNa me Medline 8
CORRESPONDENCE COMMENTARY CORRESPONDENCE e mail submissions to correspondence lancet com Hyperbaric oxygenation for cerebral palsy Sir Jean Paul Collet and colleagues report Feb 24 p 582 1 on the treatment of children with cerebral palsy strongly suggests benefit from increasing the plasma oxygen tension Workers in several studies of oxygen treatment for such children have reported benefit from hyperbaric oxygenation generally 100 at 1 5 atmospheres absolute ATA but Collet and colleagues suggest that 1 3 ATA air is as beneficial except that 1 75 ATA oxygen had more rapid results in a more disabled group of children As they state the oxygen level breathing 1 3 ATA air is equivalent to about 28 by mask at 1 0 ATA If 28 can be shown to be beneficial under controlled conditions an improved quality of life might be possible for thousands of children with cerebral palsy However the earlier use of oxygen therapy in such children may be more beneficial 2 and hyperoxia might be beneficial for the fetus in utero 3 At our centre about 250 children with cerebral palsy and brain injuries aged from 6 weeks to 14 years have been treated with hyperbaric oxygenation at pressures of up to 1 5 ATA in Vickers monoplace chambers The patients have been used as their own controls A baseline image taken with single photon emission computed tomography SPECT is taken for each patient Scanning is repeated after the series of hyperbaric treatments In more than 90 of patients improvement in blood flow and metabolism has been noted on imaging accompanied by clinical improvement especially obvious to the parents 4 Physical occupational and speech therapy are continued during the treatment period and therefore the only variable was the administration of hyperbaric oxygenation As already reported 5 there is growing evidence from the use of oxygen at increased doses that in certain brain insults there are idling neurons which are receiving enough oxygen to prevent membrane failure but not enough to allow the generation of action potentials The following case study illustrates the effects seen on SPECT A boy aged 3 5 years developed a severe lefthemiparesis after a traumatic birth with damage to the blood supply to the right hemisphere The axial view of the baseline before treatment showed severe hypoperfusion in the distribution of the right midcerebral artery figure After 77 1 h treatments of hyperbaric oxygenation at 1 5 ATA the scan was repeated figure A striking increase in flow and metabolism can be seen in the right hemisphere The patient arrived in a wheelchair but by the end of the treatment course although he still had mild weakness on the left side he was able to run We suggest that SPECT should be adopted to provide objective evidence of benefit from interventions in braininjured children R A Neubauer Ocean Medical Center Lauderdale by the Sea FL 33308 USA 1 2 3 SPECT axial slice before A C and after B D hyperbaric treatment 2052 4 Collet J P Vanasse M Marois P et al Hyperbaric oxygen for children with cerebral palsy a randomised multicentre trial Lancet 2001 357 582 86 Machado JJ Reduction of spasticity clinically observed in patients with neurological diseases submitted to hyperbaric oxygen therapy especially in children with cerebral palsy transcripts from New Horizons in Hyperbaric Medicine Annual Meeting of the American College of Hyperbaric Medicine Orlando Florida 1989 101 10 Sparacia A Sparacia B Recenti acquisizioni fisiologiche sull ossigeno in iperbarismo Minerva Anestesiologica 1991 57 187 204 Neubauer RA Hyperbaric oxygenation in 5 cerebral palsy and the brain injured child Proceedings of 3rd EPNS Congress European Paediatric Neurology Society Nice November 1989 283 89 Neubauer RA Gottlieb SF Kagan RL Enhancing idling neurons Lancet 1990 335 542 Sir Hyperbaric treatment is reported by Jean Paul Collet and colleagues1 as producing striking improvements in children with cerebral palsy The improvements were seen in children breathing oxygen at 1 75 ATA or compressed air at 1 3 ATA and were still present 3 months later This result is remarkable since drug therapy was withdrawn 6 weeks before the study and physiotherapy stopped during the treatment and 3 month assessment The beneficial effects might have been reduced by the unacceptably high rate of ear barotrauma especially in the oxygen group Unfortunately a control group was not included and the investigators claim to be unsure whether the improvements were due to pressure the additional oxygen or a participation effect related to the motivation of the parents Compressed air at 1 3 ATA increases the plasma oxygen tension from 12 7 kPa 95 mm Hg to 19 7 kPa 148 mm Hg and to increase the concentration of such a reactive substrate by 50 is certainly notable I illustrate the striking effect of similar increases in air pressure with two cases A compressed air worker fainted during decompression after completing an 8 h shift at 2 5 ATA 2 but recovered quickly He gradually developed paralysis of the legs overnight but became symptomfree on recompression However symptoms returned during decompression Over the next 9 days in the pressure chamber the patient lost consciousness several times and developed limb paralysis Small increases in air pressure reversed the symptoms on each occasion A girl aged 16 years trekking in Nepal became ataxic during a descent from 3505 m altitude 3 which is 0 36 atmospheres less than sea level pressure She worsened and was THE LANCET Vol 357 June 23 2001 For personal use Only reproduce with permission from The Lancet Publishing Group
CORRESPONDENCE placed in a hyperbaric chamber After 15 min pressurised to nearly sea level she recovered completely The pressure was maintained for 2 h but 1 h after decompression she worsened to semiconsciousness She again recovered on compression and was kept in the chamber for 4 days In the compressed air worker gas bubbles initiated symptoms but relapses of neurological decompression sickness are associated with damage to the blood brain barrier In studies of the exercise tolerance of patients with chronic obstructive pulmonary disease taken from Jerusalem to the Dead Sea workers noted improvements that lasted for 2 weeks after return to the higher altitude 5 Oxygen is not a drug and because it is metabolised there is no simple dose response curve If therapy with 28 oxygen at 1 0 ATA is as effective for children with cerebral palsy as air or oxygen under hyperbaric conditions many children could benefit However these positive results suggest that both hyperbaric air and oxygen therapy can be recommended for such children since these children had major handicaps and neurological or neuropsychological status did not worsen Philip B James Wolfson Hyperbaric Medicine Unit Ninewells Hospital and Medical School Dundee DD1 9SY UK 1 2 3 4 5 Collett J P Varnasse M Marois P et al Hyperbaric oxygen for children with cerebral palsy a randomised multicentre trial Lancet 2001 357 582 86 Campbell Golding F Griffiths P Hempleman V Paton WDM Walder DN Decompression sickness during construction of the Dartford tunnel Br J Ind Med 1960 17 167 70 Austin D Gamow bag for acute mountain sickness Lancet 1998 351 1815 Hills BA James PB Microbubble damage to the blood brain barrier relevance to decompression sickness Undersea Biomed Res 1991 18 111 16 Kramer MB Springer C Berkman N et al Rehabilitation of hypoxemic patients with COPD at low altitudes at the Dead Sea the lowest place on Earth Chest 1998 113 571 75 Authors reply Sir We compared hyperbaric oxygen treatment with sham hyperbaric oxygen treatment slightly pressurised room air to improve children with cerebral palsy Our conclusion was that the global improvements in the two treatment groups might be related to the context of the intervention and the selection of motivated parents A possible effect of increased pressure THE LANCET Vol 357 June 23 2001 cannot be ruled out because of the slight increase in partial arterial pressure of oxygen nevertheless the same increase in blood oxygen can be reached by simple mask administration of 28 fractional inspiration oxygen without increased pressure which needs to be assessed before it can be recommended Therefore hyperbaric oxygen treatment is not necessary to improve cerebral palsy in children As R A Neubauer acknowledges this finding is good news because children will not have to face the risk related to hyperbaric oxygen treatment therapy1 and the family will not have to support the costs The cases presented by Neubauer do not provide scientific results but are simple anecdotal reports of changes in SPECT tomography under exposure to hyperbaric oxygen treatment This change is not surprising with hyperbaric oxygen treatment since oxygen is such a reactive substrate as P B James notes In the report of one such case 2 Neubauer says clearly that many variables must be taken into account besides grey matter metabolism We agree including the complex interaction between mind and body as an independent factor 3 We think that these observations should be used to generate hypotheses only Their presentation to the public patients or family is inappropriate for two reasons with our degree of knowledge relation of the changes in the brain image to the sole effect of increased partial arterial pressure of oxygen is impossible more importantly no causal association can be made between the changes in the brain image and the clinical improvement that is especially obvious to the parents The two cases presented by James deal with the health difficulties caused by changes in atmospheric pressure case one is an accident due to rapid decompression case two is the report of a severe case of acute mountain sickness caused by low atmospheric pressure in altitude Treatment was successful in the two patients as expected However the cases do not relate at all to the situation of children with cerebral palsy and no extrapolation can be made between the two situations The two letters illustrate the confusion that prevails in the domain of hyperbaric treatment for which scientific evidence is lacking leading clinicians to rely on anecdotal evidence Among four references presented by Neubauer only one is an article reference 3 published in a national journal two are references of meeting presentations references 1 and 4 and one is a letter reference 5 Our study is the first randomised controlled trial in this field and our results show that hyperbaric oxygen treatment is not better than sham therapy On the other hand there is evidence of many possible side effects after hyperbaric oxygen therapy 4 J P Collet M Lassonde S D Tremblay J Lacroix A Majnemer Randomised Clinical Trial Unit Jewish General Hospital SMBD Department of Epidemiology and School of Physical and Occupational Therapy McGill University 3755 C te Sainte Catherine Montreal QC H3T 1E2 Canada Paediatric Neurology Department Sainte Justine Hospital Montreal Psychology Department University of Montreal and Centre Hospitalier H tel Dieu de L vis L vis 1 2 3 4 Nuthall G Seear M Lepwsky M Wensley Skippen S Hukin J Hyperbaric oxygen therapy for cerebral palsy two complications of treatment Pediatrics 2000 106 e80 Neubauer RA Gottlieb SF Kagan RL Enhancing idling neurons Lancet 1990 335 542 Damasio AR Human emotions and the mind body problem science of mind body interaction an exploration of integrative mechanisms Washington National Institutes of Health 2001 Tibbles P Edelsberg J Hyperbaric oxygen therapy N Engl J Med 1996 334 1642 48 Sir Jean Paul Collet and colleagues1 conclude that hyperbaric oxygen does not improve the condition of children with cerebral palsy compared with those exposed to slightly pressurised air Nevertheless they wonder whether improvement is due to slightly pressurised air rather than a bias from study participation We treated eight adults with toxic encephalopathy impaired brain function secondary to exposure to pesticides solvents and other neurotoxic compounds Patients were given ten daily treatment sessions of 1 h each with 1 32 ATA and an oxygen concentration of 24 mild treatment As done by Collet and colleagues we measured attention and reaction time by use of a test of variables of attention However we added SPECT brain scanning before and after hyperbaric oxygen therapy to objectively assess results 2 4 The figure shows three dimensional displays of SPECT of the cerebral hemispheres of a representative patient before and after treatment with mild therapy Our computer program makes a regional quantitative comparison of an individual s scan 2053 For personal use Only reproduce with permission from The Lancet Publishing Group
SYNOPSIS In April 2014 a controlled longitudinal study to assess the effects of intensive rehabilitation combined with hyperbaric oxygen therapy HBOT on gross motor function in 150 children with cerebral palsy CP was published in the Undersea Hyperbaric Medical Society UHMS This is the first study that compared the effects of different hyperbaric dosages combined with rehabilitation in children with CP to a control group who received only rehabilitation In addition this study is the first empirical study recognized by the UHMS that demonstrated the efficacy for mild pressure HBOT Furthermore this study has shown that a therapeutic effect can be achieved without administering 100 oxygen for which compressed room air provided nearly identical results The eight month study commenced after assigning the children into four groups The control group consisted of children who did not undergo hyperbaric treatments and participated in intensive rehabilitation only The three other groups were assigned to hyperbaric treatment in addition to receiving intensive rehabilitation The rehabilitation program was applied for two hours per day six days a week over six months and consisted of a half hour of individual therapies including physical therapy occupational therapy speech therapy and special education All three HBOT groups received 40 one hour sessions six days a week Every child received the same intensive rehabilitation care by the same therapist team at the same center using the same protocol and the same duration of follow up The first HBOT group was treated at 1 3 atmospheres absolute ATA with compressed air 21 oxygen No supplemental oxygen was given to this group The second HBOT group was treated at 1 5 ATA with 100 oxygen delivered through a hood system Finally the third HBOT group was treated at 1 75 ATA also with 100 oxygen delivered through a hood system As expected with intensive therapies all four groups improved However the findings demonstrated that the three groups treated with different dosages of HBOT improved significantly more than the control group The HBOT groups gross and fine motor GMFM function variations were on average 3 times higher than the control For the three HBOT groups there was no significant statistical difference between the observed improvements The study found that administering mild pressure HBOT at 1 3 ATA has the potential to be equally effective when compared to higher pressures for children with CPo Furthermore the U S Agency for Healthcare Research and Quality AHRQ analyzed the results of this study and arrived at the same conclusions The AHRQ report said The possibility that pressurized room air had a beneficial effect on motor function should be considered the leading explanation In this context the increase of upwards to 50 plasma oxygenation achieved by compressed air at 1 3 ATA was of significance This study provides further credibility to the substantial effects of HBOT at mild pressure An Mukherjee M D 1 Maxime Raison PIr D 2 Tanm Sahn M D 3 Anand Arya NlPt 4 Jean LAmbert Ph D 5 Pierre Marois M D 2 Philip B James M B 6 Audrey Parent B Sc 2 Lm Ballaz PII D 2 1 SI ubJllltn Hospital Kalkaji New Delhi India 2 Centre lie Readaptation Marie Enfant Centre Hospitalier Universitaire Saintejustine Montreal Quebec Canada 3 lndraprastha Apollo Hospital New Delhi India 4 UDAAN for the Disabled Project of FSMHP C 27 Dllyallllnd Colany Lajplltnagar New Delhi India 5 Department of Social and PrHentive Medicine School of Medicine Un versite de MOlltrelll iHontrelll Quebec Canada 6 Professor Emeritus University of Dundee Nethergate Dundee Scotland
UHM2014 VOL 41 NO 2 HB02 THERAPY IN CHILDREN WITH CEREBRAL PALSY Intensive rehabilitation combined with HB02 therapy in children with cerebral palsy A controlled longitudinal study Arun Mukherjee MD 1 Maxime Raison Ph D 2 Tarun Sahni MD 3 Anand Arya MPt4 Jean Lambert Ph D 5 Pierre Marois MD 2 Philip B James M B 6 Audrey Parent B Sc 2 Laurent Ballaz Ph D 2 Shubham Hospital Kalkaji New Delhi India 2 Centre de Readaptation Marie Enfant Centre Hospitalier Universitaire Sainte Justine Montreal Quebec Canada 3 IndraprasthaApollo Hospital New Delhi India 4 UDAAN for the Disabled Project ofFSMHP C 27 Dayanand Colony Lajpatnagar New Delhi India 1 Department of Social and Preventive Medicine School of Medicine Universite de Montreal Montreal Quebec Canada 6 Professor Emeritus University of Dundee Nethergate Dundee Scotland 5 CORRESPONDING AUTHOR Laurent Ballaz Ph D laurent ballaz uqam ca ABSTRACT Objective The present study aimed to assess the Each subject effect treated one hour per day six days per week during of intensive hyperbaric rehabilitation oxygen HB02 combined with therapy on gross motor measure Methods We carried out an open observational ments platform independent after beginning cerebral palsy with follow up with over eight months to compare the effects of standard intensive rehabili tation only control group n 20 to standard tensive rehabilitation different hyperbaric in Gross motor function was evaluated and at two four six and eight showed over the course of the treatments p
UHM 2014 VOL 41 NO 2 HB02 THERAPY IN CHILDREN WITH CEREBRAL PALSY children with CP around the world 9 Using high quality SPECT imagery several studies of children with CP and of adults after a stroke have shown that HB02 therapy may regenerate or revive cells in the ischemic penumbra in the brain 7 10 11 This increased vascular activity would allow the reactivation of idling neurons 6 10 11 12 as HB02 therapy is known to increase neovascularization in wound healing The higher tissue oxygen levels provided by HB02 therapy might also favor better metabolism and function of unaffected cells 13 14 To date despite several reports of benefit the use of HB02 therapy for CP has met opposition which has even polarized the field of clinical HB02 therapy 1518 The first pilot study 19 reported the positive effects of HB02 therapy on 25 carefully selected children with the form of CP known as spastic diplegia The improvements were measured both on gross and fine motor function Based on the results of this pilot study a double blind randomized multicenter trial n 111 of HB02 therapy for children with CP was conducted by Collet et al 20 This study included only two groups of children one treated at 1 75 atmospheres absolute atm abs with 100 Oz while the other breathed air at 1 3 atm abs Some involved in the statistical analysis of the results regarded the use of compressed air at 1 3 atm abs to be an inactive placebo although this was opposed by the clinicians The controversy required the appointment of an independent adjudicator by the Lancet who agreed that such a change in pressure and increase in the level of oxygen could not be referred to as a sham treatment In fact exposure to 1 3 atm abs increases the arterial plasma oxygen concentration Pa02 by nearly 50 21 It was little recognized at the time that blood flow in the physiological range of oxygen concentrations is controlled by the interaction between nitric oxide and hemoglobin 22 Changes in oxygen levels also regulate genes involved in angiogenesis and neutrophil activity in inflammation 23 As the best dosage of oxygen for the treatment of children with CP is not known a sham control group should have been included to ensure an adequate experimental design The controversy was highlighted by an editorial comment entitled Hype or hope published in the same issue ofthe Lancet journal 24 After the courses of treatment the improvements on gross motor function were impressive and equivalent in both groups Improvements in language and neuropsychological functions were also recorded in both treatment groups There are two ways of interpreting the results either the two treatments were equally effective or the improvements were all caused by a participation effect Based on the major improvements reported the latter interpretation is inappropriate 25 but has unfortunately been promoted as evidence that hyperbaric treatment is ineffective in CP children 26 restricting further research on the subject The aim of this present study is to answer the questions raised by the study by Collet et al 20 by assessing the effect of different dosages of hyperbaric treatment combined with intensive rehabilitation on motor function in children with CPo METHODS Participants A total of 150 children with CP were selected for the study among those attending rehabilitation at the Foundation for Spastic and Mentally Handicapped PersonsUDAAN FSMHP UDAAN center in Delhi India All participants had to meet the following inclusion criteria children up to teen age of either sex with all types of CP any cognitive and motor development level Children were excluded if there were other developmental or genetic disorders uncontrolled epilepsy or asthma as well as ear nose or throat disorders Forty percent of all of our participants had minor to moderate epilepsy due to their injured brain Half of them were significant enough to be on antiepileptic medication It was the parents decision to include their children in the HBOz therapy groups Participants who were not assigned to HB02 therapy groups were assigned to the control group All participants were engaged in the same intensive rehabilitation program at FSMHP UOAAN Only the children who did not default on at least six months of standard therapies were assessed Quality magnitude and type of care were uniform across all four groups Participants characteristics are described in Table 1 The study was approved by the ethics committee of Apollo Hospital Delhi and the parents informed voluntary written consent was required after medical clearance Treatments The study covers a 10 year span of treatments during which the three different dosages of hyperbaric oxygen were used The different dosages were not implemented at the same time and the children were offered the HB02 therapy available at the time of their inclusion in the protocol which means that no selection bias occurred in the choice of dosage
UHM 2014 VOL 41 NO 2 HB02 THERAPY IN CHILDREN WITH CEREBRAL PALSY Table 1 Partlelpants characteristics Gender M F GMFM Age yrs baseline score Mean range Mean SO Groups Diagnostics Control 11 20 Athetoid CP 11 2 Hemiplegic CP 11 2 Diplegic CP 11 4 Quadriplegic CP n 12 13 7 3 5 1 to 17 29 6 13 0 1 3 atm abs 11 40 Athetoid CP 11 3 Hemiplegic CP 11 0 Diplegic CP 11 16 Quadriplegic CP 11 12 29 11 4 9 1t011 29 6 14 8 1 5 atm abs n 32 Athetoid CP 11 3 Hemiplegic CP n 1 Diplegic CP 11 15 Quadriplegic CP n 13 23 9 4 3 1 to 12 34 3 15 6 40 18 4 3 1 to 13 32 5 11 8 1 75 atm abs 11 58 Athetoid CP 11 6 Hemiplegic CP 11 2 Diplegic CP 11 19 Quadriplegic CP 11 31 atm abs atmosphere absolute CP cerebral palsy F female GMFM gross motor function measurement M male Every child received the same intensive rehabilitation care by the same therapist team at the same center using the same protocol and the same duration of follow up The rehabilitation program was applied for two hours day six days week over six months and consisted of a half hour of individual therapies of physical therapy occupational therapy speech therapy and special education For hyperbaric therapy the children were assigned to four groups A No hyperbaric treatments rehabilitation only control group n 20 B 40 sessions one hour day six days week at 1 3 atm abs air 21 O2 room air n 40 C 40 sessions one hour day six days week at 1 5 atm abs HB02 100 O2 n 32 D 40 sessions one hour day six days week at 1 75 atm abs HB02 100 O2 n 58 All hyperbaric treatments were given six days week during seven weeks In all treatment sessions the total amount of time spent in the hyperbaric chambers was 90 minutes as IS minutes for either compression and decompression was taken HB02 using 100 oxygen was delivered through a hood inside a muitiplace hyperbaric chamber at a local tertiary care hospital using pressures of 1 75 or 1 5 atm abs Hyperbaric air treatment at 1 3 atm abs using room air at 21 oxygen was carried out using a soft chamber We carried out initial and periodic assessment of lung and ENT passages and temporarily stopped hyperbaric therapy whenever there was any air passage obstruction or inflammation Children with a previous history of epilepsy were referred to a pediatric neurologist and the anti epileptic dosages were increased marginally during the hyperbaric treatments period Evaluation procedures In all children gross motor function was systematically evaluated before the treatments and at four and six months after the beginning of the treatments by the same therapists who were accustomed to undertaking the evaluations To have more data and when possible we were often able to evaluate the children at two and eight months after the beginning of treatments The gross motor function measure GMFM66 27 was applied to every child It is a criterion based observational measure 66 items that assesses motor function in five dimensions A lying and rolling B sitting C crawling and kneeling D standing and E walking running and jumping
lJHM 2014 VOL 41 NO 2 HB02 THERAPY IN CIllLDREN WITH CEREBRAL PALSY Table 2 GMFM observed mean before and aHer H802 therapy GMFM observed mean SD Before HB02 Control 29 6 13 0 1 3 atm abs 21 O2 29 6 14 8 1 5 atm abs 100 02 1 7 atm abs 100 O2 2 months after beginning HB02 4 months after beginning HB02 6 months after beginning HB02 8 months after beginning HB02 31 0 12 8 32 4 12 8 36 2 13 6 38 6 14 3 40 8 14 2 34 3 15 6 39 3 15 4 42 5 15 3 46 4 17 0 32 5 11 8 37 2 10 8 42 1 10 4 46 7 9 7 atm abs atmosphere absolute GMFM 33 4 13 1 gross motor function measurement Each item is scored on a four point scale and the test gives numeric results for each dimensions as well as a total score The score is reported as a percentage of the maximum score 100 generally obtained in a normal 5 year old child Data analysis Linear mixed models were used to analyze the GMFM data Such models permit the data to exhibit correlations and non constant variances These models therefore provide the flexibility of modeling not only the means of the data but also their variances and co variances Treatments were considered as fixed factors and month and age were considered as co variables Month was time dependent while age was time independent Random components were introduced to depict individual trajectories over months with separate intercepts and slopes A maximum likelihood approach was used to estimate the coefficients and an unstructured random effect covariance matrix was utilized Linearity for month and interactions treatment x month were tested Information criteria such as the Akaike criterion and the 21n likelihood and residual values were used to verify the quality of adjustment Pearson product moment correlation coefficient r was calculated to quantify the interrelationship among the GMFM variation and GMFM level before HB02 therapy RESULTS As expected groups were similar on the GMFM level at baseline p 0 429 and each group including the control group showed improvement in the GMFM scores over the course of the treatments p
UHM 2014 VOL 41 NO 2 HB02 TIIERAPY IN CHll DREN WITH CEREBRAL PALSY A study on patients with advanced lung disease has been undertaken in Jerusalem Variable Coefficient 8 SE 8 p value T While maintained on supplemental oxygen they were taken down to the Dead Sea where they 7 45 0 000 Constant 24 65 3 31 breathed only ambient air A statistically signifi1 3 atm abs 1 91 3 65 0 52 0 602 cant increase in walking distance was recorded 1 5 atm abs 2 91 3 73 0 78 0 437 which persisted for a month after returning to Jerusalem The increase in pressure achieved by 1 75 atm abs 1 42 0 42 3 39 0 675 descending to the Dead Sea was just 0 06 atm abs Month 0 46 0 18 2 52 0 013 30 Compressed air at a pressure 0 3 atm abs over ambient cannot be considered a placebo LnAge 4 96 1 66 2 99 0 003 and a recent paper discussed the osmotic effects 1 3 atm abs month 0 90 0 22 4 14 0 000 of a sudden increase in pressure 31 In addition 1 5 atm abs month 0 94 0 23 4 16 0 000 most of the children included in our series were barely in a position to have the mental maturity 1 75 atm abs month 1 04 0 210 4 95 0 000 to understand what was being done for them atm abs atmospheres absolute GMF gross motor function measurement The results of the present study strongly support the fact that HB02 therapy even in Table 4 Predicted GMFM from fixed effects models small dosage can improve motor function and in each group increase the effects of standard rehabilitation The amount and quality of changes observed in our study Group Model are also in accordance with the results obtained in Control group GMFM 24 65 0 46 Month 4 96 LnAge other studies on HB02 therapy in CP 10 19 20 1 3 atm abs group GMFM 22 75 1 36 Month 4 96 LnAge The authors are aware that Lacey et al 32 have recently conducted a randomized control study in 1 5 atm abs group GMFM 27 56 1 40 Month 4 96 LnAge which they compared two different hyperbaric treat1 75 atm abs group GMFM 26 07 1 50 Month 4 96 LnAge ments one of which 14 O2 at 1 5 atm abs has atm abs atmospheres absolute GMFM gross motor function never been used on CP children before and was conmeasurement sidered by these authors as a control group These authors present their study as a definitive answer to Table 3 Fixed effects estimation for GMFM clinically important The improvement seen in all other outcomes is also striking Moreover the U S Agency for Healthcare Research and Quality AHRQ analyzed the results of the study and arrived at the same conclusions 25 The AHRQ report mentioned that The possibility that pressurized room air had a beneficial effect on motor function should be considered the leading explanation However our study has like that of Collet et at 20 clearly demonstrated the benefit of treatment with compressed air at 1 3 atm abs because we included a control group thus the effect of hyperbaric conditions cannot be attributed to a participation or placebo effect In fact the placebo effect is a temporary phenomenon that lasts for a few weeks 29 and not for the eight months we have found benefit in our follow up Human physiology works within a narrow band for optimal activity In this context the increase of almost 50 in plasma oxygenation achieved by compressed air at 1 3 atm abs was of significance hyperbaric therapy inefficacy in children with CP even if major concerns can be addressed and explain the discrepancy with the present study First despite the fact that in the control group the condition simulated 21 oxygen at room air this treatment must not be considered as a placebo treatment because no one knows exactly the potential physiologic effects ofthis hyperbaric treatment Secondly the change in GMFM in the HB02 group was 1 5 in two months which is more than most changes measured with recognized treatments in CP 9 Thirdly Lacey et al included only 20 participants per group and stopped the study prematurely which avoided possibility of the results reaching a threshold for significance These concerns have been addressed in a letter to the Annals of Neurology 33 The Gross Motor Function Classification Scale GMFCS classifies CP disabilities into five levels based on the GMFM measurement at a given age The natural gross motor progression of children with CP usually
WM 2014 VOL 41 NO 2 HB02 THERAPY IN CHILDREN WITH CEREBRAL PALSY Figure 1 Rate of gross motor function measurement improvement GMFM improvement per month 1 8 1 6 1 4 1 2 1 0 0 8 0 6 0 4 0 2 0 0 Control 1 3 atm abs 21 02 1 5 atm abs 100 02 1 7 atm abs 100 02 significantly different from the control group p
I UHM 2014 VOL 41 NO 2 HB02 THERAPY IN CHILDREN WITH CEREBRAL PALSY follows a curve similar to a logarithmic curve 27 The children with the highest level of abilities are classified in Level I while Level 5 regroups the children with the most severe form of motor disability Figure 2 The progression of children with CP should naturally follow the curves corresponding to their level of disabilities 27 Figure 2 shows that the mean initial GMFM values of the four groups would classify them between Level 4 and Level 5 of the GMFCS By end of six months of therapy all three hyperbaric groups had improved to Level 4 whereas the control group did not change its disability level There are risks associated with the high oxygen pressures used in diving but they are not relevant to the much lower pressures used in this study The rate of change of pressure was slow as the pressurization took 15 minutes and only three children were excluded because of ear pain on compression None of the participants needed ear canal grommet use There were no other side effects Our study shows that HB02 therapy when combined with rehabilitation has many more positive effects than rehabilitation alone As seen on SPECT imaging hyperbaric treatment appears to reactivate certain damaged areas of the brain It is however obvious that the recovering brain must be trained to work to its full potential to gain the best results This highlights the importance of rehabilitation after or during HB02 therapy Further research is needed to explore the cerebral plasticity processes that follow hyperbaric treatment Improvement in function comfort and the independence of children with disabling neurological conditions could lead to better health and quality of life as well as important cost savings in the long term Secondly the evaluations were not blinded We certainly recognize that it was not ideal but it was difficult for us in a longitudinal study conducted in a relatively small center and involving human interaction and evaluation by the same therapists for blinded evaluations to have been undertaken CONCLUSION A longitudinal study in children with cerebral palsy has been conducted The study compared three different dosages of hyperbaric oxygen combined with intensive rehabilitation with a control group receiving only rehabilitation The rate of improvement in GMFM score was significantly superior in the three hyperbaric groups compared to the control group There was no difference between the three HB02 therapy groups The amount of changes are similar to the results obtained in the multiple studies on HB02 therapy in CP that have been published and are more important than the improvements measured with standard recognized therapies alone in CP The very important difference observed in treated vs controlled children can only be a genuine beneficial effect of HB02 therapy Based on the results of this and other studies of HB02 therapy in CP children HB02 combined with rehabilitation should be recommended for children with CPo Acknowledgments We acknowledge with thanks the significant role played by the Ministry of Social Justice and Empowerment Govt of India Mrs Kamala Biswas Mrs Nenu Mathur Mr B R Arora the Trustees and many other sponsors corporate donors and well wishers without whose regular inflow of grants and donations to the FSMHP UDAAN non profit charitable organization this long term ongoing study could not have been LIMITATIONS There were several limitations inherent to this study First participant repartition between groups was not randomized It was the parents decision to include their children in HB02 therapy groups and participants who were not assigned to HB02 groups were automatically assigned to the control group The different dosages of HB02 were not implemented at the same time over a lO year period which means that no selection bias occurred in the treatment or dosage choice possible We also thank Dr Paul Harch President of the Inter national Hyperbaric Association United States and Mr Tom Foxfor their constant encouragement and guidance which was invaluable for our study In conclusion we must thank the many dedicated and good therapists whose high quality of one to one rehabilitation made this trial a success and who worked hard to set a standardfor other institutions tofollow The authors report that no conflict of interest exists with this submission
UHM 2014 VOL 41 NO 2 HB02 THERAPY IN CHILDREN WITH CEREBRAL PALSY I REFERENCES 14 Harch PG Kriedt CL Weisend MP Van Meter KW 1 Arpino C Vescio MF De Luca A and Curatolo P Efficacy of intensive versus non intensive physiotherapy children with cerebral palsy a meta analysis 2010 33 165 71 2 Cowan F Rutherford M Groenendaal in Int J Rehab Res cognitive and motor function in a rat traumatic brain injury F et al Origin and timing of brain lesions in term infants with neonatal encephalopathy Lancet 2003 361 736 742 comparison CI Kim DG brain SPECT in cerebral palsy with MRI J Nucl Med 1998 39 619 23 4 Legido A Price ML Wolfson B etal Technetium 99mTc HMPAO model Undersea Hyperb Med 2001 28 28 9 15 Muller Bolla M Collet JP Ducruet T Robinson A Side effects of hyperbaric oxygen therapy in children with 3 Lee JD Kim DI Ryu YR Whang GJ Park Technetium 99m ECD Sutherland RJ Low pressure hyperbaric oxygen therapy LPHBOT induces cerebrovascular changes and improves SPECT in children and adolescents with cerebral palsy Undersea Hyperb Med 2006 33 237 44 16 Essex C Hyperbaric oxygen and cerebral palsy no proven benefit and potentially harmfull Dev Med Child Neurol 2003 45 213 5 17 Marois P Vanasse M Letters to the Editor Hyperbaric neurologic disorders J Child Neurol 1993 8 227 234 oxygen therapy and cerebral palsy Dev Med Child Neurol 5 Astrup J Siesjo BK Symon L Thresholds in cerebral ischemia the ischemic penumbra Stroke 1981 12 723 725 2003 45 646 8 6 Neubauer RA Gottlieb SF and Kagan RL Enhancing Undersea Hyperb Med 2007 34 1 6 idling neurons Lancet 1990 335 542 7 Efrati S Fishlev G Bechor Y et al Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PloS one 2013 8 e53716 8 Siddique MS Fernandes HM Wooldridge TD Fenwick JD Slomka P and Mendelow AD Reversible ischemia around intracerebral hemorrhage emission computerized tomography a single photon study J Neurosurg 2002 19 Montgomery D Goldberg J Amar M et al Effects of hyperbaric oxygen therapy on children with spastic diplegic cerebral palsy a pilot project Undersea Hyperb Med 1999 26 235 242 20 Collet J P Vanasse M Marois P et al Hyperbaric oxygen for children with cerebral palsy a randomised multicentre trial Lancet 2001 357 582 6 21 James PB Hyperbaric oxygenation for cerebral palsy 96 736 41 9 Senechal C Larivee S Richard E Marois P Hyperbaric oxygenation 18 Gottlieb SF Neubauer RA Marois P Vanasse M Letters to the Editor HB02 and cerebral palsy in children therapy in the treatment of cerebral palsy A review and comparison to currently accepted therapies Journal of American Physicians and Surgeons 2007 12 109 10 Golden Z Neubauer R Golden C Greene L Marsh J Mleko A Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy Int J Neurosci 2002 112 119 31 Lancet 2001 357 2052 2053 22 Stamler JS Jia L Eu JP et al Blood flow regulation by S nitrosohemoglobin in the physiological oxygen gradient Science 1997 276 2034 2037 23 Cramer T Yamanishi Y Clausen BE et al HIF la is essential for myeloid cell mediated inflammation 24 Talking points Hyperbaric oxygen Hype or hope 11 Harch PG Van Meter KW Gottlieb SF Staab P The effect of HEOT tailing treatment on neurological residual Lancet 2001 357 567 25 AHRQ Systems to rate the strength of scientific and SPECT brain images in type II cerebral DCI CAGE evidence Evidence Report Technology Assessment Undersea Hyperb Med 1994 21 22 3 Rockville Md AHRQ 2003 12 Neubauer V Neubauer RA Harch PG HBO in the management of cerebral palsy Textbook of Hyperbaric Medicine Seattle Hogrefe Huber 2004 13 Harch PG Kriedt CL Wei send MP Van Meter KW Sutherland RJ Low pressure hyperbaric oxygen therapy induces cerebrovascular Cell 2003 112 645 657 changes and improves cognitive no 47 26 Bell E Wallace T Chouinard I Shevell M Racine E Responding to requests of families for unproven interventions in neurodevelopmental disorders hyperbaric oxygen treat ment and stem cell therapy in cerebral palsy Dev Disabil Res Rev 2011 17 19 26 27 Palisano R Rosenbaum P Walter S Russell D Wood E and motor function in a rat traumatic brain injury model Galuppi B Development Undersea Hyperb Med 1996 23 48 gross motor function in children with cerebral palsy Dev Med and reliability of a system to classify Child Neurol 1997 39 214 223
UHM 2014 VOL 41 NO 2 HB02 TIIERAPYIN 28 Mychaskiw G 2nd How many deaths will it take till they know Monkeys madmen and the standard of evidence Undersea Hyperb Med 2012 39 795 797 29 Hyland ME Using the placebo response in clinical practice Clin Med 2003 3 347 50 30 Kramer MR Springer C Berkman N et al Rehabilitation of hypoxemic patients with COPD at low altitude at the dead sea the lowest place on earth Chest 1998 113 571 575 CHILDREN WITH CEREBRAL PALSY 31 Babchin A Levich E Melamed Y Shivashinsky G Osmotic phenomena in application of hyperbaric treatment Biointerfaces 2011 83 128 132 32 Lacey DJ Stolfi A and Pilati LE Effects of hyperbaric oxygen on motor function in children with cerebral palsy Ann Neurol 2012 72 695 703 33 Marois P Hyperbaric oxygen treatment Ann Neurol 2013 Jul 74 1 149 I LOVE DOING THESE tREATMENTS RJ Mitte from the hit TV show Breaking Bad U
D J D Perrins P B James Neubauer et al 3 reported that one or more lesions disappeared in 11 of 35 patients 31 4 after 1 hour of HBO2 T hyperbaric oxygen treatment Short term controlled trials have shown that a course of HBO2T benefits many multiple sclerosis patients Fischer et al 4 in New York University performed the first randomised placebo controlled double blind trial Improvement in balance and bladder function were found in 12 of 17 patients P 0 0001 Those patients with a less severe form of the disease had a more favourable and long lasting response After a year with no further treatment the treated group showed a positive change P 0 0008 Barnes et al 5 found overall benefit in their treated group P 0 03 and a year later there was less deterioration in cerebellar function P 0 03 They called for further studies Two other controlled studies have reported sustained benefit with follow on treatment Oriani et al 6 used patients with a low Kurtzke disability score 7 and compared 22 controls with 22 patients treated each week for a year They detected an appreciable difference in outcome P 0 01 Pallotta et al 8 followed 22 patients for 8 years All received an initial course of 20 treatments and 11 were treated thereafter with 2 sessions every 20 days Figure 2 The frequency of relapses decreased dramatically in 35 Initial course of 20 sessions 30 11 Control patients 25 Involvement by physicians has been restricted to data collection and advice The records provide a unique opportunity to evaluate the effectiveness of long lasting courses of HBO2T Seven hundred and three patients were followed up for 10 14 years since first receiving a course of treatment They breathed oxygen from an oronasal mask in a chamber filled with air In an initial course five daily treatments of one hour were given at 1 5 atm abs If two or more symptoms improved a course of twenty treatments was completed at this pressure Otherwise the pressure was raised in weekly increments of 0 25 atm abs until a response was obtained or five treatments at 2 0 atm abs had no effect Thereafter the patients were invited to return for a follow on treatment on a weekly basis or failing that as often as they felt the need or found it possible The bladder improvements observed in other studies were confirmed Table 1 Table 1 Urinary Frequency of 523 Patients Before and After the Initial Course Frequency Before Initial course After Initial course _ x Improvement _ x Night time 1232 2 4 651 1 2 47 Daytime 3873 7 4 2960 5 7 24 No follow on Total 20 number of relapses each year 15 10 11 Treated patients x 2 monthly 10 every six months 5 0 1977 1978 1979 1980 1981 1982 1983 1984 1985 YEAR Fig 2 Incidence of relapses in 22 patients with and without regular HBO2T followed for 8 years by Pallotta et al 8 the prolonged treatment group Methods Since 1982 over 15 000 MS patients have received treatment by the MS National Therapy Centres run by a UK Charity They use single lock multiplace chambers and are distributed throughout the UK and Ireland Figure 3 Shetland Assessments were made between two and four years and again between six and eight years after the initial course A third survey was conducted between ten and fourteen years By now 126 had died 8 were over 60 years old when first treated 99 had become lost to follow up 29 had suffered injuries that affected their KDS value and 2 had had their original diagnosis revised 447 therefore remained for analysis Results The records provide a unique opportunity to evaluate the effectiveness of long lasting courses of HB02T for MS Thirty eight of the patients who had received less than 10 follow on treatments had deteriorated by a mean 0f 2 0 on the KDS Twenty five patients receiving more than 400 treatments had only deteriorated by 1 0 point An analysis reveals that about 300 treatments in 10 years about once a fortnight are required to delay progression of Relapsing Remitting patients while more than 500 treatments say once a week are more effective After 10 years 23 of the 447 patients remaining eligible for study had not deteriorated and 7 had improved As might be expected those with a low Kurtzke score do well Figure 4 Long term controlled studies are impractical in a multicentre setting as patients do not comply with the protocol However it is possible to compare groups of patients who have received different treatment regimes Figure 5 Fig 3 The location of the MS National Therapy Centres Jersey 46
Long term hyperbaric oxygenation retards progression of multiple sclerosis 2 2 5 Relapsing Remitting n 26 4 Improved 4 At least 6 treatments in every quarter 1 5 n 22 n 13 2 0 4 7 16 5 Mean 1 5 increase in Kurtzke 1 value Mean change in Kurtzke value in 10 14 years n 20 n 15 7 1 24 8 n 13 8 2 18 100 treatments 9 3 5 Paired t 3 14 14 0 5 4 n 11 p 0 01 n 22 Deteriorated 0 5 20 100 101 200 201 300 301 400 401 500 2 501 600 3 4 4 5 5 5 5 6 6 5 7 Initial Kurtzke value Number of treatments in 10 14 years Fig 4 The increase in Kurtzke value in patients with Relapsing Remitting MS related to the number of treatments over 10 14 years Fig 5 Patients who received at least 6 treatments in every quarter compared with those receiving less than 100 in 10 14 years A search of the records has revealed 1384 patients who were first treated 17 or more years previously and 104 11 are still attending for regular treatment Table 2 gives the details of 117 patients who have attended regularly without interruption for 5 to 17 years Between 5 and 15 years the Kurtzke value of Relapsing Remitting patients has not increased by more than one point years 38 of the final group of 447 patients were still attending regularly The cost of each treatment in this charity setting is about 10 so that the benefit may be obtained for less than 300 US 450 a year The earlier treatment is started in the disease the better Many patients continue to attend as their symptoms particularly frequency of micturition are only controlled by regular attendance Some arrange their holidays so as to be near a Centre Others having difficulty reaching a Centre become so dependent on regular treatment that they install simple monoplace chambers in their own homes The social and economic advantages to be gained from such a regime are obvious The Therapy Centres have now been providing hyperbaric treatment for twenty two years without a serious incident This has established that low pressure facilities can play an important part in the care of MS patients The treatment has been shown to be practicable cost effective and very safe After 10 or more Table 2 Details of 117 patients who have attended regularly for 5 17 years No of patients MS Type Average difference in Kurtzke value 13 Relapsing Remitting 0 6 19 Chronic Progressive 1 2 Chronic Static 0 75 17 Relapsing Remitting 1 24 Chronic Progressive 0 8 8 Chronic Static 0 5 12 16 Relapsing Remitting Chronic Progressive 0 1 6 Chronic Static 2 Attended For Average no of treatments 5 10 years 323 351 248 464 10 15 years 523 488 14 years 466 494 664 117 References 1 Compston DAS The dissemination of multiple sclerosis The Langdon Brown lecture 1989 J Royal Coll Phys 1990 243 207 181 2 Miller DH et al Proton magnetic resonance spectroscopy of an acute and chronic lesion in multiple sclerosis Lancet 1991 337 58 59 3 Neubauer RA Gottlieb SF Kagan RL Magnetic resonance imaging in multiple sclerosis following hyperbaric oxygen First Swiss Symposium on Hyperbaric Medicine Basel Foundation for Hyperbaric Medicine 1986 4 Fischer BH Marks M Reich T Hyperbaric oxygen treatment of multiple sclerosis a randomised placebo controlled double blind study N Engl J Med 1983 308 181 6 5 Barnes MP Bates D Cartlidge NEF et al Hyperbaric oxygen and multiple sclerosis short term results of a placebo controlled double blind trial Lancet 1985 ii 297 3006 6 Oriani G Barbieri S Cislaghi G Albonico G et al Hyperbaric oxygen in multiple sclerosis a placebo controlled double blind randomised study with evoked potential studies J Hyp Med 1990 5 237 45 47
D J D Perrins P B James 7 Kurtzke JF On the evaluation of disability in multiple sclerosis Neurology 1961 11 686 94 8 Pallotta R Anceschi S Costilgliola N et al Prospecttive di terapia iperbarica nella sclerosi a placce Ann Med Nav 1980 85 57 62 that is highly relevant for our understanding of the disease in several aspects The conclusions are sound and the results of this investigation will be very helpful for the better treatment and effective patient care in the field Reviewer 1 The paper by Perrins and James evaluate the effect of prolonged courses of hyperbaric oxygen treatment HBO2T on the progressive deterioration of multiple sclerosis MS in relatively large number of patients The study is well designed and addresses an important and clinically very relevant issue not well addressed before The study is well conducted and designed to cover long term follow up and outcome Anonymous 48 Reviewer 2 The study is well designed and addresses very important issue The findings could be of general interest and provide new insight in patient care The authors should be commended on their achievement Anonymous
MINI REVIEW published 23 September 2021 doi 10 3389 fragi 2021 678543 Integrative Role of Hyperbaric Oxygen Therapy on Healthspan Age Related Vascular Cognitive Impairment and Dementia Priya Balasubramanian 1 Jordan Delfavero 1 Adam Nyul Toth 1 2 Amber Tarantini 1 Rafal Gulej 1 and Stefano Tarantini 1 3 4 1 Vascular Cognitive Impairment and Neurodegeneration Program Department of Biochemistry and Molecular Biology University of Oklahoma Health Sciences Center Oklahoma City OK United States 2International Training Program in Geroscience Institute of Biophysics Biological Research Centre E tv s Lor nd Research Network ELKH Szeged Hungary 3International Training Program in Geroscience Doctoral School of Basic and Translational Medicine Department of Public Health Semmelweis University Budapest Hungary 4Department of Health Promotion Sciences College of Public Health University of Oklahoma Health Sciences Center Oklahoma City OK United States Edited by Morten Scheibye Knudsen University of Copenhagen Denmark Reviewed by Shahaf Peleg Leibniz Institute for Farm Animal Biology FBN Germany Eszter Farkas University of Szeged Hungary Correspondence Stefano Tarantini stefano tarantini ouhsc edu Specialty section This article was submitted to Interventions in Aging a section of the journal Frontiers in Aging Received 09 March 2021 Accepted 09 September 2021 Published 23 September 2021 Citation Balasubramanian P Delfavero J Nyul Toth A Tarantini A Gulej R and Tarantini S 2021 Integrative Role of Hyperbaric Oxygen Therapy on Healthspan Age Related Vascular Cognitive Impairment and Dementia Front Aging 2 678543 doi 10 3389 fragi 2021 678543 Frontiers in Aging www frontiersin org Growing life expectancy will contribute to the on going shift towards a world population increasingly comprised of elderly individuals This demographic shift is associated with a rising prevalence of age related diseases among all age related pathologies it has become crucial to understand the age associated cognitive changes that remain a major risk factor for the development of vascular cognitive impairment and dementia VCID Furthermore age related Alzheimer s disease and other neurogenerative diseases with vascular etiology are the most prominent contributing factors for the loss of cognitive function observed in aging Hyperbaric Oxygen Therapy HBOT achieves physiologic effects by increasing oxygen tension PO2 raising oxygen tissue levels decreasing intracranial pressure and relieving cerebral edema Many of the bene cial effects of HBOT exert their protective effects at the level of the microcirculation Furthermore the microcirculation s exquisite pervasive presence across every tissue in the body renders it uniquely able to in uence the local environment of most tissues and organs including the brain As such treatments aimed at restoring aging induced functional and structural alterations of the cerebral microcirculation may potentially contribute to the amelioration of a range of age related pathologies including vascular cognitive impairment Alzheimer s disease and vascular dementias Despite the presented evidence the ef cacy and safety of HBOT for the treatment of age related vascular cognitive impairment and dementia remains understudied The present review aims to examine the existing evidence indicative of a potential therapeutic role for HBOT induced hyperoxia against age related cerebromicrovascular pathologies contributing to cognitive impairment dementia and decreased healthspan in the elderly Keywords aging neurovascular coupling neurodegeneration geroscience aging dementia cognitive function 1 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention INTRODUCTION HBOT range between 2 and 3 atmospheres absolute ATA for 60 120 min which is 2 3 times what is normally experienced at sea level Kranke et al 2015 HBOT as an adjuvant treatment has been widely researched in models of cerebrovascular injury such as stroke and has shown great promise for improving the recovery time and reducing the disability rate Zhai et al 2016 Because both ischemic and hemorrhagic strokes result in regional hypoxia which imposes a major pathological stress in the brain HBOT achieves physiologic effects by increasing oxygen tension PO2 raising oxygen tissue levels decreasing intracranial pressure and relieving cerebral edema Sukoff and Ragatz 1982 Many of the bene cial effects of HBOT exert their protective effects at the level of the microcirculation Furthermore the microcirculation s exquisite pervasive presence across every tissue in the body renders it uniquely able to in uence the local environment of most tissues and organs including the brain As such treatments aimed at restoring aging induced functional and structural alterations of the cerebral microcirculation may potentially contribute to the amelioration of a range of age related pathologies including vascular cognitive impairment Alzheimer s disease and vascular dementias Despite the presented evidence the ef cacy and safety of HBOT for the treatment of age related vascular cognitive impairment and dementia remains understudied The present review aims to examine the existing evidence indicative of a potential therapeutic role for HBOT induced hyperoxia against age related cerebromicrovascular pathologies contributing to cognitive impairment dementia and decreased healthspan The number of individuals over the age of 65 is expected to increase by more than 50 percent before 2050 In the United States alone the existing population of 40 million elderlies will grow to nearly 90 million within the next 30 years Harada et al 2013 Growing life expectancy will contribute to the on going shift towards a world population increasingly comprised of elderly individuals This demographic shift is associated with a rising prevalence of age related diseases Jaul and Barron 2017 Yabluchanskiy et al 2018 Among all age related pathologies it has become crucial to understand the age associated cognitive changes that remain a major risk factor for the development of vascular cognitive impairment and dementia VCID Furthermore age related Alzheimer s disease and other neurodegenerative diseases with vascular etiology are the most prominent contributing factors for the loss of cognitive function observed in aging Schneider et al 2007 Felsky et al 2019 and at the same time play a crucial role in the quality of life of older adults and impose a signi cant nancial burden on our society Dallmeyer et al 2017 The brain receives between 15 and 20 of the cardiac output under resting conditions To carry out its critical functions and maintain cognitive abilities the brain requires a constant supply of oxygen and nutrients as well as adequate cerebral blood ow CBF for the washout of metabolic by products generated by actively ring neurons and glia populations Cerebral metabolism is highly active and requires 20 of the body s available oxygen while the brain represents only 2 of an individual s total mass Without enough oxygen or with low blood oxygen levels the onset of hypoxia and hypoglycemia pose a signi cant threat to brain function resulting in cellular injury and neurodegeneration Falkowska et al 2015 In humans as well as in all mammals the oxygen storage capacity in the central nervous system is limited and even momentary interruptions in the oxygen supply rapidly impair neuronal function Angelova et al 2015 To prevent ischemic damage stimulus evoked changes in neural activity are closely coupled to metabolism cerebral blood oxygenation and dynamic modulation of CBF under normal physiological conditions This feed forward mechanism termed neurovascular coupling NVC matches CBF which supplies the brain with oxygen and nutrients to the metabolic needs of activated neurons Iadecola 2004 Park et al 2007 Tarantini et al 2017a Ungvari et al 2017a Tarantini et al 2017b Clinical and experimental studies have revealed an age related functional impairment of the neurovascular unit which likely contributes to neurovascular dysfunction and cognitive decline in aging and in age related neurodegenerative diseases Tarantini et al 2017c Hyperbaric oxygen therapy HBOT has been utilized in the treatment of a multitude of medical conditions since its rst documentation in 1662 Aero chalinos 1664 and then widely used during the 19th century to treat for decompression sickness Al Waili et al 2005 This noninvasive highly translatable therapy is delivered by a procedure in which 100 pure oxygen is administered at greater than atmospheric pressure The typical pressures used to administer Frontiers in Aging www frontiersin org MECHANISMS OF HBOT IN THE VASCULATURE IMPLICATIONS FOR HEALTHSPAN AND COGNITIVE FUNCTION Vascular Mechanisms Treatments and therapies that aim to improve vascular and cerebrovascular health have been associated with increased health span period of healthy living in aging Brown et al 2007 Drummond et al 2011 Seals et al 2016 Administration of 100 percent oxygen to a patient in a pressurized environment results in hemoglobin saturation Unbound extra oxygen can dissolve in the plasma producing hyperoxygenated blood Goyal et al 2019 so that the dissolved fraction becomes the main source of O2 available to cells Demchenko et al 2005 Hyperoxygenation together with higher atmospheric pressure have been observed to exert multiple effects on the brain and its cerebrovasculature Figure 1 ranging from restoration of blood brain barrier BBB permeability Li et al 2018a improved angiogenesis Johnson and Wilgus 2014 edema reduction Sukoff and Ragatz 1982 Yagishita et al 2017 to the modulation of perceived painful stimuli Sutherland et al 2016 Cerebromicrovascular mechanisms are also extensively studied in the context of age related vascular dementias It is well recognized that age related microvascular rarefaction Tucsek et al 2014 increased BBB permeability Li et al 2018a endothelial dysfunction Herrera et al 2010 Ungvari et al 2 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention FIGURE 1 Summary representation of the cerebrovascular effects of hyperbaric oxygen treatment A Representation of a branching cerebral arteriole In young healthy individuals inhaled 21 O2 is suf cient to ensure adequate brain oxygenation B Age related cerebromicrovascular disease is associated with increased BBB permeability neuroin ammation declining endothelial function mitochondrial dysfunction oxidative stress loss of Nrf2 activity increase in senescent cell burden and NAD depletion C Administration of 100 percent oxygen in a pressurized environment results in hemoglobin saturation and hyperoxygenated plasma Hyperoxygenation exerts multiple bene cial effects that ameliorate and reverse brain microvascular pathologies D HBOT targets many of the age related impairments in vascular mechanisms that drive regulation of blood ow and cognition 2018a in ammation Csiszar et al 2014 Ungvari et al 2018b Fulop et al 2018 and impairment of neurovascular coupling responses Tarantini et al 2017c are among critical factors in the development of cerebromicrovascular pathologies associated with neurodegeneration and loss of cognitive function which are responsible for loss of quality of life and diminished healthspan in aging Over the past decades a growing number of studies have implicated HBOT for the treatment of vascular dementias through the following possible mechanisms increased oxygen supply and tissue oxygen partial pressure pO2 relieving cerebral edema Sukoff and Ragatz 1982 decreasing intracranial pressure promoting tissue healing and angiogenesis Johnson and Wilgus 2014 improved metabolism reduced apoptosis alleviating oxidative stress increased mitochondrial function and promoting cell differentiation and regeneration Robertson and Hart 1999 Feldmeier 2003 Wang et al 2016 Figure 1 During inhalation of normobaric air arterial pO2 is approximately 100 and 55 mmHg in the tissues However when breathing 100 percent oxygen at 3 ATA arterial pO2 can increase to about 2 000 mmHg and to 500 mmHg in the tissues Tibbles and Edelsberg 1996 By exceeding the oxygen carrying capacity of hemoglobin the oxygen in solution saturates the blood plasma and can better oxygenate areas where red blood cells cannot reach or where hemoglobin oxygen carriage is impaired Figure 1C such as in microvascular injury or carbon monoxide poisoning Leach et al 1998 Phillips 2000 Frontiers in Aging www frontiersin org HBOT not only provides increased access of oxygen to damaged tissue via plasma saturation but also encourages new blood vessel formation by activation transcription factors such as VEGF Goyal et al 2019 Although the mechanisms are not fully understood HBOT is a well established treatment for decompression sickness This condition affects individuals that experience trauma surgery or deep sea diving resulting in the formation of air embolisms Additional therapeutic targets that deserve more investigation include cognition As such recent studies have aimed to investigate the cellular and molecular mechanisms underlying HBOT to better understand its potential clinical role in age related cognitive impairment HBOT is particularly effective in wound healing it works by amplifying the oxygen diffusion gradients along ischemic wounds promoting extracellular matrix synthesis required for angiogenesis Knighton et al 1981 Hunt 1988 Microvascular Mechanisms In the cerebral microvasculature age related pathological changes include loss of vascular density Tucsek et al 2014 and decreased angiogenesis Lin et al 2018 increased incidence of ischemic and hemorrhagic microvascular injury Ungvari et al 2017b and neuroin ammation which is associated with loss of cognitive function The physiological basis and documented effects of HBOT as it was studied on peripheral vasculature and tissues could be applied to the cerebral microvasculature to study the potential therapeutic effects of hyperoxia against agerelated vascular cognitive impairment In healthy vasculature 3 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention loss of hippocampal neurons following lateral uid percussion injury Other prominent features of aging are pro in ammatory phenotypic alterations of cerebral vessels mediated by the decreased activity of Nrf2 NF E2 related factor 2 a key redox sensitive transcription factor which is a key modulator for the expression of antioxidant and detoxicant enzymes as well as factors involved in repair of oxidative macromolecular damages and other cell survival pathways Several recent studies have shown that Nrf2 activity exerts multifaceted antiaging vasoprotective effects against the pathogenesis of agerelated vascular cognitive impairment Ungvari et al 2010 Ungvari et al 2011a Valcarcel Ares et al 2012 Tarantini et al 2018a Recent studies administering HBOT in isolated human microvascular endothelial cells Godman et al 2010 and diabetic mice Verma et al 2015 have identi ed HBOT as a Nrf2 activator and mediated oxidative stress response as one of the primary responders to HBOT HBOT has also been widely used as a treatment adjunct for vascular disease and in addition to increasing oxygen delivery to the marginally perfused ischemic hypoxic tissues HBOT has also been shown to promote angiogenesis and improve cellular metabolism that has been impaired by hypoxia while signi cantly reducing post ischemic edema an effect that persists after treatment Goyal et al 2019 Dietary habits leading to metabolic stress and aging have been linked to a decline in microvascular density both in the brain of mouse models of aging Balasubramanian et al 2020 In a recent study the measured hippocampal microvascular rarefaction and the loss of hippocampal dependent cognitive function positively correlated Tucsek et al 2014 Endothelial cells lining the brain microvasculature have been found to be particularly sensitive to these stressors Ungvari et al 2011b and could be implicated in the age dependent loss of neurovascular coupling responses Tarantini et al 2017c Tarantini et al 2018b Tarantini et al 2019a Levit et al 2020 and brain microvascular rarefaction Tucsek et al 2014 Additionally HBOT induced angiogenesis and broplasia has been shown to promote healing to radiated tissue This is especially useful because radiated tissue does not spontaneously revascularize due to their unique wounding pattern Goyal et al 2019 Aged mice exhibit vascular endothelial growth factor VEGF signaling insuf ciency Grunewald et al 2021 At the molecular level increase in VEGF production mediates the effects of HBOT on angiogenesis Several mechanisms have been put forth to explain how HBOT induces VEGF signaling to promote angiogenesis The rst mechanism involves increase in VEGF at the transcriptional level which is mediated by HBOT induced binding of the transcription factor AP 1 to VEGF promoter In vitro studies in human umbilical endothelial cells show that stress activated protein kinase c June N terminal kinase SAPK JNK pathway and the extracellular signal regulated kinase ERK pathway are involved in HBOT mediated increase in VEGF transcription through AP 1 Lee et al 2006 The second mechanism involves HIF 1 mediated VEGF induction The intermittent normoxic periods between the HBOT session is sensed as hypoxia and results in increase in HIF1 which hyperoxia has been found to rapidly elicit robust vasoconstriction S V 1990 however Zamboni demonstrated that the increased oxygen carriage of hyperoxygenated plasma compensated well for the reduced ow of red blood cells Additionally microvascular blood ow in ischemic tissue is in fact improved with HBOT Zamboni et al 1993 Further studies showed hyperoxia had bene cial microcirculatory and metabolic effects by limiting the loss of ATP production and decreased accumulation of lactate in ischemic tissue Cianci et al 2013 Other researchers have been interested in the consequences of HBOT on CBF studies using laser doppler owmetry Chavko et al 1998 suggested no systematic changes Zhang et al 1995 or small improvements in CBF Thom et al 2002 in response to HBOT induced nNOS activation However Sato measured the production of cortical NO during HBOT in rats and found that NO production was improved proportionally to the CBF increase Sato et al 2001 Cellular Mechanisms The coenzyme NAD plays a critical role in cellular bioenergetics and adaptive stress responses Its depletion has emerged as a fundamental feature of aging Imai and Guarente 2014 Kane and Sinclair 2018 causing defects in nuclear and mitochondrial functions and resulting in many age associated pathologies Verdin 2015 including vascular dementia Fricker et al 2018 Alzheimer s disease Gong et al 2013 Hou et al 2018 and vascular cognitive impairment Tarantini et al 2019a Tarantini et al 2019b Kiss et al 2019 In a recent study mitochondrial NADH redox state were assessed in the brain of awake rats undergoing HBOT treatment NADH was found to be oxidized to NAD in parallel to the tissue oxygenation increase showing maximal tissue oxygenation and greatest accumulation of cellular mitochondrial NAD after HBOT Meirovithz et al 2007 Another study found HBOT signi cantly increased the level of NAD 6 h after MCAO suggesting that the hyperoxygenation exerts a long lasting effect Hu et al 2017 This evidence suggests that treatments aimed at boosting NAD levels may contribute as a promising avenue to counter age associated cognitive decline by restoring CBF improving tissue pO2 and ameliorating cellular bioenergetics in the brain Dave et al 2003 Mouchiroud et al 2013 Rajman et al 2018 A growing body of evidence implicates bioenergetic de cits mitochondrial dysfunction and impaired reduction oxidation redox homeostasis in the age related development of neurodegenerative diseases Mandal et al 2012 Venkateshappa et al 2012 Grimm and Eckert 2017 and cognitive impairment Mandal et al 2012 Studies investigating the effects of HBOT on mitochondrial function Dave et al 2003 and cellular energetics in endothelial progenitor cells Hauer Jensen 2017 Hsu et al 2019 and neurons Yang et al 2016 have shown that HBOT signi cantly modulates the basal respiration improved respiratory capacity and increased mitochondrial mass following a single HBOT session Bullock et al Zhou et al 2007 found that hypoxia alone increased cerebral ATP levels in rats while HBOT improved cognitive recovery and reduced the Frontiers in Aging www frontiersin org 4 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention subsequently induces VEGF expression and angiogenesis Cimino et al 1985 In summary HBOT has been showed to have complex effects on oxygen transport and microvascular hemodynamics The potential bene cial effects of HBOT such as reduction in hypoxia decreased edema pro angiogenic effects on the microcirculation and preservation of tissue energetics and metabolism through NAD repletion should be further investigated to understand their potential therapeutic effects against microvascular mechanisms of vascular aging and the associated loss of cognitive function formation on Matrigel plates especially in cells treated twice daily Among other conditions HBOT has shown possible ef cacy to treat vascular dementia in experimental models Xiao et al 2012 The growing enthusiasm and appreciation for the potential microvascular therapeutic role of experimental hyperoxia is re ected by recent studies aimed at developing models to quantify hyperoxia driven microvascular changes Milstein et al 2016 In a rat model of cerebral ischemia reperfusion injury it was found that hyperbaric oxygen exposure restored the permeability of the BBB by increasing expression of caveolin 1 and tight junction protein ZO 1 Li et al 2018a Stimulus evoked NVC responses are known to decrease with age and with age associated pathologies Tarantini et al 2017b Tarantini et al 2017c Tarantini et al 2018b Tarantini et al 2019a Lindauer et al Lindauer et al 2010 investigated the role of HBOT in the modulation of NVC responses using laser doppler owmetry in anesthetized rats equipped with a cranial window and found no HBOT effect on neuronal activity and neurovascular coupling during functional activation Lindauer et al 2010 In contrast a more recent study by Cardenas et al found that stimulus evoked BOLD fMRI signals were improved by HBOT in rats Cardenas et al 2015 This discrepancy could be accounted by the more super cial cortical layer mesured by doppler versus the deeper layers imaged with fMRI Interestingly it was discovered that administration of HBOT for 60 min daily for 14 consecutive days improved pathophysiological and cognitive outcomes in the 3xTg Alzheimer s disease mouse model by attenuating neuroin ammation Shapira et al 2018a Shapira et al 2018b HBOT has been shown to reduce pain using animal models Early clinical research indicates HBOT may also be useful in modulating human pain however further studies are required to determine whether HBOT is a safe and ef cacious treatment modality for chronic pain conditions Sutherland et al 2016 Whole brain irradiation WBI is an established model of accelerated aging Warrington et al 2013 gamma irradiation induces senescence in healthy tissues Csipo et al 2020 and leads to progressive cognitive dysfunction and gait alterations Ungvari et al 2017a Currently new strategies are being sought out to preserve cognitive abilities in patients undergoing radiation therapy against brain metastases Robin and Rusthoven 2018 Irradiated organs develop hypovascular hypocellular hypoxic tissue that does not revascularize spontaneously In a rabbit model HBOT demonstrated a dramatic increase in vascular density over both normobaric oxygen and air breathing control Marx et al 1990 suggesting that HBOT may stimulate anti aging effects by restoring microvascular endothelial function associated with the preservation of cognitive abilities The presented animal studies expand the eld of high pressure oxygen therapy and provide evidence leading to prospective hypothesis testing for the vasculoprotective role of HBOT and its contribution to the modulation of cerebral microvascular mechanisms regulating angiogenesis BBB permeability Li et al 2018a bioenergetics and reginal modulation of CBF via neurovascular coupling responses and their relationship with cognitive function EXPERIMENTAL MODELS FOR HBOT Although HBOT is available and used worldwide in human medicine many scienti c discoveries that report its bene cial effects for human diseases were rst investigated in animal models primarily rodents mice rats and rabbits but also dogs cats and pigs Edwards 2010 Current protocols for murine HBOT administration include use of speci cally designed homemade devices Avraham Lubin et al 2011 Lu et al 2016 and commercially available hyperbaric chambers such as the p 1100 from Barotec Hanyuda Doguchi et al 2014 To mimic hyperbaric therapy that is administered to humans mice breathe pure oxygen at pressures ranging from 2 to 4 ATA for 60 90 min daily for at least a week A minimum of 15 min of pressurization and depressurization is often allowed for animals to adjust to the changes in pressure Animal models have demonstrated that HBOT creates the necessary oxygen gradients between the hyperoxygenated blood and injured tissues promoting several bene cial effects in multiple pathologies As the relationship between cerebral microvascular health and cognitive function has become wellrecognized De Silva and Faraci 2016 great scienti c interest is devoted to understanding the potential therapeutic effects HBOT speci cally exerts on the brain and its microvasculature Studies conducted in animal models suggest that HBOT has powerful bene cial effects in the microvascular endothelial layer of cells lining the small vessels a recent study demonstrated microcirculatory pro angiogenic processes are accelerated by HBOT Knighton et al 1981 Hunt 1988 Goyal et al 2019 and that angiogenesis is promoted through regulation of vascular endothelial growth factor Johnson and Wilgus 2014 which then restores tissue pO2 within the injured tissue and reestablishes adequate oxygen delivery for regeneration and repair Hopf et al 2005 Sheikh et al 2005 Rodriguez et al 2008 In vitro hyperoxia has been shown to induce endothelial progenitor cells secretion of exosomes which improved the bioactivity of microvascular endothelial cells in the lungs Zhang et al 2019 In a study by Giardina et al genome wide gene expression microarray analysis in human microvascular endothelial cells revealed that HBOT upregulated genes involved in protein damage control and identi ed Nrf2 upregulation as one of the primary consequences following HBOT Godman et al 2010 In this study HBOT induced Nrf2 upregulation and other gene expression changes associated with enhanced endothelial tube Frontiers in Aging www frontiersin org 5 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention TABLE 1 Summary of relevant clinical ndings testing the ef cacy and safety of HBOT for the treatment of age related vascular cognitive impairment and dementia The highlighted studies present existing evidence indicative of a potential therapeutic role for HBOT induced hyperoxia against age related cerebromicrovascular pathologies contributing to cognitive impairment dementia and decreased healthspan Vascular clinical evidence for HBOT Treatment 100 Oxygen by mask at 2 ATA for 90 min with 5min air breaks every 20 min daily 100 Oxygen at 2 4 ATA at 37 C for 60 min 100 Oxygen at 2 5 ATA 100 Oxygen at 2 ATA twice daily for 90 min each day 100 Oxygen by mask at 2 ATA for 90 min with 5min air breaks every 20 min daily 100 Oxygen at 2 4 ATA for 120 min daily 100 Oxygen at 2 4 ATA over 8 weeks 100 Oxygen by mask at 2 ATA for 45 min 100 Oxygen at 2 ATA for 80 min 100 Oxygen at 2 ATA 100 Oxygen at 2 ATA for 60 min 5 days per week Duration Age Outcome 60 days 64 y o Twice day 30 sessions Human cells 68 y o 15 days 72 y o Increases telomere length Decreases immunosenescence in isolated blood cells Increased Nrf2 pathway activation Increased endothelial tube formations on Matrigel Gains in post treatment performance on psychological tests of cognitive functioning No enhanced cognitive functioning 60 days 69 y o 28 sessions 30 sessions Single exposure 5 days week 45 y o 20 51 y o 22 68 y o 18 20 y o 4 weeks 12 weeks n a 68 y o Increased cerebral blood ow Cognitive enhancements in healthy aging adults Improved attention information processing speed and executive function Regression of cerebral edema and radionecrosis No effect on post concussive symptoms after mild TBI Cognitive motor single tasks and multitasking performance scores were signi cantly enhanced Improved memory correlated with enhanced functional connectivity in the left hippocampus FMD plasma NO and CGRP signi cantly increased Improved cognitive function in vascular dementia patients CLINCAL EVIDENCE FOR HBOT Hachmo et al 2020 Godman et al 2010 Jacobs et al 1969 Raskin et al 1978 Hadanny et al 2020 Cihan et al 2009 Wolf et al 2012 Vadas et al 2017 Yu et al 2015 Li et al 2018b Xu et al 2019 percent oxygen at 2 ATA for a total duration of 15 sessions some of the treated participants reported increased visual acuity in addition to improvements across a range of cognitive domains Edwards and Hart 1974 In these studies the bene cial effect of hyperbaric oxygen was presumed to be due to improved blood ow providing compelling evidence of the relationship between restoration of tissue oxygenation and improvement in function The clinical evidence for the role of HBOT against cognitive decline in the elderly is not without controversy in a report Raskin et al focused on the psychological and psychomotor test variables administered prior to and following hyperbaric oxygen treatment and failed to detect any cognitive differences as a function of sex CO2 loading test or presumed evidence of cerebrovascular disease Raskin et al 1978 In 2012 Xiao et al published a Cochrane review analyzing the effectiveness and safety of HBOT for vascular dementia Xiao et al 2012 However the evidence they presented was insuf cient to support HBOT as an effective treatment for patients with vascular dementia since only one study involving 64 patients was included This work compared HBOT as an adjuvant to donepezil against donepezil alone Patients receiving HBOT plus donepezil had signi cantly better cognitive function than the donepezil only group after 12 weeks of treatment measured by MMSE scoring or by Hasegawa s Dementia Rating Scale HDS A very recent clinical meta analysis on the ef cacy and safety of hyperbaric oxygen as that HBOT can be recommended as an effective and safe complementary therapy for the treatment of vascular dementia You et al 2019 This meta analysis included twenty ve randomized clinical trials and included almost 2 000 patients that underwent HBOT between 2008 and 2017 The results indicated that HBOT markedly improved the Mini Mental State Examination MMSE scores Vascular Cognitive Impairment In humans age related vascular cognitive impairment accounts for about 30 percent of all cases of dementia second only to Alzheimer s disease which accounts for 60 percent Kalaria et al 2008 The symptoms of vascular dementia and VCI are consequences of accumulation of age related vascular phenotypical alterations pathologically affecting the structure and function of the cerebral microvasculature Jellinger 2004 Iadecola 2013 Ungvari et al 2018a Ungvari et al 2018b Finding preventative and therapeutic prospects remains one of the greatest challenges in the eld of geroscience as many laboratories and investigators have dedicated their efforts to develop therapeutic strategies against VCI Smith et al 2017 Growing evidence in animal models has warranted the necessity for human clinical trials to investigate the role of HBOT against VCI in humans Table 1 The combination of pure oxygen and higher pressure leads to increases in tissue oxygenation while also targeting oxygen and pressure sensitive genes The result is restored and enhanced tissue metabolism Extant studies in rodents demonstrated that among other effects HBOT can improve the blood supply and promote neurogenesis in the piriform cortex Zhang et al 2010 and in the hippocampus J Y 2007 to enhance learning and memory however the exact mechanisms remain unclear In humans the early works performed by Jacobs et al in 1969 on a group of 13 elderly male patients with a mean age of 68 indicate that intermittent hyperoxygenation can improve cognitive function in the elderly with the bene cial effects outlasting the duration of the increased pO2112 In another study performed a few years later on a cohort of 20 elderly individuals treated with 100 Frontiers in Aging www frontiersin org References 6 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention activities of daily living by Barthel index and total ef cacy rate while adverse effects were not statistically different between HBOT and control groups You et al 2019 Subgroup analysis revealed that 7 8 weeks of 60 min HBOT administration produce the maximum therapeutic effect to VCI patients and the positive outcomes are more precise and reliable within this administration regimen To provide some mechanistic insight a recent study published this year from Xu et al included a total of 158 patients with vascular dementia which were randomly divided into control and hyperbaric oxygen groups Xu et al 2019 HBOT was administered 5 days per week for 12 weeks with each session lasting 60 min each at 2 ATA 100 O2 The ndings from Xu et al concluded that after the treatment period patients receiving HBOT not only showed signi cantly higher MMSE scores but also exhibited higher serum Humanin levels compared to control which highly correlated with MMSE scores Humanin is a mitochondrialderived peptide with strong neuroprotective effects Z rate et al 2019 which has been found to prevent cognitive decline in clinical and experimental studies Yen et al 2018 HBOT cognitive protection and pro vascular effects bene cially extend to the vascular endothelium In a study 98 patients admitted with chest discomfort were divided in a control group to receive conventional treatment and a hyperbaric oxygen administration group which received HBOT in addition to conventional treatment Patients who were administered additional HBOT therapy for 4 weeks exhibited improved ow mediated vasodilation FMD response of the brachial artery increased plasma nitric oxide NO increased calcitonin gene related peptide CGRP and decreased levels of endothelin 1 ET 1 and high sensitivity C reactive protein hsCRP Li et al 2018b The HBOT induced improvement in cognitive performance is not limited to individuals suffering from age related VCI A prospective double blind randomized control crossover trial including 22 healthy volunteers showed that compared to the performance at normobaric conditions both cognitive and motor single tasks scores were signi cantly enhanced by the hyperbaric oxygen environment Vadas et al 2017 Currently the U S Food and Drug Administration FDA and the undersea and hyperbaric medical society UHMS are the key agencies providing guidelines and indications for marketing and use of HBOT Weaver 2014 Fife et al 2016 At this time HBOT is approved for the medical treatment of 13 conditions 1 decompression illness 2 carbon monoxide poisoning 3 air or gas embolism 4 crush injury syndrome 5 clostridial myositis and myonecrosis 6 adjunctive treatment of selected problem wounds 7 chronic refractory osteomyelitis 8 exceptional blood loss anemia 9 necrotizing soft tissue infections 10 late radiation tissue injury 11 thermal burns 12 ischemic skin graft and aps and 13 intracranial abscess Fife et al 2016 Since among its proven bene cial effects HBOT has the unique ability to ameliorate tissue hypoxia reduce pathologic in ammation mitigate ischemia reperfusion injury as well as reduce brain edema the Department of Defense DoD has funded trials to evaluate the use of HBOT in chronic traumatic brain injury TBI which thus far is not supported Frontiers in Aging www frontiersin org by the evidence Wolf et al 2012 Cifu et al 2014a Cifu et al 2014b Walker et al 2014 Miller et al 2015 Patients with TBI may present cognitive de cits within the rst 24 h after trauma in the so called acute phase which in turn may lead to long term cognitive impairment and decrease in quality of life The outcome of this research initiative proved that in two randomized clinical trials comprised of 143 active duty or veteran military personnel composite total scores improved from baseline with administration of HBOT Weaver et al 2019 WBI is a mainstream therapy for patients with both identi able brain metastases and is associated with signi cant neurotoxicity However it also promotes accelerated senescence in healthy tissues and leads to progressive cognitive dysfunction in up to 50 of tumor patients Ungvari et al 2017a The longterm risk for radiation induced brain in ammation and necrosis inducing secondary cognitive impairments are increasing concerns Currently there is no effective treatment for preventing long term radiation induced brain damage HBOT is currently indicated as an experimental therapy for patients with suspected radiation induced neurotoxicity and was proven to reduce further development of radiation damage In a case report a 45 year old man who developed brain radionecrosis in the right frontal and left temporoparietal lobes and after receiving WBI was referred to HBOT administration After HBOT both clinical and cognitive ndings improved suggesting that akin to experimental results Warrington et al 2013 treatments that restore cerebromicrovascular function after WBI related injuries are associated with improved health outcomes Cihan et al 2009 Duration and HBOT exposure are not standardized however administration of HBOT for 2 h day 5 days week for 3 months Hadanny et al 2020 was able to produce cognitive improvements The authors of this recent study measured in 63 healthy active adults changes in cognitive function via a standardized battery of comprehensive computerized cognitive assessments and CBF by functional magnetic resonance imaging The results showed improved attention cognitive processing speeds and executive function adding to the growing body of evidence that HBOT has regenerative effects on the brain Hadanny et al 2020 Remarkably this is the rst study to demonstrate the bene cial pro cognitive effects of HBOT on healthy older subjects Hadanny et al 2020 providing evidence for the potential effects of HBOT on the healthspan of aged individuals Similarly a double blind placebo controlled clinical trial provided additional supporting evidence for the bene cial effects of HBOT by testing the effect of HBOT on brain function and cognitive outcomes in mildly cognitively impaired elderly individuals with diabetes BenAri et al 2020 Although there is clinical and experimental evidence in favor of HBOT to improve cognitive function in patients with age related vascular pathologies oxygen therapy is not without consequences and should be administered with caution As such the mechanism of HBOT warrants further investigation Overall the available evidence suggested that application of HBOT as adjuvant therapy has additional bene ts on VCI patients individuals exposed to WBI and individuals suffering from TBI and is generally regarded as safe 7 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention Other Interesting Clinical Effects of HBOT through formation of peroxynitrite ONOO however O2 toxicity induced seizures are relatively rare 0 01 at typical clinical treatment pressures 2 ATA 3 ATA and are dif cult to predict on an individual basis Oxygen toxicity quickly resolves after withdrawal of oxygen and can be easily mitigated by limiting the duration of HBOT sessions and by providing additional air breaks Heyboer et al 2017 HBOT also increases the risk of pulmonary edema in patients with compromised left ventricular function There are limited published data two studies reported their incidence at 1 in 1 000 0 1 and 1 in 4 500 0 02 Abel et al 2000 Weaver and Churchill 2001 While the etiology is not fully known it appears to be related to hyperbaric oxygen inducing increased systemic vascular resistance and decreased cardiac output Whalen et al 1965 Abel et al 2000 in this highrisk population Heyboer et al 2017 Individuals that reside in high altitude environments are exposed to decreased oxygen tension Currently the effects of HBOT on high altitude dwellers has not been examined however individuals that are consistently exposed to lower environmental pO2 have shown higher hemoglobin concentration Mairb url et al 1985 The effects of HBOT on these populations is unclear since during HBOT oxygen can be carried by hyperoxygenated plasma in addition to saturated hemoglobin An additional interesting clinical nding shows that HBOT could aid in perinatal resuscitation of the newborn with perinatal asphyxia Yilmaz et al 2020 Con icting evidence has shown that excessive oxygen may cause retinopathy or bronchopulmonary dysplasia providing evidence against the use of HBOT in neonates Liu et al 2006 However HBOT has been used to treat newborns with neonatal hypoxicischemic encephalopathy in clinical studies in China The time window of HBOT is still controversial In clinical studies HBOT is usually initiated within one to 7 days after birth administered one to three times per day at 0 15 0 17 MPa for 60 120 min and continued for one to four courses of treatment Liu et al 2006 FUTURE DIRECTIONS Hyperbaric oxygen increases brain pO2 by saturating blood oxygen and therefore increasing the volume of oxygenated tissue around small vessels establishing a steeper O2 diffusion gradient between blood and tissue Demchenko et al 2005 The combination of pure oxygen and higher pressure leads to increases in brain tissue oxygenation while also targeting oxygen and pressure sensitive genes altogether promoting resilience in aging No consensus exists indicating the exact adequate clinical levels for achieving medically bene cial results Nonetheless supplementary oxygen is routinely administered in patients with adequate oxygen saturation levels with the belief that it will improve oxygen delivery in patients with distressed tissues af icted by ischemic insults Importantly there is newly gathered evidence suggesting that daily 1 h long HBOT administrations for 4 8 weeks may provide bene cial effects against vascular dementia while limiting the adverse effects of transient oxygen toxicity Table 1 HBOT has been recommended and used for a wide range of medical conditions with a varying evidence base The concept and its therapeutic potential that increased tissue oxygenation can be achieved through increased blood PO2 has fascinated physicians and researchers for centuries Evidence for the widespread use of HBOT for decompression sickness and air embolism is robust and well proven The UHMS reviews new evidence and published recommendations for the use of HBOT over the years the list of indicated conditions which warrant the use of HBOT has increased and at this time there are 14 conditions for which hyperoxia is a recommended therapy Weaver 2014 Although signi cant progress has been achieved in identifying the appropriate pathologies for which HBOT could serve a therapeutic role research efforts should persist in this direction to advance our understanding of the multifaceted effects of HBOT as there lays the potential to develop innovative strategies to improve biological endpoints affected by aging Additionally understanding how HBOT would affect the cerebral microcirculation in aging to ameliorate vascular health span and cognitive outcome in the elderly population is ADVERSE EFFECTS OF HBOT HBOT is relatively safe but this type of treatment does carry some risks mainly due to the increased pressure and hyperoxia Jacobs et al 1969 Most pressure induced barotrauma is preventable by proper equalization techniques or tympanostomy tubes Vrabec et al 1998 and otitis media can be prevented with pseudoephedrine Brown et al 1992 More severe barotrauma is rare but may include tympanic rupture tinnitus and vertigo Pulmonary barotrauma and pneumothorax are extremely rare The hyperoxia poses a rehazard Shef eld and Desautels 1997 with 77 human fatalities reported from 1923 to 1996 However better practices and improved safety regulations have driven that number down In North America from 1968 to 2009 there were no reported deaths related to re in any facilities operating hyperbaric chambers that complied with the national re protection association codes Some con icting evidence suggests that high pressure HBOT may not be for everyone especially for individuals with uncontrolled pre existing conditions such as hypertension For those individuals a milder pressure might be required Some studies have reported cerebral vasoconstriction Lambertsen et al 1953 and decreased total or regional CBF Visser et al 1996 Omae et al 1998 in healthy volunteers and patients breathing 100 percent O2 at 3 4 ATA However those transitory uctuations were driven by the immediate increase in blood O2 concentration and CBF was quickly restored In some studies HBOT increased the production of oxygen free radicals which can oxidize membrane lipids and proteins and cause DNA damage Gill and Bell 2004 and inhibit bacterial metabolic functions Memar et al 2018 Central nervous system CNS exposure to high above 2 000 mmHg pO2 may result in oxygen toxicity rstly recognized by Paul Bert in 1878 Kellogg 1978 NO has been implicated as a mediator for CNS oxygen toxicity Frontiers in Aging www frontiersin org 8 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention of high interest for our aging society The mechanisms involved in HBOT induced vasculoprotective effects are multifaceted Cellular and molecular mechanisms of vascular aging such as BBB permeability increased in ammation mitochondrial dysfunction oxidative stress loss of Nrf2 activity and NAD depletion contribute to the pathogenesis of age related cerebromicrovascular diseases Figure 1 Growing evidence presented in this review suggests that HBOT targets these very same processes ameliorating and reversing microvascular pathologies such as endothelial dysfunction Godman et al 2010 microvascular rarefaction Dhamodharan et al 2019 Yu et al 2019 improved blood brain barrier features Li et al 2018a mitochondrial function Nukhet Aylin Burns et al 2018 Lippert and Borlongan 2019 cellular metabolism in ammation and oxidative stress Efrati and Ben Jacob 2014 as well as ameliorating decreased NVC responses Cardenas et al 2015 which contribute to the development of age related neurodegeneration and VCI Further studies are warranted to explore the cerebromicrovascular effects of HBOT in animal models of aging If evidence is present to suggest that a wellcontrolled regimen of hyperoxia would be bene cial to the cerebral microcirculation it could be hypothesized that such a treatment may be promising as a potential therapy to increase resilience in aging and to delay or ameliorate age related vascular cognitive impairment and dementias associated with vascular pathologies and impaired cerebral tissue oxygenation AUTHOR CONTRIBUTIONS PB JD AN T RG AT and ST researched wrote reviewed and approved the manuscript FUNDING This work was supported by grants from the American Heart Association and the NIA K01 AG073614 to ST the American Federation for Aging Research to PB the NIA supported Geroscience Training Program in Oklahoma T32AG052363 the NIA supported Oklahoma Nathan Shock Center and the NIGMS supported Center of Biomedical Research Excellence 1P20GM125528 Chavko M Braisted J C Outsa N J and Harabin A L 1998 Role of Cerebral Blood Flow in Seizures from Hyperbaric Oxygen Exposure Brain Res 791 75 82 doi 10 1016 s0006 8993 98 00083 3 Cianci P Slade J B Jr Sato R M and Faulkner J 2013 Adjunctive Hyperbaric Oxygen Therapy in the Treatment of thermal burns Undersea Hyperb Med 40 89 108 doi 10 1016 0305 4179 94 90099 x Cifu D X Hart B B West S L Walker W and Carne W 2014 The Effect of Hyperbaric Oxygen on Persistent Postconcussion Symptoms J Head Trauma Rehabil 29 11 20 doi 10 1097 htr 0b013e3182a6aaf0 Cifu D X Walker W C West S L Hart B B Franke L M Sima A et al 2014 Hyperbaric Oxygen for Blast Related Postconcussion Syndrome ThreeMonth Outcomes Ann Neurol 75 277 286 doi 10 1002 ana 24067 Cihan Y B Uzun G Yildiz and D nmez H 2009 Hyperbaric Oxygen Therapy for Radiation Induced Brain Necrosis in a Patient with Primary central Nervous System Lymphoma J Surg Oncol 100 732 735 doi 10 1002 jso 21387 Cimino F Balestra C Germonpr P De Bels D Tillmans F Saija A et al 1985 Pulsed High Oxygen Induces a Hypoxic like Response in Human Umbilical Endothelial Cells and in Humans J Appl Physiol 1985 113 1684 1689 doi 10 1152 japplphysiol 00922 2012 Csipo T Lipecz A Ashpole N M Balasubramanian P and Tarantini S 2020 Astrocyte Senescence Contributes to Cognitive Decline Geroscience 42 51 55 doi 10 1007 s11357 019 00140 9 Csiszar A Gautam T Sosnowska D Tarantini S Banki E Tucsek Z et al 2014 Caloric Restriction Confers Persistent anti oxidative Pro angiogenic and anti in ammatory Effects and Promotes anti aging miRNA Expression Pro le in Cerebromicrovascular Endothelial Cells of aged Rats Am J Physiology Heart Circulatory Physiol 307 H292 H306 doi 10 1152 ajpheart 00307 2014 Dallmeyer S Wicker P and Breuer C 2017 How an aging Society affects the Economic Costs of Inactivity in Germany Empirical Evidence and Projections Eur Rev Aging Phys Act 14 18 doi 10 1186 s11556 017 0187 1 Dave K R Prado R Busto R Raval A P Bradley W G Torbati D et al 2003 Hyperbaric Oxygen Therapy Protects against Mitochondrial Dysfunction and Delays Onset of Motor Neuron Disease in Wobbler Mice Neuroscience 120 113 120 doi 10 1016 s0306 4522 03 00244 6 De Silva T M and Faraci F M 2016 Microvascular Dysfunction and Cognitive Impairment Cell Mol Neurobiol 36 241 258 doi 10 1007 s10571 015 0308 1 Demchenko I T Luchakov Y I Moskvin A N Gutsaeva D R Allen B W Thalmann E D et al 2005 Cerebral Blood Flow and Brain Oxygenation in REFERENCES Abel F L McNamee J E Cone D L Clarke D and Tao J 2000 Effects of Hyperbaric Oxygen on Ventricular Performance Pulmonary Blood Volume and Systemic and Pulmonary Vascular Resistance Undersea Hyperb Med 27 67 73 Aero chalinos N H 1664 Dancer North Palm Beach Florida Best Publishing Company Al Waili N S Butler G J Beale J Abdullah M S Hamilton R W B Lee B Y et al 2005 Hyperbaric Oxygen in the Treatment of Patients with Cerebral Stroke Brain Trauma and Neurologic Disease Adv Ther 22 659 678 doi 10 1007 bf02849960 Angelova P R Kasymov V Christie I Sheikhbahaei S Turovsky E Marina N et al 2015 Functional Oxygen Sensitivity of Astrocytes J Neurosci 35 10460 10473 doi 10 1523 jneurosci 0045 15 2015 Avraham Lubin B C R Dratviman Storobinsky O El S D B Hasanreisoglu M and Goldenberg Cohen N 2011 Neuroprotective Effect of Hyperbaric Oxygen Therapy on anterior Ischemic Optic Neuropathy Front Neur 2 23 doi 10 3389 fneur 2011 00023 Balasubramanian P DelFavero J Ungvari A Papp M Tarantini A Price N et al 2020 Time restricted Feeding TRF for Prevention of age Related Vascular Cognitive Impairment and Dementia Ageing Res Rev 64 101189 doi 10 1016 j arr 2020 101189 BenAri O Efrati S Sano M Bendlin B B Lin H Liu X et al 2020 A Double Blind Placebo Controlled Clinical Trial Testing the Effect of Hyperbaric Oxygen Therapy on Brain and Cognitive Outcomes of Mildly Cognitively Impaired Elderly with Type 2 Diabetes Study Design Alzheimers Dement N Y 6 e12008 doi 10 1002 trc2 12008 Brown K A Didion S P Andresen J J and Faraci F M 2007 Effect of Aging MnSOD De ciency and Genetic Background on Endothelial Function Arterioscler Thromb Vasc Biol 27 1941 1946 doi 10 1161 atvbaha 107 146852 Brown M Jones J and Krohmer J 1992 Pseudoephedrine for the Prevention of Barotitis media a Controlled Clinical Trial in Underwater Divers Ann Emerg Med 21 849 852 doi 10 1016 s0196 0644 05 81033 9 Cardenas D P Muir E R Huang S Boley A Lodge D and Duong T Q 2015 Functional MRI during Hyperbaric Oxygen Effects of Oxygen on Neurovascular Coupling and BOLD fMRI Signals Neuroimage 119 382 389 doi 10 1016 j neuroimage 2015 06 082 Frontiers in Aging www frontiersin org 9 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention Hadanny A Daniel Kotovsky M Suzin G Boussi Gross R Catalogna M Dagan K et al 2020 Cognitive Enhancement of Healthy Older adults Using Hyperbaric Oxygen a Randomized Controlled Trial Aging Albany NY 12 13740 13761 doi 10 18632 aging 103571 Harada C N Natelson Love M C and Triebel K L 2013 Normal Cognitive aging Clin Geriatr Med 29 737 752 doi 10 1016 j cger 2013 07 002 Hauer Jensen M 2017 Investigating the Effects of Hyperbaric Oxygen on Mitochondrial Function of Endothelial Progenitor Cells FASEB J Herrera M D Mingorance C Rodr guez Rodr guez R and Alvarez de Sotomayor M 2010 Endothelial Dysfunction and aging an Update Ageing Res Rev 9 142 152 doi 10 1016 j arr 2009 07 002 Heyboer M 3rd Sharma D Santiago W and McCulloch N 2017 Hyperbaric Oxygen Therapy Side Effects De ned and Quanti ed Adv Wound Care 6 210 224 doi 10 1089 wound 2016 0718 Hopf H W Gibson J J Angeles A P Constant J S Feng J J Rollins M D et al 2005 Hyperoxia and angiogenesis Wound Repair Regen 13 558 564 doi 10 1111 j 1524 475x 2005 00078 x Hou Y Lautrup S Cordonnier S Wang Y Croteau D L Zavala E et al 2018 NAD Supplementation Normalizes Key Alzheimer s Features and DNA Damage Responses in a New AD Mouse Model with Introduced DNA Repair De ciency Proc Natl Acad Sci USA 115 E1876 E1885 doi 10 1073 pnas 1718819115 Hsu S L Yin T C Shao P L Chen K H Wu R W Chen C C et al 2019 Hyperbaric Oxygen Facilitates the Effect of Endothelial Progenitor Cell Therapy on Improving Outcome of Rat Critical Limb Ischemia Am J Transl Res 11 1948 1964 Hu Q Manaenko A Bian H Guo Z Huang J L Guo Z N et al 2017 Hyperbaric Oxygen Reduces Infarction Volume and Hemorrhagic Transformation through ATP NAD Sirt1 Pathway in Hyperglycemic Middle Cerebral Artery Occlusion Rats Stroke 48 1655 1664 doi 10 1161 strokeaha 116 015753 Hunt T K 1988 The Physiology of Wound Healing Ann Emerg Med 17 1265 1273 doi 10 1016 s0196 0644 88 80351 2 Iadecola C 2004 Neurovascular Regulation in the normal Brain and in Alzheimer s Disease Nat Rev Neurosci 5 347 360 doi 10 1038 nrn1387 Iadecola C 2013 The Pathobiology of Vascular Dementia Neuron 80 844 866 doi 10 1016 j neuron 2013 10 008 Imai S i and Guarente L 2014 NAD and Sirtuins in aging and Disease Trends Cel Biol 24 464 471 doi 10 1016 j tcb 2014 04 002 J Y 2007 Effect of Hyperbaric Oxygen Therapy on ability of Learning and Memory and Hippocampal Pyramidal Cell in Vascular Dementia Rats Chin J Rehabil Theor Pract 13 1032 1035 Jacobs E A Winter P M Alvis H J and Small S M 1969 Hyperoxygenation Effect on Cognitive Functioning in the aged N Engl J Med 281 753 757 doi 10 1056 nejm196910022811402 Jaul E and Barron J 2017 Age Related Diseases and Clinical and Public Health Implications for the 85 Years Old and over Population Front Public Health 5 335 doi 10 3389 fpubh 2017 00335 Jellinger K A 2004 Pathology and Pathophysiology of Vascular Cognitive Impairment A Critical Update Panminerva Med 46 217 226 Johnson K E and Wilgus T A 2014 Vascular Endothelial Growth Factor and Angiogenesis in the Regulation of Cutaneous Wound Repair Adv Wound Care 3 647 661 doi 10 1089 wound 2013 0517 Kalaria R N Maestre G E Arizaga R Friedland R P Galasko D Hall K et al 2008 Alzheimer s Disease and Vascular Dementia in Developing Countries Prevalence Management and Risk Factors Lancet Neurol 7 812 826 doi 10 1016 s1474 4422 08 70169 8 Kane A E and Sinclair D A 2018 Sirtuins and NAD in the Development and Treatment of Metabolic and Cardiovascular Diseases Circ Res 123 868 885 doi 10 1161 circresaha 118 312498 Kellogg R H 1978 La Pression Barom trique Paul Bert s Hypoxia Theory and its Critics Respiration Physiol 34 1 28 doi 10 1016 0034 5687 78 90046 4 Kiss T Balasubramanian P Valcarcel Ares M N Tarantini S Yabluchanskiy A Csipo T et al 2019 Nicotinamide Mononucleotide NMN Treatment attenuates Oxidative Stress and Rescues angiogenic Capacity in aged Cerebromicrovascular Endothelial Cells a Potential Mechanism for the Prevention of Vascular Cognitive Impairment Geroscience 41 619 630 doi 10 1007 s11357 019 00074 2 Rats Breathing Oxygen under Pressure J Cereb Blood Flow Metab 25 1288 1300 doi 10 1038 sj jcbfm 9600110 Dhamodharan U Karan A Sireesh D Vaishnavi A Somasundar A Rajesh K et al 2019 Tissue speci c Role of Nrf2 in the Treatment of Diabetic Foot Ulcers during Hyperbaric Oxygen Therapy Free Radic Biol Med 138 53 62 doi 10 1016 j freeradbiomed 2019 04 031 Doguchi H Saio M Kuniyoshi S Matsuzaki A and Yoshimi N 2014 The Enhancing Effects of Hyperbaric Oxygen on Mouse Skin Carcinogenesis J Toxicol Pathol 27 67 72 doi 10 1293 tox 2013 0046 Drummond G R Selemidis S Griendling K K and Sobey C G 2011 Combating Oxidative Stress in Vascular Disease NADPH Oxidases as Therapeutic Targets Nat Rev Drug Discov 10 453 471 doi 10 1038 nrd3403 Edwards A E and Hart G M 1974 Hyperbaric Oxygenation and the Cognitive Functioning of the aged J Am Geriatr Soc 22 376 379 doi 10 1111 j 15325415 1974 tb04845 x Edwards M L 2010 Hyperbaric Oxygen Therapy Part 2 application in Disease J Vet Emerg Crit Care San Antonio 20 289 297 doi 10 1111 j 14764431 2010 00535_1 x Efrati S and Ben Jacob E 2014 Re ections on the Neurotherapeutic Effects of Hyperbaric Oxygen Expert Rev Neurotherapeutics 14 233 236 doi 10 1586 14737175 2014 884928 Falkowska A Gutowska I Goschorska M Nowacki P Chlubek D and Baranowska Bosiacka I 2015 Energy Metabolism of the Brain Including the Cooperation between Astrocytes and Neurons Especially in the Context of Glycogen Metabolism Ijms 16 25959 25981 doi 10 3390 ijms161125939 Feldmeier J J 2003 Undersea and Hyperbaric Medical Society Hyperbaric Oxygen 2003 Indications and Results The Hyperbaric Oxygen Therapy Committee Report 141 Felsky D Roostaei T Nho K Risacher S L Bradshaw E M Petyuk V et al 2019 Neuropathological Correlates and Genetic architecture of Microglial activation in Elderly Human Brain Nat Commun 10 409 doi 10 1038 s41467018 08279 3 Fife C E Eckert K A and Carter M J 2016 An Update on the Appropriate Role for Hyperbaric Oxygen Plast Reconstr Surg 138 107S 116S doi 10 1097 prs 0000000000002714 Fricker R A Green E L Jenkins S I and Grif n S M 2018 The In uence of Nicotinamide on Health and Disease in the Central Nervous System Int J Tryptophan Res 11 1178646918776658 doi 10 1177 1178646918776658 Fulop G A Kiss T Tarantini S Balasubramanian P Yabluchanskiy A Farkas E et al 2018 Nrf2 De ciency in aged Mice Exacerbates Cellular Senescence Promoting Cerebrovascular In ammation Geroscience 40 513 521 doi 10 1007 s11357 018 0047 6 Gill A L and Bell C N A 2004 Hyperbaric Oxygen its Uses Mechanisms of action and Outcomes QJM 97 385 395 doi 10 1093 qjmed hch074 Godman C A Chheda K P Hightower L E Perdrizet G Shin D G and Giardina C 2010 Hyperbaric Oxygen Induces a Cytoprotective and angiogenic Response in Human Microvascular Endothelial Cells Cell Stress and Chaperones 15 431 442 doi 10 1007 s12192 009 0159 0 Gong B Pan Y Vempati P Zhao W Knable L Ho L et al 2013 Nicotinamide Riboside Restores Cognition through an Upregulation of Proliferator activated Receptor Coactivator 1 Regulated secretase 1 Degradation and Mitochondrial Gene Expression in Alzheimer s Mouse Models Neurobiol Aging 34 1581 1588 doi 10 1016 j neurobiolaging 2012 12 005 Goyal A Chonis T and Cooper J S 2019 Hyperbaric Cardiovascular Effects StatPearls Treasure Island FL Grimm A and Eckert A 2017 Brain aging and Neurodegeneration from a Mitochondrial point of View J Neurochem 143 418 431 doi 10 1111 jnc 14037 Grunewald M Kumar S Sharife H Volinsky E Gileles Hillel A Licht T et al 2021 Counteracting age Related VEGF Signaling Insuf ciency Promotes Healthy aging and Extends Life Span Science 373 373 doi 10 1126 science abc8479 Hachmo Y Hadanny A Abu Hamed R Daniel Kotovsky M Catalogna M Fishlev G et al 2020 Hyperbaric Oxygen Therapy Increases Telomere Length and Decreases Immunosenescence in Isolated Blood Cells a Prospective Trial Aging Albany NY 12 22445 22456 doi 10 18632 aging 202188 Frontiers in Aging www frontiersin org 10 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention Knighton D R Silver I A and Hunt T K 1981 Regulation of Wound Healing angiogenesis Effect of Oxygen Gradients and Inspired Oxygen Concentration Surgery 90 262 270 Kranke P Bennett M H Martyn St James M Schnabel A Debus S E and Weibel S 2015 Hyperbaric Oxygen Therapy for Chronic Wounds Cochrane Database Syst Rev 2015 CD004123 doi 10 1002 14651858 CD004123 pub4 Lambertsen C J Kough R H Cooper D Y Emmel G L Loeschcke H H and Schmidt C F 1953 Oxygen Toxicity Effects in Man of Oxygen Inhalation at 1 and 3 5 Atmospheres upon Blood Gas Transport Cerebral Circulation and Cerebral Metabolism J Appl Physiol 5 471 486 doi 10 1152 jappl 1953 5 9 471 Leach R M Rees P J and Wilmshurst P 1998 ABC of Oxygen Hyperbaric Oxygen Therapy BMJ 317 1140 1143 doi 10 1136 bmj 317 7166 1140 Lee C C Chen S C Tsai S C Wang B W Liu Y C Lee H M et al 2006 Hyperbaric Oxygen Induces VEGF Expression through ERK JNK and C Jun AP 1 activation in Human Umbilical Vein Endothelial Cells J Biomed Sci 13 143 156 doi 10 1007 s11373 005 9037 7 Levit A Hachinski V and Whitehead S N 2020 Neurovascular Unit Dysregulation white Matter Disease and Executive Dysfunction the Shared Triad of Vascular Cognitive Impairment and Alzheimer Disease Geroscience 42 445 465 doi 10 1007 s11357 020 00164 6 Li H Z Chen J F Liu M and Shen J 2018 Effect of Hyperbaric Oxygen on the Permeability of the Blood Brain Barrier in Rats with Global Cerebral Ischemia reperfusion Injury Biomed Pharmacother 108 1725 1730 doi 10 1016 j biopha 2018 10 025 Li Y Zhang H Liang Y Wang W Xu T Zhang J et al 2018 Effects of Hyperbaric Oxygen on Vascular Endothelial Function in Patients with Slow Coronary Flow Cardiol J 25 106 112 doi 10 5603 cj a2017 0132 Lin P Y Sung P H Chung S Y Hsu S L Chung W J Sheu J J et al 2018 Hyperbaric Oxygen Therapy Enhanced Circulating Levels of Endothelial Progenitor Cells and Angiogenesis Biomarkers Blood Flow in Ischemic Areas in Patients with Peripheral Arterial Occlusive Disease J Clin Med 7 doi 10 3390 jcm7120548 Lindauer U Leithner C Kaasch H Rohrer B Foddis M F chtemeier M et al 2010 Neurovascular Coupling in Rat Brain Operates Independent of Hemoglobin Deoxygenation J Cereb Blood Flow Metab 30 757 768 doi 10 1038 jcbfm 2009 259 Lippert T and Borlongan C V 2019 Prophylactic Treatment of Hyperbaric Oxygen Treatment Mitigates In ammatory Response via Mitochondria Transfer CNS Neurosci Ther 25 815 823 doi 10 1111 cns 13124 Liu Z Xiong T and Meads C 2006 Clinical Effectiveness of Treatment with Hyperbaric Oxygen for Neonatal Hypoxic Ischaemic Encephalopathy Systematic Review of Chinese Literature BMJ 333 374 doi 10 1136 bmj 38776 731655 2f Lu Z Ma J Liu B Dai C Xie T Ma X et al 2016 Hyperbaric Oxygen Therapy Sensitizes Nimustine Treatment for Glioma in Mice Cancer Med 5 3147 3155 doi 10 1002 cam4 851 Mairb url H Gassmann M and Muckenthaler M U 1985 Geographical ancestry affects normal Hemoglobin Values in High altitude Residents J Appl Physiol 1985 129 1451 1459 doi 10 1152 japplphysiol 00025 2020 Mandal P K Tripathi M and Sugunan S 2012 Brain Oxidative Stress Detection and Mapping of anti oxidant Marker Glutathione in Different Brain Regions of Healthy Male female MCI and Alzheimer Patients Using Non invasive Magnetic Resonance Spectroscopy Biochem Biophysical Res Commun 417 43 48 doi 10 1016 j bbrc 2011 11 047 Marx R E Ehler W J Tayapongsak P and Pierce L W 1990 Relationship of Oxygen Dose to angiogenesis Induction in Irradiated Tissue Am J Surg 160 519 524 doi 10 1016 s0002 9610 05 81019 0 Meirovithz E Sonn J and Mayevsky A 2007 Effect of Hyperbaric Oxygenation on Brain Hemodynamics Hemoglobin Oxygenation and Mitochondrial NADH Brain Res Rev 54 294 304 doi 10 1016 j brainresrev 2007 04 004 Memar M Y Ghotaslou R Samiei M and Adibkia K 2018 Antimicrobial Use of Reactive Oxygen Therapy Current Insights Idr Vol 11 567 576 doi 10 2147 idr s142397 Miller R S Weaver L K Bahraini N Churchill S Price R C Skiba V et al 2015 Effects of Hyperbaric Oxygen on Symptoms and Quality of Life Among Frontiers in Aging www frontiersin org Service Members with Persistent Postconcussion Symptoms JAMA Intern Med 175 43 52 doi 10 1001 jamainternmed 2014 5479 Milstein D M J Helmers R Hackmann S Belterman C N W van Hulst R A and de Lange J 2016 Sublingual Microvascular Perfusion Is altered during Normobaric and Hyperbaric Hyperoxia Microvasc Res 105 93 102 doi 10 1016 j mvr 2016 02 001 Mouchiroud L Houtkooper R H and Auwerx J 2013 NAD metabolism A Therapeutic Target for age Related Metabolic Disease Crit Rev Biochem Mol Biol 48 397 408 doi 10 3109 10409238 2013 789479 Nukhet Aylin Burns K J K Zhou D and Martin H J 2018 Investigating the Effects of Hyperbaric Oxygen on Mitochondrial Function of Endothelial Progenitor Cells FASEB J 31 711 7 Omae T Ibayashi S Kusuda K Nakamura H Yagi H and Fujishima M 1998 Effects of High atmospheric Pressure and Oxygen on Middle Cerebral Blood Flow Velocity in Humans Measured by Transcranial Doppler Stroke 29 94 97 doi 10 1161 01 str 29 1 94 Park L Anrather J Girouard H Zhou P and Iadecola C 2007 Nox2 derived Reactive Oxygen Species Mediate Neurovascular Dysregulation in the aging Mouse Brain J Cereb Blood Flow Metab 27 1908 1918 doi 10 1038 sj jcbfm 9600491 Phillips T J 2000 Hyperbaric Oxygen Therapy a Therapy in Search of a Disease Dermatol Surg 26 1167 1170 doi 10 1046 j 1524 4725 2000 00296 x Rajman L Chwalek K and Sinclair D A 2018 Therapeutic Potential of NADBoosting Molecules The In Vivo Evidence Cel Metab 27 529 547 doi 10 1016 j cmet 2018 02 011 Raskin A Gershon S Crook T H Sathananthan G and Ferris S 1978 The Effects of Hyperbaric and Normobaric Oxygen on Cognitive Impairment in the Elderly Arch Gen Psychiatry 35 50 56 doi 10 1001 archpsyc 1978 01770250052005 Robertson P W and Hart B B 1999 Assessment of Tissue Oxygenation Respir Care Clin N Am 5 221 263 Robin T P and Rusthoven C G 2018 Strategies to Preserve Cognition in Patients with Brain Metastases A Review Front Oncol 8 415 doi 10 3389 fonc 2018 00415 Rodriguez P G Felix F N Woodley D T and Shim E K 2008 The Role of Oxygen in Wound Healing a Review of the Literature Dermatol Surg 34 1159 1169 doi 10 1111 j 1524 4725 2008 34254 x S V 1990 Cardiovascular Changes Induced by Hyperbaric Oxygen Therapy Undersea Biomed Res 17 117 Sato T Takeda Y Hagioka S Zhang S and Hirakawa M 2001 Changes in Nitric Oxide Production and Cerebral Blood Flow before Development of Hyperbaric Oxygen Induced Seizures in Rats Brain Res 918 131 140 doi 10 1016 s0006 8993 01 02984 5 Schneider J A Arvanitakis Z Bang W and Bennett D A 2007 Mixed Brain Pathologies account for Most Dementia Cases in CommunityDwelling Older Persons Neurology 69 2197 2204 doi 10 1212 01 wnl 0000271090 28148 24 Seals D R Justice J N and LaRocca T J 2016 Physiological Geroscience Targeting Function to Increase Healthspan and achieve Optimal Longevity J Physiol 594 2001 2024 doi 10 1113 jphysiol 2014 282665 Shapira R Efrati S and Ashery U 2018 Hyperbaric Oxygen Therapy as a New Treatment approach for Alzheimer s Disease Neural Regen Res 13 817 818 doi 10 4103 1673 5374 232475 Shapira R Solomon B Efrati S Frenkel D and Ashery U 2018 Hyperbaric Oxygen Therapy ameliorates Pathophysiology of 3xTg AD Mouse Model by attenuating Neuroin ammation Neurobiol Aging 62 105 119 doi 10 1016 j neurobiolaging 2017 10 007 Shef eld P J and Desautels D A 1997 Hyperbaric and Hypobaric Chamber Fires a 73 year analysis Undersea Hyperb Med 24 153 164 Sheikh A Y Rollins M D Hopf H W and Hunt T K 2005 Hyperoxia Improves Microvascular Perfusion in a Murine Wound Model Wound Repair Regen 13 303 308 doi 10 1111 j 1067 1927 2005 130313 x Smith E E Cieslak A Barber P Chen J Chen Y W Donnini I et al 2017 Therapeutic Strategies and Drug Development for Vascular Cognitive Impairment J Am Heart Assoc 6 doi 10 1161 JAHA 117 005568 Sukoff M H and Ragatz R E 1982 Hyperbaric Oxygenation for the Treatment of acute Cerebral Edema Neurosurgery 10 29 38 doi 10 1227 00006123198201000 00006 11 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention Sutherland A M Clarke H A Katz J and Katznelson R 2016 Hyperbaric Oxygen Therapy A New Treatment for Chronic Pain Pain Pract 16 620 628 doi 10 1111 papr 12312 Tarantini S Valcarcel Ares N M Yabluchanskiy A Fulop G A Hertelendy P Gautam T et al 2018 Treatment with the Mitochondrial Targeted antioxidant Peptide SS 31 Rescues Neurovascular Coupling Responses and Cerebrovascular Endothelial Function and Improves Cognition in aged Mice Aging Cell 17 e12731 doi 10 1111 acel 12731 Tarantini S Fulop G A Kiss T Farkas E Z lei Sz n si D Galvan V et al 2017 Demonstration of Impaired Neurovascular Coupling Responses in TG2576 Mouse Model of Alzheimer s Disease Using Functional Laser Speckle Contrast Imaging Geroscience 39 465 473 doi 10 1007 s11357 0179980 z Tarantini S Tran C H T Gordon G R Ungvari Z and Csiszar A 2017 Impaired Neurovascular Coupling in aging and Alzheimer s Disease Contribution of astrocyte Dysfunction and Endothelial Impairment to Cognitive Decline Exp Gerontol 94 52 58 doi 10 1016 j exger 2016 11 004 Tarantini S Valcarcel Ares M N Toth P Yabluchanskiy A Tucsek Z Kiss T et al 2019 Nicotinamide Mononucleotide NMN Supplementation Rescues Cerebromicrovascular Endothelial Function and Neurovascular Coupling Responses and Improves Cognitive Function in aged Mice Redox Biol 24 101192 doi 10 1016 j redox 2019 101192 Tarantini S Valcarcel Ares M N Yabluchanskiy A Tucsek Z Hertelendy P Kiss T et al 2018 Nrf2 De ciency Exacerbates Obesity Induced Oxidative Stress Neurovascular Dysfunction Blood Brain Barrier Disruption Neuroin ammation Amyloidogenic Gene Expression and Cognitive Decline in Mice Mimicking the Aging Phenotype J Gerontol A Biol Sci Med Sci 73 853 863 doi 10 1093 gerona glx177 Tarantini S Yabluchanksiy A F l p G A Hertelendy P Valcarcel Ares M N Kiss T et al 2017 Pharmacologically Induced Impairment of Neurovascular Coupling Responses alters Gait Coordination in Mice Geroscience 39 601 614 doi 10 1007 s11357 017 0003 x Tarantini S Yabluchanskiy A Csipo T Fulop G Kiss T Balasubramanian P et al 2019 Treatment with the poly ADP Ribose Polymerase Inhibitor PJ 34 Improves Cerebromicrovascular Endothelial Function Neurovascular Coupling Responses and Cognitive Performance in aged Mice Supporting the NAD Depletion Hypothesis of Neurovascular aging Geroscience 41 533 542 doi 10 1007 s11357 019 00101 2 Thom S R Bhopale V Fisher D Manevich Y Huang P L and Buerk D G 2002 Stimulation of Nitric Oxide Synthase in Cerebral Cortex Due to Elevated Partial Pressures of Oxygen an Oxidative Stress Response J Neurobiol 51 85 100 doi 10 1002 neu 10044 Tibbles P M and Edelsberg J S 1996 Hyperbaric oxygen Therapy N Engl J Med 334 1642 1648 doi 10 1056 nejm199606203342506 Tucsek Z Toth P Tarantini S Sosnowska D Gautam T Warrington J P et al 2014 Aging Exacerbates Obesity Induced Cerebromicrovascular Rarefaction Neurovascular Uncoupling and Cognitive Decline in Mice Journals Gerontol Ser A Biol Sci Med Sci 69 1339 1352 doi 10 1093 gerona glu080 Ungvari Z Bagi Z Feher A Recchia F A Sonntag W E Pearson K et al 2010 Resveratrol Confers Endothelial protection via activation of the antioxidant Transcription Factor Nrf2 Am J Physiology Heart Circulatory Physiol 299 H18 H24 doi 10 1152 ajpheart 00260 2010 Ungvari Z Bailey Downs L Gautam T Sosnowska D Wang M Monticone R E et al 2011 Age Associated Vascular Oxidative Stress Nrf2 Dysfunction and NF B Activation in the Nonhuman Primate Macaca mulatta Journals Gerontol Ser A Biol Sci Med Sci 66A 866 875 doi 10 1093 gerona glr092 Ungvari Z Bailey Downs L Sosnowska D Gautam T Koncz P Losonczy G et al 2011 Vascular Oxidative Stress in aging a Homeostatic Failure Due to Dysregulation of NRF2 Mediated antioxidant Response Am J PhysiologyHeart Circulatory Physiol 301 H363 H372 doi 10 1152 ajpheart 01134 2010 Ungvari Z Tarantini S Donato A J Galvan V and Csiszar A 2018 Mechanisms of Vascular Aging Circ Res 123 849 867 doi 10 1161 circresaha 118 311378 Ungvari Z Tarantini S Hertelendy P Valcarcel Ares M N F l p G A Logan S et al 2017 Cerebromicrovascular Dysfunction Predicts Cognitive Decline and Gait abnormalities in a Mouse Model of Whole Frontiers in Aging www frontiersin org Brain Irradiation Induced accelerated Brain Senescence Geroscience 39 33 42 doi 10 1007 s11357 017 9964 z Ungvari Z Tarantini S Kirkpatrick A C Csiszar A and Prodan C I 2017 Cerebral Microhemorrhages Mechanisms Consequences and Prevention Am J Physiology Heart Circulatory Physiol 312 H1128 H1143 doi 10 1152 ajpheart 00780 2016 Ungvari Z Tarantini S Kiss T Wren J D Giles C B Grif n C T et al 2018 Endothelial Dysfunction and angiogenesis Impairment in the ageing Vasculature Nat Rev Cardiol 15 555 565 doi 10 1038 s41569 018 0030 z Vadas D Kalichman L Hadanny A and Efrati S 2017 Hyperbaric Oxygen Environment Can Enhance Brain Activity and Multitasking Performance Front Integr Neurosci 11 25 doi 10 3389 fnint 2017 00025 Valcarcel Ares M N Gautam T Warrington J P Bailey Downs L Sosnowska D de Cabo R et al 2012 Disruption of Nrf2 Signaling Impairs angiogenic Capacity of Endothelial Cells Implications for Microvascular aging Journals Gerontol Ser A Biol Sci Med Sci 67 821 829 doi 10 1093 gerona glr229 Venkateshappa C Harish G Mahadevan A Srinivas Bharath M M and Shankar S K 2012 Elevated Oxidative Stress and Decreased antioxidant Function in the Human hippocampus and Frontal Cortex with Increasing age Implications for Neurodegeneration in Alzheimer s Disease Neurochem Res 37 1601 1614 doi 10 1007 s11064 012 0755 8 Verdin E 2015 NAD in aging Metabolism and Neurodegeneration Science 350 1208 1213 doi 10 1126 science aac4854 Verma R Chopra A Giardina C Sabbisetti V Smyth J A Hightower L E et al 2015 Hyperbaric Oxygen Therapy HBOT Suppresses Biomarkers of Cell Stress and Kidney Injury in Diabetic Mice Cell Stress and Chaperones 20 495 505 doi 10 1007 s12192 015 0574 3 Visser G H Van Hulst R A Wieneke G H and Van Huffelen A C 1996 Transcranial Doppler Sonographic Measurements of Middle Cerebral artery Flow Velocity during Hyperbaric Oxygen Exposures Undersea Hyperb Med 23 157 165 Vrabec J T Clements K S and Mader J T 1998 Short term Tympanostomy in Conjunction with Hyperbaric Oxygen Therapy Laryngoscope 108 1124 1128 doi 10 1097 00005537 199808000 00004 Walker W C Franke L M Cifu D X and Hart B B 2014 Randomized Sham Controlled Feasibility Trial of Hyperbaric Oxygen for Service Members with Postconcussion Syndrome Neurorehabil Neural Repair 28 420 432 doi 10 1177 1545968313516869 Wang F Wang Y Sun T and Yu H l 2016 Hyperbaric Oxygen Therapy for the Treatment of Traumatic Brain Injury a Meta analysis Neurol Sci 37 693 701 doi 10 1007 s10072 015 2460 2 Warrington J P Ashpole N Csiszar A Lee Y W Ungvari Z and Sonntag W E 2013 Whole Brain Radiation Induced Vascular Cognitive Impairment Mechanisms and Implications J Vasc Res 50 445 457 doi 10 1159 000354227 Weaver L K 2014 Hyperbaric Oxygen Therapy Indications 13th edition New York NY Undersea and Hyperbaric Medical Society Weaver L K Churchill S Churchill S Wilson S H Hebert D Deru K et al 2019 A Composite Outcome for Mild Traumatic Brain Injury in Trials of Hyperbaric Oxygen Uhm 46 341 352 doi 10 22462 13 15 2019 11 Weaver L K and Churchill S 2001 Pulmonary Edema associated with Hyperbaric Oxygen Therapy Chest 120 1407 1409 doi 10 1378 chest 120 4 1407 Whalen R E Saltzman H A Holloway D H Jr McIntosh H D Sieker H O and Brown I W Jr 1965 Cardiovascular and Blood Gas Responses to Hyperbaric Oxygenation Am J Cardiol 15 638 646 doi 10 1016 00029149 65 90350 4 Wolf G Cifu D Baugh L Carne W and Profenna L 2012 The Effect of Hyperbaric Oxygen on Symptoms after Mild Traumatic Brain Injury J Neurotrauma 29 2606 2612 doi 10 1089 neu 2012 2549 Xiao Y Wang J Jiang S and Luo H 2012 Hyperbaric Oxygen Therapy for Vascular Dementia Cochrane Database Syst Rev CD009425 doi 10 1002 14651858 CD009425 pub2 Xu Y Wang Q Qu Z Yang J Zhang X and Zhao Y 2019 Protective Effect of Hyperbaric Oxygen Therapy on Cognitive Function in Patients with Vascular Dementia Cel Transpl 28 1071 1075 doi 10 1177 0963689719853540 12 September 2021 Volume 2 Article 678543
Balasubramanian et al HBOT as Human Aging Intervention Zhai W W Sun L Yu Z Q and Chen G 2016 Hyperbaric Oxygen Therapy in Experimental and Clinical Stroke Med Gas Res 6 111 118 doi 10 4103 2045 9912 184721 Zhang J Sam A D Klitzman B and Piantadosi C A 1995 Inhibition of Nitric Oxide Synthase on Brain Oxygenation in anesthetized Rats Exposed to Hyperbaric Oxygen Undersea Hyperb Med 22 377 382 Zhang T Yang Q W Wang S N Wang J Z Wang Q Wang Y et al 2010 Hyperbaric Oxygen Therapy Improves Neurogenesis and Brain Blood Supply in Piriform Cortex in Rats with Vascular Dementia Brain Inj 24 1350 1357 doi 10 3109 02699052 2010 504525 Zhang X Lu A Li Z Sun J Dai D and Qian L 2019 Exosomes Secreted by Endothelial Progenitor Cells Improve the Bioactivity of Pulmonary Microvascular Endothelial Cells Exposed to Hyperoxia In Vitro Ann Transl Med 7 254 doi 10 21037 atm 2019 05 10 Zhou Z Daugherty W P Sun D Levasseur J E Altememi N Hamm R J et al 2007 Protection of Mitochondrial Function and Improvement in Cognitive Recovery in Rats Treated with Hyperbaric Oxygen Following Lateral Fluid Percussion Injury J Neurosurg 106 687 694 doi 10 3171 jns 2007 106 4 687 Yabluchanskiy A Ungvari Z Csiszar A and Tarantini S 2018 Advances and Challenges in Geroscience Research An Update Acta Physiol Hung 105 298 308 doi 10 1556 2060 105 2018 4 32 Yagishita K au fnm Oyaizu T Aizawa J and Enomoto M 2017 The Effects of Hyperbaric Oxygen Therapy on Reduction of Edema and Pain in Athletes with Ankle Sprain in the Acute Phase A Pilot Study Sport Exerc Med Open J 3 10 16 doi 10 17140 semoj 3 141 Yang L Hei M Y Dai J J Hu N and Xiang X Y 2016 Effect of Hyperbaric Oxygenation on Mitochondrial Function of Neuronal Cells in the Cortex of Neonatal Rats after Hypoxic Ischemic Brain Damage Braz J Med Biol Res 49 e5187 doi 10 1590 1414 431X20165187 Yen K Wan J Mehta H H Miller B Christensen A Levine M E et al 2018 Humanin Prevents Age Related Cognitive Decline in Mice and Is Associated with Improved Cognitive Age in Humans Sci Rep 8 14212 doi 10 1038 s41598 018 32616 7 Yilmaz A Kaya N Meric R Bayramli Z Oroglu B Celkan T T et al 2020 Use of Hyperbaric Oxygen Therapy of Purpura Fulminans in an Extremely Low Birth Weight Preterm A Case Report J Neonatal Perinatal Med Online ahead of print doi 10 3233 NPM 20042 You Q Li L Xiong S q Yan Y f Li D Yan N n et al 2019 Meta Analysis on the Ef cacy and Safety of Hyperbaric Oxygen as Adjunctive Therapy for Vascular Dementia Front Aging Neurosci 11 86 doi 10 3389 fnagi 2019 00086 Yu M Yuan H S Li Q Li Q and Teng Y F 2019 Combination of CellsBased Therapy with apelin 13 and Hyperbaric Oxygen Ef ciently Promote Neovascularization in Ischemic animal Model Eur Rev Med Pharmacol Sci 23 2630 2639 doi 10 26355 eurrev_201903_17413 Yu R Wang B Li S Wang J Zhou F Chu S et al 2015 Cognitive Enhancement of Healthy Young adults with Hyperbaric Oxygen A Preliminary Resting State fMRI Study Clin Neurophysiol 126 2058 2067 doi 10 1016 j clinph 2015 01 010 Zamboni W A Roth A C Russell R C Graham B Suchy H and Kucan J O 1993 Morphologic analysis of the Microcirculation during Reperfusion of Ischemic Skeletal Muscle and the Effect of Hyperbaric Oxygen Plast Reconstr Surg 91 1110 1123 doi 10 1097 00006534 199305000 00022 Z rate S C Traetta M E Codagnone M G Seilicovich A and Rein s A G 2019 Humanin a Mitochondrial Derived Peptide Released by Astrocytes Prevents Synapse Loss in Hippocampal Neurons Front Aging Neurosci 11 123 doi 10 3389 fnagi 2019 00123 Frontiers in Aging www frontiersin org Con ict of Interest The authors declare that the research was conducted in the absence of any commercial or nancial relationships that could be construed as a potential con ict of interest Publisher s Note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their af liated organizations or those of the publisher the editors and the reviewers Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher Copyright 2021 Balasubramanian Delfavero Nyul Toth Tarantini Gulej and Tarantini This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY The use distribution or reproduction in other forums is permitted provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited in accordance with accepted academic practice No use distribution or reproduction is permitted which does not comply with these terms 13 September 2021 Volume 2 Article 678543
www aging us com AGING 2020 Vol 12 Advance Research Paper Hyperbaric oxygen therapy increases telomere length and decreases immunosenescence in isolated blood cells a prospective trial Yafit Hachmo1 Amir Hadanny2 3 4 Ramzia Abu Hamed1 Malka Daniel Kotovsky2 Merav Catalogna2 Gregory Fishlev2 Erez Lang2 Nir Polak2 Keren Doenyas2 Mony Friedman2 Yonatan Zemel 2 Yair Bechor2 Shai Efrati1 2 3 5 1 Research and Development Unit Shamir Medical Center Zerifin Israel The Sagol Center for Hyperbaric Medicine and Research Shamir Assaf Harofeh Medical Center Zerifin Israel 3 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 4 Bar Ilan University Ramat Gan Israel 5 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Equal contribution 2 Correspondence to Amir Hadanny Shai Efrati email hadannya shamir gov il efratishai outlook com https orcid org 0000 0001 5523 999X Keywords telomere senescence aging hyperbaric oxygen length Received September 3 2020 Accepted October 22 2020 Published November 18 2020 Copyright 2020 Yafit et al This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY 3 0 which permits unrestricted use distribution and reproduction in any medium provided the original author and source are credited ABSTRACT Introduction Aging is characterized by the progressive loss of physiological capacity At the cellular level two key hallmarks of the aging process include telomere length TL shortening and cellular senescence Repeated intermittent hyperoxic exposures using certain hyperbaric oxygen therapy HBOT protocols can induce regenerative effects which normally occur during hypoxia The aim of the current study was to evaluate whether HBOT affects TL and senescent cell concentrations in a normal non pathological aging adult population Methods Thirty five healthy independently living adults aged 64 and older were enrolled to receive 60 daily HBOT exposures Whole blood samples were collected at baseline at the 30th and 60th session and 1 2 weeks following the last HBOT session Peripheral blood mononuclear cells PBMCs telomeres length and senescence were assessed Results Telomeres length of T helper T cytotoxic natural killer and B cells increased significantly by over 20 following HBOT The most significant change was noticed in B cells which increased at the 30th session 60th session and post HBOT by 25 68 40 42 p 0 007 29 39 23 39 p 0 0001 and 37 63 52 73 p 0 007 respectively There was a significant decrease in the number of senescent T helpers by 37 30 33 04 post HBOT P
examined HBOT s effects on TL and senescent cell accumulation Telomeres are tandem nucleotide repeats located at the end of the chromosomes which maintain genomic stability Telomeres shorten during replication mitosis due to the inherent inability to fully replicate the end part of the lagging DNA strand 2 Telomere length TL measuring between 4 to 15 kilobases gradually shorten by 20 40 bases per year and is associated with different diseases low physical performance and cortical thinning of the brain 3 5 When TL reaches a critical length cells cannot replicate and progress to senescence or programmed cell death 6 Goglin et al demonstrated that adults with shorter TLs have increased mortality rates 7 Shortened TLs can be a direct inherited trait but several environmental factors have also been associated with shortening TL including stress lack of physical endurance activity excess body mass index smoking chronic inflammation vitamins deficiency and oxidative stress 2 8 9 The aim of the current study was to evaluate whether HBOT affects TL and senescence like T cells population in aging adults RESULTS Thirty five individuals were assigned to HBOT Five patients did not complete baseline assessments and were excluded All 30 patients who completed baseline evaluations completed the interventions Due to the low quality of blood samples low number of cells or technician error four patients were excluded from the telomere analysis and 10 patients from senescent cell analysis Figure 1 The baseline characteristics and comparison of the cohorts following exclusion of the patients are provided in Table 1 There were no significant differences between the three groups Table 1 Cellular senescence is an arrest of the cell cycle which can be caused by telomere shortening 10 as well as other aging associated stimuli independent of TL such as non telomeric DNA damage 1 The primary purpose of senescence is to prevent propagation of damaged cells by triggering their elimination via the immune system The accumulation of senescent cells with aging reflects either an increase in the generation of these cells and or a decrease in their clearance which in turn aggravates the damage and contributes to aging 1 Telomere length Compared to the baseline the T helper telomere lengths were significantly increased at the 30th session and postHBOT by 21 70 40 05 p 0 042 23 69 39 54 p 0 012 and 29 30 38 51 p 0 005 respectively Figure 2 However repeated measures analysis shows a non significant trend F 4 663 p 0 06 Table 2 and Figure 2 A growing body of research has found several pharmacological agents that can reduce the telomere shortening rate 11 12 Several lifestyle interventions including endurance training diets and supplements targeting cell metabolism and oxidative stress have reported relatively small effects 2 5 on TL3 2 8 9 Compared to baseline telomere lengths of B cells increased significantly at the 30th session 60th session and post HBOT by 25 68 40 42 p 0 007 29 39 23 39 p 0 0001 and 37 63 52 73 p 0 007 respectively Figure 2 Repeated measures analysis shows a significant within group effect F 0 390 p 0 017 Table 2 and Figure 2 Hyperbaric oxygen therapy HBOT utilizes 100 oxygen in an environmental pressure higher than one absolute atmospheres ATA to enhance the amount of oxygen dissolved in body s tissues Repeated intermittent hyperoxic exposures using certain HBOT protocols can induce physiological effects which normally occur during hypoxia in a hyperoxic environment the so called hyperoxic hypoxic paradox 13 16 In addition it was recently demonstrated that HBOT can induce cognitive enhancements in healthy aging adults via mechanisms involving regional changes in cerebral blood flow 17 On the cellular level it was demonstrated that HBOT can induce the expression of hypoxia induced factor HIF vascular endothelial growth factor VEGF and sirtuin SIRT stem cell proliferation mitochondrial biogenesis angiogenesis and neurogenesis 18 However no study to date has Compared to baseline natural killer cells telomer lengths significantly increased at the 30th session p 0 045 and at the 60th session by 20 56 33 35 p 0 013 Post HBOT telomere lengths increased by 22 16 44 81 post HBOT p 0 06 Table 2 and Figure 2 Repeated measures analysis indicates that there was no additional significant effect after the 30th session F 0 812 p 0 391 www aging us com Compared to baseline cytotoxic T cells had a nonsignificant increase at the 30th session by 18 29 45 62 p 0 11 followed by a significant increase of 24 13 40 88 at the 60th session p 0 0019 and 19 59 33 98 post HBOT p 0 023 Repeated measures analysis indicates that there was no additional significant effect after the 30th session F 1 159 p 0 310 Table 2 and Figure 2 2 AGING
Senescent cells telomere length by more than 20 in an aging population with B cells having the most striking change In addition HBOT decreased the number of senescent cells by 10 37 with T helper senescent cells being the most effected There was a non significant decrease in the number of senescent T helpers at the 30th session and 60th session by 19 66 80 03 p 0 09 and 11 67 94 30 p 0 20 respectively However there was a significant drop in the number of senescent T helpers by 37 30 33 04 postHBOT P
Table 1 Baseline characteristics HBOT N Age years BMI Males Females Complete blood count Hemoglobin White blood cells PBMC Platelets Telomere analysis Senescent analysis P value 30 25 83 3 20 66 6 68 41 13 2 67 56 14 35 66 70 16 00 0 917 26 77 3 20 26 89 3 34 27 14 3 81 0 946 16 53 3 13 52 0 10 50 0 0 987 14 47 7 12 48 0 10 50 0 0 987 6 33 1 25 6 57 1 15 6 58 1 29 0 707 14 02 1 40 13 92 1 35 13 97 1 49 0 969 39 96 6 75 39 25 6 64 38 59 6 63 0 774 239 87 1 39 244 08 43 0 254 05 41 4 0 559 4 13 3 4 16 0 2 10 0 0 841 4 13 3 4 16 0 3 15 8 0 956 4 13 3 4 16 0 3 15 0 0 961 1 3 3 1 4 0 0 0 680 7 23 3 5 20 0 6 30 0 0 733 3 10 2 8 0 2 10 0 0 961 5 16 7 5 20 0 4 20 0 0 936 1 3 3 0 1 5 0 0 561 7 23 3 4 16 0 5 25 0 0 755 Chronic medical conditions Atrial fibrillation Hypothyroidism Obstructive sleep apnea Asthma BPH GERD Osteoporosis Rheumatic arthritis Osteoarthritis Diabetes mellitus Hypertension Dyslipidemia Ischemic heart disease History of smoking 3 10 3 12 0 2 10 0 0 966 7 23 3 5 20 0 5 25 0 0 918 16 53 3 14 56 0 12 60 0 0 897 2 6 7 1 4 0 2 10 0 0 725 10 33 3 8 32 0 7 35 0 0 978 8 26 7 6 24 0 5 25 0 0 974 Chronic medications Anti aggregation ACE Inhibitors ARB blockers Beta blockers Calcium blockers Alpha blockers Diuretics Statins Oral hypoglycemic Bisphosphonates Proton pump inhibitors Hormones Benzodiazepines SSRI reactive oxygen species ROS and cellular scavengers Telomeres are highly sensitive to oxidative DNA damage which can induce telomere shortening and dysfunction 26 The association between oxygen www aging us com 6 20 6 24 0 6 30 0 0 720 5 16 7 5 20 0 3 15 0 0 901 3 10 3 12 0 2 10 0 0 966 7 23 3 5 20 0 6 30 0 0 733 2 6 7 1 4 0 1 5 0 0 906 10 33 3 9 36 0 7 35 0 0 978 1 3 3 1 4 0 1 5 0 0 958 1 3 3 1 4 0 1 5 0 0 958 3 10 3 12 0 3 15 0 0 726 3 10 3 12 0 2 10 0 0 966 3 10 2 8 0 1 5 0 0 816 5 16 7 5 20 0 3 15 0 0 990 and or oxidative stress and telomere length has been debated for the past several decades Human cell culture studies consistently show that mild oxidative stress accelerates telomere shortening whereas antioxidants 4 AGING
and free radical scavengers decrease shortening rates and increase the cellular proliferative lifespan 27 Several clinical studies on pathological conditions such as diabetes inflammatory diseases Parkinson s disease have shown correlations between oxidative stress markers reactive oxygen species scavengers levels and telomere length 28 However healthy individuals did not show similar results 29 longer than the T1 2 of ROS upon return to normoxia following repeated hyperoxic exposures there are significantly higher levels of scavengers and increased antioxidant activity 13 18 Thus similar to physical exercise and caloric restriction a daily repeated HBOT protocol can induce the hormesis phenomenon Single exposures increase ROS generation acutely triggering the antioxidant response and with repeated exposures the response becomes protective 13 18 Exposing cell cultures to a hyperbaric environment has been previously suggested to induce significant oxidative stress and premature cells senescence 30 However this was based on isolated cells grown in a hyperbaric incubator and not on the complex biological system of humans as in this study Similar to the current study a previous prospective one year observational study in divers exposed to intense hyperbaric oxygen showed significant telomere elongation in leukocytes 31 As used in the current study the HBOT protocol utilizes the effects induced by repeated intermittent hyperoxic exposures the so called hyperoxic hypoxic paradox 13 18 These intermittent hyperoxic exposures induce an adaptive response which includes increased upregulation of antioxidants genes 32 and production of antioxidants scavengers that adjust to the increased ROS generation causing the ROS scavenger ratio to gradually becomes similar to the ratio under a normal oxygen environment However because the scavenger elimination half life T1 2 is significantly Additionally intermittent hyperoxic exposures induce many of the physiological responses that occur during hypoxia 13 HBOT induces the release of transcription factors called hypoxic induced factors HIF and increase their stability and activity 14 In turn HIF induces a cellular cascade including vascular endothelial growth factor and angiogenesis induction mitochondria biogenesis stem cells mobilization and SIRT1 increased activity 18 Our study confirms increased HIF expression is induced by repetitive HBOT exposures which gradually decreases towards normalization of HIF levels at nonmonic environment Currently many interventions that genetically or pharmacologically senolytic drugs remove senescent cells have been developed in animal models and are waiting for safety and efficacy evaluations in humans 33 The current study suggests a non pharmacological method clinically available with well established safety Figure 2 Telomere length changes with HBOT Mean SEM p
Table 2 Telomere length and senescent cell changes post HBOT Absolute changes Baseline 30th Session 60th Session Repeated measures Relative changes Post HBOT 30th session 60th session Post HBOT F p PBMC PBMC N 25 2 55 0 53 0 15 0 40 4 91 16 70 1 987 t 0 09 PBMC N 20 2 50 0 53 0 13 0 31 4 21 11 99 1 810 t 0 07 Relative telomeres length N 25 Natural killer 9 27 1 91 11 77 5 14 0 045 10 73 2 73 0 013 11 75 4 22 0 06 25 02 51 42 20 56 33 35 22 16 44 81 0 812 0 391 B cells 8 36 2 02 10 22 3 04 0 007 11 23 3 58 0 0001 11 17 2 98 0 007 25 68 40 42 29 39 23 39 37 63 52 73 7 390 0 017 T Helper 8 04 1 82 9 92 3 68 0 042 9 63 2 17 0 012 10 20 2 77 0 005 21 70 40 05 23 69 39 54 29 30 38 51 4 663 0 063 T Cytotoxic 8 26 1 54 9 83 4 08 0 11 10 08 3 33 0 019 10 15 2 74 0 023 18 29 45 62 24 13 40 88 19 59 33 98 1 159 0 310 Senescent cells of T cells N 20 T Helper 10 29 5 42 7 84 7 09 0 09 8 51 7 45 0 20 6 22 4 88
MATERIALS AND METHODS profile for senescent cells populations decrease Our protocol included 60 sessions of 100 oxygen at 2 ATA including three air breaks during each session to utilize the hyperoxic hypoxic paradox and minimize the risk of oxygen toxicity Interestingly both TL and senescent cell reduction peaked at the 30th session However the dose response curve related to the applied pressure time and number of HBOT exposures and its relation to HIF expression and its related regenerative effects are still not fully understood and further studies are needed to find the optimal HBOT protocols Subjects Thirty five adults without pathological cognitive declines aged 64 and older who lived independently in good functional and cognitive status were enrolled The study was performed between 2016 2020 in the Shamir Assaf Harofeh Medical Center Israel Included patients did not have cardiac or cerebrovascular ischemia histories for the last year prior to inclusion Exclusion criteria included previous treatment with HBOT for any reason during the last three months any history of malignancy during the last year any pathological cognitive decline severe chronic renal failure GFR 8 fasting glucose 200 immunosuppressants MRI contraindications including BMI 35 active smoking or pulmonary diseases Hyperbaric oxygen therapy is a well established treatment modality for non healing wounds radiation injuries as well as different hypoxic or ischemic events such as carbon monoxide toxicity infections etc In recent years a growing evidence from pre clinical as well as clinical trials demonstrate the efficacy of HBOT for neurological indications including idiopathic sudden sensorineural hearing loss 34 post stroke and post traumatic brain injury 35 41 central sensitization syndrome such as fibromyalgia syndrome 42 43 and age related cognitive decline 17 and animal models of Alzheimer s disease 44 For the first time the current study aimed to evaluate the physiological effect on the cellular level in aging humans without any functional limiting disease Study design The study protocol was approved by Institutional Review Board of the Shamir Medical Center Israel The study was performed as a prospective clinical trial After signing an informed consent and undergoing a baseline evaluation the subjects were assigned to HBOT Measurement points were evaluated at baseline half point of the treatment protocol 30th session the day of the last HBOT session and 1 2 weeks after the HBOT Study limitations The current study has several limitations and strengths to consider First the limited sample size has to be taken into account Second the lack of control group However the study suggests impressive results on TL and senescent cell clearance which weren t observed in other interventions Moreover the baseline telomere length values of our cohort match the expected values for the aging population 45 47 Third the duration of the effect has yet to be determined in long term follow ups Fourth telomerase activity was not evaluated due to the method chosen for blood preservation and evaluation Nevertheless several strengths should be stressed In this study CD28 was used as a biomarker for senescent cells whereas CD57 was not available as a confirmatory marker for T cell senescence Biomarkers were assessed on specific leukocytes populations rather than using the entire PBMCs as one group The isolated HBOT effect was measured and participants were monitored for not making any lifestyle changes such as nutrition and exercise medications or any other intervention that may have acted as possible confounders The study cohort included only patients treated by HBOT which is part of a larger cohort of normal ageing population studied at the Shamir medical center Israel NCT02790541 17 Interventions The HBOT protocol was administrated in a Multiplace Starmed 2700 chamber HAUX Germany The protocol comprised of 60 daily sessions five sessions per week within a three month period Each session included breathing 100 oxygen by mask at 2ATA for 90 minutes with 5 minute air breaks every 20 minutes Compression decompression rates were 1 meter minute During the trial neither lifestyle and diet changes nor medications adjustments were allowed Blood samples Whole blood samples were collected into EDTA tubes using a standard technique at baseline at the half point of the HBOT protocol 30th session the day of the last HBOT session 60th session and 1 2 weeks following the last HBOT session In summary the study indicates that HBOT can induce significant senolytic effects including significant increased telomere length and clearance of senescent cells in aging populations www aging us com 7 AGING
Peripheral isolation blood mononuclear cells PBMCs analysis the relative telomere length RTL was calculated for CD3 CD4 T helper CD3 CD8 Tcytotoxic CD3 CD56 natural killer and CD19 B cells The RTL value was calculated as the ratio between the telomere signal of each sample and the control cell TCL 1301 cell line with correction for the DNA index of G0 1 cells Sample cells and control cells were analyzed separately for DNA ploidy using propidium iodide staining to standardize the number of telomere ends per cell and thereby telomere length per chromosome See Figure 4 for FACS analysis example Whole blood was diluted using phosphate buffered saline PBS Density gradient separation was performed using Leucosep tubes filled with Lymphoprep The tubes were then centrifuged at 1000 g for 10 min at 25 C degrees Following centrifugation the cell layers buffy coat were immediately collected via pipette and transferred to 50 mL conical centrifuge tubes resuspended with sufficient 1X PBS to a volume of 50 mL and centrifuged at 300 g for 10 min at 25 C degrees Following removal of the supernatant each sample was labeled Immunophenotyping Percentages of CD3 CD4 CD28 null T cells senescent T helpers and CD3 CD8 CD28 null T cells senescent T cytotoxics were determined by flow cytometric analysis PBMC were stained with VioBlue conjugated anti CD3 Viogreen conjugated anti CD8 PE VIO 770A conjugated anti CD4 and APC VIO 770A anti CD28 antibodies Miltenyi Biotec Cells were analyzed with a MACSQuant Flow Cytometer Miltenyi Biotec The percentage of CD28null T cells within the CD4 or CD8 T cell population was then calculated Telomere length Telomeres were labelled according to the Dako PNA FITC kit protocol Code K5327 On a single cell suspension consisting of a mixture of PBMCs sample cells and TCL 1301 cell line control cells the DNA was denatured for 10 minutes at 82 C in a microcentrifuge tube either in the presence of hybridization solution without probe or in hybridization solution containing the fluorescein conjugated PNA telomere probe The hybridization took place in the dark at room temperature RT overnight The hybridization was followed by two 10 minute post hybridization washes with a wash solution at 40 C The sample was then labeled with CD4 CD8 CD3 CD19 and CD56 conjugated antibodies in an appropriate buffer for further flow cytometric analysis 48 49 Each sample was run in duplicate Following flow cytometric Hypoxia induced factor HIF 1alpha Intracellular HIF1a staining was performed with APC conjugated anti HIF1a antibody or corresponding Isotype Control R D systems following fixation and permeabilization Life Technologies Cells were analyzed with a MACSQuant Flow Cytometer Miltenyi Biotec and the percentage of HIF1a expressing PBMCs was determined Figure 4 Example of Flow Fish data analysis of T helper subpopulation Each blood sample was either stained with PNA probe b or without a following by antibodies staining CD3 CD4 CD8 CD16 CD19 before data acquisition www aging us com 8 AGING
Statistical analysis Unless otherwise specified continuous data were expressed as means standard deviation The normal distribution for all variables was tested using the Kolmogorov Smirnov test One way ANOVA was performed to compare variables between and within the three groups at baseline 2 Tsoukalas D Fragkiadaki P Docea AO Alegakis AK Sarandi E Vakonaki E Salataj E Kouvidi E Nikitovic D Kovatsi L Spandidos DA Tsatsakis A Calina D Association of nutraceutical supplements with longer telomere length Int J Mol Med 2019 44 218 26 https doi org 10 3892 ijmm 2019 4191 PMID 31115552 3 Starkweather AR Alhaeeri AA Montpetit A Brumelle J Filler K Montpetit M Mohanraj L Lyon DE JacksonCook CK An integrative review of factors associated with telomere length and implications for biobehavioral research Nurs Res 2014 63 36 50 https doi org 10 1097 NNR 0000000000000009 PMID 24335912 4 Puhlmann LM Valk SL Engert V Bernhardt BC Lin J Epel ES Vrticka P Singer T Association of short term change in leukocyte telomere length with cortical thickness and outcomes of mental training among healthy adults a randomized clinical trial JAMA Netw Open 2019 2 e199687 https doi org 10 1001 jamanetworkopen 2019 9687 PMID 31553468 5 str m MJ von Bonsdorff MB Per l MM Salonen MK Rantanen T Kajantie E Simonen M Pohjolainen P Haapanen MJ Guzzardi MA Iozzo P Kautiainen H Eriksson JG Telomere length and physical performance among older people the helsinki birth cohort study Mech Ageing Dev 2019 183 111145 https doi org 10 1016 j mad 2019 111145 PMID 31491428 6 Xie Z Jay KA Smith DL Zhang Y Liu Z Zheng J Tian R Li H Blackburn EH Early telomerase inactivation accelerates aging independently of telomere length Cell 2015 160 928 39 https doi org 10 1016 j cell 2015 02 002 PMID 25723167 7 Goglin SE Farzaneh Far R Epel ES Lin J Blackburn EH Whooley MA Change in leukocyte telomere length predicts mortality in patients with stable coronary heart disease from the heart and soul study PLoS One 2016 11 e0160748 https doi org 10 1371 journal pone 0160748 PMID 27783614 8 Armanios M Telomeres and age related disease how telomere biology informs clinical paradigms J Clin Invest 2013 123 996 1002 https doi org 10 1172 JCI66370 PMID 23454763 9 Richards JB Valdes AM Gardner JP Paximadas D Kimura M Nessa A Lu X Surdulescu GL Swaminathan R Spector TD Aviv A Higher serum vitamin D concentrations are associated with longer leukocyte telomere length in women Am J Clin Nutr 2007 86 1420 25 Categorical data is expressed in numbers and percentages and compared by chi square tests Univariate analyses were performed using Chi Square Fisher s exact test to identify significant variables P
https doi org 10 1093 ajcn 86 5 1420 PMID 17991655 17 Hadanny A Daniel Kotovsky M Suzin G Boussi Gross R Catalogna M Dagan K Hachmo Y Abu Hamed R Sasson E Fishlev G Lang E Polak N Doenyas K et al Cognitive enhancement of healthy older adults using hyperbaric oxygen a randomized controlled trial Aging Albany NY 2020 12 13740 61 https doi org 10 18632 aging 103571 PMID 32589613 10 Bodnar AG Ouellette M Frolkis M Holt SE Chiu CP Morin GB Harley CB Shay JW Lichtsteiner S Wright WE Extension of life span by introduction of telomerase into normal human cells Science 1998 279 349 52 https doi org 10 1126 science 279 5349 349 PMID 9454332 18 Hadanny A Efrati S The hyperoxic hypoxic paradox Biomolecules 2020 10 958 https doi org 10 3390 biom10060958 PMID 32630465 11 Townsley DM Dumitriu B Liu D Biancotto A Weinstein B Chen C Hardy N Mihalek AD Lingala S Kim YJ Yao J Jones E Gochuico BR et al Danazol treatment for telomere diseases N Engl J Med 2016 374 1922 31 https doi org 10 1056 NEJMoa1515319 PMID 27192671 19 Freitas Simoes TM Cof n M Blasco MA Sober n N Foronda M Serra Mir M Roth I Valls Pedret C Dom nech M Ponferrada Ariza E Calvo C Rajaram S Sabat J et al Walnut consumption for two years and leukocyte telomere attrition in mediterranean elders results of a randomized controlled trial Nutrients 2018 10 1907 https doi org 10 3390 nu10121907 PMID 30518050 12 Coutts F Palmos AB Duarte RR de Jong S Lewis CM Dima D Powell TR The polygenic nature of telomere length and the anti ageing properties of lithium Neuropsychopharmacology 2019 44 757 65 https doi org 10 1038 s41386 018 0289 0 PMID 30559463 20 Dimauro I Scalabrin M Fantini C Grazioli E Beltran Valls MR Mercatelli N Parisi A Sabatini S Di Luigi L Caporossi D Resistance training and redox homeostasis correlation with age associated genomic changes Redox Biol 2016 10 34 44 https doi org 10 1016 j redox 2016 09 008 PMID 27687219 13 Cimino F Balestra C Germonpr P De Bels D Tillmans F Saija A Speciale A Virgili F Pulsed high oxygen induces a hypoxic like response in human umbilical endothelial cells and in humans J Appl Physiol 1985 2012 113 1684 89 https doi org 10 1152 japplphysiol 00922 2012 PMID 23042909 21 Werner CM Hecksteden A Morsch A Zundler J Wegmann M Kratzsch J Thiery J Hohl M Bittenbring JT Neumann F B hm M Meyer T Laufs U Differential effects of endurance interval and resistance training on telomerase activity and telomere length in a randomized controlled study Eur Heart J 2019 40 34 46 https doi org 10 1093 eurheartj ehy585 PMID 30496493 14 Sunkari VG Lind F Botusan IR Kashif A Liu ZJ Yl Herttuala S Brismar K Velazquez O Catrina SB Hyperbaric oxygen therapy activates hypoxia inducible factor 1 HIF 1 which contributes to improved wound healing in diabetic mice Wound Repair Regen 2015 23 98 103 https doi org 10 1111 wrr 12253 PMID 25532619 22 Sanft T Usiskin I Harrigan M Cartmel B Lu L Li FY Zhou Y Chagpar A Ferrucci LM Pusztai L Irwin ML Randomized controlled trial of weight loss versus usual care on telomere length in women with breast cancer the lifestyle exercise and nutrition LEAN study Breast Cancer Res Treat 2018 172 105 12 https doi org 10 1007 s10549 018 4895 7 PMID 30062572 15 Milovanova TN Bhopale VM Sorokina EM Moore JS Hunt TK Hauer Jensen M Velazquez OC Thom SR Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo J Appl Physiol 1985 2009 106 711 28 https doi org 10 1152 japplphysiol 91054 2008 PMID 19023021 23 Mason C Risques RA Xiao L Duggan CR Imayama I Campbell KL Kong A Foster Schubert KE Wang CY Alfano CM Blackburn GL Rabinovitch PS McTiernan A Independent and combined effects of dietary weight loss and exercise on leukocyte telomere length in postmenopausal women Obesity Silver Spring 2013 21 E549 54 https doi org 10 1002 oby 20509 PMID 23640743 16 Yang Y Wei H Zhou X Zhang F Wang C Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor extracellular signal regulated kinase signaling after traumatic brain injury Neuroreport 2017 28 1232 38 https doi org 10 1097 WNR 0000000000000901 PMID 28953090 www aging us com 10 AGING
24 Krishna BH Keerthi GS Kumar CK Reddy NM Association of leukocyte telomere length with oxidative stress in yoga practitioners J Clin Diagn Res 2015 9 CC01 03 https doi org 10 7860 JCDR 2015 13076 5729 PMID 25954614 antioxidant gene expression Ann N Y Acad Sci 2010 1197 178 83 https doi org 10 1111 j 1749 6632 2009 05393 x PMID 20536847 33 Pignolo RJ Passos JF Khosla S Tchkonia T Kirkland JL Reducing senescent cell burden in aging and disease Trends Mol Med 2020 26 630 38 https doi org 10 1016 j molmed 2020 03 005 PMID 32589933 25 Tehfe M Dowden S Kennecke H El Maraghi R Lesperance B Couture F Letourneau R Liu H Romano A Erratum to nab paclitaxel plus gemcitabine versus gemcitabine in patients with metastatic pancreatic adenocarcinoma canadian subgroup analysis of the phase 3 MPACT trial Adv Ther 2017 34 277 79 https doi org 10 1007 s12325 016 0442 2 PMID 27885491 34 LE W Hyperbaric Oxygen Therapy Indications UHMS 2008 12th edition 215 218 35 Boussi Gross R Golan H Fishlev G Bechor Y Volkov O Bergan J Friedman M Hoofien D Shlamkovitch N Ben Jacob E Efrati S Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 2013 8 e79995 https doi org 10 1371 journal pone 0079995 PMID 24260334 26 Barnes RP Fouquerel E Opresko PL The impact of oxidative DNA damage and stress on telomere homeostasis Mech Ageing Dev 2019 177 37 45 https doi org 10 1016 j mad 2018 03 013 PMID 29604323 27 von Zglinicki T Oxidative stress shortens telomeres Trends Biochem Sci 2002 27 339 44 https doi org 10 1016 s0968 0004 02 02110 2 PMID 12114022 36 Efrati S Fishlev G Bechor Y Volkov O Bergan J Kliakhandler K Kamiager I Gal N Friedman M BenJacob E Golan H Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS One 2013 8 e53716 https doi org 10 1371 journal pone 0053716 PMID 23335971 28 Sampson MJ Winterbone MS Hughes JC Dozio N Hughes DA Monocyte telomere shortening and oxidative DNA damage in type 2 diabetes Diabetes Care 2006 29 283 89 https doi org 10 2337 diacare 29 02 06 dc05 1715 PMID 16443874 37 Mukherjee A Raison M Sahni T Arya A Lambert J Marois P James PB Parent A Ballaz L Intensive rehabilitation combined with HBO2 therapy in children with cerebral palsy a controlled longitudinal study Undersea Hyperb Med 2014 41 77 85 PMID 24851544 29 Reichert S Stier A Does oxidative stress shorten telomeres in vivo a review Biol Lett 2017 13 20170463 https doi org 10 1098 rsbl 2017 0463 PMID 29212750 38 Hadanny A Golan H Fishlev G Bechor Y Volkov O Suzin G Ben Jacob E Efrati S Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restor Neurol Neurosci 2015 33 471 86 https doi org 10 3233 RNN 150517 PMID 26409406 30 Oh S Lee E Lee J Lim Y Kim J Woo S Comparison of the effects of 40 oxygen and two atmospheric absolute air pressure conditions on stress induced premature senescence of normal human diploid fibroblasts Cell Stress Chaperones 2008 13 447 58 https doi org 10 1007 s12192 008 0041 5 PMID 18465208 39 Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E Efrati S Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 2015 33 943 51 https doi org 10 3233 RNN 150585 PMID 26484702 31 Shlush LI Skorecki KL Itzkovitz S Yehezkel S Segev Y Shachar H Berkovitz R Adir Y Vulto I Lansdorp PM Selig S Telomere elongation followed by telomere length reduction in leukocytes from divers exposed to intense oxidative stress implications for tissue and organismal aging Mech Ageing Dev 2011 132 123 30 https doi org 10 1016 j mad 2011 01 005 PMID 21320523 40 Hadanny A Rittblat M Bitterman M May Raz I Suzin G Boussi Gross R Zemel Y Bechor Y Catalogna M Efrati S Hyperbaric oxygen therapy improves neurocognitive functions of post stroke patients a retrospective analysis Restor Neurol Neurosci 2020 38 93 107 https doi org 10 3233 RNN 190959 PMID 31985478 32 Godman CA Joshi R Giardina C Perdrizet G Hightower LE Hyperbaric oxygen treatment induces www aging us com 11 AGING
41 Tal S Hadanny A Sasson E Suzin G Efrati S Hyperbaric oxygen therapy can induce angiogenesis and regeneration of nerve fibers in traumatic brain injury patients Front Hum Neurosci 2017 11 508 https doi org 10 3389 fnhum 2017 00508 PMID 29097988 45 Steenstrup T Kark JD Verhulst S Thinggaard M Hjelmborg JV Dalg rd C Kyvik KO Christiansen L Mangino M Spector TD Petersen I Kimura M Benetos A et al Telomeres and the natural lifespan limit in humans Aging Albany NY 2017 9 1130 42 https doi org 10 18632 aging 101216 PMID 28394764 42 Efrati S Golan H Bechor Y Faran Y Daphna Tekoah S Sekler G Fishlev G Ablin JN Bergan J Volkov O Friedman M Ben Jacob E Buskila D Hyperbaric oxygen therapy can diminish fibromyalgia syndrome prospective clinical trial PLoS One 2015 10 e0127012 https doi org 10 1371 journal pone 0127012 PMID 26010952 46 Shammas MA Telomeres lifestyle cancer and aging Curr Opin Clin Nutr Metab Care 2011 14 28 34 https doi org 10 1097 MCO 0b013e32834121b1 PMID 21102320 47 Teubel I Elchinova E Roura S Fern ndez MA G lvezMont n C Moliner P de Antonio M Lup n J Bay sGen s A Telomere attrition in heart failure a flow FISH longitudinal analysis of circulating monocytes J Transl Med 2018 16 35 https doi org 10 1186 s12967 018 1412 z PMID 29463269 43 Hadanny A Bechor Y Catalogna M Daphna Tekoah S Sigal T Cohenpour M Lev Wiesel R Efrati S Hyperbaric oxygen therapy can induce neuroplasticity and significant clinical improvement in patients suffering from fibromyalgia with a history of childhood sexual abuse randomized controlled trial Front Psychol 2018 9 2495 https doi org 10 3389 fpsyg 2018 02495 PMID 30618929 48 Baerlocher GM Lansdorp PM Telomere length measurements in leukocyte subsets by automated multicolor flow FISH Cytometry A 2003 55 1 6 https doi org 10 1002 cyto a 10064 PMID 12938182 49 Baerlocher GM Lansdorp PM Telomere length measurements using fluorescence in situ hybridization and flow cytometry Methods Cell Biol 2004 75 719 50 https doi org 10 1016 s0091 679x 04 75031 1 PMID 15603450 44 Shapira R Efrati S Ashery U Hyperbaric oxygen therapy as a new treatment approach for Alzheimer s disease Neural Regen Res 2018 13 817 18 https doi org 10 4103 1673 5374 232475 PMID 29863011 www aging us com 12 AGING
93 Restorative Neurology and Neuroscience 38 2020 93 107 DOI 10 3233 RNN 190959 IOS Press Hyperbaric oxygen therapy improves neurocognitive functions of post stroke patients a retrospective analysis Amir Hadannya b c e Mor Rittblatb Mor Bittermanb Ido May Razb Gil Suzinb Rahav Boussi Grossb Yonatan Zemelb Yair Bechorb Merav Catalognab and Shai Efratib d e f a Neurosurgery Department Galilee Medical Center Naharyia Israel Center for Hyperbaric Medicine and Research Assaf Harofeh Medical Center Zeri n Israel c Galilee Faculty of Medicine Bar Ilan University Israel d Research and Development Unit Assaf Harofeh Medical Center Zeri n Israel e Sackler School of Medicine Tel Aviv University Tel Aviv Israel f Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel b Sagol Abstract Background Previous studies have shown that hyperbaric oxygen therapy HBOT can improve the motor functions and memory of post stroke patients in the chronic stage Objective The aim of this study is to evaluate the effects of HBOT on overall cognitive functions of post stroke patients in the chronic stage The nature type and location of the stroke were investigated as possible modifiers Methods A retrospective analysis was conducted on patients who were treated with HBOT for chronic stroke 3 months between 2008 2018 Participants were treated in a multi place hyperbaric chamber with the following protocols 40 to 60 daily sessions 5 days per week each session included 90 min of 100 oxygen at 2 ATA with 5 min air brakes every 20 minutes Clinically significant improvements CSI were defined as 0 5 standard deviation SD Results The study included 162 patients 75 3 males with a mean age of 60 75 12 91 Of them 77 47 53 had cortical strokes 87 53 7 strokes were located in the left hemisphere and 121 suffered ischemic strokes 74 6 HBOT induced a significant increase in all the cognitive function domains p 0 05 with 86 of the stroke victims achieving CSI There were no significant differences post HBOT of cortical strokes compared to sub cortical strokes p 0 05 Hemorrhagic strokes had a significantly higher improvement in information processing speed post HBOT p 0 05 Left hemisphere strokes had a higher increase in the motor domain p 0 05 In all cognitive domains the baseline cognitive function was a significant predictor of CSI p 0 05 while stroke type location and side were not significant predictors Conclusions HBOT induces significant improvements in all cognitive domains even in the late chronic stage The selection of post stroke patients for HBOT should be based on functional analysis and baseline cognitive scores rather than the stroke type location or side of lesion Keywords HBOT stroke cognitive function hyperbaric oxygen 1 Introduction Corresponding author Amir Hadanny Sagol Center for Hyperbaric Medicine and Research Assaf Harofeh Medical Center Zerifin Israel Tel 972 8 9779395 E mail Amir had gmail com Stroke is the second most cause of mortality and the third leading cause for disability worldwide Langhorne Bernhardt Kwakkel 2011 Lozano et al 2012 Ojaghihaghighi Vahdati Mikaeilpour Ramouz 2017 Ottenbacher Jannell 1993 Powers 0922 6028 20 35 00 2020 IOS Press and the authors All rights reserved This article is published online with Open Access and distributed under the terms of the Creative Commons Attribution Non Commercial License CC BY NC 4 0
94 A Hadanny et al HBOT cognitive effect in post stroke patients et al 2018 When strokes transpire whether they are ischemic or hemorrhagic the injured brain region correlates with its related loss of function which may be visual motor sensory or cognitive impairments Most stroke studies focus on motor functions However it is estimated that nearly half of the survivors suffer from different degrees of cognitive dysfunction Kelly Hayes et al 2003 Lee Joshi Wang Pashos Christensen 2007 Yoneda et al 2005 The two leading subtypes of stroke are ischemic stroke in 68 of the cases and the less frequent hemorrhagic stroke in 32 of the cases Caplan 1989 Krishnamurthi et al 2013 Powers et al 2018 Zhang Lo Mychaskiw Colohan 2005 Even though the two pathophysiological processes are diametrically opposed during the initiation phase in the subacute chronic phase they culminate in comprised blood supply and subsequent brain ischemia Caplan 1989 Krishnamurthi et al 2013 Powers et al 2018 When the insult results in cognitive dysfunction usually more than one cognitive domain is involved such as memory attention and visual spatial VS Al Qazzaz Ali Ahmad Islam Mohamad 2014 Cumming Marshall Lazar 2013 The significant factors that affect the cognitive impairments severity are older age previous history of stroke and the pre injury global cognitive function GCF Ballard Rowan Stephens Kalaria Kenny 2003 Mok et al 2004 Patel Coshall Rudd Wolfe 2003 Rasquin Verhey van Oostenbrugge Lousberg Lodder 2004 It has been shown that hemorrhagic strokes cause significantly more cognitive impairments compared to ischemic strokes and are more associated with cognitive deficits across multiple domains Cumming et al 2013 Cortical strokes were found with higher proportions of cognitive impairments in the memory domain than subcortical ones Lange Waked Kirshblum DeLuca 2000 Nys et al 2007 Schouten Schiemanck Brand Post 2009 Yet higher cortical functions such as expressive aphasia were significantly impaired in subcortical stroke patients as well as lower performances in the information processing speed IPS domain compared with cortical stroke patients Lange et al 2000 Nys et al 2007 T Wagner A Cushman 2017 With respect to dominant vs non dominant hemispheric lesion there is evidence of a more severe cognitive impairments and an overall higher incidence of dementia following an insult in the dominant hemisphere Censori et al 1996 de Oliveira Correia Marin Sde Ferreira Bertolucci 2013 Tatemichi et al 1993 Reducing the impact of post stroke cognitive impairment is an important goal due to the higher mortality and institutionalization rates of those patients Pasquini Leys Rousseaux Pasquier Henon 2007 Tatemichi et al 1994 Rehabilitation includes a multidisciplinary approach which includes physiotherapy speech and language therapy cognitive rehabilitation therapy medications and more However these programs have limited success Hebert et al 2016 Prvu Bettger Stineman 2007 Roine Kajaste Kaste 1993 Williams Jiang Matchar Samsa 1999 Cognitive recovery after stroke occurs mainly within the first 30 days with some post stroke patients continuing to gain progress up to three months from injury yet even with domain specific interventions improvement is minimal Langhorne et al 2011 Maulden Gassaway Horn Smout DeJong 2005 Ovbiagele Nguyen Huynh 2011 Hyperbaric oxygen therapy HBOT the applica tion of hyperbaric pressure in conjunction with increased oxygen content has been shown in several clinical studies to have the capacity to induce neuroplasticity even years after an acute insult Boussi Gross et al 2013 Boussi Gross et al 2015 Efrati Ben Jacob 2014 Efrati et al 2013 Efrati et al 2015 Hadanny Efrati 2016 Hadanny Fishlev Bechor Meir Efrati 2016 Hadanny et al 2015a 2015b Tal et al 2015a 2015b Tal Hadanny Sasson Suzin Efrati 2017 Yildiz et al 2004 The elevated oxygen concentration in the blood and injured tissue during treatment Calvert Cahill Zhang 2007 Niklas Brock Schober Schulz Schneider 2004 Reinert et al 2003 helps supply the energy needed to regenerate damaged brain tissue It has been shown that HBOT induced neuroplasticity is mediated by stimulating cell proliferation Mu et al 2013 neurogenesis of endogenous neural stem cells Yang et al 2008 regeneration of axonal white matter Chang et al 2009 improved maturation and myelination of injured neural fibers Haapaniemi Nylander Kanje Dahlin 1998 Vilela Lazarini Da Silva 2008 and stimulation of axonal growth thus increasing the ability of neurons to function and communicate with each other Bradshaw Nelson Fanton Yates Kagan Hallet 1996 Mukoyama Iida Sobue 1975 A retrospective analysis of post stroke patients in the late chronic stage revealed that HBOT can significantly improve the memory domain Boussi Gross et al 2015 However the overall neurocognitive effects of HBOT and its
A Hadanny et al HBOT cognitive effect in post stroke patients relation to the different stroke types and anatomical locations were not investigated yet The aim of the current study is to investigate the effects of HBOT on the overall cognitive domains of post stroke patients in the late chronic stage The nature type and location of the stroke as possible modifiers of HBOT effects were also investigated 2 Methods 2 1 Participants A retrospective study including post stroke patients more than three months post injury treated with HBOT between January 2008 and December 2017 The study was approved by our Institutional Review Board approval number 0206 17 ASF Inclusion criteria stroke more than three months prior to their first cognitive evaluation completion of 40 or 60 hyperbaric oxygen sessions and at least two cognitive evaluations 1 3 weeks prior to the first HBOT session to and 1 3 weeks after last HBOT session Exclusion criteria insufficient details of stroke nature history of a potential additional brain injury traumatic brain injury anoxic brain injury subarachnoid hemorrhage etc lack of pre or post HBOT cognitive evaluations 2 2 Study design The data were collected retrospectively from patients medical records and included age gender level of education handedness stroke details type injured hemisphere location of stroke time from injury to HBOT symptoms prior to treatment number of HBOT sessions chronic medical conditions diabetes mellitus type II DM II hypertension HTN dyslipidemia ischemic heart disease IHD previous stroke smoking status and chronic prescribed medications anti aggregation AA statins hypoglycemic medications HTN medications Data of the HBOT protocol and adverse events were also collected The main analysis was to compare the stroke nature hemorrhagic and ischemic including all stroke locations cortical subcortical atypical locations i e cerebellum or brain stem and multiple locations A second analysis i e the location analysis compared the two main stroke locations cortical and subcortical To minimize unknown hemisphere dom 95 inance in left handed patients a third analysis i e the dominance analysis included only the right handed patients for evaluating the effect of the injured hemisphere 2 3 Stroke subsets Patients were divided into different groups based on their stroke prerequisites retrieved from original imaging and medical records by anatomical location cortical i e frontal temporal parietal and occipital cortex or subcortical i e basal ganglia BG cerebellum pons internal capsule and thalamus by the injured hemisphere right or left and by stroke type ischemic or hemorrhagic See Fig 1 2 4 Hyperbaric oxygen treatment Participants were treated in a multi place hyperbaric chamber Haux Life Support GmbH Germany with the following protocols 40 to 60 daily sessions 5 days per week each session included 90 min of 100 oxygen at 2 ATA with 5 min air breaks every 20 minutes 2 5 Cognitive evaluation All the patients were inspected using the NeuroTrax computerized cognitive testing battery NeuroTrax Corporation Bellaire TX The NeuroTrax system and a detailed description of the tests included were detailed in previous publications Achiron et al 2013 Thaler et al 2012 Zur Naftaliev Kesler 2014 and are also available on the NeuroTrax website In brief NeuroTrax tests evaluate multiple aspects of brain cognitive functions including memory executive function EF visuospatial skills VS verbal function VF attention information processing speed IPS and motor skills MS Cognitive domain scores were normalized for age gender and education specific levels The participants completed two validated alternate test forms of the NeuroTrax test battery at baseline and post HBOT to allow for iterative administrations with minimal learning effects Test retest reliability of the tests were found to be high in both normal and injured populations without significant learning effects except in the VF VS domains Dwolatzky et al 2003 L Melton 2005 Due to the low test retest reliability of these domains they were not evaluated in the current study
96 A Hadanny et al HBOT cognitive effect in post stroke patients Fig 1 Flowchart of the patients included in the study 2 6 Statistical analysis Data were expressed as mean SD for parametric variables and frequencies and percentages for nonparametric variables Parametric variables were analyzed by paired sample T tests for intra group comparison and independent sample t tests for intergroup comparison whereas nonparametric variables were analyzed by Pearson Chi square test or Fisher s exact test where suitable to identify significant variables Normal distribution for all continuous variables was tested using the Kolmogorov Smirnov test Clinically significant improvement CSI was defined as an absolute increase of 7 5 points of the normalized score 0 5 of one standard deviation in at least one cognitive domain The cut off for CSI was determined by previous studies Fischer et al 2000 Schwid Goodman Weinstein McDermott Johnson 2007 Multiple linear regression models were performed to determine independent predictors for the post treatment cognitive score Multivariate logistic regression models were performed to control for potential confounders and to determine independent predictors for CSI Models included the following covariates age sex stroke type location of stroke along with side of injured hemisphere time from injury to HBOT chronic medical conditions DM II HTN dyslipidemia IHD active smoking number of HBOT sessions and baseline score before HBOT treatment
A Hadanny et al HBOT cognitive effect in post stroke patients 97 The alpha level was set to 0 05 p Value 0 05 The data were statistically analyzed using SPSS version 22 software of injury 87 strokes 53 7 were located in the right hemisphere and 62 strokes 38 3 were in the left hemisphere Baseline participants characteristics are summarized in Table 1 3 Results 3 2 Cognitive function changes 3 1 Participants characteristics Basic analysis results revealed statistically significant improvements of all the cognitive domains after HBOT by 2 34 20 p 0 05 see Table 2 The memory domain had the most prominent improvements of mean absolute change MAC 6 19 20 p 0 0004 see Table 2 CSI was achieved in 86 of the patients in the entire cohort see Fig 4 The effects of the HBOT on the cognitive scores is summarized in Table 2 Of the 351 patients who were assed for eligibility a total of 162 met the inclusion criteria and were included in the final analysis Fig 1 The patients average age was 60 75 12 91 years old 23 83 and 122 75 3 were males The average time from the stroke to HBOT was 2 78 3 3 years Regarding the stroke type 121 patients 74 69 suffered from an ischemic stroke while 41 25 31 had a hemorrhagic stroke In 50 patients 30 86 the stroke was in the subcortical level while 77 patients 47 53 had a stroke in the cortical level and the remaining 35 patients 21 6 were affected in atypical locations or multiple locations With respect to the side 3 2 1 Ischemic vs hemorrhagic At baseline there were significant differences in baseline characteristics between patients with ischemic compared to patients with hemorrhagic stroke which included age presence of comorbidities Table 1 Patients baseline characteristics Analysis Entire cohort n 162 Location analysis n 127 Dominance analysis n 110 Age years Sex Males Dominant hand Right Time from injury Num of HBOT sessions 40 sessions 60 sessions Type of stroke Ischemic Hemorrhagic Location of injury Subcortical Cortical Atypical multiple locations Side of injury Right Left Bilateral Symptoms Cognitive Motor Speech CN Ataxia Comorbidities DM II HTN Dyslipidemia IHD Previous stroke Smoker Medications AA Statins DM II medications HTN medications 60 75 12 91 122 75 3 120 74 1 2 78 3 3 26 16 136 84 121 74 69 41 25 31 54 33 3 80 49 4 28 17 3 62 38 3 87 53 7 13 8 77 47 5 132 81 5 65 40 1 67 41 4 57 35 2 48 29 6 107 66 107 66 39 24 1 18 11 1 29 17 9 105 64 8 104 64 2 37 22 8 107 66 60 86 12 57 97 76 4 94 74 2 53 2 95 22 17 3 105 82 7 98 77 17 29 22 8 50 39 4 77 60 6 53 41 7 74 58 3 60 47 2 104 81 9 54 42 5 54 42 5 39 30 7 37 29 1 82 64 6 82 64 6 30 23 6 12 9 4 23 18 1 78 61 4 79 62 2 27 21 3 84 66 1 61 23 12 3 78 70 9 110 100 2 63 3 18 20 18 2 90 81 8 85 77 3 25 22 7 36 32 7 58 52 7 16 14 5 56 50 9 54 49 1 49 44 5 90 81 8 43 39 1 46 41 8 34 30 9 28 25 5 74 67 3 75 68 2 28 25 5 10 9 1 15 13 6 70 63 6 72 65 5 20 18 2 74 67 3 Data are expressed as means standard deviation Cerebellum insult only HBOT hyperbaric oxygen treatment CN cranial nerves DM II diabetic mellitus type 2 HTN hypertension AA anti aggregates
98 A Hadanny et al HBOT cognitive effect in post stroke patients Table 2 Cognitive domains mean absolute changes of the entire cohort GCF Memory EF Attention IPS MS Pre score Post score Pre Post MAC P value 87 48 12 26 82 09 19 32 88 61 14 15 85 19 17 08 83 54 15 45 91 91 17 13 91 14 12 10 88 29 19 15 91 09 12 65 87 83 15 75 86 34 17 07 95 21 15 89 3 53 7 68 6 12 15 46 2 54 10 37 2 95 12 63 2 34 9 28 3 96 14 27 0 05 see Supplementary
Data are expressed as means standard deviation Significant by two tailed paired t test Bold text marks statistical significance P 0 05 GCF global cognitive function EF executive function VS visual spatial IPS information processing speed MS motor skills 0 686 0 153 0 834 0 685 0 2 0 608 87 8 14 28 81 96 18 94 90 29 15 14 86 33 18 33 81 21 14 07 90 18 18 59 88 81 11 77 87 15 18 9 89 68 14 69 84 93 17 57 85 24 16 99 91 9 15 48 0 1 0 788 0 009 0 012 0 28 0 362 84 95 13 53 80 72 20 18 85 19 15 11 80 8 19 57 82 7 16 61 89 69 19 58 88 76 11 26 81 68 18 4 92 37 13 61 88 44 14 02 83 55 14 22 92 79 16 25 0 214 0 043 0 992 0 56 0 106 0 667 85 42 11 36 76 82 21 06 88 63 13 98 83 8 15 73 79 66 14 09 92 93 15 15 88 18 12 52 83 87 18 45 88 6 14 26 85 65 17 54 84 68 15 7 91 56 17 79 GCF Memory EF Attention IPS MS P Value Location analysis Cortical Subcortical Ischemic hemorrhagic analysis Ischemic Hemorrhagic P Value Table 4 Pre hyperbaric oxygen treatment cognitive domains scores Rt Injury Dominance analysis Lt Injury P Value A Hadanny et al HBOT cognitive effect in post stroke patients 99 Fig I Moreover there were no significant changes in the CSI between subcortical strokes compared to cortical strokes 90 vs 87 23 p 0 05 see Fig 4 3 2 3 Dominant vs non dominant hemisphere Including only right handed patients at baseline there were significant differences in speech and motor symptoms between patients with left dominant hemisphere strokes compared to right non dominant hemisphere strokes p 0 05 see Table 6 There were no significant differences at baseline cognitive function between the dominant and non dominant hemisphere strokes p 0 05 see Table 4 Post HBOT there were significantly larger increases in MAC in the motor domains for patients with left hemisphere strokes compared to right hemisphere strokes 8 02 vs 1 42 p 0 023 see Fig 3 There were no other significant differences for the surplus cognitive domains p 0 05 see Fig 3 There were no significant changes in the CSI between left dominant hemisphere strokes compared to right non dominant hemisphere stroke patients 90 57 vs 76 47 p 0 05 see Fig 4 3 3 Cognitive scores outcome predictors Forward stepwise multivariate linear regression models were performed on the entire cohort as well as on the location and dominance cohorts The only major statistically significant predictor on the postHBOT score in all of the domains and analyses was the baseline cognitive domain score Age gender handedness stroke details type injured hemisphere location time from injury to HBOT number of HBOT sessions chronic medical conditions DM II HTN dyslipidemia IHD previous stroke smoking status chronic prescribed medications AA statins DM II medications HTN medications had no effect in most domains HTN was a significant predictor on post HBOT score in the GCS for the dominance analysis only and the number of HBOT sessions was a significant predictor on post HBOT in the EF domain for all analyses Forward stepwise multivariate logistic regression models were performed on the three different analyses to evaluate significant predictors for CSI percentage Low baseline cognitive memory domain score was the only statistically significant predictor on the CSI prevalence in the main and location analyses OR 0 94 0 909 0 972 p 0 0003
100 A Hadanny et al HBOT cognitive effect in post stroke patients Fig 2 Hemorrhagic ischemic stroke MAC comparison of cognitive scores post HBOT Only the IPS domain was significantly increased after HBOT for the hemorrhagic stroke patients compared to ischemic strokes Statistical significance p 0 05 is marked by Bars represent means standard deviation Abbreviations MAC mean absolute change HBOT hyperbaric oxygen treatment GCS global cognitive scale EF executive function IPS information processing speed MS motor skills Table 5 Baseline characteristics comparison of patients with cortical and subcortical strokes Location analysis Subcortical n 50 Cortical n 77 P value Age years Sex males Dominant hand right Time from injury Type of stroke Ischemic Hemorrhagic Side of injury Right Left Symptoms Cognitive Motor Speech CN Ataxia Comorbidities DM II HTN Dyslipidemia IHD Previous stroke Smoker Medications AA Statins DM II medications HTN medications 62 31 11 28 42 84 36 72 2 58 2 87 35 70 15 30 22 44 28 56 23 46 43 86 15 30 20 40 20 40 19 38 38 76 34 68 10 20 7 14 9 18 27 54 31 62 13 26 36 72 59 91 13 32 55 71 4 58 75 3 2 51 3 63 81 8 14 18 2 31 40 3 46 59 7 37 48 1 61 79 2 39 50 6 34 44 2 19 24 7 18 23 4 44 57 1 48 62 3 20 26 5 6 5 14 18 2 51 66 2 48 62 3 14 18 2 48 62 3 0 296 0 091 0 679 0 895 0 121 0 676 0 823 0 321 0 019 0 647 0 077 0 087 0 026 0 518 0 443 0 192 0 979 0 175 0 97 0 311 0 097 Data are expressed as means standard deviation Significant by two tailed paired t test Bold text marks statistical significance P 0 05 CN cranial nerves DM II diabetic mellitus type 2 HTN hypertension AA anti aggregates OR 0 948 0 912 0 985 p 0 007 respectively In the dominance analysis the low baseline cognitive memory domain score and shorter times that passed since the event to HBOT were the statistically significant predictors on the post HBOT score OR 0 949 0 912 0 986 p 0 008 OR 0 82 0 692 0 972 p 0 022 respectively 3 4 Safety There were twelve 7 4 side effect reports in the entire cohort Eight experienced barotrauma 8 162 4 93 Barotraumas were mild and all patients fully recovered after a few days In addition three patients 1 85 reported minor otalgia without objective
A Hadanny et al HBOT cognitive effect in post stroke patients 101 Table 6 Baseline characteristics comparison of patients with dominant and non dominant strokes Rt handed analysis Non dominant n 56 Dominant n 54 P value Age years Sex males Time from injury 60 73 13 78 38 67 9 2 57 2 59 44 78 6 12 21 4 20 35 7 29 51 8 7 12 5 21 37 5 50 89 3 13 23 2 20 35 7 17 30 4 14 25 37 66 1 37 66 1 13 23 2 2 3 6 10 17 9 35 62 5 35 62 5 12 22 2 34 60 7 61 75 10 65 40 74 1 2 7 3 72 41 75 9 13 24 1 16 29 6 29 53 7 9 16 7 28 51 9 40 74 1 30 55 6 26 48 1 17 31 5 14 25 9 37 68 5 38 70 4 15 27 8 8 14 8 5 9 3 35 64 8 37 68 5 8 14 3 40 74 1 0 668 0 477 0 827 0 741 Type of stroke Location of injury Symptoms Comorbidities Medications Ischemic Hemorrhagic Subcortical Cortical Atypical Locations Cognitive Motor Speech CN Ataxia DM II HTN Dyslipidemia IHD Previous stroke Smoker AA Statins DM II medications HTN medications 0 72 0 132 0 04 0 0004 0 19 0 9 0 912 0 787 0 632 0 587 0 044 0 19 0 803 0 511 0 286 0 137 Data are expressed as means standard deviation Significant by two tailed paired t test Bold text marks statistical significance P 0 05 CN cranial nerves DM II diabetic mellitus type 2 HTN hypertension AA anti aggregates Fig 3 Dominant non dominant MAC comparison of cognitive scores post HBOT The motor domain was significantly increased after HBOT at the dominant i e left sided stroke patients compared to non dominant strokes Statistical significance p 0 05 is marked by Bars represent means standard deviation Abbreviations MAC mean absolute change HBOT hyperbaric oxygen treatment GCS global cognitive scale EF executive function IPS information processing speed MS motor skills barotrauma One patient 0 06 reported a mild headache during recompression In addition two patients with histories of known seizures prior to HBOT suffered seizures after a few sessions of HBOT The seizures did not occur while in the hyperbaric chamber and once the patients reported about them their anti epileptic drugs were modified and they resumed HBOT shortly 4 Discussion In the current study the effect of HBOT on poststroke patients in the late chronic stages was analyzed Even though the patients were treated after a median of 1 5 3 3 years post stroke there were significant cognitive improvements in all the cognitive domains which were measured using objective computerized
102 A Hadanny et al HBOT cognitive effect in post stroke patients Fig 4 Clinically significant improvement comparisons of hemorrhagic vs ischemic cortical vs sub cortical and dominant vs non dominant stroke patients Scores were not significantly different in all the domains p 0 05 Bars represent percentages tests Moreover clinical significant improvements CSI were achieved in 86 of patients with the most significant measurable improvements gained in the dominant hemisphere stroke patients Low baseline memory score was the significant predictor for CSI Hemorrhagic stroke patients had significantly higher improvement in IPS but no other differences were found compared to ischemic strokes There were no significant differences in HBOT effects on subcortical compared to cortical strokes Patients with strokes located in the dominant hemisphere had significantly larger improvement in the MS domain In the current study there were significant improvements in all the cognitive domains which reconfirms previous studies that evaluated the therapeutic effect of HBOT in the chronic late stage of post stroke patients Boussi Gross et al 2015 Hadanny et al 2015a Emily R Rosario et al 2018 Vila Balcarce Abiusi Dominguez Pisarello 2005 In a previous study there were significant improvements in the neurological functions tested by the National Institutes of Health stroke scale NIHSS activities of daily living ADL and quality of life Efrati et al 2013 However cognitive domains were not reported A later retrospective study reported significant improvements in the memory domain after HBOT Yet the other cognitive domains were not explored and the stroke nature was not evaluated as a possible confounder Boussi Gross et al 2015 Churchill published a prospective study Churchill et al 2013 that included 22 patients at least one year after stroke HBOT induced improvement in symptoms reports 51 memory 51 attention concentration 48 balance coordination 45 endurance 20 sleep However on standardized evaluations of cognition and questionnaires no significant changes were reported Another small prospective study on seven patients showed verbal memory and executive function improvements in addition to sleep and quality of life changes E R Rosario et al 2018 The differences between hemorrhagic and ischemic strokes were mild but evident in the high cognitive function domain i e the IPS which correlates with the usually more severe outcomes of post hemorrhagic stroke patients and the cognitive deficits across multiple domains Cumming et al 2013 This domain is more sensitive than the other cognitive domains to an insult due to its integrating role on other domains and its influence on down Fig 5 Cortical subcortical i e BG MAC comparison of cognitive scores post HBOT Scores MAC were not significantly different in all the domains p 0 05 Bars represent means standard deviation Abbreviations MAC mean absolute change HBOT hyperbaric oxygen treatment GCS global cognitive scale EF executive function IPS information processing speed MS motor skills
A Hadanny et al HBOT cognitive effect in post stroke patients stream processes which is manifested in the domains score Nevertheless hemorrhagic stroke patients showed significant improvements post HBOT and the low baseline cognitive domain score remained the major predictor for the post HBOT domain score The lack of any significant differences after HBOT between cortical and subcortical strokes is surprising Similar to our study previous studies showed subcortical stroke patients have higher post stroke cognitive scores compared to cortical stroke patients Gottesman Hillis 2010 Kalaria Ballard 2001 However post HBOT there were no significant differences between the two types Even though it is expected that subcortical strokes will have lower proportions of memory impairments and conversely for the IPS domain no such differences were seen after HBOT treatment Our results indicate that the excess oxygen from HBOT treatments functions on all ischemic areas regardless of their anatomical area As expected the higher improvements in the MS domain seen in the dominant stroke patients lies in the basic functionality of the dominant side The lack of any significant difference regarding HBOT s beneficial effects to the stroke s origin and location could be explained by the common pathophysiological final path of injury i e ischemic metabolic dysfunctional cells in injured non necrotic brain regions As seen in previous studies stroke patients may have chronic penumbra even years after the insult which can be identified using SPECT imaging Churchill et al 2013 Jacobs Winter Alvis Small 1969 Oxygenation improves energy metabolism in the border zones of focal cerebral ischemia represented by significant reduction of areas with tissue acidosis and areas with ATP depletion Sun Marti Veltkamp 2008 Sun Strelow Mies Veltkamp 2011 HBOT can also decrease the post ischemic inflammatory response by reducing blood brain barrier damage Veltkamp et al 2005 inflammatory cytokines release Yu Xue Liang Zhang Zhang 2015 and suppresses the aggravated response of astrocytes and microgliosis Gunther et al 2005 Recently it was shown HBOT mitigates the inflammatory response of the neuronal cells through the transfer of mitochondria from astrocytes Lippert Borlongan 2019 HBOT reduces apoptosis which enables to preserve more brain tissues and promote neurologic functional recovery Yin et al 2003 Opening of mitochondrial ATP sensitive potassium channel plays a role in this antiapoptotic effect of early hyperbaric oxygenation Lou Chen Ding Eschenfelder Deuschl 103 2006 The intermittent hyperoxic exposure during HBOT can induce hypoxia inducible factor 1 alpha HIF 1 by the so called Hyperoxic Hypoxic paradox Duan Shao Yu Ren 2015 Milosevic et al 2009 Poli Veltkamp 2009 Soejima et al 2013 HIF 1 is transcriptional regulator of genes involved in angiogenesis energy metabolism and neuronal cell proliferation induced by HBOT Duan et al 2015 Milosevic et al 2009 Poli Veltkamp 2009 Soejima et al 2013 In summary HBOT induces neuroplasticity by two main physiological effects increasing tissue oxygenation the rate limiting factor for all regenerative mechanisms and the repeated oxygen level fluctuations which increases HIF 1 which in turn triggers the regenerative processes in the metabolically injured brain areas regardless of the stroke origin Efrati Ben Jacob 2014 Efrati et al 2013 Therefore the selection of stroke patients for HBOT should be based on functional imaging and baseline cognitive domain scores rather than stroke type location or side of lesion The current study presents the largest cohort of post stroke patients treated with HBOT in the late chronic stage However it has several limitations which are mostly related to the fact that data were collected retrospectively Still the findings presented here are in agreement with previous prospective RCT s in which the neuroplasticity effects of HBOT were established 28 37 48 These therapeutic effects were seen in our study in the chronic stage when patients are not expected to improve Another study limitation is the missing data on the treatment s long term effects Further long term prospective studies should be performed Another important limitation relates to the HBOT protocol which was inconsistent in the cohort where several patients received 40 sessions compared to 60 sessions in most patients Although significant neurotherapeutic effects were shown with both these protocols the optimal protocol which induces maximal neuroplasticity with minimal side effects remains unknown 5 Conclusions HBOT was found in the largest post stroke population published to induce significant improvements in all cognitive function domains even at the late chronic stage Patients selection for HBOT should be based on functional imaging and baseline cogni
104 A Hadanny et al HBOT cognitive effect in post stroke patients tive function regardless of stroke type and location Further studies are needed to validate these findings for the optimal patient selection Acknowledgments We would like to thank Dr Mechael Kanovsky for his editing of this manuscript Funding No external funding source was used for this study References Achiron A Chapman J Magalashvili D Dolev M Lavie M Bercovich E Barak Y 2013 Modeling of cognitive impairment by disease duration in multiple sclerosis A cross sectional study PloS One 8 8 e71058 doi 10 1371 journal pone 0071058 Al Qazzaz N K Ali S H Ahmad S A Islam S Mohamad K 2014 Cognitive impairment and memory dysfunction after a stroke diagnosis A post stroke memory assessment Neuropsychiatric Disease and Treatment 10 1677 1691 doi 10 2147 NDT S67184 Ballard C Rowan E Stephens S Kalaria R Kenny R A 2003 Prospective follow up study between 3 and 15 months after stroke Improvements and decline in cognitive function among dementia free stroke survivors 75 years of age Stroke 34 10 2440 2444 doi 10 1161 01 STR 0000089923 29724 CE Boussi Gross R Golan H Fishlev G Bechor Y Volkov O Bergan J Efrati S 2013 Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 8 11 e79995 doi 10 1371 journal pone 0079995 Boussi Gross R Golan H Volkov O Bechor Y Hoofien D Beeri M S Efrati S 2015 Improvement of memory impairments in poststroke patients by hyperbaric oxygen therapy Neuropsychology 29 4 610 621 doi 10 1037 neu0000149 Bradshaw P O Nelson A G Fanton J W Yates T KaganHallet K S 1996 Effect of hyperbaric oxygenation on peripheral nerve regeneration in adult male rabbits Undersea Hyperbaric Medicine Journal of the Undersea and Hyperbaric Medical Society Inc 23 2 107 113 Calvert J W Cahill J Zhang J H 2007 Hyperbaric oxygen and cerebral physiology Neurological Research 29 2 132141 doi 10 1179 016164107X174156 Caplan L R 1989 Intracranial branch atheromatous disease A neglected understudied and underused concept Neurology 39 9 1246 1250 related with neuropsychological deficits in carbon monoxide intoxication after hyperbaric oxygen therapy Journal of Neurotrauma 26 8 1263 1270 doi 10 1089 neu 2008 0619 Churchill S Weaver L K Deru K Russo A A Handrahan D Orrison W W Jr Elwell H A 2013 A prospective trial of hyperbaric oxygen for chronic sequelae after brain injury HYBOBI Undersea Hyperbaric Medicine Journal of the Undersea and Hyperbaric Medical Society Inc 40 2 165 193 Cumming T B Marshall R S Lazar R M 2013 Stroke cognitive deficits and rehabilitation still an incomplete picture International Journal of Stroke Of cial Journal of the International Stroke Society 8 1 38 45 doi 10 1111 j 17474949 2012 00972 x de Oliveira F F Correia Marin Sde M Ferreira Bertolucci P H 2013 Communicating with the non dominant hemisphere Implications for neurological rehabilitation Neural Regeneration Research 8 13 1236 1246 doi 10 3969 j issn 1673 5374 2013 13 009 Duan S Shao G Yu L Ren C 2015 Angiogenesis contributes to the neuroprotection induced by hyperbaric oxygen preconditioning against focal cerebral ischemia in rats The International Journal Neuroscience 125 8 625 634 doi 10 3109 00207454 2014 956101 Dwolatzky T Whitehead V Doniger G M Simon E S Schweiger A Jaffe D Chertkow H 2003 Validity of a novel computerized cognitive battery for mild cognitive impairment BMC Geriatrics 3 4 doi 10 1186 1471 23183 4 Efrati S Ben Jacob E 2014 Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Review in Neurotherapeutics 14 3 233 236 doi 10 1586 14737175 2014 884928 Efrati S Fishlev G Bechor Y Volkov O Bergan J Kliakhandler K Golan H 2013 Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PloS One 8 1 e53716 doi 10 1371 journal pone 0053716 Efrati S Golan H Bechor Y Faran Y Daphna Tekoah S Sekler G Buskila D 2015 Hyperbaric oxygen therapy can diminish fibromyalgia syndrome prospective clinical trial PLoS One 10 5 e0127012 doi 10 1371 journal pone 0127012 Fischer J S Priore R L Jacobs L D Cookfair D L Rudick R A Herndon R M Kooijmans Coutinho M F 2000 Neuropsychological effects of interferon beta 1a in relapsing multiple sclerosis Multiple Sclerosis Collaborative Research Group Annals of Neurology 48 6 885 892 Gottesman R F Hillis A E 2010 Predictors and assessment of cognitive dysfunction resulting from ischaemic stroke The Lancet Neurology 9 9 895 905 doi 10 1016 S14744422 10 70164 2 Censori B Manara O Agostinis C Camerlingo M Casto L Galavotti B Mamoli A 1996 Dementia after first stroke Stroke 27 7 1205 1210 Gunther A Kuppers Tiedt L Schneider P M Kunert I Berrouschot J Schneider D Rossner S 2005 Reduced infarct volume and differential effects on glial cell activation after hyperbaric oxygen treatment in rat permanent focal cerebral ischaemia The European Journal of Neuroscience 21 11 3189 3194 doi 10 1111 j 1460 9568 2005 04151 x Chang C C Lee Y C Chang W N Chen S S Lui C C Chang H W Wang Y L 2009 Damage of white matter tract cor Haapaniemi T Nylander G Kanje M Dahlin L 1998 Hyperbaric oxygen treatment enhances regeneration of the
A Hadanny et al HBOT cognitive effect in post stroke patients 105 rat sciatic nerve Experimental Neurology 149 2 433 438 doi 10 1006 exnr 1997 6745 icans with different stroke subtypes Advances in Therapy 24 2 258 268 Hadanny A Efrati S 2016 The efficacy and safety of hyperbaric oxygen therapy in traumatic brain injury Expert Review of Neurotherapeutics 16 4 359 360 doi 10 1586 14737175 2016 1157018 Lippert T Borlongan C V 2019 Prophylactic treatment of hyperbaric oxygen treatment mitigates inflammatory response via mitochondria transfer CNS Neuroscience Therapeutics 25 8 815 823 doi 10 1111 cns 13124 Hadanny A Fishlev G Bechor Y Meir O Efrati S 2016 Nonhealing Wounds Caused by Brown Spider Bites Application of Hyperbaric Oxygen Therapy Advances in Skin Wound Care 29 12 560 566 doi 10 1097 01 ASW 0000504578 06579 20 Lou M Chen Y Ding M Eschenfelder C C Deuschl G 2006 Involvement of the mitochondrial ATP sensitive potassium channel in the neuroprotective effect of hyperbaric oxygenation after cerebral ischemia Brain Research Bulletin 69 2 109 116 doi 10 1016 j brainresbull 2005 11 009 Hadanny A Golan H Fishlev G Bechor Y Volkov O Suzin G Efrati S 2015a Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restorative Neurology and Neuroscience 33 4 471 486 doi 10 3233 RNN150517 Lozano R Naghavi M Foreman K Lim S Shibuya K Aboyans V Memish Z A 2012 Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010 a systematic analysis for the Global Burden of Disease Study 2010 Lancet 380 9859 2095 2128 doi 10 1016 S01406736 12 61728 0 Hadanny A Golan H Fishlev G Bechor Y Volkov O Suzin G Efrati S 2015b Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restorative Neurology and Neuroscience 33 4 471 486 doi 10 3233 RNN150517 Maulden S A Gassaway J Horn S D Smout R J DeJong G 2005 Timing of initiation of rehabilitation after stroke Archives of Physical Medicine and Rehabilitation 86 12 Suppl 2 S34 S40 doi 10 1016 j apmr 2005 08 119 Hebert D Lindsay M P McIntyre A Kirton A Rumney P G Bagg S Teasell R 2016 Canadian stroke best practice recommendations Stroke rehabilitation practice guidelines update 2015 International Journal of Stroke Of cial Journal of the International Stroke Society 11 4 459 484 doi 10 1177 1747493016643553 Jacobs E A Winter P M Alvis H J Small S M 1969 Hyperoxygenation effect on cognitive functioning in the aged The New England Journal of Medicine 281 14 753 757 doi 10 1056 NEJM196910022811402 Kalaria R N Ballard C 2001 Stroke and cognition Current Atherosclerosis Reports 3 4 334 339 Kelly Hayes M Beiser A Kase C S Scaramucci A D Agostino R B Wolf P A 2003 The influence of gender and age on disability following ischemic stroke the Framingham study Journal of Stroke and Cerebrovascular Diseases The Of cial Journal of National Stroke Association 12 3 119 126 doi 10 1016 S1052 3057 03 00042 9 Krishnamurthi R V Feigin V L Forouzanfar M H Mensah G A Connor M Bennett D A Group G B D S E 2013 Global and regional burden of first ever ischaemic and haemorrhagic stroke during 1990 2010 Findings from the Global Burden of Disease Study 2010 The Lancet Global Health 1 5 e259 281 doi 10 1016 S2214 109X 13 700895 L Melton J 2005 Psychometric Evaluation of the Mindstreams Neuropsychological Screening Tool Lange G Waked W Kirshblum S DeLuca J 2000 Organizational strategy influence on visual memory performance after stroke cortical subcortical and left right hemisphere contrasts Archives of Physical Medicine and Rehabilitation 81 1 89 94 Langhorne P Bernhardt J Kwakkel G 2011 Stroke rehabilitation Lancet 377 9778 1693 1702 doi 10 1016 S0140 6736 11 60325 5 Lee W C Joshi A V Wang Q Pashos C L Christensen M C 2007 Morbidity and mortality among elderly Amer Milosevic J Adler I Manaenko A Schwarz S C Walkinshaw G Arend M Schwarz J 2009 Non hypoxic stabilization of hypoxia inducible factor alpha HIF alpha Relevance in neural progenitor stem cells Neurotox Research 15 4 367 380 doi 10 1007 s12640 009 9043 z Mok V C Wong A Lam W W Fan Y H Tang W K Kwok T Wong K S 2004 Cognitive impairment and functional outcome after stroke associated with small vessel disease Journal of Neurology Neurosurgery and Psychiatry 75 4 560 566 Mu J Ostrowski R P Soejima Y Rolland W B Krafft P R Tang J Zhang J H 2013 Delayed hyperbaric oxygen therapy induces cell proliferation through stabilization of cAMP responsive element binding protein in the rat model of MCAo induced ischemic brain injury Neurobiology of Disease 51 133 143 doi 10 1016 j nbd 2012 11 003 Mukoyama M Iida M Sobue I 1975 Hyperbaric oxygen therapy for peripheral nerve damage induced in rabbits with clioquinol Experimental Neurology 47 3 371 380 Niklas A Brock D Schober R Schulz A Schneider D 2004 Continuous measurements of cerebral tissue oxygen pressure during hyperbaric oxygenation HBO effects on brain edema and necrosis after severe brain trauma in rabbits Journal of the Neurological Sciences 219 1 2 77 82 doi 10 1016 j jns 2003 12 013 Nys G M van Zandvoort M J de Kort P L Jansen B P de Haan E H Kappelle L J 2007 Cognitive disorders in acute stroke Prevalence and clinical determinants Cerebrovascular Diseases 23 5 6 408 416 doi 10 1159 000101464 Ojaghihaghighi S Vahdati S S Mikaeilpour A Ramouz A 2017 Comparison of neurological clinical manifestation in patients with hemorrhagic and ischemic stroke World Journal of Emergency Medicine 8 1 34 38 doi 10 5847 wjem j 1920 8642 2017 01 006 Ottenbacher K J Jannell S 1993 The results of clinical trials in stroke rehabilitation research Archives of Neurology 50 1 37 44
106 A Hadanny et al HBOT cognitive effect in post stroke patients Ovbiagele B Nguyen Huynh M N 2011 Stroke epidemiology Advancing our understanding of disease mechanism and therapy Neurotherapeutics The Journal of the American Society for Experimental NeuroTherapeutics 8 3 319 329 doi 10 1007 s13311 011 0053 1 Schwid S R Goodman A D Weinstein A McDermott M P Johnson K P 2007 Cognitive function in relapsing multiple sclerosis Minimal changes in a 10 year clinical trial Journal of the Neurological Sciences 255 1 57 63 doi 10 1016 j jns 2007 01 070 Pasquini M Leys D Rousseaux M Pasquier F Henon H 2007 Influence of cognitive impairment on the institutionalisation rate 3 years after a stroke Journal of Neurology Neurosurgery and Psychiatry 78 1 56 59 doi 10 1136 jnnp 2006 102533 Soejima Y Hu Q Krafft P R Fujii M Tang J Zhang J H 2013 Hyperbaric oxygen preconditioning attenuates hyperglycemia enhanced hemorrhagic transformation by inhibiting matrix metalloproteinases in focal cerebral ischemia in rats Experimental Neurology 247 737 743 doi 10 1016 j expneurol 2013 03 019 Patel M Coshall C Rudd A G Wolfe C D 2003 Natural history of cognitive impairment after stroke and factors associated with its recovery Clinical Rehabilitation 17 2 158 166 doi 10 1191 0269215503cr596oa Poli S Veltkamp R 2009 Oxygen therapy in acute ischemic stroke experimental efficacy and molecular mechanisms Current Molecular Medicine 9 2 227 241 doi 10 2174 156652409787581619 Powers W J Rabinstein A A Ackerson T Adeoye O M Bambakidis N C Becker K American Heart Association Stroke C 2018 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke A Guideline for Healthcare Professionals From the American Heart Association American Stroke Association Stroke 49 3 e46 e110 doi 10 1161 STR 0000000000000158 Prvu Bettger J A Stineman M G 2007 Effectiveness of multidisciplinary rehabilitation services in postacute care state of the science A review Archives of Physical Medicine and Rehabilitation 88 11 1526 1534 doi 10 1016 j apmr 2007 06 768 Rasquin S M Verhey F R van Oostenbrugge R J Lousberg R Lodder J 2004 Demographic and CT scan features related to cognitive impairment in the first year after stroke Journal of Neurology Neurosurgery and Psychiatry 75 11 1562 1567 doi 10 1136 jnnp 2003 024190 Reinert M Barth A Rothen H U Schaller B Takala J Seiler R W 2003 Effects of cerebral perfusion pressure and increased fraction of inspired oxygen on brain tissue oxygen lactate and glucose in patients with severe head injury Acta Neurochirurgica 145 5 341 349 discussion 349 350 doi 10 1007 s00701 003 0027 0 Roine R O Kajaste S Kaste M 1993 Neuropsychological sequelae of cardiac arrest Jama 269 2 237 242 Rosario E R Kaplan S E Khonsari S Vazquez G Solanki N Lane M Rosenberg S S 2018 The Effect of Hyperbaric Oxygen Therapy on Functional Impairments Caused by Ischemic Stroke Neurology Research International 2018 12 doi 10 1155 2018 3172679 Rosario E R Kaplan S E Khonsari S Vazquez G Solanki N Lane M Rosenberg S S 2018 The Effect of Hyperbaric Oxygen Therapy on Functional Impairments Caused by Ischemic Stroke Neurology Research International 2018 3172679 doi 10 1155 2018 3172679 Schouten E A Schiemanck S K Brand N Post M W 2009 Long term deficits in episodic memory after ischemic stroke evaluation and prediction of verbal and visual memory performance based on lesion characteristics Journal of Stroke and Cerebrovascular Diseases The Of cial Journal of National Stroke Association 18 2 128 138 doi 10 1016 j jstrokecerebrovasdis 2008 09 017 Sun L Marti H H Veltkamp R 2008 Hyperbaric oxygen reduces tissue hypoxia and hypoxia inducible factor 1 alpha expression in focal cerebral ischemia Stroke 39 3 10001006 doi 10 1161 STROKEAHA 107 490599 Sun L Strelow H Mies G Veltkamp R 2011 Oxygen therapy improves energy metabolism in focal cerebral ischemia Brain Research 1415 103 108 doi 10 1016 j brainres 2011 07 064 T Wagner M A Cushman L 2017 Intellectual and Memory Functions After Cortical and Subcortical Stroke Vol 2 Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E Efrati S 2015a Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged postconcussion syndrome due to traumatic brain injury Restorative Neurology and Neuroscience 33 6 943 951 doi 10 3233 RNN 150585 Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E Efrati S 2015b Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged postconcussion syndrome due to traumatic brain injury Restorative Neurology and Neuroscience 33 6 943 951 doi 10 3233 RNN 150585 Tal S Hadanny A Sasson E Suzin G Efrati S 2017 Hyperbaric Oxygen Therapy Can Induce Angiogenesis and Regeneration of Nerve Fibers in Traumatic Brain Injury Patients Frontiers in Human Neuroscience 11 508 doi 10 3389 fnhum 2017 00508 Tatemichi T K Desmond D W Paik M Figueroa M Gropen T I Stern Y et al 1993 Clinical determinants of dementia related to stroke Annals of Neurology 33 6 568 575 doi 10 1002 ana 410330603 Tatemichi T K Paik M Bagiella E Desmond D W Pirro M Hanzawa L K 1994 Dementia after stroke is a predictor of long term survival Stroke 25 10 1915 1919 Thaler A Mirelman A Gurevich T Simon E OrrUrtreger A Marder K Consortium L A J 2012 Lower cognitive performance in healthy G2019S LRRK2 mutation carriers Neurology 79 10 1027 1032 doi 10 1212 WNL 0b013e3182684646 Veltkamp R Siebing D A Sun L Heiland S Bieber K Marti H H Schwaninger M 2005 Hyperbaric oxygen reduces blood brain barrier damage and edema after transient focal cerebral ischemia Stroke A Journal of Cerebral Circulation 36 8 1679 1683 doi 10 1161 01 STR 0000173408 94728 79 Vila J F Balcarce P E Abiusi G R Dominguez R O Pisarello J B 2005 Improvement in motor and cognitive impairment after hyperbaric oxygen therapy in a selected
A Hadanny et al HBOT cognitive effect in post stroke patients group of patients with cerebrovascular disease A prospective single blind controlled trial Undersea Hyperbaric Medicine Journal of the Undersea and Hyperbaric Medical Society Inc 32 5 341 349 Vilela D S Lazarini P R Da Silva C F 2008 Effects of hyperbaric oxygen therapy on facial nerve regeneration Acta oto laryngologica 128 9 1048 1052 doi 10 1080 00016480701827525 Williams G R Jiang J G Matchar D B Samsa G P 1999 Incidence and occurrence of total first ever and recurrent stroke Stroke 30 12 2523 2528 Yang Y J Wang X L Yu X H Wang X Xie M Liu C T 2008 Hyperbaric oxygen induces endogenous neural stem cells to proliferate and differentiate in hypoxic ischemic brain damage in neonatal rats Undersea Hyperbaric Medicine Journal of the Undersea and Hyperbaric Medical Society Inc 35 2 113 129 Yildiz S Kiralp M Z Akin A Keskin I Ay H Dursun H Cimsit M 2004 A new treatment modality for fibromyalgia syndrome Hyperbaric oxygen therapy The Journal of International Medical Research 32 3 263 267 doi 10 1177 147323000403200305 Yin D Zhou C Kusaka I Calvert J W Parent A D Nanda A Zhang J H 2003 Inhibition of apopto 107 sis by hyperbaric oxygen in a rat focal cerebral ischemic model Journal of Cerebral Blood Flow and Metabolism Of cial Journal of the International Society of Cerebral Blood Flow and Metabolism 23 7 855 864 doi 10 1097 01 WCB 0000073946 29308 55 Yoneda Y Okuda S Hamada R Toyota A Gotoh J Watanabe M Hasegawa Y 2005 Hospital cost of ischemic stroke and intracerebral hemorrhage in Japanese stroke centers Health Policy 73 2 202 211 doi 10 1016 j healthpol 2004 11 016 Yu M Xue Y Liang W Zhang Y Zhang Z 2015 Protection mechanism of early hyperbaric oxygen therapy in rats with permanent cerebral ischemia Journal of Physical Therapy Science 27 10 3271 3274 doi 10 1589 jpts 27 3271 Zhang J H Lo T Mychaskiw G Colohan A 2005 Mechanisms of hyperbaric oxygen and neuroprotection in stroke Pathophysiology The Of cial Journal of the International Society for Pathophysiology 12 1 63 77 doi 10 1016 j pathophys 2005 01 003 Zur D Naftaliev E Kesler A 2014 Evidence of Multidomain Mild Cognitive Impairment in Idiopathic Intracranial Hypertension Journal of Neuro Ophthalmology The Of cial Journal of the North American Neuro Ophthalmology Society doi 10 1097 WNO 0000000000000199
Received 14 November 2019 Accepted 26 December 2019 Published online 13 April 2020 DOI 10 1002 trc2 12008 RESEARCH ARTICLE A double blind placebo controlled clinical trial testing the effect of hyperbaric oxygen therapy on brain and cognitive outcomes of mildly cognitively impaired elderly with type 2 diabetes Study design Ori BenAri1 2 HungMo Lin4 Israel Sandler7 Shai Efrati2 3 Xiaoyu Liu4 Amir Hadanny2 3 Mary Sano4 Barbara B Bendlin5 Inbar Sela1 Ganit Almog1 Abigail Livny1 2 6 Simona Ben Haim8 9 Michal Schnaider Beeri1 4 Roy Sagi3 Derek LeRoith4 Ramit Ravona Springer1 2 10 1 The Joseph Sagol Neuroscience Center Sheba Medical Center Tel Hashomer Ramat Gan Israel 2 Sackler Faculty of Medicine Tel Aviv University Tel Aviv Israel 3 Sagol center for Hyperbaric Medicine Research Shamir Assaf Harofeh Medical Center Be er Ya akov Israel 4 Department of Psychiatry Icahn School of Medicine at Mount Sinai New York New York USA 5 Wisconsin Alzheimer s Disease Research Center University of Wisconsin Madison School of Medicine and Public Health Madison Wisconsin USA 6 Division of Diagnostic Imaging Sheba Medical Center Tel Hashomer Ramat Gan Israel 7 Department of Nuclear Medicine Sheba Medical Center Tel Hashomer Ramat Gan Israel 8 Department of Biophysics and Nuclear Medicine Hadassah University Hospital Ein Kerem Jerusalem Israel 9 Institute of Nuclear Medicine University College London Hospitals NHS Trust London UK 10 Department of Psychiatry Sheba Medical Center Tel Hashomer Ramat Gan Israel Correspondence Michal Schnaider Beeri Department of Psychiatry One Gustave L Levy Place Box 1230 New York NY 10029 6574 USA E mail michal beeri mssm edu Abstract Introduction Type 2 diabetes T2D is a risk factor for dementia Ischemia due to vascular pathology is hypothesized to be an underlying mechanism for this association Hyperbaric oxygen therapy HBOT is a treatment in which oxygen enriched air up to Funding information National Institutes of Health Grant Award Number AG051545 Michal Schnaider Beeri and Ramit RavonaSpringer contributed equally to this study 100 is administered to patients in a chamber at a pressure above one atmosphere absolute HBOT is approved for the treatment of T2D ischemic non healing wounds Evidence from animal studies and small clinical trials suggests that HBOT improves hypoxic ischemic brain injuries consequently inducing brain angiogensis leading to cognitive improvement Methods We present the design of the first double blind placebo controlled clinical trial on brain and cognitive outcomes in elderly n 154 with T2D and mild cognitive impairment to compare the effects of HBOT versus sham normal air with 1 1 ATA pressure in the first and last 5 minutes of the session Eligible candidates are randomized with equal probability to HBOT and sham Outcomes are assessed before and after treatment and at 6 and 12 month follow up The primary cognitive outcome is global This is an open access article under the terms of the Creative Commons Attribution NonCommercial License which permits use distribution and reproduction in any medium provided the original work is properly cited and is not used for commercial purposes c 2020 The Authors Alzheimer s Dementia Translational Research Clinical Interventions published by Wiley Periodicals Inc on behalf of Alzheimer s Association Alzheimer s Dement 2020 6 e12008 https doi org 10 1002 trc2 12008 wileyonlinelibrary com journal trc 1 of 9
2 of 9 BENARI ET AL cognitive change indexed by a composite sum of z scores of four executive functions and four episodic memory tests The primary neurobiological outcome is cerebral blood flow CBF via arterial spin labeling magnetic resonance imaging ASL MRI and cerebral glucose utilization via fluorodeoxyglucose positron emission tomography FDG PET Secondary outcome measures are specific cognitive domains executive function and episodic memory and functional measures Clinical Dementia Rating sum of boxes activities of daily living Efficacy analyses will be performed for the intent to treat sample Discussion Recent studies suggest that HBOT induces neuroplasticity and improves cognition in post stroke and traumatic brain injury patients However its effect on cognition cerebral blood flow and brain glucose utilization in T2D patients at high dementia risk is yet to be determined If effective this study may provide strong evidence for the brain and cognitive benefits of HBOT in this population KEYWORDS dementia hyperbaric oxygen therapy mild cognitive impairment type 2 diabetes 1 BACKGROUND In addition to cerebrovascular disease there is evidence for neurodegeneration in T2D Brain volume loss in the form of smaller total The estimated worldwide number of people with dementia is brain20 and gray matter 21 and larger cerebrospinal fluid CSF 15 vol 50 million 1 projected to triple by 2050 2 Cumulative evidence shows umes have been demonstrated in elderly patients with T2D Smaller that about 30 of late life dementia cases may be attributable to mod hippocampi were found in both middle aged22 24 and older T2D ifiable risk factors among which type 2 diabetes T2D contributes 6 patients 25 26 Even pre diabetic states such as impaired glucose tol to 8 3 T2D and pre diabetic states impaired fasting glucose obesity erance insulin resistance 27 and higher fasting glucose levels28 have metabolic syndrome are associated with increased risk for dementia4 been associated with lower hippocampal volume and medial tempo and mild cognitive impairment MCI worse cognitive functioning ral lobe volumes 29 The heterogeneous mechanisms underlying brain and brain hypometabolism 5 People with T2D vs without have 1 5 atrophy are not necessarily associated with neuronal loss or AD to 2 8 increased risk for dementia 6 8 The contribution of diabetes to related mechanisms 5 Accordingly people with T2D vs without show dementia is expected to grow with the accelerating T2D prevalence 9 hypometabolism of glucose in AD signature brain regions but do not because there is no known treatment to halt T2D related cognitive have greater amyloid load as demonstrated by amyloid PET17 and in decline postmortem studies 30 31 Cerebrovascular pathology has been demon Several mechanisms have been proposed to underlie the detrimen strated by some 32 33 but not other 34 previous studies to underlie brain tal effects of T2D on the brain 6 Cerebrovascular pathology and related atrophy in T2D Moreover cerebrovascular pathology in the form of ischemia constitutes a major factor 10 demonstrated by the high preva WMH rather than brain atrophy was associated with cognitive out lence of stroke 11 lacunar infarcts 12 microbleeds 13 and white matter comes in patients with T2D 35 Overall the evidence points toward a hyperintensities WMH 14 observed in T2D Likewise reduced cere bral blood flow CBF 14 and impaired cerebrovascular reactivity15 major role of cerebrovascular disease either directly or indirectly in T2D related cognitive compromise have also been observed in T2D Cerebrovascular disease16 and lower Hyperbaric oxygen therapy HBOT is a treatment in which CBF 5 17 mediate the adverse effects of T2D and metabolic syn oxygen enriched air up to 100 is administered to patients in a drome on cognition further supporting these pathological processes chamber at a pressure above one atmosphere absolute 1 ATA as underlying mechanisms Reduced CBF in the absence of brain atro which is the ambient sea level atmospheric pressure For peripheral phy has been shown in older adults with T2D 18 suggesting that CBF vasculature related disease a well accepted clinical indication for alterations occur early before cerebral atrophy and structural changes HBOT is non healing ischemic foot ulcers for which there is broad occur Lower CBF is found in individuals with metabolic syndrome a evidence for significant improvements with HBOT through stim state preceding T2D 19 and mediates the relationship of metabolic syn ulation of regenerative processes and angiogenesis 36 Similarly in drome with poorer memory function further supporting the notion that the brain based on previous evidence in animals and relatively new reduced CBF may be an early important marker of risk for cognitive human clinical trials it was demonstrated that HBOT can induce decline and dementia in T2D 5 neuroplasticity and improve CBF in ischemic non recoverable brain
3 of 9 BENARI ET AL regions leading to cognitive improvements even years after the acute insult 37 39 Angiogenesis is induced by HBOT through upregulation of RESEARCH IN CONTEXT hypoxia inducible factor 1 and vascular endothelial growth factor 1 Systematic review This trial examines the efficacy of including in the hippocampus 40 HBOT also increased vascular density hyperbaric oxygen therapy HBOT in improving cogni in the hippocampus improved spatial learning in rodents reduced tion in mildly cognitively impaired elderly with type 2 cortical infarct area and improved CBF in adult rats with vascular diabetes T2D who have high dementia risk T2D is a dementia 41 vascular disease culminating in a deficiency of oxygen It is well established that glucose utilization is impaired in cortical in the tissues and which affects the blood vessels in regions with ischemia 42 43 Conversely in animal models neuronal the brain increasing risk for cerebrovascular disease hypometabolism is improved with HBOT 44 suggesting that intracel which is an important factor in the risk of developing lular bioavailability of oxygen attenuates the deleterious effects of Alzheimer s disease ischemia on neuronal glucose utilization In humans HBOT has been 2 Interpretation The trial will be a randomized controlled associated with improvement in neurological and functional outcomes trial in which one group will experience conditions in the in post stroke patients 45 and with cognitive performance38 even hyperbaric chamber where the rate of oxygen is higher years after the acute stroke These improvements correlated with than in the normal environment and the second group brain activity as demonstrated by single photon emission computed will serve as a control in which the conditions in the tomography 38 46 Similarly HBOT had positive effects compared to hyperbaric chamber will be the condition found in the hyperbaric air on neurological and cognitive outcomes in a small normal environment n 26 randomized controlled trial of patients with cerebrovascular 3 Future directions If effective this study may provide disease 47 HBOT compared with normobaric oxygen was associated strong evidence for the brain and cognitive benefits of with increased CBF in frontal and temporal regions in healthy young HBOT in this population adults 48 Numerous therapies previously developed for the treatment of dementia have failed Late introduction of treatment at a phase in which the brain is overwhelmed by pathology has been proposed as a leading explanation for the failure of clinical trials 49 The neuropatho sures of cognition executive function and episodic memory are sec logical process of dementia starts 15 to 35 years before clinically overt ondary outcomes symptoms providing a window of opportunity for prevention MCI50 is Aim 2 Determine the impact of HBOT on neuronal function Flu considered to be a prodromal state preceding dementia and the stage orodeoxyglucose positron emission tomography F18 FDG PET at which interventions aimed at dementia prevention may be effective measuring cerebral glucose utilization is the outcome People with MCI have 10 to 15 risk for conversion to dementia 10 Aim 3 Determine the mediation effects of CBF and glucose utiliza times the risk for those without MCI 51 With regard to T2D individu tion To examine whether CBF and glucose utilization mediate HBOT als with T2D and pre T2D52 compared to those without T2D6 53 previ effects on cognitive function ous studies demonstrated up to 1 6 increased risk for MCI and higher risk of conversion from MCI to dementia Moreover WMH indicative of cerebrovascular pathology are associated with worse cognitive and 2 METHODS brain volume outcomes in people with MCI comparing to AD and comparing to healthy controls 54 Altogether these findings suggest that 2 1 Participants addressing vascular pathology may have a beneficial impact on cognition among individuals with T2D and particularly among individuals This study is a collaboration among the Icahn School of Medicine who are both T2D and MCI New York the Sheba Medical Center Israel and the Shamir Assaf Given the biological plausibility of HBOT for T2D related cognitive Harofeh Medical Center Israel Participants are recruited in Israel compromise our research group is testing the extent to which the cog primarily from the center of Israel area see Figure 1 Recruitment nitive compromise in T2D may be addressed by the improvement in eligibility criteria and brain and cognitive outcomes are assessed at vascular function by HBOT therapy on the brain This report describes Sheba HBOT and sham therapy are performed at the Sagol Center the design of our pilot double blind placebo controlled clinical trial for Hyperbaric Medicine Research Shamir Assaf Harofeh Medical examining the short and long term effects of HBOT on cognition CBF Center Israel Elderly patients n 154 with T2D and MCI amnestic and cerebral glucose utilization in T2D patients with MCI or non amnestic will be enrolled Mini Mental State Examination The specific aims of the trial are to MMSE score 24 and Clinical Dementia Rating CDR 0 5 are required An informant must be available to provide supplemental Aim 1 Determine the impact of HBOT on cognitive function The pri information throughout the trial Participants are recruited through mary outcome is a composite measure of cognitive function balancing advertisements mailing lists of elderly interested in receiving health tests of both executive and memory function Domain specific mea related updates word of mouth and talks in the community Table 1
4 of 9 BENARI ET AL TA B L E 1 Eligibility criteria Inclusion criteria Exclusion criteria 1 2 3 4 5 1 Brain disease that affects cognition eg Parkinson s disease schizophrenia 2 Stroke 3 Epilepsy 4 Chest pathology incompatible with HBOT 5 Inner ear disease 6 Claustrophobia 7 Treatment with cholinesterase inhibitors 8 An indication for HBOT 9 Previous HBOT treatment 10 Cancer or other medical illnesses requiring intensive therapy 11 Proliferative retinopathy T2D diagnosis MCI diagnosis Age 65 years Hebrew fluency An informant Abbreviations HBOT hyperbaric oxygen chamber MCI mild cognitive impairment T2D type 2 diabetes Staff from Sheba who assesses outcomes remain blinded and do not meet participants during their intervention 2 3 Procedures Table 2 presents study procedures for each participant After undergoing an informed consenting process the eligibility screening includes a medical and neurological clinical evaluation to confirm T2D and MCI diagnoses Each assessment incudes medication review that may indicate an exclusion intake of cholinesterase inhibitors At baseline eligible patients are tested on outcome measures Cognitive affective by the Beck Depression Inventory see the supporting information F I G U R E 1 Central Israel where most participants live Arrows mark the approximate location of the Sheba Medical Center and Asaf Harofeh Medical Center and functional assessments are repeated after the intervention to test short term effects and after 6 and 12 months to test longer term effects CBF and cerebral glucose utilization FDG PET are repeated after the intervention and at 12 months to evaluate neuropathological processes relevant to T2D Physical exams and blood sugar summarizes eligibility criteria Participants are preferably from central tests for safety monitoring occur before randomization and after the Israel relatively close to Asaf Harofeh where HBOT treatment is intervention when a questionnaire examines whether blindness was performed Figure 1 maintained 2 2 2 4 Randomization and blinding of intervention HBOT intervention Using the SAS PROC Plan v9 4 55 eligible participants are randomized HBOT is administrated in a multiplace chamber HAUX 2700 The unit with equal probability to the HBOT and sham interventions with a total comprises a seating area with comfortable chairs for 12 participants of 77 for each When a cluster of three to six participants is filled with resembling an airplane Figure 2 and is staffed by a nurse who stays a maximum wait of 3 weeks the intervention for that cluster will begin throughout the session The HBOT protocol includes 60 daily sessions Therefore the number of clusters may vary Three study technicians of 90 minutes of 100 oxygen at 2 ATA with 5 minute air breaks every who activate HBOT or sham protocol sessions are the only unblinded 20 minutes 5 days week This hyperbaric oxygen treatment protocol is staff who have the key for the participants group assignments All par used clinically for treatment of ischemic non healing wounds diabetic ticipants and other clinic staff remain blinded to group assignment foot or post radiation injury and was used in a previous clinical trial
5 of 9 BENARI ET AL TA B L E 2 Summary of study procedures Screening Informed consent X Medication review X Eligibility assessment X Cognitive testing Functional assessment CDR Baseline 6 months 12 months X X X X X X X X X X X X X X X X X ADL and IADL After intervention End of interventiona Beck depression inventory X X CBF X X X Cerebral glucose utilization X X X Randomization X Physical exam X X X Adverse event monitoringa X Blindness testing X a The intervention protocol begins within 3 weeks after baseline assessment and ends after 60 HBOT sham treatments A physician is always present during the HBOT sham sessions and a nurse is in the chamber throughout the whole treatment so adverse events are closely monitored at each session of the intervention Abbreviations ADL Activities of Daily Living CBF cerebral blood flow HBOT hyperbaric oxygen chamber IADL Instrumental Activities of Daily Living 2 5 Sham intervention The sham control condition replicates all experiential aspects of the HBOT therapy except for the degree of pressure and oxygen levels The sham condition exposes subjects to 1 1 ATA which provides a pressure sensation in addition to the noise of air circulation Pressure then decreases very slowly during the next half hour in the last 5 minutes of the session air is circulated again with its related noise Sham and HBOT sessions are never adjacent so participants from the two groups cannot meet and compare sessions This sham model makes the two conditions very comparable FIGURE 2 Hyperbaric oxygen chamber 2 6 Outcome measures Primary cognitive outcome The primary outcome was a composite sum of z scores of four executive function tests Trails B Mazes in post stroke patients 46 Study nurses monitor adverse events AEs Digit Symbol and Category Fluency and four episodic memory during all sessions and a physician is present in the hyperbaric cen tests immediate and delayed recall of the word list from the ter during each session While in the chamber participants may drink Alzheimer s Disease Assessment Scale Cognitive Subscale ADAS read write sleep hear music with headphones or watch TV Video Cog and immediate and delayed recall of Logical Memory Story I games laptops phones or other electronic devices are not allowed in from the Wechsler Memory Scale III These functions are affected the chamber Each participant has his her own mask The atmospheric by T2D56 and commonly evaluated in other MCI trials 57 58 Z scores pressure increases to 2 ATA during the first 5 minutes of the ses are reversed if necessary so that a positive value reflects better sion which is accompanied by the sound of circulating air Participants performance feel ear pressure the nurse advises releasing it by pumping the ears Secondary cognitive outcomes These are domain specific closing the nose with fingers and pushing air In the last 5 minutes of composites four tests each for executive function and episodic the session the pressure is slowly decreased to 1 ATA Additional pro memory both affected by T2D 56 59 and benefitted by HBOT 38 cedures performed before entrance to the chamber are described in the supporting information Secondary outcomes The four measures are the CDR scale and an alternative scoring sum of boxes described in the supporting
6 of 9 BENARI ET AL TA B L E 3 Two group t test of equal means equal n sa outcome measure will be excluded from all its analyses maximum likelihood estimation methods will be used on missing data from an Outcome Sham mean change D1 unobserved outcome follow up visit Overall cognition z score CBFb CGU at each time after intervention by mixed model analysis of covari 0 020 0 450 0 08 ance ANCOVA with time of assessment baseline or outcome as For all outcome measures baseline will be compared to outcomes the within subjects factor treatment group HBOT vs sham as the HBOT mean change D2 0 224 2 28 2 065 Difference in means D1 D2 0 244 2 73 2 145 SD both groups 0 50 between subjects factor and baseline value of the outcome measure as the covariate For CBF and cerebral glucose utilization as exploratory analyses linear mixed effects models will be used to assess relationships between treatment group fixed effect and the longi 5 60 4 40 Minimum N per group 67 67 67 Enrollment N per groupb 77 77 77 tudinal trend random intercept and slope for each subject assessed post intervention and after 12 months Because CBF derived from ASL perfusion may represent combined effects of neural metabolism and Abbreviations CBF cerebral blood flow CGU cerebral glucose utilization a Test of significance level 0 05 b Assuming a 13 drop out rate two sided test power 80 effect size 0 49 vascular effects a secondary ANCOVA of CBF changes from baseline to 12 weeks will adjust for cerebral glucose metabolism Changes in CBF and cerebral glucose utilization will be further explored as mediators of the relationship between treatment group and the change in cognition information based on participant and informant interviews and the activities of daily living ADL and IADL questionnaires 2 8 Power analysis and sample size justification Cognitive outcomes Power is presented for detecting the difference in 2 6 1 Neuroimaging mean change from baseline to 12 weeks in overall cognition z scores between the sham and HBOT treatment groups Power calculations CBF Participants undergo a full magnetic resonance imaging MRI are based on two sample t tests and are conducted with a two sided protocol to acquire CBF and ancillary scans on a 3 Tesla 3T Philips 5 significance level Table 3 The predicted mean change in the sham Ingenia scanner using a 32 channel radio frequency coil The MRI group from baseline to 12 weeks is 0 02 based on the Israel Dia protocol includes arterial spin labeling ASL T2 weighted fluid betes and Cognitive Decline IDCD study Assuming a standard devi attenuated inversion recovery T2 FLAIR resting state functional MRI ation SD of 0 50 in both the sham and HBOT groups with a minimum fMRI and T1 weighted imaging additional information on proce sample size of 67 patients per arm we have 80 power to detect an dures and image processing is provided in the supporting information improvement in the HBOT group of 0 224 a medium effect size of Cerebral glucose utilization Participants undergo an F18 FDG 0 49 To account for an anticipated dropout rate of 13 conservative PET scan to examine cerebral glucose metabolism on a Philips Vereos compared to 5 in our previous stroke study46 we plan to enroll scanner using digital photon counting Procedures are detailed in the 77 patients per group for a total of 154 patients In a previous supporting information trial assessing the efficacy of HBOT years after mild traumatic brain injury 61 an effect size of 0 47 was detected for information speed processing which is clinically comparable to our primary outcome mea 2 7 Statistical analysis plan sure of overall cognition An HBOT trial for stroke patients46 showed an effect size of 0 49 for the National Institutes of Health stroke scale Efficacy analyses will be performed for the intent to treat ITT suggesting our detectable effect size of 0 49 is plausible sample our primary analysis and for fully and partially compliant CBF outcomes Power is presented for detecting the difference in per protocol PP samples The ITT sample will include all participants the mean changes in CBF and cerebral glucose utilization between the in the group to which they were randomized regardless of any pro sham and HBOT groups Assuming a mean change in CBF of 0 45 in tocol deviation including non compliance AEs or loss of follow up the sham group and an SD of 5 6 in both groups with a minimum sample The PP samples will include participants in the group according to size of 67 patients per arm we have 80 power to detect an improve the intervention actually received with separate analyses for those ment in the HBOT group of 2 28 an effect size of 0 49 To account for who were fully compliant at least 80 of sessions completed and for an anticipated dropout rate of 13 we plan to enroll 77 patients per those who were partially compliant at least one session completed A group for a total of 154 patients complier average causal effect analysis60 using a latent class modeling Cerebral glucose utilization outcomes Assuming a mean change in approach will also be performed on both fully and partially compliant the sham group of 0 08 and an SD of 4 40 in both groups with 67 samples Participants missing a baseline value of a continuous efficacy patients per group we are powered to detect an improvement in the
7 of 9 BENARI ET AL HBOT group of 2 065 an effect size of 0 49 According to literature may be preferable to 1 3 ATA given that the latter has been shown to sources 5 62 these are observable effect sizes increase tissue oxygenation by 50 in a mouse model 69 Our study focuses on cerebrovascular disease and cerebral glucose uptake as the primary underlying mechanisms however HBOT 3 DISCUSSION has also been suggested to affect other mechanisms relevant to diabetes related brain insult including improved blood brain barrier This study aims to examine the effect of HBOT versus sham on cogni features 45 mitochondrial function 70 cellular metabolism inflamma tion CBF and brain glucose utilization in elderly patients with T2D who tion and oxidative stress 39 are at high dementia risk due to MCI If our results support the hypothesis of beneficial effects of HBOT Our design has few limitations Assessment of outcomes and HBOT for individuals with both T2D and MCI a future randomized controlled therapy are performed in two different hospitals imposing some bur trial will have a strong rationale to broaden the eligibility criteria to den on participants but ensuring blindness of the team to the group include cognitively normal pre T2D older adults It will also provide assignment Several patient groups who may benefit from the treat crucial information for optimizing design for planning a multi center ment are not included such as pre T2D conditions which already show large scale clinical trial to provide definitive evidence for the benefits brain alterations associated with cognitive impairment of HBOT for the brain and cognition in T2D patients at high risk for The prevalence of T2D is increasing worldwide and its deleterious dementia effect sizes subgroups benefitting most design biomark role on cognition and dementia is increasingly recognized 5 Cere ers cognitive outcomes recruitment strategies and attrition Because brovascular pathology is hypothesized to be a significant contributor HBOT is widely available and well tolerated the success may suggest to T2D related poor cognitive outcomes as demonstrated by the testing HBOT efficacy in non T2D elderly with MCI as well association of brain hypoperfusion independent of brain atrophy with worse cognitive performance in patients with T2D 14 Currently FUNDING HBOT s approved U S Food and Drug Administration FDA indication This work was supported by the National Institutes of Health grant in the context of T2D includes the treatment of diabetes related number AG051545 ischemic foot ulcers63 preliminary results also point to its efficacy in improving neurological and brain activity outcomes in post stroke 46 REFERENCES and vascular dementia 64 While the biological plausibility of HBOT in 1 Prince M Wimo A Guerchet M Ali G Wu Y Prina M Alzheimer s Disease International World Alzheimer Report 2015 The Global Impact of Dementia An Analysis of Prevalence Incidence Cost and Trends 2015 London Alzheimer s Disease International 2019 2 Kivipelto M Mangialasche F Ngandu T Lifestyle interventions to prevent cognitive impairment dementia and Alzheimer disease Nat Rev Neurol 2018 14 11 653 666 3 Norton S Matthews FE Barnes DE Yaffe K Brayne C Potential for primary prevention of Alzheimer s disease an analysis of populationbased data Lancet Neurol 2014 13 788 794 4 Li W Huang E An update on type 2 diabetes mellitus as a risk factor for dementia J Alzheimers Dis 2016 53 393 402 5 Birdsill AC Carlsson CM Willette AA et al Low cerebral blood flow is associated with lower memory function in metabolic syndrome Obesity 2013 21 1313 1320 6 Biessels GJ Despa F Cognitive decline and dementia in diabetes mellitus mechanisms and clinical implications Nat Rev Endocrinol 2018 14 591 7 Schneider JA Aggarwal NT Barnes L Boyle P Bennett DA The neuropathology of older persons with and without dementia from community versus clinic cohorts J Alzheimers Dis 2009 18 691 701 8 Beeri MS Goldbourt U Silverman JM et al Diabetes mellitus in midlife and the risk of dementia three decades later Neurology 2004 63 19021907 9 NCD Risk Factor Collaboration NCD RisC Worldwide trends in diabetes since 1980 a pooled analysis of 751 population based studies with 4 4 million participants Lancet 2016 387 15131530 10 Zeadin MG Petlura CI Werstuck GH Molecular mechanisms linking diabetes to the accelerated development of atherosclerosis Can J Diabetes 2013 37 345 350 11 Tziomalos K Spanou M Bouziana SD et al Type 2 diabetes is associated with a worse functional outcome of ischemic stroke World J Diabetes 2014 5 939 T2D related cognitive outcomes is supported ours is the first study to date to test the impact of HBOT on cognitive function in T2D Two 1970s studies evaluated efficacy of HBOT at 2 5 ATA two daily 90 minute sessions for 15 days in dementia No beneficial effects were found for 13 patients with cortical atrophy and eight with evidence of cerebrovascular disease 65 For 40 older adult participants with cognitive impairment hyperbaric or normobaric oxygen therapy did not show significant improvement 66 These studies had a short intervention period which might have been too short to determine an effect Moreover the small sample size in both studies limited the power to detect an effect More recently in 64 patients with vascular dementia randomization to HBOT as an adjuvant to donepezil improved cognition versus donepezil alone This study had some methodological limitations including no sham group and no blinding In addition the study protocol was not fully revealed 67 suggesting more work is necessary Our protocol design is based on regenerative medicine paradigms which postulate that changes in oxygen availability rather than steady state hypoxic or hyperoxic conditions are required to induce processes required for angiogenesis and neurogenesis 68 The present study addresses several limitations of previous studies 1 patients with T2D have compromised cerebral vasculature leading to chronic mild hypoxia and poorer CBF that HBOT may remedy 2 patients have MCI rather than frank dementia so some brain vasculature changes may be reversible preventing or delaying dementia 3 sham therapy is preferable to a crossover control condition 4 we assess longer term HBOT effects 12 months 5 our sample size is larger and thus more sufficiently powered to predict HBOT effects and 6 sham at 1 1 ATA
8 of 9 12 van Harten B Oosterman JM van Loon B JP Scheltens P Weinstein HC Brain lesions on MRI in elderly patients with type 2 diabetes mellitus Eur Neurol 2007 57 70 74 13 Cordonnier C Al Shahi Salman R Wardlaw J Spontaneous brain microbleeds systematic review subgroup analyses and standards for study design and reporting Brain 2007 130 1988 2003 14 De Bresser J Reijmer YD Van Den Berg E et al Microvascular determinants of cognitive decline and brain volume change in elderly patients with type 2 diabetes Dement Geriatr Cogn Disord 2010 30 381 386 15 Last D Alsop DC Abduljalil AM et al Global and regional effects of type 2 diabetes on brain tissue volumes and cerebral vasoreactivity Diabetes Care 2007 30 1193 1199 16 Qiu C Sigurdsson S Zhang Q et al Diabetes markers of brain pathology and cognitive function the Age Gene Environment Susceptibility Reykjavik study Ann Neurol 2014 75 138 146 17 Roberts RO Knopman DS Cha RH et al Diabetes and elevated hemoglobin A1c levels are associated with brain hypometabolism but not amyloid accumulation J Nucl Med 2014 55 759 764 18 Bangen KJ Werhane ML Weigand AJ et al Reduced regional cerebral blood flow relates to poorer cognition in older adults with type 2 diabetes Front Aging Neurosci 2018 10 270 19 Eckel RH Grundy SM Zimmet PZ The metabolic syndrome Lancet 2005 365 1415 1428 20 Espeland MA Bryan RN Goveas JS et al Influence of type 2 diabetes on brain volumes and changes in brain volumes results from the women s health initiative magnetic resonance imaging studies Diabetes Care 2013 36 90 97 21 Saczynski JS Siggurdsson S Jonsson PV et al Glycemic status and brain injury in older individuals the Age Gene Environment Susceptibility Reykjavik study Diabetes Care 2009 32 1608 1613 22 Moran C Phan TG Chen J et al Brain atrophy in type 2 diabetes regional distribution and influence on cognition Diabetes Care 2013 36 4036 4042 23 Bruehl H Wolf OT Convit A A blunted cortisol awakening response and hippocampal atrophy in type 2 diabetes mellitus Psychoneuroendocrinology 2009 34 815 821 24 Gold S Dziobek I Sweat V et al Hippocampal damage and memory impairments as possible early brain complications of type 2 diabetes Diabetologia 2007 50 711 719 25 Korf ES White LR Scheltens P Launer LJ Brain aging in very old men with type 2 diabetes the Honolulu Asia Aging study Diabetes Care 2006 29 2268 2274 26 den Heijer T Vermeer S Van Dijk E et al Type 2 diabetes and atrophy of medial temporal lobe structures on brain MRI Diabetologia 2003 46 1604 1610 27 Convit A Wolf OT Tarshish C De Leon MJ Reduced glucose tolerance is associated with poor memory performance and hippocampal atrophy among normal elderly Proc Natl Acad Sci 2003 100 2019 2022 28 Cherbuin N Sachdev P Anstey KJ Higher normal fasting plasma glucose is associated with hippocampal atrophy the PATH study Neurology 2012 79 1019 1026 29 Willette AA Xu G Johnson SC et al Insulin resistance brain atrophy and cognitive performance in late middle aged adults Diabetes Care 2013 36 443 449 30 Beeri MS Silverman JM Davis KL et al Type 2 diabetes is negatively associated with Alzheimer s disease neuropathology J Gerontol A Biol Sci Med Sci 2005 60 471 475 31 Arvanitakis Z Schneider J Wilson R et al Diabetes is related to cerebral infarction but not to AD pathology in older persons Neurology 2006 67 1960 1965 32 Exalto L Whitmer R Kappele L Biessels G An update on type 2 diabetes vascular dementia and Alzheimer s disease Exp Gerontol 2012 47 858 864 BENARI ET AL 33 Moran C M nch G Forbes JM et al Type 2 diabetes skin autofluorescence and brain atrophy Diabetes 2015 64 279 283 34 Van Harten B Oosterman J Muslimovic D Van Loon B JP Scheltens P Weinstein HC Cognitive impairment and MRI correlates in the elderly patients with type 2 diabetes mellitus Age Ageing 2007 36 164 170 35 Mankovsky B Zherdova N van den Berg E Biessels GJ de Bresser J Cognitive functioning and structural brain abnormalities in people with type 2 diabetes mellitus Diabet Med 2018 35 1663 1670 36 Mathieu D Marroni A Kot J Tenth European Consensus Conference on Hyperbaric Medicine recommendations for accepted and nonaccepted clinical indications and practice of hyperbaric oxygen treatment Diving Hyperb Med 2017 47 24 32 37 Asl MT Yousefi F Nemati R Assadi M 99mTc ECD brain perfusion SPECT imaging for the assessment of brain perfusion in cerebral palsy CP patients with evaluation of the effect of hyperbaric oxygen therapy Int J Clin Exp Med 2015 8 1101 38 Boussi Gross R Golan H Volkov O et al Improvement of memory impairments in poststroke patients by hyperbaric oxygen therapy Neuropsychology 2015 29 610 39 Efrati S Ben Jacob E Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Rev Neurother 2014 14 233 236 40 Sunkari VG Lind F Botusan IR et al Hyperbaric oxygen therapy activates hypoxia inducible factor 1 HIF 1 which contributes to improved wound healing in diabetic mice Wound Repair Regen 2015 23 98 103 41 Choudhury R Hypoxia and hyperbaric oxygen therapy a review Int J Gen Med 2018 11 431 42 Saito H Kuroda S Hirata K et al Validity of dual MRI and 18F FDG PET imaging in predicting vulnerable and inflamed carotid plaque Cerebrovasc Dis 2013 35 370 377 43 Murata T Omata N Fujibayashi Y et al Neurotoxicity after hypoxia during ischemia due to glutamate with without free radicals as revealed by dynamic changes in glucose metabolism Brain Res 2000 865 259 263 44 Zhang Y Yang Y Tang H et al Hyperbaric oxygen therapy ameliorates local brain metabolism brain edema and inflammatory response in a blast induced traumatic brain injury model in rabbits Neurochem Res 2014 39 950 960 45 Machida T Takata F Matsumoto J et al Contribution of thrombinreactive brain pericytes to blood brain barrier dysfunction in an in vivo mouse model of obesity associated diabetes and an in vitro rat model PLoS One 2017 12 e0177447 46 Efrati S Fishlev G Bechor Y et al Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS One 2013 8 e53716 47 Vila J Balcarce P Abiusi G Dominguez R Pisarello J Improvement in motor and cognitive impairment after hyperbaric oxygen therapy in a selected group of patients with cerebrovascular disease a prospective single blind controlled trial Undersea Hyperb Med 2005 32 341 48 Micarelli A Jacobsson H Larsson S Jonsson C Pagani M Neurobiological insight into hyperbaric hyperoxia Acta Physiologica 2013 209 69 76 49 Anderson RM Hadjichrysanthou C Evans S Wong MM Why do so many clinical trials of therapies for Alzheimer s disease fail Lancet 2017 390 2327 2329 50 Winblad B Palmer K Kivipelto M et al Mild cognitive impairment beyond controversies towards a consensus report of the International Working Group on Mild Cognitive Impairment J Intern Med 2004 256 240 246 51 Petersen RC Negash S Mild cognitive impairment an overview CNS Spectr 2008 13 45 53 52 Cooper C Sommerlad A Lyketsos CG Livingston G Modifiable predictors of dementia in mild cognitive impairment a systematic review and meta analysis Am J Psychiatry 2015 172 323 334
9 of 9 BENARI ET AL 53 Luchsinger JA Reitz C Patel B Tang M X Manly JJ Mayeux R Relation of diabetes to mild cognitive impairment Arch Neurol 2007 64 570575 54 Vipin A Foo HJL Lim JKW et al Regional white matter hyperintensity influences grey matter atrophy in mild cognitive impairment J Alzheimers Dis 2018 66 1 17 55 Inc SI The randomization for this paper was generated using SAS softc 2019 SAS Institute ware Version 9 4 of the SAS System Copyright Inc SAS and all other SAS Institute Inc product or service names are registered trademarks or trademarks of SAS Institute Inc Cary NC USA 2019 56 Wong RHX Scholey A Howe PRC Assessing premorbid cognitive ability in adults with type 2 diabetes mellitus a review with implications for future intervention studies Curr Diab Rep 2014 14 547 57 Marshall GA Rentz DM Frey MT et al Executive function and instrumental activities of daily living in mild cognitive impairment and Alzheimer s disease Alzheimers Dement 2011 7 300 308 58 Salloway S Ferris S Kluger A et al Efficacy of donepezil in mild cognitive impairment a randomized placebo controlled trial Neurology 2004 63 651 657 59 Palta P Schneider AL Biessels GJ Touradji P Hill Briggs F Magnitude of cognitive dysfunction in adults with type 2 diabetes a meta analysis of six cognitive domains and the most frequently reported neuropsychological tests within domains J Int Neuropsychol Soc 2014 20 278291 60 Dunn G Complier average causal effect CACE estimation In Lovric M ed International Encyclopedia of Statistical Science Berlin Heidelberg Springer Berlin Heidelberg 2011 273 274 61 Boussi Gross R Golan H Fishlev G et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 2013 8 e79995 62 B sing KA Sch nberg SO Brade J Wasser K Impact of blood glucose diabetes insulin and obesity on standardized uptake values in tumors and healthy organs on 18F FDG PET CT Nucl Med Biol 2013 40 206213 63 Zhao D Luo S Xu W Hu J Lin S Wang N Efficacy and safety of hyperbaric oxygen therapy used in patients with diabetic foot a metaanalysis of randomized clinical trials Clin Ther 2017 39 2088 2094 e2 64 Xu Y Wang Q Qu Z Yang J Zhang X Zhao Y Protective effect of hyperbaric oxygen therapy on cognitive function in patients with vascular dementia Cell Transplant 2019 28 8 1071 1075 65 Thompson LW Davis GC Obrist WD Heyman AH Effects of hyperbaric oxygen on behavioral and physiological measures in elderly demented patients J Gerontol 1976 31 23 28 66 Raskin A Gershon S Crook TH Sathananthan G Ferris S The effects of hyperbaric and normobaric oxygen on cognitive impairment in the elderly Arch Gen Psychiatry 1978 35 50 56 67 Wang S Tao Z Ding S Cheng J Bensong Y Wang Y Hyperbaric oxygen combined with donepezil in the treatment of vascular dementia Chinese J Physical Med Rehabilitat 2009 31 478 480 68 Rocco M D Itri L De Bels D Corazza F Balestra C The normobaric oxygen paradox a new tool for the anesthetist Minerva Anestesiol 2014 80 72 69 Neuman TS Thom SR Physiology and Medicine of Hyperbaric Oxygen Therapy E Book NewYork NY Elsevier Health Sciences 2008 70 Yu Q Fang D Swerdlow RH Yu H Chen JX Yan SS Antioxidants rescue mitochondrial transport in differentiated Alzheimer s disease transmitochondrial cybrid cells J Alzheimers Dis 2016 54 679 690 SUPPORTING INFORMATION Additional supporting information may be found online in the Supporting Information section at the end of the article How to cite this article BenAri O Efrati S Sano M et al A double blind placebo controlled clinical trial testing the effect of hyperbaric oxygen therapy on brain and cognitive outcomes of mildly cognitively impaired elderly with type 2 diabetes Study design Alzheimer s Dement 2020 6 e12008 https doi org 10 1002 trc2 12008
www aging us com AGING 2021 Vol 13 No 17 Research Paper Hyperbaric oxygen therapy alleviates vascular dysfunction and amyloid burden in an Alzheimer s disease mouse model and in elderly patients Ronit Shapira1 Amos Gdalyahu1 Irit Gottfried1 Efrat Sasson4 Amir Hadanny4 Shai Efrati2 3 4 Pablo Blinder1 2 Uri Ashery1 2 1 School of Neurobiology Biochemistry and Biophysics The George S Wise Faculty of Life Sciences Tel Aviv University Tel Aviv Israel 2 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel 3 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 4 Sagol Center for Hyperbaric Medicine and Research Assaf Harofeh Medical Center Be er Ya akov Israel Correspondence to Uri Ashery email uria tauex tau ac il Keywords Alzheimer s disease hyperbaric oxygen therapy vascular dysfunction cerebral blood flow amyloid burden Received March 4 2021 Accepted August 10 2021 Published September 9 2021 Copyright 2021 Shapira et al This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY 3 0 which permits unrestricted use distribution and reproduction in any medium provided the original author and source are credited ABSTRACT Vascular dysfunction is entwined with aging and in the pathogenesis of Alzheimer s disease AD and contributes to reduced cerebral blood flow CBF and consequently hypoxia Hyperbaric oxygen therapy HBOT is in clinical use for a wide range of medical conditions In the current study we exposed 5XFAD mice a well studied AD model that presents impaired cognitive abilities to HBOT and then investigated the therapeutical effects using two photon live animal imaging behavioral tasks and biochemical and histological analysis HBOT increased arteriolar luminal diameter and elevated CBF thus contributing to reduced hypoxia Furthermore HBOT reduced amyloid burden by reducing the volume of pre existing plaques and attenuating the formation of new ones This was associated with changes in amyloid precursor protein processing elevated degradation and clearance of A protein and improved behavior of 5XFAD mice Hence our findings are consistent with the effects of HBOT being mediated partially through a persistent structural change in blood vessels that reduces brain hypoxia Motivated by these findings we exposed elderly patients with significant memory loss at baseline to HBOT and observed an increase in CBF and improvement in cognitive performances This study demonstrates HBOT efficacy in hypoxia related neurological conditions particularly in AD and aging INTRODUCTION In recent years it has become clear that vascular dysfunction is entwined in the pathogenesis of Alzheimer s disease AD and cognitive decline during aging 1 3 Vascular risk factors such as obesity diabetes atherosclerosis smoking and hypertension are major risk factors for AD 4 Cerebral amyloid angiopathy CAA the deposition of A peptide in cerebral vessel walls is the most common vascular pathology in AD 5 6 Both AD and CAA are associated with reduced cerebral blood flow CBF www aging us com 20935 which precedes the clinical onset of dementia 7 10 and correlates with the degree of cognitive impairment in AD 1 11 Accordingly CBF has been proposed as a marker for disease severity 12 Cerebral hypoperfusion 13 15 and the cerebral hypoxia that ensues 16 17 have also been detected in animal models of AD This hypoperfusion has been attributed to several mechanisms including reduced vascular density 18 19 constriction of cerebral arterioles 20 21 and impaired neurovascular coupling 22 23 Cerebral hypoperfusion is also associated with accelerated cognitive decline 3 24 and increased risk AGING
of dementia in the general population 2 Therefore developing treatments that target vascular dysfunction as well as other AD pathologies could be a promising avenue for treating the disease and improving cognitive performances in healthy elderly populations suffering from cognitive decline cerebral hypoxia by increasing blood vessel diameter Furthermore by tracking single plaques in vivo over weeks we show for the first time that HBOT reduces the volume of pre existing plaques and the appearance of newly formed plaques RESULTS Hyperbaric oxygen therapy HBOT the medical administration of 100 oxygen at environmental pressure greater than one atmosphere absolute ATA 25 is in clinical use for a wide range of medical conditions At present there are only 13 FDA approved indications for HBOT including non healing ischemic wounds post radiation injuries decompression sickness burn repair carbon monoxide intoxication and diabetic ulcers 26 In addition there is a growing number of off label treatments 27 like usages of HBOT to induce neuroplasticity and improve neurocognitive functions in post traumatic brain injuries TBI or post stroke patients 28 29 Further clinical trials that are being performed these days and additional basic scientific studies aiming to understand HBOT s mechanisms of action will most probably expand the use of HBOT to other areas By increasing the dissolved oxygen content of the blood HBOT can sustain tissues with minimal perfusion 25 30 Evidence from clinical studies demonstrated that HBOT induces recovery of cognitive functions in post TBI patients 31 32 by inducing cerebral angiogenesis increasing cerebral blood flow and volume and improving cerebral white and grey microstructures 33 Elevation of CBF and restoration of physical abilities and cognitive functions were also shown in stroke patients 34 35 However our ability to investigate the underlying mechanisms of these HBOT mediated effects in patients is very limited At the same time animal models offer major advantages in advancing our understanding of the cellular and molecular mechanisms leading to increased CBF Recently it was shown that HBOT improved cognitive performance in animal models of Alzheimer s disease 17 36 and improved the metabolic status and cognitive scores of AD and amnestic mild cognitive impairment patients 37 39 However it is not known if HBOT mitigates cerebrovascular dysfunction in AD Therefore we investigated the effects of HBOT on CBF and cognitive decline in the 5XFAD mouse model of AD that presents aggressive accumulation of amyloid load 40 cerebrovascular abnormalities 15 41 42 and cognitive impairment 40 as well as in elderly individuals suffering from significant memory loss We report that HBOT improves CBF and cognitive function in both AD mice and elderly patients with significant memory loss HBOT elevated CBF and reduced www aging us com 20936 HBOT reduces the amyloid load of 5XFAD mice by reducing the number of newly formed plaques and decreasing the volume of existing plaques We first asked if increasing oxygen delivery to the brain by administrating HBOT reduced amyloid burden To that end we employed a custom made HBO chamber to expose 6 month old 5XFAD and wild type wt mice to HBOT at 2 ATA for 60 minutes per day 5 days a week for 4 weeks i e 20 treatments To assess the effect of HBOT on amyloid burden in the treated 5XFAD mice brains were stained with anti A pan antibodies 4G8 directed against epitope 17 24 Figure 1 We found significant reduction in amyloid burden in the hippocampus of HBO treated 5XFAD mice as manifested by the reduced percentage of hippocampal area displaying 4G8 immunoreactivity 54 32 P 0 0353 Figure 1A 1B decreased numbers of plaques 31 58 P 0 0217 Figure 1C and smaller plaque size 18 94 P 0 0125 by Welch s correction Figure 1D relative to control 5XFAD mice exposed to normobaric conditions We then analyzed the levels of soluble TBS fraction and insoluble Formic Acid fraction levels of A 42 and A 40 in the hippocampus by ELISA Figure 1E 1F Following 1 month of HBOT levels of insoluble A 42 were reduced by 56 FA fraction P 0 0292 by Welch s correction Figure 1F while A 40 levels were reduced by 45 FA fraction P 0 0356 Figure 1F in HBO treated 5XFAD mice compared with control 5XFAD mice In contrast soluble A 42 and A 40 levels were unchanged TBS fraction Figure 1E Collectively these data demonstrate that HBOT reduced the amyloid load in the hippocampal formation of 5XFAD mice To study the dynamics of plaque formation and growth in vivo we addressed changes in amyloid plaques before and after HBOT of the same mice by performing longitudinal in vivo two photon imaging via introduction of a cranial window over the barrel cortex 43 We then stained amyloid plaques in vivo with methoxy X04 and imaged the same A plaques before and after one month of exposure to HBOT or control conditions Initially we investigated whether HBOT affected the volume of preexisting plaques by tracing the volume of single plaques before and after each treatment in the same animals Figure 2A 2B AGING
We classified pre existing plaques into sub populations according to their initial volume Figure 2B and evaluated the effect of HBOT on these groups We found that without treatment small pre existing plaques ranging in volume from 2 800 m3 exhibited a greater increment in volume 2 83 fold than did larger preexisting plaques Larger plaques with volumes ranging 801 2000 m3 medium sized plaques showed only a Figure 1 HBOT reduces amyloid plaques in the hippocampal area of 6 month old 5XFAD mice Amyloid plaques were visualized by immunostaining with anti A antibodies 4G8 A Representative images of A in the hippocampal field of HBO treated 5XFAD n 10 lower panel and control 5XFAD mice n 10 upper panel left and middle panels x4 magnification scale bar 1000 m right panel x20 magnification scale bar 200 m B Quantification of the percentage of hippocampal area occupied by plaques C Number of plaques D Mean size of plaques E F Soluble A was initially extracted from hippocampi with TBS by ultracentrifugation and then insoluble A was extracted with 70 formic acid FA after ultra centrifugation ELISA analysis of soluble E and insoluble F A 40 and A 42 in hippocampal lysates of HBO treated 5XFAD and control 5XFAD mice n 5 group B C F t test D F welch correction t test Values represent means SEM P 0 05 P 0 01 www aging us com 20937 AGING
Figure 2 HBOT reduces the population of newly formed plaques and reduces the volume of pre existing plaques Amyloid plaques were visualized in vivo using two photon microscopy imaging in live animals by injecting methoxy X04 24 h before every imaging session A Representative images of plaques in the somatosensory cortex of HBO treated 5XFAD n 4 right panel and control 5XFAD mice n 3 left panel before upper panel and after 1 month of treatment lower panel red circles indicate the change in specific plaques scale bar 50 m B Analysis of the volume of pre existing plaques before and after each treatment in the same animal categorized according to initial plaque size C D Distribution of plaque populations by volume in control 5XFAD C before N 1619 after N 3180 and HBO treated 5XFAD mice D before N 3425 after N 3524 Two way ANOVA with repeated measures and post hoc Fisher LSD tests were performed Values represent means SEM P 0 05 P 0 001 P 0 0001 www aging us com 20938 AGING
1 17 fold increase and plaques with sized 2001 m3 large plaques showed no increase in volume Figure 2B This is in accordance with previous studies that demonstrated that smaller plaques present a higher rate of increased volume relative to larger plaques in AD models 44 45 Strikingly HBOT halted the significant increase in volume of the small pre existing plaques P 0 3387 Figure 2B left panel and facilitated reductions in the volumes of medium sized P 0 0001 Figure 2B middle panel and large plaques P 0 0000001 Figure 2B right panel It should be noted that the initial averaged volume of pre existing plaques was similar between treatment groups at all volume ranges Figure 2B yet HBOT had differential effects on the growth of smaller plaques and the breakdown of larger plaques Averaging all plaque sizes uncovered that in control 5XFAD mice existing plaques increased in size by 12 3 on average over 1 month P 0 0499 while existing plaques in HBOtreated 5XFAD mice decreased by 40 05 on average P 0 001 two way ANOVA with repeated measures data not shown We next analyzed the total number of plaques to learn about pre existing and novel plaques and found that in 5XFAD mice the number of plaques nearly doubled over the course of one month 1 96 fold change suggesting that high and rapid synthesis of newlyformed plaques had occurred Figure 2C However in HBO treated 5XFAD mice the number of plaques was unchanged over the same period 1 03 fold change Figure 2D Assessing the distribution of plaque volumes revealed that while there was a dramatic increase in that plaque population with volumes ranging from 2 400 m3 in control 5XFAD mice over the course of a month in HBO treated 5XFAD mice the distribution of plaque volumes did not change during a month of treatment Figure 2C 2D Taken together these results suggest that HBOT both attenuates the appearance of newly formed plaques and causes a reduction in the volume of pre existing plaques HBOT reduces abnormal processing of amyloid precursor protein and increases levels of A degradation and clearance To understand the molecular mechanisms that contribute to the observed reduction in amyloid burden we next assessed key proteins involved in amyloid precursor protein APP processing and A degradation and clearance First levels of the secretase cleaved Cterminal fragment of APP CTF or C99 and the secretase cleaved C terminal fragment of APP CTF or C83 were measured 46 HBO treatment significantly reduced C99 levels in 5XFAD mice www aging us com 20939 40 41 P 0 0060 Figure 3A 3B and induced no change in levels of the C83 fragment in 5XFAD mice P 0 7198 Figure 3A 3C suggesting that HBOT reduced secretase BACE1 mediated cleavage of APP Indeed BACE1 levels were found to be reduced in the HBO treated mice Supplementary Figure 1C 1D As we previously showed with the 3xTg mouse model 17 the levels of full length APP were also unchanged upon HBO treatment of 5XFAD mice Supplementary Figure 1A 1B whereas the levels of the secretase ADAM10 were reduced by HBOT Supplementary Figure 1C 1E In addition while the levels of presenilin 1 PSE a component of the secretase complex were also significantly reduced in 5XFAD mice following HBOT Supplementary Figure 1C 1E no changes were found in the levels of nicastrin another component of the secretase complex Supplementary Figure 1C 1E HBOT has been shown to affect microglial function and increase A clearance thus contributing to neuroprotection 17 47 Analysis of plaqueassociated microglia showed that following HBOT the number of microglia per plaque increased suggesting that HBOT induced microglial recruitment to the plaques possibly supporting plaque degradation Supplementary Figure 1F We next examined whether HBO treatment affects insulin degrading enzyme IDE a key enzyme responsible for the degradation of A peptides 48 IDE levels were significantly increased in HBO treated 5XFAD mice as compared to controls 72 58 P 0 009 Figure 3D 3E suggesting that HBOT increased A degradation Low density lipoprotein receptorrelated protein 1 LRP1 plays a role in clearing A from the brain across the blood brain barrier and into the systemic circulation 49 50 or clearing A from the parenchyma into neurons 51 and astrocytes 52 LRP1 levels were significantly increased in HBOtreated 5XFAD mice as compared to controls 65 16 P 0 0008 Figure 3F 3G suggesting that HBOT increases A clearance Taken together these results suggest that HBOT attenuates amyloid burden by reducing A synthesis via a decrease in APP cleaving enzymes and by enhancing A elimination via increased activities of degradation and clearance pathways HBOT alleviates the reduction in vessel diameter and increases blood flow and arteriolar lumen size in 5XFAD mice Abnormalities in microvessels found near A plaquedeposited areas in 5XFAD mice contribute to reduced AGING
CBF 15 To gain insight into the effects of HBOT on CBF we used in vivo two photon microscopy to address the cortical vasculature of the same mouse before and after a month of exposure to HBOT or control conditions Figure 4 Such analysis revealed that in control 5XFAD mice there was significant reduction in vessel diameters over the course of the month 8 57 P 0 0002 paired t test Figure 4A 4B In contrast no significant reduction in blood vessel diameters was observed in HBO treated 5XFAD mice 0 53 Figure 4A 4B P 0 2206 paired t test The fold change in vessel diameters showed a downward trend in the control group as compared to the HBOtreated group P 0 0601 t test Figure 4B To measure blood flow velocity in specific blood vessels the vascular serum was labeled with a fluorescent dye FITC conjugated to high molecular weight dextran to prevent dye leakage from the vasculature The velocities of non fluorescent red blood cells RBCs were then tracked on this fluorescent background by tracing RBC movement over distance and time 53 54 RBC velocity was elevated following one month of HBOT as compared to control normobaric conditions yet not significantly control 2 70 HBOT 54 89 fold change P 0 0652 ttest Figure 4C However RBC flow which provides a complete description of blood flow in each vessel showed significant improvement following HBOT control 20 35 HBOT 82 82 fold change P 0 014 t test Figure 4D These results directly show that HBOT alleviated reductions in blood vessel diameter and therefore contributed to increased blood flow in 5XFAD mice Figure 3 HBOT reduces abnormal processing of APP and attenuates A degradation and clearance in 5XFAD mice A Representative immunoblot assays of the carboxyl terminal fragment CTF and CTF B C Quantification of western blots in A presented as percentages of wt control normalized to GAPDH levels n 5 6 group D G Representative immunoblot assays of IDE protein D and LRP1 in F E G Quantification of western blots in D F respectively presented as percentages of wt controls normalized to GAPDH levels n 5 6 group Two way ANOVA and post hoc Fisher LSD tests were performed Values represent means SEM P 0 05 P
Finally we double stained the vasculature using antibodies raised against anti smooth muscle actin antibody SMA antibody and A 4G8 antibody and measured arteriolar wall thickness luminal diameter and the A area around arterioles in hippocampal and cortical areas in the brains of mice exposed to HBOT or normobaric conditions Figure 5 In both the hippocampal and cortical areas SMA staining revealed that control 5XFAD mice displayed decreased luminal diameters hippocampus 11 22 P 0 0107 cortex 17 14 P 0 0407 Figure 5A 5B 5F 5G respectively higher arteriolar wall thickness hippocampus 19 75 P 0 0308 cortex 31 74 P 0 0077 Figure 5A 5C 5F 5H respectively and high A deposition around arterioles as compared to wt mice Similar changes were observed in AD patients as compared to non AD controls 55 56 Arteriolar luminal diameter reduction in particular has been suggested to play a role in cerebral hypoperfusion during AD progression 56 Following HBOT the luminal diameter was greatly increased in both hippocampal 13 798 P 0 016 Figure 5A 5B and cortical areas 25 59 P 0 0064 Figure 5F 5G of HBO treated 5XFAD mice as compared to control mice HBO treatment did not change arteriolar wall thickness of 5XFAD mice in Figure 4 HBOT alleviates the reduction in vessel diameter in 5XFAD mice and increases blood flux In vivo two photon microscopy imaging and measurements of diameter and velocity in blood vessels of the somatosensory cortex in 5XFAD mice using spatially optimized line scans A Representative images of fluorescently stained vessels of the somatosensory cortex of an HBO treated 5XFAD mouse right panel and a control 5XFAD mouse left panel before upper panel and after a month of treatment lower panel Line scan patterns are superimposed on the vessels Lines of the scan path along the length were used to calculate RBC velocity V while lines across the diameter of the vessels were used to calculate diameter D The line scans generated from the path can be stacked sequentially as a function of time to produce a raw cascade image right of each image Vessel diameter was calculated as the full width at half maximum of a time average of several scans across the width of a vessel RBC velocity was calculated from the angle of the RBC streaks B D Quantification of vessel diameter B RBC velocity in the blood vessels C and RBC flow D normalized to each treatment group baseline value Paired t tests and student t tests were performed Values represent means SEM P 0 05 P 0 001 www aging us com 20941 AGING
hippocampal areas P 0 4387 Figure 5A 5C yet caused a decrease in wall thickness in cortical areas of treated 5XFAD mice as compared to control mice 16 56 P 0 0477 Figure 5F 5G Finally no changes were measured in A deposition around arterioles in both hippocampal Figure 5D 5E and cortical areas Figure 5I 5J following HBOT These findings corroborate our in vivo imaging results showing a narrowing of blood vessels in 5XFAD mice over a month Figure 4 and suggest a mitigating effect of HBOT on vascular parameters Collectively these results suggest improved blood perfusion following HBOT HBOT reduces hypoxia and hypoxia inducible factor 1 HIF 1 levels in 5XFAD mice We next investigated whether the changes in CBF following HBOT reduced hypoxia in the hippocampal area of 5XFAD mice Fourteen days following the last session of HBO or control treatment mice were injected with Hypoxyprobe a label which is only activated and detectable in hypoxic cells characterized by a partial pressure of oxygen below 10 mm Hg
increase P 0 0076 Figure 6A 6B and CA1 8 19fold increase P 0 0021 Figure 6A 6C as compared with the same areas in their wt counterparts Remarkably HBOT significantly reduced the reactivity of Hypoxyprobe in the hippocampal formation of 5XFAD mice in both CA3 3 11 fold decrease P 0 0145 Figure 6A 6C and CA1 2 48fold decrease P 0 0261 Figure 6A 6C relative to 5XFAD control mice To corroborate our finding and identify the molecular pathway affected by HBOT levels of the oxygen Figure 6 HBOT reduces hypoxia and HIF1 transcription factor levels in the hippocampal area of 6 month old 5XFAD mice A Uptake of Hypoxyprobe by low oxygen bearing cells was visualized by immunostaining Representative images of the presence of hypoxia in the hippocampal field of HBO treated wt n 4 right upper panel and 5XFAD mice n 4 right lower panel and control wt n 5 left upper panel and 5XFAD mice n 3 left lower panel x4 magnification scale bar 1000 m B C Quantification of the percentage of the CA3 B and CA1 C areas presenting Hypoxyprobe related fluorescence D Western blots of HIF 1 from hippocampi extracted from HBO treated and control 5XFAD mice and wt littermates E Quantification of Western blots in D presented as percentage of wt control normalized to GAPDH levels n 4 5 group Two way ANOVA and post hoc Fisher LSD tests were performed Values represent means SEM P 0 05 P 0 01 P 0 001 www aging us com 20943 AGING
tension dependent transcriptional factor hypoxia inducible factor 1 HIF 1 were tested Under normoxic conditions HIF 1 is degraded However under hypoxic conditions HIF1 is stabilized and its levels are increased 57 HIF1 levels increased in 5XFAD mice as compared to wt littermates 55 17 P 0 0003 Figure 6D 6E HBOT significantly reduced HIF1 levels in 5XFAD mice 24 12 P 0 0056 Figure 6D 6E Taken together these experiments indicate a high degree of hypoxia in the hippocampal area of 5XFAD mice that can be significantly reduced by HBOT Furthermore these results demonstrate that HBOT reduced the hypoxic state in 5XFAD mice even 14 days after the last HBO session suggesting that HBOT induced a long lasting effect by increasing arteriolar lumen volume and elevating blood flow HBOT improves the performance of 5XFAD mice in behavioral tasks Finally we explored if the mitigating effects of HBO treatment on AD pathology are associated with an improvement in the performance of 5XFAD mice in behavioral tasks We found that HBO treated 5XFAD mice showed improved nest construction abilities given how they built nests with higher walls and attained higher nest scores Supplementary Figure 2 Moreover the treated mice showed improved exploratory behavior as compared to control 5XFAD mice Supplementary Figure 2 Spatial recognition memory was investigated by testing the natural preference of mice for exploring novel over familiar spatial contexts in a Y maze test Figure 7A Control 5XFAD mice showed a decreased time index in this assay as compared to their wt littermates wt control 0 7367 0 02168 vs 5XFAD control 0 5596 0 03382 P 0 00013 Figure 7A HBOT significantly reversed this trend 5XFAD HBO 0 6572 0 03378 vs 5XFAD control 0 5596 0 03382 P 0 0362 Figure 7A We then tested the effect of HBOT on hippocampus dependent contextual memory by performing trace fear conditioning 58 60 Control 5XFAD mice showed impaired contextual memory relative to their wt littermates as reflected by lower freezing activity in the training chamber 24 h following conditioning wt control 23 29 3 140 vs 5XFAD control 12 81 2 516 P 0 0377 Figure 7B Interestingly this impairment was recovered in HBOtreated 5XFAD mice 5XFAD HBO 29 10 4 321 vs 5XFAD control 12 81 2 516 P 0 0019 Figure 7B Taken together these results suggest that HBOT ameliorated the performances of 5XFAD mice in memory and behavioral tasks HBOT increases cerebral blood flow and improves cognitive performances in elderly patients To understand whether the ability of HBOT to change CBF and affect cognitive function also applied to elderly people we performed a human study NCT02790541 in which six elderly patients age 70 00 2 68 years with significant memory loss at baseline memory domain score 100 were treated with HBOT 60 daily HBOT sessions within 3 months CBF and cognitive function were evaluated before and after HBOT CBF was measured by MRI dynamic susceptibility contrast sequential imaging while Figure 7 HBOT improves performance of 5XFAD mice in cognitive tasks A In the Y maze test HBO treated 5XFAD mice showed better spatial memory as reflected in the time index which is displayed as the ratio novel novel familiar to time in each arm B In the trace fear conditioning assay mice underwent conditioning involving 6 rounds of tone shock pairing with a trace interval On the following day the mice were exposed to the same context with no exposure to tone or shock Results of contextual freezing are expressed as the percent of total time spent frozen in the training context Two way ANOVA with without repeated measures and post hoc Fisher LSD tests were performed Values represent means SEM P 0 05 P 0 01 P 0 001 www aging us com 20944 AGING
cognitive functions were evaluated using computerized cognitive tests Following HBOT there were significant CBF increases in several brain areas including Brodmann areas 1 2 32 34 40 42 43 and 48 Figure 8A 8B At baseline patients attained a mean global cognitive score 102 4 7 3 similar to the average score in the general population normalized for age and education level 100 while memory scores were significantly lower 86 6 9 2 Cognitive assessment following HBOT revealed a significant increase in the global cognitive score 102 4 7 3 to 109 5 5 8 p 0 004 where memory attention and information processing speed domain scores were the most ameliorated Figure 8C Moreover post HBOT mean memory scores improved to the mean score 100 9 7 8 normalized per age and education level 100 The improvements in these scores correlate with improved short and working memory and reduced times of calculation and response as well as increased capacity to choose and concentrate on a relevant stimulus Together with our findings using an AD mouse model and the similar effects observed following HBO treatment of stroke and TBI patients we suggest that HBOT mediates structural changes in blood vessels that increase CBF reduce brain hypoxia and improve cognitive performance DISCUSSION In recent decades the development of drugs for Alzheimer s disease has primarily targeted beta amyloid and tau pathologies However the failures of recent clinical trials suggest that alternative strategies for AD treatment should be considered 61 63 One promising alternative target is vascular dysfunction as it is detected in the early stages of AD correlates with disease progression and affects disease outcome Improved vascular function and CBF can also improve cognition in the elderly 2 3 9 24 64 In this study we explored this option by manipulating oxygen levels in an Alzheimer s disease mouse model and in an elderly patient population The results revealed that increasing oxygen delivery to the brain through HBO treatment improved several aspects of AD pathology including vascular dysfunction plaque burden and behavior HBOT induced vascular changes also led to increased CBF and reduced cerebral hypoxia that continued weeks after treatment This study also demonstrated that HBOT improved vascular parameters in 5XFAD mice Over the course of one month the diameters of cortical blood vessels in these mice were reduced by 8 5 and as a result the blood flow was decreased by 20 This is in accordance with Poiseuille s model which shows that even minimal changes in vessel diameter can have a dramatic effect on the rate of blood flow e g blood vessel narrowing by 6 reduces blood flow by 22 65 66 In 5XFAD mice neutrophil adhesion led to stalled capillaries and reduced CBF 15 Indeed narrower vessels as we observed can accelerate neutrophil adhesion and lead to stalled capillaries HBOT alleviated the thinning of and increased the flow of blood in cortical blood vessels Moreover we showed that the HBOT induced increase in blood flow Figure 8 CBF and cognitive function are improved following HBOT of patients CBF and cognitive functions of six patients suffering from memory decline at baseline and following 60 HBOT sessions A Average normalized CBF maps DSC at baseline and post HBOT B Significant average CBF changes in Brodmann areas at baseline and post HBOT C Average cognitive domain scores Neurotrax at baseline and post HBOT www aging us com 20945 AGING
was accompanied by an elevation of arteriole luminal diameters and a reduction in hypoxia in 5XFAD mice Interestingly reduced hypoxia was detected even 14 days after the last round of HBO treatment suggesting that structural changes in blood vessels contribute to the reduced CBF of 5XFAD mice and that HBOT can significantly alleviate this reduction in turn leading to reduced cerebral hypoxia Hence HBOT induces changes in the basic pathophysiology of the disease which last at least for 2 weeks after HBOT is completed Increased CBF and higher oxygen delivery can improve or boost brain function HBOT induces cognitive enhancement in both young 67 and elderly healthy subjects through regional changes in CBF 68 HBOT has also been shown to increase CBF and improve EEG measurements 34 global cognitive scores 33 69 and PET scans 70 of post stroke and TBI patients In the context of Alzheimer s disease animal studies have shown that supplementation of oxygen 71 72 or HBOT 17 36 results in improved cognitive performance 71 and enhanced cerebral blood volume 72 Moreover an immediate increase in CBF due to a reduction in the number of stalled capillaries led to rapid improvement in the performance of 5XFAD mice in spatial and working memory tasks 15 Recent human studies have shown that HBOT can improve cognitive functions of mild cognitive impairment MCI AD and vascular dementia patients 37 39 73 and ameliorate the reduced brain metabolism of MCI and AD patients 37 39 Here we showed that HBOT increases CBF and improves cognitive function in elderly individuals suffering from significant memory loss as well as increasing CBF alleviating cerebral hypoxia and improving behavioral deficits in 5XFAD mice Yet as the number of subjects in our human HBOT experiments was relatively small n 6 expanding these efforts with a larger cohort could strengthen our findings Taken together these data suggest that oxygen is a rate limiting factor for both normal cognitive function and for tissue recovery in Alzheimer s disease Tracking plaques in the somatosensory cortex over time provided insight into the dynamics of plaques in vivo and revealed that over one month the number of plaques in 5XFAD mice nearly doubled with their volume increasing suggesting that high and rapid synthesis of plaques occurs in this model Moreover small plaques exhibited greater size increments relative to larger plaques This is in agreement with other reports 44 45 74 although not with the work of Hefendehl et al 75 Remarkably HBOT reduced the appearance of newly formed plaques and contributed to a reduction in the size of existing medium sized to large www aging us com 20946 plaques suggesting that HBOT affects both the synthesis of A and its degradation and clearance This claim is further supported by our findings that HBOT attenuated the excessive generation of A 42 and formation of A plaques by reducing levels of BACE1 secretase and presenilin1 a component of the secretase leading to reduced levels of the C terminal A fragment CTF C99 and of the insoluble fraction of A 42 In addition HBOT elevated IDE and LRP1 levels thus promoting A degradation and clearance These findings are in accordance with evidence showing that elevating either activity of the degradation pathway by enhancing IDE levels 76 77 or of clearance pathway by changing LRP1 levels 78 leads to a reduction in amyloid burden Our finding that the number of microglia per plaque volume increased following HBOT suggests that microglia were recruited to plaques possibly supporting plaque degradation 79 80 Taken together it seems that HBOT ameliorates the pathways of A 42 generation accumulation and degradation and thus contributes to the reduced appearance of novel plaques and breakdown of existing plaques Accumulating evidence has demonstrated that cerebral hypoperfusion and hypoxia result in A generation and accumulation 81 83 Hypoxia induces A generation by facilitating and secretase cleavage of APP 84 87 and A accumulation by decreasing levels of enzymes responsible for A degradation such as neprilysin NEP 88 90 and IDE 91 Indeed most AD patients present CAA and degenerative changes affecting arterioles and capillaries and many show ischemic parenchymal abnormalities These are the result of structural vascular disease and or reduction in blood flow in critical brain areas 92 93 Eliminating A via the vasculature is an important route for clearing brain A such that impairment of this process due to cerebral hypoperfusion results in A accumulation and the generation of vascular amyloidosis and dense core plaques 94 This positive feedback loop in which vascular factors increase neurodegenerative deterioration and vice versa facilitates disease progression 95 Here we have shown that HBOT reduces hypoxia increases CBF and ameliorates arterioles structure as well as promoting A degradation and clearance resulting in reduced amyloid burden These findings further show the tight interplay between vascular pathology and neurodegeneration and demonstrate the potency of HBOT in countering hypoxia related neurological conditions particularly AD In summary we showed here that HBOT offers multifaceted neuroprotective effects on the complex pathology of Alzheimer s disease and also improves CBF and cognition in humans Targeting various pathways involved in the basic pathophysiology of AD AGING
may offer a more potent strategy for modifying disease progression To this point HBOT has been demonstrated to ameliorate the pathology and improve behavior in three AD mouse models namely 3xTg AD 5XFAD and APP PS1 mice 17 36 Given that HBOT is considered a safe and tolerable treatment currently being used in the clinic the increasing number of clinical trials showing that HBOT improves cognitive function in patients suffering from chronic brain damage the pre clinical studies elucidating mechanisms of HBOT action and the fact that there is presently no effective intervention for AD HBOT should be considered as a therapeutic approach to slow the progression or even improve the pathophysiology responsible for this disease MATERIALS AND METHODS Mice Transgenic mice Tg6799 co overexpressing FAD mutations of human APP the Swedish mutation K670N M671L the Florida mutation I716V and the London mutation V717I and PS1 M146L L286V transgenes under transcriptional control of the neuronspecific mouse Thy 1 promoter 40 were used Hemizygous transgenic mice were crossed with C57BL 6 breeders for 10 generations Genotyping was verified by PCR analysis of tail DNA All animal experiments followed the Principles of laboratory animal care NIH publication No 86 23 revised 1985 and were performed in accordance with animal protocols approved by the Tel Aviv University Animal Care Committee Reporting was in accordance with ARRIVE guidelines Hyperbaric oxygen therapy HBOT Six month old male heterozygous 5XFAD mice and wild type wt C57BL 6 littermate mice were randomly assigned to two groups HBO treated and controls exposed to normobaric conditions For HBOT animals were administered 100 oxygen at a pressure of 2 ATA in a custom made monochamber Supplementary Figure 3 intended for small animals for 60 minutes per day 5 days a week for 4 weeks i e 20 treatments Before compression was initiated the monochamber was washed with 100 oxygen for 5 min to enrich oxygen content Compression and decompression were performed gradually over 5 min Oxygen levels inside the chamber following compression reached saturation of 96 as measured by an oxygen analyzer 320BRC model Teledyne Analytical Instruments Animals in the control group were placed inside the monochamber for 60 min at 1 ATA without additional treatment n 20 www aging us com 20947 Behavioral testing The effects of HBOT on mouse memory and behavior were evaluated using a battery of behavioral tests The nest building test was administered before and after 1 month of HBOT or control treatments Tests were performed 24 h following the last HBOT control treatment and was ended 48 h prior to sacrifice to reduce stress Y maze test Mice were placed at the distal end of the entrance arm and allowed to explore the maze for 5 min with only the familiar arm available for exploration After a 2 min delay the mice were reintroduced into the maze with two arms familiar and novel available for exploration and documented for 2 min The ratios of time spent and the frequency of visits to the novel arm were calculated as the time or visit frequency in the novel arm divided by the sum of time or visit frequency in both the novel and familiar arms The maze was cleaned with 40 ethanol between sessions Arms were changed randomly between animals yet were kept similar for each animal Trace fear conditioning Mice were placed in a training chamber After a 120 s baseline period the mice received five pairings of the Conditional stimulus CS tone 5 kHz 70 dB and Unconditional stimulus US shock 2 s 0 7 mA The CS and US were separated by a 18 s empty trace interval which increased hippocampal dependency The inter trial interval was set at 90 s 96 The training chamber was wiped with 40 ethanol between sessions Twenty four hours later the mice were again placed in the training chamber and the percentage of behavioral freezing i e the absence of all but respiratory movement during a 5 min test session was measured contextual memory using a FreezeFrame automated scoring system Coulbourn Instruments Biochemical and histological analyses Mice were anesthetized with ketamine and xylazine and perfused transcardially with PBS Brains were then excised and halved and each hemisphere was further processed for either biochemical or histological analysis as outlined below Antibodies used in this project are listed in Supplementary Table 1 Immunochemistry One brain hemisphere was fixed overnight with 4 paraformaldehyde in 0 1 M phosphate buffer pH 7 4 and AGING
then placed in 30 sucrose for 48 h Frozen coronal sections 30 m were then cut on a sliding microtome collected serially and stored in cryoprotectant containing glycerin ethylene glycol and 0 1 M sodium phosphate buffer pH 7 4 at 20 C until use Three four freefloating sections per animal at bregma 1 35 mm and bregma 2 78 were immunostained with the following primary antibodies biotinylated mouse anti A 17 24 4G8 1 200 Signet Laboratories and FITC conjugated mouse anti smooth muscle actin SMA 1 1000 SigmaAldrich Sections were first blocked with 10 20 normal goat serum in PBST 0 1 triton x 100 in PBS for 2 h at room temperature and then incubated for 24 h at 4 C with the primary antibodies dissolved in 2 w v normal goat serum in PBST Binding of the primary antibodies was visualized by incubating the sections for 1 5 h at room temperature with secondary antibodies depending on the primary antibodies used The sections were then mounted on slides coated with dry gelatin A staining was similarly performed except that prior to blocking the sections were incubated with 70 formic acid for 6 min to increase antigen retrieval before antibody staining The sections were visualized using an EVOS FL microscope Thermo Fisher 4 and 20x magnifications or a confocal scanning laser microscope SP8 LEICA Control experiments revealed no staining in sections that lacked the first antibodies and were used to determine the threshold for intensity quantification Intensity of the immunofluorescent staining above threshold level was calculated with the Image Pro Plus system version 5 1 Media Cybernetics For SMA analysis images were acquired from arterioles in cortical and hippocampal areas using a confocal microscope Leica SP8 40 magnification All images were acquired in a random manner blinded to subject Vessels showing positive SMA signals and ranging in size from 10 50 m were analyzed with FIJI ImageJ software National Institutes of Health Bethesda MD A minimum of 10 and 25 arterioles were imaged for cortical and hippocampal areas per animal respectively For hippocampal arterioles luminal diameter was measured as an average of the inner diameters across the section For penetrating arterioles diameter was assessed by determining the minimum axis of the ellipse which is the arteriolar minor axis Wall thickness of the medial layer was determined by measuring the external and luminal diameters and then taking half of the difference Hypoxyprobe staining On the day the mice were sacrificed half of each treatment group were injected intraperitoneally i p www aging us com 20948 with 60 mg kg of Hypoxyprobe 1 pimonidazole hydrochloride Hypoxyprobe Burlington MA 30 min before tissue harvesting to detect hypoxia Pimonidazole is distributed to all tissues including the brain but only forms stable adducts with thiol groups in proteins peptides and amino acids found in hypoxic cells under conditions of partial pressure of oxygen below 10 mm Hg at 37 C Brains were excised and one brain hemisphere was fixed in paraformaldehyde followed by 30 sucrose as described above Freefloating sections were immunostained with rabbit antipimonidazole antibodies 1 500 and visualized by Alexa Fluor 488 conjugated goat anti rabbit secondary antibodies 1 1000 The sections were then mounted on dry gelatin coated slides and visualized using an EVOS FL microscope Thermo Fisher 4 magnification Immunoblotting One brain hemisphere was snap frozen in liquid nitrogen and stored at 80 C until use The hippocampus was excised on ice at 4 C Proteins were dissolved in 200 l lysis buffer containing 7 5 mM HEPES pH 7 1 5 mM EDTA 1 5 mM EGTA 0 375 mM DTT protease inhibitor cocktail P8340 Sigma phosphatase inhibitor cocktail P5726 Sigma and 2 5 SDS Amresco Pure Technology Grade Protein concentrations were determined using Bradford reagent Bio Rad Laboratories Hercules CA Equal amounts of protein were separated on 4 20 Bis Tris gels BioRad and transferred to nitrocellulose membranes Membranes were blocked overnight in 5 w v non fat milk in 0 1 Tween 20 in Tris buffered saline TBS After blocking the membranes were incubated for 1 h at room temperature with primary antibodies specified in Supplementary Table 1 The membranes were then washed in Tween TBS for 20 min and incubated at room temperature with specific horseradish peroxidase conjugated secondary antibodies as specified in Supplementary Table 1 for 60 min Antibody binding was revealed using enhanced chemiluminescent substrate Pierce and band intensity was quantified with ImageQuant TL software Amersham Glyceraldehyde 3 phosphate dehydrogenase GAPDH levels were used to verify uniform loading of the samples A enzyme linked immunosorbent assay ELISA Protein extraction was prepared by sequential ultracentrifugation of brain sub region homogenates Frozen tissues of hippocampus from 5XFAD mice were weighed and mechanically homogenized in four volumes of ice cold TBS supplemented with protease inhibitors Sigma P8340 phosphatase inhibitors AGING
Sigma P5726 and 2 mM EDTA Samples were ultracentrifuged at 350 000 g for 30 min at 4 C and the collected supernatant was labeled as the protein TBS fraction TBS The pellet was dissolved in 200 l of 70 formic acid supplemented with phosphatase and protease inhibitor cocktails and rotated for 2 h at RT The tubes were then centrifuged at 350 000 g for 30 min at 4 C The supernatant was collected and 20 volumes of 1M Tris were added to generate protein FA fraction FA Levels of A 42 and A 40 in the hippocampus were quantified with a amyloid x 42 ELISA Kit Biolegend 842401 and a amyloid x 40 ELISA Kit Biolegend 842301 respectively Levels of A 42 and A 40 are presented as pg ml A to total protein mg ml protein pg mg For visualization of blood plasma mice were injected with 20 l FITC 5 w v i v Sigma Aldrich via the infraorbital vein before imaging Blood cell velocity was measured in blood vessels using arbitrary scan patterns as previously described 100 The same vessels were assessed prior to and following 1 month of HBO control treatment Procedures for blood flow measurement and analysis have been described previously 54 The diameter of a blood vessel and the velocity of RBCs therein can be combined to determine absolute RBC flux which provides a complete description of blood flow in each vessel 54 101 and is given by Cranial window generation and two photon imaging where V is the time averaged RBC velocity at the center line of the vessel and D is the lumen diameter 54 Cranial windows were generated as previously reported 97 Carprofen Pfizer 15 g 25 g mouse analgesia was administered sub cutaneously prior to surgery Mice were anesthetized with isoflurane 5 for induction 1 2 thereafter the scalp and connective tissues were excised and the skull was covered with cyanoacrylamide A 3 mm diameter craniotomy was performed over the barrel cortex primary somatosensory cortex Bregma rostral 1 5 lateral 3 mm and a custom made 3 mm cover glass was placed and sealed with cyanoacrylate glue The dry glue was covered with dental acrylic An aluminum metal bar with two traded holes was attached to the skull During surgery and until full recovery the mouse was kept at 37 C using a heated plate Ringer s solution 1 ml was administered sub cutaneous after surgery For imaging mice were anesthetized with isoflurane 5 for induction 1 5 thereafter in pure oxygen The mice were mounted in a custom made stage using a preattached head bar and their temperature was maintained at 37 C using a heated plate Imaging was conducted with a custom modified two photon laser scanning microscope based on a Sutter MOM apparatus controlled by MPScope 2 0 software 98 using 810 nm excitation For plaque imaging mice n 3 4 per group were injected i p with 10 mg kg methoxy X04 TOCRIS 4920 batch no 2A 175057 5 mg ml in 10 DMSO 45 propylene glycol 45 PBS pH 7 5 24 h prior to each imaging session 99 The same 3 4 fields of view 200 400 m in depth were imaged per animal before and after 1 month of exposure to HBOT or control treatments and plaques were sorted according to their volume 3D reconstruction of the Methoxy X04 plaques was done using Imaris V7 1 1 software Imaris RRID SCR_007370 www aging us com 20949 Flow 8 VD 2 Human subjects The study population comprised adults 5 males 1 female with significant memory decline aged 64 years and older who lived independently and who were in good functional and cognitive status The study was performed between 2016 2020 at the Shamir AssafHarofeh Medical Center Israel Patients included in the study did not have cardiac or cerebrovascular ischemia histories for the last year prior to inclusion Exclusion criteria included previous treatment with HBOT for any reason during the last three months any history of malignancy during the last year any pathological cognitive decline severe chronic renal failure GFR 30 uncontrolled diabetes mellitus HbA1C 8 fasting glucose 200 taking immunosuppressants MRI contra indications active smoking or pulmonary diseases Recruitment was based on social media posts and advertisements The study protocol was approved by the Institutional Review Board of Shamir Medical Center 0172 15 ASF Clinical trial registration NCT02790541 HBO treatment of human subjects HBOT protocol was administered in a multiplace Starmed 2700 chamber Haux Germany The protocol consisted of 60 daily sessions at 5 sessions per week within a three month period Each session included breathing 100 oxygen by mask at 2ATA for 90 min with 5 min air breaks every 20 min Compression and decompression rates were 1 m min Cognitive assessments Cognitive functions were assessed using the NeuroTrax computerized testing battery supervised by a certified AGING
neuropsychologist NeuroTrax tests evaluate multiple aspects of brain cognitive function including memory executive function attention information processing speed visual spatial verbal and motor skills The global cognitive domain evaluates the overall performance in all of the above categories Cognitive domain scores were normalized for age gender and education Participants completed validated alternate test forms of the NeuroTrax test battery at baseline and post HBOT to allow for iterative administration with minimal learning effects Test retest reliability of the tests was found to be high in both normal and injured populations without significant learning effects except in the verbal fluency VF and visual spatial VS domains that were not evaluated in the current study MRI scans MRI scans were performed on a MAGNETOM Skyra 3T scanner configured with 20 channel receiver head coils Siemens Healthcare Erlangen Germany Fifty T2 weighted gradient echo echo planar imaging EPI volumes were acquired Two repetitions were performed before a bolus injection of gadoliniumDTPA Gd DTPA 0 2 ml kg administered at 5 ml sec and 48 repetitions were performed after injection of GdDTPA Sequence parameters were TR 2 300 ms TE 40 ms flip angle 30 voxel size 1 8 x1 8 matrix 128 x 128 number of slices 25 and slice thickness 3 9 mm Pre processing of the perfusion MRI data was preformed using SPM software version 12 UCL London UK and included motion correction and coregistration with MPRAGE T1 images Individual gray matter GM and white matter WM segmentation of T1 anatomy was also performed to extract mean perfusion values Whole brain quantitative perfusion analysis was done as described 102 103 CBF values were normalized Statistical analysis Statistical analyses performed are described in each figure legend Data from nest building test and twophoton microscopy experiments were analysed by twoway ANOVA repeated measures followed by a Fisher LSD post hoc test Comparing analysis of all 4 treatment genotype groups was done using two way ANOVA followed by a Fisher LSD post hoc test Student s t test and t test with Welch s correction were used to compare two groups of data Data are presented as mean standard error of the mean SEM For all analyses statistical significance was accepted at P 0 05 and trends were defined when P 0 10 For MRI analysis and cognitive tests of humans the Kolmogorov Smirnov test paired T tests and FDR www aging us com 20950 corrections were used For MRI analysis spatial normalization to the MNI Montreal Neurological Institute atlas followed by gaussian smoothing of 4 mm FWHM full width at half maximum was applied Abbreviations AD Alzheimer s disease CTF secretase cleaved Cterminal fragment A amyloid beta APP amyloid precursor protein ATA atmosphere absolute BACE1 secretase 1 CTF secretase 1 cleaved C terminal fragment CAA cerebral amyloid angiopathy CBF cerebral blood flow HBOT hyperbaric oxygen therapy HIF 1 hypoxia inducible factor 1 IDE insulin degrading enzyme LRP1 low density lipoprotein receptor related protein 1 MCI mild cognitive impairment PSE presenilin 1 RBCs red blood cells TBI traumatic brain injury AUTHOR CONTRIBUTIONS RS performed all 5XFAD mice experiments and analysis and was involved in writing the manuscript AG was involved in performing the two photon experiments and writing the manuscript IG was involved in coordinating some of the experiments and writing the manuscript ES was involved in performing and analyzing the MRI data AH was involved in performing human related experiments SE was involved in designing some of the experiments in discussions and writing the manuscript PB coordinated the two photon experiments was involved in experiment design and analysis and UA was involved in coordinating the study designing experiments analysis and writing the manuscript ACKNOWLEDGMENTS We thank Dr Lior Bikovski for help with the behavioral tests carried out at the Myers Neuro Behavioral Core Facility of Tel Aviv University We also thank Drs Robert Vasssar and Danny Frenkel for providing the 5XFAD mice and Drs Eitan Okun and Tomer Illouz for constructive discussions We further thank Mr Israel Shreger help in building the HBO chamber CONFLICTS OF INTEREST The authors declare that they have no conflicts of interest AH ES work for AVIV Scientific LTD SE is a co founder and shareholder at AVIV Scientific LTD FUNDING This work was supported in part by the Israeli Ministry of Science Technology and Space grant 3 12069 and AGING
Israel Science Foundation ISF grants 953 16 and 2141 20 and the Deutsche Forschungsgemeinschaft DFG NA 207 10 1 and The Aufzien Family Center for the Prevention and Treatment of Parkinson s Disease at Tel Aviv University to U A and by the European Research Council ERC 639416 and Israel Science Foundation ISF grants 1019 15 and 1994 15 to P B 2016 7 11934 https doi org 10 1038 ncomms11934 PMID 27327500 8 de Eulate RG Go i I Galiano A Vidorreta M Recio M Riverol M Zubieta JL Fern ndez Seara MA Reduced Cerebral Blood Flow in Mild Cognitive Impairment Assessed Using Phase Contrast MRI J Alzheimers Dis 2017 58 585 95 https doi org 10 3233 JAD 161222 PMID 28453476 9 Ruitenberg A den Heijer T Bakker SL van Swieten JC Koudstaal PJ Hofman A Breteler MM Cerebral hypoperfusion and clinical onset of dementia the Rotterdam Study Ann Neurol 2005 57 789 94 https doi org 10 1002 ana 20493 PMID 15929050 REFERENCES 1 2 3 4 5 Roher AE Debbins JP Malek Ahmadi M Chen K Pipe JG Maze S Belden C Maarouf CL Thiyyagura P Mo H Hunter JM Kokjohn TA Walker DG et al Cerebral blood flow in Alzheimer s disease Vasc Health Risk Manag 2012 8 599 611 https doi org 10 2147 VHRM S34874 PMID 23109807 Wolters FJ Zonneveld HI Hofman A van der Lugt A Koudstaal PJ Vernooij MW Ikram MA and Heart Brain Connection Collaborative Research Group Cerebral Perfusion and the Risk of Dementia A PopulationBased Study Circulation 2017 136 719 28 https doi org 10 1161 CIRCULATIONAHA 117 02744 8 PMID 28588075 Akoudad S Wolters FJ Viswanathan A de Bruijn RF van der Lugt A Hofman A Koudstaal PJ Ikram MA Vernooij MW Association of Cerebral Microbleeds With Cognitive Decline and Dementia JAMA Neurol 2016 73 934 43 https doi org 10 1001 jamaneurol 2016 1017 PMID 27271785 Santos CY Snyder PJ Wu WC Zhang M Echeverria A Alber J Pathophysiologic relationship between Alzheimer s disease cerebrovascular disease and cardiovascular risk A review and synthesis Alzheimers Dement Amst 2017 7 69 87 https doi org 10 1016 j dadm 2017 01 005 PMID 28275702 Vinters HV Cerebral amyloid angiopathy A critical review Stroke 1987 18 311 24 https doi org 10 1161 01 str 18 2 311 PMID 3551211 6 Jellinger KA Alzheimer disease and cerebrovascular pathology an update J Neural Transm Vienna 2002 109 813 36 https doi org 10 1007 s007020200068 PMID 12111471 7 Iturria Medina Y Sotero RC Toussaint PJ MateosP rez JM Evans AC and Alzheimer s Disease Neuroimaging Initiative Early role of vascular dysregulation on late onset Alzheimer s disease based on multifactorial data driven analysis Nat Commun www aging us com 20951 10 Benedictus MR Leeuwis AE Binnewijzend MA Kuijer JP Scheltens P Barkhof F van der Flier WM Prins ND Lower cerebral blood flow is associated with faster cognitive decline in Alzheimer s disease Eur Radiol 2017 27 1169 75 https doi org 10 1007 s00330 016 4450 z PMID 27334014 11 Bradley KM O Sullivan VT Soper ND Nagy Z King EM Smith AD Shepstone BJ Cerebral perfusion SPET correlated with Braak pathological stage in Alzheimer s disease Brain 2002 125 1772 81 https doi org 10 1093 brain awf185 PMID 12135968 12 Binnewijzend MA Schoonheim MM Sanz Arigita E Wink AM van der Flier WM Tolboom N Adriaanse SM Damoiseaux JS Scheltens P van Berckel BN Barkhof F Resting state fMRI changes in Alzheimer s disease and mild cognitive impairment Neurobiol Aging 2012 33 2018 28 https doi org 10 1016 j neurobiolaging 2011 07 003 PMID 21862179 13 Niwa K Kazama K Younkin SG Carlson GA Iadecola C Alterations in cerebral blood flow and glucose utilization in mice overexpressing the amyloid precursor protein Neurobiol Dis 2002 9 61 68 https doi org 10 1006 nbdi 2001 0460 PMID 11848685 14 Li H Guo Q Inoue T Polito VA Tabuchi K Hammer RE Pautler RG Taffet GE Zheng H Vascular and parenchymal amyloid pathology in an Alzheimer disease knock in mouse model interplay with cerebral blood flow Mol Neurodegener 2014 9 28 https doi org 10 1186 1750 1326 9 28 PMID 25108425 15 Cruz Hern ndez JC Bracko O Kersbergen CJ Muse V Haft Javaherian M Berg M Park L Vinarcsik LK Ivasyk I Rivera DA Kang Y Cortes Canteli M Peyrounette M et al Neutrophil adhesion in brain capillaries reduces cortical blood flow and impairs memory function in Alzheimer s disease mouse models Nat Neurosci AGING
2019 22 413 20 https doi org 10 1038 s41593 018 0329 4 PMID 30742116 138 3716 33 https doi org 10 1093 brain awv327 PMID 26598495 16 Lin AJ Liu G Castello NA Yeh JJ Rahimian R Lee G Tsay V Durkin AJ Choi B LaFerla FM Chen Z Green KN Tromberg BJ Optical imaging in an Alzheimer s mouse model reveals amyloid dependent vascular impairment Neurophotonics 2014 1 011005 https doi org 10 1117 1 NPh 1 1 011005 PMID 25133200 17 Shapira R Solomon B Efrati S Frenkel D Ashery U Hyperbaric oxygen therapy ameliorates pathophysiology of 3xTg AD mouse model by attenuating neuroinflammation Neurobiol Aging 2018 62 105 19 https doi org 10 1016 j neurobiolaging 2017 10 007 PMID 29141186 18 Paris D Patel N DelleDonne A Quadros A Smeed R Mullan M Impaired angiogenesis in a transgenic mouse model of cerebral amyloidosis Neurosci Lett 2004 366 80 85 https doi org 10 1016 j neulet 2004 05 017 PMID 15265595 19 Ielacqua GD Schlegel F F chtemeier M Xandry J Rudin M Klohs J Magnetic Resonance Q Mapping Reveals a Decrease in Microvessel Density in the arcA Mouse Model of Cerebral Amyloidosis Front Aging Neurosci 2016 7 241 https doi org 10 3389 fnagi 2015 00241 PMID 26834622 20 Niwa K Porter VA Kazama K Cornfield D Carlson GA Iadecola C A beta peptides enhance vasoconstriction in cerebral circulation Am J Physiol Heart Circ Physiol 2001 281 H2417 24 https doi org 10 1152 ajpheart 2001 281 6 H2417 PMID 11709407 21 Luo F Seifert TR Edalji R Loebbert RW Hradil VP Harlan J Schmidt M Nimmrich V Cox BF Fox GB Noninvasive characterization of beta amyloid 1 40 vasoactivity by functional magnetic resonance imaging in mice Neuroscience 2008 155 263 69 https doi org 10 1016 j neuroscience 2008 04 021 PMID 18534764 22 Louren o CF Ledo A Barbosa RM Laranjinha J Neurovascular uncoupling in the triple transgenic model of Alzheimer s disease Impaired cerebral blood flow response to neuronal derived nitric oxide signaling Exp Neurol 2017 291 36 43 https doi org 10 1016 j expneurol 2017 01 013 PMID 28161255 23 Kimbrough IF Robel S Roberson ED Sontheimer H Vascular amyloidosis impairs the gliovascular unit in a mouse model of Alzheimer s disease Brain 2015 www aging us com 20952 24 Yata K Tomimoto H Chronic cerebral hypoperfusion and dementia Neurol Clin Neurosci 2014 2 129 34 https doi org 10 1111 ncn3 124 25 Thom SR Hyperbaric oxygen its mechanisms and efficacy Plast Reconstr Surg 2011 Suppl 1 127 131S 41S https doi org 10 1097 PRS 0b013e3181fbe2bf PMID 21200283 26 Matera DV Smith B Lam B Revisiting the expanded use of hyperbaric oxygen therapy for treatment of resistant migraines Med Gas Res 2019 9 238 40 https doi org 10 4103 2045 9912 273963 PMID 31898611 27 Price M Hyperbaric Oxygen Therapy The Difference Between FDA Approval and FDA Non Approval 2021 https www rehabmart com post hyperbaric oxygentherapy the difference between fda approval and fdanonapproval 28 Zhai WW Sun L Yu ZQ Chen G Hyperbaric oxygen therapy in experimental and clinical stroke Med Gas Res 2016 6 111 18 https doi org 10 4103 2045 9912 184721 PMID 27867477 29 Pekovic S Dacic S Krstic D Jeremic R Djelic M Brkic P Hyperbaric Oxygen Therapy in Traumatic Brain Injury Cellular and Molecular Mechanisms In Drenjan evi I editor Hyperbaric Oxygen Treatment in Research and Clinical Practice Rijeka IntechOpen 2018 30 Gill AL Bell CN Hyperbaric oxygen its uses mechanisms of action and outcomes QJM 2004 97 385 95 https doi org 10 1093 qjmed hch074 PMID 15208426 31 Hadanny A Abbott S Suzin G Bechor Y Efrati S Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post traumatic brain injury patients retrospective analysis BMJ Open 2018 8 e023387 https doi org 10 1136 bmjopen 2018 023387 PMID 30269074 32 Shandley S Wolf EG Schubert Kappan CM Baugh LM Richards MF Prye J Arizpe HM Kalns J Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy Undersea Hyperb Med 2017 44 257 69 https doi org 10 22462 5 6 2017 6 PMID 28779582 33 Tal S Hadanny A Sasson E Suzin G Efrati S Hyperbaric AGING
Oxygen Therapy Can Induce Angiogenesis and Regeneration of Nerve Fibers in Traumatic Brain Injury Patients Front Hum Neurosci 2017 11 508 https doi org 10 3389 fnhum 2017 00508 PMID 29097988 N Cerebrovascular pathology during the progression of experimental Alzheimer s disease Neurobiol Dis 2016 88 107 17 https doi org 10 1016 j nbd 2016 01 001 PMID 26774030 34 Chen L Li F Gu D Hyperbaric oxygen therapy for cerebral blood flow and electroencephalogram in patients with acute cerebral infarction Choice for therapeutic occasion Neural Regen Res 2007 2 171 74 https doi org 10 1016 S1673 5374 07 60038 3 42 Kook SY Seok Hong H Moon M Mook Jung I Disruption of blood brain barrier in Alzheimer disease pathogenesis Tissue Barriers 2013 1 e23993 https doi org 10 4161 tisb 23993 PMID 24665385 35 Rosario ER Kaplan SE Khonsari S Vazquez G Solanki N Lane M Brownell H Rosenberg SS The Effect of Hyperbaric Oxygen Therapy on Functional Impairments Caused by Ischemic Stroke Neurol Res Int 2018 2018 3172679 https doi org 10 1155 2018 3172679 PMID 30402285 36 Choi J Kwon HJ Lee JE Lee Y Seoh JY Han PL Hyperoxygenation revitalizes Alzheimer s disease pathology through the upregulation of neurotrophic factors Aging Cell 2019 18 e12888 https doi org 10 1111 acel 12888 PMID 30746828 37 Harch PG Fogarty EF Hyperbaric oxygen therapy for Alzheimer s dementia with positron emission tomography imaging a case report Med Gas Res 2019 8 181 84 https doi org 10 4103 2045 9912 248271 PMID 30713673 38 Xu Y Wang Q Qu Z Yang J Zhang X Zhao Y Protective Effect of Hyperbaric Oxygen Therapy on Cognitive Function in Patients with Vascular Dementia Cell Transplant 2019 28 1071 75 https doi org 10 1177 0963689719853540 PMID 31134827 43 Holtmaat A Bonhoeffer T Chow DK Chuckowree J De Paola V Hofer SB H bener M Keck T Knott G Lee WC Mostany R Mrsic Flogel TD Nedivi E et al Longterm high resolution imaging in the mouse neocortex through a chronic cranial window Nat Protoc 2009 4 1128 44 https doi org 10 1038 nprot 2009 89 PMID 19617885 44 Yan P Bero AW Cirrito JR Xiao Q Hu X Wang Y Gonzales E Holtzman DM Lee JM Characterizing the appearance and growth of amyloid plaques in APP PS1 mice J Neurosci 2009 29 10706 14 https doi org 10 1523 JNEUROSCI 2637 09 2009 PMID 19710322 45 Burgold S Bittner T Dorostkar MM Kieser D Fuhrmann M Mitteregger G Kretzschmar H Schmidt B Herms J In vivo multiphoton imaging reveals gradual growth of newborn amyloid plaques over weeks Acta Neuropathol 2011 121 327 35 https doi org 10 1007 s00401 010 0787 6 PMID 21136067 46 Thinakaran G Koo EH Amyloid precursor protein trafficking processing and function J Biol Chem 2008 283 29615 19 https doi org 10 1074 jbc R800019200 PMID 18650430 39 Chen J Zhang F Zhao L Cheng C Zhong R Dong C Le W Hyperbaric oxygen ameliorates cognitive impairment in patients with Alzheimer s disease and amnestic mild cognitive impairment Alzheimers Dement N Y 2020 6 e12030 https doi org 10 1002 trc2 12030 PMID 32548235 47 Heneka MT Kummer MP Stutz A Delekate A Schwartz S Vieira Saecker A Griep A Axt D Remus A Tzeng TC Gelpi E Halle A Korte M et al NLRP3 is activated in Alzheimer s disease and contributes to pathology in APP PS1 mice Nature 2013 493 674 78 https doi org 10 1038 nature11729 PMID 23254930 40 Oakley H Cole SL Logan S Maus E Shao P Craft J Guillozet Bongaarts A Ohno M Disterhoft J Van Eldik L Berry R Vassar R Intraneuronal beta amyloid aggregates neurodegeneration and neuron loss in transgenic mice with five familial Alzheimer s disease mutations potential factors in amyloid plaque formation J Neurosci 2006 26 10129 40 https doi org 10 1523 JNEUROSCI 1202 06 2006 PMID 17021169 48 Miners JS Barua N Kehoe PG Gill S Love S A degrading enzymes potential for treatment of Alzheimer disease J Neuropathol Exp Neurol 2011 70 944 59 https doi org 10 1097 NEN 0b013e3182345e46 PMID 22002425 41 Giannoni P Arango Lievano M Neves ID Rousset MC Baranger K Rivera S Jeanneteau F Claeysen S Marchi www aging us com 20953 49 Ramanathan A Nelson AR Sagare AP Zlokovic BV Impaired vascular mediated clearance of brain amyloid beta in Alzheimer s disease the role regulation and restoration of LRP1 Front Aging Neurosci 2015 7 136 https doi org 10 3389 fnagi 2015 00136 AGING
PMID 26236233 50 Kanekiyo T Liu CC Shinohara M Li J Bu G LRP1 in brain vascular smooth muscle cells mediates local clearance of Alzheimer s amyloid J Neurosci 2012 32 16458 65 https doi org 10 1523 JNEUROSCI 3987 12 2012 PMID 23152628 51 Kanekiyo T Cirrito JR Liu CC Shinohara M Li J Schuler DR Shinohara M Holtzman DM Bu G Neuronal clearance of amyloid by endocytic receptor LRP1 J Neurosci 2013 33 19276 83 https doi org 10 1523 JNEUROSCI 3487 13 2013 PMID 24305823 52 Liu CC Hu J Zhao N Wang J Wang N Cirrito JR Kanekiyo T Holtzman DM Bu G Astrocytic LRP1 Mediates Brain A Clearance and Impacts Amyloid Deposition J Neurosci 2017 37 4023 31 https doi org 10 1523 JNEUROSCI 3442 16 2017 PMID 28275161 53 Dirnagl U Kaplan B Jacewicz M Pulsinelli W Continuous measurement of cerebral cortical blood flow by laser Doppler flowmetry in a rat stroke model J Cereb Blood Flow Metab 1989 9 589 96 https doi org 10 1038 jcbfm 1989 84 PMID 2674168 54 Shih AY Driscoll JD Drew PJ Nishimura N Schaffer CB Kleinfeld D Two photon microscopy as a tool to study blood flow and neurovascular coupling in the rodent brain J Cereb Blood Flow Metab 2012 32 1277 309 https doi org 10 1038 jcbfm 2011 196 PMID 22293983 55 Stopa EG Butala P Salloway S Johanson CE Gonzalez L Tavares R Hovanesian V Hulette CM Vitek MP Cohen RA Cerebral cortical arteriolar angiopathy vascular beta amyloid smooth muscle actin Braak stage and APOE genotype Stroke 2008 39 814 21 https doi org 10 1161 STROKEAHA 107 493429 PMID 18258839 56 Merlini M Wanner D Nitsch RM Tau pathologydependent remodelling of cerebral arteries precedes Alzheimer s disease related microvascular cerebral amyloid angiopathy Acta Neuropathol 2016 131 737 52 https doi org 10 1007 s00401 016 1560 2 PMID 26988843 57 Ogunshola OO Antoniou X Contribution of hypoxia to Alzheimer s disease is HIF 1alpha a mediator of neurodegeneration Cell Mol Life Sci 2009 66 3555 63 https doi org 10 1007 s00018 009 0141 0 PMID 19763399 58 Huerta PT Sun LD Wilson MA Tonegawa S Formation of temporal memory requires NMDA receptors within www aging us com 20954 CA1 pyramidal neurons Neuron 2000 25 473 80 https doi org 10 1016 s0896 6273 00 80909 5 PMID 10719900 59 Misane I Tovote P Meyer M Spiess J Ogren SO Stiedl O Time dependent involvement of the dorsal hippocampus in trace fear conditioning in mice Hippocampus 2005 15 418 26 https doi org 10 1002 hipo 20067 PMID 15669102 60 Fanselow MS Contextual fear gestalt memories and the hippocampus Behav Brain Res 2000 110 73 81 https doi org 10 1016 s0166 4328 99 00186 2 PMID 10802305 61 Anderson RM Hadjichrysanthou C Evans S Wong MM Why do so many clinical trials of therapies for Alzheimer s disease fail Lancet 2017 390 2327 29 https doi org 10 1016 S0140 6736 17 32399 1 PMID 29185425 62 Huang LK Chao SP Hu CJ Clinical trials of new drugs for Alzheimer disease J Biomed Sci 2020 27 18 https doi org 10 1186 s12929 019 0609 7 PMID 31906949 63 Long JM Holtzman DM Alzheimer Disease An Update on Pathobiology and Treatment Strategies Cell 2019 179 312 39 https doi org 10 1016 j cell 2019 09 001 PMID 31564456 64 Zonneveld HI Loehrer EA Hofman A Niessen WJ van der Lugt A Krestin GP Ikram MA Vernooij MW The bidirectional association between reduced cerebral blood flow and brain atrophy in the general population J Cereb Blood Flow Metab 2015 35 1882 87 https doi org 10 1038 jcbfm 2015 157 PMID 26154865 65 de la Torre JC Mussivand T Can disturbed brain microcirculation cause Alzheimer s disease Neurol Res 1993 15 146 53 https doi org 10 1080 01616412 1993 11740127 PMID 8103579 66 de la Torre JC Cerebral hemodynamics and vascular risk factors setting the stage for Alzheimer s disease J Alzheimers Dis 2012 32 553 67 https doi org 10 3233 JAD 2012 120793 PMID 22842871 67 Vadas D Kalichman L Hadanny A Efrati S Hyperbaric Oxygen Environment Can Enhance Brain Activity and Multitasking Performance Front Integr Neurosci 2017 11 25 https doi org 10 3389 fnint 2017 00025 PMID 29021747 68 Hadanny A Daniel Kotovsky M Suzin G Boussi Gross R Catalogna M Dagan K Hachmo Y Abu Hamed R Sasson E Fishlev G Lang E Polak N Doenyas K et al AGING
Cognitive enhancement of healthy older adults using hyperbaric oxygen a randomized controlled trial Aging Albany NY 2020 12 13740 61 https doi org 10 18632 aging 103571 PMID 32589613 69 Harch PG Fogarty EF Staab PK Van Meter K Low pressure hyperbaric oxygen therapy and SPECT brain imaging in the treatment of blast induced chronic traumatic brain injury post concussion syndrome and post traumatic stress disorder a case report Cases J 2009 2 6538 https doi org 10 4076 1757 1626 2 6538 PMID 19829822 70 Golden ZL Neubauer R Golden CJ Greene L Marsh J Mleko A Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy Int J Neurosci 2002 112 119 31 https doi org 10 1080 00207450212027 PMID 12325401 71 Wang H Wang Y Hong X Li S Wang Y Quantitative Proteomics Reveals the Mechanism of Oxygen Treatment on Lenses of Alzheimer s Disease Model Mice J Alzheimers Dis 2016 54 275 86 https doi org 10 3233 JAD 160263 PMID 27567828 72 Shabir O Sharp P Rebollar MA Boorman L Howarth C Wharton SB Francis SE Berwick J Enhanced Cerebral Blood Volume under Normobaric Hyperoxia in the J20hAPP Mouse Model of Alzheimer s Disease Sci Rep 2020 10 7518 https doi org 10 1038 s41598 020 64334 4 PMID 32371859 73 You Q Li L Xiong SQ Yan YF Li D Yan NN Chen HP Liu YP Meta Analysis on the Efficacy and Safety of Hyperbaric Oxygen as Adjunctive Therapy for Vascular Dementia Front Aging Neurosci 2019 11 86 https doi org 10 3389 fnagi 2019 00086 PMID 31057392 74 Dong J Revilla Sanchez R Moss S Haydon PG Multiphoton in vivo imaging of amyloid in animal models of Alzheimer s disease Neuropharmacology 2010 59 268 75 https doi org 10 1016 j neuropharm 2010 04 007 PMID 20398680 75 Hefendehl JK Wegenast Braun BM Liebig C Eicke D Milford D Calhoun ME Kohsaka S Eichner M Jucker M Long term in vivo imaging of amyloid plaque appearance and growth in a mouse model of cerebral amyloidosis J Neurosci 2011 31 624 29 https doi org 10 1523 JNEUROSCI 5147 10 2011 PMID 21228171 76 Li H Wu J Zhu L Sha L Yang S Wei J Ji L Tang X Mao www aging us com 20955 K Cao L Wei N Xie W Yang Z Insulin degrading enzyme contributes to the pathology in a mixed model of Type 2 diabetes and Alzheimer s disease possible mechanisms of IDE in T2D and AD Biosci Rep 2018 38 BSR20170862 https doi org 10 1042 BSR20170862 PMID 29222348 77 Lu XY Huang S Chen QB Zhang D Li W Ao R Leung FC Zhang Z Huang J Tang Y Zhang SJ Metformin Ameliorates A Pathology by Insulin Degrading Enzyme in a Transgenic Mouse Model of Alzheimer s Disease Oxid Med Cell Longev 2020 2020 2315106 https doi org 10 1155 2020 2315106 PMID 32377293 78 Shinohara M Sato N Kurinami H Takeuchi D Takeda S Shimamura M Yamashita T Uchiyama Y Rakugi H Morishita R Reduction of brain beta amyloid Abeta by fluvastatin a hydroxymethylglutaryl CoA reductase inhibitor through increase in degradation of amyloid precursor protein C terminal fragments APP CTFs and Abeta clearance J Biol Chem 2010 285 22091 102 https doi org 10 1074 jbc M110 102277 PMID 20472556 79 Daria A Colombo A Llovera G Hampel H Willem M Liesz A Haass C Tahirovic S Young microglia restore amyloid plaque clearance of aged microglia EMBO J 2017 36 583 603 https doi org 10 15252 embj 201694591 PMID 28007893 80 Martorell AJ Paulson AL Suk HJ Abdurrob F Drummond GT Guan W Young JZ Kim DN Kritskiy O Barker SJ Mangena V Prince SM Brown EN et al Multi sensory Gamma Stimulation Ameliorates Alzheimer s Associated Pathology and Improves Cognition Cell 2019 177 256 71 e22 https doi org 10 1016 j cell 2019 02 014 PMID 30879788 81 Dickstein DL Walsh J Brautigam H Stockton SD Jr Gandy S Hof PR Role of vascular risk factors and vascular dysfunction in Alzheimer s disease Mt Sinai J Med 2010 77 82 102 https doi org 10 1002 msj 20155 PMID 20101718 82 Beach TG Wilson JR Sue LI Newell A Poston M Cisneros R Pandya Y Esh C Connor DJ Sabbagh M Walker DG Roher AE Circle of Willis atherosclerosis association with Alzheimer s disease neuritic plaques and neurofibrillary tangles Acta Neuropathol 2007 113 13 21 https doi org 10 1007 s00401 006 0136 y PMID 17021755 83 Bannai T Mano T Chen X Ohtomo G Ohtomo R Tsuchida T Koshi Mano K Hashimoto T Okazawa H Iwatsubo T Tsuji S Toda T Iwata A Chronic cerebral AGING
hypoperfusion shifts the equilibrium of amyloid oligomers to aggregation prone species with higher molecular weight Sci Rep 2019 9 2827 https doi org 10 1038 s41598 019 39494 7 PMID 30808940 84 Bazan NG Lukiw WJ Cyclooxygenase 2 and presenilin1 gene expression induced by interleukin 1beta and amyloid beta 42 peptide is potentiated by hypoxia in primary human neural cells J Biol Chem 2002 277 30359 67 https doi org 10 1074 jbc M203201200 PMID 12050157 85 Li L Zhang X Yang D Luo G Chen S Le W Hypoxia increases Abeta generation by altering beta and gamma cleavage of APP Neurobiol Aging 2009 30 1091 98 https doi org 10 1016 j neurobiolaging 2007 10 011 PMID 18063223 86 Liu H Qiu H Yang J Ni J Le W Chronic hypoxia facilitates Alzheimer s disease through demethylation of secretase by downregulating DNA methyltransferase 3b Alzheimers Dement 2016 12 130 43 https doi org 10 1016 j jalz 2015 05 019 PMID 26121910 87 Zhang X Zhou K Wang R Cui J Lipton SA Liao FF Xu H Zhang YW Hypoxia inducible factor 1alpha HIF1alpha mediated hypoxia increases BACE1 expression and beta amyloid generation J Biol Chem 2007 282 10873 80 https doi org 10 1074 jbc M608856200 PMID 17303576 88 Nalivaeva NN Belyaev ND Lewis DI Pickles AR Makova NZ Bagrova DI Dubrovskaya NM Plesneva SA Zhuravin IA Turner AJ Effect of sodium valproate administration on brain neprilysin expression and memory in rats J Mol Neurosci 2012 46 569 77 https doi org 10 1007 s12031 011 9644 x PMID 21932040 89 Fisk L Nalivaeva NN Boyle JP Peers CS Turner AJ Effects of hypoxia and oxidative stress on expression of neprilysin in human neuroblastoma cells and rat cortical neurones and astrocytes Neurochem Res 2007 32 1741 48 https doi org 10 1007 s11064 007 9349 2 PMID 17486446 90 Wang Z Zhang XJ Li T Li J Tang Y Le W Valproic acid reduces neuritic plaque formation and improves learning deficits in APP Swe PS1 A246E transgenic mice via preventing the prenatal hypoxia induced down regulation of neprilysin CNS Neurosci Ther 2014 20 209 17 https doi org 10 1111 cns 12186 www aging us com 20956 PMID 24289518 91 de Dios C Bartolessis I Roca Agujetas V BarberoCamps E Mari M Morales A Colell A Oxidative inactivation of amyloid beta degrading proteases by cholesterol enhanced mitochondrial stress Redox Biol 2019 26 101283 https doi org 10 1016 j redox 2019 101283 PMID 31376793 92 Thomas T Miners S Love S Post mortem assessment of hypoperfusion of cerebral cortex in Alzheimer s disease and vascular dementia Brain 2015 138 1059 69 https doi org 10 1093 brain awv025 PMID 25688080 93 Toledo JB Arnold SE Raible K Brettschneider J Xie SX Grossman M Monsell SE Kukull WA Trojanowski JQ Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer s Coordinating Centre Brain 2013 136 2697 706 https doi org 10 1093 brain awt188 PMID 23842566 94 Mazza M Marano G Traversi G Bria P Mazza S Primary cerebral blood flow deficiency and Alzheimer s disease shadows and lights J Alzheimers Dis 2011 23 375 89 https doi org 10 3233 JAD 2010 090700 PMID 21098977 95 Rius P rez S Tormos AM P rez S Tal ns Visconti R Vascular pathology Cause or effect in Alzheimer disease Neurologia Engl Ed 2018 33 112 20 https doi org 10 1016 j nrl 2015 07 010 PMID 26385017 96 Moore MD Cushman J Chandra D Homanics GE Olsen RW Fanselow MS Trace and contextual fear conditioning is enhanced in mice lacking the alpha4 subunit of the GABA A receptor Neurobiol Learn Mem 2010 93 383 87 https doi org 10 1016 j nlm 2009 12 004 PMID 20018248 97 Gdalyahu A Tring E Polack PO Gruver R Golshani P Fanselow MS Silva AJ Trachtenberg JT Associative fear learning enhances sparse network coding in primary sensory cortex Neuron 2012 75 121 32 https doi org 10 1016 j neuron 2012 04 035 PMID 22794266 98 Nguyen QT Dolnick EM Driscoll J Kleinfeld D MPScope 2 0 A computer system for two photon laser scanning microscopy with concurrent plasmamediated ablation and electrophysiology In Frostig RD editor In vivo Optical Imaging of Brain Function 2nd ed Boca Raton FL CRC Press Taylor Francis 2009 117 42 PMID 26844327 AGING
99 Klunk WE Bacskai BJ Mathis CA Kajdasz ST McLellan ME Frosch MP Debnath ML Holt DP Wang Y Hyman BT Imaging Abeta plaques in living transgenic mice with multiphoton microscopy and methoxy X04 a systemically administered Congo red derivative J Neuropathol Exp Neurol 2002 61 797 805 https doi org 10 1093 jnen 61 9 797 PMID 12230326 100 Driscoll JD Shih AY Drew PJ Cauwenberghs G Kleinfeld D Two photon imaging of blood flow in the rat cortex Cold Spring Harb Protoc 2013 2013 759 67 https doi org 10 1101 pdb prot076513 PMID 23906919 101 Shih AY Friedman B Drew PJ Tsai PS Lyden PD Kleinfeld D Active dilation of penetrating arterioles restores red blood cell flux to penumbral neocortex after focal stroke J Cereb Blood Flow Metab 2009 29 738 51 https doi org 10 1038 jcbfm 2008 166 PMID 19174826 www aging us com 20957 102 Ostergaard L Weisskoff RM Chesler DA Gyldensted C Rosen BR High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part I Mathematical approach and statistical analysis Magn Reson Med 1996 36 715 25 https doi org 10 1002 mrm 1910360510 PMID 8916022 103 Ostergaard L Sorensen AG Kwong KK Weisskoff RM Gyldensted C Rosen BR High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part II Experimental comparison and preliminary results Magn Reson Med 1996 36 726 36 https doi org 10 1002 mrm 1910360511 PMID 8916023 AGING
SUPPLEMENTARY MATERIALS Supplementary Methods Quantifying plaque associated microglia For analysis of plaque associated microglia costaining of Iba1 and amyloid plaques was conducted using biotinylated mouse anti A 17 24 4G8 1 200 Signet Laboratories and rabbit anti Iba1 antibodies 1 700 Wako as detailed in Immunochemistry section and the number of microglia associated to plaque and the volumes of plaque m3 in the CA1 area were measured with FIJI Image J software National Institutes of Health Bethesda MD Then microglia number was normalized per plaque volume Open field test Animals were placed in the center of an open field 40 cm 40 cm 30 cm and exploration was assessed for 5 min Cages were cleaned with ethanol following each session Antibodies list All antibodies used are detailed below in Supplementary Table 1 Behavioral testing The effects of HBOT on memory and behavior in mice were evaluated using a battery of behavioral tests Tests were performed 24hr following the last HBO control treatment and finished 48 h prior to sacrifice to reduce stress Nest building test The ability of 5XFAD and wt mice to build a nest over night was assessed prior to and following 1 month of HBOT or control normobaric conditions Mice were placed individually into cages with bedding covering the www aging us com floor to a depth of 0 5 cm and 2 round pressed cotton batting nestlets about one hour before the dark phase and the results were assessed the next morning Results were assessed by scoring nest construction according to the established system of Deacon 1 2 with a 5 point scale and measuring nests height 20958 REFERENCES 1 Deacon R Assessing burrowing nest construction and hoarding in mice J Vis Exp 2012 e2607 https doi org 10 3791 2607 PMID 22258546 2 Deacon RM Assessing nest building in mice Nat Protoc 2006 1 1117 19 https doi org 10 1038 nprot 2006 170 PMID 17406392 AGING
Supplementary Figures Supplementary Figure 1 Western blots of proteins involved in the APP processing pathway in hippocampi extracted from HBO treated and control 5XFAD mice and wt littermates A Representative immunoblots of the full APP protein detected by 6E10 antibodies B Quantification of western blots in A presented as percentages of levels in 5XFAD controls normalized to GAPDH levels n 4 5 group C Representative immunoblots of APP processing enzymes ADAM10 and BACE1 and proteins comprising the secretase complex PSE1 and nicastrin D E Quanti cation of the western blots in C presented as percentages of levels in wt controls normalized to GAPDH levels ADAM10 37 67 P 0 0082 BACE1 18 16 P 0 0011 PSE 25 62 P 0 000001 n 4 5 group Two way ANOVA and post hoc Fisher LSD tests were performed F Values represent means SEM P 0 05 P
Supplementary Figure 2 HBOT improves performance of 5XFAD in behavioral tasks Overnight nest building was assessed by nest building score A and height B before and after a month of HBO or control normobaric treatment of 5XFAD mice and their wt littermates C D In the open field test HBO treated 5XFAD mice show higher locomotive activity than control 5XFAD mice as demonstrated by distances covered C No changes were observed between HBO treated 5XFAD mice and control mice in terms of navigation in the open field as reflected by the number of times the center of the arena was crossed D Values represent means SEM P 0 05 P
Supplementary Table Supplementary Table 1 List of antibodies used for this research Antibody Biotin conjugated anti A mouse mAb 4G8 FITC conjugated mouse anti smooth muscle actin SMA Streptavidin conjugated goat anti rabbit Ab 488 conjugated goat anti rabbit Rabbit anti Iba1 Application IHC Source Covance SIG 39240 Dilution 1 200 IHC Sigma Aldrich F3777 1 1 000 IHC IHC IHC 1 1 000 1 1 000 1 700 HRP conjugated Goat anti rabbit Ab WB HRP conjugated Goat anti mouse Ab WB Mouse anti GAPDH Rabbit anti ADAM10 pAb Rabbit anti BACE1 Rabbit anti Nicastrin mAb Mouse anti Presenilin 1 mAb Rabbit anti Insulin degrading enzyme Rabbit anti Low density lipoprotein receptor related protein 1 WB WB WB WB WB WB Invitrogen S11226 Jackson ImmunoResearch Laboratories WAKO 019 19741 Jackson ImmunoResearch Laboratories 111 035 144 Jackson ImmunoResearch Laboratories 115 035 003 Abcam ab9484 Abcam ab1997 Sigma Aldrich B0681 Cell Signaling D65G7 9447 Chemicon Ab 5232 Abcam ab32216 WB Abcam ab92544 www aging us com 20961 1 10 000 1 15 000 1 1 000 1 500 1 1 000 1 5 000 1 500 1 1 000 1 1 000 AGING
Hussein et al The Egyptian Journal of Neurology Psychiatry and Neurosurgery 2020 56 93 https doi org 10 1186 s41983 020 00225 9 The Egyptian Journal of Neurology Psychiatry and Neurosurgery CASE REPORT Open Access Hyperbaric oxygen therapy after acute ischemic stroke with large penumbra a case report Omar Hussein1 Khalid Sawalha2 Ahmed Abd Elazim1 Diana Greene Chandos1 and Michel T Torbey1 Abstract Background Hyperbaric oxygen therapy HBOT for the treatment of acute stroke has been under the radar for a long time Previous studies have not been able to prove efficacy Several factors might have contributed to such inconsistent results The timing of delivering the hyperbaric oxygen in relation to the stage of stroke evolution may be an important factor This was not taken into account in the previous studies as there was no feasible and standardized method to assess the penumbra in the acute phase Now with the perfusion scan appearing as a key player in the acute stroke management precise stroke patient selection for hyperbaric oxygen therapy deserves a second chance similar to mechanical thrombectomy Case presentation A 62 year old female patient who presented with acute large vessel stroke was not eligible for chemical or mechanical thrombectomy There was a large penumbra on imaging She got treated with several sessions of hyperbaric oxygen over a 2 week period immediately after stroke The patient showed significant improvement on the follow up perfusion imaging as well as some clinical improvement The more impressive radiological improvement was probably due to the presence of relatively large core infarction at baseline affecting functional brain areas The patient continued to improve clinically on her 6 month follow up visit Conclusion Our case demonstrates immediate stroke related penumbra improvement associated with HBOT Based on that we anticipate a potential role for HBOT in acute stroke management considering precise patient selection Future randomized controlled trials are needed and should take that in consideration Keywords Hyperbaric oxygen therapy Acute ischemic stroke HBOT Penumbra Precision medicine Background The ischemic penumbra is the region of the brain that surrounds the core infarcted tissue This region is not apoptotic yet but is at risk of progressing to an expanded core infarction unless an intervention is taken Contrarily cerebral oligemia is the region of the brain tissue that is temporary ischemic following a stroke but is likely to recover spontaneously and thus considered benign In a nutshell a core infarction is an unsalvageable tissue a penumbra is a potentially salvageable tissue but with Correspondence Khalid Sawalhamd baystatehealth org 2 Department of Internal Medicine University of Massachusetts Medical School Baystate Campus Worcester USA Full list of author information is available at the end of the article intervention and finally oligemia is a spontaneously salvageable tissue 1 There have been remarkable advances in brain imaging in the last decade specifically in the perfusion studies In 1980 Dr Leon Axel has set the ground for perfusion scans to be used in mapping the cerebral blood flow by his theoretical analysis at the time 2 With multiple techniques and softwares arising e g RAPID software 3 4 since then differentiation between the core penumbra and oligemia was made possible 5 With such advances vascular neurologists and neuroradiologists are able to determine with high precision the region of ischemic brain that is salvageable This has opened the way to reinvestigate the usefulness of mechanical thrombectomy again The Author s 2020 Open Access This article is licensed under a Creative Commons Attribution 4 0 International License which permits use sharing adaptation distribution and reproduction in any medium or format as long as you give appropriate credit to the original author s and the source provide a link to the Creative Commons licence and indicate if changes were made The images or other third party material in this article are included in the article s Creative Commons licence unless indicated otherwise in a credit line to the material If material is not included in the article s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use you will need to obtain permission directly from the copyright holder To view a copy of this licence visit http creativecommons org licenses by 4 0
Hussein et al The Egyptian Journal of Neurology Psychiatry and Neurosurgery after failing in prior studies IMS III 6 SYNTHESIS EXPANSION 7 and MR RESCUE 8 Failure of these trails was attributed to lack of precision in patient selection due inconsistency in neuroimaging as well as using the Merci device instead of the stent retriever for mechanical thrombectomy From 2015 through 2018 some breakthrough clinical trials MR CLEAN 9 REVA SCAT 10 ESCAPE 11 SWIFT PRIME 12 EXTEND 1A 13 DIFFUSE 3 14 and DAWN 15 has reintroduced mechanical thrombectomy in the management of acute ischemic stroke within a window of up to 24 h from symptoms onset respectively with remarkable success Of note the first three trials have relied on noncontrast CT head and CT angiography while the later four have relied on the perfusion scans RAPID software Consequently mechanical thrombectomy for acute stroke management has made its way in the 2015 and 2018 AHA ASA updated guidelines 16 A large multicenter meta analysis done by the HERMES group 17 showed that favorable outcomes were seen in 46 of patients enrolled in the intervention arm as compared to 27 in the control arm when pooled data from the first 5 trials were analyzed On the other hand When Diffuse 3 and DAWN trials were co analyzed 47 of the intervention group versus 15 of the control group showed favorable outcomes despite of the large window gap for intervention between the two analyses In another analysis by the HERMES group they showed that the estimated ischemic core volume was independently associated with functional independence and functional improvement 18 This indicates that mechanical thrombectomy relies heavily on the perfusion imaging results and thus precise patient selection is warranted Recent human and animal studies showed that the penumbra can extend beyond 48 h and are associated 2020 56 93 Page 2 of 7 with worse outcomes if not treated 19 21 In a DAWN trial subanalysis 21 patients who were enrolled into the study actually met the perfusion imaging criteria but did not meet the time window which extended beyond 24 h The average time from last known well to mechanical thrombectomy was 54 5 h range 24 1 155 7 h The results of this subanalysis were similar to the main DAWN trial It showed that the benefit from mechanical thrombectomy extends beyond the 24 h time window It came to the conclusion that the tissue window based on the perfusion scans is a more accurate parameter than the time window 22 Likewise HBOT for acute cerebral ischemia has failed in the past A recent 2014 Cochrane review 23 concluded that HBOT is not superior to conventional treatment in terms of 6 month mortality rate prior to the mechanical thrombectomy era Despite that few studies showed some functional and clinical improvement on the larger scale these results were inconsistent Logically like mechanical thrombectomy achieving reperfusion and increasing oxygen tension help improving oxygenation to ischemic areas Unlike mechanical thrombectomy HBOT is not expected to reach the core infarction due to blocked blood supply and thus expectedly may have less chance for reperfusion injury Nonetheless mechanical thrombectomy achieves reperfusion whereas HBOT delay tissue demise until revascularization is achieved or a collateral circulation is maintained Again precision in patient selection is a key We present a case of acute symptomatic ICA occlusion who was not a candidate for mechanical or chemical thrombectomy After obtaining the family consent the patient received several sessions of HBOT Fig 1 over 2 weeks immediately after the stroke Remarkable improvement on serial perfusion scans was evident Fig 1 Hyperbaric chamber Image of the used hyperbaric chamber Model 3300 company s name Sechrist Anaheim California USA year of manufacture 2010
Hussein et al The Egyptian Journal of Neurology Psychiatry and Neurosurgery Case presentation A 62 year old fully functioning woman with history of hypertension and obesity presented with sudden onset right sided weakness and global aphasia Her last knownwell was 24 h and thus not eligible for chemical or mechanical thrombectomy Her initial NIH stroke scale NIHSS was 22 CT Head showed left MCA hyperdense sign and watershed hypodensity in the left subcortical area CT Angiography showed a long segment occlusion of left internal carotid artery just cranial to bifurcation extending cranially to the level of carotid terminus There was opacification of left A1 segment via ACOM trace opacification of the left ophthalmic artery and left MCA branches by left posterior communication artery with minimal reconstitution peripherally by the leptomeningeal collaterals Fig 2 The initial CT perfusion CBF 30 and T max 6 0 s showed an ischemic tissue size of 147 ml Fig 3 The patient received the conventional stroke 2020 56 93 Page 3 of 7 therapy for secondary prevention including aspirin 81 mg daily and a lipid lowering medication along with physical therapy and speech therapy The patient required therapeutic hypertension due to blood pressure dependent mental status and aphasia fluctuations indicating unstable collaterals Therapeutic hypertension using vasopressors was maintained for 2 days post stroke Systolic blood pressure was maintained between 160 and 180 mmH2O However the patient received five sessions of hyperbaric oxygen therapy HBOT hyperbaric chamber model 3300 company s name Sechrist Anaheim CA USA year of manufacture 2010 over a 2 week period that started in post stroke day 2 after stopping therapeutic hypertension HBOT was performed in post stroke day 2 PSD 2 PSD 4 PSD 7 PSD 10 and PSD 15 During that period permissive hypertension was allowed Systolic blood pressure was running between 100 and 140 mmH2O Each HBOT session consisted of 2 h 100 O2 at 2 5 ATA Fig 2 Computed tomography angiogram Presenting computed tomography angiographic study showing complete occlusion of left intracranial portion of the internal carotid artery at the level of carotid terminus red arrow a Compared to the patent right middle cerebral artery MCA b there was trace opacification of left MCA branches blue arrow by left posterior communication artery red arrow c with minimal reconstitution peripherally by the leptomeningeal red arrows d
Hussein et al The Egyptian Journal of Neurology Psychiatry and Neurosurgery 2020 56 93 Page 4 of 7 Fig 3 CT perfusion serial computed tomography perfusion studies over 2 weeks using the RAPID software a The initial CT perfusion on presentation showing a core infarction of 58 ml ischemia of 147 ml mismatch volume of 89 ml and mismatch ratio of 2 5 b d Follow up CTperfusion studies after starting hyperbaric oxygen therapy HBOT presented in order showing ischemia reduction b 77 ml c 38 ml and d 48 ml Although there is a slight increase in the penumbra after the fifth session of HBOT a clear trend of penumbra reduction is seen through the follow up studies compared to the initial study Although the amount of clinical improvement is less than the radiological improvement the relatively large core infarction and its location might be the determinant of that perfusion clinical mismatched improvement Serial CT perfusion studies were done after the HBOT sessions Fig 3 The first follow up CT perfusion done after 2 sessions of HBOT showed reduction of the ischemic area to 77 ml Her NIHSS improved to 16 The second follow up CT perfusion after 2 more sessions of HBOT showed further reduction of the ischemic area to 38 ml Her NIHSS improved to 12 The final CT perfusion done after fifth session of HBOT showed near stabilization of the ischemic area at 48 ml Her NIHSS improved to 10 Her global aphasia improved only motor aphasia partially persisted and there was no clinical deterioration despite normalization of the blood pressure after 2 days due to evidence of small intracerebral hemorrhage Her 6 month follow up visit showed improvement of her aphasia and motor functions Her modified ranking scale was four as she still needs assistance with walking Discussion The patient showed significant improvement on the follow up perfusion imaging as well as some clinical improvement The lack of full clinical improvement was probably due to the presence of relatively large core infarction at baseline affecting functional brain areas The proposed beneficial mechanism of HBOT includes counteracting hypoxia by inducing hyperoxemia which leads to improved perfusion and oxygenation of the penumbra and the brain microcirculation 24 While this action seems exciting it is not specific for hyperbaric oxygen and reports of normobaric oxygen therapy NBOT delivery in the acute stroke presumptively lead to the same effect 25 While NBO is feasible quick and easy to use it lacks an equivalent neuroprotective effect as HBOT In an animal study that compared
Hussein et al The Egyptian Journal of Neurology Psychiatry and Neurosurgery HBOT NBOT and normobaric air the HBOT only had significantly smaller infarct size with no difference in the brain oxygenation indicating the presence of neuroprotective effect in the HBOT group 26 The neuroprotective effect of HBOT comes from the antioxidant 27 and anti inflammatory effects associated with it The antioxidant effect is paradoxical and controversial as it has been also reported to induce an oxidative stress injury in the brain However this might be related to whether revascularization prior to HBOT was achieved or not In other words prior revascularization might increase the risk of oxidative injury However preserving HBOT for strokes that are not eligible to revascularization might sound reasonable The anti inflammatory effect is maintained through inhibition of leucocyte activation regulate abnormal cellular metabolites recovering the blood brain barrier and thus reducing the cerebral edema 24 28 32 Other factors leading to neuroprotection with HBOT have been described These include mitochondrial regulation 33 decreased cortical and hippocampal caspase 3 34 increased growth factors 35 and reduction in hypoxia inducible factor 1 36 A major risk of HBOT as mentioned before is the worsened oxidative stress with HBOT leading to glutamate inducted excitotoxic cell death 37 Similar effect was reported with NBOT 38 Another potential risk of HBOT is that it might theoretically lead to a steal phenomenon which can be detrimental This means routing of the blood from the ischemic tissue to the normal brain tissue due to vasodilatation of the vessels on the normal side This occurs when there is a persistent arterial occlusion that lead to hypercarbia in the ischemic region that leads to decreased flow velocities in that region at the expected time of normal brain vasodilatation induced by HBOT 39 leading to blood shift to the normal non ischemic areas This usually leads to worsening of the patient s manifestations after an initial improvement 40 While there has not been reports associating the steal phenomenon with HBOT it remains a potential risk of the treatment The timing of HBOT for acute stroke treatment is another controversial topic While in the past it was believed that the earlier the treatment was started the better the outcomes will be 41 More recently it is believed that later onset whether acutely 2 5 days poststroke or chronically and longer course HBOT has significant effect on neurogeneration 42 44 As previously mentioned the previous 2014 Cochrane review was conducted before the recent breakthrough trials for validation of mechanical thrombectomy guided by the perfusion scans precise selection of patients Despite that the authors found no good evidence to show that HBOT improves clinical outcomes when applied during acute presentation of ischemic stroke this was attributed to insufficient evidence by 11 RCTs 2020 56 93 Page 5 of 7 The possibility of clinical benefit was not excluded Similar reviews discussing failure of mechanical thrombectomy as a treatment for stroke exist before those breakthrough trials However they kept the door opened for further modifications 45 46 Nonetheless reemergence of mechanical thrombectomy after the establishment of reliable brain perfusion scanning pursued 47 48 In the new era of precision medicine 49 and perfusion guided therapy for acute ischemic stroke HBOT as an alternative therapy for acute ischemic stroke for which the traditional reperfusion methods are difficult to achieve should be readdressed This is especially true if a significant penumbra exists Conditions like symptomatic critical carotid stenosis and critical vertebral and or basilar arteries stenosis or occlusion are also eligible especially if the surgical option is contraindicated unachievable or will be delayed While an alternative therapy like therapeutic hypertension is always an option it might have significant side effects like bleeding and or organ damage like myocardial infarction Based on that we anticipate a larger potential role for HBOT in acute stroke management in the future considering precise patient selection Follow up randomized controlled trials RCT should take that in consideration Limitation The intention of this report like any other case report is never to create an attribution association or correlation but to report an observation and draw attention for the need for such RCT Case reports are important tools to report observations Most major discoveries or trials were based on observations from case reports or case series We obtained a CT perfusion scan immediately after each hyperbaric therapy which showed consistent improvement This is the observation that we are reporting This might be the result of natural resolution and thus we recommend that a randomized control trial should be conducted Without the report of observations we will never be able to conduct such trials Nonetheless the persistence of penumbra beyond 48 h is not so common While this might be unexpected by some it strengthen our argument that HBOT might be useful in the prevention of demise of the penumbra Mechanical thrombectomy itself as a treatment for stroke showed initial failure IMS III SYNTHESIS EXPANSION and MR RESCUE Without persistent clinicians reporting association of benefit after precise selection of patients based on the relatively newly developed CT perfusion imaging they would have never been able to re conduct trials like MR CLEAN REVASCAT ESCAPE SWIFT PRIME EXTEND 1A DIFFUSE 3 and DAWN that have proven the correlation
Hussein et al The Egyptian Journal of Neurology Psychiatry and Neurosurgery Another limitation is the presence of a confounding factor for HBOT which is the induced therapeutic hypertension This only lasted for 2 days While this could certainly contribute to the initial improvement the continued improvement over the pursuing 2 weeks while on HBOT might indicate a potential role for such intervention Conclusion HBOT as a salvage therapy for the cerebral ischemic penumbra is potentially beneficial and deserves a second chance of evaluation after precise selection of patients with large vessel occlusion LVO strokes Although it carries potential risks like oxidative injury this is theoretically less significant than those associated with mechanical revascularization as the dead tissue is not subject to such stress HBOT if proven effective can be an alternative adjunctive or back up therapy for the treatment of patients suffering of acute LVO stroke associated with large penumbra and with anticipated delayed or contraindicated mechanical thrombectomy Randomized controlled trials are needed to prove such hypothesis Abbreviations HBOT Hyperbaric oxygen therapy NIHSS National institution of health stroke scale NBOT Normobaric oxygen therapy Acknowledgements Not applicable Machine used Hyperbaric chamber model 3300 company s name Sechrist Anaheim CA USA year of manufacture 2010 MRI Siemens Skyra 3 Tesla Siemens Healthineers AG Germany 2014 CT scan Siemens Force Siemens Healthineers AG Germany 2014 Authors contributions All authors contributed significantly to the manuscript writing and design All authors have read and approved the manuscript OH writing manuscript and design the case report KS writing manuscript and design the case report AA literature review DG literature review reviewing manuscript MT reviewing and approving the manuscript Criticizing the content and structure of manuscript Funding All authors have no funding disclosure Availability of data and materials Data is limited to one patient in this case report Data is available whenever requested Ethics approval and consent to participate Case report s are exempted from institutional board review and ethical approval Consent for publication A written informed consent was obtained from the participant Competing interests The authors declare that they have no competing interests 2020 56 93 Page 6 of 7 Author details 1 Department of Neurology The New Mexico University Health Sciences Center Albuquerque USA 2Department of Internal Medicine University of Massachusetts Medical School Baystate Campus Worcester USA Received 11 May 2020 Accepted 31 August 2020 References 1 Wu L Wu W Tali ET Yuh WT Oligemia penumbra infarction understanding hypoperfusion with neuroimaging Neuroimaging Clin N Am 2018 28 4 599 609 2 Axel L Cerebral blood flow determination by rapid sequence computed tomography theoretical analysis Radiology 1980 Dec 137 3 679 86 3 Campbell BC Yassi N Ma H Sharma G Salinas S Churilov L et al Imaging selection in ischemic stroke feasibility of automated CT perfusion analysis Int J Stroke 2015 10 1 51 4 4 Lansberg MG Christensen S Kemp S Mlynash M Mishra N Federau C et al Computed tomographic perfusion to predict response to recanalization in ischemic stroke Ann Neurol 2017 81 849 56 5 Kamalian S Kamalian S Konstas AA Maas MB Payabvash S Pomerantz SR et al CT perfusion mean transit time maps optimally distinguish benign oligemia from true at risk ischemic penumbra but thresholds vary by postprocessing technique Am J Neuroradiol 2012 33 3 545 9 6 Broderick JP Palesch YY Demchuk AM Yeatts SD Khatri P Hill MD et al Endovascular therapy after intravenous t PA versus t PA alone for stroke N Engl J Med 2013 368 10 893 903 7 Ciccone A Valvassori L Nichelatti M Sgoifo A Ponzio M Sterzi R et al Endovascular treatment for acute ischemic stroke N Engl J Med 2013 368 904 13 8 Kidwell CS Jahan R Gornbein J Alger JR Nenov V Ajani Z et al A trial of imaging selection and endovascular treatment for ischemic stroke N Engl J Med 2013 368 10 914 23 9 Berkhemer OA Fransen PS Beumer D van den Berg LA Lingsma HF Yoo AJ et al A randomized trial of intraarterial treatment for acute ischemic stroke New Engl J Med 2015 372 11 20 10 Jovin TG Chamorro A Cobo E de Miquel MA Molina CA Rovira A et al Thrombectomy within 8 hours after symptom onset in ischemic stroke N Engl J Med 2015 372 24 2296 306 11 Goyal M Demchuk AM Menon BK Eesa M Rempel JL Thornton J et al Randomized assessment of rapid endovascular treatment of ischemic stroke N Engl J Med 2015 372 11 1019 30 12 Saver JL Goyal M Bonafe A Diener HC Levy EI Pereira VM et al Stentretriever thrombectomy after intravenous t PA vs t PA alone in stroke N Engl J Med 2015 372 24 2285 95 13 Campbell BC Mitchell PJ Kleinig TJ Dewey HM Churilov L Yassi N et al Endovascular therapy for ischemic stroke with perfusion imaging selection N Engl J Med 2015 372 11 1009 18 14 Albers GW Marks MP Kemp S Christensen S Tsai JP Ortega Gutierrez S et al Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging N Engl J Med 2018 378 8 708 18 15 Nogueira RG Jadhav AP Haussen DC et al Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct N Engl J Med 2018 378 1 11 21 16 Powers WJ Rabinstein AA Ackerson T Adeoye OM Bambakidis NC Becker K Biller J Brown M Demaerschalk BM Hoh B Jauch EC 2018 Guidelines for the early management of patients with acute ischemic stroke a guideline for healthcare professionals from the American Heart Association American Stroke Association Stroke 2018 Mar 49 3 e46 e99 17 Goyal M Menon BK van Zwam WH Dippel DW Mitchell PJ Demchuk AM et al Endovascular thrombectomy after large vessel ischaemic stroke a meta analysis of individual patient data from five randomised trials Lancet 2016 387 10029 1723 31 18 Campbell BCV Majoie CBLM Albers GW Menon BK Yassi N Sharma G et al Penumbral imaging and functional outcome in patients with anterior circulation ischaemic stroke treated with endovascular thrombectomy versus medical therapy a meta analysis of individual patient level data Lancet Neurol 2019 18 1 46 55 19 Christensen S Mlynash M Kemp S et al Persistent target mismatch profile 24 hours after stroke onset in DEFUSE 3 Stroke 2019 50 3 754 7
Hussein et al The Egyptian Journal of Neurology Psychiatry and Neurosurgery 20 Zheng W Matei N Pang J et al Delayed recanalization at 3 days after permanent MCAO attenuates neuronal apoptosis through FGF21 FGFR1 PI3K Caspase 3 pathway in rats Exp Neurol 2019 320 113007 21 McBride DW Wu G Nowrangi D et al Delayed recanalization promotes functional recovery in rats following permanent middle cerebral artery occlusion Transl Stroke Res 2018 9 2 185 98 22 Desai SM Haussen DC Aghaebrahim A et al Thrombectomy 24 hours after stroke beyond DAWN J Neurointerv Surg 2018 10 11 1039 42 23 Bennett MH Weibel S Wasiak J Schnabel A French C Kranke P Hyperbaric oxygen therapy for acute ischaemic stroke Cochrane Database Syst Rev 2014 11 CD004954 24 Bennett MH Weibel S Wasiak J Schnabel A French C Kranke P Hyperbaric oxygen therapy for acute ischemic stroke Stroke 2015 May 46 5 e109 10 25 Shi S Qi Z Lou Y Liu KJ Normobaric oxygen treatment in acute ischemic stroke a clinical perspective Med Gas Res 6 3 147 53 26 Hou H Grinberg O Williams B et al The effect of oxygen therapy on brain damage and cerebral pO 2 in transient focal cerebral ischemia in the rat Physiol Meas 2007 28 8 963 76 27 Li J Liu W Ding S Xu W Guan Y Zhang JH Sun X Hyperbaric oxygen preconditioning induces tolerance against brain ischemia reperfusion injury by upregulation of antioxidant enzymes in rats Brain Res 2008 May 19 1210 223 9 28 Mink RB Dutka AJ Hyperbaric oxygen after global cerebral ischemia in rabbits reduces brain vascular permeability and blood flow Stroke 1995 Dec 26 12 2307 12 29 Thom SR Functional inhibition of leukocyte B2 integrins by hyperbaric oxygen in carbon monoxide mediated brain injury in rats Toxicol Appl Pharmacol 1993 123 2 248 56 30 Selman WR Lust WD Pundik S Zhou Y Ratcheson RA Compromised metabolic recovery following spontaneous spreading depression in the penumbra Brain Res 2004 999 2 167 74 31 Sukoff MH Ragatz RE Hyperbaric oxygenation for the treatment of acute cerebral edema Neurosurgery 1982 10 1 29 38 32 Badr AE Yin W Mychaskiw G Zhang JH Effect of hyperbaric oxygen on striatal metabolites a microdialysis study in awake freely moving rats after MCA occlusion Brain Res 2001 916 1 2 85 90 33 Lou M Chen Y Ding M Eschenfelder CC Deuschl G Involvement of the mitochondrial ATP sensitive potassium channel in the neuroprotective effect of hyperbaric oxygenation after cerebral ischemia Brain Res Bull 2006 69 2 109 16 34 Calvert JW Zhou C Nanda A Zhang JH Effect of hyperbaric oxygen on apoptosis in neonatal hypoxia ischemia rat model published correction appears in J Appl Physiol 2004 Jan 96 1 405 J Appl Physiol 1985 2003 95 5 2072 80 35 Zhang XG Jiang ZL Wang GH et al Zhongguo Ying Yong Sheng Li Xue Za Zhi 2012 28 1 42 6 36 Sun L Marti HH Veltkamp R Hyperbaric oxygen reduces tissue hypoxia and hypoxia inducible factor 1 alpha expression in focal cerebral ischemia Stroke 2008 39 3 1000 6 37 Yusa TO Beckman JS Crapo JD Freeman BA Hyperoxia increases H2O2 production by brain in vivo J Appl Physiol 1987 Jul 1 63 1 353 8 38 Haelewyn B Chazalviel L Nicole O Lecocq M Risso JJ Abraini JH Moderately delayed post insult treatment with normobaric hyperoxia reduces excitotoxin induced neuronal degeneration but increases ischemiainduced brain damage Med Gas Res 2011 1 2 39 Unfirer S Kibel A Drenjancevic Peric I The effect of hyperbaric oxygen therapy on blood vessel function in diabetes mellitus Med Hypotheses 2008 71 5 776 80 https doi org 10 1016 j mehy 2008 06 016 40 Alexandrov AV Sharma VK Lao AY Tsivgoulis G Malkoff MD Alexandrov AW Reversed Robin Hood syndrome in acute ischemic stroke patients Stroke 2007 38 11 3045 8 41 McCormick JG Houle TT Saltzman HA Whaley RC Roy RC Treatment of acute stroke with hyperbaric oxygen time window for efficacy Undersea Hyperb Med 2011 38 5 321 34 42 Lee YS Chio CC Chang CP et al Long course hyperbaric oxygen stimulates neurogenesis and attenuates inflammation after ischemic stroke Mediat Inflamm 2013 2013 512978 43 Chen CH Chen SY Wang V et al Effects of repetitive hyperbaric oxygen treatment in patients with acute cerebral infarction a pilot study Sci World J 2012 2012 694703 2020 56 93 Page 7 of 7 44 Efrati S Fishlev G Bechor Y et al Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS One 2013 8 1 e53716 45 Yamagami H Sakai N Current status of endovascular therapy for acute ischemic stroke Rinsho Shinkeigaku 2013 53 11 1166 8 46 Mokin M Khalessi AA Mocco J et al Endovascular treatment of acute ischemic stroke the end or just the beginning Neurosurg Focus 2014 36 1 E5 47 Campbell BC Mitchell PJ Kleinig TJ et al Endovascular therapy for ischemic stroke with perfusion imaging selection N Engl J Med 2015 372 11 1009 18 48 Fisher M Albers GW Advanced imaging to extend the therapeutic time window of acute ischemic stroke Ann Neurol 2013 73 1 4 9 https doi org 10 1002 ana 23744 49 Hinman JD Rost NS Leung TW Montaner J Muir KW Brown S et al Principles of precision medicine in stroke J Neurol Neurosurg Psychiatry 2017 88 1 54 61 Publisher s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
biomolecules Review An Extra Breath of Fresh Air Hyperbaric Oxygenation as a Stroke Therapeutic Blaise Cozene Nadia Sadanandan Bella Gonzales Portillo Madeline Saft Justin Cho You Jeong Park and Cesar V Borlongan Department of Neurosurgery and Brain Repair University of South Florida Morsani College of Medicine 12901 Bruce B Downs Blvd Tampa FL 33612 USA bcozene tulane edu B C nas146 georgetown edu N S bellagonzales portillo2024 u northwestern edu B G P saftmad umich edu M S justincho usf edu J C youjeongpark usf edu Y J P Correspondence cborlong usf edu Tel 813 974 3988 Received 4 August 2020 Accepted 2 September 2020 Published 4 September 2020 Abstract Stroke serves as a life threatening disease and continues to face many challenges in the development of safe and effective therapeutic options The use of hyperbaric oxygen therapy HBOT demonstrates pre clinical effectiveness for the treatment of acute ischemic stroke and reports reductions in oxidative stress inflammation and neural apoptosis These pathophysiological benefits contribute to improved functional recovery Current pre clinical and clinical studies are testing the applications of HBOT for stroke neuroprotection including its use as a preconditioning regimen Mild oxidative stress may be able to prime the brain to tolerate full extensive oxidative stress that occurs during a stroke and HBOT preconditioning has displayed efficacy in establishing such ischemic tolerance In this review evidence on the use of HBOT following an ischemic stroke is examined and the potential for HBOT preconditioning as a neuroprotective strategy Additionally HBOT as a stem cell preconditioning is also discussed as a promising strategy thus maximizing the use of HBOT for ischemic stroke Keywords preconditioning stem cells cerebral ischemia hyperbaric oxygen therapy neuroprotection 1 Introduction Strokes occurs primarily due to interruption of blood flow to the brain and is typed as ischemic or hemorrhagic Ischemic strokes make up approximately 87 of total strokes 1 Currently the only FDA approved treatment for ischemic stroke is thrombolytic tissue plasminogen activator tPA for dissolving the blood clot and improving blood flow in the brain When tPA is administered intravenously up to 4 5 h after stroke onset in patients with acute ischemic stroke it reduces mortality and increases rates of independent ambulation when thrombolytic treatment is given early If tPA is not delivered within the given time frame it becomes associated with increased occurrences of severe hemorrhagic transformation thereby limiting the therapeutic opportunity 2 Since stroke is currently the fifth leading cause of death in the U S and someone dies of one approximately every 4 min the discovery of new and effective stroke treatments is of high necessity moving forward An ischemic stroke is caused by abrupt blood vessel occlusion that causes ischemic damage to the area of the brain supplied by the occluded artery During the acute phase of an ischemic stroke excitotoxicity oxidative stress and microglial activation occurs and causes neural death in the ischemic core 3 In the penumbra the apoptosis cascade is mainly triggered by the influx of calcium which activates calpains and ultimately mitochondrial release of cytochrome c and eventually caspase 3 4 Furthermore the intracellular calcium promotes mitochondrial dysfunction generation of reactive oxygen species and production of nitric oxide 5 Also an abnormal increase of water movement into Biomolecules 2020 10 1279 doi 10 3390 biom10091279 www mdpi com journal biomolecules
Biomolecules 2020 10 1279 2 of 26 the intracellular space occurs during the acute phase and results in edema 6 In the subacute phase aberrant neuroinflammation heightens the presence of matrix metalloproteases MMPs which cause an increase in blood brain barrier BBB permeability consequently allowing leukocytes to migrate to the damaged area of the brain and increase inflammatory activity 7 The expression of reactive oxygen species generating enzymes like NADPH oxidases NOXs is also implicated in increased BBB permeability by promoting inflammation and dysfunction of endothelial tissue 5 Other areas of the brain tissue surrounding the infarct area are vulnerable to the same exacerbating damage but other cell phenotypes can be protected and serve as an area of focus towards monitoring the motor and cognitive functional deficits that precede a stroke 8 Hyperbaric oxygen therapy HBOT serves as a potential non invasive therapy where pure oxygen can be administered in a pressurized chamber at high levels of atmospheric pressure With increased oxygenation HBOT can be used to improve oxygen flow from lungs to systemic organs and can reduce secondary brain injury effects including apoptotic pathway initiation oxidative stress and rampant inflammation 9 By restoring oxygen tension HBOT has been shown to restore cellular energy production stabilize cellular calcium decrease NOXs expression and attenuate oxidative stress 10 Mechanisms reached with hyperbaric oxygen can also be achieved at lower or normal oxygen concentrations 11 During the recovery stages where oxygen levels are close to normal HIF 1 alpha synthesis increased and a relatively hypoxic environment existed 11 In this setting MMP a hypoxic stimulus 12 and EPO production elevated as well which was also observed in healthy human subjects This suggests that similar mechanisms of HBOT can be demonstrated with lower tensions of oxygen Additionally HBOT has also proven beneficial in the treatment of other pathological diseases including traumatic brain injury TBI spinal cord injury SCI and stroke 13 Currently there are few treatment options available for many neurological diseases however experimental studies utilizing HBOT demonstrate promising results HBOT studies target ameliorating ischemic related damage to improve the quality of life of affected patients In this review the use of HBOT for ischemic stroke will be covered in depth including information on the application of HBOT preconditioning in the stroke brain and the potential of HBOT priming for stem cell transplantation Here we provide the pre clinical bases for advancing the use of HBOT as a promising target for stroke therapy 2 HBOT in Ischemic Stroke Potential Benefits and Limitations In early investigations on hyperoxia following a stroke HBOT was seen as a dangerous apparatus with few beneficial properties and was deemed to have no therapeutic value Nevertheless in the last 20 years expansive research has demonstrated the ability of HBOT to reduce the severity of infarct volume and serve as a potential treatment option 14 However HBOT must be administered during the small reperfusion window which creates a limited opportunity for effective treatment This has been a reoccurring problem with HBOT because of the difficulty associated with determining the reperfusion window and extensive imaging to determine the appropriate course of action 15 Evidently some studies indicate that delayed HBOT past the effective window of treatment actually causes worse outcomes This is suggested to be due to the role of ROS in glutamate induced excitotoxic cell death 16 Therefore further research on the use of HBOT must be conducted and carried out safely to prevent treatment with excess oxygen that could cause additional harm including obstructive pulmonary disease 16 Acute ischemic stroke AIS serves as a primary cause of death worldwide and is characterized by an occlusion of the cerebral artery The therapeutic treatment plans for AIS are however limited to date HBOT treatment serves as an option to improve AIS induced brain tissue hypoxia 17 The primary goal of acute HBOT treatment is to increase oxygen levels in the ischemic region during stroke occlusion in pursuit of minimizing hypoxic damage Studies have demonstrated the ability of HBOT to be used to enhance the arterial partial pressure of oxygen 18 increase the oxygen content 19 stabilize the blood brain barrier 20 decrease the intracranial pressure and relieve cerebral edema Moreover HBOT serves as a safe practice for the treatment of acute ischemic stroke moving forward
Biomolecules 2020 10 1279 3 of 26 In regard to chronic ischemic stroke HBOT demonstrates limited potential in treating chronic neurological deficits Nonetheless in a recent study the efficacy of HBOT in restoring memory function for chronic stroke patients revealed significant memory improvement and increased brain metabolic rate 21 Additionally patients experienced significant improvement in memory and attention testing scores 22 Studies have demonstrated that the earlier HBOT is initiated the greater its therapeutic effectiveness 23 Clinical trials have demonstrated consistent safety but inconsistent efficacy Limited studies have demonstrated the efficacy of HBOT for the treatment of chronic ischemic stroke and the data is still unreliable for further use in patients Another potential treatment for stroke that has been explored is the use of normobaric oxygen which its therapeutic efficacy has been both reported and refuted 16 24 25 The normobaric oxygen paradox NOP was introduced to describe a potent mechanism where Hypoxia Inducible Factor 1 alpha HIF 1 alpha expression is regulated by oxygen 26 Because HIF 1 alpha is responsible for erythropoietin EPO and VEGF expression normobaric oxygen may be correlated to EPO production 27 Studies hypothesize that sudden return to normoxia after a small exposure to normobaric hyperoxia would result in a relative hypoxia state 27 28 This in turn would elevate EPO production because hypoxia is a natural trigger for EPO production 26 28 Additionally relative hypoxia induced by oxygen gradient and NBO may induce reticulocyte production 28 Normobaric oxygen therapy increases dissolved oxygen levels within the bloodstream but displays controversial neuroprotective effects Specifically critical information regarding the optimal therapeutic time frame of NBO and its long term effects are still unclear Therefore it does not serve the same effectiveness as the HBOT for post and pre stroke conditions and is less of an intriguing option for preconditioning 16 24 25 Nevertheless the synergistic use of normobaric oxygen treatment accompanied by HBOT shows promise in reducing stroke mortality 2 29 Recent in vivo investigations have shown that HBOT and normobaric oxygen treatment may widen the limited window for thrombolytic therapy and various neuroprotective medications 29 30 Currently HBOT has been used as a post stroke therapy as well as a preconditioning method The goal of HBOT is to stimulate a hyperoxia environment during ischemic and reperfusion periods following a stroke Additionally HBOT may expose a patient to recurrent treatments after the initial early treatment time frame has passed 31 Preconditioning treatments have focused on exposing an individual to a mild stressor which is supposed to enhance the brain s resistance to future stressors 32 2 1 Preclinical Functional Outcomes of Post stroke HBOT Typically HBOT treatment is carried out at 2 5 atmospheres ATA for 60 90 min 33 The atmospheric pressure must not exceed the given 2 5 ATA during HBOT or it could cause oxygen toxicity increase oxidative stress throughout the body or increase the risk of seizure activity 31 The goal of HBOT treatment is to increase the oxygen concentration in the ischemic region of the brain to minimize hypoxic damage If administered after the initial treatment window continuous HBOT treatments could promote the stimulation of endogenous repair processes 34 HBOT is highly effective when administered 30 to 60 min after stroke and the potency of treatment lessens if initiation is delayed any further HBOT exhibits therapeutic potential in its ability to reduce infarct volume and improve behavioral scores in patients 14 15 Research has demonstrated different time points at which HBOT is effective such as HBOT 2 5 ATA for 2 h at 6 h after reperfusion 35 and HBOT 3 ATA 1 h at 3 and 6 h after reperfusion 36 Additionally single session HBOT is reported to be effective up to 18 h and 48 h after stroke 37 In order to determine the therapeutic effects with HBOT at various timepoints extensive and tailored treatment protocols are required On the other hand delayed treatment with HBOT 2 5 ATA 2 h at 6 or 24 h after stroke results in an increase of infarct size and causes neurological deficits 38 Little evidence has proven the effectiveness of HBOT that is given more than 48 h post stroke One study has used one session of HBOT 3 ATA 1 h and exhibited significant neuroprotective effects when delivered 72 h post stroke 20 Therefore it is imperative to deliver HBOT within the given time frame to ensure the best outcomes
Biomolecules 2020 10 1279 4 of 26 2 2 Clinical Results of HBOT in Stroke Many clinical trials have explored the use of HBOT but have revealed inconclusive results 39 Various factors including the unstable clinical status of the acute stroke patients could be the cause for varying results and prevent the patients from the given effective treatment window that is required 3 5 h after reperfusion 40 Additionally many treatment protocols could be different and take a wide variety of patients that could hinder the ability to draw reliable conclusions and comparisons between groups It is imperative to acknowledge the fact that clinical success for HBOT has been achieved and the use of HBOT has been shown to lessen levels of cerebral and myocardial biomarkers and reduce the length of stay in an intensive care unit 41 Moreover the clinical significance of HBOT should not be overlooked and further research should be carried out 42 A growing number of clinical trials have been performed and demonstrate cerebral plasticity as well as the ability of HBOT to restore memory function and improvement following a chronic stroke 21 The timing of the HBOT application is critical Conclusive studies have found that if HBOT is initiated earlier it leads to greater therapeutic effectiveness 15 23 After 12 h post ischemia the benefits of single treatment HBOT are reduced However repetitive applications of HBOT in the sub acute stroke brain document neurogenic effects 43 Studies have even demonstrated a consistent safety and the potential of using HBOT for chronic stroke patients a breakthrough finding that was thought of only as detrimental previously Nevertheless contradicting results in the use of HBOT for acute and chronic stroke patients warrant further exploration to clear up the inconsistencies in studies 3 Unpacking Mechanisms of Action of HBOT in Stroke 3 1 Physiological and Metabolic Effects The goal of HBOT is to increase perfusion and oxygenation of at risk tissue HBOT therapy can be used to enhance arterial oxygen saturation and augment tissue oxygen content via enhanced cerebral microcirculation 18 31 Additionally HBOT serves a vital role in enhancing BBB stability through MMP regulation 23 and can also decrease intracranial pressure and relieve cerebral edema 31 Secondary effects of HBOT in the ischemic brain may be prevalent due to the reduction of extracellular glutamate levels causing neural dysfunction and excitotoxic death 44 3 2 Antioxidant Effects HBOT demonstrates the ability to provide oxidative protection against stroke induced ROS and nitrosative species 45 This startling discovery reverts the fact that introducing high levels of oxygen can actually induce oxidative stress and exhibits the efficacy of HBOT Following a stroke HBOT has been proven to reduce levels of pro oxidative enzymes including malondialdehyde and increase the activity of CAT and SOD 45 Additionally other studies have found reduced stroke generated ROS in the striatum after HBOT therapy 46 HBOT also plays an effect on nitric oxide synthase and provides antioxidant protective properties 47 However various experimental designs and different durations of treatment sessions may hinder a complete understanding of the role of the HBOT for reducing oxidative damage It is important to note that HBOT treatment may cause oxidative stress but can be balanced by antioxidant mechanisms Further studies are required to determine the effects of HBOT on oxidative pathways 3 3 Anti Inflammatory Effects Aberrant inflammation is a key player in the pathogenesis of stroke and catalyst for secondary cell death in the brain Interestingly HBOT has been linked to anti inflammatory effects in the setting of ischemic stroke Experimental stroke studies have shown decreases in markers of inflammation such as tumor necrosis factor alpha and CD40 microglia in HBOT treated animals 48 49 Although the mechanism underlying the anti inflammatory effects of HBOT has not been fully elucidated pre clinical studies showed reduced secretion of inflammatory chemokines which inhibit the accumulation of
Biomolecules 2020 10 1279 5 of 26 leukocytes at the ischemic area 17 Similarly another study showed HBOT reduced myeloperoxidase activity and inhibited neutrophil infiltration of the injured tissue 50 3 4 Additional Neuroprotective Mechanisms HBOT has been linked to many pathways that preserve neural tissue and reduce apoptosis as displayed in Table 1 Mechanisms mentioned previously in this section many be heavily related to these as neuronal apoptosis is prompted via metabolic restriction inflammation and ROS Undiscovered pathways may also contribute to HBOTs efficacy Notable findings include a lower concentration of cortical and hippocampal caspase 3 51 reduced HIF 1 52 augmented growth factor levels of GDNF and NGF 53 and regulation of mitochondria 54 Furthermore HBOT has been seen to directly modulate glial cells consequently contributing to the protection of vulnerable neurons 55 4 Implications of HBOT in Other Neurological and Non Neurological Conditions 4 1 HBOT in Acute and Chronic TBI HBOT has been shown to be a safe and effective treatment for TBI specifically when conducted during the acute phase 53 56 58 Utilizing a rodent model of TBI HBOT initiated at 3 h after cortical deformation induction attenuated symptoms after histopathological analysis 59 Another murine model of TBI offered evidence that HBOT induced cognitive and learning regenerative abilities were preserved from 3 h after injury to 7 days 13 While experimental protocols such as therapeutic windows may vary HBOT consistently provides neuroprotection for acute TBI 60 Nonetheless HBOT may also translate to functional benefits in chronic TBI as well A human TBI HBOT study indicated increased cerebral perfusion and angiogenesis and ameliorated memory ability executive function information processing speed and global cognitive scores up to 27 years post injury 61 Although many studies have found similar therapeutic effects of HBOT in TBI 62 65 other studies have not supported these findings 66 4 2 HBOT in Spinal Cord Injury Overwhelming evidence has indicated that cell death responses induced by secondary injury contribute more significantly to SCIs than primary trauma 67 The following mechanisms are associated with secondary cell damage and can potentially be ameliorated by HBOT Reactive oxidative injury astrocytic glial scarring glial penetration and lymphocyte activated monocyte phagocytic macrophage generation 68 Importantly HBOT engenders neuroprotection in SCI via attenuation of anoxia and heightened rehabilitation of neurons 69 HBOT correlates with decreased oxidative enzymes apoptotic factors and inflammatory agents 70 In addition HBOT has been shown to safeguard BBB function and improve motor dysfunction post SCI 71 Notably SCI patients who underwent HBOT demonstrated substantial amelioration of neurological injury and maintained neuronal functions such as induced potential amplitude and conduction velocity more effectively than the control group 72 The mechanisms behind HBOT induced neuroprotection may involve the upregulation of vascular endothelial growth factor VEGF expression restoration of axons and inhibition of apoptosis 73 4 3 HBOT in Other Pathological Contexts Several studies have elucidated that HBOT bears curative potential in a multitude of disorders that manifest in oxidative stress inflammation and ischemic injury 74 77 HBOT has been explored as a therapeutic regimen in patients suffering from diseases that entail hypoxia of tissues such as diabetic ulcers 78 79 and acute coronary syndrome 80 81 Evidently the therapeutic abilities of HBOT may encompass tissue repair processes specific to the disease For instance HBOT imparts antimicrobial capacity in necrotizing tissue contamination 82 and enhances gas dissolution in air embolisms 83 In addition HBOT has shown promising results in psychological pathologies such as post traumatic
Biomolecules 2020 10 1279 6 of 26 stress disorder PTSD and post concussive malady that may arise following brain damage 63 After 40 HBOT treatments 15 ATA 60 min conducted within 30 days PTSD manifestations were significantly alleviated 62 84 HBOT therapy ameliorated cognitive deficits diminished anxiety and depression and augmented blood circulation via the cerebrovasculature into the white matter 65 Additionally spontaneous physiological irregularities like autism spectrum illnesses may be potential therapeutic targets for HBOT 85 however HBOT s neuroprotective effects in these disorders warrant further investigation 86 In light of the current COVID 19 pandemic clinical trials have explored HBOT in infected patients experiencing extreme respiratory distress COVID 19 infection generates a potent cytokine storm that spurs the onset of progressive hypoxia leading to severe respiratory illness 2 87 Furthermore HBOT s capacity to enhance oxygen flow and attenuate inflammation may bear curative effects in COVID 19 patients 87 In Wuhan HBOT was administered to critically ill COVID 19 patients and resulted in ameliorated hypoxia increased blood flow and mitigated immune system deficits Remarkably these patients demonstrated substantial recovery and were released from hospital care after 3 8 HBOT sessions 2 In another clinical trial COVID 19 patients demonstrated alleviated shortness of breath 87 though a significant reduction in mortality rate was not observed Therefore the potential of HBOT in COVID 19 treatment warrants further clinical investigation As copious evidence suggests HBOT similarly affords a stable safety profile in non stroke diseases when it is administered properly 5 Pre Clinical Findings with HBOT Preconditioning for Stroke HBOT preconditioning has been shown to provide therapeutic benefit in neurological diseases like ischemic stroke 42 88 The mechanism behind the protection is attributed to the introduction of mild oxidative stress which builds tolerance in endogenous cells to future insult Patient populations with a higher risk for ischemic strokes such as those with comorbidities e g obesity diabetes hypertension atherosclerosis etc may benefit from preemptive HBOT and advancements in imaging techniques that allow for more accurate prediction of stroke risk may increase the value of preconditioning therapies 89 The first pre clinical study evaluating the effects of HBOT preconditioning on a gerbil ischemic stroke model showed that the therapy conferred tolerance to ischemia and prevented neuronal death 90 The following studies using other animal models showed that HBOT was protective against transient not permanent stroke and protection was conferred in a dose dependent manner 91 A treatment of five sessions 2 5 atmosphere absolute ATA 1 h over consecutive days was more effective than three sessions at rescuing functional deficits in rats after middle cerebral artery occlusion MCAO 24 h after the last session 91 These results have been replicated by other studies including one that showed that four sessions of HBOT 2 5 ATA 1 h twice a day offered neurological and histopathological protection from MCAO 24 h after the last session 92 More aggressive treatments 3 5 ATA 1 h five consecutive days have also provided significant histopathological signs of neuroprotection 93 Other pre clinical studies have explored the therapeutic window for HBOT which suggests neuroprotection can be achieved by treatment 24 h before ischemia but not 72 h 94 However it is important to note that intensity and number of sessions may play a bigger role in treatment effects and the therapeutic window must be further investigated In the following sections we will discuss the potential mechanisms underlying neuroprotection provided by HBOT preconditioning 5 1 Preparation for Oxidative Stress HBOT primarily generates neuroprotection through its interactions with an oxidative preconditioning factor 95 Long term subjection to hypoxic environments engenders drastic oxidative strain the disarray of the antioxidant network and ultimate cell damage Initial exposure of brain tissue to non lethal hypoxia via HBOT preconditioning can shield neurons from future ischemic injury by fortifying tissue against oxidative stress As evidence suggests oxidative toxicity may be spurred by ROS and reactive nitrogen species RNS e g peroxynitrite and NO2 upregulation
Biomolecules 2020 10 1279 7 of 26 in the CNS Fortunately cells can combat ROS escalation through defense mechanisms induced by antioxidant enzymes Superoxide dismutase SOD sequesters superoxide catalase peroxidases neutralize hydrogen peroxide and glutathione S transferase off set lipid peroxides Auxiliary enzymes such as glutathione reductase GRX and glucose 6 phosphate dehydrogenase G6PD also contribute to brain tissue defense Although sparse numbers of ROS can be beneficial as they promote antioxidant enzyme pathways that make up the adaptive cellular response lethal amounts of ROS engendered by hyperoxia surpass the cellular antioxidative potential and generate oxidative damage Ischemic injury in the brain induces oxidation of proteins lipid peroxidation and augmented DNA mutation leading to cell membrane impairment disturbances in metabolism and tissue death 96 ROS levels are higher with HBOT due to increased oxygen partial pressure and upregulated H2 O2 produced by mitochondria 42 Moreover non lethal oxidative stress spurred by HBOT serves as a protective procedure stimulating antioxidative activity 95 An in vivo investigation utilizing a focal cerebral ischemia model found that HBOT preconditioning elevated SOD and CAT mechanisms in cerebral tissue leading to increased survival rates as well as ameliorated neurological function and cell damage 92 Notably the stroke afflicted penumbra and hippocampus demonstrated diminished levels of lipid peroxidation and oxidative stress biomarker malondialdehyde MDA 92 In the same way HBOT preconditioning with a spinal cord ischemia experimental model upregulated SOD and CAT processes However activation of the CAT inhibitor 3 amino 1 2 4 triazole prior to ischemic stroke abolished the beneficial effects of HBOT like spinal cord resilience to oxidative stress decreased significantly 97 When dimethylthiourea a free radical scavenger was delivered to the spinal cord ahead of HBOT the elevated SOD and CAT activity was eliminated 97 Moreover HBOT preconditioning spurs preliminary oxidative stress that prompts antioxidative mechanisms from enzymes leading to increased resistance of tissue to future ischemic damage By suppressing GRX and G6PD and elevating glutathione peroxidase GSH Px and glutathione S transferase GST pathways frequent non lethal HBOT preconditioning imparts neuroprotection against oxidative damage in the central nervous system 98 Therefore in an indirect manner HBOT attenuates oxygen toxicity through the repression of G6PD mechanisms Importantly HBOT preconditioning bolsters antioxidative processes and dilutes enzymatic activity of pro oxidants as HBOT induced diminishment of G6PD can be correlated with the truncation of GRX and the augmentation of GSH Px activity Under normal conditions HBOT promotes neuronal rehabilitation and neuroprotection by upregulating heat shock proteins HSPs particularly HSP70 99 HSP70 inhibits protein build up restores slightly denatured proteins attenuates inflammation and hinders apoptosis all of which contribute to neuroprotection 100 In addition as displayed in vitro HBOT fortifies the expression of HSP32 shielding neuronal tissue from oxidative damage and oxygen glucose deprivation OGD 92 101 HSP32 or heme oxygenase 1 breaks down heme into carbon monoxide CO biliverdin and ferrous iron Hemoprotein oxidation such as hemoglobin myoglobin and neuroglobin oxidation engender the formulation of free heme An iron atom lies in the middle of the heme molecule and can interact with H2 O2 to form deleterious hydroxyl radicals HSP32 catalyzes heme molecules leading to the generation and build up of ferritin release which in turn engenders the removal of iron thereby safeguarding tissue from oxidative injury 92 101 Importantly HSP32 is known to be incited by ROS and nitric oxide NO as the ROS p38 MAPK Nrf2 pathway and MEK1 2Bach1 regulated negative feedback modulate HSP32 activity 102 Moreover free radical production spurred by oxidative stress should promote HSP mechanisms At very low concentrations free radicals produced by mitochondria and NOXs serve a regulatory ole in cellular activity their physiological role in cellular activity ties in with the use of HBOT Nonetheless evidence points to the idea that response to HBOT may be cell specific For instance one HBOT subjection in healthy males demonstrated no elevation in HSP72 activity in peripheral blood mononuclear cells PBMC 103
textlhtlongi textpalhookbelow t LATIN SMALL LETTER T WITH PALATAL textlhookt 01AC m T LATIN CAPITAL LETTER T WITH HOOK textThook 01AD m t LATIN SMALL LETTER T WITH HOOK Biomolecules 2020 10 1279 8 of 26 texthtt textthook 01AE M T LATIN CAPITAL LETTER T WITH RETRO textTretroflexhook Additionally HBOT may impart neuroprotection against oxygen toxicity via an increase in 01AF Uhorn LATIN CAPITAL LETTER U WITH HORN NrF2 mediated antioxidant gene expression Notably more than 200 antioxidants and cytoprotective textrighthorn U genes can be turned on by the Nrf2 pathway 104 HBOT 01B0 uhorn not only promotes Nrf2 activity but also LATIN SMALL LETTER U WITH HORN textrighthorn u upregulates essential proteins involved with intracellular GSH production and transport e g GST 01B1 textupsilon LATIN CAPITAL LETTER UPSILON MRPI GCL cGT the assembly disassembly of macromolecules e g HSPA1A HSP32 and antioxidant m U 01B2 LATIN CAPITAL LETTER V WITH HOOK enzymes e g SOD1 GST which are all target genes of m V Nrf2 31 102 105 107 In addition by bolstering textVhook the expression of SirT1 in more than three various ways HBOT preconditioning imparts neuroprotection 01B3 m Y LATIN CAPITAL LETTER Y WITH HOOK Firstly Sirt1 expression can be increased by mediating the fasting induced initiation of Nrf2 signaling textYhook 01B4 m y complex that attaches to the Nrf2 promoter LATIN SMALL LETTER Y WITH HOOK upstream through the regulation of the PPAR PGC1 1 textyhook stimulating expression Secondly SirT1 expression is mediated via repression of apoptosis spurred 01B5 B Z LATIN CAPITAL LETTER Z WITH STROK Zbar by the upregulation of protein anti apoptotic Bcl 2 expression depletion of cleaved caspase 3 which B z is pro apoptotic and the removal of01B6 acetyl groups from p53 Thirdly expression of SirT1 can LATIN be SMALL LETTER Z WITH STROKE 01AB 01B7 m Z LATIN CAPITAL LETTER EZH modulated through the augmentation of FoxO which in turn elevates SOD and CAT activity under EZH textEzh oxidative stress 107 110 01B9 LATIN SMALL LETTER EZH REVERSED Indeed HBOT preconditioning can be linked to textrevyogh the inflation of nitric oxide 111 112 as shown 01BA textbenttailyogh LATIN SMALL LETTER EZH WITH TAIL in Figure 1 Serving as a key neurotransmitter NO is generated by NO synthase NOS and is a 01BB B 2 LATIN LETTER TWO WITH STROKE critical agent of neuroprotection and neurotoxicity textcrtwo 113 Following cerebral ischemia endothelial 01BE textcrinvglotstop LATIN LETTER INVERTED GLOTTAL STO NOS eNOS secretion of NO is beneficial as it stimulates vasodilation Conversely once ischemia 01BF wynn LATIN LETTER WYNN evolves further NO generated by hyperactivity of neuronal NOS nNOS and iNOS expression 01C0 textpipe LATIN LETTER DENTAL CLICK lead to cerebral injury NO released by eNOS and iNOS promote synaptic plasticity and neuronal textpipevar development whereas NO secreted by nNOS has the textvertline opposite effect attenuating neurogenesis 114 textdoublepipe Since NO improves the vasodilation01C1 of the cerebrovasculature it may fortify the oxygenation LATIN of LETTER LATERAL CLICK textdoublepipevar tissues Furthermore NO possesses the or impair apoptosis NO may also regulate 01C2capacity to favor textdoublebarpipe LATIN LETTER ALVEOLAR CLICK textdoublebarpipevar cellular metabolism in the presence of dysfunctional mitochondria On the other hand it may escalate 01C3 textrclick LATIN LETTER RETROFLEX CLICK the transit of ROS to tissues as well Additionally NO may react with free radicals to generate toxic 01C4 v DZ LATIN CAPITAL LETTER DZ WITH CARO oxidant peroxynitrite and engender01C5 nitrosative Importantly preconditioning with HBOT injury v Dz LATIN CAPITAL LETTER D WITH SMALL elevates antioxidant peroxynitrite primarily in the hippocampus 01C6and represses v dz LATIN Biomolecules 2020 10 x enzymatic activity 9 of 27 SMALL LETTER DZ WITH CARON 01C7 LATIN CAPITAL LETTER LJ demonstrating HBOT s protective capabilities 98 LJ 01C8 Lj LATIN CAPITAL LETTER L WITH SMALL 01C9 lj LATIN SMALL LETTER LJ 01CA NJ LATIN CAPITAL LETTER NJ 9 Figure 1 Hyperbaric oxygen therapy HBOT effects on Antioxidants and NO Figure 1 Hyperbaric oxygen therapy HBOT effects on Antioxidants and NO As low amounts of NO displays beneficial effects after stroke high concentrations of NO produced via iNOS or eNOS may augment neuroinflammation and neurotoxicity these negative As low amounts of NO displays beneficial effects after stroke NO highprovides concentrations of NO effects through various mechanisms including cGMP cAMP G protein JAK STAT and MAPK produced via iNOS or eNOS may augment neuroinflammation and neurotoxicity NO provides these negative effects through various mechanisms including cGMP cAMP G protein JAK STAT and MAPK dependent pathways Moreover NO is also believed to modulate specific gene expression further exacerbating inflammation and toxicity 115 Aside from NO s capacity to cause inflammation HBOT induced upregulation of eNOS and nNOS mRNA and protein along with increased NO in the hypothalamus and hippocampus may
Biomolecules 2020 10 1279 9 of 26 dependent pathways Moreover NO is also believed to modulate specific gene expression further exacerbating inflammation and toxicity 115 Aside from NO s capacity to cause inflammation HBOT induced upregulation of eNOS and nNOS mRNA and protein along with increased NO in the hypothalamus and hippocampus may amplify convulsion susceptibility following consecutive HBOT subjections which may exacerbate the risk of seizures in successive HBOT exposures 112 Notably the nonspecific NOS inhibitor L NAME eliminated HBOT induced neuroprotection indicating that elevations in Mn SOD CAT and Bcl 2 as well as apoptosis inhibition may be regulated by NO 69 Furthermore following HBOT preconditioning NO bears both neuroprotective and neurotoxic effects and thus further investigation into the mechanisms of NO after HBOT pre treatment is warranted 5 2 Reduction of Apoptosis Activation of Autophagy and Promotion of Cell Survival ROS molecules possess the ability to react with molecular components to initiate apoptosis or necrosis Inhibiting major redox systems such as thioredoxin reductases TrxR results in the production of ROS and increased cell apoptosis 116 PTSD models in rats revealed the upregulation of TrxR 1 and TrxR 2 mRNA in the hippocampus in addition to decrease levels of apoptosis of neurons after HBOT 117 Additionally HBOT preconditioning reduced cellular necrosis by modulating mitochondrial pathways Specifically cytoplasm cytochrome c levels as well as capase 3 and capase 9 activity were reduced upregulating Bcl 2 and Bax proteins linked with improved brain recovery 93 118 121 Inducing BDNF and inhibiting p38 MAPK phosphorylation also reduced the early onset of apoptosis and apoptosis progression 93 122 Therefore HBOT preconditioning in stroke evidently limits apoptosis progression by promoting anti apoptotic activity and protein expression In addition to initiating apoptosis ROS also moderates starvation induced autophagy via class III phosphoinositide 3 kinase pathway which sabotages the survival mechanism ROS induced autophagy was demonstrated when HBOT preconditioning upregulated protein expression levels of LC3 II and Beclin 1 causing autophagosomes to form in the ischemic penumbra post ischemia in rat brain models 123 Additionally HBOT preconditioning enhanced cell survival by downregulating MMP 9 expression inhibited CA1 cell damage and promoted healthy functional performance 122 Furthermore preconditioning HBOT can activate Wnt signaling pathway upregulate HIF 1 and secrete vascular endothelial growth factor VEGF to mitigate cell loss HBOT increased levels of VEGF VEGFR2 MEK1 2 Raf 1 and phosphor extracellular signal regulated kinase ERK 12 protein that further improved neurological functions 123 5 3 Immunosuppression and Immunopreparation Interestingly HBOT preconditioning has been observed to reduce and even prevent aberrant inflammation by lowering neurotoxicity microglia activity TNF expression and neuronal degeneration 42 resulting in improvement in motor function after intracerebral hemorrhage 123 Additional mechanisms include downregulation of expressions associated with post ischemic neuroinflammation such as cyclooxygenase 2 COX 2 and alleviates cognitive impairments and physiological dysfunctions by restricting pro inflammatory cytokines and caspase 3 activity in the hippocampus 55 124 Based on these findings HBOT preconditioning also alleviates cognitive impairment and protects brain functions by modulating pro inflammatory cytokines and caspase 3 pathways 55 124 5 4 Preservation of Blood Brain Barrier Edema Minimization and Angiogenesis HBOT demonstrated preservation of the blood brain barrier BBB and minimizes edema after the onset of surgical brain injuries SBI stroke either ischemic or hemorrhagic and TBI 42 125 129 These protective mechanisms exist due to the suppression of inflammatory responses by lowering hemorrhage volumes and reducing NLRP3 inflammasome expression to recover cognitive functions Furthermore HBOT preconditioning also relieved neurological dysfunctions and reduced blood
Biomolecules 2020 10 1279 10 of 26 volumes by reducing HIF 1 MMP 2 and MMP 9 42 129 However HBOT preconditioning may overexpress HSP 70 in the hippocampus which could lead to cognitive deficits and oxidative stress 130 Preconditioning of HBOT could bring protective effects of microvascular endothelial cell protection by increasing Nrf2 and HSP32 activity Recent studies however reveal the therapeutic effects of HBOT on infarction volume BBB and transformed hemorrhage in the absence of the mentioned proteins in the focal cerebral ischemia model 129 HBOT preconditioning may reduce edema via downregulation of aquaporin 4 AQP 4 expression which possess the mechanism to hinder hemorrhage and preserve neural tissue 131 Cultured astrocytes post HBOT revealed an increase in AQP 4 and VEGF demonstrating the ability to modulate BBB openings This mechanism may introduce a possible treatment option for drug transportation into the CNS 132 Additionally HBOT promotes the p44 42 pathway to help prevents the development of brain edema post intracerebral hemorrhage the activation of the pathway correlates to the cerebral ischemic tolerance that was observed 125 In vitro models highlight the protective abilities of HBOT for BBB integrity when occluding and ZO 1 activities were regulated in hypoxic settings 133 Alongside protecting BBB integrity and minimizing edema HBOT may also protect energy metabolism and tissue perfusion by stabilizing glucose levels preventing glutamate levels from increasing lowering lactate pyruvate ratios and increasing Ang 2 activity Protecting energy metabolism gave therapeutic effects including increased microvessel density reduced brain injury and alleviated post ischemic neurological deficits 44 134 5 5 Considerations for HBOT Preconditioning Protocols Hyperbaricity of 2 5 ATA and 21 O2 is not enough to promote ischemic tolerance Therefore understanding the components of HBOT in both hyperoxia and hyperbaricity scenarios is crucial to induce tolerance against ischemic injuries 135 Both preconditioning of HBOT and hypoxia possess similar efficacies in the neonatal brain However the unique defense mechanisms are used during oxidative stress 136 Regular HBOT preconditioning consists of 2 3 ATA with 60 90 min of exposure with 24 h intervals 137 139 Effective ischemic tolerance can be developed when dosed with HBOT for 3 5 days 91 135 Although HBOT also induced neuroprotection against brain injuries due to ischemia during a certain time frame 94 neuroprotection was achieved through biphasic time frames characterized by instant and delayed preconditioning effect 42 140 Instantaneous preconditioning was evident within the first hour after treatment demonstrating alterations in ion channel activities enzyme activity and secondary messengers 140 On the other hand delayed preconditioning involved cellular changes that progressed slower and developed enduring changes in gene and protein expression 140 6 HBOT Primed Stem Cells as a Promising Therapy Stem cells located within niches of the matured brain possess protective and restorative capabilities for the brain post stroke via migration to damaged sites Stem cells are armed with mechanisms such as secretion of angiogenic factors trophic factors regulation of cell death pathway anti inflammatory molecules and replacement of damaged neuronal tissues 3 However limitations exist that prevent stem cells from engaging unaided stroke recovery making therapeutic strategies that promote the brain s reparative capabilities appealing Enhancement of HBOT effects on stem cells is becoming more evident in post stroke recovery studies 141 proposing a potent role of HBOT in stem cell conditioning before cell transplantation 6 1 HBOT Effects on Endogenous Stem Cells In vivo studies reveal the profound effects of HBOT on stem cell populations as shown in Table 2 Most prominent examples include increased amounts of endogenous stem cells via enhancement of stem cells in a pressure sensitive environment 141 142 and multiplication of neural stem cells in adult brain niches 143 which have been observed in various models of TBI induced injuries 144
Biomolecules 2020 10 1279 11 of 26 and non oxygen induced injuries 145 Alongside neural stem cell proliferation HBOT possesses the ability to target damaged sites 123 proposing HBOT therapeutic effects that are not dependent on disease pathologies During circulation vasogenic endothelial progenitor cells EPCs and other specific stem cells released post HBOT may demonstrate therapeutic effects on the stroke injured brain 146 Stem cells located locally or peripherally in the brain may induce treatment benefits when combined with mechanisms of HBOT preconditioning and HBOT mechanisms in stroke An accumulation of studies has demonstrated growing interest in the mechanisms of HBOT that enhance bone marrow derived stem cell circulation 145 Investigations experimented with nitric oxide synthase inhibitors and mice administered with eNOS 141 which revealed the elusive nature of HBOT mechanisms in cerebral neurogenesis upregulation Among the various signaling and growth molecules HIF 1 alpha was stabilized by HBOT inhibiting activation of hypoxia 147 slowing down prolyl hydroxylase induced degradation 148 and enhanced signaling of Wnt beta catenin pathways that raised levels of active neural stem cells 149 High levels of ROS during NSCs proliferation may also induce their own renewal suggesting drug inhibition of ROS may downregulate ROS reproductive activity 150 and enhancement of pro NSC signaling pathways to promote NSC survival Vascular endothelial growth factor VEGF another highly important regulatory molecule and its receptors VEGFR2 ERK and CREB may be involved in HBOT induced NSC proliferation due to their significance in neurogenic pathways 151 Targeting VEGF downregulates HIF 1 alpha which is responsible for promoting hypoxia and ischemia related genes and expressions via inflammation proliferation glycolysis and angiogenesis 42 148 Past studies have demonstrated nontherapeutic effects of upregulating erythropoietin EPO another HIF 1 alpha gene target in the hippocampus and cerebral cortex including BBB permeability prevention brain edema reduction decreased infarction volume and post HBOT neurobehavioral improvement 152 153 On the other hand reduced EPO levels via HBOT promoted homing and engraftment mechanisms of transplantation of stem cells derived from the umbilical cord blood 154 Furthermore an increase in HIF 1 alpha expression was correlated to CXCR4 upregulation after HBOT 113 promoting neural crest stem progenitor cells NCSCs via inhibition of hypoxia involved signaling receptors Cytoplasmic activity of TPM1 increased and TP53 and CDKN1A a cyclin dependent kinase inhibitor decreased following HBOT which led to lower rates apoptosis and higher rates of NCSCs reproduction 113 6 2 HBOT and Exogenous Stem Cells The combination of HBOT and stem cell transplantation may reveal underlying mechanisms among these treatments This concept has been researched in neurological and non neurological settings including TBI 155 SCI 156 and diabetes mellitus 157 HBOT has been found to promote graft survival in the bone marrow peripheral blood and spleen These results were discovered after an umbilical cord blood stem cell transplantation present in a rodent model of whole body irradiation injury 158 In a murine SCI model enhanced MSC graft survival was revealed in animals with combined HBOT and cell therapy 156 These animals also displayed an alleviated inflammatory response including decreased levels of pro inflammatory mediators TNF IL 6 and IFN 156 Results from another study show a suppressed inflammatory response along with an upregulated nerve regeneration and a decrease in expression of TUNEL an apoptosis marker in combination therapy animals 159 6 3 Effects of HBOT In Vitro Potential for Stem Cell Priming Molecular signaling pathways including Wnt catenin VEGF VEGFR2 and CREB are potentially mediated by non stem cell host tissue secretions While information gained from in vivo studies guide in vitro research both stem cell and non stem cell mediated mechanisms must be analyzed The negative effects of HBOT on stem cells must also be considered HBOT reduced cell survival in mesenchymal stem cell MSC cultures 160 The augmented oxygen tension expressed by HBOT subsequently enhances the formation of ROS and releases oxidative stress on cells 161 162
Biomolecules 2020 10 1279 12 of 26 Careful evaluation of HBOT priming stem cells for transplantation must be conducted since exposure to oxidative stress in vitro may advance stem cell resiliency to oxidative stress after transplantation In vitro HBOT priming potentially has genetic molecular or transcriptomic effects on stem cells which enhanced their therapeutic viability HBOT induced oxidative stress may augment the resiliency of stem cells to the harmful post ischemic brain environment Hypoxic preconditioning of stem cells has also shown promising results It has been found to enhance graft survival after transplantation in a hemorrhagic stroke mouse model 163 Results also revealed an increase in stem cell migratory and homing ability 164 166 Cell survival and function are also boosted after transplantation 164 Hypoxia contributes to the low graft survival occurring post stroke transplantation Rampant oxidative stress is also a significant contributor to graft and endogenous cell death 167 168 Exposing stem cells to oxidative stress before transplantation has the potential to expand the survival time by allowing for genetic and phenotypic acclimation in an oxidative stress environment HBOT can also potentially increase stem cell secretome In vitro experiments demonstrate that HBOT affects the secretion profile of stem cells This involves proteins implicated in the oxidative stress response and proteins involved in neuroprotective pathways 160 After HBOT there is increased cellular nitric oxide which allows for the upregulation of growth factors including VEGF and TFGb1 160 MSC cultures also demonstrated HBOT having the ability to enhance the expression of placental growth factor P1GF This was also correlated with increased MSC tubule formation and increased migratory ability 169 HBOT has also revealed its ability to inhibit the differentiation of stem cells in culture 162 Depending on the form of transplantation administered the ability to promote stem cells may become a potential benefit of HBOT priming Table 1 Chronological Reports of the Mechanisms Regulating HBOT Induced Neuroprotection Study Jadhav et al 2009 Mu et al 2013 Lu et al 2014 Xue et al 2016 Guo et al 2016 Yang et al 2017 Discovery In surgical brain injury SBI mice HBOT preconditioning ameliorated neurological function and cerebral edema these neuroprotective effects seemed to be regulated by COX 2 mechanisms as HBOT attenuated SBI induced elevation of hypoxia inducible factor 1alpha and COX 2 activity 170 In permanent MCAO animal models daily HBOT conditioning at 48 h post surgery diminished infarct volume and improved neurological function which correlated with elevated CREB protein expression in the hippocampus and peri infarct area boosting cell multiplication Regarding acute pMCAo models HBOT increased cerebral PP1 expression alleviating CREB phosphorylation and ubiquitination spurred by ischemia Moreover HBOT s regenerative effects against ischemic stroke can be associated with CREB and PP1 mechanisms 37 In transient MCAO rat models HBOT spurred an increase in ERK1 2 signaling due to higher levels of ROS leading to the attenuation of autophagy When U0126 an inhibitor of the ERK1 2 pathway was applied infarct size and autophagy were ameliorated 171 MCAO rats subjected to HBOT preconditioning exhibited diminished infarct size improved neurological behavior and upregulated Sirt1 Nrf2 HO 1 and SOD1 expression as well as reduction of MDA Blocking of Sirt1 or Nrf2 abolished HBOT induced protective effects as Nrf2 HO 1 and SOD1 were repressed Moreover the protective actions of Sirt1 spurred by HBOT may consist of the Nrf2 antioxidant defense mechanism 172 Following successive HBOT pre treatment over five days rats underwent hyperglycemic MCAO Preconditioning with HBOT significantly ameliorated hemorrhagic transformation induced by the Nod like receptor protein 3 signaling and reduced infarct size altogether rehabilitating neurological performance HBOT s neuroprotective effects could be linked to the ROS thioredoxin interacting protein Nod like receptor protein 3 mechanism 126 HBOT ameliorated neurological impairment in TBI rats via upregulation of VEGF VEGFR2 Raf 1 MEK1 2 and ERK1 2 stimulating proliferation of neural stem cells NSC and homing of these cells to the lesion site The examination of HBOT s protective effects in vitro showed similar results as HBO drastically amplified NSC proliferation and VEGF ERK signaling 123
Biomolecules 2020 10 1279 13 of 26 Table 1 Cont Study Discovery Hu et al 2017 He et al 2019 Ying et al 2019 Zhou et al 2019 In hyperglycemia MCAO rats exposure to two atmospheres of HBO for an hour immediately after dextrose administration ameliorated depleted ATP and nitcotinamide adenine dinucleotide levels which in turn elevated silent mating type information regulation 2 homolog 1 alleviating cerebral infarct and neurological dysfunction along with repressing hemorrhagic transformation 14 Mice models of acute TBI demonstrated escalated levels of apoptotic neurons and caspase 3 activity along with attenuation of signaling pathways that regulate apoptosis in neurons e g pAkt Akt pGSK3 GSK3 and catenin By eliminating the TBI induced alterations in these pathways HBOT suppressed neuronal apoptosis 173 BDNF TrkB signaling has been shown to influence rehabilitation after SCI In vivo SCI rat models were exposed to HBOT and both dendritic synaptic deterioration and apoptosis were ameliorated which could be linked to higher levels of BDNF and TrkB activity When ANA 12 an inhibitor of the BDNF TrkB pathway was administered HBOT s neuroprotective effects were reversed indicating that HBOT s therapeutic benefits are mediated by BDNF TrkB signaling 174 Following HBOT Sprague Dawley rats with spinal cord injury SCI displayed ameliorated motor function and attenuated secondary injuries such as inflammation and glial scar production By blocking AKT and NF kB signaling HBOT repressed molecules associated with inflammation iNOS and COX 2 and glial scar generation GFAP and NG2 175 Table 2 Milestone Studies on the Use of HBOT for Stem Cells Study Yang et al 2008 Li et al 2008 Li et al 2009 Rink et al 2010 Cechin et al 2014 Hadanny et al 2015 Dai et al 2015 Yang et al 2017 Discovery Rats were subject to unilateral carotid artery ligation and then 2 h of hypoxia HBO2 was then administered following the hypoxic ischemic event The HBOT was found to upregulate neural stem cell proliferation in neurogenic environments within the adult brain 143 A murine model subjected rats to common carotid artery ligation and hypoxia for 90 min HBOT was administered 24 h prior to the hypoxic ischemic injury Results revealed that rats preconditioned with HBOT had an increased survival rate and the infarct ratio was decreased This indicates that HBOT can provide brain protection via the inhibition of neuronal apoptosis pathways 45 HBOT preconditioned rats where investigated to determine if apoptotic inhibition through a mitochondrial pathway was correlated with neuroprotection in the ischemic injury in the rat brain Preconditioning was conducted four times followed by brain evaluation Results indicated that HBO PC significantly reduced brain edema and decreased infarction volume and improved neurological recovery 117 Transient MCAO rodents outline the therapeutic potential of normobaric and hyperbaric oxygen treatments during ischemia and after ischemia HBOT treated rodents revealed inhibited leukocyte accumulation in the ischemic area due to a reduction in levels of inflammatory chemokines 50 This study allowed pancreatic progenitor cells to mature in a perfluorocarbon based culture device that could adjust the levels of pO2 Enhanced O2 exposure in vitro led to maturation and differentiation of human embryonic stem cell derived pancreatic progenitor cells 176 Patients with cardiac arrest induced chronic cognitive impairments where treated with sessions of HBOT and analyzed After administering HBOT five days per week to chronic stroke patients patients had significant improvements in memory and attention testing 22 A rabbit model seeded human adipose derived stem cells on a gelatin polycaprolactone scaffold to determine the functional and histochemical improvement of tissue engineered cartilage after HBOT The human adipose derived stem cells were found to have improved extracellular matrix secreting abilities after transplantation into a rabbit cartilage defect model when primed with HBOT 177 This study investigated the mechanism of HBOT that promote NSC proliferation and recovery following TBI The study used 24 rats split into a sham group a TBI group and an HBO treated TBI group to determine the neurological differences Neurological function was evaluated and monitored throughout the week HBOT was found to promote neural stem cell migration to areas of injury within the brain in rat models of TBI that were preconditioned with HBO 123
Biomolecules 2020 10 1279 14 of 26 Research supports the evidence that HBOT preconditioning on the healthy brain provides neuroprotective capacity Stem cell preconditioning could also be used as a viable cell therapy strategy post stroke This could also be a viable and potent dual therapy technique administered to patients with a high risk for stroke This strategy uses both a neuroprotective and neurorestorative approach The capability of HBOT to extend graft survival through oxidative stress conditioning inhibit premature differentiation augment migratory capacity enhance injury homing promote anti inflammatory mediation and upregulate trophic factors in the secretome demonstrate the potential of HBOT HBOT is a viable therapeutic strategy that can work alone or combined with other preconditioning strategies to enhance the therapeutic efficacy of transplanted stem cells in the stroke brain 6 4 Recent Literature on HBOT and Stroke Recent literature has expanded knowledge of HBOT and its underlying mechanisms all of which further elucidate its potential as a therapy for stroke stroke related symptoms and other diseases As an efficient and feasible treatment HBOT has elicited neuroprotective effects before the stroke displayed regenerative effects during the acute phase of stroke and even alleviated symptoms during the chronic phase of the stroke Furthermore many diseases that mimic stroke pathology have found HBOT similarly effective 6 4 1 Preconditioning Pretreatment with HBOT has been a focal point of research over recent years An in vitro study examined and found that HBOT preconditioning of primary rat neuronal cells PRNCs mitigates cell death via mitochondrial transfer from astrocytes PRNCs were subject to HBOT before exposure to tumor necrosis factor alpha TNF alpha or lipopolysaccharide LPS injury to induce stroke like cell death Upon examination cell viability and mitochondrial transfer were both observed at augmented levels compared to the non HBOT treated group The ability to ameliorate both stroke induced inflammation and cell death through preconditioning and mitochondrial transfer bolster this as a prophylactic therapy to prevent the devastating effects associated with stroke 178 Another investigation elucidated the effects of HBOT on a rat model of permanent MCAO HBOT lowered infarct volume and improved neurological scores in injured rats An autophagy marker Beclin 1 was seen at decreased levels after treatment Expression of fodrin1 ceased and necrosis marker PI positive cells were seen at decreased levels TUNEL positive cells an indicator of apoptosis were observed at reduced levels and caspase 3 was downregulated Taken together this data indicate that HBOT may ameliorate the detrimental effects associated with ischemia through mitigating autophagy activity apoptosis and necrosis 179 Another murine model featuring intracerebral hemorrhage investigated HBOT s ability to attenuate edema inflammation and microglia activation Pre conditioning with HBOT was conducted for five days before ICH induction MMP9 and brain edema were both less in the HBOT group when compared to control Neuronal cell death and neurological deficits were minimized in the HBOT preconditioned group Notably the expression of M1 markers was reduced consequently inhibiting microglia polarization and inflammatory pathways This was apparent when measuring the concentration of pro inflammatory cytokines TNF alpha and IL 1 with an indication that levels were downregulated Furthermore phosphorylation of JNK and STAT1 were significantly decreased in the HBOT group 180 Lastly a preconditioning combination therapy between melatonin Mel and HBOT was found to provide more favorable effects in the protection of ischemic injury induced cognitive dysfunction and compromised parenchymal integrity in rats Brain infarct area was lower in rats treated with HBOT Mel than in rats treated with either HBOT or Mel monotherapy Apoptotic autophagy and inflammatory markers indicated that combination therapy was more effective The additional benefits provided by HBOT Mel therapy warrant further investigation in the prevention of detrimental outcomes as a result of ischemic injury 181
Biomolecules 2020 10 1279 15 of 26 6 4 2 Post Stroke Treatment On top of providing robust neuroprotective effects before a stroke HBOT has also indicated efficacy in treating stroke patients post ischemia A study elucidated the effects of HBOT on chronic stroke patients who each underwent 40 60 sessions of HBOT therapy Notably 86 of patients displayed clinically significant improvements in cognitive function When comparing cortical and hemorrhagic stroke victims cortical stroke patients displayed heightened improvements in information processing Data also suggested that baseline cognitive function should be contemplated rather than stroke type and location when predicting the magnitude of clinical improvements 182 Furthermore upper limb motor dysfunction is a common debilitation after suffering a stroke HBOT therapy in combination with upper limb exercise and mental imagery EMI has shown promising results in clinical trials in improving outcomes of chronic stroke patients When HBOT EMI patients were compared to EMI patients alone there were no statistically significant differences However HBOT EMI patients showed an upward trend of improved motor function in upper limbs compared to the EMI group Although not many differences were observed data indicate that HBOT is a safe and practical therapy for chronic stroke patients and this combination therapy should be explored further in the future 183 Other than physical dysfunction mental illness may manifest after stroke A link has been found between HBOT and post stroke depression PSD a common symptom many stroke patients experience This is a devastating consequence of stroke especially in other countries where it usually goes untreated A clinical trial revealed an increased response rate and decreased depression scores post HBOT Furthermore HBOT in conjunction with antidepressants was significantly more effective than each respective monotherapy HBOT is a safe and feasible treatment to treat PSD however further elucidation is imperative 184 6 4 3 Diseases Resembling Stroke Pathology and HBOT HBOT has been explored in treating diseases with pathological links to stroke For example TBI often presents with neuronal apoptosis resembling stroke pathology HBOT was investigated on a mouse model of TBI Induction of TBI on mice resulted in activation of caspase 3 decreased levels of pGSK3 GSK3 pAkt Akt and catenin and increased the prevalence of apoptotic neurons prior to HBOT HBOT administration during the acute stage of TBI decreased apoptosis possibly through attenuating the Akt GSK3 catenin pathway Further investigation is necessary to fully comprehend the capacity of mediating this pathway and its implications within controlling TBI induced apoptosis 173 Cerebral air embolism a phenomenon that complicates many medical procedures and can provide life threatening symptoms may be attenuated via HBOT Cerebral air embolism pathology resembles that of stroke often presenting with acute cerebral ischemia induced edema A patient undergoing a right internal jugular catheter procedure soon presented with fixed gaze palsy and left sided hemiparesis upon removal of the wire Imaging supported intraparenchymal air and a bubble in the right internal jugular vein Soon after the manifestation of these symptoms the patient underwent HBOT Highly significant neurological improvements were seen over the course of the next week indicating functional recovery HBOT therapy may elicit ameliorative effects on central air embolism complications and further investigation is warranted 185 Lastly HBOT efficacy was investigated in patients with hypoxic ischemic encephalopathy HIE The subset of patients that received HBOT within nine months after the injury displayed the most significant results This group showed improvements in the disorder of consciousness as well as a more favorable coma recovery scale revised score Overall HBOT within nine months after HIE may facilitate a functional recovery 186 6 4 4 Optimizing Treatment Recent research advances have provided insightful information pertaining to HBOT and conducting the most efficient therapeutic strategy Patients contemplating HBOT therapy may
Biomolecules 2020 10 1279 16 of 26 undergo SPECT CT imaging as a predictor of HBOT efficacy A patient analysis supported a link between large penumbra size and significant benefit from HBOT This size was decreased substantially during therapy and further supported by improved clinical neurologic status and better quality of life Conversely patients with small penumbra size did not significantly improve from HBOT and the change penumbra size was negligible This data suggests that patients presenting with large penumbra size may display more significant improvements than others This imaging based method of prediction may allow the ability to efficiently select patients that could benefit more from HBOT therapy 187 Moreover HBOT for prolonged periods of time can cause oxygen toxicity It is important to evaluate effective protocols to ensure that this phenomenon does not occur during therapy A murine model exhibited that intermittent hyperbaric oxygen exposure IE HBO is linked to protection against oxygen toxicity Continuous exposure CE of HBO increased concentrations of Peroxiredoxin 6 Prdx6 protein an endogenous antioxidant indicating a relationship between the two However the IE HBO group displayed higher amounts of Prdx6 in the rat brains and lungs compared to the CE HBO group IE HBO also enhances NSGPx and GSH activity while mitigating oxidant formation in the lungs and brain Taken together IE HBO mediated Prdx6 expression can suppress oxidative damage in the brain and lungs and overall protect against oxygen toxicity 188 These findings allow for a safer and more effective treatment plan when utilizing HBOT to treat stroke and other diseases In all HBOT presents with a multitude of treatment possibilities ranging from preconditioning to treating chronic disease Moving forward research should continue to explore this prophylactic therapy to better understand the underlying mechanisms that make it so effective Similarly treatment timing session amount and treatment duration should all be elucidated to establish optimal conditions to incorporate the best results 7 Future Directions and Conclusions HBOT has the ability to preserve vulnerable neural tissue and improve outcomes in stroke models as seen in pre clinical studies However further research needs to be conducted to find the most effective regimen of HBOT Randomized controlled trials need to be administered in order to test human effectiveness Even though further research regarding HBOT needs to be studied current research has advanced our understanding of the mechanisms of HBOT specifically in the injured and healthy brain This knowledge has paved the way for the development of HBOT preconditioning strategies Although HBOT preconditioning is a viable and innovative strategy that contains benefits for certain patients limitations are present involving the ability to deliver stroke therapy HBOT has the ability to be applied as a preconditioning mechanism for stem cell transplantation Research indicates that oxidative preconditioning of stem cell grafts through HBOT may be a viable strategy to promote graft survival and optimize graft function during the post ischemic environment In order to explore this concept further research will be necessary regarding the genetic epigenetic secretome and functional influence that HBOT exerts on stem cell populations This potential therapeutic strategy would offer a hybrid approach of combining preconditioning strategies for neuroprotection in the ischemic state of the brain Author Contributions Conceptualization B C N S B G P M S J C Y J P and C V B literature analysis B C N S B G P M S J C Y J P and C V B resources C V B writing original draft preparation B C N S B G P M S J C Y J P and C V B writing review and editing B C N S B G P M S J C Y J P and C V B supervision C V B project administration C V B funding acquisition C V B All authors have read and agreed to the published version of the manuscript Funding Cesar V Borlongan is funded by National Institutes of Health NIH R01NS090962 NIH R01NS102395 and NIH R21NS109575 Acknowledgments The authors thank the entire staff of the Borlongan Neural Transplantation Laboratory for critical discussion of this manuscript Conflicts of Interest The authors declare no conflict of interest
Biomolecules 2020 10 1279 17 of 26 References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Tal S Hadanny A Berkovitz N Sasson E Ben Jacob E Efrati S Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 2015 33 943 951 CrossRef PubMed Harch P G Andrews S R Fogarty E F Lucarini J Van Meter K W Case control study Hyperbaric oxygen treatment of mild traumatic brain injury persistent post concussion syndrome and post traumatic stress disorder Med Gas Res 2017 7 156 174 CrossRef PubMed Yang Y Zhang Y G Lin G A Xie H Q Pan H T Huang B Q Liu J D Liu H Zhang N Li L et al The effects of different hyperbaric oxygen manipulations in rats after traumatic brain injury Neurosci Lett 2014 563 38 43 CrossRef Miljkovic Lolic M Silbergleit R Fiskum G Rosenthal R E Neuroprotective effects of hyperbaric oxygen treatment in experimental focal cerebral ischemia are associated with reduced brain leukocyte myeloperoxidase activity Brain Res 2003 971 90 94 CrossRef Calvert J W Zhou C Nanda A Zhang J H Effect of hyperbaric oxygen on apoptosis in neonatal hypoxia ischemia rat model J Appl Physiol 2003 95 2072 2080 CrossRef PubMed Geng C K Cao H H Ying X Zhang H T Yu H L The effects of hyperbaric oxygen on macrophage polarization after rat spinal cord injury Brain Res 2015 1606 68 76 CrossRef Oyinbo C A Secondary injury mechanisms in traumatic spinal cord injury A nugget of this multiply cascade Acta Neurobiol Exp Wars 2011 71 281 299 Wang L Li W Kang Z Liu Y Deng X Tao H Xu W Li R Sun X Zhang J H Hyperbaric oxygen preconditioning attenuates early apoptosis after spinal cord ischemia in rats J Neurotrauma 2009 26 55 66 CrossRef Shams Z Khalatbary A R Ahmadvand H Zare Z Kian K Neuroprotective effects of hyperbaric oxygen HBO therapy on neuronal death induced by sciatic nerve transection in rat BMC Neurol 2017 17 220 CrossRef Sun L Marti H H Veltkamp R Hyperbaric oxygen reduces tissue hypoxia and hypoxia inducible factor 1 alpha expression in focal cerebral ischemia Stroke 2008 39 1000 1006 CrossRef Zhang X G Jiang Z L Wang G H Li Y C Wang Y Li X Shen H M Therapeutic efficacy of hyperbaric oxygen on traumatic brain injury in the rat and the underlying mechanisms Zhongguo Ying Yong Sheng Li Xue Za Zhi 2012 28 42 46 Lou M Chen Y Ding M Eschenfelder C C Deuschl G Involvement of the mitochondrial ATPsensitive potassium channel in the neuroprotective effect of hyperbaric oxygenation after cerebral ischemia Brain Res Bull 2006 69 109 116 CrossRef PubMed Sun Y Liu D Wang Q Su P Tang Q Hyperbaric oxygen treatment of spinal cord injury in rat model BMC Neurol 2017 17 128 CrossRef PubMed Tan J W Zhang F Liu H J Li Z Hyperbaric oxygen ameliorated the lesion scope and nerve function in acute spinal cord injury patients A retrospective study Clin Biochem 2018 53 1 7 CrossRef PubMed Fu H Li F Thomas S Yang Z Hyperbaric oxygenation alleviates chronic constriction injury CCI induced neuropathic pain and inhibits GABAergic neuron apoptosis in the spinal cord Scand J Pain 2017 17 330 338 CrossRef Daruwalla J Christophi C Hyperbaric oxygen therapy for malignancy A review World J Surg 2006 30 2112 2131 CrossRef PubMed Huang G Xu J Xu L Wang S Li R Liu K Zheng J Cai Z Zhang K Luo Y et al Hyperbaric oxygen preconditioning induces tolerance against oxidative injury and oxygen glucose deprivation by up regulating heat shock protein 32 in rat spinal neurons PLoS ONE 2014 9 e85967 CrossRef Hirata T Cui Y J Funakoshi T Mizukami Y Ishikawa Y Shibasaki F Matsumoto M Sakabe T The temporal profile of genomic responses and protein synthesis in ischemic tolerance of the rat brain induced by repeated hyperbaric oxygen Brain Res 2007 1130 214 222 CrossRef Gunther A Kuppers Tiedt L Schneider P M Kunert I Berrouschot J Schneider D Rossner S Reduced infarct volume and differential effects on glial cell activation after hyperbaric oxygen treatment in rat permanent focal cerebral ischaemia Eur J Neurosci 2005 21 3189 3194 CrossRef
Biomolecules 2020 10 1279 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 18 of 26 Rossignol D A Rossignol L W Hyperbaric oxygen therapy may improve symptoms in autistic children Med Hypotheses 2006 67 216 228 CrossRef Xiong L Zhu Z Dong H Hu W Hou L Chen S Hyperbaric oxygen preconditioning induces neuroprotection against ischemia in transient not permanent middle cerebral artery occlusion rat model Chin Med J 2000 113 836 839 PubMed Mu J Ostrowski R P Soejima Y Rolland W B Krafft P R Tang J Zhang J H Delayed hyperbaric oxygen therapy induces cell proliferation through stabilization of cAMP responsive element binding protein in the rat model of MCAo induced ischemic brain injury Neurobiol Dis 2013 51 133 143 CrossRef PubMed Li J Liu W Ding S Xu W Guan Y Zhang J H Sun X Hyperbaric oxygen preconditioning induces tolerance against brain ischemia reperfusion injury by upregulation of antioxidant enzymes in rats Brain Res 2008 1210 223 229 CrossRef McDonagh M S Morgan D Carson S Russman B S Systematic review of hyperbaric oxygen therapy for cerebral palsy The state of the evidence Dev Med Child Neurol 2007 49 942 947 CrossRef PubMed Danesh Sani S A Shariati Sarabi Z Feiz M R Comprehensive review of hyperbaric oxygen therapy J Craniofac Surg 2012 23 e483 e491 CrossRef Lim S W Wang C C Wang Y H Chio C C Niu K C Kuo J R Microglial activation induced by traumatic brain injury is suppressed by postinjury treatment with hyperbaric oxygen therapy J Surg Res 2013 184 1076 1084 CrossRef Wee H Y Lim S W Chio C C Niu K C Wang C C Kuo J R Hyperbaric oxygen effects on neuronal apoptosis associations in a traumatic brain injury rat model J Surg Res 2015 197 382 389 CrossRef Lim S W Sung K C Shiue Y L Wang C C Chio C C Kuo J R Hyperbaric oxygen effects on depression like behavior and neuroinflammation in traumatic brain injury rats World Neurosurg 2017 100 128 137 CrossRef Vlodavsky E Palzur E Soustiel J F Hyperbaric oxygen therapy reduces neuroinflammation and expression of matrix metalloproteinase 9 in the rat model of traumatic brain injury Neuropathol Appl Neurobiol 2006 32 40 50 CrossRef Harch P G Andrews S R Fogarty E F Amen D Pezzullo J C Lucarini J Aubrey C Taylor D V Staab P K Van Meter K W A phase I study of low pressure hyperbaric oxygen therapy for blast induced post concussion syndrome and post traumatic stress disorder J Neurotrauma 2012 29 168 185 CrossRef Borab Z Mirmanesh M D Gantz M Cusano A Pu L L Systematic review of hyperbaric oxygen therapy for the treatment of radiation induced skin necrosis J Plast Reconstr Aesthet Surg 2017 70 529 538 CrossRef PubMed Londahl M Hyperbaric oxygen therapy as treatment of diabetic foot ulcers Diabetes Metab Res Rev 2012 28 Suppl S1 78 84 CrossRef PubMed Londahl M Hyperbaric oxygen therapy as adjunctive treatment of diabetic foot ulcers Med Clin N Am 2013 97 957 980 CrossRef PubMed Shuvy M Atar D Gabriel Steg P Halvorsen S Jolly S Yusuf S Lotan C Oxygen therapy in acute coronary syndrome Are the benefits worth the risk Eur Heart J 2013 34 1630 1635 CrossRef PubMed Bennett M H Lehm J P Jepson N Hyperbaric oxygen therapy for acute coronary syndrome Cochrane Database Syst Rev 2015 CrossRef Bhutani S Vishwanath G Hyperbaric oxygen and wound healing Indian J Plast Surg 2012 45 316 324 CrossRef Perez J V Serrano A R Andal M P Aldover M C Delayed hyperbaric intervention in life threatening decompression illness Diving Hyperb Med 2017 47 257 259 CrossRef Harch P G Fogarty E F Staab P K Van Meter K Low pressure hyperbaric oxygen therapy and SPECT brain imaging in the treatment of blast induced chronic traumatic brain injury post concussion syndrome and post traumatic stress disorder A case report Cases J 2009 2 6538 CrossRef Xiong T Chen H Luo R Mu D Hyperbaric oxygen therapy for people with autism spectrum disorder ASD Cochrane Database Syst Rev 2016 10 CD010922 CrossRef Cheng O Ostrowski R P Wu B Liu W Chen C Zhang J H Cyclooxygenase 2 mediates hyperbaric oxygen preconditioning in the rat model of transient global cerebral Ischemia Stroke 2011 42 484 490 CrossRef
Biomolecules 2020 10 1279 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 19 of 26 Zhang Y Bai L Shi M Lu H Wu Y Tu J Ni J Wang J Cao L Lei P et al Features and risk factors of carotid atherosclerosis in a population with high stroke incidence in China Oncotarget 2017 8 57477 57488 CrossRef PubMed Wada K Ito M Miyazawa T Katoh H Nawashiro H Shima K Chigasaki H Repeated hyperbaric oxygen induces ischemic tolerance in gerbil hippocampus Brain Res 1996 740 15 20 CrossRef Yamashita S Hirata T Mizukami Y Cui Y J Fukuda S Ishida K Matsumoto M Sakabe T Repeated preconditioning with hyperbaric oxygen induces neuroprotection against forebrain ischemia via suppression of p38 mitogen activated protein kinase Brain Res 2009 1301 171 179 CrossRef PubMed Gao Z X Rao J Li Y H Hyperbaric oxygen preconditioning improves postoperative cognitive dysfunction by reducing oxidant stress and inflammation Neural Regen Res 2017 12 329 336 PubMed Pisoschi A M Pop A The role of antioxidants in the chemistry of oxidative stress A review Eur J Med Chem 2015 97 55 74 CrossRef PubMed Nie H Xiong L Lao N Chen S Xu N Zhu Z Hyperbaric oxygen preconditioning induces tolerance against spinal cord ischemia by upregulation of antioxidant enzymes in rabbits J Cereb Blood Flow Metab 2006 26 666 674 CrossRef PubMed Arieli Y Kotler D Eynan M Hochman A Hyperbaric oxygen preconditioning protects rats against CNS oxygen toxicity Respir Physiol Neurobiol 2014 197 29 35 CrossRef Ni X X Ni M Fan D F Sun Q Kang Z M Cai Z Y Liu Y Liu K Li R P Xu W G Heat shock protein 70 is involved in hyperbaric oxygen preconditioning on decompression sickness in rats Exp Biol Med Maywood 2013 238 12 22 CrossRef Brown I R Heat shock proteins and protection of the nervous system Ann N Y Acad Sci 2007 1113 147 158 CrossRef Huang G Diao J Yi H Xu L Xu J Xu W Signaling pathways involved in HSP32 induction by hyperbaric oxygen in rat spinal neurons Redox Biol 2016 10 108 118 CrossRef Vince R V Oliver K Midgley A W McNaughton L R Madden L A In vitro heat shock of human monocytes results in a proportional increase of inducible Hsp70 expression according to the basal content Amino Acids 2010 38 1423 1428 CrossRef PubMed Srivastava S Alfieri A Siow R C Mann G E Fraser P A Temporal and spatial distribution of Nrf2 in rat brain following stroke Quantification of nuclear to cytoplasmic Nrf2 content using a novel immunohistochemical technique J Physiol 2013 591 3525 3538 CrossRef PubMed Xu J Huang G Zhang K Sun J Xu T Li R Tao H Xu W Nrf2 activation in astrocytes contributes to spinal cord ischemic tolerance induced by hyperbaric oxygen preconditioning J Neurotrauma 2014 31 1343 1353 CrossRef PubMed Perdrizet G A Preoperative stress conditioning in humans Is oxygen the drug of choice Adv Exp Med Biol 2016 876 223 231 PubMed Xue F Huang J W Ding P Y Zang H G Kou Z J Li T Fan J Peng Z W Yan W J Nrf2 antioxidant defense pathway is involved in the neuroprotective effects of Sirt1 against focal cerebral ischemia in rats after hyperbaric oxygen preconditioning Behav Brain Res 2016 309 1 8 CrossRef Zeng Y Xie K Dong H Zhang H Wang F Li Y Xiong L Hyperbaric oxygen preconditioning protects cortical neurons against oxygen glucose deprivation injury Role of peroxisome proliferator activated receptor gamma Brain Res 2012 1452 140 150 CrossRef Yan W Fang Z Yang Q Dong H Lu Y Lei C Xiong L SirT1 mediates hyperbaric oxygen preconditioning induced ischemic tolerance in rat brain J Cereb Blood Flow Metab 2013 33 396 406 CrossRef PubMed Bian H Hu Q Liang X Chen D Li B Tang J Zhang J H Hyperbaric oxygen preconditioning attenuates hemorrhagic transformation through increasing PPARgamma in hyperglycemic MCAO rats Exp Neurol 2015 265 22 29 CrossRef Goldstein L J Gallagher K A Bauer S M Bauer R J Baireddy V Liu Z J Buerk D G Thom S R Velazquez O C Endothelial progenitor cell release into circulation is triggered by hyperoxiainduced increases in bone marrow nitric oxide Stem Cells 2006 24 2309 2318 CrossRef Liu W Li J Sun X Liu K Zhang J H Xu W Tao H Repetitive hyperbaric oxygen exposures enhance sensitivity to convulsion by upregulation of eNOS and nNOS Brain Res 2008 1201 128 134 CrossRef
Biomolecules 2020 10 1279 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 20 of 26 Chen C C Hsia C W Ho C W Liang C M Chen C M Huang K L Kang B H Chen Y H Hypoxia and hyperoxia differentially control proliferation of rat neural crest stem cells via distinct regulatory pathways of the HIF1alpha CXCR4 and TP53 TPM1 proteins Dev Dyn 2017 246 162 185 CrossRef PubMed Sawada N Liao J K Targeting eNOS and beyond Emerging heterogeneity of the role of endothelial Rho proteins in stroke protection Expert Rev Neurother 2009 9 1171 1186 CrossRef PubMed Seyfried J Wullner U Inhibition of thioredoxin reductase induces apoptosis in neuronal cell lines Role of glutathione and the MKK4 JNK pathway Biochem Biophys Res Commun 2007 359 759 764 CrossRef PubMed Peng Y Feng S F Wang Q Wang H N Hou W G Xiong L Luo Z Tan Q R Hyperbaric oxygen preconditioning ameliorates anxiety like behavior and cognitive impairments via upregulation of thioredoxin reductases in stressed rats Prog Neuro Psychopharmacol Biol Psychiatry 2010 34 1018 1025 CrossRef Li J S Zhang W Kang Z M Ding S J Liu W W Zhang J H Guan Y T Sun X J Hyperbaric oxygen preconditioning reduces ischemia reperfusion injury by inhibition of apoptosis via mitochondrial pathway in rat brain Neuroscience 2009 159 1309 1315 CrossRef Wang Y C Zhang S Du T Y Wang B Sun X Q Hyperbaric oxygen preconditioning reduces ischemiareperfusion injury by stimulating autophagy in neurocyte Brain Res 2010 1323 149 151 CrossRef Lu P G Feng H Yuan S J Zhang R W Li M Hu R Liu Z S Yin J Effect of preconditioning with hyperbaric oxygen on neural cell apoptosis after spinal cord injury in rats J Neurosurg Sci 2013 57 253 258 Lu P G Hu S L Hu R Wu N Chen Z Meng H Lin J K Feng H Functional recovery in rat spinal cord injury induced by hyperbaric oxygen preconditioning Neurol Res 2012 34 944 951 CrossRef Ostrowski R P Graupner G Titova E Zhang J Chiu J Dach N Corleone D Tang J Zhang J H The hyperbaric oxygen preconditioning induced brain protection is mediated by a reduction of early apoptosis after transient global cerebral ischemia Neurobiol Dis 2008 29 1 13 CrossRef Yang Y Wei H Zhou X Zhang F Wang C Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor extracellular signal regulated kinase signaling after traumatic brain injury Neuroreport 2017 28 1232 1238 CrossRef Gomez C R Knutson G J Clifton K B Schreiber C A Vuk Pavlovi c S Age dependent response of murine female bone marrow cells to hyperbaric oxygen Biogerontology 2012 13 287 297 CrossRef PubMed Sun L Xie K Zhang C Song R Zhang H Hyperbaric oxygen preconditioning attenuates postoperative cognitive impairment in aged rats Neuroreport 2014 25 718 724 CrossRef PubMed Qin Z Song S Xi G Silbergleit R Keep R F Hoff J T Hua Y Preconditioning with hyperbaric oxygen attenuates brain edema after experimental intracerebral hemorrhage Neurosurg Focus 2007 22 E13 CrossRef PubMed Guo Z N Xu L Hu Q Matei N Yang P Tong L S He Y Guo Z Tang J Yang Y et al Hyperbaric oxygen preconditioning attenuates hemorrhagic transformation through reactive oxygen species thioredoxin interacting protein nod like receptor protein 3 pathway in hyperglycemic middle cerebral artery occlusion rats Crit Care Med 2016 44 e403 e411 CrossRef Jadhav V Ostrowski R P Tong W Matus B Chang C Zhang J H Hyperbaric oxygen preconditioning reduces postoperative brain edema and improves neurological outcomes after surgical brain injury Acta Neurochir Suppl 2010 106 217 220 Soejima Y Hu Q Krafft P R Fujii M Tang J Zhang J H Hyperbaric oxygen preconditioning attenuates hyperglycemia enhanced hemorrhagic transformation by inhibiting matrix metalloproteinases in focal cerebral ischemia in rats Exp Neurol 2013 247 737 743 CrossRef Soejima Y Ostrowski R P Manaenko A Fujii M Tang J Zhang J H Hyperbaric oxygen preconditioning attenuates hyperglycemia enhanced hemorrhagic transformation after transient MCAO in rats Med Gas Res 2012 2 9 CrossRef Lin H Chang C P Lin H J Lin M T Tsai C C Attenuating brain edema hippocampal oxidative stress and cognitive dysfunction in rats using hyperbaric oxygen preconditioning during simulated high altitude exposure J Trauma Acute Care Surg 2012 72 1220 1227 CrossRef Fang J Li H Li G Wang L Effect of hyperbaric oxygen preconditioning on peri hemorrhagic focal edema and aquaporin 4 expression Exp Ther Med 2015 10 699 704 CrossRef Wang F Wang Y Sun T Yu H L Hyperbaric oxygen therapy for the treatment of traumatic brain injury A meta analysis Neurol Sci 2016 37 693 701 CrossRef
Biomolecules 2020 10 1279 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 21 of 26 Hao L Guo X Zou C Zhou H Tian H Zhang Y Song C Liu L Hyperbaric oxygen preconditioning ameliorates blood brain barrier damage induced by hypoxia through modulation of tight junction proteins in an in vitro model Croat Med J 2016 57 51 57 CrossRef Duan S Shao G Yu L Ren C Angiogenesis contributes to the neuroprotection induced by hyperbaric oxygen preconditioning against focal cerebral ischemia in rats Int J Neurosci 2015 125 625 634 CrossRef Dong H Xiong L Zhu Z Chen S Hou L Sakabe T Preconditioning with hyperbaric oxygen and hyperoxia induces tolerance against spinal cord ischemia in rabbits Anesthesiology 2002 96 907 912 CrossRef PubMed Freiberger J J Suliman H B Sheng H McAdoo J Piantadosi C A Warner D S A comparison of hyperbaric oxygen versus hypoxic cerebral preconditioning in neonatal rats Brain Res 2006 1075 213 222 CrossRef PubMed Theodoraki K Tympa A Karmaniolou I Tsaroucha A Arkadopoulos N Smyrniotis V Ischemia reperfusion injury in liver resection A review of preconditioning methods Surg Today 2011 41 620 629 CrossRef PubMed Liu W Liu K Tao H Chen C Zhang J H Sun X Hyperoxia preconditioning The next frontier in neurology Neurol Res 2012 34 415 421 CrossRef PubMed Tal S Hadanny A Sasson E Suzin G Efrati S Hyperbaric oxygen therapy can induce angiogenesis and regeneration of nerve fibers in traumatic brain injury patients Front Hum Neurosci 2017 11 508 CrossRef Losada D M Jordani M E Jordani M C Piccinato M A Fina C F Feres O Chies A B Evora P R e Silva O D Should preconditioning hyperbaric oxygenation protect the liver against ischemia reperfusion injury An experimental study in a rat model Transplant Proc 2014 46 56 62 CrossRef Yokobori S Mazzeo A T Hosein K Gajavelli S Dietrich W D Bullock M R Preconditioning for traumatic brain injury Transl Stroke Res 2013 4 25 39 CrossRef Sullivan R Duncan K Dailey T Kaneko Y Tajiri N Borlongan C V A possible new focus for stroke treatment Migrating stem cells Expert Opin Biol Ther 2015 15 949 958 CrossRef Thom S R Bhopale V M Velazquez O C Goldstein L J Thom L H Buerk D G Stem cell mobilization by hyperbaric oxygen Am J Physiol Hear Circ Physiol 2006 290 H1378 H1386 CrossRef Dhar M Neilsen N Beatty K Eaker S Adair H Geiser D Equine peripheral blood derived mesenchymal stem cells Isolation identification trilineage differentiation and effect of hyperbaric oxygen treatment Equine Vet J 2012 44 600 605 CrossRef Yang Y J Wang X L Yu X H Wang X Xie M Liu C T Hyperbaric oxygen induces endogenous neural stem cells to proliferate and differentiate in hypoxic ischemic brain damage in neonatal rats Undersea Hyperb Med 2008 35 13 29 Wei L Wang J Cao Y Ren Q Zhao L Li X Wang J Hyperbaric oxygenation promotes neural stem cell proliferation and protects the learning and memory ability in neonatal hypoxic ischemic brain damage Int J Clin Exp Pathol 2015 8 1752 1759 PubMed Heyboer M III Milovanova T N Wojcik S Grant W Chin M Hardy K R Lambert D S Logue C Thom S R CD34 CD45 dim stem cell mobilization by hyperbaric oxygen Changes with oxygen dosage Stem Cell Res 2014 12 638 645 CrossRef PubMed Thom S R Milovanova T N Yang M Bhopale V M Sorokina E M Uzun G Malay D S Troiano M A Hardy K R Lambert D S et al Vasculogenic stem cell mobilization and wound recruitment in diabetic patients Increased cell number and intracellular regulatory protein content associated with hyperbaric oxygen therapy Wound Repair Regen 2011 19 149 161 CrossRef PubMed Mu J Krafft P R Zhang J H Hyperbaric oxygen therapy promotes neurogenesis Where do we stand Med Gas Res 2011 1 14 CrossRef PubMed Milosevic J Adler I Manaenko A Schwarz S C Walkinshaw G Arend M Flippin L A Storch A Schwarz J Non hypoxic stabilization of hypoxia inducible factor alpha HIF alpha Relevance in neural progenitor stem cells Neurotox Res 2009 15 367 380 CrossRef Qi C Zhang J Chen X Wan J Wang J Zhang P Liu Y Hypoxia stimulates neural stem cell proliferation by increasing HIF 1 expression and activating Wnt catenin signaling Cell Mol Biol Noisy le Grand 2017 63 12 19 CrossRef
Biomolecules 2020 10 1279 22 of 26 100 Belle J E L Orozco N M Paucar A A Saxe J P Mottahedeh J Pyle A D Wu H Kornblum H I Proliferative neural stem cells have high endogenous ROS levels that regulate self renewal and neurogenesis in a PI3K Akt dependant manner Cell Stem Cell 2012 8 59 71 CrossRef 101 Lu K T Sun C L Wo P Y Y Yen H H Tang T H Ng M C Huang M L Yang Y L Hippocampal neurogenesis after traumatic brain injury is mediated by vascular endothelial growth factor receptor 2 and the Raf MEK ERK cascade J Neurotrauma 2011 28 441 450 CrossRef PubMed 102 Gu G J Li Y P Peng Z Y Xu J J Kang Z M Xu W G Tao H Y Ostrowski R P Zhang J H Sun X J Mechanism of ischemic tolerance induced by hyperbaric oxygen preconditioning involves upregulation of hypoxia inducible factor 1alpha and erythropoietin in rats J Appl Physiol 2008 104 1185 1191 CrossRef PubMed 103 Peng Z Ren P Kang Z Du J Lian Q Liu Y Zhang J H Sun X Up regulated HIF 1alpha is involved in the hypoxic tolerance induced by hyperbaric oxygen preconditioning Brain Res 2008 1212 71 78 CrossRef PubMed 104 Aljitawi O S Paul S Ganguly A Lin T L Ganguly S Vielhauer G Capitano M L Cantilena A Lipe B Mahnken J D et al Erythropoietin modulation is associated with improved homing and engraftment after umbilical cord blood transplantation Blood 2016 128 3000 3010 CrossRef PubMed 105 Zhou H X Liu Z G Liu X J Chen Q X Umbilical cord derived mesenchymal stem cell transplantation combined with hyperbaric oxygen treatment for repair of traumatic brain injury Neural Regen Res 2016 11 107 113 CrossRef PubMed 106 Geng C K Cao H H Ying X Yu H L Effect of mesenchymal stem cells transplantation combining with hyperbaric oxygen therapy on rehabilitation of rat spinal cord injury Asian Pac J Trop Med 2015 8 468 473 CrossRef PubMed 107 Estrada E J Valacchi F Nicora E Brieva S Esteve C Echevarria L Froud T Bernetti K Cayetano S M Velazquez O et al Combined treatment of intrapancreatic autologous bone marrow stem cells and hyperbaric oxygen in type 2 diabetes mellitus Cell Transplant 2008 17 1295 1304 CrossRef 108 Aljitawi O S Xiao Y Eskew J D Parelkar N K Swink M Radel J Lin T L Kimler B F Mahnken J D McGuirk J P et al Hyperbaric oxygen improves engraftment of ex vivo expanded and gene transduced human CD34 cells in a murine model of umbilical cord blood transplantation Blood Cells Mol Dis 2014 52 59 67 CrossRef 109 Pan H C Chin C S Yang D Y Ho S P Chen C J Hwang S M Chang M H Cheng F C Human amniotic fluid mesenchymal stem cells in combination with hyperbaric oxygen augment peripheral nerve regeneration Neurochem Res 2009 34 1304 1316 CrossRef 110 Schulze J Kaiser O Paasche G Lamm H Pich A Hoffmann A Lenarz T Warnecke A Effect of hyperbaric oxygen on BDNF release and neuroprotection Investigations with human mesenchymal stem cells and genetically modified NIH3T3 fibroblasts as putative cell therapeutics PLoS ONE 2017 12 e0178182 CrossRef 111 Thom S R Oxidative stress is fundamental to hyperbaric oxygen therapy J Appl Physiol 2009 106 988 995 CrossRef PubMed 112 Cheung K Y Berry A Li D Aljitawi O S Hyperbaric oxygen treatment effects on in vitro cultured umbilical cord blood CD34 cells Cytotherapy 2018 20 87 94 CrossRef PubMed 113 Wakai T Narasimhan P Sakata H Wang E Yoshioka H Kinouchi H Chan P H Hypoxic preconditioning enhances neural stem cell transplantation therapy after intracerebral hemorrhage in mice J Cereb Blood Flow Metab 2016 36 2134 2145 CrossRef PubMed 114 Hu X Wei L Taylor T M Wei J Zhou X Wang J A Yu S P Hypoxic preconditioning enhances bone marrow mesenchymal stem cell migration via Kv2 1 channel and FAK activation Am J Physiol Cell Physiol 2011 301 C362 C372 CrossRef 115 Gross R Golan H Fishlev G Bechor Y Volkov O Bergan J Friedman M Hoofien D Shlamkovitch N Ben Jacob E et al Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury Randomized prospective trial PLoS ONE 2013 8 e79995 116 Lee Y S Chio C C Chang C P Wang L C Chiang P M Niu K C Tsai K J Long course hyperbaric oxygen stimulates neurogenesis and attenuates inflammation after ischemic stroke Mediat Inflamm 2013 2013 512978 CrossRef
Biomolecules 2020 10 1279 23 of 26 117 Wei N Yu S P Gu X Taylor T M Song D Liu X F Wei L Delayed intranasal delivery of hypoxicpreconditioned bone marrow mesenchymal stem cells enhanced cell homing and therapeutic benefits after ischemic stroke in mice Cell Transplant 2013 22 977 991 CrossRef 118 Wei L Fraser J L Lu Z Y Hu X Yu S P Transplantation of hypoxia preconditioned bone marrow mesenchymal stem cells enhances angiogenesis and neurogenesis after cerebral ischemia in rats Neurobiol Dis 2012 46 635 645 CrossRef 119 Chen H Yoshioka H Kim G S Jung J E Okami N Sakata H Maier C M Narasimhan P Goeders C E Chan P H Oxidative stress in ischemic brain damage Mechanisms of cell death and potential molecular targets for neuroprotection Antioxid Redox Signal 2011 14 1505 1517 CrossRef 120 Xing C Arai K Lo E H Hommel M Pathophysiologic cascades in ischemic stroke Int J Stroke 2012 7 378 385 CrossRef 121 Venetsanou K Fildissis G Tokta R Brinias C Baltopoulos G The role of nitric oxide in cellular response to hyperbaric conditions Eur J Appl Physiol 2012 112 677 687 CrossRef PubMed 122 Shyu K G Hung H F Wang B W Chang H Hyperbaric oxygen induces placental growth factor expression in bone marrow derived mesenchymal stem cells Life Sci 2008 83 65 73 CrossRef PubMed 123 Jadhav V Ostrowski R P Tong W Matus B Jesunathadas R Zhang J H Cyclo xygoenase 2 mediates hyperbaric oxygen preconditioning induced neuroprotection in the mouse model of surgical brain injury Stroke 2009 40 3139 3142 CrossRef PubMed 124 Lu Y Kang J Bai Y Zhang Y Li H Yang X Xiang X Wang X Huang Y Su J et al Hyperbaric oxygen enlarges the area of brain damage in MCAO rats by blocking autophagy via ERK1 2 activation Eur J Pharmacol 2014 728 93 99 CrossRef 125 He H Li X He Y Hyperbaric oxygen therapy attenuates neuronal apoptosis induced by traumatic brain injury via Akt GSK3 catenin pathway Neuropsychiatr Dis Treat 2019 15 369 374 CrossRef 126 Ying X Tu W Li S Wu Q Chen X Zhou Y Hu J Yang G Jiang S Hyperbaric oxygen therapy reduces apoptosis and dendritic synaptic degeneration via the BDNF TrkB signaling pathways in SCI rats Life Sci 2019 229 187 199 CrossRef PubMed 127 Zhou Y Dong Q Pan Z Song Y Su P Niu Y Sun Y Liu D Hyperbaric oxygen improves functional recovery of the injured spinal cord by inhibiting inflammation and glial scar formation Am J Phys Med Rehabil 2019 98 914 920 CrossRef PubMed 128 Cechin S Alvarez Cubela S Giraldo J A Molano R D Villate S Ricordi C Pileggi A Inverardi L Fraker C A Dominguez Bendala J Influence of in vitro and in vivo oxygen modulation on beta cell differentiation from human embryonic stem cells Stem Cells Transl Med 2014 3 277 289 CrossRef PubMed 129 Dai N T Fan G Y Liou N H Wang Y W Fu K Y Ma K H Liu J C Chang S C Huang K L Dai L G et al Histochemical and functional improvement of adipose derived stem cell based tissue engineered cartilage by hyperbaric oxygen air treatment in a rabbit articular defect model Ann Plast Surg 2015 74 Suppl S2 S139 S145 CrossRef 130 Lippert T Borlongan C V Prophylactic treatment of hyperbaric oxygen treatment mitigates inflammatory response via mitochondria transfer CNS Neurosci Ther 2019 25 815 823 CrossRef 131 Lu K Wang H Ge X Liu Q Chen M Shen Y Liu X Pan S Hyperbaric oxygen protects against cerebral damage in permanent middle cerebral artery occlusion rats and inhibits autophagy activity Neurocrit Care 2019 30 98 105 CrossRef PubMed 132 Wang M Cheng L Chen Z L Mungur R Xu S H Wu J Liu X L Wan S Hyperbaric oxygen preconditioning attenuates brain injury after intracerebral hemorrhage by regulating microglia polarization in rats CNS Neurosci Ther 2019 25 1126 1133 CrossRef PubMed 133 Lin K C Chen K H Wallace C G Chen Y L Ko S F Lee M S Yip H K Combined therapy with hyperbaric oxygen and melatonin effectively reduce brain infarct volume and preserve neurological function after acute ischemic infarct in rat J Neuropathol Exp Neurol 2019 78 949 960 CrossRef PubMed 134 Hadanny A Rittblat M Bitterman M May Raz I Suzin G Boussi Gross R Zemel Y Bechor Y Catalogna M Efrati S Hyperbaric oxygen therapy improves neurocognitive functions of post stroke patients A retrospective analysis Restor Neurol Neurosci 2020 38 93 107 CrossRef PubMed
Biomolecules 2020 10 1279 24 of 26 135 Schiavo S Richardson D Santa Mina D Buryk Iggers S Uehling J Carroll J Clarke H Djaiani C Gershinsky M Katznelson R Hyperbaric oxygen and focused rehabilitation program A feasibility study in improving upper limb motor function after stroke Appl Physiol Nutr Metab 2020 CrossRef PubMed 136 Liang X X Hao Y G Duan X M Han X L Cai X X Hyperbaric oxygen therapy for post stroke depression A systematic review and meta analysis Clin Neurol Neurosurg 2020 195 105910 CrossRef 137 Murphy R P Donnellan J A high pressure solution for a high pressure situation Management of cerebral air embolism with hyperbaric oxygen therapy Cureus 2019 11 e5559 CrossRef 138 Sankaran R Radhakrishnan K Sundaram K R Hyperbaric oxygen therapy in patients with hypoxic ischemic encephalopathy Neurol India 2019 67 728 731 139 Golan H Makogon B Volkov O Smolyakov Y Hadanny A Efrati S Imaging based predictors for hyperbaric oxygen therapy outcome in post stroke patients Report 1 Med Hypotheses 2020 136 109510 CrossRef 140 Zhang L Zhang Y Wang Z Chen Y Li R Intermittent hyperbaric oxygen exposure mobilizing peroxiredoxin 6 to prevent oxygen toxicity J Physiol Sci 2019 69 779 790 CrossRef 141 Guzik T J Korbut R Adamek Guzik T Nitric oxide and superoxide in inflammation and immune regulation J Physiol Pharmacol 2003 54 469 487 PubMed 142 Go A S Executive summary Heart disease and stroke statistics 2014 update A report from the American Heart Association Circulation 2014 129 399 410 CrossRef PubMed 143 Knecht T Story J Liu J Davis W Borlongan C V Pena I C D Adjunctive therapy approaches for ischemic stroke Innovations to expand time window of treatment Int J Mol Sci 2017 18 2756 CrossRef PubMed 144 Stonesifer C Corey S Ghanekar S Diamandis Z Acosta S A Borlongan C V Stem cell therapy for abrogating stroke induced neuroinflammation and relevant secondary cell death mechanisms Prog Neurobiol 2017 158 94 131 CrossRef PubMed 145 Broughton B R Reutens D C Sobey C G Apoptotic mechanisms after cerebral ischemia Stroke 2009 40 e331 e339 CrossRef PubMed 146 Drummond G R Sobey C G Endothelial NADPH oxidases Which NOX to target in vascular disease Trends Endocrinol Metab 2014 25 452 463 CrossRef 147 Stokum J A Gerzanich V Simard J M Molecular pathophysiology of cerebral edema J Cereb Blood Flow Metab 2016 36 513 538 CrossRef 148 Lakhan S E Kirchgessner A Hofer M Inflammatory mechanisms in ischemic stroke Therapeutic approaches J Transl Med 2009 7 97 CrossRef 149 Wetterling F Chatzikonstantinou E Tritschler L Meairs S Fatar M Schad L R Ansar S Investigating potentially salvageable penumbra tissue in an in vivo model of transient ischemic stroke using sodium diffusion and perfusion magnetic resonance imaging BMC Neurosci 2016 17 82 CrossRef 150 Ostrowski R P Stepien K Pucko E Matyja E The efficacy of hyperbaric oxygen in hemorrhagic stroke Experimental and clinical implications Arch Med Sci 2017 13 1217 1223 CrossRef 151 Ostrowski R P Tang J Zhang J H Hyperbaric oxygen suppresses NADPH oxidase in a rat subarachnoid hemorrhage model Stroke 2006 37 1314 1318 CrossRef 152 Cimino F Balestra C Germonpr P De Bels D Tillmans F Saija A Speciale A Virgili F Pulsed high oxygen induces a hypoxic like response in human umbilical endothelial cells and in humans J Appl Physiol 2012 113 1684 1689 CrossRef PubMed 153 Ben Yosef Y Miller A Shapiro S Lahat N Hypoxia of endothelial cells leads to MMP 2 dependent survival and death Am J Physiol Cell Physiol 2005 289 C1321 C1331 CrossRef PubMed 154 Baratz Goldstein R Toussia Cohen S Elpaz A Rubovitch V Pick C G Immediate and delayed hyperbaric oxygen therapy as a neuroprotective treatment for traumatic brain injury in mice Mol Cell Neurosci 2017 83 74 82 CrossRef PubMed 155 Hu Q Manaenko A Bian H Guo Z Huang J L Guo Z N Yang P Tang J Zhang J H Hyperbaric oxygen reduces infarction volume and hemorrhagic transformation through ATP NAD sirt1 pathway in hyperglycemic middle cerebral artery occlusion rats Stroke 2017 48 1655 1664 CrossRef PubMed 156 Chang C F Niu K C Hoffer B J Wang Y Borlongan C V Hyperbaric oxygen therapy for treatment of postischemic stroke in adult rats Exp Neurol 2000 166 298 306 CrossRef
Biomolecules 2020 10 1279 25 of 26 157 Singhal A B Benner T Roccatagliata L Koroshetz W J Schaefer P W Lo E H Buonanno F S Gonzalez R G Sorensen A G A pilot study of normobaric oxygen therapy in acute ischemic stroke Stroke 2005 36 797 802 CrossRef 158 Rink C Roy S Khan M Ananth P Kuppusamy P Sen C K Khanna S Oxygen sensitive outcomes and gene expression in acute ischemic stroke J Cereb Blood Flow Metab 2010 30 1275 1287 CrossRef 159 Matchett G A Martin R D Zhang J H Hyperbaric oxygen therapy and cerebral ischemia Neuroprotective mechanisms Neurol Res 2009 31 114 121 CrossRef 160 Nemoto E M Betterman K Neuroprotective effects of hyperbaric oxygen treatment on traumatic brain injury in the rat Neurol Res 2007 29 116 126 CrossRef 161 Veltkamp R Siebing D A Sun L Heiland S Bieber K Marti H H Nagel S Schwab S Schwaninger M Hyperbaric oxygen reduces blood brain barrier damage and edema after transient focal cerebral ischemia Stroke 2005 36 1679 1683 CrossRef 162 Ploughman M Austin M W Glynn L Corbett D The effects of poststroke aerobic exercise on neuroplasticity A systematic review of animal and clinical studies Transl Stroke Res 2015 6 13 28 CrossRef PubMed 163 Hadanny A Golan H Fishlev G Bechor Y Volkov O Suzin G Ben Jacob E Efrati S Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restor Neurol Neurosci 2015 33 471 486 CrossRef PubMed 164 Ding Z Tong W C Lu X X Peng H P Hyperbaric oxygen therapy in acute ischemic stroke A review Interv Neurol 2014 2 201 211 CrossRef PubMed 165 Padma M V Bhasin A Bhatia R Garg A Singh M B Tripathi M Prasad K Normobaric oxygen therapy in acute ischemic stroke A pilot study in Indian patients Ann Indian Acad Neurol 2010 13 284 288 CrossRef PubMed 166 Shi S Qi Z Lou Y Liu K J Normobaric oxygen treatment in acute ischemic stroke A clinical perspective Med Gas Res 2016 6 147 153 PubMed 167 Donati A Damiani E Zuccari S Domizi R Scorcella C Girardis M Giulietti A Vignini A Adrario E Romano R et al Effects of short term hyperoxia on erythropoietin levels and microcirculation in critically Ill patients A prospective observational pilot study BMC Anesthesiol 2017 17 49 CrossRef 168 Khalif M Wiams K Ben Aziz M Balestra C Sosnowski M Effect of induced relative hypoxia on reticulocyte count in oncological abdominal surgery A single centre controlled randomized pilot study Int J Sci Res 2018 7 12 16 169 Muralidharan G Rao G H R Oxygen as a therapeutic drug Hyperbaric oxygen therapy Biomed Pharmacol J 2020 13 521 528 CrossRef 170 Singhal A B A Review of oxygen therapy in ischemic stroke Neurol Res 2007 29 173 183 CrossRef 171 Zhai W W Sun L Yu Z Q Chen G Hyperbaric oxygen therapy in experimental and clinical stroke Med Gas Res 2016 6 111 118 172 Godman C A Chheda K P Hightower L E Perdrizet G Shin D G Giardina C Hyperbaric oxygen induces a cytoprotective and angiogenic response in human microvascular endothelial cells Cell Stress Chaperones 2010 15 431 442 CrossRef 173 Ostrowski R P Stepien K Pucko E Matyja E Hyperbaric oxygen modalities are differentially effective in distinct brain ischemia models Med Gas Res 2016 6 39 47 CrossRef 174 Wang X L Zhao Y S Yang Y J Xie M Yu X H Therapeutic window of hyperbaric oxygen therapy for hypoxic ischemic brain damage in newborn rats Brain Res 2008 1222 87 94 CrossRef 175 Yin D Zhou C Kusaka I Calvert J W Parent A D Nanda A Zhang J H Inhibition of apoptosis by hyperbaric oxygen in a rat focal cerebral ischemic model J Cereb Blood Flow Metab 2003 23 855 864 CrossRef 176 Lou M Eschenfelder C C Herdegen T Brecht S Deuschl G Therapeutic window for use of hyperbaric oxygenation in focal transient ischemia in rats Stroke 2004 35 578 583 CrossRef 177 Yin D Zhang J H Delayed and multiple hyperbaric oxygen treatments expand therapeutic window in rat focal cerebral ischemic model Neurocrit Care 2005 2 206 211 CrossRef 178 Bennett M H Weibel S Wasiak J Schnabel A French C Kranke P Hyperbaric oxygen therapy for acute ischaemic stroke Cochrane Database Syst Rev 2014 CrossRef
Biomolecules 2020 10 1279 26 of 26 179 Sanchez E C Mechanisms of action of hyperbaric oxygenation in stroke A review Crit Care Nurs Q 2013 36 290 298 CrossRef 180 Li Y Dong H Chen M Liu J Yang L Chen S Xiong L Preconditioning with repeated hyperbaric oxygen induces myocardial and cerebral protection in patients undergoing coronary artery bypass graft surgery A prospective randomized controlled clinical trial J Cardiothorac Vasc Anesth 2011 25 908 916 CrossRef 181 Hu S L Feng H Xi G H Hyperbaric oxygen therapy and preconditioning for ischemic and hemorrhagic stroke Med Gas Res 2016 6 232 236 CrossRef 182 Hu Q Liang X Chen D Chen Y Doycheva D Tang J Tang J Zhang J H Delayed hyperbaric oxygen therapy promotes neurogenesis through reactive oxygen species hypoxia inducible factor 1alpha beta catenin pathway in middle cerebral artery occlusion rats Stroke 2014 45 1807 1814 CrossRef 183 Gao Yu C Cong Yina D Li Jun Z Fei L Hua F Effects of hyperbaric oxygen preconditioning on energy metabolism and glutamate level in the peri infarct area following permanent MCAO Undersea Hyperb Med 2011 38 91 99 184 Li Z Liu W Kang Z Lv S Han C Yun L Sun X Zhang J H Mechanism of hyperbaric oxygen preconditioning in neonatal hypoxia ischemia rat model Brain Res 2008 1196 151 156 CrossRef 185 Yang Z J Xie Y Bosco G M Chen C Camporesi E M Hyperbaric oxygenation alleviates MCAO induced brain injury and reduces hydroxyl radical formation and glutamate release Eur J Appl Physiol 2010 108 513 522 CrossRef 186 Zhou J G Fang Y Q Liu C Y Zhou Y Q Ji Y F Liu J C Effect of hyperbaric oxygen on the expression of nitric oxide synthase mRNA in cortex after acute traumatic cerebral injury Zhongguo Ying Yong Sheng Li Xue Za Zhi 2012 28 38 41 187 Yu M Xue Y Liang W Zhang Y Zhang Z Protection mechanism of early hyperbaric oxygen therapy in rats with permanent cerebral ischemia J Phys Ther Sci 2015 27 3271 3274 CrossRef 188 Lavrnja I Parabucki A Brkic P Jovanovic T Dacic S Savic D Pantic I Stojiljkovic M Pekovic S Repetitive hyperbaric oxygenation attenuates reactive astrogliosis and suppresses expression of inflammatory mediators in the rat model of brain injury Mediat Inflamm 2015 2015 498405 CrossRef 2020 by the authors Licensee MDPI Basel Switzerland This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution CC BY license http creativecommons org licenses by 4 0
Ann N Y Acad Sci ISSN 0077 8923 ANNALS OF THE NEW YORK ACADEMY OF SCIENCES Issue Aging Cancer and Age Related Diseases Hyperbaric oxygen treatment induces antioxidant gene expression Cassandra A Godman 1 Rashmi Joshi 1 Charles Giardina 1 George Perdrizet 2 and Lawrence E Hightower1 1 Department of Molecular and Cell Biology University of Connecticut Storrs Connecticut 2 Department of Surgery Morristown Memorial Hospital Morristown New Jersey Address for correspondence Cassandra A Godman 91 North Eagleville Road Unit 3125 Storrs CT 06269 Cassandra godman uconn edu Although the underlying molecular causes of aging are not entirely clear hormetic agents like exercise heat and calorie restriction may generate a mild pro oxidant stress that induces cell protective responses to promote healthy aging As an individual ages many cellular and physiological processes decline including wound healing and reparative angiogenesis This is particularly critical in patients with chronic non healing wounds who tend to be older We are interested in the potential beneficial effects of hyperbaric oxygen as a mild hormetic stress on human microvascular endothelial cells We analyzed global gene expression changes in human endothelial cells following a hyperbaric exposure comparable to a clinical treatment Our analysis revealed an upregulation of antioxidant cytoprotective and immediate early genes This increase coincided with an increased resistance to a lethal oxidative stress Our data indicate that hyperbaric oxygen can induce protection against oxidative insults in endothelial cells and may provide an easily administered hormetic treatment to help promote healthy aging Key words hyperbaric oxygen therapy oxidative stress antioxidant genes aging Nrf2 transcription factor endothelial cells Introduction Aging is a complex biological process that has been attributed to several mechanisms Currently there is only a limited and somewhat superficial knowledge of the molecular mechanisms involved in aging and longevity The interplay between cellular stressors such as reactive oxygen species ROS and protective antioxidant responses is generally understood to be an important factor for determining lifespan Factors that act to increase resistance to stress such as antioxidant enzymes and molecules were long suspected to have anti aging benefits 1 In fact studies in model organisms like C elegans D melanogaster and M musculus have linked a number of genetic loci with an enhanced stress resistance and likewise an increased lifespan 1 Rattan and colleagues have attributed the process of aging to a progressive loss of cellular function 2 This change which is defined by in creased molecular heterogeneity leads to greater susceptibility to disease and ultimately death The concept of molecular heterogeneity has been frequently invoked to explain individual variability in the aging process This variability is described as the interaction among genetic traits the environment and random events such as spontaneous genetic mutation Stress induced hormesis may be one effective way to reduce this accumulation of molecular damage thus promoting healthy aging 3 The phenomenon known as hormesis is a process that results in a functional improvement of cellular stress resistance survival and longevity in response to sub lethal levels of stress It has been proposed that hormesis can promote healthy aging One example of unhealthy aging is the decrease of angiogenesis that occurs in aged individuals which may be a major factor in slower wound healing 2 It has been shown that a sub lethal heat doi 10 1111 j 1749 6632 2009 05393 x 178 c 2010 New York Academy of Sciences Ann N Y Acad Sci 1197 2010 178 183
Godman et al stress to vascular endothelial cells improves the formation of vascular tubules in vitro which should accelerate angiogenesis and improve wound healing capabilities 4 The most widely employed hormetic stresses include exercise calorie restriction heat stress and pro oxidants Exercise requires an increase in ATP production which leads to an increased metabolism resulting in an increased production of ROS Elevated ROS induces endogenous defense mechanisms such as oxidative damage repair enzymes and antioxidants The mild oxidative stress generated through regular exercise has been associated with a decreased incidence of ROS related diseases such as heart disease type II diabetes and rheumatic arthritis 5 Alternatively calorie restriction serves to slow metabolism and reduce production of ROS again leading to reduction in the appearance of ROS related disease 6 The first nonhuman primate study of caloric restriction without malnutrition was recently published 7 This study found that caloric restriction delayed the onset of age associated diseases such as diabetes cancer and cardiovascular disease Not only is there less ROS produced metabolically but also cells in calorierestricted organisms are more efficient in neutralizing ROS using elevated antioxidant defenses Transient bouts of heat stress have also been shown to increase the lifespan of C elegans and other organisms 8 While the mechanism by which heat stress prolongs life is still under investigation one observation our lab has made is that antioxidant genes are induced following a heat stress unpublished Finally pro oxidants have also been shown to have a hormetic effect on several organisms Pro oxidants such as juglone produce low levels of ROS similar to exercise which serves to increase endogenous protective mechanisms 9 Age dependent decreases in the activity of antioxidant enzymes have been previously reported 10 11 Shih and Yen have suggested that changes in Nrf2 expression and MAPK regulation of the Nrf2 pathway are involved in these age related decreases 11 Likewise Suh and colleagues have concluded that the Nrf2 signaling pathway is able to be activated upon treatment with lipoic acid in aged rats suggesting that restoration of this protective pathway may be an effective means of slowing the aging process 12 This key observation is important to our study because it raises the possibility that hyperbaric oxygen Hyperbaric oxygen and aging therapy could reverse age related declines in antioxidant and detoxification enzymes Because the Nrf2 signaling pathway has the potential to activate over 200 antioxidant and cytoprotective genes in a variety of cells and tissues it could reduce the incidence of ROS induced age related diseases effectively promoting healthy aging Hyperbaric oxygen HBO therapy has recently been promoted as an approach to slow aging HBO treatment HBOT is the medical use of oxygen at higher than 1 atmosphere atm of pressure The therapeutic principle behind HBO stems from increasing the partial pressure of oxygen in the tissues of the body In addition HBO increases the oxygen carrying capacity of blood plasma beyond those achievable under normobaric conditions Currently it is used to treat CO poisoning delayed radiation injuries decompression sickness as well as non healing diabetic wounds and others 13 Furthermore HBO preconditioning has been shown to have hormetic effects on stress resistance and can increase the longevity of C elegans 14 Although the mechanism through which HBO increases longevity is unclear it is likely to be related to the fact that HBO can induce low levels of oxidative stressors like ROS 15 This low level of ROS could be acting to induce protective gene expression and to help cells and tissues manage various environmental and endogenous stressors more efficiently We wanted to address this possibility using human microvascular endothelial cells as our model system to study the effects of HBO These cells are a direct target of HBO during wound healing and previous research has shown that HBO can increase growth factor expression within the wound site that in turn helps stimulate angiogenesis 16 To date studies have been limited to identifying select genes involved in the HBO mechanism To gain a more global view of the genomic response of human microvascular endothelial cells to HBO we performed a microarray analysis of gene expression Using these data we sought to identify the antioxidant and cytoprotective genes induced by HBO and whether or not their induction could protect cells against lethal oxidant stresses In addition we identified the cellular pathways predicted to undergo dramatic changes following HBO treatment based upon the number of up and down regulated genes in each pathway c 2010 New York Academy of Sciences Ann N Y Acad Sci 1197 2010 178 183 179
Godman et al Hyperbaric oxygen and aging Figure 1 Experimental design This figure illustrates the basis of our experimental design Experimental design The human microvascular endothelial cell line HMEC 1 was obtained from the Centers for Disease Control and maintained at 37 C 5 CO2 in MCDB131 media supplemented with 10 FBS 1 antibiotic antimycotic 1 g ml hydrocortisone and 10 ng ml human epidermal growth factor Cells were grown to 80 90 confluency and treated with our standard HBO protocol 1 h 2 4 atm 100 O2 in CO2 independent media Control cells received a media change only mRNA was either extracted immediately following HBO 0 h or following a 24 h recovery in normal conditions Resulting RNA was quantified and run on an Illumina microarray Fig 1 Intensity values were subjected to normalization and statistical analysis Results for selected genes were validated using quantitative PCR qPCR For the viability assay cells were exposed 180 to varying concentrations of t butyl hydroperoxide after HBOT and allowed to recover for 16 h in normal culture conditions before being subjected to the MTT assay Promega Madison WI USA Results Figure 2 illustrates selected results from the microarray Intensity values from the array were normalized and analyzed using Limma SAM or SPH statistical packages to determine differentially expressed genes Log2 fold changes for selected cytoprotective genes are shown left panel Genes uncovered in this experiment include the 70 kilodalton heat shock protein HSPA1A heme oxygenase 1 HMOX1 and metallothionein 1X MT1X which collectively can provide protection from metabolic proteotoxic and oxidative forms of stress Analysis also implicated ERK MAPK signaling including the c 2010 New York Academy of Sciences Ann N Y Acad Sci 1197 2010 178 183
Godman et al Hyperbaric oxygen and aging Figure 2 Activation of cytoprotective genes following HBOT These graphs show log2 fold changes of select antioxidant left panel cytoprotective left panel and immediate early right panel genes among the different treatments and recovery periods activation of a number of immediate early genes that can potentially influence apoptotic signaling right panel Further analysis is underway to determine whether these changes affect cell survival Figure 3 shows the results of qPCR following HBOT and various recovery periods HMEC 1 cells were subjected to HBOT and allowed to recover for indicated times before RNA extraction and qPCR Relative expression for four antioxidant genes is shown P 0 05 when compared to control levels All genes have a peak activation point following HBOT and most center on the 4 h time point Figure 4 illustrates that these changes in gene expression translate to protection against a lethal oxidative stress HMEC 1 cells were plated and allowed to attach for 48 h at which time they were subjected to one round of HBO treatment 100 O2 2 4 atm 1 h and allowed to recover in normal culture conditions for 16 h Cells were treated with t butyl hydroperoxide t butyl OOH at varying concentrations for 6 h and then analyzed for cell viability using an MTS assay Cell viability in the HBO treated cultures was significantly increased under all the conditions tested P 0 05 HBO preconditioning increased the number of viable cells in the cultures treated with HBO indicating both a general stimulatory and a protective effect of HBO on endothelial cell viability These findings raise the possibility that the protection afforded by HBO may arise from the coordinated expression of antioxidant and cytoprotective genes Major targets for protection by proteins encoded by both groups of genes are likely to be proteins sensitive to oxidative damage denaturation and aggregation Discussion Our results indicate that HBOT can change gene expression in a number of cellular pathways including the Nrf2 Integrin and ERK MAPK pathways These pathways contain a number of genes that are critical in cellular defense The functional significance of these gene expression changes is supported by our finding that HBO treated cells are protected against an otherwise lethal oxidative stress These findings support the potential benefit of HBO in a number of clinical applications For example a pre conditioning HBO treatment may be an attractive option for patients about to undergo particularly stressful operations including open heart surgeries A recent study has demonstrated the ability of HBO pretreatment to protect humans from acute ischemia during coronary artery bypass grafting procedures employing cardiopulmonary bypass 17 18 More generally HBO could be a viable treatment option to slow aging because of its ability to increase endogenous antioxidant enzymes that suppress ROS induced cellular damage We have shown that after just one round of HBO expression of these protective genes increases significantly and this single treatment protects cells against a ROS insult Overall HBO is a relatively low risk procedure that could be effectively applied as a broader preventative regimen to reduce the effects of aging Ultimately we would like to link these cell culture studies with human studies to demonstrate that HBO induced gene expression changes also occur in patients where they provide a similar level of protection Analysis of the gene array data also show that HBO can stimulate proliferation of HMEC 1 cells c 2010 New York Academy of Sciences Ann N Y Acad Sci 1197 2010 178 183 181
Hyperbaric oxygen and aging Godman et al Figure 3 Validation of gene expression changes at various time points following HBOT qPCR was used to confirm some gene expression changes seen on the microarray In addition to confirmation of changes a time course study was carried out to determine the optimal activation time following HBOT Graphs show relative expression compared to control untreated cells Figure 4 HMEC 1 cells treated with HBOT were resistant to oxidative stress Left panel demonstrates the experimental design The MTS assay revealed an enhancement of cell growth following HBOT Cells also treated with t butyl OOH survived higher concentrations of the oxidant compared to untreated cells right panel 182 c 2010 New York Academy of Sciences Ann N Y Acad Sci 1197 2010 178 183
Godman et al through the activation of growth regulatory genes Endothelial cell proliferation is an important component of angiogenesis and wound healing both of which decline with age Our results also support the idea that HBO is a hormetic agent that activates antioxidant and cytoprotective genes to later protect against a lethal insult Of the hormetic agents that have been proposed for human use as antiaging treatments HBO has the advantages of minimal side effects and a track record of safe FDAapproved use for a variety of indications To be effective this treatment likely depends upon reversal of age related declines in Nrf2 signaling If studies in rats like those described above are applicable to humans HBOT becomes an appealing anti aging therapeutic option for the human population However additional research is required to establish the beneficial effects of HBO in humans and to devise specific clinical protocols that maximize protective responses of this hormetic treatment without risking potential damaging effects of excessive oxygen exposure Hyperbaric oxygen and aging 8 9 10 11 12 Conflicts of interest The authors declare no conflicts of interest References 1 Finkel T N J Holbrook 2000 Oxidants oxidative stress and the biology of ageing Nature 408 239 247 2 Rattan S I 2007 The science of healthy aging genes milieu and chance Ann N Y Acad Sci 1114 1 10 3 Rattan S I et al 2009 Heat stress and hormetin induced hormesis in human cells effects on aging wound healing angiogenesis and differentiation Dose Response 7 90 103 4 Rattan S I H Sejersen R A Fernandes W Luo 2007 Stress mediated hormetic modulation of aging wound healing and angiogenesis in human cells Ann N Y Acad Sci 1119 112 121 5 Radak Z H Y Chung S Goto 2008 Systemic adaptation to oxidative challenge induced by regular exercise Free Radic Biol Med 44 153 159 6 Mattson M P 2008 Dietary factors hormesis and health Ageing Res Rev 7 43 48 7 Colman R J et al 2009 Caloric restriction delays disease 13 14 15 16 17 18 onset and mortality in rhesus monkeys Science 325 201 204 Wu D J R Cypser A I Yashin T E Johnson 2008 The U shaped response of initial mortality in Caenorhabditis elegans to mild heat shock does it explain recent trends in human mortality J Gerontol A Biol Sci Med Sci 63 660 668 Hartwig K et al 2009 Feeding a ROS generator to Caenorhabditis elegans leads to increased expression of small heat shock protein HSP 16 2 and hormesis Genes Nutr 4 59 67 Sanz N C Diez Fernandez D Andres M Cascales 2002 Hepatotoxicity and aging endogenous antioxidant systems in hepatocytes from 2 6 12 18 and 30month old rats following a necrogenic dose of thioacetamide Biochim Biophys Acta 1587 12 20 Shih P H G C Yen 2007 Differential expressions of antioxidant status in aging rats the role of transcriptional factor Nrf2 and MAPK signaling pathway Biogerontology 8 71 80 Suh J H et al 2004 Decline in transcriptional activity of Nrf2 causes age related loss of glutathione synthesis which is reversible with lipoic acid Proc Natl Acad Sci USA 101 3381 3386 Buras J 2000 Basic mechanisms of hyperbaric oxygen in the treatment of ischemia reperfusion injury Int Anesthesiol Clin 38 91 109 Cypser J R T E Johnson 2002 Multiple stressors in Caenorhabditis elegans induce stress hormesis and extended longevity J Gerontol A Biol Sci Med Sci 57 B109 114 Rothfuss A G Speit 2002 Investigations on the mechanism of hyperbaric oxygen HBO induced adaptive protection against oxidative stress Mutat Res 508 157 165 Thom S R et al 1997 Inhibition of human neutrophil beta2 integrin dependent adherence by hyperbaric O2 Am J Physiol 272 C770 C777 Alex J et al 2005 Pretreatment with hyperbaric oxygen and its effect on neuropsychometric dysfunction and systemic inflammatory response after cardiopulmonary bypass a prospective randomized double blind trial J Thorac Cardiovasc Surg 130 1623 1630 Yogaratnam J Z et al 2006 Hyperbaric oxygen a new drug in myocardial revascularization and protection Cardiovasc Revasc Med 7 146 154 c 2010 New York Academy of Sciences Ann N Y Acad Sci 1197 2010 178 183 183
Asadamongkol and Zhang Medical Gas Research 2014 4 7 http www medicalgasresearch com content 4 1 7 MEDICAL GAS RESEARCH REVIEW Open Access The development of hyperbaric oxygen therapy for skin rejuvenation and treatment of photoaging Bralipisut Asadamongkol and John H Zhang Abstract Hyperbaric oxygen therapy HBOT a therapy that have patients breath in pure oxygen in a pressurized chamber has been long used as a treatment for conditions such as decompression sickness and carbon monoxide poisoning Oxygen recently has been found to be an important component in skin rejuvenation treatment of photoaging skin and improvement in skin complexions The interest in the use of HBOT for this purpose is continually growing and becoming more widespread In addition to aging and genetic makeup chronic UV radiation due to everyday exposure especially UV B can greatly increase the rate of wrinkle formation through increasing skin angiogenesis and degradation of extracellular matrix molecules The use of HBOT and hyperoxia conditions has been found to attenuate the formation of wrinkles from UV irradiation It accomplishes the task by possibly inhibiting various processes and pathways involved such as the HIF1 VEGF neutrophil infiltrations and MMP 2 MMP 9 which are directly involved with promoting skin angiogenesis in its active state There are currently medical aesthetic clinics that are using oxygen therapy under high pressure applied directly to skin to reduce visible wrinkles but this procedure is not widespread yet due to more research that needs to be done on this topic However this treatment for wrinkles is definitely growing due to recent studies done showing the effectiveness of oxygen therapy on wrinkles This review article will explore and summarize researches done on possible mechanisms dealing with the use of oxygen therapy for reduction of UVB caused wrinkles its side effects and its possible future improvement and use in medicine Keywords Hyperbaric oxygen therapy Wrinkles Mechanisms Photoaging Angiogenesis UVB Oxygen at standard temperature and pressure is a colorless odorless tasteless gas It can exist in its monatomic state but its preferred state is diatomic O2 It also exists in a triatomic form or more commonly known as ozone and is found in the upper limits of the atmosphere 1 2 Since its discovery oxygen has been used in treating medical conditions The first recorded use of hyperbaric air therapy was in 1662 by Nathaniel Henshaw to treat chronic conditions but it wasn t until the 1920s when Hyperbaric Oxygen Therapy HBOT really received attention and is widely noticed due to previous reports of oxygen toxicity 1 The first HBOT chamber made in the United States was in 1861 in New York but the most well known chamber was built in 1921 in Kansas 1 But due to more Correspondence johnzhang3910 yahoo com Department of Physiology Loma Linda University School of Medicine Loma Linda CA 92350 USA reports of concentrated oxygen toxicity HBO therapy was not fully approved and put into practice until the 1937 by Behnke and Shaw for decompression sickness 2 After the recorded success of HBOT its use as treatments for numerous medical conditions grew and researches on this subject widen as the treatment has shown itself to be promising At present HBOT has grown and became more than just a treatment for decompression sickness Starting from the late 1950s until now HBO is used to treat gangrene stroke post cardiac arrest patients and carbon monoxide poisoning 1 3 Uses of oxygen for rejuvenation Joseph Priestley one of the first discoverers of oxygen once said Who can tell but that in time this pure air may become a fashionable article in luxury It seems that as the world is developing and Joseph Priestley s 2014 Asadamongkol and Zhang licensee BioMed Central Ltd This is an Open Access article distributed under the terms of the Creative Commons Attribution License http creativecommons org licenses by 2 0 which permits unrestricted use distribution and reproduction in any medium provided the original work is properly credited The Creative Commons Public Domain Dedication waiver http creativecommons org publicdomain zero 1 0 applies to the data made available in this article unless otherwise stated
Asadamongkol and Zhang Medical Gas Research 2014 4 7 http www medicalgasresearch com content 4 1 7 prediction about air is becoming a reality 4 As the advancement of industrialization the supply of fresh air is steadily decreasing making good quality of air more and more of a luxury Oxygen bar has become available in some big cities such as Los Angeles and Tokyo to provide people with a supply of pure oxygen for a certain fee These places sell oxygen for recreational uses and different aromas are available for customers to choose from There are many health benefits claims made by those supporters of oxygen bars They claimed that the usage could enhance health by strengthening the immune system reduce stress increase energy and reduce headaches and sinus problems However specific researches on these oxygen bars claimed benefits have not been done Due to the reigning desire in today s society to maintain youthful appearance development of minimally invasive dermatological procedures is progressing to rejuvenate aging face Quite a few of these minimally invasive procedures have been effectively developed such as chemical peels intradermal fillers and botulinum toxins but one not yet fully understood is HBOT 5 6 HBOT as a therapy for aesthetic means is a relatively new use so there have not been a great number of researches done specifically on usage of oxygen therapy on reduction of wrinkles However from the few that has been done positive outcomes were achieved and the use of oxygen therapy for treatment of wrinkles seems an attractive option 7 8 Receiving regular treatments of HBOT is thought to increase skin elasticity and stimulate collagen production leading to reduction of wrinkles and fine lines and improvement in skin texture 9 Many dermatology clinics and even spas have utilized machines that deliver concentrated oxygen to the patient or client to treat age related skin problems Oxygen is used in skin care because it is thought that delivery of natural oxygen increases cell metabolism The use of oxygen therapy as a process of skin rejuvenation and reduction of loss of elasticity leading to formation of lines and wrinkles are becoming increasingly widespread in skin care clinics because of increasing successful results of their usage due to developing technologies However scientific evidences for those claims are waiting to be provided Causes of wrinkle formation Health of skin is related to whole body health because the skin not only acts as a physical barrier against infections from foreign materials but also controls the immune system and produces hormones and neurotransmitters 10 Wrinkles and aesthetic skin problems like blemishes and acne scars are caused by many factors such as aging exposure to the environment especially an overexposure to the sun smoking gender and poor nutrition Wrinkles caused through aging are an intrinsic factor caused aging Page 2 of 6 or genetically programmed aging that happens over time This genetically programmed aging mainly causes a decrease production of fibroblast collagen and elastin which results in skin wrinkling and elasticity loss 11 Smoking causes skin aging and wrinkles because tobacco inhibits production of collagen and increase MMP and elastosis production which degrades matrix proteins important for skin elasticity 12 Gender wise skin of women seems to receive more wrinkles than men due to perhaps the estrogen level in women Estrogen has been found to increase collagen production and skin thickness so as women age with decrease estrogen production wrinkles formation are more prominent in women than men 13 As for dietary intake increasing vitamin C and linoleic acid consumption is associated with slower aging skin while increasing fat and carbohydrates consumption causes faster skin aging 14 UV radiation causes wrinkles and skin damage which are symptoms of cutaneous aging or photoaging 15 Photoaging is characterized by epidermal hyperplasia or atrophy thickening of basement membrane and stratum corneum loss of dermal papillae unusual keratinocytes and melanocytes degradation of extracellular matrix molecules such as damage to collagen fibers excessive deposition of abnormal elastic fibers and increase of glycosaminoglycans Photoaging is also characterized by dryness rough texture abnormal pigmentation thickening of epidermis deep creases and visible wrinkles 16 UV B induces matrix metalloproteinases MMPs which degrades basement membrane and rearranges the extracellular matrix ECM and Type I Collagenase which digest Type I collagen that is important for supporting the skin are also causes of wrinkle formation 17 In addition it has been found that UV radiation can cause cutaneous angiogenesis the formation of new blood vessels from pre existing vessels that can lead to wrinkles formation by inducing the hypoxia inducible factor HIF 1 and up regulation of vascular endothelial growth factor VEGF 18 19 Figure 1 Angiogenesis has been found to be correlated to wrinkling of the skin and can be caused by not only through UV B radiation but also through hypoxic conditions There has been researches done and evidences found of hypoxic conditions leading to wrinkling through angiogenesis by affecting and increasing HIF which regulates the vascular networks 15 VEGF is a major angiogenesis factor and a target gene of HIF protein 20 21 In studies done the level of VEGF has been shown to be up regulated in areas with necrosis and areas under hypoxic conditions 22 24 Mechanisms for HBOT skin rejuvenation HIF 1 As mentioned above UV B radiation can cause angiogenesis through inducing the HIF 1 protein leading to
Asadamongkol and Zhang Medical Gas Research 2014 4 7 http www medicalgasresearch com content 4 1 7 Page 3 of 6 Figure 1 Overview of possible mechanism used by HBOT to attenuate wrinkle formation from exposure to UVB radiation UVB irradiation is shown to upregulate pathways that cause wrinkles such as the HIF 1 neutrophils and angiogenesis pathways Hyperoxic condition is shown to inhibit those pathways activated by UVB which results in decreased wrinkles formation wrinkling of skin There are two subunits to the HIF 1 protein and Of these two the subunit directly involved with hypoxic condition responses is the HIF 1 The mRNA of HIF 1 is normally made in cells In some cells the mRNA level of HIF 1 is increased during hypoxia leading to an increase in transcription of many genes including VEGF But in most cells under hypoxic conditions the mRNA level remains the same but the level of HIF 1 protein increases suggesting that during normal oxygen conditions the HIF 1 protein usually undergoes proteasomal degradation The lower oxygen tension stabilizes the HIF 1 subunit and promotes angiogenesis to compensate for the hypoxic condition 21 25 Since HIF 1 subunits are degraded under normal oxygen levels this suggests that increasing oxygen tension in the epidermal cells through use of oxygen therapy could increase proteasomal degradation of HIF 1 subunit which will decrease angiogenesis and slow down wrinkling of skin The results obtained from studies done by Kawada et al 26 showed that mice that went through UV B radiation but receive HBOT did not have a significant increase in HIF 1 protein level like the mice that received only the UV B irradiation This result supports that higher oxygen level increases HIF 1 protein degradation and suggests that increase oxygen tension can attenuate formation of wrinkles due to decrease in angiogenesis Even though the level of VEGF which is a downstream of the HIF 1 protein was found to be increased in both UVB and UVB HBO group there was a lower tendency to increase in the UVB HBO group Therefore it is possible that hyperoxia attenuates wrinkle formation through suppressing the HIF 1 angiogenesissignaling pathway 26 MMP 2 MMP 9 MMP stands for matrix metalloproteinases and these groups of proteins are zinc dependent proteins involved in remodeling of extracellular matrix and have important roles in angiogenesis morphogenesis and metastasis 27 The protein is made up of several domains mainly propeptide catalytic and hemopexin domains MMPs are also involved in degradation of collagen proteoglycans and many glycoprotein 28 MMPs are secreted as inactive zymogens pro MMP and have to be activated for full functional capacity Growth factors and cytokines are molecules that regulate the stimulation or inhibition of pro MMP synthesis usually at the transcriptional level The MMPs involved with photoaging that have shown to increase in level during experiments with human fibroblasts after UV irradiation are MMP 1 2 3 and 9 17 29 In other studies done on MMPs in epidermis of hairless mouse skin after long period of UV irradiation the levels of MMP 1 and MMP 3 did not have a significant increase However the levels of active MMP 2 and MMP 9 in addition to increase pro MMP 2 and pro MMP 9 levels were found to be significantly higher in the UVB irradiated wrinkled mice skin compared to the unexposed normal mice skin 30 MMP 2
Asadamongkol and Zhang Medical Gas Research 2014 4 7 http www medicalgasresearch com content 4 1 7 and MMP 9 also known as gelatinase A and gelatinase B respectively functions mainly to digest type IV and VII collagens which are major components of the basement membrane Also when a potent synthetic inhibitor of MMP 2 and MMP 9 CGS27023A was applied topically over a period of time significant inhibition of reduction of collagen by UVB radiation was observed and there was no significant difference between collagen levels in non irradiated mice and CGS27023Atreated mice which implies that MMP 2 and MMP 9 are have major roles in inducing skin wrinkles after UVB exposure 30 Even though MMP 2 and MMP 9 have been found to play important roles in inducing skin wrinkles and angiogenesis the results obtained in a study from putting UVB irradiated hairless mice through hyperoxic HO conditions did not show significant reduction in the levels of the MMPs 26 31 The MMP 9 level was found to be the same for UVB and UVB HO group and the MMP 2 level was found to be slightly decreased in both UVB and UVB HO group Because the level of MMP 2 in both the UVB and UVB HO group were found to be reduced whether hyperoxic conditions affect MMP 2 levels remains to be elucidated 26 Perhaps different concentrations of oxygen or different lengths of HBOT exposures need to be adjusted to obtain a more affective result Another study done on retina of mice showed that hypoxic conditions leads to increase MMP 2 level and angiogenesis through p53 affected CTGF CCN2 gene of the cysteine rich protein 61 connective tissue growth factor novel over expressed CCN which are subsets of extracellular matrix proteins Suppression of CTGF gene decreased MMP 2 levels and since CTGF gene is induced in hypoxic conditions hyperoxic conditions could potentially decrease MMP 2 levels and wrinkle formation through inhibition of the CTGF gene 32 Further research could still be done on this subject to find out if and how high oxygen concentration affects MMPs on a molecular level which could lead to explaining in more details HBO s role in wrinkles reduction Inflammatory cells infiltration Inflammatory cells especially neutrophils have the capability to be destructive and can cause damage to the extracellular matrix 33 Health conditions such as emphysema adult respiratory distress syndrome adult periodontitis rheumatoid arthritis ulcerative colitis and blistering skin disorders are mediated by tissue destructive actions of neutrophils 34 36 Neutrophils are the most abundant white blood cell and after a certain level of tissue damage experienced they will quickly leave the blood stream and move towards the site of damage Exposure to certain degree of sunlight and an erythemogenic or Page 4 of 6 erythema causing dose of UVB radiation can lead to influx of neutrophils which cause solar elastosis or break down and loss of elastic tissue 37 38 The destructive abilities of neutrophils come from the fact that it is filled with potent proteolytic enzymes capable of degrading collagen and elastic fibers thus causing damage to the extracellular matrix Neutrophils are able to release a group of serine proteases mainly the neutrophil elastase which is a potent proteolytic enzyme 39 Not much attention has been given to neutrophils regarding its role in causing wrinkles because of more studies explored the hypothesis of MMPs and HIF1 as main causes and also because rate of neutrophil infiltration can only be examined in skin recently exposed to UV radiation 30 40 In a study done by Rijken et al they found evidences that infiltrating neutrophils may be the key players in the release of proteolytic enzymes such as MMPs and neutrophil elastase that causes cutaneous damage and photoaging instead of fibroblasts and keratinocytes being the main molecules releasing the enzymes 41 It has been shown that neutrophils are able to express a few MMPs such as MMP 8 MMP 9 and MMP 12 and in addition the MMP 1 seems co localized with neutrophil elastase after sun exposure 42 43 These evidences show that it is likely that neutrophils are the cause of extracellular matrix damage that can lead to elastosis and formation of wrinkles UVB irradiation can lead to angiogenesis in the skin and these additional blood vessels might possibly be the main cause of the increase in inflammatory cells infiltration which leads to formation of wrinkles Using HBOT to treat skin wrinkles may be effective because it might be able to decrease the amount of inflammatory cells infiltration and neutrophils releasing the MMPs Direct evidence was found and shown that hyperoxic conditions are able to decrease blood flow in active muscle cells and also slow down active angiogenesis in the skin 26 44 Hyperoxia can reduce skin angiogenesis through possibly increasing degradation of the HIF1 protein and with that angiogenesis pathway being inhibited new blood vessels are not being formed and leads to reduction of infiltrating neutrophils which results in attenuating the release of MMPs in the skin However recent studies have suggested that hyperoxic conditions couldn t have only affected degradation of HIF1 and cause reduction of wrinkle formation Evidence was found showing inhibition of HIF1 protein alone was insufficient to restrain wrinkles formation by higher dose of UV radiation that led up to the regulation of the activities of MMPs 45 With conflicting evidences more research needs to be done to find out the specific conditions and mechanism of how hyperoxic condition attenuates skin wrinkle formation
Asadamongkol and Zhang Medical Gas Research 2014 4 7 http www medicalgasresearch com content 4 1 7 Thrombospondin 1 Thrombospondin 1 TSP 1 is a matricellular protein that can inhibit proliferation and migration of endothelial cells but more importantly in this case can effectively diminish angiogenesis 18 Its mRNA is produced by the basal epidermal keratinocyte in human skin and the TSP 1 protein is deposited in the basement membrane area 46 According to studies done by Kiichiro et al the epidermal over expression of TSP 1 inhibits dermal photo damage and also elastic fiber and collagen disorganization which lead to prevention of formation of skin wrinkles They also showed that TSP 1 has a potent ability to inhibit angiogenesis caused by UV B irradiation by decreasing endothelial cell proliferation and increasing its apoptosis rate 18 Mice that received chronic UVB induced skin damage and skin specific overexpression of TSP 1 compared with mice that only receive chronic UVB induced skin damage has greater reduction in skin wrinkling rate associated with the protein s effective inhibition of angiogenesis Recent evidence suggests that the ability of TSP 1 to decrease skin wrinkle not only came from its ability to inhibit angiogenesis but also its ability to inhibit activation of MMP 2 and MMP 9 by inhibiting conversions of MMPs zymogens to its active form In addition to degrading basement membrane and rearranging the extracellular matrix activation of MMP 2 is associated with increased blood vessel growth while inhibition of this protein leads to decreased angiogenesis level TSP 1 interacts with MMP 2 by binding to it which leads to the inhibition of the activity of MMP 2 47 It is also thought that MMP 9 has the ability to accelerate wrinkle formation so its interaction with TSP 1 is tested Results showed that TSP 1 does interact with and inhibits the activity of MMP 9 by binding to it in a similar way that TSP 1 binds to MMP 2 because MMP 2 and MMP 9 has similar structural domains This property of TSP 1 to inhibit MMPs contributes to its anti angiogenic effects and also to its ability to reduce UVB induced skin damage and wrinkles 18 47 Although TSP 1 has inhibitory activities that can inhibit angiogenesis and slow down wrinkle formation and hyperoxia conditions and treatments has inhibitory activity on angiogenesis and MMPs level a direct link between TSP 1 activity and hyperoxic condition has not been made Apparently more research needs to be done to investigate whether high oxygen tension can increase the level of TSP 1 leading to attenuation of skin wrinkles Conclusion The use of HBOT in medicine has come a long way since its first main use to treat decompression sickness In order for the HBOT to be used to its full potential in skin care the exact mechanisms of how high oxygen concentration reduce formation of wrinkles and photoaging Page 5 of 6 needs to be investigated The direct mechanism of how hyperoxic conditions can attenuate formation of wrinkles has not yet been established due to conflicting evidences and a need for further research on the subject The level of HIF 1 protein has shown to be reduced under hyperoxic conditions which suggests that it is degraded under high oxygen concentration and this can inhibit the expression of VEGF and skin angiogenesis Figure 1 However other evidences were found showing that the suppression of HIF1 angiogenesis pathway under hyperoxic conditions alone is not sufficient to attenuate production of MMPs angiogenesis and skin wrinkle formation Though studies have found HBOT to slow down angiogenesis others have found HBOT to be capable of promoting angiogenesis in ulcers and wounds 7 48 More supporting evidence and research is also needed for exactly how high oxygen concentration affects TSP 1 activity and the level of MMP 2 and MMP 9 This is because a direct link between TSP 1 and hyperoxia has not been found and it is not clear yet whether the MMP levels decrease in hyperoxic conditions A wider variety of different testing conditions need to be enforced to figure out the exact mechanisms Even with these missing links the use of high oxygen concentration to reduce the visibility of wrinkles have shown to be promising and effective to a certain degree since this treatment is currently being used and is becoming more widespread in spas and dermatology clinics worldwide Competing interests The authors declare that they have no competing interests Authors contributions BA did the draft of the manuscript and JHZ did the revision Both authors read and approved the final manuscript Acknowledgement This study is partially supported by NIH NS043339 to JHZ Received 2 January 2014 Accepted 20 February 2014 Published 1 April 2014 References 1 Sheridan RL Shank ES Hyperbaric oxygen treatment a brief overview of a controversial topic J Trauma 1999 47 2 426 435 2 Gill AL Bell CN Hyperbaric oxygen its uses mechanisms of action and outcomes QJM 2004 97 7 385 395 3 Edwards ML Hyperbaric oxygen therapy part 2 application in disease J Vet Emerg Crit Care 2010 20 3 289 297 4 Grainge C Breath of life the evolution of oxygen therapy J R Soc Med 2004 97 10 489 493 5 Iannitti T Capone S Palmieri B Short review on face rejuvenation procedures focus on preoperative antiseptic and anesthetic delivery by JetPeel 3 a high pressure oxygen delivery device Minerva Chir 2012 66 3 1 8 6 Ogden S Griffiths TW A review of minimally invasive cosmetic procedures Br J Dermatol 2008 159 5 1036 1050 7 Roth V Herron MS Bueno RA Jr Chambers CB Neumeister MW Stimulating angiogenesis by hyperbaric oxygen in an isolated tissue construct Undersea Hyperb Med 2011 38 6 509 514 8 Fuller AM Giardina C Hightower LE Perdrizet GA Tierney CA Hyperbaric oxygen preconditioning protects skin from UV A damage
Asadamongkol and Zhang Medical Gas Research 2014 4 7 http www medicalgasresearch com content 4 1 7 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 Cell Stress Chaperones 2013 18 1 97 107 doi 10 1007 s12192 012 0362 2 Epub 2012 Aug 3 Ishii Y Miyanaga Y Shimojo H Ushida T Tateishi T Effects of hyperbaric oxygen on procollagen messenger RNA levels and collagen synthesis in the healing of rat tendon laceration Tissue Eng 1999 5 3 279 286 Slominski A Wortsman J Neuroendocrinology of the skin Endocr Rev 2002 23 3 364 McCullough J Kelly K Prevention and treatment of skin aging Ann N Y Acad Sci 2006 1067 323 331 Morita A Tobacco smoke causes premature skin aging J Dermatol Sci 2007 48 3 169 175 Verdier Sevrain S Bonte F Gilchrest B Biology of estrogens in skin implications in skin aging Exp Dermatol 2006 15 2 83 94 Cosgrove M Franco O Granger S Murray P Mayes A Dietary nutrient intakes and skin aging appearance among middle aged American women Am J Clin Nutr 2007 86 4 1225 1231 Chung JH Eun HC Angiogenesis in skin aging and photoaging J Dermatol 2010 299 2 694 701 Gilchrest BA Skin aging and photoaging an overview J Am Acad Dermatol 1989 21 610 613 Herrmann G Wlaschek M Lange TS Prenzel K Goerz G ScharffetterKochanek K UVA irradiation stimulates the synthesis of various matrix metalloproteinases MMP in cultured human fibroblasts Exp Dermatol 1993 2 92 97 Kiichiro Y Hajimu O Detmar M Targeted overexpression of the angiogenesis inhibitor Thrombospondin 1 in the epidermis of transgenic mice prevents ultraviolet B induced angiogenesis and cutaneous photo damage J Invest Dermatol 2002 118 800 805 Tang K Breen EC Wagner H Brutsaert TD Gassmann M Wagner PD HIF and VEGF relationships in response to hypoxia and sciatic nerve stimulation in rat gastrocnemius Respir Physiol Neurobiol 2004 144 71 80 Detmar M The role of VEGF and thrombospondins in skin angiogenesis J Dermatol Sci 2000 24 S78 S84 Maxwell PH Ratcliffe PJ Oxygen sensors and angiogenesis Semin Cell Dev Biol 2002 13 29 37 Detmar M Molecular regulation of angiogenesis in the skin J Invest Dermatol 1996 106 207 208 Knighton DR Hunt TK Scheuenstuhl H Halliday BJ Werb Z Banda MJ Oxygen tension regulates the expression of angiogenesis factor by macrophages Science 1983 221 1283 1285 Shweiki D Itin A Soffer D Keshet E Vascular endothelial growth factor induced by hypoxia may mediate hypoxia initiated angiogenesis Nature 1992 359 843 845 Chen L Gajendrareddy PK DiPietro LA Differential expression of HIF 1 in skin and mucosal wounds J Dent Res 2012 91 9 871 876 Kawada S Ohtani M Ishii N Increased oxygen tension attenuates acute ultraviolet B induced skin angiogenesis and wrinkle formation Am J Physiol Regul Integr Comp Physio 2010 299 2 R694 R701 Birkedal Hansen H Proteolytic remodeling of extracellular matrix Curr Opin Cell Biol 1995 7 728 735 Amano S Ogura Y Akutsu N Matsunaga Y Kadoya K Adachi E Nishiyama T Protective effect of matrix metalloproteinase inhibitors against epidermal basement membrane damage skin equivalents partially mimic photoageing process Br J Dermatol 2005 153 2 37 46 Fisher GJ Datta SC Talwar HS Wang Z Q Varani J Kang S Voorhees JJ Molecular basis of sun induced premature skin ageing and retinoid antagonism Nature 1996 379 335 339 Inomata S Matsunaga Y Amano S Takada K Kobayashi K Tsunenaga M Nishiyama T Kohno Y Fukuda M Possible involvement of gelatinases in basement membrane damage and wrinkle formation in chronically ultraviolet B exposed hairless mouse J Invest Dermatol 2003 120 128 134 Stearns ME Rhim J Wang M Interleukin 10 IL 10 inhibition of primary human prostate cell induced angiogenesis IL 10 stimulation of tissue inhibitor of metalloproteinase 1 and inhibition of matrix metalloproteinase MMP 2 MMP 9 secretion Clin Cancer Res 1999 5 189 Chintala H Liu H Parmar R Kamalska M Kim YJ Lovett D Grant M Chaqour B Connective tissue growth factor regulates retinal neovascularization through p53 protein dependent transactivation of the matrix metalloproteinase MMP 2 gene J Biol Chem 2012 287 40570 40585 Page 6 of 6 33 Rijken F Bruijnzeel PLB The pathogenesis of photoaging the role of neutrophilis and neutrophil derived enzymes J Invest Dermatol Symp Proc 2009 14 67 72 34 Weiss SJ Tissue destruction by neutrophils N Engl J Med 1989 320 365 376 35 Gadek JE Adverse effects of neutrophils on the lung Am J Med 1992 92 27S 31S 36 Golub LM Sorsa T Lee HM Ciancio S Sorbi D Ramamurthy NS Golub LM Sorsa T Lee HM Ciancio S Sorbi D Ramamurthy NS Gruber B Salo T Konttinen YT Doxycycline inhibits neutrophil PMN type matrix metalloproteinases in human adult periodontitis gingiva J Clin Periodontol 1995 22 100 109 37 Rijken F Bruijnzeel PL van Weelden H Kiekens RC Responses of black and white skin to solar simulating radiation differences in DNA photodamage infiltrating neutrophils proteolytic enzymes induced keratinocyte activation and IL 10 expression J Invest Dermatol 2004 122 1448 1455 38 Starcher B Conrad M A role for neutrophil elastase in solar elastosis Ciba Found Symp 1995 192 338 346 39 Travis J Structure function and control of neutrophil proteinases Am J Med 1988 84 37 42 40 Fisher GJ Wang ZQ Datta SC Varani J Kang S Voorhees JJ Pathophysiology of premature skin aging induced by ultraviolet light N Engl J Med 1997 337 1419 1428 41 Rijken F Kiekens RC van den Worm E Lee PL van Weelden H Bruijnzeel PL Pathophysiology of photoaging of human skin focus on neutrophils Photochem Photobiol Sci 2006 5 184 189 42 Ilumets H Rytila P Demedts I Brusselle GG Sovijarvi A Myllarniemi M Ilumets H Rytil P Demedts I Brusselle GG Sovij rvi A Myll rniemi M Sorsa T Kinnula VL Matrix metalloproteinases 8 9 and 12 in smokers and patients with stage 0 COPD Int J Chron Obstruct Pulmon Dis 2007 2 369 379 43 Rijken F Kiekens RC Bruijnzeel PL Skin infiltrating neutrophils following exposure to solar simulated radiation could play an important role in photoageing of human skin Br J Dermatol 2005 152 321 328 44 Welch HG Bonde Petersen F Graham T Klausen K Secher N Effects of hyperoxia on leg blood flow and metabolism during exercise J Appl Physiol 1977 42 385 390 45 Kawada S Ishii N Suppression of UVB induced HIF 1 up regulation by hyperoxia does not prevent wrinkle formation associated with increased MMPs activity in mouse skin Biomed Res 2011 32 363 372 46 Wight TN Raugi GJ Mumby SM Bornstein P Light microscopic immunolocation of thrombospondin in human tissues J Histochem Cytochem 1985 33 295 302 47 Bein K Simons M Thrombospondin type 1 repeats interact with matrix metalloproteinase 2 Regulation of metalloproteinase activity J Biol Chem 2000 275 32167 32173 48 Helmers R Milstein DM van Hulst RA De Lange J Hyperbaric oxygen therapy accelerates vascularization in keratinized oral mucosal surgical flaps Head Neck 2013 doi 10 1002 hed 23437 Epub ahead of print doi 10 1186 2045 9912 4 7 Cite this article as Asadamongkol and Zhang The development of hyperbaric oxygen therapy for skin rejuvenation and treatment of photoaging Medical Gas Research 2014 4 7 Submit your next manuscript to BioMed Central and take full advantage of Convenient online submission Thorough peer review No space constraints or color figure charges Immediate publication on acceptance Inclusion in PubMed CAS Scopus and Google Scholar Research which is freely available for redistribution Submit your manuscript at www biomedcentral com submit
Study finds hyperbaric oxygen treatments reverse aging process 20 November 2020 Sackler School of Medicine and the Sagol School of Neuroscience at TAU and Founder and Director of the Sagol Center of Hyperbaric Medicine at the Shamir Medical Center and Dr Amir Hadanny chief medical research officer of the Sagol Center for Hyperbaric Medicine and Research at the Shamir Medical Center The clinical trial was conducted as part of a comprehensive Israeli research program that targets aging as a reversible condition The paper was published in Aging on November 18 2020 Human chromosomes grey capped by telomeres white Credit PD NASA PD USGOV NASA For many years our team has been engaged in hyperbaric research and therapy treatments based on protocols of exposure to high pressure oxygen at various concentrations inside a pressure chamber Professor Efrati explains Our achievements over the years included the improvement of brain functions damaged by age stroke or brain injury A new study from Tel Aviv University TAU and the Shamir Medical Center in Israel indicates that hyperbaric oxygen treatments HBOT in healthy aging adults can stop the aging of blood cells and reverse the aging process In the biological sense the adults blood cells actually grow younger as the treatments progress In the current study we wished to examine the impact of HBOT on healthy and independent aging adults and to discover whether such treatments can slow down stop or even reverse the normal aging process at the cellular level The researchers exposed 35 healthy individuals aged 64 or over to a series of 60 hyperbaric The researchers found that a unique protocol of sessions over a period of 90 days Each participant treatments with high pressure oxygen in a provided blood samples before during and at the pressure chamber can reverse two major processes associated with aging and its illnesses end of the treatments as well as some time after the series of treatments concluded The the shortening of telomeres protective regions researchers then analyzed various immune cells in located at both ends of every chromosome and the accumulation of old and malfunctioning cells in the blood and compared the results the body Focusing on immune cells containing The findings indicated that the treatments actually DNA obtained from the participants blood the study discovered a lengthening of up to 38 of the reversed the aging process in two of its major aspects The telomeres at the ends of the telomeres as well as a decrease of up to 37 in chromosomes grew longer instead of shorter at a the presence of senescent cells rate of 20 to 38 depending on the cell type and the percentage of senescent cells in the overall cell The study was led by Professor Shai Efrati of the 1 2
population was reduced significantly by 11 37 depending on cell type Today telomere shortening is considered the holy grail of the biology of aging Professor Efrati says Researchers around the world are trying to develop pharmacological and environmental interventions that enable telomere elongation Our HBOT protocol was able to achieve this proving that the aging process can in fact be reversed at the basic cellular molecular level Until now interventions such as lifestyle modifications and intense exercise were shown to have some inhibiting effect on telomere shortening Dr Hadanny adds But in our study only three months of HBOT were able to elongate telomeres at rates far beyond any currently available interventions or lifestyle modifications With this pioneering study we have opened a door for further research on the cellular impact of HBOT and its potential for reversing the aging process More information Yafit Hachmo et al Hyperbaric oxygen therapy increases telomere length and decreases immunosenescence in isolated blood cells a prospective trial Aging 2020 DOI 10 18632 aging 202188 Provided by Tel Aviv University APA citation Study finds hyperbaric oxygen treatments reverse aging process 2020 November 20 retrieved 21 January 2022 from https medicalxpress com news 2020 11 hyperbaric oxygen treatmentsreverse aging html This document is subject to copyright Apart from any fair dealing for the purpose of private study or research no part may be reproduced without the written permission The content is provided for information purposes only 2 2 Powered by TCPDF www tcpdf org
www aging us com AGING 2020 Vol 12 No 13 Research Paper Cognitive enhancement of healthy older adults using hyperbaric oxygen a randomized controlled trial Hadanny Amir1 2 3 Daniel Kotovsky Malka1 Suzin Gil1 Boussi Gross Rahav1 Catalogna Merav1 Dagan Kobi1 Hachmo Yafit5 Abu Hamed Ramzia1 Sasson Efrat1 Fishlev Gregory1 Lang Erez1 Polak Nir1 Doenyas Keren1 Friedman Mony1 Tal Sigal4 Zemel Yonatan1 Bechor Yair1 Efrati Shai1 2 5 6 1 The Sagol Center for Hyperbaric Medicine and Research Shamir Assaf Harofeh Medical Center Zerifin Israel Sackler School of Medicine Tel Aviv University Tel Aviv Israel 3 The Mina and Everard Goodman Faculty of Life Sciences Bar Ilan University Ramat Gan Israel 4 Radiology Department Shamir Medical Center Zerifin Israel 5 Research and Development Unit Shamir Medical Center Zerifin Israel 6 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel 2 Correspondence to Amir Hadanny Shai Efrati email amir had gmail com efratishai outlook com Keywords aging cognitive hyperbaric oxygen perfusion cerebral blood flow Received May 6 2020 Accepted June 9 2020 Published June 26 2020 Copyright Amir et al This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY 3 0 which permits unrestricted use distribution and reproduction in any medium provided the original author and source are credited ABSTRACT More than half of community dwelling individuals sixty years and older express concern about declining cognitive abilities The current aim was to evaluate hyperbaric oxygen therapy HBOT effect on cognitive functions in healthy aging adults A randomized controlled clinical trial randomized 63 healthy adults 64 either to HBOT n 33 or control arms n 30 for three months Primary endpoint included the general cognitive function measured post intervention control Cerebral blood flow CBF was evaluated by perfusion magnetic resonance imaging There was a significant group by time interaction in global cognitive function post HBOT compared to control p 0 0017 The most striking improvements were in attention net effect size 0 745 and information processing speed net effect size 0 788 Voxel based analysis showed significant cerebral blood flow increases in the HBOT group compared to the control group in the right superior medial frontal gyrus BA10 right and left supplementary motor area BA6 right middle frontal gyrus BA6 left middle frontal gyrus BA9 left superior frontal gyrus BA8 and the right superior parietal gyrus BA7 In this study HBOT was shown to induce cognitive enhancements in healthy aging adults via mechanisms involving regional changes in CBF The main improvements include attention information processing speed and executive functions which normally decline with aging INTRODUCTION More than half of community dwelling individuals sixty years and older express concern about declining cognitive abilities 1 Besides common pathological declines such as in Alzheimer s dementia and mild cog www aging us com 13740 nitive impairments normal cognitive aging is part of the normal aging process Processing speed conceptual reasoning memory and problem solving activities are the main domains which decline gradually over time 2 Cerebrovascular dysfunction is an additional distinctive feature of aging that includes endothelial dependent AGING
vasodilatation and regional decreases in cerebral blood flow CBF 3 4 Although not associated with a specific pathology reduced regional CBF is associated with impaired cognitive functions 5 6 A growing body of research suggests several methods for cognitive enhancement and for improving the quality of life in both healthy and pathological states Non pharmacological lifestyle interventions including exercise healthy diets and cognitive training have shown positive effects if intensively performed 7 8 Unfortunately so far pharmacological interventions did not show significant improvements in cognitive performance in normal aging and have significant risks for side effects 9 Hyperbaric oxygen therapy HBOT utilizes 100 oxygen in an environmental pressure higher than one absolute atmospheres ATA to enhance the amount Repeated intermittent hyperoxic exposures has been shown to induce physiological effects which normally occur during hypoxia in a hyperoxic environment including stem cells proliferation and generation of new blood vessels angiogenesis 10 13 Angiogenesis is induced mainly in brain regions signaling ischemia or metabolic dysfunction 13 15 In turn neovascularization can enhance cerebral blood flow 14 and consequently improve the metabolic activity 13 15 There is growing evidence from clinical studies that HBOT utilized in a repeated daily sessions protocol has neurotherapeutic effects which can improve cognitive functions in post stroke traumatic brain injury and anoxic brain damaged patients even years after the acute insult 15 19 However no study to date has examined populations The aim of the current study was to evaluate whether HBOT affects cognitive function and brain perfusion in normal non pathological aging adults RESULTS Out of 100 individuals that were contacted for participation 70 were eligible and signed an informed consent Seven patients did not complete baseline assessments and were excluded All 63 patients who completed baseline evaluations completed interventions One patient did not complete the cognitive assessment post HBOT and excluded from analysis Figure 1 The baseline characteristics and comparability of the cohort are provided in Table 1 The HBOT arm patients were Figure 1 Participants flowchart www aging us com 13741 AGING
Table 1 Baseline characteristics Total N Age years Males Right dominance Life partner Education years Working Family history Cognitive decline Cancer Ischemic heart disease Chronic medical conditions Atrial fibrillation Hypothyroidism Obstructive sleep apnea Asthma Benign prostatic hyperplasia Gastroesophageal reflux disease Osteoporosis Rheumatic arthritis Osteoarthritis Diabetes mellitus Hypertension Dyslipidemia Ischemic heart disease History of smoking Smoking pack years Quit smoking years Chronic medications Anti aggregation ACE Inhibitors ARB blockers Beta blockers Calcium blockers Alpha blockers Diuretics Statins Oral hypoglycemic Bisphosphonates Proton pump inhibitors Hormones PDE5 Inhibitors Benzodiazepines SSRI www aging us com 13742 Control HBOT P value 63 100 33 52 3 30 47 7 69 70 3 59 68 81 3 34 70 68 3 64 0 041 39 61 9 23 69 7 16 53 3 0 182 57 90 5 2 6 1 4 13 3 0 326 55 87 3 29 87 9 26 86 7 0 885 15 23 2 81 15 03 2 87 15 45 2 78 0 564 29 46 16 48 5 13 43 3 0 682 23 36 5 8 24 2 15 50 0 034 31 49 2 16 48 5 15 50 12 19 4 12 1 8 26 7 0 202 4 6 3 0 4 13 3 0 046 7 11 1 3 9 1 4 13 3 0 593 3 4 8 0 3 10 0 102 3 4 8 2 6 1 1 3 3 1 14 22 2 7 23 3 7 21 2 0 842 5 7 9 2 6 1 3 10 0 662 10 15 9 5 15 2 5 16 7 0 869 4 6 3 3 9 1 1 3 3 0 614 11 17 5 4 12 1 7 23 3 0 325 10 15 9 7 21 2 3 10 0 308 14 22 7 21 2 7 23 3 0 84 30 47 6 14 42 4 16 53 3 0 387 6 9 5 4 12 1 2 6 7 0 674 24 38 1 14 42 4 10 33 3 0 458 22 38 13 33 21 21 10 75 24 0 16 79 0 625 23 96 12 36 23 71 11 86 24 3 13 68 0 912 14 22 2 6 18 2 8 26 7 0 418 14 22 2 8 24 2 6 20 0 686 11 17 5 6 18 2 5 16 7 0 874 6 9 5 3 9 1 3 10 1 13 20 6 6 18 2 7 23 3 0 614 3 4 8 1 3 2 6 7 0 601 19 30 2 9 27 3 10 33 3 0 601 5 7 9 4 12 1 1 3 3 0 357 4 6 3 3 9 1 1 3 3 0 614 7 11 1 4 12 1 3 10 1 4 6 3 1 3 3 10 0 343 11 17 5 7 21 2 4 13 3 0 515 9 14 3 6 18 2 3 10 0 479 8 12 7 3 9 1 5 16 7 0 462 AGING
slightly older 70 7 3 6 compared to 68 8 3 3 and apart from a higher rate of atrial fibrillation in the HBOT arm 4 patients 13 3 vs no patients 0 there were no other significant differences between the two groups Table 1 RAVLT total net effect size 0 603 F 5 439 p 0 02 improved in the HBOT group compared to the control group However they were statically insignificant following multiple comparisons corrections Table 2 3 See all cognitive results in Supplementary Tables 1 2 Cognitive function Brain perfusion Results of the cognitive function evaluations are summarized in Tables 2 3 Ten subjects were excluded due to excessive head motion 1mm or 1 and ten subjects were excluded due to low AIF peak or wide AIF A total of 20 subjects from the control group and 19 subjects from the HBOT group were included in the analysis Primary endpoint Both groups had similar global cognitive scores at baseline which was higher than the average score normalized to age and education level 100 There was a significant group by time interaction in the primary endpoint of global cognitive function post HBOT compared to the control group F 10 811 p 0 0017 with a net effect size of 0 849 Tables 2 3 and Figure 2 Secondary endpoints Both groups had similar cognitive scores in all domains measured by Neurotrax at baseline The most striking improvements were in attention net effect size 0 745 F 8 445 p 0 005 and information processing speed net effect size 0 788 F 9 142 p 0 003 Figure 2 Both overall memory domain score the immediate and the delayed nonverbal memory scores were all improved post HBOT compared to the control group Tables 2 3 and Figure 2 However they were statistically insignificant following multi comparisons corrections In the CANTAB battery at baseline the HBOT group had shorter response times However they were insignificant following multiple comparison corrections Table 2 The HBOT group showed significant improvement in the set shifting task performance a subset of executive function Tables 2 3 and Figure 3 There was a significant reduction in median response time in both congruent net effect size 0 861 F 10 702 p 0 002 and incongruent trials net effect size 0 840 F 11 254 p 0 001 following HBOT Tables 2 3 and Figure 3 There was an increased performance in the visual memory task postHBOT which was statistically insignificant following multiple comparisons corrections The results of covariate adjusted age and education analyses were similar In the traditional paper and pencil tasks at baseline both groups showed similar cognitive functions in all tasks Both verbal fluency FAS semantic net effect size 0 566 F 4 646 p 0 03 and verbal memory www aging us com 13743 There was an insignificant increase in whole brain CBF p 0 054 and whole grey matter CBF p 0 057 and no significant group by time interaction in whole brain grey matter and white matter CBF p 0 05 Supplementary Table 3 Voxel based analysis revealed significant CBF increases in the HBOT group compared to the control group in the following regions right superior medial frontal gyrus BA 10 right and left supplementary motor area BA 6 right middle frontal gyrus BA 6 left middle frontal gyrus BA9 left superior frontal gyrus BA8 and the right superior parietal gyrus BA 7 Table 4 and Figure 4 There were moderate correlations between cognitive score changes and these regional perfusion changes The Neurotrax memory score change correlated to the left middle frontal gyrus CBF change BA8 r 0 379 p 0 023 and the attention score change correlated to the right middle frontal gyrus BA6 r 0 339 p 0 043 CANTAB set switching parameter changes correlated with the right superior frontal gyrus and supplementary motor area BA6 r 0 38 0 45 p75 in both groups There was a compared to none in the control group Supplementary Tables 5 6 AGING
Table 2 Neurocognitive performance changes Control Group Baseline Control HBOT Group 3 months P value Baseline N 32 Neurotrax Post HBOT 3 months P value Baseline Comparison P value Net Effect Size N 29 Primary Endpoint Global cognitive score
Table 3 Neurocognitive function repeated measures analysis F p value F p value Interaction Effect Group_by_Time F p value 7 171 0 009 34 382
the particular subset of set shifting improved significantly following HBOT compared to actual deterioration in the control group These domains are known to gradually decline within the process of normal aging and play a crucial role in the daily functioning of the elderly 2 Our results were in participants that had neither previous brain pathologies nor pathological cognitive declines such as dementia or mild cognitive impairment and had normal baseline cognitive scores The memory domain and mainly the non verbal subdomain improved in the HBOT group compared to no change in the control group However these changes did not reach corrected significance We cannot rule out the possibility that in larger sample sizes the memory domain effect would remain significant even after multi comparisons corrections Interestingly the most significant cognitive changes were found in the computerized cognitive batteries and not in the traditional psychometric pen and paper tools This may be due to the lack of proper alternative variations for the traditional tasks and low test retest validity 20 The HBOT net effect size of global cognitive score enhancement was 0 849 following 12 weeks HBOT sessions substantially more than in other enhancement modalities Colcombe et al in a meta analysis found that aerobic training in older adults improves mostly Figure 2 NeuroTrax parameters significant changes The NeuroTrax significant domains shown in boxplots with each line representing a patient flow from baseline to post intervention The central mark indicates the median and the bottom and top edges of the box indicate the 25th and 75th percentiles respectively Red symbols indicate outliers www aging us com 13746 AGING
executive function task switching followed by improvements in spatial and speed and an overall improvement with an effect size of d 0 47 21 Recently a randomized controlled trial showed only the executive function moderately improving following aerobic training d 0 36 with no significant changes in memory language and verbal fluency domains d 0 120 15 8 In contrast our study shows that HBOT has a significant large net effect size of 0 84 0 86 in the global cognitive score task switching as well as a significant net effect size in verbal fluency attention and information processing speed brain activation 22 26 In a recent study multitasking was significantly enhanced during hyperbaric oxygen exposure 27 Yu et al recently showed that five hyperbaric sessions enhance healthy young adults spatial memory correlated with increased functional connectivity in the hippocampus inferior frontal gyrus and lingual gyrus 28 However these changes were evaluated the day after the last hyperbaric session In comparison our intervention included 60 sessions within three months and to exclude transient effects of oxygen all measurements were performed at least one week after the last hyperbaric session Previous studies have demonstrated a single oxygen exposure can enhance the cognitive function such as verbal function visuospatial function through increased The current study HBOT protocol utilized the effects induced by repeated intermittent hyperoxic exposures the so called hyperoxic hypoxic paradox 10 These Figure 3 CANTAB parameters significant changes The set shifting parameters shown in boxplots with each line representing a patient flow from baseline to post intervention The central mark indicates the median and the bottom and top edges of the box indicate the 25th and 75th percentiles respectively Red symbols indicate outlie www aging us com 13747 AGING
Table 4 Brain regions with significant perfusion increases Anatomical location BA Right superior medial frontal gyrus Right supplementary motor area Left supplementary motor area Right middle frontal gyrus Right middle frontal gyrus Left middle frontal gyrus Left middle frontal gyrus Right superior frontal gyrus Right superior parietal gyrus Right superior parietal gyrus 6 6 6 6 6 9 8 10 7 7 X 10 8 14 38 38 38 26 18 48 24 Coordinates Y 30 24 0 12 4 22 32 68 18 62 Z 64 70 78 60 82 52 56 8 38 60 t value 4 63 3 72 3 92 4 56 3 8 4 52 4 13 4 04 4 41 4 21 The tables report each brain region which was found significant in a time by group repeated measures ANOVA comparing the two groups The results are showing in specific Montreal Neurological Institute MNI coordinates X sagittal Y coronal Z axial refers to Montreal Neurological Institute BA Brodmann area All coordinates emerged at a threshold of P 0 05 corrected minimum cluster size 25 200 mm3 intermittent hyperoxic exposures induce many of the physiological responses that occur during hypoxia 10 HBOT induces the release of the transcription factors called hypoxic induced factor HIF and increases their stability and activity 11 In turn HIF and HIF 2 modulate the release of the angiogenic factor vascular endothelial growth factor VEGF 29 30 VEGF is considered the master regulator of angiogenesis and induces migration of progenitor endothelial cells from the bone marrow into the circulatory system recruitment of endothelial cells from existing blood vessels and the differentiation into new formed blood vessels 31 Importantly the migration of these circulating angiogenic cells targets sites of ischemia where they promote vascular remodeling and stimulate angiogenesis 32 As seen in ischemic brain injuries neovascularization increases regional cerebral blood flow 14 31 33 34 We suggest that repeated oxygen level fluctuations may improve regional CBF and cognitive functions in healthy elderly Our protocol included 60 sessions of 100 oxygen at 2 ATA including 3 air breaks during each session in order to utilize the hyperoxic hypoxic paradox and minimize the risk for oxygen toxicity However the dose response curve related to the applied pressure time Figure 4 Brain regions with significant post hyperbaric oxygen therapy changes in cerebral blood flow www aging us com 13748 AGING
and number of HBOT exposures and its relation to HIF expression and its related regenerative effects are still not fully understood and further studies are needed to find the optimal HBOT protocols The significant improvement in CBF induced by HBOT in the current study population was in certain cortical regions This finding is in agreement with the work by Martin et al which demonstrated age related functional decline is related to reduced perfusion in specific cortical locations rather and not the global CBF but rather in the cortical regions that are the most sensitive for the age related functional decline 4 Recently another study confirmed the selective age related reductions in cortical perfusion 35 Following HBOT the increase in the CBF was in specific regions which participate in the following cognitive roles Superior medial frontal gyrus SFG BA 10 is thought to contribute to higher cognitive functions and has mostly been associated multitasking attention social cognition and episodic memory 36 37 Middle frontal gyrus MFG has been proposed as a site of convergence of the dorsal and ventral attention networks The MFG serves as a gateway to interrupt ongoing endogenous attentional processes in the dorsal attention network and reorient attention to an exogenous stimulus 38 39 Premotor cortex BA6 The premotor area and supplementary motor area SMA functions include motor sequencing and planning movements It has been shown that area 6 participates in memory attention and executive function as well as updating verbal function and updating spatial information 40 Superior frontal gyrus BA8 traditionally this area has been regarded as the frontal eye field However functional studies have shown significant participation of this area in executive function including reasoning and planning working memory and attention 41 43 Superior parietal lobule BA7 also referred as the somatosensory association cortex together with BA5 is believed to play a role in visuo motor coordination and attention In addition it seems to participate in semantic categorization tasks and temporal context recognition 44 Study limitations The current study has several limitations and strengths to consider First the limited sample size has to be taken into account possibly causing decreased sensitivity and false negative changes However the presence of www aging us com 13749 significant changes following strict statistical analyses in a small group is indicative for the relatively high potency of the intervention Second the control group was a nonintervention rather than a sham intervention Although the outcome assessors were blinded the participants were unblinded Third the duration of the effect is yet to be determined in long term follow ups Nevertheless several strengths should be stressed The isolated HBOT effect was measured as both groups were monitored for any lifestyle changes such as nutrition and exercise medications or any other intervention that may have acted as possible confounders Patients did not perform any cognitive training tasks during the trial thereby excluding training effects Both computerized cognitive batteries had alternate forms with test retest validity as well as the brain perfusion sequence and analysis Moreover the improvements in the cognitive domains correlated with the significant changes in perfusion MRIs In summary the study indicates that HBOT can induce cognitive enhancement in healthy aging populations The main improvements include attention information processing speed and executive functions which are known to decline with normal aging In correlation with the cognitive improvements HBOT induced a significant brain perfusion increase in specific brain regions with high cognitive roles MATERIALS AND METHODS Subjects Seventy adults without pathological cognitive declines aged 64 and older who lived independently in good functional and cognitive status were enrolled The study was performed between 2016 2020 in the Shamir AssafHarofeh Medical Center Israel Included patients did not have cardiac or cerebrovascular ischemia histories for the last year prior to inclusion Exclusion criteria included previous treatment with HBOT for any reason during the last three months any history of malignancy during the last year any pathological cognitive decline severe chronic renal failure GFR 8 fasting glucose 200 immunosuppressants MRI contraindications active smoking and pulmonary diseases Included patients who were diagnosed with pathological cognitive decline based on their cognitive tests were excluded Pathological cognitive decline was diagnosed by a certified neuropsychologist Study design The study protocol was approved by Institutional Review Board of Shamir medical center Israel The AGING
study was performed as a randomized prospective controlled clinical trial After signing an informed consent the subjects were assigned either to HBOT or control no intervention arms Assessors were Measurement points were evaluated at baseline and 1 2 weeks after the HBOT or control period Interventions The HBOT protocol was administrated in a multiplace Starmed 2700 chamber HAUX Germany The protocol comprised of 60 daily sessions 5 sessions per week within a three month period Each session included breathing 100 oxygen by mask at 2ATA for 90 minutes with 5 minute air breaks every 20 minutes Compression decompression rates were 1 meter minute The control arm received no active intervention as a no contact group During the trial neither lifestyle and diet changes nor medications adjustments were allowed for either group Cognitive measures Cognitive functions were assessed using two computerized batteries and one traditional paper based battery given by a certified neuropsychologist NeuroTrax computerized cognitive testing battery NeuroTrax Corporation Bellaire TX The NeuroTrax system and a detailed description of the tests included were detailed in previous publications 45 47 and are also available on the NeuroTrax website http www neurotrax com In brief the NeuroTrax tests evaluate multiple aspects of brain cognitive functions including memory executive function EF attention information processing speed IPS motor skills MS visuospatial skills VS and verbal function VF Cognitive domain scores were normalized for age gender and educationspecific levels The participants completed validated alternate test forms of the NeuroTrax test battery at baseline and post HBOT to allow for iterative administrations with minimal learning effects Test retest reliability of the tests were found to be high in both normal and injured populations without significant learning effects except in the VF and VS domains that were not evaluated in the current study 48 49 CANTAB computerized cognitive tests Cambridge cognition England 50 CANTAB is a semiautomated test battery which can be administered on a handheld tablet The battery included attention switching tasks www aging us com 13750 AST for executive function and set shifting testing pair associates learning PAL for evaluating visual memory and new learning reaction time RTI rapid visual information processing RVP for assessing sustained attention spatial span SSP for assessing visuospatial working memory and spatial working memory SWM 51 52 To combine accuracy and reaction time the inverse efficiency score IES was calculated by the following formula IES response time 1 percentage of errors Notably the patients were given different test versions of the CANTAB test battery at baseline and after the control HBOT period to allow repeated administrations with minimal learning effects The current version of CANTAB has no population norms for either parameter Traditional paper and pencil based neuropsychological tests included the Rey Osterrieth complex figure test ROCFT a popular measure of visuoconstructive skills and visual memory 53 the Rey auditory verbal learning test RAVLT a neuropsychological assessment designed to evaluate verbal memory in patients 54 the digit symbol substitution test DSST offers high sensitivity to detect overall cognitive impairment rather than a specific domain 55 a digit span DS task used to measure working memory s number storage capacity 56 the five points test 5PT is a structured and standardized test that assesses figural fluency functions which are associated with executive functioning 57 the trails making test TMT a widely used test that assesses organized visual search planning attention set shifting cognitive flexibility and divided attention all capacities thought to be executive in nature 58 the FAS test which measures phonemic word fluency which is a type of verbal fluency 59 the bells test a cancellation test which permits qualitative and quantitative evaluation of visual neglect 60 Scores were normalized to age gender and education as suggested in the manuals and presented as Z scores In case of diagnosed pathological cognitive decline using both the cognitive scores and MMSE the patients were excluded from the study Brain MRIs MRI scans were performed on a MAGNETOM Skyra 3T scanner configured with20 channel receiver head coils Siemens Healthcare Erlangen Germany The MRI protocol included dynamic susceptibility contrast DSC and post contrast high resolution MPRAGE 3D T1 weighted images AGING
MRI sequences parameters ophthalmologist before and after the control HBOT term to monitor visual acuity and cataracts DSC Fifty T2 weighted gradient echo echo planar imaging EPI volumes were acquired two repetitions before a bolus injection of gadolinium DTPA GdDTPA 0 2 ml kg administered at 5 ml sec 48 repetitions after injection of Gd DTPA Sequence parameters TR 2 300 ms TE 40ms flip angle 30 voxel size 1 8 x1 8 matrix 128x128 number of slices 25 and slice thickness 3 9 mm MPRAGE 3D was acquired in sagittal orientation with 0 9 mm isotropic resolution Sequence parameters TR 2 000 ms TE 2 41 ms flip angle 8 TI 928 ms FOV 245 x 245 and 192 contiguous slices DSC MRI analysis The preprocessing of the perfusion MRI data was preformed using the SPM software version 12 UCL London UK and included motion correction and coregistration with MPRAGE T1 images Individual gray matter GM and white matter WM segmentation of T1 anatomy was also performed to extract mean perfusion values Whole brain quantitative perfusion analysis was performed as described in previous studies 61 62 Detailed description is found in the supplementary material SI 1 Briefly MR signal intensity was converted to Gd concentrations AIF was determined automatically fitted to the gamma variate function and deconvolved on a voxel by voxel basis to calculate the CBF CBV and MTT maps Following normalization to MNI space WM and GM masking and smoothing using a 6 mm full width at half maximum Gaussian kernel statistical analysis was performed on the normalized CBF maps using the voxel based method Quality of life measures The RAND health status survey short form 36 SF 36 was used to assess quality of life SF 36 is a self report measure that evaluates physical functioning bodily pain role limitations due to physical health problems role limitations due to personal or emotional health general mental health social functioning energy fatigue and general health perception 63 65 Each scale generates a score from 0 to 100 with a high score indicating better health and less body pain Safety Participants were monitored for adverse events including barotraumas either ear or sinuses oxygen toxicity pulmonary and central nervous system Participants were examined by a certified blinded www aging us com 13751 Statistical analysis Continuous data were expressed as means standarddeviation The normal distribution for all variables was tested using the Kolmogorov Smirnov test unpaired and paired t tests were performed to compare variables between and within the two groups Net effect sizes were evaluated using Cohen s d method Continuous parameters correlations were performed using Pearson and Spearman s as appropriate Categorical data is expressed in numbers and percentages and compared by chi square tests Univariate analyses were performed using Chiidentify significant variables P
AUTHOR CONTRIBUTIONS All authors contributed substantially to the preparation of this manuscript HA ES were responsible for protocol design HA ZY BY ES DKM were responsible for patients recruitment HA DKM SG BGR DG HY AHR FG LE PN DK FM TS ZY BY were responsible for data acquisition HA CM SE and ES were responsible for data analysis All authors interpreted the data HA CM ES and ES wrote the manuscript All authors revised and finalized the manuscript 2016 283 353 64 https doi org 10 1016 j expneurol 2016 07 006 PMID 27421879 6 Berman RF Goldman H Altman HJ Age related changes in regional cerebral blood flow and behavior in sprague dawley rats Neurobiol Aging 1988 9 691 96 https doi org 10 1016 s0197 4580 88 80134 9 PMID 3062475 7 Klimova B Valis M Kuca K Cognitive decline in normal aging and its prevention a review on nonpharmacological lifestyle strategies Clin Interv Aging 2017 12 903 10 https doi org 10 2147 CIA S132963 PMID 28579767 8 Blumenthal JA Smith PJ Mabe S Hinderliter A Lin PH Liao L Welsh Bohmer KA Browndyke JN Kraus WE Doraiswamy PM Burke JR Sherwood A Lifestyle and neurocognition in older adults with cognitive impairments a randomized trial Neurology 2019 92 e212 23 https doi org 10 1212 WNL 0000000000006784 PMID 30568005 9 Fink HA Jutkowitz E McCarten JR Hemmy LS Butler M Davila H Ratner E Calvert C Barclay TR Brasure M Nelson VA Kane RL Pharmacologic interventions to prevent cognitive decline mild cognitive impairment and clinical alzheimer type dementia a systematic review Ann Intern Med 2018 168 39 51 https doi org 10 7326 M17 1529 PMID 29255847 ACKNOWLEDGMENTS We would like to thank Dr Mechael Kanovsky for his editing of this manuscript CONFLICTS OF INTEREST AH ES RBG SG BY ZY work for AVIV Scientific LTD ES is a shareholder at AVIV Scientific LTD FUNDING The study was funded by a research grant from the Sagol Network for Neuroscience established by Mr Sami Sagol REFERENCES 1 2 3 Cedres N Machado A Molina Y Diaz Galvan P Hern ndez Cabrera JA Barroso J Westman E Ferreira D Subjective cognitive decline below and above the age of 60 a multivariate study on neuroimaging cognitive clinical and demographic measures J Alzheimers Dis 2019 68 295 309 https doi org 10 3233 JAD 180720 PMID 30741680 Harada CN Natelson Love MC Triebel KL Normal cognitive aging Clin Geriatr Med 2013 29 737 52 https doi org 10 1016 j cger 2013 07 002 PMID 24094294 Zlokovic BV Neurovascular pathways to disorders Nat Rev Neurosci 2011 12 723 38 https doi org 10 1038 nrn3114 PMID 22048062 4 Martin AJ Friston KJ Colebatch JG Frackowiak RS Decreases in regional cerebral blood flow with normal aging J Cereb Blood Flow Metab 1991 11 684 89 https doi org 10 1038 jcbfm 1991 121 PMID 2050757 5 Wang L Du Y Wang K Xu G Luo S He G Chronic cerebral hypoperfusion induces memory deficits and www aging us com 13752 10 Cimino F Balestra C Germonpr P De Bels D Tillmans F Saija A Speciale A Virgili F Pulsed high oxygen induces a hypoxic like response in human umbilical endothelial cells and in humans J Appl Physiol 1985 2012 113 1684 89 https doi org 10 1152 japplphysiol 00922 2012 PMID 23042909 11 Sunkari VG Lind F Botusan IR Kashif A Liu ZJ Yl Herttuala S Brismar K Velazquez O Catrina SB Hyperbaric oxygen therapy activates hypoxia inducible factor 1 HIF 1 which contributes to improved wound healing in diabetic mice Wound Repair Regen 2015 23 98 103 https doi org 10 1111 wrr 12253 PMID 25532619 12 Milovanova TN Bhopale VM Sorokina EM Moore JS Hunt TK Hauer Jensen M Velazquez OC Thom SR Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo J Appl Physiol 1985 2009 106 711 28 https doi org 10 1152 japplphysiol 91054 2008 PMID 19023021 AGING
13 Yang Y Wei H Zhou X Zhang F Wang C Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor extracellular signal regulated kinase signaling after traumatic brain injury Neuroreport 2017 28 1232 1238 https doi org 10 1097 WNR 0000000000000901 PMID 28953090 https doi org 10 3389 fpsyg 2019 02327 PMID 31681117 21 Colcombe S Kramer AF Fitness effects on the cognitive function of older adults a meta analytic study Psychol Sci 2003 14 125 30 https doi org 10 1111 1467 9280 t01 1 01430 PMID 12661673 14 Liman TG Endres M New vessels after stroke postischemic neovascularization and regeneration Cerebrovasc Dis 2012 33 492 99 https doi org 10 1159 000337155 PMID 22517438 22 Chung SC Tack GR Lee B Eom GM Lee SY Sohn JH The effect of 30 oxygen on visuospatial performance and brain activation an fMRI study Brain Cogn 2004 56 279 85 https doi org 10 1016 j bandc 2004 07 005 PMID 15522765 15 Efrati S Fishlev G Bechor Y Volkov O Bergan J Kliakhandler K Kamiager I Gal N Friedman M BenJacob E Golan H Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS One 2013 8 e53716 https doi org 10 1371 journal pone 0053716 PMID 23335971 23 Chung SC Sohn JH Lee B Tack GR Yi JH You JH Jun JH Sparacio R The effect of transient increase in oxygen level on brain activation and verbal performance Int J Psychophysiol 2006 62 103 08 https doi org 10 1016 j ijpsycho 2006 02 006 PMID 16678926 16 Boussi Gross R Golan H Fishlev G Bechor Y Volkov O Bergan J Friedman M Hoofien D Shlamkovitch N Ben Jacob E Efrati S Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS One 2013 8 e79995 https doi org 10 1371 journal pone 0079995 PMID 24260334 17 Boussi Gross R Golan H Volkov O Bechor Y Hoofien D Beeri MS Ben Jacob E Efrati S Improvement of memory impairments in poststroke patients by hyperbaric oxygen therapy Neuropsychology 2015 29 610 21 https doi org 10 1037 neu0000149 PMID 25384125 18 Hadanny A Golan H Fishlev G Bechor Y Volkov O Suzin G Ben Jacob E Efrati S Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restor Neurol Neurosci 2015 33 471 86 https doi org 10 3233 RNN 150517 PMID 26409406 19 Hadanny A Abbott S Suzin G Bechor Y Efrati S Effect of hyperbaric oxygen therapy on chronic neurocognitive deficits of post traumatic brain injury patients retrospective analysis BMJ Open 2018 8 e023387 https doi org 10 1136 bmjopen 2018 023387 PMID 30269074 20 Bj rngrim S van den Hurk W Betancort M Machado A Lindau M Comparing traditional and digitized cognitive tests used in standard clinical evaluation a study of the digital application minnemera Front Psychol 2019 10 2327 www aging us com 13753 24 Sohn JH Chung SC Jang EH 30 oxygen inhalation enhances cognitive performance through robust activation in the brain J Physiol Anthropol Appl Human Sci 2005 24 51 53 https doi org 10 2114 jpa 24 51 PMID 15684544 25 Scholey AB Moss MC Neave N Wesnes K Cognitive performance hyperoxia and heart rate following oxygen administration in healthy young adults Physiol Behav 1999 67 783 89 https doi org 10 1016 s0031 9384 99 00183 3 PMID 10604851 26 Scholey AB Moss MC Wesnes K Oxygen and cognitive performance the temporal relationship between hyperoxia and enhanced memory Psychopharmacology Berl 1998 140 123 26 https doi org 10 1007 s002130050748 PMID 9862412 27 Vadas D Kalichman L Hadanny A Efrati S Hyperbaric oxygen environment can enhance brain activity and multitasking performance Front Integr Neurosci 2017 11 25 https doi org 10 3389 fnint 2017 00025 PMID 29021747 28 Yu R Wang B Li S Wang J Zhou F Chu S He X Wen X Ni X Liu L Xie Q Huang R Cognitive enhancement of healthy young adults with hyperbaric oxygen a preliminary resting state fMRI study Clin Neurophysiol 2015 126 2058 67 https doi org 10 1016 j clinph 2015 01 010 PMID 25703942 29 Forsythe JA Jiang BH Iyer NV Agani F Leung SW Koos RD Semenza GL Activation of vascular endothelial AGING
growth factor gene transcription by hypoxia inducible factor 1 Mol Cell Biol 1996 16 4604 13 https doi org 10 1128 mcb 16 9 4604 PMID 8756616 exogenous visual spatial orienting Neuroimage 2004 23 534 41 https doi org 10 1016 j neuroimage 2004 06 027 PMID 15488402 30 Liu Y Cox SR Morita T Kourembanas S Hypoxia regulates vascular endothelial growth factor gene 39 Japee S Holiday K Satyshur MD Mukai I Ungerleider LG A role of right middle frontal gyrus in reorienting of attention a case study Front Syst Neurosci 2015 9 23 https doi org 10 3389 fnsys 2015 00023 PMID 25784862 enhancer Circ Res 1995 77 638 43 https doi org 10 1161 01 res 77 3 638 PMID 7641334 31 Krock BL Skuli N Simon MC Hypoxia induced angiogenesis good and evil Genes Cancer 2011 2 1117 33 https doi org 10 1177 1947601911423654 PMID 22866203 40 Tanaka S Honda M Sadato N Modality specific cognitive function of medial and lateral human brodmann area 6 J Neurosci 2005 25 496 501 https doi org 10 1523 JNEUROSCI 4324 04 2005 PMID 15647494 32 Asahara T Takahashi T Masuda H Kalka C Chen D Iwaguro H Inai Y Silver M Isner JM VEGF contributes to postnatal neovascularization by mobilizing bone marrow derived endothelial progenitor cells EMBO J 1999 18 3964 72 https doi org 10 1093 emboj 18 14 3964 PMID 10406801 41 Volz KG Schubotz RI von Cramon DY Why am I unsure internal and external attributions of uncertainty dissociated by fMRI Neuroimage 2004 21 848 57 https doi org 10 1016 j neuroimage 2003 10 028 PMID 15006651 33 Grant MB May WS Caballero S Brown GA Guthrie SM Mames RN Byrne BJ Vaught T Spoerri PE Peck AB Scott EW Adult hematopoietic stem cells provide functional hemangioblast activity during retinal neovascularization Nat Med 2002 8 607 12 https doi org 10 1038 nm0602 607 PMID 12042812 34 Ergul A Abdelsaid M Fouda AY Fagan SC Cerebral neovascularization in diabetes implications for stroke recovery and beyond J Cereb Blood Flow Metab 2014 34 553 63 https doi org 10 1038 jcbfm 2014 18 PMID 24496174 35 Chen JJ Rosas HD Salat DH Age associated reductions in cerebral blood flow are independent from regional atrophy Neuroimage 2011 55 468 78 https doi org 10 1016 j neuroimage 2010 12 032 PMID 21167947 36 Burgess PW Dumontheil I Gilbert SJ The gateway hypothesis of rostral prefrontal cortex area 10 function Trends Cogn Sci 2007 11 290 98 https doi org 10 1016 j tics 2007 05 004 PMID 17548231 37 Gilbert SJ Spengler S Simons JS Steele JD Lawrie SM Frith CD Burgess PW Functional specialization within rostral prefrontal cortex area 10 a meta analysis J Cogn Neurosci 2006 18 932 48 https doi org 10 1162 jocn 2006 18 6 932 PMID 16839301 38 Mayer AR Dorflinger JM Rao SM Seidenberg M Neural networks underlying endogenous and www aging us com 13754 42 Janata P The neural architecture of music evoked autobiographical memories Cereb Cortex 2009 19 2579 94 https doi org 10 1093 cercor bhp008 PMID 19240137 43 du Boisgueheneuc F Levy R Volle E Seassau M Duffau H Kinkingnehun S Samson Y Zhang S Dubois B Functions of the left superior frontal gyrus in humans a lesion study Brain 2006 129 3315 28 https doi org 10 1093 brain awl244 PMID 16984899 44 Haines DE 2012 Fundamental Neuroscience for Basic and Clinical Applications 45 Zur D Naftaliev E Kesler A Evidence of multidomain mild cognitive impairment in idiopathic intracranial hypertension J Neuroophthalmol 2015 35 26 30 https doi org 10 1097 WNO 0000000000000199 PMID 25383589 46 Achiron A Chapman J Magalashvili D Dolev M Lavie M Bercovich E Polliack M Doniger GM Stern Y Khilkevich O Menascu S Hararai G Gurevich M Barak Y Modeling of cognitive impairment by disease duration in multiple sclerosis a cross sectional study PLoS One 2013 8 e71058 https doi org 10 1371 journal pone 0071058 PMID 23936485 47 Thaler A Mirelman A Gurevich T Simon E OrrUrtreger A Marder K Bressman S Giladi N and LRRK2 Ashkenazi Jewish Consortium Lower cognitive performance in healthy G2019S LRRK2 mutation carriers Neurology 2012 79 1027 32 AGING
https doi org 10 1212 WNL 0b013e3182684646 PMID 22914834 48 Dwolatzky T Whitehead V Doniger GM Simon ES Schweiger A Jaffe D Chertkow H Validity of a novel computerized cognitive battery for mild cognitive impairment BMC Geriatr 2003 3 4 https doi org 10 1186 1471 2318 3 4 PMID 14594456 49 L Melton J 2005 Psychometric Evaluation of the Mindstreams Neuropsychological Screening Tool 50 Zygouris S Tsolaki M Computerized cognitive testing for older adults a review Am J Alzheimers Dis Other Demen 2015 30 13 28 https doi org 10 1177 1533317514522852 PMID 24526761 51 Klekociuk SZ Summers JJ Vickers JC Summers MJ Reducing false positive diagnoses in mild cognitive impairment the importance of comprehensive neuropsychological assessment Eur J Neurol 2014 21 1330 36 https doi org 10 1111 ene 12488 PMID 24943259 52 Saunders NL Summers MJ Attention and working memory deficits in mild cognitive impairment J Clin Exp Neuropsychol 2010 32 350 57 https doi org 10 1080 13803390903042379 PMID 19787522 53 Lu PH Boone KB Cozolino L Mitchell C Effectiveness of the rey osterrieth complex figure test and the meyers and meyers recognition trial in the detection of suspect effort Clin Neuropsychol 2003 17 426 40 https doi org 10 1076 clin 17 3 426 18083 PMID 14704893 54 Vakil E Blachstein H Rey AVLT Developmental norms for adults and the sensitivity of different memory measures to age The Clinical Neuropsychologist 1997 11 356 69 https doi org 10 1080 13854049708400464 55 Jaeger J Digit symbol substitution test the case for sensitivity over specificity in neuropsychological testing J Clin Psychopharmacol 2018 38 513 19 https doi org 10 1097 JCP 0000000000000941 PMID 30124583 56 Humpstone HJ Memory span tests Psychol Clin 1919 12 196 200 PMID 28909279 57 Tucha L Aschenbrenner S Koerts J Lange KW The five point test reliability validity and normative data for children and adults PLoS One 2012 7 e46080 https doi org 10 1371 journal pone 0046080 PMID 23029395 www aging us com 13755 58 Rabin LA Barr WB Burton LA Assessment practices of clinical neuropsychologists in the united states and Canada a survey of INS NAN and APA division 40 members Arch Clin Neuropsychol 2005 20 33 65 https doi org 10 1016 j acn 2004 02 005 PMID 15620813 59 Barry D Bates ME Labouvie E FAS and CFL forms of verbal fluency differ in difficulty a meta analytic study Appl Neuropsychol 2008 15 97 106 https doi org 10 1080 09084280802083863 PMID 18568601 60 Paiva SC Viapiana VF Cardoso CO Fonseca RP Bells test are there differences in performance between adult groups aged 40 59 and 60 75 Dement Neuropsychol 2017 11 40 47 https doi org 10 1590 1980 57642016dn11 010007 PMID 29213492 61 Ostergaard L Weisskoff RM Chesler DA Gyldensted C Rosen BR High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part I mathematical approach and statistical analysis Magn Reson Med 1996 36 715 25 https doi org 10 1002 mrm 1910360510 PMID 8916022 62 Ostergaard L Sorensen AG Kwong KK Weisskoff RM Gyldensted C Rosen BR High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part II experimental comparison and preliminary results Magn Reson Med 1996 36 726 36 https doi org 10 1002 mrm 1910360511 PMID 8916023 63 Russo J Trujillo CA Wingerson D Decker K Ries R Wetzler H Roy Byrne P The MOS 36 item short form health survey reliability validity and preliminary findings in schizophrenic outpatients Med Care 1998 36 752 56 https doi org 10 1097 00005650 199805000 00015 PMID 9596066 64 McHorney CA Ware JE Jr Lu JF Sherbourne CD The MOS 36 item short form health survey SF 36 III Tests of data quality scaling assumptions and reliability across diverse patient groups Med Care 1994 32 40 66 https doi org 10 1097 00005650 199401000 00004 PMID 8277801 65 McHorney CA Ware JE Jr Raczek AE The MOS 36 item short form health survey SF 36 II Psychometric and clinical tests of validity in measuring physical and mental health constructs Med Care 1993 31 247 63 https doi org 10 1097 00005650 199303000 00006 PMID 8450681 AGING
66 Hochberg Y A Sharper Bonferroni Procedure for Multiple Tests of Significance Biometrika 1988 75 800 2 https doi org 10 1093 biomet 75 4 800 www aging us com 13756 AGING
SUPPLEMENTARY MATERIALS Supplementary Methods DSC analysis steps where AIFfit t and Cfit t are the fitted AIF t and Cm t curves respectively K is a constant x is the image num 1 Conversion of signal intensity to concentration of Gd DTPA with respect to time gamma variate parameters and Fstep is a step function defined by SI 1 MRI analysis Cm t K ln S t where Cm t is the measured concentration of GdDTPA with respect to time K is a proportionality constant that is inversely proportional to the TE and depends on the MR scanner S t is the MRI signal intensity with respect to time and so is the baseline MRI signal before the presence of Gd DTPA and after a steady state magnetization has been achieved 3 2 Arterial input function the AIF was measured automatically using the following algorithm a The volume with maximum Cm t intensity was identified 10th 13th volume Only voxels with maximum intensity in this volume were identified as AIF candidates b Only voxels with maximum intensity higher than the 96th percentile and lower than the 99 9th percentile were included c d The AIF voxel candidates were fitted to the gamma variate function using the following equation 3 Goodness of fit was evaluated and only voxels with R2 0 96 were included x K x e B Fstep x matrix of the deconvolved C t curve This equation can be solved using the SVD technique whereby the matrix AIF is decomposed into three matrices AIF AIF 1 represents the reciprocals of the diagonal elements of W When calculating AIF 1 problems arise when W contains singular values i e wj 0 or is close to 0 and will cause the curve C t to oscillate Therefore we used a cutoff threshold of 10 1 5 Calculation of CBV was performed based on the fitted Cm t and AIF CBV k Cm t dt AIF t dt the fact that the hematocrit in large vessels HCTLV was set to 0 45 is larger than the hematocrit of small vessels HCTSV was set to g ml 3 e The final AIF was an average of the Cm t signal in the voxels passing the above criteria f Normalization of AIF To allow a uniform time of injection in all subjects and DSC scans the Cm t was shifted in case of early late injection to allow a uniform AIF peak at the 10th volume 3 Gamma fitting of AIF and Cm The AIF and Cm t were fitted to the gamma variate function using the gamma fit equation see above 3 www aging us com 0 0 4 SVD deconvolution The fitted AIF was used to calculate C t the tissue response to an instantaneous arterial bolus using SVD deconvolutions was done by Ostergaard et al 1996 In short the values for the AIF and Cm t curves can be written in vector Only voxels with a shape of sharp increase and sharp decrease were included AIFfit t or C fit t 1 for x 0 for x Fstep S0 13757 6 Calculation of CBF was performed using the following equation CBV CBF C t dt Cmax where C t is the concentration of Gd DTPA in a tissue region and Cmax is the maximum of this curve 3 AGING
7 MTT was calculated 2 MTT Supplementary References Ostergaard L Sorensen AG Kwong KK Weisskoff RM Gyldensted C Rosen BR High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part II Experimental comparison and preliminary results Magn Reson Med 1996 36 726 36 https doi org 10 1002 mrm 1910360511 PMID 8916023 www aging us com Ostergaard L Weisskoff RM Chesler DA Gyldensted C Rosen BR High resolution measurement of cerebral blood flow using intravascular tracer bolus passages Part I Mathematical approach and statistical analysis Magn Reson Med 1996 36 715 25 https doi org 10 1002 mrm 1910360510 PMID 8916022 3 Smith AM Grandin CB Duprez T Mataigne F Cosnard G Whole brain quantitative CBF CBV and MTT measurements using MRI bolus tracking implementation and application to data acquired from hyperacute stroke patients J Magn Reson Imaging 2000 12 400 10 https doi org 10 1002 15222586 200009 12 33 0 co 2 c PMID 10992307 CBV CBF 8 Normalization of the CBF Since the amount of injection was not uniform between scans the CBF was normalized using a factor of 1 9 divided by the AIF peak value 1 2 13758 AGING
Supplementary Tables Please browse Full Text version to see the data of Supplementary Table 1 Supplementary Table 2 Neurocognitive function repeated measures analysis F p value F p value Interaction Effect Group_by_Time F p value 7 171 0 009 34 382
Supplementary Table 3 Global cerebral blood flow changes Control Group N 19 Whole Brain Grey Matter White Matter HBOT Group N 20 Baseline Control 3 months P value Baseline PostHBOT 3 months P value 41 34 6 22 47 79 8 84 28 40 7 35 41 55 6 78 47 93 9 89 28 57 7 17 0 88 0 94 0 88 47 13 69 58 20 9 43 29 12 6 37 50 22 7 26 61 92 8 22 30 67 4 93 0 054 0 057 0 198 Baseline Comparison P value 4 0 001 Group by time P value 0 180 0 170 Supplementary Table 4 Significant correlations between cognitive changes and perfusion changes Area BA Battery Test Parameter R P Value Right superior medial frontal gyrus 6 CANTAB Set shifting ASTLCM 0 343 0 03 Right superior medial frontal gyrus 6 CANTAB Set shifting ASTLCD 0 384 0 01 Right superior medial frontal gyrus 6 CANTAB Set shifting ASTLMD 0 455 0 004 Right superior medial frontal gyrus 6 CANTAB Set shifting ASTLICM 0 41 0 01 Right superior medial frontal gyrus 6 CANTAB Set shifting ASTLICMD 0 473 0 003 Right superior medial frontal gyrus 6 CANTAB Set shifting ASTLM 0 386 0 01 Right supplementary motor area 6 CANTAB Set Shifting ASTLCMD 0 323 0 048 Right supplementary motor area 6 CANTAB Set Shifting ASTLDM 0 363 0 025 Right supplementary motor area 6 CANTAB Set Shifting ASTLICMD 0 379 0 02 Left middle frontal gyrus 8 NeuroTrax Memory Memory 0 379 0 023 Right middle frontal gyrus 6 NeuroTrax Attention Attention 0 339 0 043 Right superior medial frontal gyrus 6 Pen and Paper RAVLT Total 0 393 0 016 Right superior medial frontal gyrus 6 Pen and Paper FAS Semantic 0 353 0 032 Right supplementary motor area 6 Pen and Paper RAVLT Total 0 394 0 016 Right superior parietal gyrus 7 Pen and Paper RAVLT Total 0 380 0 002 Supplementary Table 5 Quality of life SF 36 questionnaire changes Control Group N 33 3 months Baseline Control P value Physical function 86 97 5 41 89 25 12 99 Physical limitations 57 70 58 Emotional limitations 52 Energy Emotional well being Social function Pain General health www aging us com HBOT Group N 29 Baseline Net Comparison Effect 3 months Baseline Post HBOT P value Size P value 28 0 08 0 66 8 57 81 0 19 0 50 0 14 0 71 87 05 17 17 0 77 0 69 0 17 75 0 0 23 0 30 13760 0 75 0 65 0 92 0 93 AGING
Supplementary Table 6 Quality of life SF 36 questionnaire repeated measures analysis Main Effect of Group Main Effect of Time Interaction Effect Group_by_Time F p value F p value F p value Physical function 0 108 0 743 8 266 0 006 2 406 0 128 Physical limitations 0 096 0 758 2 025 0 162 0 580 0 450 Emotional limitations 0 379 0 541 0 296 0 589 0 814 0 372 Energy 0 274 0 604 6 281 0 016 6 908 0 012 Emotional well being 0 089 0 767 3 005 0 090 2 733 0 105 Social function 0 107 0 745 0 590 0 446 0 001 0 977 Pain 0 000 0 985 4 404 0 042 2 770 0 103 General health 0 010 0 920 7 690 0 008 0 087 0 769 www aging us com 13761 AGING
NEURAL REGENERATION RESEARCH Volume 8 Issue 35 December 2013 www nrronline org Hyperbaric oxygen therapy improves cognitive functioning after brain injury Su Liu1 Guangyu Shen1 Shukun Deng1 Xiubin Wang2 Qinfeng Wu1 Aisong Guo1 1 2 Su Liu Master Lecturer Graphical Abstract atial learning and memory abilities were improved HBOT N acetylaspartate creatine ratio and N acetylaspartate choline ratio in hippocampal CA3 region were increased The number of nerve cells in hippocampal CA3 region was increased Traumatic brain injury models were established using The number of activated astrocytes in hippocampal CA3 region was decreased Abstract Hyperbaric oxygen therapy has been widely applied and recognized in the treatment of brain injury however the correlation between the protective effect of hyperbaric oxygen therapy and changes of metabolites in the brain remains unclear To investigate the effect and potential mechanism of hyperbaric oxygen therapy on cognitive functioning in rats we established traumatic brain injury rbaric oxygen therapy at 0 2 MPa for 60 minutes per day The Morris water maze test for spatial navigation showed that the average escape latency was significantly prolonged and cognitive function decreased in rats with brain injury After treatment with hyperbaric oxy learning and memory abilities were improved Hydrogen proton magnetic resonance spectroscopy analysis showed that the N acetylaspartate creatine ratio in the hippocampal CA3 region was significantly increased at 1 week and the N acetylaspartate choline ratio was significantly increased at 2 weeks after hyperbaric oxygen therapy Nissl staining and immunohistochemical staining showed that the number of nerve cells and Nissl bodies in the hippocampal CA3 region was significantly increased and glial fibrillary acidic protein positive cells were decreased after a 2 week hyperbaric oxygen therapy treatment Our findings indicate that hyperbaric oxygen therapy significantly improves cognitive functioning in rats with traumatic brain injury and the potential mechanism is mediated by metabolic changes and nerve cell restoration in the hippocampal CA3 region Key Words neural regeneration brain injury hyperbaric oxygen magnetic resonance spectroscopy astrocytes immunohistochemistry choline creatine N acetylaspartate CA3 region Morris water maze hippocampus neuroregeneration 3334 Corresponding author Guangyu Shen Chief physician Department of Rehabilitation Medicine Affiliated Hospital of Nantong University Nantong 226001 Jiangsu Province China sgyrm 163 com Received 2013 09 04 Accepted 2013 11 02 N201303073 Acknowledgments We would like to thank Zhang ZJ and Dong YL from Department of Anatomy Medical School of Nantong University China for their excellent technical assistance Author contributions Shen GY was responsible for the study design and funds Liu S performed the experiments and wrote the paper Deng SK and Wang XB conducted the experiments Guo AS revised the article Wu QF analyzed the data All authors approved the final version of the paper Conflicts of interest None declared Ethical approval The study gained full ethical approval from the Animal Ethics Committee of Nantong College in China
INTRODUCTION Traumatic brain injury TBI is one of the contributory reasons for death and disability 1 Survivors of severe TBI often develop a variety of disorders in cognition neurophysiological function psychology and emotion and behavioral function which seriously affects their quality of life 2 4 The hippocampus is the main brain center for learning and memory ability in animals Are there any changes to nerve cells in the hippocampus after brain injury What happens to its metabolic function Hyperbaric oxygen therapy HBOT has been recognized as an effective treatment for brain injury 5 but its potential mechanism remains unclear The goals of this study are threefold to observe the influence of HBOT on cognitive function in TBI rats to explore the changes of hippocampal structure and function after HBOT to investigate the mechanism of HBOT involved in cognitive function attention after 1 year of HBOT leaving neuroimaging changes unstudied To explore the effect of HBOT on cognitive function in rats we used 1H MRS to conduct continuous observations of hippocampal tissue metabolism change in TBI rats at different time points after treatment and ratios of N acetylaspartate creatine and N acetylaspartate choline in the rat hippocampal CA3 region at the same time point after HBOT 16 In 2007 Huang proposed that glial scar hyperplasia was highly involved in spatial learning and memory defects in newborn rats with hypoxic ischemic brain injury and that HBOT reduced hippocampal neuronal loss and improved cognitive function in rats Using Nissl staining and immunofluorescence staining we observed hippocampal CA3 neurons and astrocytes in TBI rats after HBOT treatment for 2 weeks This was a broad attempt to analyze the link between hippocampal neurons and cognitive functions and to explore the HBOT actions on hippocampal neurons RESULTS In this study the Morris water maze navigation task was applied to observe the change in cognitive functions immediately after TBI and at different periods after HBOT Previous studies addressing the HBOT mechanism have been limited to the observation of the animal brain morphology apoptosis pathophysiology cytokines and neurotrophic factors at lesions after animals were killed at a certain time point 6 8 However there has been no investigation concerning the evidence at different time points Functional MRI can provide pathophysiological and functional information after brain injury in a non invasive manner It can also assist in assessing brain injury severity cognitive dysfunction structural and functional reorganization hemorrhage focus and prognosis 9 Among the functional MRI techniques hydrogen proton magnetic resonance spectroscopy 1H MRS is the only non invasive imaging technique for revealing tissue metabolism It allows continuous dynamic observation of metabolic changes at the lesion site and provides a new means for understanding the disease pathogenesis 10 Currently 1H MRS has been used for observing brain metabolic changes in multiple sclerosis and Parkinson s disease and for exploring the correlation with cognitive function 11 14 However little evidence is available regarding the dynamic observation of HBOT for 15 brain injury Churchill found that 51 of brain injury patients experienced improvement in memory and Quantitative analysis of experimental animals Thirty three Sprague Dawley rats were randomly divided into either the sham surgery group 10 only exposing the dura mater or the model group 23 TBI models were established using the Feeney s free falling method After three rats were excluded from the model group due to modeling failure the remaining 20 successful models were further assigned into the HBOT group or TBI group with ten rats in each group The HBOT group was given HBOT once per day for 2 weeks A total number of 30 rats were included in the analysis Effect of HBOT on cognitive function of TBI rats Test results from the Morris water maze task showed that the average escape latency of rats in the TBI and HBOT groups at 3 days 1 week and 2 weeks after treatment was increased compared with the sham surgery group 0 05 This demonstrates that cognitive functions were significantly decreased after brain injury in rats At 1 and 2 weeks the HBOT group had better cognitive function than the TBI group 0 05 Table 1 Effect of HBOT on brain metabolism in the hippocampal CA3 region of TBI rats 1 H MRS analysis showed that there was no significant difference in the N acetylaspartate choline and N acetylaspartate creatine ratios in the contralateral 3335
hippocampal CA3 region of rats in the TBI and HBOT groups when compared with the sham surgery group at each time point Table 2 Table 1 Effect of hyperbaric oxygen therapy HBOT on the average escape latency s of traumatic brain injury TBI rats in the Morris water maze Group HBOT TBI Sham Time after injury 3 days 1 week a 73 13 6 31 85 83 5 38a 14 75 4 12 2 weeks ab 34 76 4 43 60 48 6 67a 13 50 1 19 27 19 3 70ab 41 46 4 09a 11 42 3 19 a 0 05 sham group at the same time point b 0 05 TBI group at the same time point Data are expressed as mean SD in ten rats for each group one way analysis of variance and Student Newman Keuls test Sham Sham surgery group Compared with the sham surgery group the N acetylaspartate creatine ratio in the ipsilateral hippocampal CA3 region was significantly decreased in the TBI group 0 05 After 48 hours of treatment the decreased ratio was more apparent in the TBI and HBOT groups 0 05 After 1 and 2 weeks of treatment the N acetylaspartate creatine ratio in the HBOT group was significantly increased compared with the TBI group 0 05 Table 2 Figure 1 At 8 hours 48 hours 1 week and 2 weeks after treatment the N acetylaspartate choline ratio in the ipsilateral hippocampal CA3 region was significantly decreased in the TBI group compared with the sham surgery group 0 05 At 2 weeks after treatment the HBOT group had significantly higher N acetylaspartate choline ratios than the TBI group 0 05 Table 2 Figure 1 Effect of HBOT on histological change of the hippocampal CA3 region in TBI rats Nissl staining showed that the hippocampal CA3 neurons were tightly and neatly arranged demonstrating intact morphology and multilateral shape in the sham operated rats The nucleolus was distributed in the center and blue plaques or granular Nissl bodies were visible in the cytoplasm In the TBI group the hippocampal CA3 neurons were sparse and disorderly arranged cell spacing was widened a large number of pyknotic and necrotic neurons demonstrated atrophy and Nissl bodies were decreased or had disappeared In the HBOT group the number of nerve cells in the hippocampal CA3 region was significantly increased at 2 weeks after treatment The neurons were tightly distributed and Nissl bodies were increased compared with the TBI group Figure 2 Effect of HBOT on the glial fibrillary acidic proteinpositive cells in the hippocampal CA3 region of TBI rats An immunofluorescence assay showed that at 2 weeks after treatment glial fibrillary acidic protein positive cells in the hippocampal CA3 region exhibited intact structure and clearly visible protrusion in the sham surgery rats In the TBI group the number of glial fibrillary acidic protein positive cells and protrusions in the hippocampal CA3 region was significantly increased compared with the sham surgery group 0 01 After 2 weeks of hyperbaric oxygen therapy the number of glial fibrillary acidic protein positive cells and protrusions in the hippocampal CA3 region was significantly decreased compared with the TBI group 0 01 Data are shown in Figure 3 Table 2 Effect of hyperbaric oxygen therapy HBOT on N acetylaspartate choline NAA Ch and N acetylaspartate creatine NAA Cr ratios in the hippocampal CA3 region of traumatic brain injury TBI rats at different time points Item Contralateral hippocampus NAA Cr ratio Time after injury 8 hours 24 hours 48 hours 1 week 2 weeks HBOT 1 38 0 23 1 46 0 41 1 56 0 43 1 29 0 21 1 55 0 22 TBI 1 72 0 60 1 51 0 44 1 71 0 43 1 48 0 18 1 45 0 32 Sham 1 33 0 18 1 23 0 17 1 59 0 08 1 24 0 16 1 35 0 19 Ipsilateral hippocampus NAA Cr ratio HBOT 1 18 0 22 1 24 0 14 1 01 0 40a 1 08 0 20b 1 42 0 44b a a a a TBI 0 70 0 26 0 98 0 20 1 03 0 22 0 81 0 26 0 96 0 24a Sham 1 35 0 08 1 33 0 09 1 53 0 49 1 41 0 44 1 43 0 21 Contralateral hippocampus NAA Ch ratio HBOT 1 22 0 24 1 29 0 35 1 34 0 35 1 21 0 16 1 34 0 20 TBI 1 58 0 31 1 39 0 37 1 40 0 57 1 23 0 16 1 35 0 41 Sham 1 36 0 36 1 56 0 36 1 55 0 47 1 63 0 12 1 68 0 40 Ipsilateral hippocampus NAA Ch ratio HBOT 1 23 0 43a 1 69 0 43 1 05 0 54a 0 99 0 21a 1 51 0 25b a a a TBI 0 78 0 17 1 29 0 61 0 91 0 30 0 86 0 23 0 87 0 20a Sham 1 61 0 10 1 54 0 11 1 66 0 14 1 62 0 29 1 79 0 36 a 0 05 sham group at the same time point b 0 05 TBI group at the same time point Data are expressed as mean SD in ten rats for each group one way analysis of variance and Student Newman Keuls test Sham Sham surgery group 3336
Liu S et al Neural Regeneration Research 2013 8 35 3334 3343 B A C Figure 1 Magnetic resonance spectroscopy images of the rat hippocampal CA3 at the injury side after hyperbaric oxygen therapy for 2 weeks A In the sham surgery group the NAA peak value was significantly A higher than Cr and Ch values B B In the traumatic brain injury group the NAA value was significantly decreased while the Cr and Ch values were elevated C In the hyperbaric oxygen therapy group the NAA value was higher than that in the traumatic brain injury group Both the NAA Ch and NAA Cr ratios were increased CA3 NAA N acetylaspartate Cr creatine Ch choline A A B C D CA3 C 2 Histological changes in the Figure D hippocampal CA3 region on the injured side of traumatic brain injury rats after hyperbaric oxygen therapy for 2 weeks Nissl staining optical microscopy scale bars A 25 B D 200 White arrows indicate Nissl positive cells black arrows indicate Nissl bodies The black squares in B C and D are the areas enlarged in the insert at the right upper of each image A Black square in A and B is the observed area B In the sham surgery group hippocampal CA3 neurons were arranged tightly and the structure was intact C In the traumatic brain injury group hippocampal CA3 neurons were arranged sparsely and disordered A large number of pyknotic and necrotic neurons exhibited atrophy and Nissl bodies decreased or disappeared D In the hyperbaric oxygen therapy group the number of hippocampal CA3 neurons was increased significantly and more compact compared with those in the traumatic brain injury group The number of Nissl bodies was also increased A B Figure 3 Glial fibrillary acidic protein GFAP expression in the hippocampal CA3 region of the injured side of traumatic brain injury TBI rats after hyperbaric oxygen therapy for 2 weeks fluorescence microscopy scale bars A 100 B D 200 CA3 C E a 35 GFAP absorbance value White arrows indicate GFAP positive cells A White block is the observed hippocampal CA3 B In the sham surgery group the GFAP positive cells in hippocampal CA3 showed an intact structure with clearly visible protrusions C In the TBI group the number of GFAP positive cells and protrusions in the hippocampal CA3 region were significantly increased D In the hyperbaric oxygen therapy HBOT group the number of GFAP positive cells and protrusions in the hippocampal CA3 region were significantly decreased D 30 ab 25 20 15 10 5 0 Sham group TBI group E GFAP average absorbance values in the hippocampal CA3 region Six sections of the CA3 region were selected to measure the absorbance value in eight fields of view Then the mean absorbance values in each group were calculated aP 0 01 vs sham group bP 0 01 vs TBI group Data are expressed as mean SD in 10 rats for each group one way analysis of variance and Student Newman Keuls test sham Sham surgery HBOT group 3337
DISCUSSION Brain tissue structural impairment as a result of TBI can be divided into primary injury and secondary injury Primary injury occurs directly after the insult it is caused by a mechanical strike that immediately starts to cause damage to the axons and neurons glial cells and vessels Primary injury may trigger a cascade of biochemical reactions within several minutes such as cerebral edema local ischemia and hypoxia inflammation and massive release of excitatory amino acids Accordingly these reactions lead to cell injury death apoptosis even disability for several days or several weeks and sometimes coma These changes are referred to as secondary injury 17 19 Primary injury cannot be prevented in time because it occurs only a few seconds after the insult however secondary injury can be prevented in some cases and as such it has acquired increasing attention HBOT helps alleviate secondary brain injury following TBI In this study cognitive functioning in injured rats was assessed using a water maze task The results from this study suggest that cognitive functioning in these rats began to decline after TBI and was significantly improved after 1 week of HBOT This is consistent with previous findings 20 However the HBOT mechanism in the treatment of TBI is poorly understood Existing studies have summarized the following pathways as possible mechanisms 1 Hyperbaric oxygen increases blood oxygen content reduces intracranial pressure ameliorates cerebral edema blocks hypoxia brain edema vicious cycle and protects brain tissue around the lesion against secondary damage 21 23 2 Hyperbaric oxygen inhibits the apoptosis of nerve cells around the injury and hippocampal neurons and reduces the loss of hippocampal neurons through up regulating Bcl 2 and Bcl xl expression and down regulating Bax expression 24 25 3 Hyperbaric oxygen increases the brain metabolic rate and blood oxygen content protects mitochondrial function reduces lactate levels in the cerebrospinal fluid and increases ATP content thereby facilitating aerobic metabolism in traumatic brain tissue 26 27 4 HBOT inhibits the generation of free radicals after TBI thereby reducing lipid peroxidation it also reduces proinflammatory factor generation and promotes anti inflammatory factor production thereby reducing inflammatory reactions in brain tissue and assisting to reduce TBI secondary injury 6 28 The present study 3338 predominantly explored the mechanism of HBOT involved in the improvement of cognitive function It is known that the optimal time window for the first time for HBOT is 6 hours after TBI 17 and that repeated therapy can significantly reduce brain injury and promote the recovery of neurological function in patients with brain injury Thus we chose to begin HBOT treatment exactly 6 hours after the brain injury 1 H MRS can assess the severity of central nervous system damage qualitatively and quantitatively This damage is associated with N acetylaspartate Cr and choline creatine ratios 29 31 For example Du and colleagues 32 found a correlation between N acetylaspartate creatine N acetylaspartate choline ratios and Glasgow Coma Scale scores after severe brain injury patients had lower N acetylaspartate creatine and N acetylaspartate choline ratios and a higher choline creatine ratio Additionally 33 Carpentier showed that in severe brain injury patients with negative results demonstrated on brainstem MRI examination the N acetylaspartate creatine ratio was lower than the normal group the brainstem N acetylaspartate creatine ratio was 1 5 and the N acetylaspartate choline creatine N acetylaspartate ratio was 0 40 when the Glasgow Coma Scale score was 1 2 points In patients with a GCS score of 3 points the brainstem choline creatine ratio N acetylaspartate creatine ratio or choline choline creatine N acetylaspartate ratio was 0 40 Cognitive impairment is strongly linked with hippocampal N acetylaspartate creatine and other metabolites showing a significantly decreased 34 35 N acetylaspartate creatine ratio The N acetylaspartate peak is highest in a normal brain spectrum and its content is the most sensitive to changes of brain states thus making it a well accepted neuronal marker N acetylaspartate level in the brain directly reflects the functional state of neurons 36 The present study showed that N acetylaspartate creatine and N acetylaspartate choline ratios at the ipsilateral hippocampal CA3 of TBI rats were reduced compared with the sham group at 8 hours to 2 weeks after treatment in particular the reduction was apparent at 8 hours This evidence suggests ipsilateral hippocampal neuronal dysfunction or damage after brain injury The hippoca and memory function and brain damage causes hippocampal CA3 neuronal death 37 In this study Nissl staining results showed that at 2 weeks after brain injury hippocampal CA3 neurons were sparse and disorderly arranged a large number of pyknotic and necrotic neurons exhibited atrophy and Nissl bodies decreased or
disappeared Results from the Morris water maze task showed that cognitive functioning was significantly reduced at different time points after brain injury suggesting that cognitive impairment is closely associated with ipsilateral hippocampal neuronal necrosis structural changes and metabolic abnormalities 1 H MRS can measure trace metabolites noninvasively in the brain and assess prognosis and recovery follow 31 ing brain injury 38 39 Vagnozzi found that N acetylaspartate creatine and N acetylaspartate choline ratios were decreased in patients with mild brain injury and gradually returned to normal as the disease conditions improved Semenova 40 examined the N acetylaspartate level to detect the prognosis of children with severe brain injury after cell therapy In this study the hippocampal N acetylaspartate creatine and N acetylaspartate choline ratios were detected using 1 H MRS at different time points after HBOT The results indicated that the N acetylaspartate creatine ratio was significantly increased after 1 and 2 weeks of treatment in the HBOT group compared with the TBI group Also the N acetylaspartate choline ratio was significantly increased at 2 weeks and hippocampal neurons were repaired Meanwhile cognitive function of rats in the HBOT group was better than the TBI group Nissl staining revealed that the number of hippocampal CA3 neurons was increased significantly at 2 weeks after treatment the neurons were tightly arranged and the Nissl bodies were increased compared with the TBI group However the number of Nissl bodies was still lower than in the sham group These findings indicate that HBOT can promote the repair of hippocampal CA3 neurons and alter hippocampus metabolism thereby promoting cognitive function recovery in rats with traumatic brain injury Choline levels reflect the total choline content in the brain including phosphocholine phosphatidyl choline and glycerol phosphate 41 The majority of choline is present in glial cells It is involved in cell membrane phospholipid metabolism and reflects membrane synthesis thus an increase in the choline peak is an indicator of glial cell proliferation 42 Epileptic patients with complex partial seizures have been found to demonstrate obvious cognitive impairment and a decreased hippocampal N acetylaspartate choline creatine ratio 43 The elevated choline level indicates hippocampal neuronal necrosis and glial cell proliferation 43 Glial fibrillary acidic protein is a specific cytoskeletal protein in astrocytes and is expressed in mature astrocytes so it is recognized as an astrocyte specific molecular marker 44 In this study glial fibrillary acidic protein immunofluorescence staining showed that 2 weeks after brain injury hippocampal N acetylaspartate creatine and N acetylaspartate choline ratios decreased while glial fibrillary acidic protein expression was significantly up regulated The number of glial fibrillary acidic protein positive cells and protrusions were significantly increased and the absorbance value was also significantly higher than in the sham group At this time point 2 weeks cognitive functioning in rats in the TBI group was significantly lower than in the sham operated rats These findings indicate that cognitive impairment was closely related to glial cell proliferation in the hippocampal CA3 region and changes in hippocampal metabolism After injury to the central nervous system astrocyte proliferation has a double edged sword effect 45 46 On the one hand reactive hyperplasia of astrocytes provides nutrition for nerve tissue promotes nerve tissue repair improves neurological function and cognitive function and contributes to the clearance of myelin and neuronal debris at the injury On the other hand excessive activation and proliferation of astrocytes has toxic effects on the nerve tissue and hinders myelin or axonal regeneration thereby interfering with neuronal loop functions Sandhir and colleagues 47 found that glial fibrillary acidic protein expression was up regulated in the hippocampus after brain injury and peaked at 1 week in aged and adult rats At 3 7 14 days after injury its expression was higher than that in adult rats and longer than that in aged rats Activated astrocytes are a potential cause for cognitive function deterioration in aged rats with brain injury Preliminary studies of our research group demonstrated that at 1 4 weeks after brain injury a large number of activated glial cells was observed in the cerebral cortex around the injury site Rehabilitation training has been demonstrated to reduce the activation of astrocytes and accordingly promote neurological functional recovery after TBI in rats 48 The present study showed that the number of astrocytes and protrusions in the hippocampal CA3 region was significantly reduced after 2 weeks of HBOT After treatment the N acetylaspartate creatine and N acetylaspartate choline ratios were increased and cognitive function gradually recovered This evidence suggests that activated astrocytes affect cognitive function restoration and the potential mechanisms are mediated by metabolic change in the hippocampus Further studies are needed to explore their interaction In summary our findings show that the number of hippocampal nerve cells and the rate of metabolism vary after brain injury HBOT alleviates injury at the site of a 3339
lesion and promotes cognitive function recovery in TBI rats The potential mechanism depends on the promotion of hippocampal CA3 neuronal repair and the inhibition of astrocyte activation as well as being related to increases in hippocampal N acetylaspartate creatine and N acetylaspartate choline ratios Meanwhile as a non invasive detection method for metabolites 1 H MRS technique provides important information for brain injury diagnosis treatment and prognosis evaluation Some limitations of the study warrant mention First the sample in our experiment was relatively small which may have affected the results Second our two researchers had previous experience working with HBOT this may have had an effect on the treatment outcomes Future studies are planned to analyze the therapeutic effect of HBOT on different degrees of brain injury in patients of different ages MATERIALS AND METHODS Design A randomized controlled animal experiment Time and setting Experiments were performed at the Experimental Animal Center of Nantong University China and Department of Rehabilitation Medicine Affiliated Hospital of Nantong University China from May 2012 to January 2013 Materials Thirty three healthy adult male Sprague Dawley rats of clean grade weighing 300 350 g were provided by the Experimental Animal Center of Nantong University China license number SYXK Su 2012 0031 Experimental disposals were in accordance with the issued by the Ministry Science and Technology of China 49 Methods Establishing TBI models The TBI models were established in rats using Feeney s weight drop method with slight modifications 50 In brief rats were anesthetized with an intraperitoneal injection of 1 sodium pentobarbital 40 mg kg and their heads were fixed in a stereotaxic apparatus WPI Sarasota Florida USA after shaving parietal hair A median sagittal incision was made on the scalp under routine disinfection exposing the bregma Then a bone window 3340 4 0 mm diameter was cut at 3 0 mm posterior to the bregma and 3 0 mm right lateral to the sagittal suture A 25 g weight was allowed to fall from 30 cm height onto the right brain to produce a moderate impact injury at 3 5 mm diameter and 3 0 mm compression depth 750 g cm The model was defined successful when it caused a hematoma in the cortex immediately after injury The dura mater was exposed in the sham operated rats however they received no impact HBOT interventions Rats subjected to the HBOT were placed in a homemade cage and transferred to a single hyperbaric oxygen chamber Shanghai 701 Institute Yangyuan Medical HBO Chamber Factory Shanghai China HBOT was given at 6 hours after injury 17 the oxygen pressure was first increased for 15 minutes to 0 2 MPa then maintained stationary for 60 minutes and finally decreased for 15 minutes to atmospheric pressure During the therapy pure oxygen ventilation was given for 10 minutes to avoid CO2 accumulation After the pressure was decreased rats were taken out of the chamber The therapy was performed once per day for 2 weeks Assessment of cognitive function after HBOT Morris water maze equipment was provided by Shanghai Softmaze Information Technology Co Ltd Shanghai China All rats were allowed to swim freely for 2 minutes 1 day prior to the modeling to adapt the environment At 2 and 9 days after treatment a 5 day spatial navigation test was performed to detect average escape latency and to assess spatial learning and memory ability three times per day at an interval of 5 minutes After the test was complete rats were allowed to stay on the platform for 20 seconds Rats entered the water pool from the fourth quadrant and the platform was located at the first quadrant During the whole experiment the platform was maintained in the same quadrant The rat swimming route and the time taken to find the platform were recorded this was the escape latency The time limit for each test was 120 seconds The rats that failed to find the platform within 120 seconds had their time recorded as 120 seconds The latency was calculated at 3 days 1 week and 2 weeks after treatment 1 H MRS and data analysis Rats were scanned using 1H MRS with small animal dedicated coils using a Signa 3 0 T MR scanner Signa Excite HD GE Healthcare Fairfield CT USA at 8 hours 24 hours 48 hours 1 week and 2 weeks after treatment The scalp was scanned from the bregma through 10 layers at 1 8 mm thickness and 0 2 mm gap
Bilateral hippocampi were selected as regions of interest in the coronal T2FSE Scanning parameters two dimensional multi voxel spectroscopy PRESS sequence repetition time 5 000 ms echo time 115 9 ms frequency 90 256 field of view 5 0 cm number of excitations 4 0 region of interest 2 4 mm2 voxel thickness 7 mm voxel size 2 4 mm 2 4 mm 7 0 mm duration 5 minutes and 28 seconds The N acetylaspartate creatine and choline contents were recorded N acetylaspartate choline and N acetylaspartate creatine ratios were calculated Chemical shift images obtained using two dimensional multi voxel spectroscopy were scanned and processed using commercial software Functool 2 The N acetylaspartate choline and N acetylaspartate creatine ratios were calculated with the relative quantitative values of the hippocampal CA3 metabolites Nissl staining for the morphology of rat hippocampal CA3 nerve cells At 2 weeks after treatment rats were anesthetized with 1 sodium pentobarbital 40 mg kg and the heart was rapidly perfused with 0 9 physiology 150 mL and fixed in 4 paraformaldehyde 250 mL Subsequently the rats were killed the brains were removed and fixed in 4 paraformaldehyde for 6 hours dehydrated in sucrose gradient precipitated and serially sectioned into coronal frozen sections Leica Microsystems Heidelberg Ger sections were rinsed with 0 01 mol L PBS pH 7 4 three times for 15 minutes each The controls were incubated with normal goat serum 1 50 instead of primary antibody and the result was negative The glial fibrillary acidic protein positive cells in the hippocampal CA3 region were observed under fluorescence microscope 200 magnification Leica and image analysis was performed using JEDA 801 Series morphological analysis software Jiangsu JEDA Science Technology Development Co Ltd Nanjing Jiangsu Province China Six sections in each rat were randomly selected to calculate the mean absorbance value in eight fields of view 2 cm 2 cm Statistical analysis Data are expressed as mean SD and were analyzed using SPSS 17 0 software SPSS Chicago IL USA Differences between the groups were compared with one way analysis of variance and the StudentNewman Keuls test A value of 0 05 was considered a statistically significant difference Research background The proliferation of glial scar formation is closely linked with spatial learning and memory defects in neonatal rats after hypoxic ischemic brain damage Hyperbaric oxygen therapy can reduce hippocampal neuronal loss and improve cognitive function in rats Research frontiers Hydrogen magnetic resonance spectroscopy imaging techniques have been used for observations of brain tissue metabolism and cognitive function changes in mul sections was stained with cresyl violet for 20 minutes rinsed with distilled water for 5 minutes and differentiated in 75 and 95 ethanol for 1 minute The differentiation was controlled under endoscopy and was terminated when the background was clean and Nissl bodies were clearly visible After differentiation sections were rapidly immersed in ethanol for dehydration xylene transparency and mounting Nissl bodies in the cytoplasm of hippocampal CA3 nerve cells were observed under optical microscope Leica sease and other diseases The role of hydrogen ion magnetic resonance spectroscopy in dynamic observation of hyperbaric oxygen therapy on brain injury is rarely reported Clinical significance This study was the first to observe changes of hippocampus metabolites in rats with traumatic brain injury at different courses of hyperbaric oxygen therapy using hydrogen ion magnetic resonance spectroscopy This was a broad attempt to provide evidence for understanding the effect of hyperbaric oxygen therapy in traumatic brain injury Immunofluorescence staining of glial fibrillary acidic protein expression in the rat hippocampal CA3 region Sections adjacent to the stained sections were rinsed blocked and incubated with 8 normal goat serum for 1 hour After the serum was discarded sections were incubated with mouse anti rat glial fibrillary acidic protein monoclonal antibody Millipore Corporation Billerica MA USA at 4 C overnight and Alexa Fluor 595 labeled goat anti mouse antibody Invitrogen Carlsbad CA USA 1 1 000 at room temperature for 1 hour Then sections were mounted with 50 glycerol Between each step Academic terminology Magnetic resonance spectroscopy the only non invasive technique for the determination of certain chemical compositions in tissue it is the product of magnetic resonance imaging and magnetic resonance spectroscopy and it provides another functional analysis and diagnostic method in addition to magnetic resonance imaging Peer review This study observed the correlation between changes of hippocampal CA3 neurons and expression of glial fibrillary acidic protein in rats after hyperbaric oxygen therapy In addition the potential mechanism underlying hyperbaric oxygen therapy on improving cognitive functions was analyzed These 3341
experimental findings provide a reliable theoretical basis for choosing an optimal hyperbaric oxygen therapy scheme for the clinical treatment of brain injury REFERENCES 1 2 3 4 5 6 7 8 9 10 11 12 13 14 3342 Flanagan SR Cantor JB Ashman TA Traumatic brain injury future assessment tools and treatment prospects Neuropsychiatr Dis Treat 2008 4 5 877 892 Broomhall LG Clark CR McFarlane AC et al Early stage assessment and course of acute stress disorder after mild traumatic brain injury J Nerv Ment Dis 2009 197 3 178 181 Bales JW Wagner AK Kline AE et al Persistent cognitive dysfunction after traumatic brain injury A dopamine hypothesis Neurosci Biobehav Rev 2009 33 7 981 1003 Fujimoto ST Longhi L Saatman KE et al Motor and cognitive function evaluation following experimental traumatic brain injury Neurosci Biobehav Rev 2004 28 4 365 378 Thom SR Hyperbaric oxygen its mechanisms and efficacy Plast Reconstr Surg 2011 127 1 131S 141S Lin KC Niu KC Tsai KJ et al Attenuating inflammation but stimulating both angiogenesis and neurogenesis using hyperbaric oxygen in rats with traumatic brain injury J Trauma Acute Care Surg 2012 72 3 650 659 Rockswold SB Rockswold GL Zaun DA et al A prospective randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism intracranial pressure and oxygen toxicity in severe traumatic brain injury J Neurosurg 2010 112 5 1080 1094 Palzur E Zaaroor M Vlodavsky E et al Neuroprotective effect of hyperbaric oxygen therapy in brain injury is mediated by preservation of mitochondrial membrane properties Brain Res 2008 1221 126 133 Pang HP Wu GY Progress in the research of functional magnetic resonance imaging in traumatic brain injury Fangshexue Shijian 2010 12 25 12 15 Jansen JF Backes WH Nicolay K et al 1H MR spectroscopy of the brain absolute quantification of metabolites Radiology 2006 240 2 318 332 Kirov II Tal A Babb JS et al Serial proton MR spectroscopy of gray and white matter in relapsing remitting MS Neurology 2013 80 1 39 46 Giorgio A De Stefano N Cognition in multiple sclerosis relevance of lesions brain atrophy and proton MR spectroscopy Neurol Sci 2010 31 Suppl 2 S245 248 Metarugcheep P Hanchaiphiboolkul S Viriyavejakul A et al The usage of proton magnetic resonance spectroscopy in Parkinson s disease J Med Assoc Thai 2012 95 7 949 952 Nie K Zhang Y Huang B et al Marked N acetylaspartate and choline metabolite changes in Parkinson s disease patients with mild cognitive impairment Parkinsonism Relat Disord 2013 19 3 329 334 15 Churchill S Weaver LK Deru K et al A prospective trial of hyperbaric oxygen for chronic sequelae after brain injury HYBOBI Undersea Hyperb Med 2013 40 2 165 193 16 Huang Z Liu J Cheung PY et al Long term cognitive impairment and myelination deficiency in rat model of perinatal hypoxic ischemic brain injury Brain Res 2009 1301 100 109 17 Wang GH Zhang XG Jiang ZL et al Neuroprotective effects of hyperbaric oxygen treatment on traumatic brain injury in the rat J Neurotrauma 2010 27 9 1733 1743 18 Shlosberg D Benifla M Kaufer D et al Blood brain barrier breakdown as a therapeutic target in traumatic brain injury Nat Rev Neurol 2010 6 7 393 403 19 Werner C Engelhard K Pathophysiology of traumatic brain injury Br J Anaesth 2007 99 1 4 9 20 Wolf G Cifu D Baugh L et al The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury J Neurotrauma 2012 29 17 2606 2612 21 Vlodavsky E Palzur E Soustiel JF Hyperbaric oxygen therapy reduces neuroinflammation and expression of matrix metalloproteinase 9 in the rat model of traumatic brain injury Neuropathol Appl Neurobiol 2006 32 1 40 50 22 Hayakawa T Kanai N Kuroda R et al Response of cereborspinal fluid pressure to hyperbaric oxygenation J Neurol Neurosurg Psychiatry 1971 34 5 580 586 23 Fu M Zhao H Zhang LD et al Effects of hyperbaric oxygen therapy on the brain trauma injury in rabbits with magnetic resonance imaging Zhongguo hanghaiyixue yu Gaoqiya Yixue Zazhi 2011 18 2 82 85 24 Vlodavsky E Palzur E Feinsod M et al Evaluation of the apoptosis related proteins of the BCL 2 family in the traumatic penumbra area of the rat model of cerebral contusion treated by hyperbaric oxygen therapy a quantitative immunohistochemical study Acta Neuropathol 2005 110 2 120 126 25 Liu Z Jiao QF You C et al Effect of hyperbaric oxygen on cytochrome C Bcl 2 and Bax expression after experimental traumatic brain injury in rats Chin J Traumatol 2006 9 3 168 174 26 Daugherty WP Levasseur JE Sun D et al Effects of hyperbaric oxygen therapy on cerebral oxygenation and mitochondrial function following moderate lateral fluidpercussion injury in rats J Neurosurg 2004 101 3 499504 27 Gossett WA Rockswold GL Rockswold SB et al The safe treatment monitoring and management of severe traumatic brain injury patients in a monoplace chamber Undersea Hyperb Med 2010 37 1 35 48 28 Zhang XG Wang GH Li YC et al The influences of hyperbaric oxygen on the oxidative stress variables and pro anti inflammatory cytokines in rats after traumatic brain injury Chin J Appl Physiol 2010 26 3 373 375 29 Barkovich AJ Baranski K Vigneron D et al Proton MR spectroscopy for the evaluation of brain injury in asphyxiated term neonates AJNR Am J Neuroradiol 1999 20 8 1399 1405
30 Xu S Zhuo J Racz J et al Early microstructural and metabolic changes following controlled cortical impact injury in rat a magnetic resonance imaging and spectroscopy study J Neurotrauma 2011 28 10 2091 2102 31 Vagnozzi R Signoretti S Cristofori L et al Assessment of metabolic brain damage and recovery following mild traumatic brain injury a multicentre proton magnetic resonance spectroscopic study in concussed patients Brain 2010 133 11 3232 3242 32 Du Y Li Y Lan Q 1H Magnetic resonance spectroscopy correlates with injury severity and can predict coma duration in patients following severe traumatic brain injury Neurol India 2011 59 5 679 684 33 Carpentier A Galanaud D Puybasset L et al Early morphologic and spectroscopic magnetic resonance in 34 35 36 37 38 39 40 otrauma 2006 23 5 674 685 Zhou H Lu WJ Teng GJ et al The study of cognitive function and proton magnetic resonance spectroscopy on hippocampus in patients with type 2 diabetes mellitus Linchuang Yixue Yingxiang Jishu 2009 25 8 1367 1370 Sun YA He XB Miao CC et al Magnetic resonance spectroscopy in evaluating hippocampus changes of patients with mild cognitive impairment Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu 2009 13 26 5098 5103 Lucetti C Del Dotto P Gambaccini G et al Proton magnetic resonance spectroscopy 1H MRS of motor cortex and basal ganglia in de n Neurol Sci 2001 22 1 69 70 Lei Z Deng P Li J et al Alterations of A type potassium channels in hippocampal neurons after traumatic brain injury J Neurotrauma 2012 29 2 235 245 Signoretti S Marmarou A Aygok GA et al Assessment of mitochondrial impairment in traumatic brain injury using high resolution proton magnetic resonance spectroscopy J Neurosurg 2008 108 1 42 52 Wang HZ Qiu SJ Lv XF et al Diffusion tensor imaging and 1H MRS study on radiation induced brain injury after nasopharyngeal carcinoma radiotherapy Clin Radiol 2012 67 4 340 345 Semenova NA Sidorin SV Akhadov TA et al Effect of cell therapy on metabolite content in brain structures of children with consequences of severe brain injury 1H magnetic resonance spectroscopy study Bull Exp Biol Med 2011 151 4 532 535 41 42 43 44 45 46 47 48 Faster metabolite 1 h transverse relaxation in the elder human brain PLoS One 2013 8 10 Nicola SD Balestr P Dotti MT et al Severe metabolite abnormalities in the white matter of patients with vacuolating megalencephalic leukoencephalopathy with subcortical cyst a proton spectroscopic imaging study J Neurol 2001 248 5 403 409 Ye B Huang HP Che CH et al Correlation analysis of cognitive function and changes in proton magnetic resonance spectroscopy of the hippocampus in patients with complex partial seizures Zhonghua Shenjing Yixue Zazhi 2010 9 2 158 161 Li D Li P He Z et al Human intravenous immunoglobulins suppress seizure activities and inhibit the activation of GFAP positive astrocytes in the hippocampus of picrotoxin kindled rats Int J Neurosci 2012 122 4 200 208 Vartak Sharma N Ghorpade A Astrocyte elevated gene 1 regulates astrocyte responses to neural injury implications for reactive astrogliosis and neurodegeneration J Neuroinflammation 2012 9 195 Barreto G White RE Ouyang Y et al Astrocytes targets for neuroprotection in stroke Cent Nerv Syst Agents Med Chem 2011 11 2 164 173 Sandhir R Onyszchuk G Berman NE Exacerbated glial response in the aged mouse hippocampus following controlled cortical impact injury Exp Neurol 2008 213 2 372 380 Liu S Shen GY Wu QF et al The effects of rehabilitative training on neural function and the expression of glial fibrillary acidic protein and ionized calcium binding adaptor molecule 1 after traumatic brain injury Zhonghua Wuli Yixue yu Kangfu Zazhi 2008 34 6 415 420 49 Republic of China Guidance Suggestions for the Care and Use of Laboratory Animals 2006 09 30 50 Feeney DM Boyeson MG Linn RT et al Responses to cortical injury I Methodology and local effects of contusions in the rat Brain Res 1981 211 1 67 77 Reviewed by James K Frenchman B Peng ZR Sun XJ Edited by Wang J Yang Y Li CH Song LP Liu WJ Zhao M 3343
ORIGINAL RESEARCH published 27 September 2017 doi 10 3389 fnint 2017 00025 Hyperbaric Oxygen Environment Can Enhance Brain Activity and Multitasking Performance Dor Vadas 1 Leonid Kalichman 2 Amir Hadanny 3 4 5 and Shai Efrati 3 4 6 1 The Israeli Rehabilitation Center for Stroke and Brain Injury Rehovot Israel 2 Department of Physical Therapy Faculty of Health Sciences Recanati School for Community Health Professions Ben Gurion University of the Negev BeerSheva Israel 3 Sagol Center for Hyperbaric Medicine and Research Asaf Harofeh Medical Center Zerifin Israel 4 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 5 Galilee Faculty of Medicine Bar Ilan University Ramat Gan Israel 6 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Background The Brain uses 20 of the total oxygen supply consumed by the entire body Even though
Vadas et al Oxygen and Maximal Brain Performance INTRODUCTION MATERIALS AND METHODS The brain is the body s largest consumer of oxygen utilizing roughly 20 of the total oxygen and consuming 25 30 of the total glucose Lennie 2003 Even though
Vadas et al Oxygen and Maximal Brain Performance RESULTS 100 oxygen for 45 min In the control session in order to manipulate the participants the chamber pressure was increased for less than a minute so they felt some pressure in the ears and a flow of 21 oxygen was used for the masks The tests tasks were initiated 30 min after the masks were on within the chamber Cognitive performance was evaluated by a symbol digit test example in Appendix 1 and the motor performance was evaluated by the units of beans that were transferred from a plate to a cup One of the tasks in the motor assessment scale testMASS Appendix 2 The dual tasking was a combination of the cognitive and the motor tests which were done simultaneously Twenty four healthy participants signed an informed consent and were included in the study Two patients were excluded One did not complete the crossed evaluation as required by study protocol and the other could not adjust to the hyperbaric conditions Accordingly a total of 22 healthy volunteers were included in the final analysis 11 females and 11 males age 22 68 years mean 42 13 years with 12 30 education years at the time of the study mean 16 4 years Baseline participant characteristics are summarized in Table 1 The results of the cognitive and the motor tests are summarized in Table 2 A significant performance decline was observed in all tests scores when performed dual tasks compared to single tasks in both normobaric and HBO environments p 0 001 for both The SDMT cognitive task was considered the primary task and the motor task was considered the distraction when we analyzed the dual task performance at the two different environments SDMT scores the number of correct answers minus the incorrect answers in the test were significantly increased when performed under the HBO environment compared to the normobaric environment Table 2 Figures 2 4 The improvement in SDMT in the HBO environment was significant when tested either as a single 43 9 11 6 vs 40 2 9 8 p 0 001 Figure 2 or as a dual task 38 7 11 7 vs 35 2 10 8 p 0 006 Figure 3 Motor task scores were also significantly increased when performed under the HBO environment compared to the normobaric environment The improvement in the motor task results or the number of bean units that were transferred from the plate to the cup under the HBO environment was significantly higher either as a single 83 8 9 3 vs 89 3 11 5 p 0 001 or as a dual task 51 4 14 7 vs 56 14 2 p 0 029 Cognitive Attention Symbol Digit Modality Test SDMT The symbol digit modalities test SDMT Appendix 1 is a test used to assess divided attention visual scanning tracking and motor speed Strauss et al 2006 In this test participants are presented with series of symbols each indicates a different number While they are repeatedly presented with those different symbols they are asked to write the adequate number next to each symbol the Appendix includes an example of the task recoding The test was found to be reliable in four different forms in healthy and cognitive impaired conditions McCaffrey 1988 Hinton Bayre and Geffen 2005 Dickinson et al 2007 Paramenter 2007 Three different forms of the SDMT were used in each evaluation session The first was a try out for the test ensuring that the task was understood The second tested the ability to perform an individual task The third form was used in combination of the motor task for examining dual task performance Standard administration procedures were followed as indicated in the test manual Smith 1973 The score of the test is the number of correct substitutions during a 90 s interval Motor Task Transferring of Beans Motor performance was evaluated by the motor assessment scale test MAS Appendix 2 transferring individual beans between two tea cups an arm s length away The MAS test was found to be reliable for assessing advance hand motor functioning in post stroke patients Carr 1985 Pool and Whiteny 1988 One of the advantages of this task is that during its performance the participant is not required to have full vision focus on the hands allowing the participant to do other tasks In addition the test can be easily performed under the conditions inside a hyperbaric chamber The MAS score is based on the number of beans that were successfully transferred in the given time 90 s TABLE 1 Patient baseline characteristics All participants Number of participants Gender Statistical Analysis Female 11 Male 11 Age 42 13 Years of education 16 3 4 TABLE 2 Cognitive and motor task scores Statistical analysis was done using SPSS software version 22 0 Continuous data are expressed by mean STD standard deviation and compared by an independent t test for intergroup comparison and by a paired t test for intra group comparison P values 0 05 were considered statistically significant All randomly allocated patients were included in the safety analysis and those that went through all the assessments were included in the efficacy analyses Frontiers in Integrative Neuroscience www frontiersin org 22 General 3 Room air Hyperbaric oxygen Single task Cognitive 40 2 9 8 43 9 11 6 P 0 001 Dual task Cognitive 35 2 10 8 38 7 11 7 P 0 006 Single task Motor 83 8 9 3 89 3 11 5 P 0 001 Dual task Motor 51 4 14 7 56 14 2 P 0 029 P value September 2017 Volume 11 Article 25
Vadas et al Oxygen and Maximal Brain Performance FIGURE 2 Cognitive single task during hyperbaric oxygen compared to normal environments SDMT Symbol Digit Modality Test FIGURE 4 General cognitive score during hyperbaric oxygen compared to normal environment SDMT Symbol Digit Modality Test exposure the immediate effect on neuro cognitive performance cannot be related to the neuroplasticity effects of HBO but rather to a limiting factor preventing the brain to function at a higher capacity This finding means that oxygen is indeed a limiting factor for brain performance at standard conditions in healthy human beings The minimal effective dosages of pressure and oxygen concentration are still unknown and future studies are needed to test this issue by evaluating the optimal case specific dose response curves Efrati and Ben Jacob 2014 There is a huge variability in HBO dosages 1 3 2 4 ATA used in previous studies aimed to induce neuroplasticity in post stroke and TBI patients Boussi Gross et al 2013 Efrati and Ben Jacob 2014 Tal et al 2015 Hadanny and Efrati 2016 Oxygen is not a drug and because it is mainly metabolized in the mitochondria its pharmacodynamics varies greatly from patient to patient Thus no simple dose response curve has been defined so far Emphasizing the latter there are many case reports illustrating the significant effect of relatively low increases in air pressure Golding et al 1960 Austin 1998 For example the Dead Sea altitude 402 m below sea level 1 05 ATM can serve as a good model for a relatively low hyperbaric environment The beneficial effect of this slight increase in air partial pressure is well known and was studied and evaluated in different populations Kramer et al 1998 Falk et al 2006 Goldbart et al 2007 With respect to the current study the aim was to confirm that oxygen is indeed a rate limiting factor for enhancing the activity and not to investigate the minimal effective dosage oxygen For that purpose we chose to use 100 oxygen at 2 ATA as the challenge dose Now that we have demonstrated that indeed oxygen is a limiting factor further studies are needed to evaluate the dose response curve related to enhancing brain cognitive performance In today s modern life there is an increased need for multitasking which is unfortunately limited Carrier et al 2009 The inability to perform well while multitasking could have severe and even life threatening consequences as was FIGURE 3 Cognitive score during dual task during hyperbaric oxygen compared to normal environments SDMT Symbol Digit Modality Test DISCUSSION The study s findings indicate that even for healthy individuals oxygen at normal conditions is a limiting factor for brain activity The ability to perform cognitive and or motor tasks as a single or a combined task multitask was evaluated at a normal air oxygen environment and at HBO a hyperbaric oxygen enriched environment Increasing oxygenation using a HBO environment significantly enhanced both cognitive and motor performance Significant improvements were found for both single tasks as well as simultaneous multiple tasks Many studies have confirmed that environments low in oxygen levels have a negative effect on performing single and multiple tasks Shukitt Hale et al 1998 Lieberman et al 2005 A study performed by Yu et al evaluated the effect of repeated exposure to HBO treatment for healthy individuals Yu et al 2015 Their study demonstrates that repeated daily HBO sessions 5 days per week 80 min with 100 at 2 ATA can enhance memory performance The improved memory correlated with enhanced functional connectivity in the left hippocampus right inferior frontal and lingual gyri as demonstrated by fMRI analysis Yu et al 2015 In the current study the immediate effect of a single HBO environment exposure was evaluated in healthy volunteers Since it is a single Frontiers in Integrative Neuroscience www frontiersin org 4 September 2017 Volume 11 Article 25
Vadas et al Oxygen and Maximal Brain Performance found in emergency room care physicians Chisholm et al 2000 and in military drone pilots Shanker and Richtel 2011 Considering that an oxygen enriched environment could enhance performance improve multitasking and decision making the use of this environment could have a significant impact for those who needs it However before being used for large scale populations the minimal and maximal effective dosage should be evaluated In addition to immediately enhancing brain cognitive functions there is growing convincing evidence that HBO therapy can revitalize chronically damage brain tissue in patients suffering from chronic neuro cognitive impairment due to TBI stroke or anoxic brain damage even years after the acute insult Boussi Gross et al 2013 Efrati et al 2013 Efrati and Ben Jacob 2014 Hadanny et al 2015 Tal et al 2015 Hadanny and Efrati 2016 As detailed above brain metabolism reaches its upper limit of oxygen consumption even at normal healthy conditions which makes it dependent on cerebral blood flow CBF for its oxygen supply After brain insults when the CBF is compromised there is a further decrease in oxygen delivery to the injured brain tissue and oxygen becomes a limiting factor for brain recovery Hadanny and Efrati 2015 Consequently achieving higher tissue oxygen delivery by using higher paO2 is crucial for maintaining the sufficient oxygenation needed for the damaged brain tissue Hadanny and Efrati 2015 Clinical studies published in recent years present convincing evidences that HBO therapy HBOT can assist in brain repair BoussiGross et al 2013 2015 Efrati and Ben Jacob 2014 In addition to delivering sufficient oxygen to the brain for tissue repair HBOT might initiate cellular and vascular repair mechanisms and improve cerebral vascular flow Efrati and Ben Jacob 2014 At the cellular level HBOT can improve mitochondrial function in both neurons and glial cells improve blood brain barrier and inflammatory reactions reduce apoptosis alleviate oxidative stress increase levels of neutrophils and nitric oxide and upregulate axon guidance agents Efrati and Ben Jacob 2014 Moreover the effects of HBOT on neurons can be mediated indirectly by glial cells including astrocytes Efrati and Ben Jacob 2014 HBOT may also promote neurogenesis of the endogenous neural stem cells Efrati and Ben Jacob 2014 At the vascular level HBOT was found to have a role in initiating and or facilitating angiogenesis and cell proliferation needed for axonal regeneration Efrati and Ben Jacob 2014 Another potential effect of HBOT may be its possible contribution to perception Perception provides meaning for sensation Mendez Balbuena et al has shown that by providing audio tactile stimulation the sensory experience perception of vision could be expended Mendez Balbuena et al 2015 It might be possible that enhanced brain activity by HBOT may also increase sensory perception However it was not directly evaluated in the current study and it could be an interesting goal for additional studies The current study has several challenges and potential limitations One important limitation relates to the test re test learning effect due to the crossover design Every participant has performed the tests twice under both conditions in separate sessions To overcome this limitation participants were randomly divided into two groups in a way that part of the participants started under the HBO environment and the other part started with the sham environment normobaric with room air Accordingly the two groups are almost matched for their learning effect The other challenge is related to generating the control intervention that would mimic hyperbaric environment where participants can sense the increased pressure in their ears To overcome this challenge the chamber pressure was increased and then gradually decreased during the control session so that the participants felt some pressure in their ears and a flow of 21 oxygen was used for the masks The tests tasking were initiated 30 min after the masks were on within the chamber and the pressure at that time was already reduced back to sea level during the placebo session CONCLUSION The improvement in performance of both single and multitasking while in a HBO environment supports the hypothesis that oxygen is indeed a rate limiting factor for brain activity Hyperbaric oxygenation can serve as an environment for enhancing brain performance Such a brain enhancing environment can be of significant importance when many skills are becoming more and more dependent on enhanced cognitive functions and multitasking Further studies are needed to evaluate the optimal oxygen performance relation for maximal brain performance AUTHOR CONTRIBUTIONS All authors listed have made a substantial direct and intellectual contribution to the work and approved it for publication SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at http journal frontiersin org article 10 3389 fnint 2017 00025 full supplementary material REFERENCES Boussi Gross R Shlamkovitch N Golan H Fishlev G Bechor Y Volkov O et al 2013 Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury randomized prospective trial PLoS ONE 8 e79995 doi 10 1371 journal pone 0079995 Carr J H 1985 Investigation of a new motor assessment scale for stroke patients J Am Phys Ther Assoc 65 175 180 doi 10 1093 ptj 65 2 175 Carrier L M Cheever N A Rosen L D Benitez S and Chang J 2009 Multitasking across generations multitasking choices and difficulty ratings Austin D 1998 Gammow bag for acute mountain sickness Lancet 52 325 326 doi 10 1016 S0140 6736 05 78781 X Boussi Gross R Golan H Volkov O Bechor Y Hooflen D Schnaider Beeri M et al 2015 Improvement of memory impairments in poststroke patients by hyperbaric oxygen therapy Am Psychol Assoc 29 610 621 doi 10 1037 neu0000149 Frontiers in Integrative Neuroscience www frontiersin org 5 September 2017 Volume 11 Article 25
Vadas et al Oxygen and Maximal Brain Performance McCaffrey R J 1988 A comparison of the trail making test symbol digit modalities test and the Hooper visual organization test in an inpatient substance abuse population Arch Clin Neurospsychol 3 181 187 doi 10 1093 arclin 3 2 181 Mendez Balbuena I Huidobro N Silva M Flores A Trenado C et al 2015 Effect of mechanical tactile noise on amplitude of visual evoked potencial multisensory stochastic resonance J Neurophysiol 114 2132 2143 doi 10 1152 jn 00457 2015 Mortazavi A Eisenberg M Langleben D Ernst P and Schiff R 2003 Altitude related hypoxia risk assessment and management for passen aircraft Aviat Space Environ Med 74 922 927 Moss M C and Scholey A B 1996 Oxygen administration enhanses memory formation in healthy young adults Psychopharmacology 124 255 260 doi 10 1007 BF02246665 Paramenter B 2007 Screening for cognitive impairment in multiple sclerosis using the Symbol digit modalities test Mult Scler 13 52 57 doi 10 1177 1352458506070750 Pool J L and Whiteny S 1988 Motor assessment scale for stroke patients concurrent validity and interrater reliability Arch Phys Med Rehabil 69 195 197 Shanker T and Richtel M 2011 In New Military Data OverLoad Can Be Deadly New York NY New York Times Shukitt Hale B Banderet L F and Louis H R 1998 Elevation dependent symptom mood and performance changes produced by exposure to hypobaric hypoxia Int J Aviat Psychol 8 319 334 doi 10 1207 s15327108ijap0804_1 Smith A 1973 Symbol Digit Modaity Test Los Angeles CA Western Psychological Services Sokoloff L Mangold R Wechsler R L Kennedy C and Kety S S 1955 The effect of mental arithmetic on cerebral circulation and metabolism Clin Investig 34 7 Pt 1 1101 1108 doi 10 1172 JCI103159 Spelke E Hirst W and Neosser U 1976 Skills of diveded attention Cognition 4 215 230 doi 10 1016 0010 0277 76 90018 4 Strauss E Sherman E M S and Spreen O A C 2006 Psychological Tests Administration Norms and Commentary 3rd Edn Oxford University Press Tal S Hadanny A Berkovits N Sasson E Ben Jacob E and Efrati S 2015 Hyperbaric oxygen may induce angiogenesis in patients suffering from prolonged post concussion syndrome due to traumatic brain injury Restor Neurol Neurosci 33 943 951 doi 10 3233 RNN 1 50585 Tombu M N Asplund C L Dux P E Godwin D and Martin J W 2011 A unified attentional bottleneck in the human brain Proc Natl Acad Sci U S A 118 13426 13431 doi 10 1073 pnas 1103583108 West J B 2002 Commuting to high altitude value of oxygen enrichment of room air High Altitude Med Biol 3 223 235 doi 10 1089 15270290260131948 West J B 2003 Improving oxygenation at high altitued acclimatization and O2 enrichment High Alt Med Biol 3 389 394 doi 10 1089 1527029037691 92340 Yu R Wang B Shumei L Junging W Feng Z Shufang C et al 2015 Cognitive enhancement of healthy young adults with hyperbaric oxygen a preliminary resting state fMRI study Clin Neurophysiol 126 2058 2067 doi 10 1016 j clinph 2015 01 010 Zauner A 2002 Brain oxygenation and energy metabolism part 1 biological function Neurosurgery 51 289 302 doi 10 1227 00006123 200208000 00003 in three generations of Americans Comput Hum Behav 25 483 489 doi 10 1016 j chb 2008 10 012 Chisholm C D Collison E K Nelson D R and Cordell W H 2000 Emergency department workplace interruptions are emergency physicians Interrupt driven and Multitasking Acad Emerg Med 7 1239 1243 doi 10 1111 j 1553 2712 2000 tb00469 x Choi M H Kim J H Kim H J Choi J S Yi Jeong H and Chung S C 2013 Correlation between cognitive ability measured by responsetime of 1 back task and changes of SpO2 by supplying three different levels of oxygen in the elderly Gerontology 13 384 387 doi 10 1111 j 1447 0594 2012 00911 x Dickinson D Ramsey M E and Gold J M 2007 Overlooking the obvious A meta analytic comparison of Digit Symbol Coding tasts and other cognitive measures in schizophrenea Arch Gen Psychiatry 64 532 542 doi 10 1001 archpsyc 64 5 532 Donohue S E James B Eslick A N and Mitroff S R 2012 Cognitive pitfall Videogame players are not immunme to dual task costs Atten Percept Psychophys 4 803 809 doi 10 3758 s13414 012 0323 y Efrati S and Ben Jacob E 2014 Reflections on the neurotherapeutic effects of hyperbaric oxygen Expert Rev Neurother 14 233 236 doi 10 1586 14737175 2014 884928 Efrati S Fishlve G Bechor Y Volkov O Bergan J Kiakhandler K et al 2013 Hyperbaric oxygen induces late neuroplasticity in post stroke patients randomized prospective trial PLoS ONE 8 e53716 doi 10 1371 journal pone 0053716 Falk B Nini A Zigel L Yahav Y Aviram M Rivlin J et al 2006 Effect of low altitude at the Dead Sea on exercise capacity and cardiopulmonary response to exercise in cystic fibrosis patients with moderate to severe lung disease Pediatr Pulmonol 41 234 241 doi 10 1002 ppul 20342 Goldbart A Cohen A Weitzman D and Tal A 2007 Effects of rehabilitation winter camps at the Dead Sea on European cystic fibrosis patients Isr Med Assoc J 9 806 809 Golding F C Griffiths P Hempleman H V Paton W D M and Walder D N 1960 Decompression sickness during construction of the dartford tunnel Occup Environ Med 17 167 180 doi 10 1136 oem 17 3 167 Hadanny A and Efrati S 2015 Oxygen a limiting factor for brain recovery Crit Care 19 307 doi 10 1186 s13054 015 1034 2 Hadanny A and Efrati S 2016 Treatment of persistent postconcussion syndrome due to mild traumatic brain injury current status and future directions Expert Rev Neruother 8 875 887 doi 10 1080 14737175 2016 1205487 Hadanny A Golan H Fishlev G Bechor Y Volkov O Suzin G et al 2015 Hyperbaric oxygen can induce neuroplasticity and improve cognitive functions of patients suffering from anoxic brain damage Restor Neurol Neurosci 33 471 486 doi 10 3233 RNN 150517 Han S W and Marois R 2013 The source of dual task limitation serial or parallel processing of multiple response selection Atten Percept Psychophys 75 1395 1405 doi 10 3758 s13414 013 0513 2 Hinton Bayre A and Geffen G 2005 Comparability reliability and practice effects on alternate forms of the digit symbol substitution and symbol digit modalities test Psychol Assess 17 237 241 doi 10 1037 1040 3590 17 2 237 Kramer M R Springer C Berkman N Glazer M Bublil M Bar Yishay E et al 1998 Rehabilitation of hypoxemic patients with COPD at low altitude at the Dead Sea the lowest place on earth Chest 113 571 575 doi 10 1378 chest 113 3 571 Lennie P 2003 The copst of cortical computation Curr Biol 13 493 497 doi 10 1016 S0960 9822 03 00135 0 Lieberman P Morney A Hochstadt J Larson M and Mather S 2005 Mount everest A space analogue for speech monitoring of cognitive deficit and stress Aviat Space Environ Med 76 198 207 Malle C Quinette P Laisney M Bourrilhon C Boissin J Desgranges B et al 2013 Working memory impairment in pilots exposed to acute hypobaric hypoxia Aviat Space Environ Med 84 773 779 doi 10 3357 ASEM 3482 2013 Frontiers in Integrative Neuroscience www frontiersin org Conflict of Interest Statement The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest Copyright 2017 Vadas Kalichman Hadanny and Efrati This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY The use distribution or reproduction in other forums is permitted provided the original author s or licensor are credited and that the original publication in this journal is cited in accordance with accepted academic practice No use distribution or reproduction is permitted which does not comply with these terms 6 September 2017 Volume 11 Article 25
Parkinson s and HBOT Parkinson s disease or PD is a disorder of the central nervous system that impairs motor skills speech and other mental functions PD belongs to a group called movement disorders These disorders typically produce muscle rigidity tremor and a general slowing of physical movement PD affects adults of all ages but is not considered fatal However late stage Parkinson s may lead to choking pneumonia or serious falls all of which can cause death or disability What HBOT can do The symptoms of Parkinson s can vary in type and severity therefore it can be difficult to predict results Often HBOT has been discovered effective by accident as in the case where a diabetic patient tried HBOT for a foot ulcer but found that the treatment vastly improved his Parkinson s symptoms After 50 years of HBOT treatment we do know that hyperbaric oxygen will not worsen PD Numerous animal studies have shown that HBOT works as an anti inflammatory and may be used in this way to alleviate the symptoms of PD Why is Parkinson s Disease amenable to oxygen therapy Extensive animal research has demonstrated a non specific chronic inflammatory condition in the substantia nigra of the brain Hyperbaric Oxygen Therapy HBOT has been shown to be an anti inflammatory drug in many conditions Anecdotal evidence of many patients with well established PD have been treated with HBOT for other conditions such as diabetic foot ulcers For example a patient with advanced PD who is confined to a wheelchair may get up and walk across the room after a series of HBOT What benefits can I expect from oxygen therapy for Parkinson s Disease Since every patient is different it is hard to predict the result in each individual case However we know from 50 years of experience that HBOT is safe and will not make the patient worse The usual course of oxygen therapy is once daily five days a week M F for eight weeks If a significant response is noted after 40 HBOT additional treatments may be helpful One Two Punch Glutathione and HBOT Julian Whitaker MD Parkinson s disease is caused by the degeneration of neurons in the area of the brain that manufactures dopamine a neurotransmitter that affects movement As dopamine production drops characteristic tremors and speech balance and motor problems develop The primary treatment for Parkinson s is drugs that replace or mimic dopamine and though these meds improve symptoms they do not slow disease progression and their side effects increase with long term use Although there s a lot that medical science does not know about Parkinson s we do know that free radical damage contributes to its progressive nature That s why we use glutathione Glutathione HBOT to the Rescue Glutathione is a powerful natural antioxidant and patients with Parkinson s have dangerously low levels of glutathione in the affected area of the brain Boosting stores of this protective antioxidant not only guards against further damage it also enhances the function of surviving neurons
Unfortunately oral glutathione has a hard time crossing the blood brain barrier so supplements aren t very helpful When glutathione is infused intravenously however it hits its target Most patients see dramatic improvements after just a handful of treatments and many perk up after their first infusion Even better studies suggest that benefits last for two to four months after a treatment course Our patients with Parkinson s disease are also treated with hyperbaric oxygen therapy HBOT is highly beneficial for stroke multiple sclerosis and brain injuries It floods the brain with oxygen slows neuronal degeneration mobilizes rejuvenating stem cells and enhances angiogenesis the growth of new blood vessels that nurture damaged areas It is the combination of these two treatments working synergistically that provides such remarkable results Serious Condition Serious Intervention Parkinson s is a serious condition that requires serious intervention Coenzyme Q10 vitamin E fish oil curcumin creatine and vitamin D along with N acetyl cysteine and vitamin C both of which boost glutathione levels show promise in improving symptoms and even slowing progression I certainly recommend taking them However these supplements do not come close to approaching the therapeutic power of IV glutathione and HBOT Sadly very few medical facilities offer these therapies In fact many physicians don t know a thing about them Furthermore although benefits are enduring they don t last forever and maintenance treatments are required for optimal function I don t know what it s going to take to get conventional physicians to embrace IV glutathione and HBOT but don t hold your breath waiting for your doc to come around I strongly urge you to find a treatment center near you and if you can t consider coming to the Whitaker Wellness Institute Recommendations The suggested daily doses of supplements for Parkinson s disease are coenzyme Q10 a minimum of 1 200 IU vitamin E 400 800 IU fish oil 6 8 g curcumin 1 000 2 000 mg creatine 10 g vitamin D 2 000 4 000 IU N acetyl cysteine 1 200 1 800 mg and vitamin C 1 000 2 000 mg Look for them in your health food store or call 800 810 6655 to order Take in divided doses References Hoggard M et al Hyperbaric oxygen treatment on a Parkinson s disease patient a case study Proceedings of the 14th International Congress of Hyperbaric Medicine San Francisco CA 2002 Sechi G et al Reduced intravenous glutathione in the treatment of early Parkinson s disease Prog Neuropsychopharmacol Biol Psychiatry 1996 Oct 20 7 1159 1170 Modified from Health Healing with permission from Healthy Directions LLC Photocopying reproduction or quotation strictly prohibited without written permission from the publisher Hyperbaric Oxygenation During the Complex Treatment of Parkinsonism V Ya Neretin M A Lobov S V Kotov G F Cheskidova G S Mo1chanova and 0 G Safronova Neurology Department headed by Prof V Ya Neretin M F Viadimirsky Regional Research Institute of Clinical Medicine Director G A Onopriyenko Moscow Hyperbaric oxygenation HBO2 was used to treat 64 patients suffering from parkinsonism of diverse etiology HBO2 sessions were provided daily 8 12 per course treatment pressure ranged from 1 3 to 2 atm and exposure time ranged
from 40 to 60 minutes A marked beneficial effect was noted in 55 patients HBO2 treatment produced better results in the presence of vascillar parkinsonism in patients under 65 years of age and when the history of disease ranged from 1 to 5 years The akineticorigid syndrome regressed to a greater extent with HBO2 proving to be less effective when trembling hyperkinesis was present Submitted to the editorial office on 03 March 1988 Hyperbaric Oxygen Treatment on a Parkinson s Disease Patient A Case Study Hoggard ML Johnson KE and Shirachi DY Chico Hyperbaric Center Chico CA 95926 and Department of Physiology and Pharmacology T J Long School of Pharmacy University of the Pacific Stockton CA 95207 USA INTRODUCTION Parkinson s Disease PD is a chronic neurodegenerative disorder which is characterized by the loss of dopaminergic neurons whose cell bodies are located in the substantia nigra pars compacta SNpc and project to the striatum The initiation of this neuronal degeneration is not known however the process of neuronal loss is suggested to occur via apoptosis rather than by necrosis 1 With the onset of the neurodegeneration of these neurons is the associated loss of the neurotransmitter dopamine DA from its nerve endings and its subsequent release in the striatum The major symptoms which are observed due to the progressive loss in function of the nigro striatal dopaminergic neurons may be one or more of the following resting tremor rigidity bradykinesia and or postural instability The actual clinical manifestation of the disease in any one patient is highly dependent upon the degree of severity of the neuronal loss age of the patient and the length of time passed between the onset of the symptoms and the time of diagnosis Early detection is important in order to institute a therapeutic strategy to relieve the symptoms and or delay the progression of the disease state The major treatment strategy currently used is to affect the function of DA Because systemically administered DA does not cross the blood brain barrier Levodopa pro drug is administered which is taken up into the brain Since Levodopa is metabolized both peripherally and centrally to DA by a DOPA decarboxylase carbidopa an inhibitor of this enzyme is administered in combination with Levodopa to decrease its metabolism peripherally increasing its uptake into the brain DA agonists and monamine oxidase B MAO B inhibitors are also administered as a monotherapy or as an adjunct to Levodopa carbidopa Sinemet therapy depending upon the clinical condition Taking a very different approach in the treatment of PD Borromei et al in 1996 showed that hyperbaric oxygen HBO therapy appeared to be effective in ameliorating many of the behavioral and motor deficits observed in PD patients 2 The objective of this study was to determine whether HBO therapy might enhance the effects of an antiparkinson treatment in a PD patient as an adjunct therapeutic modality METHODS Brief patient history A 72 year old male was diagnosed with idiopathic PD and placed on Sinemet 10 100 three doses 3 times daily One year after diagnosis for PD the patient was diagnosed with total occlusion of the right coronary artery A successful total occlusion angioplasty was performed and he was placed on Lopressor and Lipitor 10 mg daily There were no complications from this surgical procedure Eighteen months after being diagnosed as a PD patient he was treated with hyperbaric oxygen HBO at 1 9 ATA for 90 min The patient was treated daily 5 times each week for 5 weeks 25 treatments During the treatment the patient gradually reduced his dose of Sinemet until he was completely off of this medication between the 3rd and 4th week of HBO treatment At this point his physician placed him on selegiline 10mg twice daily
Clinical testing The patient s voice and speech were evaluated by a speech language pathologist and the Jebsen Taylor hand function test was performed by an occupational therapist prior to and after the end of the HBO therapy The patient was informed of all aspects of hyperbaric oxygen therapy including all risks of adverse effects according to the Declaration of Helsinki The patient also signed an informed consent form detailing the treatment and the rights of the patient RESULTS Voice and speech There was little change in the overall evaluation of voice and speech after HBO therapy Communication status changed very little He appeared to be talking more and his rate was somewhat improved He still had difficulty projecting his voice Jebsen Taylor Hand Function Test The results of this test are shown in Table 1 In testing the dominant hand there were small increments of improvement after HBO The total improvement was more than 10 while the improvement in the non dominant hand was nearly 32 During the treatment period the patient voluntarily reduced his Sinemet doses until he was completely off the drug after 3 4 weeks of HBO therapy which was an unexpected result He has continued to remain off of Sinemet therapy No complications or adverse side effects such as myopia were observed The long term exposure of HBO was tolerated well by the patient DISCUSSION PD is characterized by the loss of dopaminergic neurons of the nigro striatal pathway It is not clear how this neuronal degeneration is initiated but there appears to be a number of potential ways in which this might occur in any one individual including genetics disease drugs or other chemicals oxidative stress and or other environmental factors However once it is initiated there seems to be agreement that the degenerative process involves apoptosis and not necrosis The results of this study suggest that HBO might be a possible new modality of treatment for PD because it appeared to be able to replace Sinemet as a therapeutic regimen The mechanism by which the HBO effect might be occurring may be partly due to an anti apoptotic effect It has been shown that HBO increased the expression of Bcl 2 protein a major anti apoptotic protein in treating forebrain cerebral ischemia in gerbils 3 The Bcl 2 protein has also been elevated by repeated HBO treatment in normal gerbils 4 So it is possible that HBO in this study inhibited the apoptotic pathway involved in the progressive neuronal degeneration by stimulating the expression of the Bcl 2 proteins Other possible HBO effects should not be discounted such as improved oxygen perfusion due to increased extravascular oxygen diffusion and to possible angiogenesis 5 Axonal repair and regeneration and or synaptogenesis could occur due to increased expression of neurotrophin s since HBO has been shown to increase vascular endothelial growth factor 6 and act synergistically with platelet derived growth factor and transforming growth factor beta 7 The results of this case study agree with much of the results observed in the clinical study by Borromei and his coworkers It is not clear from their study whether some of their patients were concurrently being treated with anti parkinson drugs In our study HBO replaced the Sinemet therapy and appeared to improve the clinical condition Thus results from this case study suggest that HBO therapy might be a potential therapeutic modality in treating patients suffering from PD without causing untoward side effects such as dyskinesia observed in long term Sinemet therapy In conclusion we suggest that HBO therapy might be neuroprotective in nature to the nigro striatal neurons by acting as an antiapoptotic process This could stabilize neuronal function thereby potentially decreasing the progression of the neurodegeneration observed in Parkinson s Disease
REFERENCES 1 Thatte U and Dahanukar S Apoptosis clinical relevance and pharmacological manipulation Drugs 1997 54 4 511 532 2 Borromei A OTI efficiency in decompensated complicated Parkinson s Disease In Proceedings of the International Joint Meeting on Hyperbaric and Underwater Medicine Marroni A Oriani G and Wattel F eds XII International Congress on Hyperbaric Medicine Milano Italy 1996 pp 599 604 3 Zhou J G Liu J C and Fang Y Q Effect of hyperbaric oxygen on the expression of proteins Bcl 2 and Bax in the gerbil hippocampus CA1 following forebrain ischemia reperfusion Chin J Appl Physiol 2000 16 4 298 301 4 Wada K Miyazawa T Nomura N Yano A Tsuzuki N Nawashiro H and Shima K Mn SOD and Bcl 2 expression after repeated hyperbaric oxygen Acta Neurochir 2000 Suppl 76 285 290 5 Marx RE Radiation injury to tissue In Kindwall EP Ed Hyperbaric Medicine Practice Best Publishing Co Flagstaff AZ 1995 450 455 6 Sheikh AY Gibson JJ Rollins MD Hopf HW Hussain Z and Hunt TK Effect of hyperoxia on vascular growth factor levels in a wound model Arch Surg 2000 135 11 1293 97 7 Zhao LL Davidson JD Wee SC Roth SI and Mustoe TA Effect of hyperbaric oxygen and growth factors on rabbit ear ischemic ulcers Arch Surg 1994 129 10 1043 9 Table 1 Jebsen Taylor Hand Function Test Clinical Testing Time in sec Pre HBO Post HBO Writing 14 12 Card Turning 7 6 Manipulating Small Objects 11 11 Simulated Feeding 11 10 Stacking Small Objects 8 5 Lifting Large Light Objects 11 10 Lifting Large Heavy Objects 8 6 Total 70 60 Writing 41 28 Card Turning 8 4 Manipulating Small Objects 11 7 Simulated Feeding 12 12 Stacking Small Objects 13 8 Lifting Large Light Objects 9 6 Lifting Large Heavy Objects 7 5 101 70 Dominant Hand Non Dominant Hand Total
The Second Wave Of Oxygen Hyperbaric Oxygen therapy HBOT There is growing interest in the use of HBOT to treat the neurotoxicity induced by long term alcohol and psychostimulant abuse Even in the absence of double blind studies there is enough positive anecdotal information and case studies to warrant intensive investigation in residential treatment An example is the case of a 19 year old serious drug abuser with a preliminary brain SPECT scan that looked as bad as the scan of a demented 74 year old man The scan of the drug abuser showed a marked improvement in blood flow after just one HBOT session Harch 2007 It is conjectured that the mechanism of benefit involves supplying additional oxygen to hasten the combustion of neurotoxins that accumulate in the brain from the excess intake of alcohol Previous research from our laboratory showed that raising endorphin levels in the brain increases blood flow in the reward site of the brain Blum et al 1985 Synaptose raises brain levels of endorphins by preventing their breakdown Coupled with an enhanced oxygenation by HBOT the synergy should translate to improving brain health in addicts Brain healing is necessary in order to overcome neurological deficits that result from SUD HBOT has been used to successfully treat a myriad of other neurologically based disorders including traumatic brain injuries cardiovascular accidents post traumatic stress disorder dementia and Parkinson s Disease Harch PG and Mccoullough The Oxygen Revolution Hatherleigh Press 2007 NewYork page 151 152 Hyperbaric Oxygenation Therapy In an Italian study 55 of 63 patients showed significant improvement after hyperbaric oxygenation therapy This therapy is beginning to be widely used in neurodegenerative conditions particularly movement disorders More and more research is being published on the benefits of HBOT in Parkinson s disease syndrome Research suggests that glutathione a critically important brain chemical is deficient in Parkinson s patients and may play a significant role in the treatment of this disease Glutathione is a powerful antioxidant and helps to prevent free radical damage to brain tissue So far the intravenous use of glutathione has shown promising results in reducing tremors and improving movement and balance Ongoing clinical trials suggest that multi modality therapy combining intravenous glutathione with Hyperbaric Oxygenation Therapy HBOT and nutritional supplementation may be more effective than glutathione alone HOC is currently conducting clinical trials on combination therapy for Parkinson s disease and is looking for participants Please contact Dr Tasreen Alibhai ND at 604 520 3941 for further information Video References http www youtube com watch v ECncQzGXrC4 http www youtube com watch v nbFs9NN__Mk feature related http www youtube com watch v 78PXByMI5J8
The role of Hyperbaric Oxygen Dr Nur Ozyilmaz MD Integrative Health Specialist Consultant Paediatrician International Hyperbaric Medical Foundation 12th International Symposium August 10 12th 2018 Denver Colorado
Case I 64 years old previously relatively fit and healthy female History of chronic constipation gingivitis anosmia Develops tremor bradykinesia voice changes rigid facial expression stooped posture loss of swinging of left arm small cramped writing intermittent dystonia on hands and feet Diagnosed with
Disease Parkinson disease PD is a chronic progressive neurodegenerative disease of the nervous system characterized by the cardinal features of rigidity bradykinesia tremor and postural instability
Categories 1 Parkinsonism a group of disorders with Basal Ganglia dysfunction 2 PD or idiopathic Parkinsonism The most common form 3 Secondary Parkinsonism Viruses toxins drugs tumors 4 Parkinsonism plus syndromes conditions that mimic PD symptoms caused by some other neurodegenerative diseases
Etiology The mechanisms of PD remain elusive Several genes identified including SNCA PARKIN DJ 1 PINK 1 and disease oxidative stress mitochondrial and proteseomal dysfunction and inflammatory system involvement Autoimmune disease
Signs and symptoms Tremor Subtle decrease in dexterity Decreased arm swing on the first involved side Soft voice Decreased facial expression Sleep disturbances Decreased sense of smell Symptoms of autonomic dysfunction eg constipation sweating abnormalities sexual dysfunction seborrheic dermatitis A general feeling of weakness malaise Depression or anhedonia Slowness in thinking
Diagnosis PD is a clinical diagnosis No laboratory biomarkers exist for the condition Findings on routine MRI and CT scan are unremarkable MRI is useful to exclude strokes tumors multiinfarct state hydrocephalus and the lesions of Wilson disease PET and DaT scans
Treatment Symptomatic drug therapy Levodopa carbidopa The gold standard of symptomatic treatment Monoamine oxidase MAO B inhibitors Other dopamine agonists eg ropinirole pramipexole Anticholinergic agents eg trihexyphenidyl benztropine Treatment for non motor symptoms Sildenafil citrate Viagra For erectile dysfunction Polyethylene glycol For constipation Modafinil For excessive daytime somnolence Methylphenidate For fatigue potential for abuse and addiction Deep brain stimulation
Continuing Case I Investigations FBC U E LFT Bone Profile CRP Normal MRI Normal Stool comprehensive test Candida overgrowth low beneficial bacteria Urine organic and amino acids high benzoic acid arabinase Citramalic Acid Phenylacetic Hydroxyisobutyric Acid Pyroglutamic Acid Toxicity PCB pesticides mercury aluminum
Treatment Nutrition LCHF altered with ketogenic diet Exercise Optimizing gut flora Treating candida overgrowth Detoxification Optimizing methylation pathway Supplements glutathione precursors antioxidants anti inflammatories Low dose naltrexone Bioresonance PEMFR Non laser light therapy HBOT x 40 sessions
At the time of diagnosis in 2012 2018 Moderate memory loss Vivid dreams Sustained depression with vegetative symptoms insomnia poor appetite loss of interest Less assertive than usual None None None Normal Normal Normal Moderately slow small mostly legible Can cut most foods with some difficulty Needs assistance with buttoning sleeves Normal Rare falling Occasional freezing Mild difficulty no swing left arm Moderate bothersome to patient Frequent painful sensations Normal Normal Normal Normal Normal Normal Normal None None Normal Left leg only when anxious Occasional Scale I Mentation Behavior and Mood Intellectual Impairment Thought Disorder Depression Motivation Initiative II Activities of Daily Living Speech Salivation Swallowing Handwriting Cutting Food Handling utensils Dressing Hygiene Falling Freezing when Walking Walking Tremor Sensory Complaints Normal
At the time of diagnosis in 2012 2018 Monotone but understandable Masked face loss of facial express Moderate in amplitude present most of the time Slight present with action Marked FROM full range of achieved Moderately impaired Moderately impaired Frequently unable to arise without help Moderately stooped posture Short steps with shuffles Impaired Moderate slowness small amplitude of movement Normal Normal Only left leg when anxious Scale III Motor Examination Speech Facial Expression Tremor at Rest Action or Postural Tremor of Hands Rigidity Finger Taps Leg Agility Arising from Chair Posture Gait Postural Stability Bradykinesia None Absent Normal Normal Normal Mostly normal Normal Normal Minimal slowness
At the time of diagnosis in 2012 2018 Dyskinesia Daily None Early Morning Dystonia Daily None Insomnia Severe Resolved Scale In summary 6 years after diagnosis of PD Not on any PD medication Disease not progressing Significant improvement with complete resolution of majority of the symptoms
Case II 53 years old male CEO 1 Parkinsonism 2005 40 years old 2 Reduced uptake in the left putamen and minimally reduced uptake in the left caudate and right putamen DAT scan December 2005 3 Right hip replacement July 2009 4 Bilateral STN stimulators inserted November 2012 5 Medtronic ACTIVA PC box replacement August 2017 Present complaints Painful dyskinesia dystonia left leg tremor walking with extreme difficulty insomnia Medications Stalevo 125mg qds and Amantadine 100mg
Case II Progress Before HBOT After 20 sessions of HBOT with no other intervention Upper body dyskinesia 30 improvement Left leg tremor 50 improvement walking with extreme difficulty only short distance 30 improvement Severe rigidity full range of motion achieved with difficulty 50 improvement Freezing when walking 50 improvement Poor quality interrupted sleep Sleeps well
Numerous in vivo and in vitro studies confirms that HBOT induces neurogenesis Wang XL et al Hyperbaric oxygen promotes the migration and differentiation of endogenous neural stem cells in neonatal rats with hypoxic ischemic brain damage Zhongguo Dang Dai Er Ke Za Zhi 2009 11 9 749 52 PubMed Zhang XY et al The role of beta catenin signaling pathway on proliferation of rats neural stem cells after hyperbaric oxygen therapy in vitro Cell Mol Neurobiol 2011 31 1 101 9 doi 10 1007 s10571 0109559 z PubMed Milosevic J et al Non hypoxic stabilization of hypoxia inducible factor alpha HIF alpha relevance in neural progenitor stem cells Neurotox Res 2009 15 4 367 80 doi 10 1007 s12640 009 9043z PubMed Cross Ref Godman CA et al Hyperbaric oxygen treatment induces antioxidant gene expression Ann N Y Acad Sci 2010 1197 178 83 doi 10 1111 j 1749 6632 2009 05393 x PubMed Yang YJ et al Hyperbaric oxygen induces endogenous neural stem cells to proliferate and differentiate in hypoxic ischemic brain damage in neonatal rats Undersea Hyperb Med 2008 35 2 113 29 PubMed Zhang T et al Hyperbaric oxygen therapy improves neurogenesis and brain blood supply in piriform cortex in rats with vascular dementia Brain Inj 2010 24 11 1350 7 doi 10 3109 02699052 2010 504525 PubMed Gunther A et al Reduced infarct volume and differential effects on glial cell activation after hyperbaric oxygen treatment in rat permanent focal cerebral ischaemia Eur J Neurosci 2005 21 11 3189 94 doi 10 1111 j 1460 9568 2005 04151 x PubMed
Potential mechanisms of HBOT and HIF
Biomed Res Int 2014 2014 308654 doi 10 1155 2014 308654 Epub 2014 Jun 24 Evidence of inflammatory system involvement in Parkinson s disease
disease Cytokines and other soluble molecules IL 1 IL 2 IL 4 IL 6 IL 10 TNF IFN TGF IL 6 MMP 3 IL 17 and IL 18 Pattern recognition receptors PRRs TLRs TLR 1 2 3 and 7 NLRs and complements Immune cells Microglia monocyte NK cell T cell and B cell
Potential benefit of HBOT
Gut Brain Axis
Lewy pathology has been described in neurons of the enteric nervous system in nearly at autopsy The enteric nervous system not only contains a variety of functionally distinct enteric neurons but also harbors a prominent component of glial cells the socalled enteric glial cells which like astrocytes of the central nervous system contribute to support protect and maintain the neural network recently shown that enteric glial cell dysfunction occurs in PD
Combining HBOT with other treatment modalities Nutrition Ketogenic Diet Optimizing gut microbiome Tailored supplements vitamins and minerals Cannabidiol Low dose naltrexone Near infrared light therapy Repetitive transcranial magnetic stimulation Pulsed electromagnetic field therapy Exercise
Cannabidiol Disease and Movement Disorders further explored this possibility and assessed the effects of oral cannabidiol CBD and inhaled cannabis in disease Maureen A Leehey MD Professor of Neurology and Chief of the Movement Disorders Division at the University of Colorado in Aurora and colleagues conducted a phase II open label dose escalation study to evaluate the safety and tolerability of CBD Epidiolex disease Over a 31 day treatment period patients received 5 7 5 10 15 and 20 mg kg day doses of CBD 13 patients mean total UPDRS score significantly decreased from 45 9 at baseline to 36 4 at the final visit UPDRS motor score decreased from 27 3 to 20 3 Mean rigidity from 9 14 to 6 29 Laurie K Mischley ND PhD MPH Associate Clinical Investigator at Bastyr University Research Institute in Kenmore Washington and disease tremor using motion sensors and qualitative interviews
LDN low dose naltrexone blocks opioid receptors in the brain for few hours and creates regulated production of the endogenous opioids beta endorphin and metenkephalin as well as increased expression of opioid receptors both endogenous and exogenous opioids immune modulators suppress microglial activation via its antagonistic effect on toll like receptor 4 TLR4 a non opioid receptor that is found on macrophages such as microglia
Neuron Photomodulation light therapy
Neuroscience Research 132 2018 58 62 Contents lists available at ScienceDirect Neuroscience Research journal homepage www elsevier com locate neures Short Communication Mild hyperbaric oxygen inhibits the decrease of dopaminergic neurons in the substantia nigra of mice with MPTP induced Parkinson s disease Yuina Kusuda a Ai Takemura a Masaki Nakano b Akihiko Ishihara a a b Laboratory of Cell Biology and Life Science Graduate School of Human and Environmental Studies Kyoto University Sakyo ku Kyoto 606 8501 Japan Laboratory of Functional Biology Graduate School of Biostudies Kyoto University Sakyo ku Kyoto 606 8501 Japan a r t i c l e i n f o Article history Received 4 August 2017 Received in revised form 15 November 2017 Accepted 24 November 2017 Available online 28 November 2017 Keywords Balance beam test Dissolved oxygen Enhanced atmosphere absolute Immunohistochemistry Increased oxygen concentration Oxidative metabolism Rotarod test a b s t r a c t We examined whether exposure to mild hyperbaric oxygen inhibits the decrease of dopaminergic neurons in the substantia nigra of a neurotoxic animal model with Parkinson s disease Mice injected with 1 methyl 4 phenyl 1 2 3 6 tetrahydropyridine hydrochloride and probenecid twice a week were divided into two groups mice with mild hyperbaric oxygen and those without The mice with mild hyperbaric oxygen were exposed to 1317 hPa with 45 oxygen for 3 h three times a week The decrease in dopaminergic neurons of mice with Parkinson s disease was inhibited by 11 weeks of exposure to mild hyperbaric oxygen We conclude that exposure to mild hyperbaric oxygen is effective in preventing the progression of Parkinson s disease 2017 The Authors Published by Elsevier Ireland Ltd This is an open access article under the CC BY license http creativecommons org licenses by 4 0 Parkinson s disease is a progressive neurodegenerative disorder in the elderly that is characterized by typical motor symptoms such as resting tremors rigidity bradykinesia and gait disturbances Adler 2005 The conventional therapy using levodopa and dopamine agonists for Parkinson s disease focuses primarily on relieving motor symptoms Another therapy for Parkinson s disease includes chronic exercise Bergen et al 2002 Hirsch et al 2003 Pothakos et al 2009 However it is difficult to completely prevent the degeneration of dopaminergic neurons with these therapies Exposure to mild hyperbaric oxygen at 1266 1317 hPa with 35 45 oxygen increases the level of oxygen in blood especially the oxygen dissolved in blood plasma and facilitates oxidative metabolism in the mitochondrial tricarboxylic acid cycle in cells and tissues Ishihara et al 2005 Matsumoto et al 2007 Metabolic syndrome Takemura and Ishihara 2017 lifestyle related diseases Gu et al 2010 Nagatomo et al 2010a 2011 and arthritis Nagatomo et al 2010b are inhibited and or improved when rodents are exposed to mild hyperbaric oxygen Corresponding author E mail address ishihara akihiko 8s kyoto u ac jp A Ishihara Parkinson s disease results from the progressive decrease of dopaminergic neurons in the substantia nigra Dauer and Przedborski 2003 although the mechanisms for this decrease have not fully been clarified It is suggested that exposure to mild hyperbaric oxygen inhibits the decrease in dopaminergic neurons which would result in an improvement of Parkinson s disease because of the enhancement of oxidative metabolism in dopaminergic neurons All experimental and animal care procedures were approved by the Guidelines for the Care and Use of Laboratory Animals issued by the Institutional Animal Experiment Committee of Kyoto University Kyoto Japan and conducted in accordance with the National Institute of Health Guide for the Care and Use of Laboratory Animals All efforts were made to minimize both the number of animals used and their suffering Four week old male C57BL 6JJmsSlc mice were divided into the control CON Parkinson s disease PD and Parkinson s disease with mild hyperbaric oxygen PDO groups n 12 in each group All mice were housed under normobaric conditions that is 1013 hPa with 20 9 oxygen The PD and PDO groups were injected with 1 methyl 4 phenyl 1 2 3 6 tetrahydropyridine hydrochloride MPTP 20 mg kg body weight and probenecid 250 mg kg body weight twice a week Tuesday and Thursday https doi org 10 1016 j neures 2017 11 008 0168 0102 2017 The Authors Published by Elsevier Ireland Ltd This is an open access article under the CC BY license http creativecommons org licenses by 4 0
Y Kusuda et al Neuroscience Research 132 2018 58 62 from 7 to 18 weeks of age Meredith et al 2008 In addition the PDO group was exposed to mild hyperbaric oxygen at 1317 hPa with 45 oxygen using a chamber for exposure to mild hyperbaric oxygen Japan Patent No 5076067 dated September 7 2012 Inventor Akihiko Ishihara for 3 h 11 00 14 00 h three times a week Monday Wednesday and Friday All mice were evaluated for motor functions using rotarod and balance beam tests at 16 17 and 18 weeks of age The rotarod test consisted of a 3 cm diameter cylinder rotating at 22 rpm The amount of time before the mouse dropped off the cylinder was recorded For the balance beam test the time taken by the mouse to move a distance of 50 cm on a 5 mm diameter stick and the number of times that the mouse s feet slid off the stick were recorded Food and water were provided ad libitum to all mice The room was maintained in a controlled 12 h light dark cycle dark period from 20 00 08 00 h at 22 2 C with 45 55 relative humidity After 11 weeks of the experimental period the mice were anesthetized using sodium pentobarbital 30 mg kg body weight via intraperitoneal injection The mice were perfused using phosphate buffered saline pH 7 4 followed by 4 paraformaldehyde and 2 glutaraldehyde The brains were isolated fixed and embedded in paraffin Serial 4 m thick sections were cut using a microtome and mounted onto slides The sections were incubated in primary antibody anti tyrosine hydroxylase TH antibody EMD Millipore Corporation Germany overnight washed with tris buffered saline with Tween 20 TBST and incubated in secondary antibody biotinylated rabbit immunoglobulin G VECTOR Laboratories USA for 60 min After washing with TBST the sections were incubated using VECTASTAIN Elite ABC kit VECTOR Laboratories USA for 30 min They were then rinsed with TBST incubated using a DAB substrate kit VECTOR Laboratories USA for 6 min cleared and mounted For each mouse TH positive neurons in the substantia nigra were counted in five consecutive sections Repeated sampling of the same neurons on the serial sections was avoided by confirming the position of individual neurons The data are expressed as mean and standard deviation Oneway analysis of variance ANOVA was used to evaluate the differences among the CON PD and PDO groups When the differences were found to be significant by ANOVA individual group comparisons were made using Scheff s post hoc test Statistical significance was set at P 0 05 There were no differences in the body weight among the three groups at 7 CON 22 0 0 6 g PD 22 0 0 9 g PDO 22 7 1 0 g F 2 368 P 0 109 and 18 CON 26 9 1 4 g PD 26 5 1 1 g PDO 27 0 1 1 g F 0 467 P 0 632 weeks of age the first and last stages of the experiment respectively There were no differences in the amount of time before the mouse dropped off the cylinder during the rotarod test among the CON PD and PDO groups at 16 F 0 369 P 0 696 17 F 1 028 P 0 378 and 18 F 0 672 P 0 521 weeks of age Fig 1A During the balance beam test there were no differences in the time taken by the mouse to move a distance of 50 cm on the stick among the CON PD and PDO groups at 16 F 0 218 P 0 805 and 18 F 0 217 P 0 807 weeks of age Fig 1B however there were differences at 17 weeks of age F 3 694 P 0 05 The time taken by the mouse to move a distance of 50 cm on the stick was shorter in the PDO group than in the CON group at 17 weeks of age P 0 05 There were differences in the number of times that the mouse s feet slid off the stick during the balance beam test among the CON PD and PDO groups at 16 F 14 590 P 0 05 17 F 11 313 P 0 05 and 18 F 8 135 P 0 05 weeks of age Fig 1C The number of times that the mouse s feet slid off the stick was higher in the PD group than in the CON and PDO groups at 16 17 and 18 weeks of age P 0 05 for all weeks There were differences in the number of dopaminergic neurons in the substantia nigra among the CON PD and PDO groups 59 Fig 1 Rotarod and balance beam tests for the CON PD and PDO groups The amount of time before the mouse dropped off a cylinder rotating at a speed of 22 rpm was recorded for the rotarod test A The time taken by the mouse to move a distance of 50 cm on a 5 mm diameter stick B and the number of times that the mouse s feet slid off the stick C were recorded for the balance beam test CON control PD Parkinson s disease PDO Parkinson s disease with mild hyperbaric oxygen Data are expressed as mean and standard deviation of 12 mice a P 0 05 compared with CON b P 0 05 compared with PD Figs 2 and 3 F 39 230 P 0 05 The number of dopaminergic neurons in the substantia nigra was lower in the PD group than in the CON P 0 05 and PDO P 0 05 groups The number of dopaminergic neurons in the substantia nigra was lower in the PDO group than in the CON group P 0 05 This study examined the effects of exposure to mild hyperbaric oxygen on motor functions and dopaminergic neurons in the substantia nigra of mice with MPTP induced Parkinson s disease Exposure to mild hyperbaric oxygen improved motor functions in mice with Parkinson s disease the number of times that the mouse s feet slid off the stick decreased following exposure to mild hyperbaric oxygen in the PDO group Fig 1C We observed that exposure to mild hyperbaric oxygen facilitates oxidative metabolism particularly in pathways in the mitochondrial tricarboxylic acid cycle thus enhancing the oxidative capacity of skeletal muscle fibers and the spinal motoneurons innervating them Ishihara et al 2005 Matsumoto et al 2007 It is suggested that exposure to mild hyperbaric oxygen has an effect on the neu
60 Y Kusuda et al Neuroscience Research 132 2018 58 62 Fig 2 Representative sections of the substantia nigra in control A B C Parkinson s disease D E F and Parkinson s disease with mild hyperbaric oxygen G H I mice stained for tyrosine hydroxylase activity B and C E and F and H and I extended A D and G respectively Scale bars on G and I are 200 and 100 m respectively
Y Kusuda et al Neuroscience Research 132 2018 58 62 Fig 3 Numbers of anti tyrosine hydroxylase antibody positive neurons in the substantia nigra for the CON PD and PDO groups TH tyrosine hydroxylase positive Data are expressed as mean and standard deviation of 12 mice a P 0 05 compared with CON b P 0 05 compared with PD 61 2003 Oter et al 2005 2007 Gesell and Trott 2007 Excessive atmospheric pressure and oxygen concentration especially in treatments with 100 oxygen have been shown to increase the number of invasive inflammatory cells Folz et al 1999 and cause excessive production of reactive oxygen species in several tissues and organs Narkowicz et al 1993 In this study the condition of mild hyperbaric oxygen was produced using 1317 hPa and 45 oxygen Such side effects including oxidative stress and barotrauma are not induced by these conditions Nagatomo et al 2012 Exposure to mild hyperbaric oxygen also poses negligible risk of fire and explosion because of relatively low atmospheric pressure and oxygen concentration We conclude that exposure to mild hyperbaric oxygen at 1317 hPa with 45 oxygen inhibits the decrease of dopaminergic neurons which results in the improvement of Parkinson s disease because it activates oxidative metabolism in dopaminergic neurons Conflict of interest romuscular system which is largely related to motor functions in mice with Parkinson s disease Therefore the number of times that the mouse s feet slid off the stick was decreased by exposure to mild hyperbaric oxygen In contrast there were no effects of exposure to mild hyperbaric oxygen on the amount of time before the mouse dropped off the cylinder Fig 1A or the time taken by the mouse to move a distance of 50 cm on the stick Fig 1B The reasons for differences in the motor function of these tests were not elucidated in this study Multiple performance tests e g rotarod balance beam pole and open field tests are required for the evaluation of motor functions in mice with Parkinson s disease because of behavioral anomalies in individual mice The decrease in the number of dopaminergic neurons in the substantia nigra of mice with Parkinson s disease was inhibited by exposure to mild hyperbaric oxygen Fig 3 Increased atmospheric pressure accompanied by a high oxygen concentration enhances the partial pressure of oxygen and increases dissolved oxygen in blood plasma Ishihara et al 2014 When water vapor pressure concentration of carbon dioxide in the alveolus and the respiratory exchange ratio are set at 47 mmHg 40 mmHg and 0 85 respectively the estimated levels of oxygen dissolved in blood plasma under mild hyperbaric oxygen conditions at 1317 hPa with 45 oxygen 1 18 ml dL blood plasma are 3 7 times those under normobaric conditions at 1013 hPa with 20 9 oxygen 0 32 ml dL blood plasma Exposure to mild hyperbaric oxygen enhances the oxidative capacity of pathways in the mitochondrial tricarboxylic acid cycle thus improving oxidative metabolism in cells and tissues Therefore we hypothesized that exposure to mild hyperbaric oxygen inhibits the decrease in dopaminergic neurons induced by Parkinson s disease because it activates oxidative metabolism in the dopaminergic neurons It is suggested that peroxisome proliferator activated receptor coactivator 1 PGC 1 is one of the factors that contributes to the improvement in oxidative metabolism of dopaminergic neurons in Parkinson s disease because cell oxidative metabolism mitochondrial biogenesis oxidative stress and gene expression are regulated by PGC 1 which is a transcriptional coactivator Wu et al 1999 Liang and Ward 2006 A previous study Mud et al 2012 observed that transgenic mice overexpressing PGC 1 are resistant to both dopaminergic neuron degeneration in the substantia nigra and dopamine disappearance in the striatum Hyperbaric oxygen therapy which is an established medical treatment and is usually conducted under conditions of 2026 3039 hPa with 100 oxygen induces many diseases and complications including atherosclerosis cataract retinopathy myocardial infarction hypertension diabetes renal failure and uremia Padgaonkar et al 2000 Griendling and FitzGerald The authors have no conflict of interest to report References Adler C H 2005 Nonmotor complications in Parkinson s disease Mov Disord 20 Suppl 11 S23 S29 Bergen J L Toole T Elliott 3rd R G Wallace B Robinson K Maitland C G 2002 Aerobic exercise intervention improves aerobic capacity and movement initiation in Parkinson s disease patients Neurorehabiitation 17 161 168 Dauer W Przedborski S 2003 Parkinson s disease mechanisms and models Neuron 39 889 909 Folz R J Abushamaa A M Suliman H B 1999 Extracellular superoxide dismutase in the airways of transgenic mice reduces inflammation and attenuates lung toxicity following hyperoxia J Clin Invest 103 1055 1066 Gesell L B Trott A 2007 De novo cataract development following a standard course of hyperbaric oxygen therapy Undersea Hyperb Med 34 389 392 Griendling K K FitzGerald G A 2003 Oxidative stress and cardiovascular injury Part I basic mechanisms and in vivo monitoring of ROS Circulation 108 1912 1916 Gu N Nagatomo F Fujino H Takeda I Tsuda K Ishihara A 2010 Hyperbaric oxygen exposure improves blood glucose level and muscle oxidative capacity in rats with type 2 diabetes Diabetes Technol Ther 12 125 133 Hirsch M A Toole T Maitland C G Rider R A 2003 The effects of balance training and high intensity resistance training on persons with idiopathic Parkinson s disease Arch Phys Med Rehabil 84 1109 1117 Ishihara A Kawano F Okiura T Morimatsu F Ohira Y 2005 Hyperbaric exposure with high oxygen concentration enhances oxidative capacity of neuromuscular units Neurosci Res 52 146 152 Ishihara A Nagatomo F Fujino H Kondo H 2014 Exposure to mild hyperbaric oxygen increases blood flow and resting energy expenditure but not oxidative stress J Sci Res Rep 3 1886 1896 Liang H Ward W F 2006 PGC 1 a key regulator of energy metabolism Adv Physiol Educ 30 145 151 Matsumoto A Okiura T Morimatsu F Ohira Y Ishihara A 2007 Effects of hyperbaric exposure with high oxygen concentration on the physical activity of developing rats Dev Neurosci 29 452 459 Meredith G E Totterdell S Potashkin J A Surmeier D J 2008 Modeling PD pathogenesis in mice advantage of a chronic MPTP protocol Parkinsonism Relat Disord 14 Suppl 2 S112 S115 Mud G M kel J Liberto V D Tselykh T V Olivieri M Piepponen P Eriksson O M lki A Bonomo A Kairisalo M Aguirre J A Korhonen L Belluardo N Lindholm D 2012 Transgenic expression and activation of PGC 1 protect dopaminergic neurons in the MPTP mouse model of Parkinson s disease Cell Mol Life Sci 69 1153 1165 Nagatomo F Fujino H Takeda I Ishihara A 2010a Effects of hyperbaric oxygenation on blood pressure levels of spontaneously hypertensive rats Clin Exp Hypertens 32 193 197 Nagatomo F Gu N Fujino H Okiura T Morimatsu F Takeda I Ishihara A 2010b Effects of exposure to hyperbaric oxygen on oxidative stress in rats with type II collagen induced arthritis Clin Exp Med 10 7 13 Nagatomo F Roy R R Takahashi H Edgerton V R Ishihara A 2011 Effect of exposure to hyperbaric oxygen on diabetes induced cataracts in mice J Diabetes 3 301 308 Nagatomo F Fujino H Kondo H Ishihara A 2012 Oxygen concentrationdependent oxidative stress levels in rats Oxid Med Cell Longev 10 1155 2012 381763 Narkowicz C K Vial J H McCartney P W 1993 Hyperbaric oxygen therapy increases free radical levels in the blood of humans Free Radic Res Commun 19 71 80
62 Y Kusuda et al Neuroscience Research 132 2018 58 62 Oter S Korkmaz A Topal T Ozcan O Sadir S Ozler M Ogur R Bilgic H 2005 Correlation between hyperbaric oxygen exposure pressures and oxidative parameters in rat lung brain and erythrocytes Clin Biochem 38 706 711 Oter S Topal T Sadir S Ozler M Uysal B Ay H Yaren H Korkmaz A Akin A 2007 Oxidative stress levels in rats following exposure to oxygen at 3 atm for 0 120 min Aviat Space Environ Med 78 1108 1113 Padgaonkar V A Leverenz V R Fowler K E Reddy V N Giblin F J 2000 The effects of hyperbaric oxygen on the crystallins of cultured rabbit lenses a possible catalytic role of copper Exp Eye Res 71 371 383 Pothakos K Kurz M J Lau Y S 2009 Restorative effect of endurance exercise on behavioral deficits in the chronic mouse model of Parkinson s disease with severe neurodegeneration BMC Neurosci 10 http dx doi org 10 1186 14712202 10 6 Takemura A Ishihara A 2017 Mild hyperbaric oxygen inhibits growth related decrease in muscle oxidative capacity of rats with metabolic syndrome J Atheroscler Thromb 24 26 38 Wu Z Puigserver P Andersson U Zhang C Adelmant G Mootha V Troy A Cinti S Lowell B Scarpulla R C Spiegelma B M 1999 Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC 1 Cell 98 115 124
applied sciences Review A Systematic Review of Oxygen Therapy for the Management of Medication Related Osteonecrosis of the Jaw MRONJ Roberto Sacco 1 2 3 Racheal Leeson 4 Joseph Nissan 5 Sergio Olate 6 Carlos Henrique Bettoni Cruz de Castro 7 Alessandro Acocella 8 and Anand Lalli 9 1 2 3 4 5 6 7 8 9 Oral Surgery Department Barts and the London School of Medicine and Dentistry London E1 2AT UK CPD Department Eastman Dental Institute University College of London London WC1X 8LT UK Oral Surgery Department King s College Hospital London SE5 9RW UK Oral Surgery Department Eastman Dental Institute University College of London London WC1X 8LD UK r leeson ucl ac uk Oral Rehabilitation Department School of Dentistry Tel Aviv University Tel Aviv 69978 Israel nissandr post tau ac il Oral and Maxillofacial Surgery Department Universidad de La Frontera Temuco 1145 Chile sergio olate ufrontera cl Oral Surgery Department Pontif cia Universidade Cat lica de Minas Gerais Belo Horizonte 30535 360 Barzil carlosbettoni1 yahoo com br Private Practice Florence 50129 Italy alessandroacocella yahoo it Centre for Oral Immunobiology and Regenerative Medicine Barts and the London School of Medicine and Dentistry London E1 4NS UK a lalli qmul ac uk Correspondence r sacco ucl ac uk Received 22 January 2019 Accepted 6 March 2019 Published 12 March 2019 Abstract Background Medication related osteonecrosis of the jaw MRONJ can be a life changing iatrogenic complication of antiresorptive and antiangiogenic drug therapy It is most often associated with high doses of these medications that are used to prevent skeletal related events in patients with cancer and bone pathologies Unfortunately managing MRONJ lesions has proven difficult and remains a major challenge for clinicians Due to the lack of efficacy in treating MRONJ by surgical modalities local debridement and free flap reconstruction the nonsurgical management of MRONJ is still advocated to aid healing or avoid disease progression The aim of this systematic review is to identify analyse and understand the published evidence related to the success of oxygen therapies such as ozone OT and hyperbaric oxygen HBO in treating MRONJ Material and methods A multi database PubMed MEDLINE EMBASE CINAHL and Cochrane CENTRAL systematic search was performed by three authors The identified articles were independently assessed for their risk of bias Any type of study evaluating humans treated with antiresorptive and antiangiogenic drugs were considered The aim is primarily to evaluate the success of OT and HBO in resolving MRONJ and secondarily to identify any improvements in quality of life QoL rate of complications time to event and severity of side effects related to these treatments Results In total just 13 studies were eligible for analysis A pooled total of 313 patients HBO group n 82 OT group n 231 described in these studies have shown good tolerance for oxygen therapies Complete resolution of MRONJ was reported in 44 58 of OT patients but only 5 17 of the HBO group Progression of MRONJ was reported only in the HBO studies in 10 34 of cases 6 patients The quality of evidence was low or very low in all studies This was due to limitations in how the studies were designed run and reported Conclusions Based on the limited data available it is difficult to suggest OT is better or worse than HBO or whether it is better than a placebo As the level of evidence available is low this necessitates larger well designed trials to justify these interventions for patients affected by MRONJ Appl Sci 2019 9 1026 doi 10 3390 app9051026 www mdpi com journal applsci
Appl Sci 2019 9 1026 2 of 23 Keywords osteonecrosis bisphosphonate related osteonecrosis of the jaw antiresorptive drugs antiangiogenic drugs ozone therapy hyperbaric oxygen therapy 1 Introduction The term medication related osteonecrosis of the jaws MRONJ refers to a potentially serious iatrogenic complication of treatment with medications such as antiangiogenic or antiresorptive drugs These drug families are used primarily for the treatment of malignancies e g multiple myeloma or bone metastases but also have important roles in the management of osteoporosis Paget s disease and hypercalcemia The bone targeting agents BTAs can reduce the risk of skeletal related adverse events to protect the skeleton in patients with primary or secondary bone pathology 1 2 Since the first reports of bisphosphonate related osteonecrosis of the jaw in 2003 an increasing number of reports have been published showing similar clinical complications associated with other drugs New evidence has shown that along with bisphosphonates BPs other BTAs such as denosumab also cause osteonecrosis of the jaw bones In addition monoclonal antibodies able to bind and selectively inhibit vascular endothelial growth factor A VEGF A specifically mammalian target of rapamycin mTOR inhibitors can also cause similar lesions 3 5 For this reason the term MRONJ was adopted in the 2014 position paper of the American Association of Oral and Maxillofacial Surgeons AAOMS 3 The medications currently reported to be associated with MRONJ are listed in Table 1 antiresorptive drugs and Table 2 antiangiogenic agents 6 7 The AAOMS position paper states that patients may be considered to have MRONJ if all the following characteristics are present current or previous treatment with antiresorptive or antiangiogenic agents exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for longer than 8 weeks and no history of radiation therapy to the jaws or obvious metastatic disease to the jaws However it is accepted that some patients may present with non specific symptoms and may not have evidence of exposed bone such as those classified as Stage 0 by the AAOMS staging system 8 The term stage 0 was first used by Mawardi et al to gather suspected MRONJ cases presenting with clinical and radiological signs of disease other than intraoral bone exposure 9 The AAOMS classification and staging system is based entirely on the intraoral presentation which they propose should also guide potential treatment This has been criticised in studies where it was highlighted that radiological findings are an important part of the clinical picture necessary for accurate MRONJ staging Tables 3 and 4 6 8 10 The major risk factor for the development of MRONJ is dento alveolar surgery with a history of tooth extraction or oral surgery procedure apicectomy or cystectomy reported in 52 to 80 of patients with MRONJ 11 13 The overall risk of developing MRONJ after dento alveolar surgery in patients on IV bisphosphonates ranges from 1 6 to 14 8 in comparison to 0 5 for patients taking oral bisphosphonates 6 To date there is no current standard for the treatment of MRONJ associated with antiresorptive or antiangiogenic drug therapy Several treatment options have been described with the earlier stages of MRONJ reportedly responding well to conservative management such as topical or systemic antibiotics or limited bone debridement although this still remains controversial 14 15 Ozone therapy OT and hyperbaric oxygen therapy HBO have been reported as effective adjunctive therapies in situations where normal bony wound healing is impaired such as osteoradionecrosis and chronic osteomyelitis of the jaw 16 18
Appl Sci 2019 9 1026 3 of 23 Table 1 Antiresorptive drugs associated with medication related osteonecrosis of the jaws MRONJ Btl Bottle IM Intramuscular IV Intravenous MM Multiple myeloma PO Orally SC Subcutaneous SRE Skeletal related event Tab Tablet Pharmacologic Active Ingredient Formulation Route of Administration Alendronic acid sodium salt Tab 70 mg Tab 10 mg PO Treatment of postmenopausal osteoporosis 70 mg week Treatment of osteoporosis in men 70 mg week Treatment and prevention of osteoporosis induced by glucocorticoids 70 mg week Alendronic acid cholecalciferol Tab 70 mg 5600 UI PO Treatment of postmenopausal osteoporosis in patients with unsupplemented vitamin D deficit 70 mg week Ibandronic acid monosodium salt monohydrate Tab 50 mg Btl 6 mg 6 mL Tab 150 mg Btl 3 mg 3 mL PO IV PO IV Prevention of SREs in breast cancer patients with bone metastases 50 mg day p o or 6 mg every 3 4 weeks iv Treatment of hypercalcemia of malignancy Treatment of postmenopausal osteoporosis in patients at high risk of fracture 150 mg 4 weeks p o or 3 mg every 3 months iv Neridronate acid sodium salt Btl 25 mg 2 mL Btl 100 mg 8 mL IV IM IV Risedronic acid Tab 35 mg Tab 5 mg PO Treatment of postmenopausal osteoporosis 35 mg weekly or 5 mg daily Treatment and prevention of osteoporosis induced by glucocorticoids 35 mg weekly or 5 mg daily Treatment of Paget s disease Indication and Frequency Osteogenesis imperfecta 2 mg kg 3 months Treatment of Paget s disease different schedules Zoledronic acid monohydrate Btl 4 mg 5 mL Btl 5 mg 100 mL IV IV Prevention of SREs in cancer patients with bone metastases or MM 4 mg every 3 4 weeks Treatment of hypercalcemia of malignancy Treatment of osteoporosis in postmenopausal women in men at increased risk of fracture including those with a recent hip fracture from minor trauma 5 mg once per year Treatment of Paget s disease Denosumab Btl 120 mg Btl 60 mg SC SC Prevention of SREs in cancer patients with bone metastases 120 mg every 4 weeks Treatment of hypercalcemia of malignancy Osteoporosis 60 mg sc every 6 months
Appl Sci 2019 9 1026 4 of 23 Table 2 Antiangiogenic drugs associated with MRONJ IV Intravenous MM Multiple myeloma PO Orally SC Subcutaneous Btl Bottle Tab Tablet Pharmacologic Active Ingredient Formulation Route of Administration Indication and Frequency Bevacizumab Btl 400 mg Btl 100 mg IV Metastatic breast cancer 10 mg kg every 2 weeks or 15 mg kg every 3 weeks colorectal cancer 5 mg kg or 10 mg kg every 2 weeks lung ovarian cancer 7 5 mg kg or 15 mg kg every 3 weeks renal cell cancer 10 mg kg every 2 weeks glioblastoma 10 mg kg every 2 weeks Sunitinib Tab 12 5 mg PO Renal cell cancer GISTs and neuroendocrine tumours 50 mg day for 4 weeks Sorafenib Tab 200 mg PO Renal cell cancer 800 mg day Pazopanib Tab 200 mg Tab 400 mg PO Renal cell cancer 200 800 mg day Thalidomide Tab 50 mg PO Myeloma 400 mg day for 6 weeks Lenalidomide Tab 5 10 15 and 25 mg PO Myeloma tailored doses Everolimus Tab 5 and 10 mg PO Renal cell cancer breast cancer 10 mg every day Temsirolimus Btl 30 mg IV Renal cell cancer 25 mg every week Table 3 MRONJ staging from the American Association of Oral and Maxillofacial Surgeons AAOMS position paper 2014 6 Stage MRONJ Clinical Findings At risk category No apparent necrotic bone in patients who have been treated with either oral or IV bisphosphonates Stage 0 No clinical evidence of necrotic bone but non specific clinical findings radiographic changes and symptoms Stage 1 Exposed and necrotic bone or fistulae that probes to bone in patients who are asymptomatic and have no evidence of infection Stage 2 Exposed and necrotic bone or fistulae that probes to bone associated with infection as evidenced by pain and erythema in the region of the exposed bone with or without purulent drainage Stage 3 Exposed and necrotic bone or a fistula that probes to bone in patients with pain infection and one or more of the following exposed and necrotic bone extending beyond the region of alveolar bone i e inferior border and ramus in the mandible maxillary sinus and zygoma in the maxilla resulting in pathologic fracture extra oral fistula oral antral oral nasal communication or osteolysis extending to the inferior border of the mandible of sinus floor
Appl Sci 2019 9 1026 5 of 23 Table 4 MRONJ staging clinical and radiological findings proposed by Campisi et al 2011 10 Stage MRONJ Features Stage 1 Focal ONJ Clinical signs and symptoms bone exposure sudden dental mobility non healing post extraction socket mucosal fistula swelling abscess formation trismus and gross mandible deformity hypoesthesia paraesthesia of the lips CT signs increased bone density limited to the alveolar bone region trabecular thickening and focal osteosclerosis with or without the following signs markedly thickened and sclerotic lamina dura persisting alveolar socket and cortical disruption Stage 2 Diffuse ONJ Clinical signs and symptoms same as stage 1 CT signs increased bone density extended to the basal bone diffuse osteosclerosis with or without the following signs prominence of the inferior alveolar nerve canal periosteal reaction sinusitis sequestra formation and oro antral fistula Stage 3 Complicated ONJ Same as stage 2 with one or more of the following Clinical signs and symptoms extra oral fistula displaced mandibular stumps and nasal leakage of fluids CT signs osteosclerosis of adjacent bones zygoma and hard palate pathologic mandibular fracture and osteolysis extending to the sinus floor HBO increases local concentrations of reactive nitrogen species RNS and reactive oxygen species ROS by providing substrates oxygen and L arginine for nitric oxide synthase as well as by the generation of superoxide 19 20 ROS and RNS influence osteoclast OC differentiation and activity and participate in the regulation of various aspects of bone metabolism 21 23 Nitric oxide NO is constitutively synthesised by both OCs and osteoblasts OBs and has contrasting biphasic effects At lower levels NO decreases bone resorption and stimulates its turnover whereas at higher concentrations NO promotes inflammatory processes and inhibits bone formation 24 Indeed ROS stimulate the expression of receptor activator of nuclear factor kappa B ligand RANKL changing the RANKL osteoprotegerin ratio and favouring OC differentiation and avoiding osteopetrosis in animal models 22 25 Authors have also suggested that HBO generated ROS could induce suppression of OC activity and promote bone healing 21 23 Recent research has shown that HBO generated ROS and RNS induce stem cell mobilisation vasculogenesis mitochondrial biogenesis and preconditioning 26 29 Ozone dissolves physically in biological water physiological saline plasma lymph urine All these reagents act as donor electrons and are oxidisable and participate in the ozonation process and the consequent formation of ROSs and lipid oxidation products LOPs These molecules are responsible for the biochemical actions of ozone and function as biochemical regulators of inflammation at distinct times and physiological concentrations 30 31 Through interactions with cellular components and depending on the concentration of ozone in the tissue these molecules can trigger biological effects that are either therapeutic or detrimental to health 30 31 During normal metabolism osteoclasts platelets lymphocytes neutrophils monocytes and fibroblasts can induce the formation of ROS 32 33 When in excess these ROSs can trigger damage to cellular constituents extracellular components and affect the metabolism of the cells responsible for extracellular matrix synthesis fundamental in tissue repair which leads to apoptosis and cellular necrosis 34 35 The aim of this review is to analyse all available evidence and evaluate the reported outcome of oxygen therapy as treatment for patients affected by MRONJ
Appl Sci 2019 9 x FOR PEER REVIEW 6 of 26 The aim of this review is to analyse all available evidence and evaluate the reported outcome of oxygen therapy as treatment for patients affected by MRONJ Appl Sci 2019 9 1026 6 of 23 2 Material and Methods systematic review was performed according to Preferred Reporting Items for Systematic 2 This Material and Methods Reviews and Meta Analyses PRISMA guidelines 36 The following databases were interrogated This systematic review was performed according to Preferred Reporting Items for Systematic PubMed EMBASE CINAHL and the Central Register were of Controlled Trials Reviews andMEDLINE Meta Analyses PRISMA guidelines 36 Cochrane The following databases interrogated PubMed MEDLINE EMBASE CINAHL and the Cochrane Register and of Controlled CENTRAL A three stage screening approach was used to Central ensure precision the qualityTrials of the CENTRAL A three stage screening approach was used to ensure precision and the quality of the search The screening of titles and abstracts was carried out independently by three authors RS RL search The screening of titles and abstracts was carried out independently by three authors RS RL and SO eliminate any irrelevant material i e reviews animal studies non clinical studies and and SO toto eliminate any irrelevant material i e reviews animal studies non clinical studies and studiesthat that did not report patients undergoing oxygen therapy treatments Disagreements Disagreementswere were studies did not report patients undergoing oxygen therapy treatments resolved by discussion until a consensus was reached resolved by discussion until a consensus was reached A data screening and abstraction form was used to A data screening and abstraction form was used to 1 Verify the study eligibility derived from the inclusion exclusion criteria 1 Verify the study eligibility derived from the inclusion exclusion criteria 2 2 Carry Carryout outthe themethodological methodologicalquality qualityassessment assessment 3 3 Extract data on study characteristics and studies Extract data on study characteristics andoutcomes outcomesfor forthe theincluded included studies Identification Theauthors authorsofofany anystudies studieseligible eligibleforforinclusion inclusionininthe thereview review unless unlesswithout withoutsufficient sufficient The information were contacted directly Figure information were contacted directly Figure 1 1 PubMed EMBASE Medline CINAHL CENTRAL 78 81 55 9 8 Screening Screened papers after removing duplicates 126 Excluded by Titles Abstract Eligible 104 Manual Screened Full text Search 22 0 Excluded Articles Included 9 Final Selection 13 Figure 1 Study flow diagram Figure 1 Study flow diagram
Appl Sci 2019 9 1026 7 of 23 3 Criteria for Inclusion in this Review 3 1 Types of Studies The types of studies included in the research strategy were published or unpublished randomised controlled trials case controlled trials case series retrospective studies and case reports Papers were obtained from January 2003 to September 2018 Animal studies reviews and those studies including patients with a previous history of radiation therapy to the head and neck regions were excluded No language restrictions were imposed to the search 3 2 Types of Participants The review considered studies involving patients who developed MRONJ and subsequently underwent OT and or HBO treatment No restriction of age gender or ethnic origin was applied There was also no restriction on the minimum number of patients included in the studies 3 3 Types of Interventions Patients affected by MRONJ who underwent OT and or HBO as either standalone or adjuvant treatment were considered 3 4 Objectives The objectives was to assess the therapeutic effects of HBO and OT in patients exposed to antiresorptive or antiangiogenic drugs and affected by MRONJ Moreover it was to assess the effects of OT and HBO therapy as standalone or adjuvant treatments either singly or in combination to other treatments in people with manifest MRONJ 4 Types of Outcome Measures Primary outcomes Healing of MRONJ as indicated by one or more of the following indicators Improvement in the clinical grade of the lesions according to the AAOMS staging of MRONJ Table 3 Wound healing yes or no Plain film radiological examination improvement of sclerotic changes mottling and bone fragmentation improvement of formed sequestrum or persistent extraction sockets computed tomography CT scan magnetic resonance imaging MRI surface area of the bone disease localisation evidence of bone marrow disease positron emission tomography PET CT imaging decreased abnormal focal uptake 37 Healing of sinus tract or deep periodontal pockets Rate of progression of MRONJ Secondary outcomes Quality of life QoL Time to event Rate of complications and side effects of the intervention For the complications outcome measure interventions involving an interruption or delay of antiresorptive or antiangiogenic treatments or progression of the underlying disease e g fracture in osteoporosis or disease progression in cancer were considered to be complications of the intervention
Appl Sci 2019 9 1026 8 of 23 For QoL measures we reported whether validated scales were used Non validated scales were not excluded a priori QoL had to have been measured at baseline and at least once during follow up 5 Data Extracted Data extracted from the studies included number of patients patient gender and age predisposing factors for and localisation of MRONJ type of antiangiogenic or antiresorptive drugs and their cumulative dose clinical indications for the drug or combined therapy type of intervention complications follow up time MRONJ evolution and MRONJ recurrence All selected papers were carefully read to identify author s year of publication study design population and treatment characteristics In the case of missing information we contacted the authors and allowed six weeks for a reply If the information was still missing we then indicated the missing data as Not Reported NR in the text and tables 6 Review Quality Assessment Data Two review authors RS AL appraised the risk of bias in the included study with the tool recommended by the Cochrane Handbook for Systematic Reviews of Interventions as appropriate for randomised control trials RCTs 38 Moreover the authors used the CARE Checklist for case report and the Modified Delphi Checklist for the case series studies 39 40 We referred instances of disagreement in risk of bias assessments to one of the other members of the review team SO and resolved them by discussion 7 Results A total of 13 articles were included in this review Of these 6 reported patients treated with HBO and 7 articles included patients treated using OT All the published data described patients treated from 2006 to 2015 The types of articles included in this research were case series n 9 case reports n 3 and RCTs n 1 41 53 Results were expressed as descriptive statistics because of significant heterogeneity in the published data 7 1 List of Excluded Studies Currently the treatment of MRONJ is controversial but many researchers agree that intravenous drug administration or longer period of drug intake contribute to high risk of developing MRONJ 54 56 We originally considered 22 studies to be potentially eligible for inclusion but after inspection of the full papers 9 were excluded for not meeting the inclusion criteria for this review 57 65 Table 5 Table 5 List of excluded studies Authors Type of Intervention Number of Patients Type of Drug Type of Study Outcome Petrucci et al 2007 57 OT Surgery 12 IV BP Letter to editor 8 patients 75 achieved complete resolution of ONJ and 4 25 achieved improvement with persistence of lesion Agrillo et al 2007 58 OT prevention strategy for dental extraction 15 NR Case Series No development of ONJ Yamazaki et al 2010 59 HBO 1 Oral BP Abstract Improvement with persistence of lesion Karakinaris et al 2013 60 HBO Drug holiday Surgery 25 Unclear Poster Presentation All patients free from ONJ Salcedo Gil et al 2013 61 Retrospective Comparative HBO group vs No HBO group as adjuvant therapy 15 HBO Vs 15 No HBO BP Poster Presentation Significant improvement with persistence of lesion and or stabilization
Appl Sci 2019 9 1026 9 of 23 Table 5 Cont Authors Type of Intervention Number of Patients Type of Drug Type of Study Outcome Zaslavskaya et al 2013 62 OT removal of sequestrum 30 IV BP Poster Presentation All patients free from ONJ Asaka 2014 63 HBO Minimal surgery 8 NR Poster Presentation All patients presented good clinical and radiological result Hamada 2014 64 HBO Surgery stopping BP 3 IV BP and Oral BP Poster Presentation All patients free from ONJ Yahoo et al 2018 65 OT Surgery 2 One on DZB and one on IV BP Poster Presentation All patients free from ONJ 7 2 HBO Study Analysis In total just 6 articles were included in the analysis of HBO therapy comprising case reports n 2 case series n 3 and RCTs n 1 All studies were published from 2006 to 2015 A total of 82 patients with a mean age 66 3 45 female 54 88 and 37 male 45 12 cases were treated using different protocols of HBO therapy Tables 6 and 7 None of the manuscripts reported patients treated with antiangiogenic drugs Table 6 Studies included in the hyperbaric oxygen HBO analysis including number of patients treated and evidence level Case series CS case report CR randomised control clinical trial RCT Levels of Evidence for Prognostic Studies Adapted from the American Society of Plastic Surgeons https www plasticsurgery org Documents medical professionals health policy evidence practice ASPS Rating Scale March 2011 pdf Author s Type of Study Total Number of Patients Level of Evidence Shimura et al 2006 41 CR 1 Level 5 Lee et al 2007 42 CS 2 Level 4 Freiberger et al 2007 43 CS 16 Level 4 Lee et al 2011 44 CS 13 Level 4 Freiberger et al 2012 45 RCT 49 3 patients died at early stage of study Level 2 Fatema et al 2015 46 CR 1 Level 5 The reported indications for antiresorptive drug treatment were multiple myeloma 37 80 osteoporosis 21 95 breast cancer 18 29 prostate cancer 4 88 non Hodgkin lymphoma 2 44 sarcoidosis 1 22 and macroglobulinaemia 1 22 In addition a significant number of patients were logged with no specific indication n 10 12 20 Table 8 The most common site for MRONJ was the mandible 18 29 followed by the maxilla 3 65 In 2 43 of patients MRONJ lesions were reported in both Table 7 However in 75 60 the MRONJ site was not reported NR The drug most commonly responsible of MRONJ was Zoledronate 12 19 but only 33 patients out of 82 had this detail reported 40 24 HBO was most commonly used as a neoadjuvant and or adjuvant therapy followed by surgery in 4 studies out of 6 In one study the HBO therapy was given as standalone treatment Table 9 The patients were followed for a period of time ranging from 1 to 32 months At the end of the follow up MRONJ was seen as completely resolved in 5 17 of the cases n 3 while the majority 48 27 of the patients n 28 were reported to have some benefit due to stability or improvement of the disease presentation In just 10 34 of patients n 6 the disease progressed but for 13 patients 22 41 data were not available Table 10
Appl Sci 2019 9 1026 10 of 23 Table 7 HBO Preoperative epidemiologic analysis age sex predisposing factors and site of the necrosis involved M male F female not reported NR Standard of Care StC Study Patient Numbers Age Sex Triggering Cause Site of the Necrosis Involved Shimura et al 2006 41 1 60 M Spontaneous 1 in mandible Lee et al 2007 42 2 84 F 76 M Dental implant Bone graft surgery 1 in the maxilla 1 in the mandible Freiberger et al 2007 43 16 63 F 69 F 57 M 53 M 70 M 45 F 62 M 59 M 78 F 56 M 52 M 52 F 72 M 77 M 43 F 63 M total patients 6 female and 10 male NR 12 in the mandible 2 in the maxilla 2 in both maxilla and mandible Lee et al 2011 44 13 62 M 87 M 54 F 81 F 68 M 75 F 70 F 70 F 57 F 83 F 76 M 74 F 62 F total patients 4 male and 9 female NR NR Freiberger et al 2012 45 27 StC group 22 HBO StC group Total Patients 46 3 early dead during study 2 on the StC StC group and 1 on the HBO StC group mean age 66 years 57 female NR NR Fatema et al 2015 46 1 80 F Dental extraction 1 in the mandible
Appl Sci 2019 9 1026 11 of 23 Table 8 HBO preoperative pharmacological analysis type of drugs indication for drug therapy and time of drug exposure Minodronate MI Zoledronate acid ZOL Pamidornate PAM Bisphosphonate BP Alendronate ALD Risedronate RES Ibadronate IBA Osteoporosis OP Multiple Myeloma MM Breast Cancer BC Sarcoidosis SC Prostate Cancer PC non Hodgkin lymphoma nHL Unclear the number expressed do not match the actual sample analysed Not reported NR Study Type of Drug Indication for Drug Therapy Time of Drug Exposure Shimura et al 2006 41 MI MM 1 32 months Lee et al 2007 42 2 ALD OP 2 1 in more than 108 months 1 NR Freiberger et al 2007 43 2 ZOL PAM 7 ZOL 6 BP unknown 1 PAM BC 3 MM 10 Macroglobulinemia 1 SC 1 PC 1 Unclear Lee et al 2011 44 ZOL 3 ALD 6 RES 3 IBA 1 OP 7 MM 1 PC 3 nHL 2 NR Freiberger et al 2012 45 Unclear OP C group 5 S group 3 MM C group 9 S group 10 BC C group 7 S group 5 Other indication C group 6 S group 4 Unclear Fatema et al 2015 46 RES OP 24 months
Appl Sci 2019 9 1026 12 of 23 Table 9 HBO operative analysis including type of intervention and the stage of the disease Platelet Rich Plasma PRP Standard of Care StC Antibiotics ABX Mouthwash MW American Association of Oral and Maxillofacial Surgery AAOMS not applicable N A Study Type of Intervention Number of Cycles Pre Operative Number of Cycles Post Operative AAOMS Staging of Disease Shimura et al 2006 41 HBO clarithromycin and levofloxacin followed by dexamethasone at 20 mg daily for 4 days N A N A Stage 2 Lee et al 2007 42 Sequestrectomy PRP No 1 case 20 HBO at 2 4 atmospheres pressure for 90 min The other case no HBO due to medical condition No 2 case NR No 1 10 HBO at the conclusion of surgical treatment The other case no HBO due to medical condition No 2 case NR NR Freiberger et al 2007 43 11 Debridement 1 Resection 4 just HBO Unclear Unclear NR Lee et al 2011 44 Unclear NR NR Stage 0 4 Stage I 1 Stage 2 5 Stage 3 3 Freiberger et al 2012 45 StC surgery ABX MW 21 Control Group HBO StC surgery ABX MW 25 Study Group 0 40 NR Fatema et al 2015 46 Drug Holiday ABX surgery 20 10 Stage 2
Appl Sci 2019 9 1026 13 of 23 Table 10 HBO analysis of the MRONJ status at the end of follow up not reported NR poor patient compliance PPC computer tomography CT RCT Freiberger et al 2012 45 showed no statistically significant improvement in cure rate compared to placebo but there was improvement in secondary outcome Study Follow up Time Type of Special Investigation Used during Patients Follow up Treatment Complications during the Study MRONJ Status after Treatment at the End of Follow up Shimura et al 2006 41 NR NR Patient developed acute otitis media HBO interrupted and re started Stable Lee et al 2007 42 9 months CT 1 NR 1 Complete resolution Freiberger et al 2007 43 From 1 to 32 months NR PPC 1 Multiple surgery 2 HBO therapy more than one time 4 Remission 8 50 Stable 2 12 5 Progression 6 37 5 Lee et al 2011 44 NR NR NR NR 17 of 25 68 improved Complete resolution Freiberger et al 2012 45 24 months NR Fatality 3 after 3 months HBO declined 1 Immediate Crossover to HBO Group 2 Late Crossover to HBO 3 Fatema et al 2015 46 NR NR
Appl Sci 2019 9 1026 14 of 23 7 3 OT Study Analysis For OT there were just 7 studies for analysis Study types were described as case reports n 1 and case series n 6 All these studies were published from 2006 to 2014 Table 11 Table 11 Studies included in the OT analysis including number of patients treated and evidence level Case series CS Case report CR Levels of Evidence for Prognostic Studies Adapted from the American Society of Plastic Surgeons https www plasticsurgery org Documents medicalprofessionals health policy evidence practice ASPS Rating Scale March 2011 pdf Author s Type of Study Total Number of Patients Level of Evidence Agrillo et al 2006 47 Agrillo et al 2007 48 Ripamonti et al 2011 49 Agrillo et al 2012 50 Ripamonti et al 2012 51 Brakus et al 2013 52 Brozoski et al 2014 53 CS CS CS CS CS CR CS 30 33 10 131 24 1 2 Level 4 Level 4 Level 4 Level 4 Level 4 Level 5 Level 4 A total of 231 patients were reported 124 female 53 67 and 74 male 32 03 with 14 28 of patients n 33 of unreported gender Patients were treated using different OT protocols The pooled mean of age of these patients was 60 7 years The most common indications for antiresorptive treatment was multiple myeloma 35 93 breast cancer 27 70 prostate cancer 6 49 lung cancer 6 49 renal cancer 3 46 uterine cancer 0 43 non Hodgkin lymphoma 0 43 and osteoporosis with lymphoma and thyroid cancer 4 76 In a significant number of patients 14 28 the drug therapy indication was not reported Tables 12 and 13 The most common site for MRONJ was the mandible 43 72 followed by the maxilla 22 94 In 8 65 of cases MRONJ was reported in both and the site was not reported in 24 67 of cases Table 12 The drug most commonly responsible for MRONJ was Zoledronate 14 71 However only 37 patients out of 231 had details of the specific MRONJ associated drug reported 16 01 OT was most commonly used as a neoadjuvant and or adjuvant therapy followed by surgery in 6 studies out of 7 Table 14 The patients were followed for a period of time ranging from 7 to 36 months At the end of the follow up MRONJ was completely resolved in 44 58 of patients n 103 whilst 22 94 showed some improvement or remission of the disease n 53 No progression of the disease has been reported in any studies Table 15 however for 30 patients 12 98 this data was not available
Appl Sci 2019 9 1026 15 of 23 Table 12 OT Preoperative epidemiologic analysis age sex predisposing factors and site of the necrosis involved Male M female F not reported NR Study Age Sex MRONJ Aetiology Site of Necrosis Agrillo et al 2006 47 10 M and 20 F age ranging from 46 to 79 years old mean age was 63 years Unclear 7 patients 23 3 in the maxilla 18 patients 60 in the mandible 5 patients presented with exposed necrotic bone in both maxilla and mandible 16 7 Agrillo et al 2007 48 Unclear Unclear Unclear Ripamonti et al 2011 49 2 M and 8 F age ranging from 53 to 77 years old mean age 65 years old 8 patients after extraction 2 from prosthetic dentures 9 in the mandible and 1 in the maxilla Agrillo et al 2012 50 49 M and 82 F age ranging from 38 and 82 years old mean age was 60 years old 70 52 came after dental extraction with exposure of necrotic bone in the same area 36 27 5 spontaneous exposure of alveolar bone 25 patients NR 43 patients 33 in the maxilla 73 patients 55 2 in the mandible 15 patients presented with exposed necrotic bone in both maxilla and mandible 11 8 Ripamonti et al 2012 51 12 M and 12 F age ranging 41 80 years old mean age 62 5 years old NR NR Brakus et al 2013 52 1 F 68 year old Dental extraction Maxilla Brozoski et al 2014 53 1 M 68 year old 1 F 62 year old 2 patients dental extraction 1 Maxilla 1 Mandible
Appl Sci 2019 9 1026 16 of 23 Table 13 Preoperative pharmacological analysis type of drugs indication for drug therapy and time of drug exposure Zoledronate acid ZOL Pamidornate PAM Alendronate ALD Risedronate RES Osteoporosis OP Multiple Myeloma MM Breast Cancer BC Prostate Cancer PC Unclear the number expressed do not match the actual sample analysed Not reported NR Non Hodgkin Lymphoma nHL Lung Cancer LC Uterine Cancer UC Renal cancer RC Thyroid cancer TC Study Type of Drug Indication for Drug Therapy Time of Drug Exposure Agrillo et al 2006 47 NR 23 MM 5 BC 1 UC 1 PC NR Agrillo et al 2007 48 NR NR NR Ripamonti et al 2011 49 9 ZOL 1 PAM 6 BC 2 MM 1 PC 1 nHL NR NR 56 MM 41 BC 11 LC 8 PC 8 RC 7 OP Lymphoma and TC NR Ripamonti et al 2012 51 24 ZOL 11 BC 4 PC 4 LC 3 OP 2 MM Ranging from 10 to 18 months Brakus et al 2013 52 PAM BC 42 months Brozoski et al 2014 53 1 ZOL 1 ALD RES 1 PC 1 OP 21 months ZOL 48 months ALD 24 months RES Agrillo et al 2012 50 Table 14 Ozone therapy OT operative analysis including type of intervention and the stage of the disease Spontaneous expulsion of necrotic bone SENB antibiotics ABX American Association of Oral and Maxillofacial Surgery AAOMS not reported NR Study Type of Intervention Number of Cycles Pre Operative Number of Cycles Post Operative AAOMS Staging of Disease Agrillo et al 2006 47 Surgical debridement ABX Unclear Unclear Stage 1 Agrillo et al 2007 48 Surgical debridement 1 8 session of 3 min OT ABX antifungal 1 8 session of 3 min OT ABX antifungal Vitamin C NR Ripamonti et al 2011 49 ABX ultrasonic scaling 3 to10 applications of OT oil mean applications were 5 5 None NR Weitzman et al 2007 staging utilised Agrillo et al 2012 50 Curettage or sequestrectomy None Unclear NR Ripamonti et al 2012 51 ABX followed by SENB and or sequestrectomy 3 to 38 applications of OT gas mean applications were 11 None No AAOMS used Weitzman et al 2007 Brakus et al 2013 52 Debridement ABX initially eventually radical surgery 7 applications None Stage 2 Brozoski et al 2014 53 Mouthwash Surgical debridement Unclear None Stage 2 1 Stage NR 1
Appl Sci 2019 9 1026 17 of 23 Table 15 OT analysis of the MRONJ status at the end of follow up Orthopantomograph OPG not reported NR Study Follow up Time Type of Special Investigation Used during Patient s Follow Up Treatment Complications during the Study MRONJ Status after Treatment at the End of Follow Up Agrillo et al 2006 47 NR NR NR NR 18 patients 54 completed healing of the lesion 10 patients 30 experienced reduction of the lesion dimension 5 patients 16 showed no clinically relevant improvement outcomes on the lesion Agrillo et al 2007 48 7 months NR NR Ripamonti et al 2011 49 8 months NR None Agrillo et al 2012 50 Unclear NR 37 patients withdrawn from the research 57 patients had complete resolution 60 28 patients had reduction of the dimension of lesions 30 9 patients 10 showed no clinically relevant improvement outcomes on the lesion Ripamonti et al 2012 51 Range 12 to 36 months mean 18 months NR 7 patients interrupted the treatment with OT for disease progression and 1 for fear of an experimental therapy 16 patients have shown complete resolution of the MRONJ Brakus et al 2013 52 Unclear Unclear None Reduction of the dimension of lesions Brozoski et al 2014 53 36 months 1 18 months 1 OPG None Complete resolution All patients have shown sign of healing of the lesion
Appl Sci 2019 9 1026 18 of 23 8 Risk of Bias and Review Quality Assessment In all three case report studies we identified a lack of clarity in many of the thirteen domains of the CARE Checklist with missing information We found that the lack of clarity was predominantly on follow up and diagnostic procedures at the time of follow up Hence we concluded the level of bias to be high for all the included case reports In the nine case series studies we reported a consistent lack of clarity in some of the seven domains of the Modified Delphi Checklist These were predominantly regarding the outcome measurement methods hence we considered the level of bias to be high for all case series studies The only eligible RCT was an evaluation of adjuvant HBO therapy for people undergoing surgery The authors of the study did not mention the generation of randomisation sequences but reported the concealment of allocation using a series of opaque envelopes containing the assignment and we therefore rated the level of risk as unclear The personnel involved in the study were not blinded because this was deemed to be impractical The loss of patients to follow up was substantial and although a clear description of losses and withdrawals was given data analysis was performed as treated Moreover the study had a very high and unbalanced rate of crossovers between study arms Therefore we considered the level of risk of bias to be high across the study 41 53 9 Discussion Antiresorptive drugs are known to improve the quality of life for patients affected by bone metastasis osteoporosis osteopenia and Paget disease Moreover the new antiangiogenic drugs have been shown to be effective treatment modalities for a number of cancers Unfortunately increased use of these drugs has also increased the numbers of patients developing MRONJ The risk appears to be highest in patients who require intravenous drug administration or an intake period greater than two years 12 54 55 Moreover the literature suggests that local and systemic factors such as periodontal disease and diabetes might act as predisposing factors in developing MRONJ Although no gold standard is currently available for the treatment of MRONJ a number of studies debate which MRONJ stage benefits the most from surgical or conservative therapy 15 56 In general the common opinion appears to be that for early stages of the disease stage 0 or I conservative management might be sufficient 6 54 The purpose of this systematic review was to analyse the current evidence related to the treatment of MRONJ when using oxygen therapy OT and HBO Our findings indicate that the oxygen therapy has been used as a neoadjuvant or adjuvant therapy and may represent a viable complementary treatment or an alternative in advanced stage disease stage II and III where patients are unfit for aggressive surgery such as jaw resections or microvascular reconstruction Despite the majority of studies reviewed presenting low quality evidence with a high risk of bias there is some evidence to show the total resolution of MRONJ in 44 58 of patients with OT and 5 17 of patients with HBO although this could equally have happened without these interventions In addition in a number of OT studies the spontaneous sequestration of necrotic bone was followed by a spontaneous expulsion 47 53 The only reported cases of MRONJ progression were amongst patients treated with HBO 10 34 n 6 Unfortunately these outcomes were not reported for 13 73 n 43 which could represent further cases of disease progression This review also found that in the majority of the MRONJ cases antiresorptive drugs were explicitly discontinued if deemed safe from the oncological point of view 41 53 However it is unclear if the discontinuation strategy leads to a better surgical outcome due to the long skeletal life of some antiresorptive drugs Amongst all the studies we have found several perplexities which have had an impact in the quality of the research Indeed we have noticed that in 11 articles out of 13 there was no mention of any specific investigations during the patients follow up Only Lee et al 42 and Brozoski et al 53 have reported during the follow up that patients had either a CT or an orthopantomograph OPG to assess the radiological aspect of the MRONJ lesions Moreover other important data were missing
Appl Sci 2019 9 1026 19 of 23 in many of the articles such as cumulative drug dose prior to developing MRONJ and patients predisposing factors such as other medical conditions and dental history Only one article utilised a QoL questionnaire to assess baseline and post treatment levels at six months The questionnaire evaluates six health domains physical mental social general perceived health and self esteem and four dysfunction measurements anxiety depression pain and disability reporting no statistically significant differences between the two groups 45 It is understandable that due to the limited incidence of MRONJ it is difficult to improve the quality of evidence unless a common effort is applied Therefore the authors believe that additional high level evidence studies such as multi centre studies case controlled studies or randomised controlled trials are necessary to support the efficacy and the success of oxygen therapy in managing MRONJ The authors advocate in general that the following rules should be applied for MRONJ treatment research protocols Diagnosis and staging of the disease should be assessed with standardised reproducible scales and should be calibrated amongst the clinicians involved in the study If randomisation is feasible it should be carried out and described in sufficient detail to allow an assessment of whether it produced comparable groups Common quantifiable and clinically relevant endpoints time to complete wound healing pain specific investigations treatment acceptability and participant satisfaction should be described in a sufficiently detailed manner A long follow up period of at least six months is essential if treatment effects on indolent often long standing MRONJ sites are to be detected 10 Conclusions MRONJ is becoming an increasingly significant iatrogenic complication for patients undergoing antiresorptive and antiangiogenic drug therapy as these important medications reduce the morbidity and mortality rates associated with the primary disease Unfortunately the management of MRONJ remains controversial This is the first systematic review of oxygen therapy for the management of MRONJ and highlights the absence of high level evidence in the literature Therefore it is currently difficult to suggest OT is better or worse than HBO or whether it is better than a placebo In the absence of effective MRONJ treatment strategies the available data does however suggest that further well designed clinical studies are warranted to improve the evidence base for both OT and HBO in the management of MRONJ Author Contributions Roberto Sacco Racheal Leeson and Anand Lalli conceived the presented systematic review idea and the design of the study Roberto Sacco Joseph Nissan Sergio Olate Carlos Henrique Bettoni Cruz de Castro and Alessandro Acocella contributed to the acquisition analysis and the interpretation of data for the work Roberto Sacco Racheal Leeson Joseph Nissan Sergio Olate Carlos Henrique Bettoni Cruz de Castro Alessandro Acocella and Anand Lalli drafted the paper revised it critically and finally approved the version to be published Funding This research received no external funding Acknowledgments We would like to thank Professor Stefano Fedele Oral Medicine Department Eastman Dental Institute London UK for the comments that greatly improved the manuscript Conflicts of Interest The authors declare no conflict of interest References 1 Coleman R Body J J Aapro M Hadji P Herrstedt J Bone health in cancer patients ESMO clinical practice guidelines Ann Oncol 2014 25 Suppl 3 iii124 iii137 CrossRef PubMed
Appl Sci 2019 9 1026 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 of 23 Hanley D A McClung M R Davison K S Dian L Harris S T Miller P D Lewiecki E M Kendler L K Writing Group for the Western Osteoporosis Alliance Western osteoporosis alliance clinical practice series Evaluating the balance of benefits and risks of long term osteoporosis therapies Am J Med 2017 130 862 e1 862 e7 CrossRef PubMed Ruggiero S L Mehrotra B Rosenberg T J Engroff S L Osteonecrosis of the jaws associated with the use of bisphosphonates A review of 63 cases J Oral Maxillofac Surg 2004 62 527 534 CrossRef PubMed Sivolella S Lumachi F Stellini F Favero L Denosumab and anti angiogenetic drug related osteonecrosis of the jaw An uncommon but potentially severe disease Anticancer Res 2013 33 1793 1798 PubMed Brunello A Saia G Bedogni A Scaglione D Basso U Worsening of osteonecrosis of the jaw during treatment with sunitinib in a patient with metastatic renal cell carcinoma Bone 2009 44 173 175 CrossRef PubMed Ruggiero S L Dodson T B Fantasia J Goodday R Aghaloo T Mehrotra B O Ryan F American Association of Oral and Maxillofacial Surgeons position paper on medication related osteonecrosis of the jaw 2014 update J Oral Maxillofac Surg 2014 72 1938 1956 CrossRef PubMed Rosella D Papi P Giardino R Cicalini E Piccoli L Pompa G Medication related osteonecrosis of the jaw Clinical and practical guidelines J Int Soc Prev Community Dent 2016 6 97 104 PubMed Ruggiero S L Dodson T B Assael L A Landesberg R Marx R E Mehrotra B American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate related osteonecrosis of the jaws 2009 update J Oral Maxillofac Surg 2009 67 2 12 PubMed Mawardi H Treister N Richardson P Anderson K Munshi N Faiella R A Woo S B Sinus tracts an early sign of bisphosphonate associated osteonecrosis of the jaws J Oral Maxillofac Surg 2009 67 593 601 CrossRef Campisi G Lo Russo L Agrillo A Vescovi P Fusco V Bedogni A BRONJ expert panel recommendation of the Italian Societies for Maxillofacial Surgery SICMF and Oral Pathology and Medicine SIPMO on Bisphosphonate Related Osteonecrosis of the Jaws Risk assessment preventive strategies and dental management Ital J Maxillofac Surg 2011 22 103 124 Vahtsevanos K Kyrgidis A Verrou E Katodritou E Triaridis S Andreadis C G Boukovinas I Koloutsos G E Teleioudis Z Kitikidou K et al Longitudinal cohort study of risk factors in cancer patients of bisphosphonate related osteonecrosis of the jaw J Clin Oncol 2009 27 5356 5362 CrossRef PubMed Saad F Brown J E Van Poznak C Ibrahim T Stemmer S M Stopeck A T Diel I J Takahashi S Shore N Henry D H et al Incidence risk factors and outcomes of osteonecrosis of the jaw Integrated analysis from three blinded active controlled phase III trials in cancer patients with bone metastases Ann Oncol 2012 23 1341 1347 CrossRef PubMed Heufelder M J Hendricks J Remmerbach T Frerich B Hemprich A Wilde F Principles of oral surgery for prevention of bisphosphonate related osteonecrosis of the jaw Oral Surg Oral Med Oral Pathol Oral Radiol 2014 117 e429 e435 CrossRef PubMed Voss P J Joshi Oshero J Kovalova M ller A Veigel Merino E A Sauerbier S Al Jamali J Lemound J Metzger M C Schmelzeisen R Surgical treatment of bisphosphonate associated osteonecrosis of the jaw Technical report and follow up of 21 patients J Craniomaxillofac Surg 2012 40 719 725 CrossRef PubMed Marx R E Sawatari Y Fortin M Broumand V Bisphosphonate induced exposed bone osteonecrosis osteopetrosis of the jaws Risk factors recognition prevention and treatment J Oral Maxillofac Surg 2005 63 1567 1575 CrossRef PubMed Marx R E A new concept in the treatment of osteoradionecrosis J Oral Maxillofac Surg 1983 41 351 CrossRef Knighton D R Fiegel V D Halverson T Schneider S Brown T Wells C L Oxygen as an antibiotic The effect of inspired oxygen on bacterial clearance Arch Surg 1990 125 97 CrossRef Seidler V Linetskiy I Hub lkov H Stankov H mucler R Maz nek J Ozone and its usage in general medicine and dentistry A review article Prague Med Rep 2008 109 5 13 Boykin J V Jr Baylis C Hyperbaric oxygen therapy mediates increased nitric oxide production associated with wound healing A preliminary study Adv Skin Wound Care 2007 20 382 CrossRef
Appl Sci 2019 9 1026 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 21 of 23 Allen B W Demchenko I T Piantadosi C A Two faces of nitric oxide Implications for cellular mechanisms of oxygen toxicity J Appl Physiol 2009 106 662 CrossRef Lee N K Choi Y G Baik J Y Han S Y Jeong D W Bae Y S Kim N Lee S Y A crucial role for reactive oxygen species in RANKL induced osteoclast differentiation Blood 2005 106 852 CrossRef Bai X C Lu D Liu A L Zhang Z M Li X M Zou Z P Zeng W S Cheng B L Luo S Q Reactive oxygen species stimulates receptor activator of NF kappaB ligand expression in osteoblast J Biol Chem 2005 280 17497 CrossRef PubMed Reddy S V Regulatory mechanisms operative in osteoclasts Crit Rev Eukaryot Gene Expr 2004 14 255 CrossRef PubMed Van t Hof R J Ralston S H Nitric oxide and bone Immunology 2001 103 255 CrossRef PubMed Khosla S Minireview The OPG RANKL RANK system Endocrinology 2001 142 5050 CrossRef PubMed Li Z Liu W Kang Z Lv S Han C Yun L Sun X Zhang J Mechanism of hyperbaric oxygen preconditioning in neonatal hypoxia ischemia rat model Brain Res 2008 1196 151 CrossRef Thom S R Bhopale V M Velazquez O C Goldstein L J Thom L H Buerk D G Stem cell mobilization by hyperbaric oxygen Am J Physiol Heart Circ Physiol 2006 290 H1378 CrossRef Lee C C Chen S C Tsai S C Wang B W Liu Y C Lee H M Shyu K G Hyperbaric oxygen induces VEGF expression through ERK JNK and c Jun AP 1 activation in human umbilical vein endothelial cells J Biomed Sci 2006 13 143 CrossRef Gutsaeva D R Suliman H B Carraway M S Demchenko I T Piantadosi C A Oxygen induced mitochondrial biogenesis in the rat hippocampus Neuroscience 2006 137 493 CrossRef Bocci V Ozone as Janus This controversial gas can be either toxic or medically useful Mediat Inflamm 2004 13 3 11 CrossRef Bocci V A Scientific and medical aspects of ozone therapy State of the Art Arch Med Res 2006 37 425 435 CrossRef Re L Maysouf M N Men ndez S Le n O S S nchez G M Hern ndez F Ozone therapy Clinical and basic evidence of its therapeutic potential Arch Med Res 2008 39 17 26 CrossRef Gracer R I Bocci V Can the combination of localized proliferative therapy with minor ozonated autohemotherapy restore the natural healing process Med Hypotheses 2005 65 752 759 CrossRef PubMed Bhusari B M Mahajan R Rajbhoj S Shah P Reactive Oxygen Species Its Role in Periodontal Disease J Dent Med Sci 2014 13 52 59 Cardoso C C Carvalho J C Ovando E C Macedo S B Dall Aglio R Ferreira L R Action of ozonized water in preclinical inflammatory models Pharmacol Res 2000 42 51 54 CrossRef Liberati A Altman D G Tetzlaff J Mulrow C G tzsche P C Ioannidis J P Clarke M Devereaux P J Kleijnen J Moher D The PRISMA statement for reporting systematic reviews andmeta analyses of studies that evaluate healthcare interventions Explanation and elaboration Br Med J 2009 339 b2700 CrossRef Raje N Woo S B Hande K Yap J T Richardson P G Vallet S Treister N Hideshima T Sheehy N Chhetri S et al Clinical radiographic and biochemical characterization of multiple myeloma patients with osteonecrosis of the jaw Clin Cancer Res 2008 14 2387 2395 CrossRef Higgins J P T Green S Eds Cochrane Handbook for Systematic Reviews of Interventions Version 5 1 0 updated March 2011 The Cochrane Collaboration 2011 Available online www cochrane handbook org accessed on 22 December 2018 Riley D S Barber M S Kienle G S Aronson J K von Schoen Angerer T Tugwell P Kiene H Helfand M Altman D G Sox H et al CARE guidelines for case reports Explanation and elaboration document J Clin Epidemiol 2017 89 218 235 CrossRef Moga C Guo B Schopflocher D Harstall C Development of a Quality Appraisal Tool for Case Series Studies Using a Modified Delphi Technique 2012 Available online https www ihe ca publications development of a quality appraisal tool for case series studies using a modified delphi technique pdf accessed on 22 December 2018
Appl Sci 2019 9 1026 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 22 of 23 Shimura K Shimazaki C Taniguchi K Akamatsu S Okamoto M Uchida R Nomura K I Inaba T Horiike S Kanamura N Hyperbaric oxygen in addition to antibiotic therapy is effective for bisphosphonate inducedosteonecrosis of the jaw in a patient with multiple myeloma Int J Hematol 2006 84 343 345 CrossRef Lee C Y David T Nishime M Use of platelet rich plasma in the management of oral biphosphonate associated osteonecrosisof the jaw A report of 2 cases J Oral Implantol 2007 33 371 382 CrossRef Freiberger J J Padilla Burgos R Chhoeu A H Kraft K H Boneta O Moon R E Piantadosi C A Hyperbaric oxygen treatment and bisphosphonate induced osteonecrosis of the jaw A case series J Oral Maxillofac Surg 2007 65 1321 1327 CrossRef Lee C Y Pien F D Suzuki J B Identification and treatment of bisphosphonate associated actinomycotic osteonecrosis of the jaws Implant Dent 2011 20 331 336 CrossRef Freiberger J J Padilla Burgos R McGraw T Suliman H B Kraft K H Stolp B W Moon R E Piantadosi C A What is the role of hyperbaric oxygen in the management of bisphosphonate relatedosteonecrosis of the jaw A randomized controlled trial of hyperbaric oxygen as an adjunct to surgery and antibiotics J Oral Maxillofac Surg 2012 70 1573 1583 CrossRef Fatema C N Sato J Yamazaki Y Hata H Hattori N Shiga T Tamaki N Kitagawa Y FDG PET may predict the effectiveness of hyperbaric oxygen therapy in a patient with bisphosphonate related osteonecrosis of the jaw Report of a case Odontology 2015 103 105 108 CrossRef Agrillo A Petrucci M T Tedaldi M Mustazza M C Marino S M Gallucci C Iannetti G New therapeutic protocol in the treatment of avascular necrosis of the jaws J Craniofac Surg 2006 17 1080 1083 CrossRef Agrillo A Ungari C Filiaci F Priore P Iannetti G Ozone therapy in the treatment of avascular bisphosphonate related jaw osteonecrosis J Craniofac Surg 2007 18 1071 1075 CrossRef Ripamonti C I Cislaghi E Mariani L Maniezzo M Efficacy and safety of medical ozone O 3 delivered in oil suspension applications for the treatment of osteonecrosis of the jaw in patients with bone metastases treated with bisphosphonates Preliminary results of a phase I II study Oral Oncol 2011 47 185 190 CrossRef Agrillo A Filiaci F Ramieri V Riccardi E Quarato D Rinna C Gennaro P Cascino F Mitro V Ungari C Bisphosphonate related osteonecrosis of the jaw BRONJ 5 year experience in the treatment of 131 cases with ozone therapy Eur Rev Med Pharmacol Sci 2012 16 1741 1747 Ripamonti C I Maniezzo M Boldini S Pessi M A Mariani L Cislaghi E Efficacy and tolerability of medical ozone gas insufflations in patients with osteonecrosis of the jaw treated with bisphosphonates Preliminary data Medical ozone gas insufflation in treating ONJ lesions J Bone Oncol 2012 1 81 87 CrossRef Brakus I Brakus R B Poljak K Zore I F Aquacel Ag and Ozone in Bisphosphonate Induced Osteonecrosis of the Jaws BIONJ Therapy A Case Report Acta Stomatal Croat 2013 47 241 245 CrossRef Brozoski M A Lemos C A Da Gra a Nacl rio Homem M Deboni M C Adjuvant aqueous ozone in the treatment of bisphosphonate induced necrosis of the jaws Report of two cases and long term follow up Minerva Stomatol 2014 63 35 41 Henry D H Costa L Goldwasser F Hirsh V Hungria V Prausova J Scagliotti G V Sleeboom H Spencer A Vadhan Raj S Randomized double blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer excluding breast and prostate cancer or multiple myeloma J Clin Oncol 2011 29 1125 1132 CrossRef Fung P P L Bedogni G Bedogni A Petrie A Porter S Campisi G Bagan J Fusco V Saia G Acham S Time to onset of bisphosphonate related osteonecrosis of the jaws A multicenter retrospective cohort study Oral Dis 2017 23 477 483 CrossRef Stockmann P Vairaktaris E Wehrhan F Seiss M Schwarz S Spriewald B Neukam F W Nkenke E Osteotomy and primary wound closure in bisphosphonate associated osteonecrosis of the jaw A prospective clinical study with 12 months follow up Support Care Cancer 2010 18 449 460 CrossRef Petrucci M T Gallucci C Agrillo A Mustazza M C Fo R Role of ozone therapy in the treatment of osteonecrosis of the jaws in multiple myeloma patients Haematologica 2007 92 1289 1290 CrossRef
Appl Sci 2019 9 1026 58 59 60 61 62 63 64 65 23 of 23 Agrillo A Sassano P Rinna C Priore P Iannetti G Ozone therapy in extractive surgery on patients treated with bisphosphonates J Craniofac Surg 2007 18 1068 1070 CrossRef Yamazaki Y Kitagawa Y Hata H Abe T Murai C Shiga T Tamaki N Use of FDG PET to evaluate hyperbaric oxygen therapy for bisphosphonate related osteonecrosis of the jaw Clin Nucl Med 2010 35 590 591 CrossRef Karakinaris G Triantafillidou K Bisphosphonate related osteonecrosis of the jaws Treatment protocol including hyperbaric oxygen therapy and surgical intervention Oral Oncol 2013 49 S80 S92 Salcedo Gil C A Iriarte Ortabe J I Pastor Fortea M J Lasa Menendez V Batle Vidal J M Hyperbaric oxygen as an adjuntive therapy in the treatment of bisphosphonate related osteonecrosis of the jaws Int J Oral Maxillofac Surg 2013 42 1190 Zaslavskaya N Drobyshev A Volkow A Dikopova N Shipkova T Efficiency of ozone therapy in the treatment of bisphosphonate related osteonecrosis of the jaws in patients with malignant diseases Int J Oral Maxillofac Surg 2013 42 1192 CrossRef Asaka T Kitagawa Y Hata H Sato J Satoh A Miyakoshi M The usefulness of FDG PET for monitoring hyperbaric oxygen therapy in treatment of bisphosphonate related osteonecrosis of jaws BRONJ J Oral Maxillofac Surg 2014 72 e90 CrossRef Hamada S Surgical treatment with hyperbaric oxygen in the management of bisphosphonate related osteonecrosis of jaw J Oral Maxillofac Surg 2014 72 e91 e92 CrossRef Yahoo A L Soares A L Bortolotti C Gil D G Gadelha M E Teixeira C H The use of medicinal ozone in the treatment of maxillary bone necrosis medications related MRNOJ Support Care Cancer 2018 26 LB029 2019 by the authors Licensee MDPI Basel Switzerland This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution CC BY license http creativecommons org licenses by 4 0
2022 8 22 Hadanny et al Sports Medicine Open https doi org 10 1186 s40798 021 00403 w Open Access ORIGINAL RESEARCH ARTICLE Effects of Hyperbaric Oxygen Therapy on Mitochondrial Respiration and Physical Performance in Middle Aged Athletes A Blinded Randomized Controlled Trial Amir Hadanny1 2 3 Yafit Hachmo4 Daniella Rozali1 Merav Catalogna1 Eldad Yaakobi1 Marina Sova4 Hadar Gattegno4 Ramzia Abu Hamed4 Erez Lang1 Nir Polak1 Mony Friedman1 Shachar Finci1 Yonatan Zemel1 Yair Bechor1 Noga Gal5 and Shai Efrati1 2 5 6 Abstract Introduction Hyperbaric oxygen therapy HBOT has been used to increase endurance performance but has yet to be evaluated in placebo controlled clinical trials The current study aimed to evaluate the effect of an intermittent HBOT protocol on maximal physical performance and mitochondrial function in middle aged master athletes Methods A double blind randomized placebo controlled study on 37 healthy middle aged 40 50 master athletes was performed between 2018 and 2020 The subjects were exposed to 40 repeated sessions of either HBOT two absolute atmospheres ATA breathing 100 oxygen for 1 h or SHAM 1 02ATA breathing air for 1 h Results Out of 37 athletes 16 HBOT and 15 SHAM allocated athletes were included in the final analysis Following HBOT there was a significant increase in the maximal oxygen consumption VO2Max p 0 010 effect size es 0 989 and in the oxygen consumption measured at the anaerobic threshold VO2AT es 0 837 compared to the SHAM group Following HBOT there were significant increases in both maximal oxygen phosphorylation capacity es 1 085 p 0 04 maximal uncoupled capacity es 0 956 p 0 02 and mitochondrial mass marker MTG p 0 0002 compared to the SHAM sessions Conclusion HBOT enhances physical performance in healthy middle age master athletes including VO2max power and VO2AT The mechanisms may be related to significant improvements in mitochondrial respiration and increased mitochondrial mass Trial Registration ClinicalTrials gov Identifier https clini caltr ials gov ct2 show NCT03 524989 May 15 2018 Keywords Hyperbaric oxygen therapy Aging athlete Athletic training Oxygen consumption Mitochondrial function Key points Correspondence amir had gmail com 1 The Sagol Center for Hyperbaric Medicine and Research Shamir AssafHarofeh Medical Center Zerifin Israel Full list of author information is available at the end of the article The current study is the first blinded randomized controlled trial evaluating the effect of repeated HBOT exposures on physical performance The study indicates that HBOT can enhance physical performance in healthy adults The main improve The Author s 2022 Open Access This article is licensed under a Creative Commons Attribution 4 0 International License which permits use sharing adaptation distribution and reproduction in any medium or format as long as you give appropriate credit to the original author s and the source provide a link to the Creative Commons licence and indicate if changes were made The images or other third party material in this article are included in the article s Creative Commons licence unless indicated otherwise in a credit line to the material If material is not included in the article s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use you will need to obtain permission directly from the copyright holder To view a copy of this licence visit http creat iveco mmons org licen ses by 4 0
Hadanny et al Sports Medicine Open 2022 8 22 ments include maximal oxygen consumption power and the anaerobic threshold By the use of muscle biopsies it was demonstrated that the mechanisms related to HBOT induce significant increase in mitochondrial respiration and mitochondrial mass Introduction Maximal aerobic fitness evaluated by measuring the maximal oxygen capacity VO2max and anaerobic threshold AT strongly correlates with skeletal muscle mitochondria content mitochondrial quantity and skeletal muscle respiratory capacity i e mitochondrial respiration mitochondrial quality 1 3 At the cellular level athletic training can increase both mitochondrial quality and quantity parallel to the improvements in VO2max and AT measured during maximal cardiopulmonary exercise tests CPET 2 4 Moreover it has been established that mitochondria respiration and density differ between untrained and trained individuals 5 6 Several approaches have been suggested to enhance aerobic fitness by inducing mitochondrial adaptions beyond standard physical exercises One of the commonly used approaches includes training under hypoxic conditions Due to its systemic and peripheral stimulation hypoxic training creates metabolic stress at the cellular level which intensifies mitochondrial adaptations However controlled trials demonstrated contradictory results in both mitochondrial respiration and aerobic fitness 7 8 The main reason lies in the fact that performance deteriorates during hypoxic exposures because of the low oxygen supply to the muscles Unlike hypoxia muscles perform better under hyperoxia and therefore normobaric hyperoxia may temporarily enhance endurance and sprint interval performances while breathing oxygen 9 However long term mitochondrial adaptations and aerobic fitness changes were not observed after standard exposure to normobaric hyperoxia 9 Hyperbaric oxygen therapy HBOT utilizes 100 oxygen in an environmental pressure higher than one absolute atmosphere ATA Repeated intermittent hyperoxic exposures have been shown to induce physiological effects which normally occur during hypoxia in a hyperoxic environment 10 13 Thus intermittent fluctuations can potentially induce mitochondrial adaptations without the harmful hypoxic environment 14 Previous evidence shows that hyperbaric oxygen can enhance aerobic performances and increase VO2Max by 10 14 during HBOT exposure 15 Recently Burgos et al demonstrated that 3 weeks of intermittent HBOT sessions increase endurance performances in a pilot study Page 2 of 12 on 12 young soccer players with a moderate effect size on power output and VO2Max 16 However the effect of intermittent hyperbaric exposures on performance was never evaluated in a blinded randomized controlled manner The aim of the current study was to evaluate the effect of an intermittent HBOT protocol on maximal physical performance and its effect on mitochondrial function in middle age master athletes Methods Study Design A double blind randomized 1 1 ratio placebo controlled study of healthy middle aged master athletes The study was done between May 2018 and December 2020 and the protocol was approved by the Shamir Medical Center institutional review board The study was registered in the National Institutes of Health NIH clinical trials registry number NCT03524989 30 04 2018 The study was performed in the Shamir Medical Center All methods were performed in accordance with the relevant guidelines and regulations in accordance with the Declaration of Helsinki Subjects Thirty seven healthy master athletes aged 40 50 who performed aerobic sports at least four times a week at moderate high performance for their age group with no significant musculoskeletal injury in the past 3 months were enrolled Exclusion criteria included previous treatment with HBOT for any reason during the last 3 months debilitating significant musculoskeletal injury lung pathologies middle or inner ear pathologies claustrophobia chronic illness chronic medications or active smoking Athletes were recruited via advertisements and social media Informed consent was obtained from all subjects All the athletes were requested to continue their current training regimen with no changes in volume or training intensity Randomization and Masking After signing an informed consent the athletes were randomly assigned 1 1 to either the HBOT or the SHAMplacebo groups The randomization code was generated by a nurse coordinator who was masked to the study and was not involved in the execution of the study Until study closure the treatment codes were available only to this nurse and the HBOT technicians Participant enrollment was done by physicians who were masked to the study randomization Assessors were also blinded to the athletes intervention assignment To evaluate the blinding following the first session the athletes were asked to discreetly answer a two question
Hadanny et al Sports Medicine Open 2022 8 22 questionnaire about their perception of whether they were allocated to the treatment or SHAM group All data were stored in a dedicated database and were checked for accuracy and completeness A masked data review was done before code breaking and analysis according to a standard procedure at our unit Interventions Both the HBOT and SHAM placebo protocols were conducted in a multiplace Starmed 2700 chamber HAUX Germany Pressure gauges and informative screens within the chamber were disconnected for the athletes blinding The protocol comprised of 40 daily sessions five sessions per week within a 2 month period The athletes were instructed to maintain their usual training program throughout the study The HBOT protocol included breathing 100 oxygen by mask at 2ATA for 60 min with no air breaks Compression decompression rates were 1 m min The SHAM placebo protocol included breathing 21 oxygen by mask at 1 02 ATA for 60 min In order to achieve blinding and have the athletes perform pressure equalization compression to 1 2 ATA was performed for the first 5 min 0 4 m min followed by decompression to 1 02 ATA 0 4 m min in the following 5 min The minimal added 0 02 ATA was mandatory for blinding and for avoiding chamber door opening during the session Outcomes The athletes were evaluated at baseline 1 2 weeks prior to their interventional protocol and 1 2 weeks after the last HBOT SHAM session Cardiopulmonary Maximal Exercise Test CPET Exercise tests were conducted on an E100 cycle ergometer COSMED Rome Italy Gas exchange was measured by a Quark CPET system COSMED with breath bybreath sampling technology and integrated heartrate and exercise ECG monitoring and recording with a 12 lead ECG system COSMED Rome Italy Data were collected on a dedicated computer using the Omnia Metabolic Modules software COSMED Before each test the gas analyzers and flow meter were calibrated The start of the protocol included a one minute rest without pedaling followed by a 2 min warm up The testing protocol included a ramp power increase of 30 watts every minute starting from 0 W while pedaling cadence had to be maintained at 70 rpm Exhaustion was reached when cadence could not be maintained above 70 rpm or when a participant terminated the test Subsequently a threeminute recovery with a pedaling workload of 0 W was initiated Page 3 of 12 Maximal Exercise Tests A blinded physiologist performed analysis of each CPET test separately masked from the athletes name group allocation date of performance and whether the test was a baseline or post intervention measurement The breath by breath dataset was averaged in epochs of seven breaths and both VO2Max and VO2AT VO2 at the ventilatory anaerobic threshold were determined according to classic criteria based on the plateau in the VO2 plot with increasing workload for VO2Max 17 and minute ventilation VE respiratory exchange ratio RER endtidal partial pressure of oxygen PetO2 ratio of minute ventilation to oxygen consumption VE VO2 and the ratio of minute ventilation to carbon dioxide VE VCO2 for VO2AT 18 Compared parameters were maximal power output maximal oxygen consumption VO2Max anaerobic oxygen consumption VO2AT breathing reserve BR RER heartrate V E and volume of CO2 expired VCO2 Mitochondrial Respiration Muscle samples were taken from the gluteus maximus by a fine needle biopsy technique using a TruCut biopsy needle and a 14G puncture cannula after prepping draping and local anesthesia The gluteus maximus muscle was chosen to minimize any interference with the athletes daily training and increase participation rates Athletes underwent muscle biopsies at baseline 1 2 weeks prior to intervention and upon its completion 1 2 weeks post intervention Muscle tissue of about 5 10 mg was immediately put in ice cold biopsy preservation solution BIOPS Samples were immediately transferred to saponin solution for membrane permeabilization for 25 min followed by two cycles of 10 min each in respiration medium MiR05 prior to experimentation Samples were analyzed by high resolution respirometry Mitochondrial respiration was measured using the Oroboros Oxygraph 2 K Oroboros Instruments Innsbruck Austria This device allows to simultaneously record the O2 concentration in two parallel chambers calibrated for 2 ml of respiration medium MiR05 Mitochondrial respiration was quantified in terms of oxygen flux JO2 based on the rate of change of the O 2 concentration in the chambers normalized for wet tissue volume Two mg wet weight samples were added to each Oxygraph chamber and normalized to the amount of tissue per chamber The titration sequence used for the human muscle samples was as follows 10 mM pyruvate 5 mM malate stepwise titration of 2 5 mM ADP 10 M cytochrome c 10 mM glutamate 10 mM succinate stepwise titration of 0 5 M carbonyl cyanide
Hadanny et al Sports Medicine Open 2022 8 22 p trifluoromethoxy phenylhydrazone FCCP 0 5 M rotenone and 5 M antimycin A A measure of the proton leak leak was obtained following the addition of pyruvate and malate A stepwise titration of ADP to saturated concentrations allowed us to selectively quantify the activity of complex I CI the oxygen consumption rate through the NADH pathway Ten M cytochrome c was added as an internal control to survey the integrity of the outer mitochondrial membrane Glutamate was added to evaluate its additive effect on CI activity The maximum oxidative capacity through complex I II maximum OxPhos was determined after the addition of the FADH2 pathway substrate succinate Subsequent injections of the uncoupler FCCP allowed obtaining the maximum respiratory activity in the uncoupled state maximum uncoupled Finally the selective complex II activity CII was obtained at the end of the titration sequence by adding the complex I inhibitor rotenone in the maximum uncoupled state In a final step complex III was inhibited by the administration of antimycin A Mitochondrial Markers Muscle samples were taken from the gluteus maximus by a fine needle biopsy technique see above at baseline 1 2 weeks prior to intervention and upon its completion 1 2 weeks post intervention Following membrane permeabilization by saponin samples were immersed in 4 paraformaldehyde for 6 h and then transferred to 70 ethanol for preservation until paraffin embedding Due to the small size of the sample following immersion it was not organized in a specific orientation Paraffinembedded sections were de paraffinized rehydrated and washed in phosphate buffered saline PBS Antigen retrieval was performed in 1 mM EDTA pH 8 0 for 40 min After blocking with 5 normal goat serum Abcam ab7481 supplemented by 2 BSA for one hour at RT sections were incubated with primary antibodies for MNF1 2 1 100 PGC 1 alpha Abcam ab54481 1 200 and OPA1 Abcam ab157457 1 300 overnight at 4 C followed by a secondary antibody for one hour at 4 C and followed by either goat anti mouse or goat anti rabbit secondary antibodies Abcam 1 500 for one hour at RT The sections were then mounted using Fluoroshield mounting medium with DAPI ab104139 Control samples were exposed to only the secondary antibody to rule out unspecific staining Mitochondrial mass was evaluated with the MitoTracker Green FM dye Molecular Probes as previously described 19 Briefly following deparaffinization and rehydration the sections were incubated for 30 min at room temperature with 100 nM MitoTracker Green FM followed by rinses with PBS Page 4 of 12 Stained slides were imaged for fluorescence using a Lionheart FX Automated Fluorescent Microscope Total intensity divided by total area in three random fields for each experimental sample was measured with Lionheart FX Gene 5 image analysis software Fluorescence intensity values for each experimental group were averaged and presented as mean fluorescent intensity MFI Pulmonary Function Measurements of pulmonary functions were performed using the KoKo Sx1000 spirometer Nspire Health USA 1 2 weeks prior to and after the last HBOT SHAM session The equipment was calibrated using a 3 l syringe before performing measurements according to the manufacturer s instructions Measurements were performed by a trained technician The forced expiratory maneuvers were performed as recommended by the guidelines 19 The forced vital capacity FVC forced expiratory volume in 1 s FEV1 the Tiffeneau Pinelli index FEV1 FVC and peak expiratory flow rate PEF were taken as the highest readings obtained from at least three satisfactory forced expiratory maneuvers Mean forced midexpiratory flow rate FEF25 75 and forced expiratory flow rates at 25 50 and 75 of FVC expired FEF25 FEF50 and FEF75 were taken as the best values from flow volume loops not differing by 5 from the highest FVC Body Composition An Inbody720 body composition analyzer Biospace Co South Korea was used to detect the human body composition based on recommendations provided in the user manual The athletes bare feet stood on the pedal plate electrode hands naturally hanging down and holding the hand electrode gently and the angle between the trunk and upper limbs was maintained at 15 Indexes included basal metabolic rate lean body weight intracellular fluid extracellular fluid body water content skeletal muscle body fat abdominal obesity etc Weight was measured in kilograms with the athletes barefoot in minimal clothing by a digital scale Beurer Germany and height was measured in centimeters BMI was calculated as the weight in kilograms divided by the square of the height in meters kg m2 Athletes underwent body composition analysis at baseline 1 2 weeks prior to intervention and upon its completion and 1 2 weeks post intervention Physical Measurements A trained physical therapist who was masked from group allocation performed physical measurements including
Hadanny et al Sports Medicine Open 2022 8 22 range of motion vertical jump maximal quadriceps power a step test and an agility test Safety Athletes were monitored for adverse events including barotraumas either ear or sinuses and oxygen toxicity pulmonary and central nervous system Statistical Analysis Continuous data are expressed as means standarddeviation Normal distributions for all variables were tested using the Kolmogorov Smirnov test Unpaired and paired t tests were performed to compare variables between and within the two groups Net effect sizes were evaluated using Cohen s d method Categorical data are expressed in numbers and percentages and were compared by chi square tests Univariate analyses were performed using chi square Fisher s exact test to identify significant variables P
Hadanny et al Sports Medicine Open 2022 8 22 Page 6 of 12 Table 1 Athletes characteristics All N 31 SHAM N 15 HBOT N 16 Significance Age years 44 1 2 96 44 60 2 87 43 63 3 05 0 368 Males 26 83 9 12 80 0 14 87 5 Experience 10 97 6 30 11 33 6 88 10 63 5 90 0 76 Triathlon 10 32 3 7 43 8 Running 13 41 9 Sport type 0 65F 0 02 Swimming 2 6 5 3 30 4 26 7 9 56 3 2 13 3 0 Cycling 3 9 7 3 20 0 Other 3 9 7 3 20 0 Previous injuries 6 19 4 2 33 3 4 25 0 65F Baseline athletes parameters are summarized in Table 1 There was no difference between the groups as to any of the baseline characteristics except for training type In the HBOT arm all athletes were runners or triathletes whereas in the SHAM control group there were also swimmers cyclists and others p 0 02 Blinding Evaluation Athlete blinding was achieved where 63 of HBOT group perceived their sessions as SHAM and 53 of the SHAM group perceived their sessions as SHAM p 0 60 Fig 2 Physical Performance Evaluation There were no significant differences between the groups in CPET parameters at baseline Following HBOT there was a significant increase in the maximal oxygen consumption VO2Max 2834 50 556 65 ml min to 2956 19 540 85 ml min group X time interaction F 7 57 p 0 010 with a large net effect size of 0 989 0 210 1 76 compared to the SHAM group Table 2 Similar results were noted in VO2 kg Table 2 Oxygen consumption measured at the anaerobic threshold VO2AT was significantly increased in the HBOT group 1196 56 218 29 ml min to 1326 56 249 11 ml min group X time F 5 43 p 0 026 with a large net effect size of 0 837 0 071 1 604 compared to the SHAM group Table 2 The HBOT group demonstrated a significant increase in maximal power compared to the SHAM group with a large net effect size of 0 808 0 04 1 57 group X time interaction F 5 05 p 0 03 Table 2 In addition compared to the SHAM group there was a significant decrease in breathing reserve in the HBOT group with a large net effect size 0 91 0 168 0 140 group X time interaction F 6 44 p 0 016 Table 2 No significant differences were noted in body composition and pulmonary function measurements between the groups at baseline and following HBOT SHAM Table 3 In addition there were no significant differences in range of motion upper or lower limbs power vertical jump or agility Table 3 Mitochondrial Respiration Evaluation Thirty athletes from those included in the final analysis consented to muscle biopsies Three athletes refused to undergo their second biopsy and five athletes biopsies did not pass quality control for respiration analysis Thus mitochondrial respiration was assessed in 10 HBOT athletes and 12 SHAM athletes Since there were significant differences between the groups in the baseline mitochondrial respiration parameters an ANCOVA was performed Fig 2 SHAM protocol quality control Rates of group allocation perception by the HBOT group subjects A and SHAM group subjects B
Hadanny et al Sports Medicine Open 2022 8 22 Page 7 of 12 Table 2 CPET changes SHAM Placebo N 15 Baseline HBOT N 16 SHAM P value Baseline Post HBOT P value Baseline comparison P value Net effect size Time X group interaction F P Primary endpoint VO2Max mL min 2673 33 748 03 2631 07 751 31 0 14 2834 50 556 65 2956 19 540 85 0 03 0 49 0 989 0 210 1 76 7 57 0 010 VO2AT mL min 1210 87 239 80 1208 53 266 18 0 93 1196 56 218 29 1326 56 249 11 0 01 0 86 0 837 0 071 1 604 5 43 0 026 Secondary endpoints Power watts 256 27 66 43 254 73 68 25 0 78 277 37 46 14 290 93 51 87 0 004 0 31 0 808 0 04 1 57 5 05 0 03 VO2 Kg mL kg min 36 08 9 08 35 51 8 85 0 15 42 00 9 80 43 86 9 04 0 02 0 09 1 019 0 238 1 800 8 04 0 008 BR 32 64 12 42 36 77 12 05 0 14 35 71 13 07 30 67 15 05 0 05 0 508 0 91 0 168 0 140 6 44 0 016 VO2AT VO2Max 46 95 8 98 47 25 7 32 0 77 42 48 4 33 45 46 8 29 0 15 0 08 0 424 0 138 1 167 1 39 0 247 VO2MAX maximal oxygen consumption VO2AT oxygen consumption at the anaerobic threshold Kg Kilograms BR breathing reserve P
Hadanny et al Sports Medicine Open 2022 8 22 Page 8 of 12 Table 3 Pulmonary function and body composition SHAM Placebo N 16 Baseline SHAM HBOT N 16 3 months Baseline Post HBOT 3 months Baseline comparison P value P value Net effect size P value Time X group interaction F P Pulmonary function FEV1 liters 3 79 0 48 3 89 0 57 0 29 3 46 0 37 3 42 0 40 0 64 0 08 0 469 1 16 0 29 0 435 1 375 FVC1 liters 4 71 0 79 4 91 0 71 0 09 4 21 4 27 4 27 0 49 0 61 0 11 0 404 0 77 0 38 0 462 1 271 FEV1 FVC 0 80 0 04 0 79 0 05 0 45 0 82 0 08 0 81 0 05 0 31 0 30 0 437 0 42 0 52 0 431 1 305 FEF25 75 liters 3 59 0 85 3 64 0 83 0 77 3 77 1 05 3 29 0 62 0 12 0 66 0 751 3 29 0 08 0 136 1 638 Body composition Weight kilograms 73 58 11 34 73 09 12 02 0 21 68 46 6 70 67 91 6 60 0 16 0 13 0 092 0 01 0 91 0 828 0 642 BMI 24 16 2 42 23 94 2 62 0 10 23 21 2 53 23 01 2 47 0 16 0 29 0 120 0 03 0 86 0 614 0 856 BFM kilograms 14 2 4 67 13 71 5 19 0 13 11 33 4 66 10 43 4 39 0 04 0 09 0 030 0 60 0 44 0 704 0 765 SMM kilograms 33 51 5 63 33 55 5 63 0 85 32 16 3 73 32 4 3 75 0 11 0 43 0 214 0 58 0 44 0 951 0 522 TBW liters 43 48 6 64 43 42 6 69 0 84 41 78 4 60 42 03 4 65 0 21 0 41 0 133 0 75 0 39 0 869 0 602 ICW liters 27 23 4 32 27 27 4 31 0 82 26 19 2 87 26 38 2 86 0 08 0 43 0 226 0 55 0 46 0 926 0 510 Physical measurements Knee ROM degrees 61 45 12 99 62 75 15 85 0 62 61 77 11 77 59 69 13 55 0 48 0 94 0 327 0 74 0 39 0 456 1 111 Quads max power kilograms 20 9 7 32 18 7 7 59 0 07 22 34 5 40 21 66 5 36 0 66 0 55 0 296 0 61 0 44 1 079 0 486 Vertical jump centimeters 39 27 8 42 38 38 5 43 0 53 40 1 7 85 40 49 8 89 0 68 0 79 0 297 0 62 0 44 1 081 0 485 Step test beats minute 135 69 15 61 127 07 17 59 0 012 136 13 20 62 133 42 16 57 0 54 0 95 0 626 2 64 0 11 1 438 0 186 Agility test seconds 15 99 1 69 16 25 2 07 0 85 15 86 1 16 15 40 1 62 0 36 0 81 0 251 0 42 0 52 0 549 1 052 FEV1 forced expiratory volume in one second FVC forced vital capacity FEF25 75 percentage of the predicted value for forced expiratory flow at 25 75 of forced vital capacity BMI body mass index BFM body fat mass SMM skeletal muscle mass TBW total body water ICW intracellular water P
Hadanny et al Sports Medicine Open 2022 8 22 Page 9 of 12 Table 4 Mitochondrial respiration changes SHAM Placebo N 12 Baseline HBOT N 10 SHAM 3 months Baseline Post HBOT 3 months Baseline Comparison P P value value Net effect size ANCOVA P 9 72 1 90 11 98 5 60 0 17 0 32 0 429 0 47 1 33 3 80 0 06 P value Primary endpoint Leak pmol s mg 8 51 3 26 7 34 3 92 0 15 Complex I Pyruvate Malate Glutamate pmol s mg 43 14 16 03 35 21 16 37 0 03 58 05 16 05 63 75 19 99 0 21 0 04 1 120 7 31 0 01 0 160 2 080 Complex II uncoupled pmol s mg 44 03 13 13 46 32 10 10 0 49 61 32 14 39 63 19 14 40 0 65 0 008 1 223 2 19 0 15 0 250 2 195 Maximal cou 74 78 20 40 72 22 21 23 0 66 pled capacity Succinate 97 85 22 21 105 56 21 61 0 26 0 019 1 085 4 89 0 04 0 129 2 041 pmol s mg Maximal uncoupled capacity pmol s mg 117 30 37 96 121 49 29 51 0 56 0 036 0 956 6 04 0 02 0 013 1 898 87 94 22 99 80 36 23 81 0 24 P
Hadanny et al Sports Medicine Open 2022 8 22 Page 10 of 12 Fig 3 Mitochondrial mass changes High resolution micrograph of muscle staining with MTG demonstrates a significant increase in the mitochondrial mass marker MTG compared to the SHAM group 17 12 20 2 vs 8 54 8 41 p 0 0002 Positive counts are represented by green dots Greener brighter images reflect higher counts of MTG staining in parallel to aerobic fitness as observed by VO2Max following HBOT compared to the SHAM group Previous studies have shown that humans exploit 90 of their mitochondrial capacity while performing maximal exercise at VO2Max 31 Thus acute exposure to normobaric or hyperbaric hyperoxia can increase VO2Max temporarily if the subject is breathing increased oxygen levels which is usually impractical during real world exercises sports However this temporary effect would not induce long term mitochondrial adaptations neither in number nor in respiration In our study athletes underwent multiple intermittent hyperbaric exposures which enabled the mentioned cellular changes The fact that both CPET and mitochondrial biopsies were done more than 1 week after the last HBOT session further supports the conclusion that repeated HBOT induces significant biological changes and the beneficial effect is not related to the transient increase in oxygen delivery Hypoxic training has been suggested to enhance aerobic fitness with long term effects Hypoxia indeed induces the hypoxic induced factor 1 HIF1 transcription factor which initiates a cascade of reactions to cope with the new energetic crisis of low oxygen 14 However due to the continuous insufficient level of oxygen the number of mitochondria is reduced less generation of new mitochondria and mitochondrial respiration is inhibited to adapt and preserve life 32 In comparison during repeated intermittent hyperbaric exposures the relative changes in oxygen availability rather than the constant hypoxia hyperoxia have a more dominant effect on HIF1 induction 10 33 36 HIF1 is increased and promotes mitochondrial biogenesis and mitochondrial respiration changes which are possible as oxygen supplies remain at normal or super normal states 14 This phenomenon has been referred as the hyperoxic hypoxic paradox i e increased HIF and its associated cascade at hyperoxic states 14 Thus intermittent hyperbaric exposures can be compared to intense interval training which induces mitochondrial adaptations in both number and respiration Our study shows for the first time in humans that both mitochondrial respiration both coupled and uncoupled and mass are enhanced following HBOT compared to no changes in the SHAM group
Hadanny et al Sports Medicine Open 2022 8 22 PGC 1 is a critical regulator of mitochondrial biogenesis in skeletal muscle and promotes this process in response to exercise to maintain a balance between energy need and energy supply Previous studies have suggested that HBOT increases PGC 1 following repeated exposures 23 MNF1 2 are involved in the outer mitochondrial membrane fusion while OPA1 mediates fusion of the inner mitochondrial membrane 37 MNF2 is associated with reduced mitophagy leading to the accumulation of damaged mitochondria OPA1 is a sensor of physical activity and decreases with aging related changes 38 Although all three increased in the HBOT group they were not statistically significant These findings may be explained by the small sample size n 12 of available muscle biopsies These results may also be related to the timing of the muscle biopsies Taken 2 weeks following the last session active biogenesis may have ended and mitochondrial mass has increased MTG enables accurate measurements of mitochondrial mass independent of the mitochondrial function and respiration 39 In the current study the HBOT group subsample had increased mitochondrial mass compared to the SHAM group subsample The current study has several limitations First the relatively small sample size has to be considered possibly causing decreased sensitivity However the presence of significant changes following strict statistical analyses in a small group is indicative of the relatively high potency of the intervention Second the duration of the effect is yet to be determined in long term follow up studies Third the protocol was 40 sessions of 100 oxygen at two ATA HBOT exposure However the optimal number of sessions and protocol of each session remains to be determined Lastly there were differences in baseline mitochondrial respiration between the two groups which may be related to the heterogenicity of the participants athletes Mitochondrial respiration variability is expected and has been reported within healthy adults 31 40 In the current study we mitigated these differences using ANCOVA Conclusions The study indicates that HBOT can enhance physical performance in healthy master athletes The main improvements include maximal oxygen consumption power and the anaerobic threshold By the use of muscle biopsies it was demonstrated that the mechanisms related to HBOT induce significant improvement in mitochondrial respiration and increase mitochondrial mass Abbreviations VO2max Maximal oxygen capacity AT Anaerobic threshold CPET Maximal cardiopulmonary exercise tests HBOT Hyperbaric oxygen therapy ATA Absolute atmosphere NIH National Institutes of Health VE Minute ventilation RER PetO2 Ratio of minute ventilation to oxygen consumption VE VO2 Page 11 of 12 BR Breathing reserve RER Respiratory exchange ratio VE Minute ventilation VCO2 Volume of CO2 expired PetO2 End tidal partial pressure of oxygen JO2 Oxygen flux CI Oxidative capacity through complex I maximum OxPhos Oxidative capacity through complex I II CII Oxidative capacity through complex II PBS Phosphate buffered saline MFI Mean fluorescent intensity FVC Forced vital capacity FEV1 Forced expiratory volume in 1 s PEF Peak expiratory flow rate FEF25 75 Forced expiratory flow at 25 75 of forced vital capacity FEF25 Forced expiratory flow rates at 25 of FVC expired FEF50 Forced expiratory flow rates at 50 of FVC expired FEF75 Forced expiratory flow rates at 75 of FVC expired ANOVA Analysis of variance ANCOVA Analysis of covariance FDR False discovery rate HIF1 Hypoxic induced factor 1 BMI Body mass index BFM Body fat mass SMM Skeletal muscle mass TBW Total body water ICW Intracellular water Acknowledgements We would like to thank Dr Mechael Kanovsky for his editing of this manuscript Authors contributions All authors contributed substantially to the preparation of this manuscript AH and SE were responsible for protocol design AH DR YZ YB EY and SE were responsible for patients recruitment AH YH DR MS HG RAH EL NP MF SF YZ YB and NG were responsible for data acquisition AH MC YH and SE were responsible for data analysis All authors interpreted the data AH MC YE and SE wrote the manuscript All authors revised and finalized the manuscript Funding The study was funded by the Shamir Medical Center Research Fund Availability of data and materials The datasets used and or analyzed during the current study are available from the corresponding author on reasonable request Declarations Ethics approval and consent to participate The study was approved by Shamir Medical Center institutional review board approval number 244 16 All patients signed an informed consent form Consent for publication Not applicable Competing interests Amir Hadanny Eldad Yaakobi Yair Bechor and Yonatan Zemel work for AVIV Scientific LTD Shai Efrati is a shareholder and co founder of AVIV Scientific LTD Yafit Hachmo Daniella Rozali Merav Catalogna Marina Sova Hadar Gattegno Ramzia Abu Hamed Erez Lang Nir Polak Money Friedman Shachar Finci and Noga Gal declare they have no competing interests Author details 1 The Sagol Center for Hyperbaric Medicine and Research Shamir AssafHarofeh Medical Center Zerifin Israel 2 Sackler School of Medicine Tel Aviv University Tel Aviv Israel 3 Bar Ilan University Ramat Gan Israel 4 Research and Development Unit Shamir Medical Center Zerifin Israel 5 Physical Therapy Department Shamir Medical Center Zerifin Israel 6 Sagol School of Neuroscience Tel Aviv University Tel Aviv Israel Received 30 September 2021 Accepted 21 December 2021 References 1 Booth FW Narahara KA Vastus lateralis cytochrome oxidase activity and its relationship to maximal oxygen consumption in man Pflugers Arch 1974 349 4 319 24 2 Hoppeler H Howald H Conley K Lindstedt SL Claassen H Vock P et al Endurance training in humans aerobic capacity and structure of skeletal muscle J Appl Physiol 1985 59 2 320 7
ISSN 2320 5407 Int J Adv Res 8 07 1535 1537 Journal Homepage www journalijar com Article DOI 10 21474 IJAR01 11421 DOI URL http dx doi org 10 21474 IJAR01 11421 RESEARCH ARTICLE EFFECTIVENESS OF HYPERBARIC OXYGEN THERAPY FOR TREATMENT OF POSTMENOPAUSAL OSTEOPOROSIS A CASE REPORT 1 2 3 Alan A Katz M D1 Gurvinder Singh B S 2 and Kristin Thomson DHSc PA C3 MD FACEP FAAEM UHM ABEM Medical Director Hyperbaric Medical Solutions USA NYS Advanced EMT USA Clinical Staff and Research Coordinator Hyperbaric Medical Solutions USA Manuscript Info Abstract Manuscript History Received 28 May 2020 Final Accepted 30 June 2020 Published July 2020 Key words Hyperbaric Oxygenation Osteoporosis Hyperbaric Oxygen Therapy Postmenopausal Osteoporosis Osteogenesis Postmenopausal osteoporosis is a common degenerative bone disease that can be challenging to manage when a patient does not respond to or tolerate conventional treatment plans like estrogen replacement therapy bisphosphonates and vitamin supplementation This case represents a 63 year old woman with refractory postmenopausal osteoporosis who demonstrated measurable improvement in her bone density and bone turnover marker serum C terminal telopeptide after completing hyperbaric oxygen therapy treatment Hyperbaric oxygen therapy s effect on bone regeneration and remodeling warrants further studies on its effectiveness on improving bone health and as an adjunctive therapy option in osteoporosis patients Copyright IJAR 2020 All rights reserved Introduction Postmenopausal osteoporosis is a common degenerative bone disease that can be challenging to manage when a patient does not respond to or tolerate conventional treatment plans 1 2 Hyperbaric oxygenation s effects on osteoporosis has not been extensively studied but has shown other beneficial effects including improved angiogenesis decreased inflammation reduced marrow edema and an increase in circulating stem cells 9 When a patient is not responding to conventional treatment hyperbaric oxygen may be considered as a future adjunctive therapy and the effect on bone regeneration and remodeling warrants further studies We present a case of investigational outpatient hyperbaric oxygenation therapy in a postmenopausal female with advancing osteoporosis Case Presentation A 63 year old Caucasian postmenopausal female presented to an outpatient hyperbaric oxygen therapy facility for consultation regarding her advancing osteoporosis The patient had been initially diagnosed with age related osteoporosis at the age of 55 by her family medicine physician Since diagnosis the patient was unsuccessful with standard therapy and supplemental vitamins due to intolerance of the medication side effects bisphosphonates alendronate risedronate led to the development of muscle cramps and esophagitis The patient was offered targeted therapy with the monoclonal antibody denosumab but refused to start therapy due to the fear of developing additional side effects The patient attempted estrogen replacement therapy in addition to supplementation with calcium vitamin K2 and vitamin D3 boron and riboflavins yielding no improvement in bone mineral density Over a four year period the patient lost 14 of her hip density and but did not experience any fractures The patient s osteoporosis Fracture Risk Assessment Tool results indicated a 10 year probability of major osteoporotic fracture of 13 Past medical history consisted of hypothyroidism and panic disorder and she utilized levothyroxine Corresponding Author Kristin Thomson DHSc PA C Address Hyperbaric Medical Solutions USA 1535
ISSN 2320 5407 Int J Adv Res X X 1535 1537 for thyroid supplementation for the past 15 years She does not smoke and nor does she drink alcohol or caffeine excessively She considers herself physically active since she hikes walks and dances regularly during the week The only family history of osteoporosis was identified in her cousin and aunt Hyperbaric oxygen therapy HBOT was initiated The patient received 20 daily sessions over four weeks of hyperbaric treatment in a monoplace chamber The patient understood the investigational nature of hyperbarics role in the treatment of osteoporosis prior to starting therapy Each session consisted of hyperbaric therapy for 90minutes at 2 0 ATA Air breaks were provided during treatment to reduce the risk of oxygen toxicity and the patient did not report any adverse reactions while receiving hyperbaric therapy Baseline laboratory tests were performed and revealed thyroid function phosphorus 25 OH Vitamin D calcium and bone alkaline phosphatase levels all within normal ranges Dual X ray absorptiometry DXA scans and laboratory assays of serum bone alkaline phosphatase bone ALP and serum C terminal telopeptide of cross links of type I collagen CTx were obtained prior to and after hyperbaric therapy Table 1 At the conclusion of therapy the patient s serum CTx levels had decreased by 33 indicating a general decrease in bone resorption This is further supported by a decrease in serum bone ALP levels and slight improvement in bone mineral density based on lumbar DXA scans Discussion Osteoporosis is the most common degenerative bone disease affecting 200 million women worldwide that is characterized by reduced bone density osteoporosis leads to more than 8 9 million fractures a year 1 2 Osteoporosis associated with a decrease in estrogen production in women aged 51 to 64 has been shown to increase the incidence of vertebral radial and ulnar fractures in its early stages eventually progressing to more complex fractures involving the femoral neck in the absence of adequate treatment 2 Clinicians identify long term osteoporotic changes by obtaining measurements of bone mineral density obtained via dual X ray absorptiometry Additionally serum Cterminal telopeptide of type I collagen has been utilized as a bone turnover marker and can provide prognostic information on fracture risk 3 As type I collagen is degraded during bone resorption the c terminal telopeptide is released and this marker can also be used in the evaluation of the potential efficacy of osteoporosis treatment therapies 4 5 Key recommendations for the treatment of postmenopausal osteoporosis include calcium vitamin D supplementation bisphosphonates and estrogen replacement therapy 4 6 7 Some postmenopausal women do not respond to conventional therapy The role of hyperbaric oxygen therapy in improving bone turnover and density has yet to be studied in women who do not adequately respond to conventional treatment The beneficial effects of hyperbaric oxygen therapy include improved angiogenesis decreased inflammation reduced marrow edema and an increase in circulating stem cells 9 By elevating the plasma and tissue concentrations of oxygen HBOT has been shown to increase the rate of osteoblast differentiation and osteoclast suppression leading to a general shift towards bone regeneration A study on femoral head necrosis patients revealed a reduction in bone lesion size and an increase in serum osteoprotegerin OPG in response to HBOT The association of OPG and receptor activator of nuclear factor kappa B ligand RANKL prevents RANKL from binding to its transmembrane protein in osteoclasts receptor activator of nuclear factor kappa B RANK Increased OPG will reduce RANKL RANK binding and osteoclastogenesis and bone resorption is inhibited 8 9 According to Yano et al postmenopausal osteoporotic women had higher levels of OPG than age matched controls and higher OPG concentrations in osteoporotic patients with lower bone mass It is theorized that the increased OPG level in osteoporotic women is a compensatory feedback response to increased osteoclast activity 8 9 This case represents a 63 year old woman with refractory postmenopausal osteoporosis who demonstrated measurable improvement in her bone density and bone turnover markers after completing hyperbaric oxygen therapy treatment Hyperbaric oxygen therapy s effect on bone regeneration and remodeling warrants further studies on its effectiveness on improving bone health and as an adjunctive therapy option in osteoporosis patients Table 1 Lumbar dual X ray absorptiometry T Score and serum C terminal telopeptide of cross links of type I collagen before and after initiating hyperbaric oxygen treatment Date Lumbar DXA T Score Date CTx Value pg mL 2005 1 5 2 2017 574 2008 1 8 12 2017 598 2011 2 7 5 2018 596 1536
ISSN 2320 5407 1 2019 3 8 2 2019 3 6 Value at initiation of HBOT series At conclusion of HBOT series Int J Adv Res X X 1535 1537 11 2018 2 2019 552 377 References 1 2 3 4 5 6 7 8 9 Johnell O Kanis JA An estimate of the worldwide prevalence and disability associated with osteoporotic fractures Osteoporosis International 2006 17 12 1726 1733 doi 10 1007 s00198 006 0172 4 World Health Organization Assessment of osteoporosis at the primary health care level Summary Report of a WHO Scientific Group Geneva WHO 2007 Greenblatt MB et al Bone Turnover Markers in the Diagnosis and Monitoring of Metabolic Bone Disease Clin Chem 2017 63 2 464 474 doi 10 1373 clinchem 2016 259085 Tella SH Gallagher JC Prevention and treatment of postmenopausal osteoporosis J Steroid Biochem Mol Biol 2014 142 155 170 doi 10 1016 j jsbmb 2013 09 008 Avbersek Luznik I et al Activity or mass concentration of bone specific alkaline phosphatase as a marker of bone formation Clinical Chemical Laboratory Medicine 2007 45 8 1014 1018 doi 10 1515 CCLM 2007 186 Wu CH et al Consensus statement on the use of bone turnover markers for short term monitoring of osteoporosis treatment in the Asia Pacific region J Clin Densitom2019 doi org 10 1016 j jocd 2019 03 004 Jeremiah MP et al Diagnosis and Management of Osteoporosis Am Fam Physician 2015 Aug 15 92 4 261 8 Yano K Isuke Tsuda E Washida N et al Immunological characterization of circulating osteoprotegerin osteoclastogenesis inhibitory factor increased serum concentrations in postmenopausal women with osteoporosis J Bone Miner Res 1999 14 518 27 Vezzani G et al Hyperbaric oxygen therapy modulates serum OPG RANKL in femoral head necrosis patients J Enzyme Inhib Med Chem 2017 32 1 707 711 doi 10 1080 14756366 2017 1302440 1537
Hadanny et al Sports Medicine Open 2022 8 22 3 Jacobs RA Lundby C Mitochondria express enhanced quality as well as quantity in association with aerobic fitness across recreationally active individuals up to elite athletes J Appl Physiol 2013 114 3 344 50 4 Holloszy JO Biochemical adaptations in muscle Effects of exercise on mitochondrial oxygen uptake and respiratory enzyme activity in skeletal muscle J Biol Chem 1967 242 9 2278 82 5 van Loon LJ Jeukendrup AE Saris WH Wagenmakers AJ Effect of training status on fuel selection during submaximal exercise with glucose ingestion J Appl Physiol 1985 1999 87 4 1413 20 6 Zoll J Sanchez H N Guessan B Ribera F Lampert E Bigard X et al Physical activity changes the regulation of mitochondrial respiration in human skeletal muscle J Physiol 2002 543 Pt 1 191 200 7 Robach P Bonne T Fluck D Burgi S Toigo M Jacobs RA et al Hypoxic training effect on mitochondrial function and aerobic performance in hypoxia Med Sci Sports Exerc 2014 46 10 1936 45 8 Pesta D Hoppel F Macek C Messner H Faulhaber M Kobel C et al Similar qualitative and quantitative changes of mitochondrial respiration following strength and endurance training in normoxia and hypoxia in sedentary humans Am J Physiol Regul Integr Comp Physiol 2011 301 4 R1078 87 9 Sperlich B Zinner C Hauser A Holmberg HC Wegrzyk J The impact of hyperoxia on human performance and recovery Sports Med 2017 47 3 429 38 10 Cimino F Balestra C Germonpre P De Bels D Tillmans F Saija A et al Pulsed high oxygen induces a hypoxic like response in human umbilical endothelial cells and in humans J Appl Physiol 1985 2012 113 11 1684 9 11 Sunkari VG Lind F Botusan IR Kashif A Liu ZJ Yla Herttuala S et al Hyperbaric oxygen therapy activates hypoxia inducible factor 1 HIF 1 which contributes to improved wound healing in diabetic mice Wound Repair and Regeneration Official Publication of the Wound Healing Society and the European Tissue Repair Society 2015 23 1 98 103 12 Milovanova TN Bhopale VM Sorokina EM Moore JS Hunt TK Hauer Jensen M et al Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo J Appl Physiol 1985 2009 106 2 711 28 13 Yang Y Wei H Zhou X Zhang F Wang C Hyperbaric oxygen promotes neural stem cell proliferation by activating vascular endothelial growth factor extracellular signal regulated kinase signaling after traumatic brain injury NeuroReport 2017 28 18 1232 8 14 Hadanny A Efrati S The hyperoxic hypoxic paradox Biomolecules 2020 10 6 15 Cabric M Medved R Denoble P Zivkovic M Kovacevic H Effect of hyperbaric oxygenation on maximal aerobic performance in a normobaric environment J Sports Med Phys Fitness 1991 31 3 362 6 16 Burgos C Henriquez Olguin C Andrade DC Ramirez Campillo R Araneda OF White A et al Effects of exercise training under hyperbaric oxygen on oxidative stress markers and endurance performance in young soccer players a pilot study J Nutr Metab 2016 2016 5647407 17 Howley ET Bassett DR Jr Welch HG Criteria for maximal oxygen uptake review and commentary Med Sci Sports Exerc 1995 27 9 1292 301 18 Ghosh AK Anaerobic threshold its concept and role in endurance sport Malays J Med Sci MJMS 2004 11 1 24 36 19 Miller MR Hankinson J Brusasco V Burgos F Casaburi R Coates A et al Standardisation of spirometry Eur Respir J 2005 26 2 319 38 20 Wen D Utesch T Wu J Robertson S Liu J Hu G et al Effects of different protocols of high intensity interval training for VO2max improvements in adults a meta analysis of randomised controlled trials J Sci Med Sport 2019 22 8 941 7 21 Colin Pennington MSK The exercise effect on the anaerobic threshold in response to graded exercise Int J Health Sci 2015 3 1 22 Albouaini K Egred M Alahmar A Wright DJ Cardiopulmonary exercise testing and its application Heart 2007 93 10 1285 92 23 Suzuki J Endurance performance is enhanced by intermittent hyperbaric exposure via up regulation of proteins involved in mitochondrial biogenesis in mice Physiol Rep 2017 5 15 24 Kurt B Kurt Y Karslioglu Y Topal T Erdamar H Korkmaz A et al Effects of hyperbaric oxygen on energy production and xanthine oxidase levels in striated muscle tissue of healthy rats J Clin Neurosci 2008 15 4 445 50 25 DeCato TW Bradley SM Wilson EL Harlan NP Villela MA Weaver LK et al Effects of sprint interval training on cardiorespiratory fitness Page 12 of 12 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 while in a hyperbaric oxygen environment Undersea Hyperb Med 2019 46 2 117 24 Bassett DR Jr Howley ET Limiting factors for maximum oxygen uptake and determinants of endurance performance Med Sci Sports Exerc 2000 32 1 70 84 Joyner MJ Coyle EF Endurance exercise performance the physiology of champions J Physiol 2008 586 1 35 44 Weibel ER Hoppeler H Exercise induced maximal metabolic rate scales with muscle aerobic capacity J Exp Biol 2005 208 Pt 9 1635 44 Van Hall G Jensen Urstad M Rosdahl H Holmberg HC Saltin B Calbet JA Leg and arm lactate and substrate kinetics during exercise Am J Physiol Endocrinol Metab 2003 284 1 E193 205 Coyle EF Sidossis LS Horowitz JF Beltz JD Cycling efficiency is related to the percentage of type I muscle fibers Med Sci Sports Exerc 1992 24 7 782 8 van der Zwaard S de Ruiter CJ Noordhof DA Sterrenburg R Bloemers FW de Koning JJ et al Maximal oxygen uptake is proportional to muscle fiber oxidative capacity from chronic heart failure patients to professional cyclists J Appl Physiol 1985 2016 121 3 636 45 Thomas LW Ashcroft M Exploring the molecular interface between hypoxia inducible factor signalling and mitochondria Cell Mol Life Sci 2019 76 9 1759 77 Balestra C Germonpre P Hypoxia a multifaceted phenomenon the example of the normobaric oxygen paradox Eur J Appl Physiol 2012 112 12 4173 5 Fratantonio D Virgili F Zucchi A Lambrechts K Latronico T Lafere P et al Increasing oxygen partial pressures induce a distinct transcriptional response in human PBMC a pilot study on the normobaric oxygen paradox Int J Mol Sci 2021 22 1 De Bels D Tillmans F Corazza F Bizzari M Germonpre P Radermacher P et al Hyperoxia alters ultrastructure and induces apoptosis in leukemia cell lines Biomolecules 2020 10 2 Kappler M Taubert H Eckert AW Oxygen sensing homeostasis and disease N Engl J Med 2011 365 19 1845 6 author reply 6 Song Z Ghochani M McCaffery JM Frey TG Chan DC Mitofusins and OPA1 mediate sequential steps in mitochondrial membrane fusion Mol Biol Cell 2009 20 15 3525 32 Damiano S Muscariello E La Rosa G Di Maro M Mondola P Santillo M Dual role of reactive oxygen species in muscle function can antioxidant dietary supplements counteract age related sarcopenia Int J Mol Sci 2019 20 15 Doherty E Perl A Measurement of mitochondrial mass by flow cytometry during oxidative stress React Oxyg Species Apex 2017 4 10 275 83 Jacobs RA Rasmussen P Siebenmann C Diaz V Gassmann M Pesta D et al Determinants of time trial performance and maximal incremental exercise in highly trained endurance athletes J Appl Physiol 1985 2011 111 5 1422 30 Publisher s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
The Journal of Physiological Sciences 2019 69 573 580 https doi org 10 1007 s12576 019 00678 5 REVIEW Mild hyperbaric oxygen mechanisms and effects Akihiko Ishihara1 Received 10 September 2018 Accepted 15 April 2019 Published online 6 May 2019 The Physiological Society of Japan and Springer Japan KK part of Springer Nature 2019 Abstract Adequate oxygen supply by exposure to mild hyperbaric oxygen at appropriately high atmospheric pressure 1266 1317 hPa and increased oxygen concentration 35 40 oxygen has a possibility of improving the oxidative metabolism in cells and tissues without barotrauma and excessive production of reactive oxygen species Therefore metabolic syndrome and lifestyle related diseases including type 2 diabetes and hypertension in rats were inhibited and or improved by exposure to mild hyperbaric oxygen It accelerated the growth induced increase in oxidative capacity of the skeletal muscle in rats and inhibited the age related decrease in oxidative capacity of the skeletal muscle in mice A decrease in dopaminergic neurons in the substantia nigra of mice with Parkinson s disease was inhibited by exposure to mild hyperbaric oxygen This review describes the beneficial effects of exposure to mild hyperbaric oxygen on some metabolic diseases and their perspectives Keywords Dissolved oxygen Mild hyperbaric oxygen Oxidative metabolism Introduction Oxygen is essential for energy production in most cells and is carried by red blood cells that flow in blood vessels The oxygen bound to hemoglobin in red blood cells is referred to as the oxygen bound to hemoglobin The oxygen dissolved in blood plasma is referred to as the dissolved oxygen Although the quantity of dissolved oxygen is less than that of oxygen bound to hemoglobin it can flow to peripheral cells especially those in the brain heart and eyes even if capillaries are very narrow since it is dissolved directly in blood plasma Fig 1a Enhanced atmospheric pressure and or increased oxygen concentration can increase the oxygen content especially the dissolved oxygen content in blood plasma 1 2 Fig 1b Exposure to mild hyperbaric oxygen at 1266 1317 hPa with 35 40 oxygen inhibited metabolic syndrome 3 and lifestyle related diseases including type 2 diabetes 4 and hypertension 5 in experimental animals since it improved oxidative metabolism which was lower than that in controls 6 Akihiko Ishihara ishihara akihiko 8s kyoto u ac jp 1 Laboratory of Cell Biology and Life Science Graduate School of Human and Environmental Studies Kyoto University Sakyo ku Kyoto 606 8501 Japan However side effects associated with enhanced atmospheric pressure and or increased oxygen concentration including barotrauma and excessive production of reactive oxygen species in tissues and organs are thought to occur Hyperbaric oxygen therapy at 2026 3039 hPa with 100 oxygen for medical treatment is associated with the risk of inducing myopia and cataracts 7 9 A previous study 7 reported that exposure to hyperbaric oxygen at 2534 hPa with 100 oxygen for 2 2 5 h twice a week up to 100 sessions induces cataracts in guinea pigs Similarly myopia and cataracts developed in human lenses after exposure to prolonged hyperbaric conditions of 2026 2534 hPa with 100 oxygen for 90 min once a day from 150 to 850 sessions 8 however it was rarely seen to occur after only 48 sessions of hyperbaric oxygen conditions at 2534 hPa for 90 min 9 Hyperbaric oxygen therapy increases the number of invasive inflammatory cells in mice 10 and causes excessive production of reactive oxygen species in rats 11 12 rabbits 13 and humans 14 Excessive production of reactive oxygen species plays a key role in the pathogenesis of many diseases and their complications generation of free radicals and increased levels of oxidative stress are associated with atherosclerosis cataracts retinopathy myocardial infarction hypertension diabetes renal failure and uremia 15 17 In addition regardless of pressure oxygen treatments involving 40 oxygen have shown adverse effects e g damage of erythrocytes due to reactive oxygen species 13 Vol 0123456789
574 The Journal of Physiological Sciences 2019 69 573 580 a b red blood cell oxygen bound to hemoglobin dissolved oxygen hemoglobin blood vessel Fig 1 Schematic diagram depicting the distribution of oxygen bound to hemoglobin and dissolved oxygen in blood vessels under normobaric a and mild hyperbaric oxygen b conditions Abundant hemoglobin is distributed in red blood cells and up to four oxygen molecules can bind to one hemoglobin oxygen bound to hemoglobin The other kind of oxygen is dissolved in blood plasma dissolved oxygen The quantity of dissolved oxygen is less than that of oxygen bound to hemoglobin Enhanced atmospheric pressure and or oxygen concentration can increase oxygen in the body especially dissolved oxygen in blood plasma In addition dissolved oxygen is able to flow to the peripheral cells especially those in the brain heart and eyes even if capillaries are very narrow since it is dissolved directly in blood plasma and reduced quantity of oxygen bound to hemoglobin in rats 18 Exposure to mild hyperbaric oxygen at a low oxygen concentration 35 40 oxygen does not result in enhanced levels of oxidative stress in rats 5 19 and humans 20 Based on previous findings from experimental animal and human clinical studies the effects of exposure to mild hyperbaric oxygen at 1266 1317 hPa with 35 40 oxygen are summarized in Table 1 It is noteworthy that these findings were obtained in the first step of exposure to mild hyperbaric oxygen Therefore it is expected to define a suitable recommendation regarding a generally applicable protocol for exposure to mild hyperbaric oxygen in the subsequent step This review describes the beneficial effects of exposure to mild hyperbaric oxygen on some metabolic diseases and related perspectives lipoprotein cholesterol and triglyceride levels 21 22 Experimental animals with metabolic syndrome have a nonsense mutation in the leptin receptor 23 24 Rats with metabolic syndrome have a low oxidative capacity in the skeletal muscle compared to normal rats 6 25 Reduced oxidative capacity in the skeletal muscle is suggested to impair glucose metabolism and increase the risk of development of metabolic syndrome 6 21 22 25 Rats with metabolic syndrome exposed to mild hyperbaric oxygen had lower blood pressure blood glucose total cholesterol triglyceride and insulin levels but higher adiponectin levels than those not exposed to mild hyperbaric oxygen 3 In addition rats with metabolic syndrome exposed to mild hyperbaric oxygen had high oxidative capacity and increased levels of peroxisome proliferatoractivated receptor coactivator 1 Pgc 1 mRNA which plays an important role in oxidative metabolism by regulating mitochondrial biogenesis in the skeletal muscle 26 27 Exposure to mild hyperbaric oxygen is thus considered to inhibit the growth related increase in blood glucose levels and decrease the muscle oxidative capacity of rats with metabolic syndrome owing to the improved oxidative metabolism 3 Metabolic syndrome Metabolic syndrome linked to chronic physical inactivity and consumption of a high fat and high calorie diet is characterized by obesity high blood pressure and increased blood glucose low density 13
The Journal of Physiological Sciences 2019 69 573 580 575 Table 1 Effects of exposure to mild hyperbaric oxygen reported in previous studies Species Metabolic syndrome Type 2 diabetes SHR NDmcr cp rat GK rat OLETF rat GK rat Diabetes induced cataracts Repeated inbreeding of diabetic mouse Hypertension SHR Arthritis Collagen induced DA rat Parkinson s disease MTPT injected C57BL 6JJmsSlc mouse Pigmentation Male subject irradiated with UVB Female subject Proliferation Aged hairless Hos HR 1 mouse Metabolism Human Skeletal muscle fiber Spinal motoneuron Infertility Wistar rat Wistar rat Aged ICR mouse Wistar rat GK rat Woman with intractable infertility Effects References Inhibition of metabolic syndrome Inhibition of type 2 diabetes Inhibition of type 2 diabetes Improvement of type 2 diabetes Inhibition of cataracts Inhibition of hypertension Inhibition of arthritis Inhibition of decrease in dopaminergic neuron Melanin pigmentation turns light Senile spot size becomes small Improvement of proliferative activity of epidermal basal cell Decrease in SpO2 increase in resting HR and energy expenditure Increase in oxidative capacity Inhibition of atrophy Improvement of oxidative capacity Increase in oxidative capacity Improvement of oxidative capacity Improvement of the outcome of in vitro fertilization 3 4 36 37 38 39 46 5 19 86 62 62 60 20 63 64 83 69 63 64 44 96 SHR spontaneously hypertensive rat GK Goto Kakizaki OLETF Otsuka Long Evans Tokushima Fatty DA dark Agouti UVB ultraviolet B ICR Institute of Cancer Research MPTP 1 methyl 4 phenyl 1 2 3 6 tetrahydropyridine hydrochloride SpO2 peripheral oxygen saturation HR heart rate Type 2 diabetes In general blood glucose hemoglobin A1c HbA1c and triglyceride levels are higher in patients with diabetes than in healthy lean people Hyperglycemia worsens vascular disorders including a stroke myocardial infarction retinopathy nephropathy and peripheral neuropathy Patients with type 2 diabetes have decreased oxidative capacity in the skeletal muscle similar to those with metabolic syndrome 28 Decreased oxidative capacity in the skeletal muscle of patients with diabetes is suggested to be related to insulin resistance and impaired glucose metabolism Both nonobese and obese rats with diabetes which were developed as Goto Kakizaki 29 30 and Otsuka Long Evans Tokushima Fatty 31 models respectively have lower oxidative capacity in the skeletal muscle than that of normal rats 32 34 Zucker diabetic fatty rats show similar muscle properties as obese rats with diabetes 35 Blood glucose HbA1c and triglyceride levels were higher in non obese and obese rats with diabetes than in normal rats 33 34 and those levels improved by exposure to mild hyperbaric oxygen 4 36 In the skeletal muscle Pgc 1 myogenin and myogenic factor 5 mRNA levels and oxidative capacity were higher in rats with diabetes exposed to mild hyperbaric oxygen than in those not exposed to mild hyperbaric oxygen 37 38 The growth related increase in blood glucose levels in rats with type 2 diabetes was inhibited by exposure to mild hyperbaric oxygen 4 36 38 The decreased blood glucose levels induced by exposure to mild hyperbaric oxygen in rats with type 2 diabetes were maintained even after these rats were subsequently returned to breeding under normobaric conditions 39 The increased blood glucose levels of adult rats with type 2 diabetes not exposed to mild hyperbaric oxygen were lowered even if they were exposed to mild hyperbaric oxygen afterward 39 These results indicate that low blood glucose levels in rats with type 2 diabetes can be maintained by exposure to mild hyperbaric oxygen compared to those not exposed to mild hyperbaric oxygen both when blood glucose levels are increasing during growth 36 38 and after blood glucose levels are high in adulthood 39 Exposure to mild hyperbaric oxygen therefore seems to prevent the decrease in oxidative capacity of the skeletal muscle of rats with type 2 diabetes irrespective of their age 36 38 In addition exposure to mild hyperbaric oxygen is effective for the inhibition 4 36 38 as well as improvement 39 of hyperglycemia in rats with type 2 diabetes The morphological and histochemical properties of fibers in the skeletal muscle correspond well with those of spinal motoneurons that innervate muscle fibers 40 43 A previous study 44 had shown decreased oxidative capacity of spinal motoneurons in rats with type 2 diabetes In addition this study 44 had examined the effects of exposure to mild hyperbaric oxygen on oxidative capacity 13
576 of spinal motoneurons The inhibition of growth related decrease in oxidative capacity of spinal motoneurons by exposure to mild hyperbaric oxygen corresponds well with that observed in muscle fibers innervated by spinal motoneurons thereby implying that the properties and responses of spinal motoneurons and their innervating muscle fibers are closely related under diabetic as well as normal conditions 44 Diabetes induced cataracts Cataracts are characterized by an accumulation of sorbitol mediated by aldose reductase activity The polyol pathway is the major contributor to diabetes induced cataracts i e the denaturation of lens protein since an increased flux of glucose via this pathway leads to diabetic lesions in the lens and large quantities of glucose are reduced to sorbitol which is not metabolized any further 45 The increased availability of oxygen by exposure to mild hyperbaric oxygen inhibited the growth related increase in blood glucose levels in rats with type 2 diabetes thereby delaying cataract formation induced by the accumulation of sorbitol in the lens 46 Hypertension Spontaneously hypertensive rats SHRs were developed by repeated inbreeding of normal Wistar Kyoto rats which exhibited high blood pressure levels 47 SHRs exposed to mild hyperbaric oxygen showed lower systolic and diastolic blood pressure levels than those of age matched SHRs not exposed to mild hyperbaric oxygen 5 Furthermore SHRs exposed to mild hyperbaric oxygen had lower oxidative stress and higher antioxidant levels than age matched SHRs not exposed to mild hyperbaric oxygen 5 Abnormalities of central neural mechanisms regulating the peripheral sympathetic outflow i e an enhanced sympathetic activation and catecholamine metabolism following neurotransmitter release from nerve endings have been associated with hypertension 48 49 An enhanced sympathetic activation in rats with hypertension is mediated by the overproduction of highly reactive oxygen species which induces sympathoexcitation and thus hypertension 50 51 whereas exposure to mild hyperbaric oxygen has been suggested to eliminate reactive oxygen species and maintain normal blood pressure levels 5 An enhancement of oxidative metabolism in cells and tissues increases the carbon dioxide concentration in the surrounding region which in turn facilitates blood flow in blood vessels 52 53 13 The Journal of Physiological Sciences 2019 69 573 580 Arthritis Exposure to mild hyperbaric oxygen is effective in decreasing levels of reactive oxygen species overproduced in arthritis 19 Oxidative stress and C reactive protein levels are high in rats with arthritis 54 whereas the levels shifted to those in normal rats by exposure to mild hyperbaric oxygen 19 Arthritic joints are characterized by hypoxia caused by an increased oxygen demand and decreased blood flow triggered by the increased intraarticular pressure 55 57 Therefore exposure to mild hyperbaric oxygen is effective in reducing reactive oxygen species levels overproduced during arthritis 19 Pigmentation and proliferation The skin undergoes age related degenerative changes including tissue dehydration and transepidermal water loss 58 Proliferation of epidermal basal cells decreases with age 59 Exposure to mild hyperbaric oxygen has been reported to accelerate the proliferative activity of epidermal basal cells in aged mouse skin 60 An adequate oxygen supply from exposure to mild hyperbaric oxygen may accelerate the turnover rate of aged skin by enhancing the proliferative activity of epidermal basal cells Therefore the dissolved oxygen which is increased by exposure to mild hyperbaric oxygen is considered to diffuse from the dermis to the epidermis through blood microcirculation thus accelerating proliferation of epidermal basal cells and inhibiting epidermal aging 60 Suppression of ultraviolet B irradiation induced pigmentation is due at least in part to the reduction in prostaglandin synthesis via the inhibition of cyclooxygenase by indomethacin and to the induction of annexin or lipocortin by corticosteroids 61 Exposure to mild hyperbaric oxygen was found to accelerate the fading of ultraviolet B irradiation induced melanin pigmentation of the skin 62 Furthermore senile spot sizes on faces became smaller after exposure to mild hyperbaric oxygen 62 Keratinocyte proliferation and epidermal cell regeneration are considered to be activated by enhanced oxidative metabolism induced by exposure to mild hyperbaric oxygen which may be effective for damage repair in the epidermis Adaptation of the neuromuscular system Exposure to mild hyperbaric oxygen facilitates oxidative metabolism particularly in pathways such as the mitochondrial tricarboxylic acid cycle thus enhancing the oxidative
The Journal of Physiological Sciences 2019 69 573 580 capacity of skeletal muscle fibers and the spinal motoneurons innervating them 63 64 Growing rats exposed to mild hyperbaric oxygen exhibited greater voluntary running activities compared to those maintained under normobaric conditions without exposure to mild hyperbaric oxygen the oxidative capacity of muscle fibers and the innervating spinal motoneurons in rats increased after exposure to mild hyperbaric oxygen 64 Reduction in skeletal muscle mass is one of the most striking features of the aging process 65 Atrophy and reduced oxidative capacity of the skeletal muscle have been observed with age 66 67 Muscle atrophy in aged rats is associated with reduced activity levels of certain enzymes involved in oxidative metabolism 68 An agerelated decrease in oxidative capacity of the skeletal muscle in mice was reported to be reversed by exposure to mild hyperbaric oxygen 69 as much as by exercise in aged rats 70 Exposure to mild hyperbaric oxygen has an advantage over exercise since it can increase the dissolved oxygen content owing to the enhanced atmospheric pressure and or increased oxygen concentration which does not occur in exercise Therefore it is concluded that exposure to mild hyperbaric oxygen reduces the age related decrease in oxidative capacity of the skeletal muscle due to the improvement in oxidative metabolism 69 Chronic inactivity as in hind limb unloading and microgravity exposure induces atrophy and degenerative changes in the skeletal muscle and its fibers 71 75 as well as in spinal motoneurons that innervate the muscle fibers 76 82 Muscle atrophy and decreased oxidative capacity were shown to be unaffected by either pre or post conditioning with exposure to mild hyperbaric oxygen 83 In contrast the degenerative changes were almost restored to normal levels after reloading when pre and post conditionings with exposure to mild hyperbaric oxygen were combined 83 Only a combination of pre and post conditionings is considered to activate the signaling cascades required for the recovery from atrophy and decreased oxidative capacity of the skeletal muscle Parkinson s disease Parkinson s disease is a progressive neurodegenerative disorder in the elderly that is characterized by typical motor symptoms such as resting tremors rigidity bradykinesia and gait disturbances 84 Parkinson s disease results from the progressive decrease in dopaminergic neurons in the substantia nigra 85 Exposure to mild hyperbaric oxygen was shown to inhibit the decrease in dopaminergic neurons in the substantia nigra of a neurotoxic experimental animal with Parkinson s disease 86 The number of times the feet of the mouse slid off the stick in a balance beam test was fewer in 577 mice with Parkinson s disease exposed to mild hyperbaric oxygen than in those not exposed to mild hyperbaric oxygen 86 PGC 1 a transcriptional co activator may be one of the factors that contribute to the improvement in oxidative metabolism of dopaminergic neurons in Parkinson s disease 87 since oxidative metabolism mitochondrial biogenesis oxidative stress and gene expression are regulated by PGC 1 88 89 It is concluded that exposure to mild hyperbaric oxygen activates oxidative metabolism in the dopaminergic neurons in the substantia nigra and inhibits the reduction in dopaminergic neurons thereby resulting in the inhibition of Parkinson s disease 86 Infertility Hyperbaric oxygen therapy an established medical treatment usually conducted under conditions of 2026 3039 hPa with 100 oxygen has been investigated for improving female 90 93 and male 94 95 infertility However several side effects including barotrauma and excessive production of reactive oxygen species associated with hyperbaric oxygen therapy have been reported 7 12 14 Low metabolism in the uterus and ovaries may be a factor responsible for infertility since the former reduces the ability of fertilized eggs to remain in the uterus Exposure to mild hyperbaric oxygen has been suggested to enhance oxygen supply to cells and tissues thus improving oxidative metabolism without barotrauma and excessive production of reactive oxygen species In a recent study 96 37 women with intractable infertility who had previously received over 5 embryo transfers with a low clinical pregnancy rate 4 9 and without birth were exposed to mild hyperbaric oxygen before receiving any further embryo transfer As a result 13 women achieved clinical pregnancy with a rate of 13 8 5 women gave birth after in vitro fertilization treatment Two women achieved natural conception and gave birth However 1 woman had an extra uterine pregnancy and 5 women had miscarriages Perspectives on exposure to mild hyperbaric oxygen Exposure to mild hyperbaric oxygen is effective for elderly people those with physical disability as well as injured athletes since no special movement needs to be performed under mild hyperbaric oxygen conditions In future exposure to mild hyperbaric oxygen may be investigated for 1 prevention and improvement of dementia 2 improvement of functional imbalances of autonomic sympathetic and parasympathetic nerves e g menopausal disorders and emotional instability 3 maintenance and improvement of 13
578 immunity health and physical fitness and 4 early recovery from an injury Further studies are required to solve these problems and define a useful protocol for exposure to mild hyperbaric oxygen Compliance with ethical standards Ethical approval This article does not contain any studies with animals or human participants performed by the author References 1 Tibbles PM Edelsberg JS 1996 Hyperbaric oxygen therapy N Engl J Med 334 1642 1648 2 Leach RM Rees PJ Wilmshurst P 1998 Hyperbaric oxygen therapy BMJ 317 1140 1143 3 Takemura A Ishihara A 2017 Mild hyperbaric oxygen inhibits growth related decrease in muscle oxidative capacity of rats with metabolic syndrome J Atheroscler Thromb 24 26 38 4 Yasuda K Aoki N Adachi T Tsujimoto G Gu N Matsunaga T Kikuchi N Tsuda K Ishihara A 2006 Hyperbaric exposure with high oxygen concentration inhibits growth associated increase in the glucose level of diabetic Goto Kakizaki rats Diabetes Obes Metab 8 714 715 5 Nagatomo F Fujino H Takeda I Ishihara A 2010 Effects of hyperbaric oxygenation on blood pressure levels of spontaneously hypertensive rats Clin Exp Hypertens 32 193 197 6 Nagatomo F Gu N Fujino H Takeda I Tsuda K Ishihara A 2009 Skeletal muscle characteristics of rats with obesity diabetes hypertension and hyperlipidemia J Atheroscler Thromb 16 576 585 7 Giblin FJ Padgaonkar VA Leverenz VR Lin LR Lou MF Unakar NJ Dang L Dickerson JE Jr Reddy VN 1995 Nuclear light scattering disulfide formation and membrane damage in lenses of older guinea pigs treated with hyperbaric oxygen Exp Eye Res 60 219 235 8 Palmquist BM Philipson B Barr PO 1984 Nuclear cataract and myopia during hyperbaric oxygen therapy Br J Ophthalmol 68 113 117 9 Gesell LB Trott A 2007 De novo cataract development following a standard course of hyperbaric oxygen therapy Undersea Hyperb Med 34 389 392 10 Folz RJ Abushamaa AM Suliman HB 1999 Extracellular superoxide dismutase in the airways of transgenic mice reduces inflammation and attenuates lung toxicity following hyperoxia J Clin Invest 103 1055 1066 11 Oter S Korkmaz A Topal T Ozcan O Sadir S Ozler M Ogur R Bilgic H 2005 Correlation between hyperbaric oxygen exposure pressures and oxidative parameters in rat lung brain and erythrocytes Clin Biochem 38 706 711 12 Oter S Topal T Sadir S Ozler M Uysal B Ay H Yaren H Korhmaz A Akin A 2007 Oxidative stress levels in rats following exposure to oxygen at 3 atm for 0 120 min Aviat Space Environ Med 78 1108 1113 13 Padgaonkar VA Leverenz VR Fowler KE Reddy VN Giblin FJ 2000 The effects of hyperbaric oxygen on the crystallins of cultured rabbit lenses a possible catalytic role for copper Exp Eye Res 71 371 383 13 The Journal of Physiological Sciences 2019 69 573 580 14 Narkowicz CK Vial JH McCartney PW 1993 Hyperbaric oxygen therapy increases free radical levels in the blood of humans Free Radic Res Commun 19 71 80 15 Maier CM Chan PH 2002 Role of superoxide dismutases in oxidative damage and neurodegenerative disorders Neuroscientist 8 323 334 16 Griendling KK FitzGerald GA 2003 Oxidative stress and cardiovascular injury part I basic mechanisms and in vivo monitoring of ROS Circulation 108 1912 1916 17 Dalle Donne I Rossi R Colombo R Giustarini D Milzani A 2006 Biomarkers of oxidative damage in human disease Clin Chem 52 601 623 18 Nagatomo F Fujino H Kondo H Ishihara A 2012 Oxygen concentration dependent oxidative stress levels in rats Oxid Med Cell Longev https doi org 10 1155 2012 38176 3 19 Nagatomo F Gu N Fujino H Okiura T Morimatsu F Takeda I Ishihara A 2010 Effects of exposure to hyperbaric oxygen on oxidative stress in rats with type II collagen induced arthritis Clin Exp Med 10 7 13 20 Ishihara A Nagatomo F Fujino H Kondo H 2014 Exposure to mild hyperbaric oxygen increases blood flow and resting energy expenditure but not oxidative stress J Sci Res Rep 3 1886 1896 21 Nagatomo F Fujino H Kondo H Takeda I Tsuda K Ishihara A 2012 High fat diet induced reduction of PGC 1 mRNA levels and oxidative capacity in the soleus muscle of rats with metabolic syndrome Nutr Res 32 144 151 22 Nagatomo F Fujino H Kondo H Kouzaki K Gu N Takeda I Tsuda K Ishihara A 2012 The effects of running exercise on oxidative capacity and PGC 1 mRNA levels in the soleus muscle of rats with metabolic syndrome J Physiol Sci 62 105 114 23 Koletsky S 1973 Obese spontaneously hypertensive rats a model for study of atherosclerosis Exp Mol Pathol 19 53 60 24 Koletsky S 1975 Pathologic findings and laboratory data in a new strain of obese hypertensive rats Am J Pathol 80 129 142 25 Nagatomo F Fujino H Kondo H Gu N Takeda I Ishioka N Tsuda K Ishihara A 2011 PGC 1 mRNA level and oxidative capacity of the plantaris muscle in rats with metabolic syndrome hypertension and type 2 diabetes Acta Histochem Cytochem 44 73 80 26 Miura S Kai Y Ono M Ezaki O 2003 Overexpression of peroxisome proliferator activated receptor coactivator 1 downregulates GLUT4 mRNA in skeletal muscles J Biol Chem 278 31385 31390 27 Mortensen OH Frandsen L Schjerling P Nishimura E Grunnet N 2006 PGC 1 and PGC 1 have both similar and distinct effects on myofiber switching towards an oxidative phenotype Am J Physiol Endocrinol Metab 291 E807 E816 28 Ishihara A Nagatomo F Fujino H Kondo H Tsuda K 2012 Lifestyle related disease and skeletal muscle J Phys Fit Sports Med 1 17 27 29 Goto Y Kakizaki M Masaki N 1975 Spontaneous diabetes produced by selective breeding of normal Wistar rats Proc Jpn Acad 51 80 85 30 Goto Y Kakizaki M Masaki N 1976 Production of spontaneous diabetic rats by repetition of selective breeding Tohoku J Exp Med 119 85 90 31 Kawano K Hirashima T Mori S Saitoh Y Kurosumi M Natori T 1992 Spontaneous long term hyperglycemic rat with diabetic complications Otsuka Long Evans Tokushima Fatty OLETF strain Diabetes 41 1422 1428 32 Yasuda K Ishihara A Adachi T Shihara N Seino Y Tsuda K 2001 Growth related changes in skeletal muscle fiber type and insulin resistance in diabetic Otsuka Long Evans Tokushima Fatty rats Acta Histochem Cytochem 34 371 382 33 Yasuda K Nishikawa W Iwanaka N Nakamura E Seino Y Tsuda K Ishihara A 2002 Abnormality in fibre type distribution of
The Journal of Physiological Sciences 2019 69 573 580 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 soleus and plantaris muscles in non obese diabetic Goto Kakizaki rats Clin Exp Pharmacol Physiol 29 1001 1008 Yasuda K Adachi T Kikuchi N Tsujimoto G Aoki N Tsuda K Ishihara A 2006 Effects of running exercise on fibre type distribution of soleus and plantaris muscles in diabetic Otsuka LongEvans Tokushima fatty rats Diabetes Obes Metab 8 311 321 Adachi T Kikuchi N Yasuda K Anahara R Gu N Matsunaga T Yamamura T Mori C Tsujimoto G Tsuda K Ishihara A 2007 Fibre type distribution and gene expression levels of both succinate dehydrogenase and peroxisome proliferator activated receptor coactivator 1 of fibres in the soleus muscle of Zucker diabetic fatty rats Exp Physiol 92 449 455 Yasuda K Adachi T Gu N Matsumoto A Matsunaga T Tsujimoto G Tsuda K Ishihara A 2007 Effects of hyperbaric exposure with high oxygen concentration on glucose and insulin levels and skeletal muscle fiber properties in diabetic rats Muscle Nerve 35 337 343 Matsumoto A Nagatomo F Yasuda K Tsuda K Ishihara A 2007 Hyperbaric exposure with high oxygen concentration improves altered fiber types in the plantaris muscle of diabetic Goto Kakizaki rats J Physiol Sci 57 133 136 Nagatomo F Takemura A Roy RR Fujino H Kondo H Ishihara A 2018 Mild hyperbaric oxygen inhibits the growth related decline in skeletal muscle oxidative capacity and prevents hyperglycemia in rats with type 2 diabetes J Diabetes 10 753 763 Gu N Nagatomo F Fujino H Takeda I Tsuda K Ishihara A 2010 Hyperbaric oxygen exposure improves blood glucose level and muscle oxidative capacity in rats with type 2 diabetes Diabetes Technol Ther 12 125 133 Ishihara A Roy RR Edgerton VR 1995 Succinate dehydrogenase activity and soma size of motoneurons innervating different portions of the rat tibialis anterior Neuroscience 68 813 822 Ishihara A Hori A Roy RR Oishi Y Talmadge RJ Ohira Y Kobayashi S Edgerton VR 1997 Perineal muscles and their innervation metabolic and functional significance of the motor unit Acta Anat 159 156 166 Ishihara A Itoh K Itoh M Hirofuji C 2000 Effect of hypobaric hypoxia on rat soleus muscle fibers and their innervating motoneurons a review Jpn J Physiol 50 561 568 Nakatani T Nakashima T Kita T Ishihara A 2003 Cell size and oxidative enzyme activity of type identified fibers in rat hindlimb muscles a review Acta Histochem Cytochem 36 105 114 Takemura A Ishihara A 2016 Mild hyperbaric oxygen improves decreased oxidative capacity of spinal motoneurons innervating the soleus muscle of rats with type 2 diabetes Neurochem Res 41 2336 2344 Chung SSM Ho ECM Lam KSL Chung SK 2003 Contribution of polyol pathway to diabetes induced oxidative stress J Am Soc Nephrol 14 Suppl 3 233 236 Nagatomo F Roy RR Takahashi H Edgerton VR Ishihara A 2011 Effect of exposure to hyperbaric oxygen on diabetesinduced cataracts in mice J Diabetes 3 301 308 Okamoto K Aoki K 1963 Development of a strain of spontaneously hypertensive rats Jpn Circ J 27 282 293 Patel KP Kline RL Mercer PF 1981 Noradrenergic mechanisms in the brain and peripheral organs of normotensive and spontaneously hypertensive rats at various ages Hypertension 3 682 690 Grassi G 1998 Role of the sympathetic nervous system in human hypertension J Hypertens 16 1979 1987 Kishi T Hirooka Y Kimura Y Ito K Shimokawa H Takeshita A 2004 Increased reactive oxygen species in rostral ventrolateral medulla contribute to neural mechanisms of hypertension in stroke prone spontaneously hypertensive rats Circulation 109 2357 2362 Lindley TE Doobay MF Sharma RV Davisson RI 2004 Superoxide is involved in the central nervous system activation and 579 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 sympathoexcitation of myocardial infarction induced heart failure Circ Res 94 402 409 Matsumoto T Tanaka M Ikeji T Maeshige N Sakai Y Akisue T Kondo H Ishihara A Fujino H 2019 Application of transcutaneous carbon dioxide improves capillary regression of skeletal muscle in hyperglycemia J Physiol Sci 69 317 326 Matsumoto T Tanaka M Nakanishi R Takuwa M Hirabayashi T Ono K Ikeji T Maeshige N Sakai Y Akisue T Kondo K Ishihara A Fujino H 2019 Transcutaneous carbon dioxide attenuates impaired oxidative capacity in skeletal muscle in hyperglycemia Gen Physiol Biophys accepted Okiura T Nagatomo F Gu N Taguchi Y Morimatsu F Ishihara A 2008 Bone density of the femur and fiber cross sectional area and oxidative enzyme activity of the tibialis anterior muscle in type II collagen induced arthritic mice J Physiol Sci 58 221 227 Woodruff T Blake DR Freeman J Andrews FJ Salt P Lunec J 1986 Is chronic synovitis an example of reperfusion injury Ann Rheum Dis 45 608 611 Cross CE Halliwell B Borish ET Pryor WA Ames BN Saul RL McCord JM Harman D 1987 Oxygen radicals and human disease Ann Intern Med 107 526 545 Blake DR Merry P Unsworth J Kidd BL Outhwaite JM Ballard R Morris CJ Gray L Lunec J 1989 Hypoxic reperfusion injury in the inflamed human joint Lancet 11 289 293 Wilhelm KP Cua AB Maibach HI 1991 Skin aging effect on transepidermal water loss stratum corneum hydration skin surface pH and casual sebum content Arch Dermatol 127 1806 1809 Grove GL Kligman AM 1983 Age associated changes in human epidermal cell renewal J Gerontol 38 137 142 Nishizaka T Nomura T Higuchi K Takemura A Ishihara A 2018 Mild hyperbaric oxygen activates the proliferation of epidermal basal cells in aged mice J Dermatol 45 1141 1144 Flower RJ 1986 Background and discovery of lipocortins Agents Actions 17 255 262 Nishizaka T Nomura T Sano T Higuchi K Nagatomo F Ishihara A 2011 Hyperbaric oxygen improves UVB irradiation induced melanin pigmentation and diminishes senile spot size Skin Res Tech 17 332 338 Ishihara A Kawano F Okiura T Morimatsu F Ohira Y 2005 Hyperbaric exposure with high oxygen concentration enhances oxidative capacity of neuromuscular units Neurosci Res 52 146 152 Matsumoto A Okiura T Morimatsu F Ohira Y Ishihara A 2007 Effects of hyperbaric exposure with high oxygen concentration on the physical activity of developing rats Dev Neurosci 29 452 459 Schiaffino S Dyar KA Ciciliot S Blaauw B Sandri M 2013 Mechanisms regulating skeletal muscle growth and atrophy FEBS J 280 4294 4314 Ishihara A Naitoh H Katsuta S 1987 Effects of ageing on the total number of muscle fibers and motoneurons of the tibialis anterior muscles in the rat Brain Res 435 355 358 Ishihara A Araki H 1988 Effects of age on the number and histochemical properties of muscle fibers and motoneurons in the rat extensor digitorum longus muscle Mech Ageing Dev 45 213 221 Hirofuji C Ishihara A Roy RR Itoh K Itoh M Edgerton VR Katsuta S 2000 SDH activity and cell size of tibialis anterior motoneurons and muscle fibers in SAMP6 Neuroreport 11 823 828 Nishizaka T Nagatomo F Fujino H Nomura T Sano T Higuchi K Takeda I Ishihara A 2010 Hyperbaric oxygen exposure reduces age related decrease in oxidative capacity of the tibialis anterior muscle in mice Enzyme Res https doi org 10 4061 2010 82476 3 Ishihara A Taguchi S 1993 Effect of exercise on age related muscle atrophy Neurobiol Aging 14 331 335 13
580 71 Ishihara A Oishi Y Roy RR Edgerton VR 1997 Influence of two weeks of non weight bearing on rat soleus motoneurons and muscle fibers Aviat Space Environ Med 68 421 425 72 Ishihara A Kawano F Ishioka N Oishi H Higashibata A Shimazu T Ohira Y 2004 Effects of running exercise during recovery from hindlimb unloading on soleus muscle fibers and their spinal motoneurons in rats Neurosci Res 48 119 127 73 Ishihara A Fujino H Nagatomo F Takeda I Ohira Y 2008 Gene expression levels of heat shock proteins in the soleus and plantaris muscles of rats after hindlimb suspension or spaceflight J Physiol Sci 58 413 417 74 Nagatomo F Fujino H Kondo H Suzuki H Kouzaki M Takeda I Ishihara A 2011 PGC 1 and FOXO1 mRNA levels and fiber characteristics of the soleus and plantaris muscles in rats after hindlimb unloading Histol Histopathol 26 1545 1553 75 Ishihara A Nagatomo F Terada M Fujino H Kondo H Ishioka N 2015 Effects of microgravity on the mouse triceps brachii muscle Muscle Nerve 52 63 68 76 Ishihara A Ohira Y Roy RR Nagaoka S Sekiguchi C Hinds WE Edgerton VR 1996 Influence of spaceflight on succinate dehydrogenase activity and soma size of rat ventral horn neurons Acta Anat 157 303 308 77 Ishihara A Ohira Y Roy RR Nagaoka S Sekiguchi C Hinds WE Edgerton VR 1997 Effects of 14 days of spaceflight and nine days of recovery on cell body size and succinate dehydrogenase activity of rat dorsal root ganglion neurons Neuroscience 81 275 279 78 Ishihara A Ohira Y Roy RR Nagaoka S Sekiguchi C Hinds WE Edgerton VR 2000 Comparison of the response of motoneurons innervating perineal and hind limb muscles to spaceflight and recovery Muscle Nerve 23 753 762 79 Ishihara A Ohira Y Roy RR Nagaoka S Sekiguchi C Hinds WE Edgerton VR 2002 Succinate dehydrogenase activity in rat dorsolateral ventral horn motoneurons at L6 after spaceflight and recovery J Gravit Physiol 9 39 48 80 Ishihara A Yamashiro J Matsumoto A Higashibata A Ishioka N Shimazu T Ohira Y 2006 Comparison of cell body size and oxidative enzyme activity in motoneurons between the cervical and lumbar segments in the rat spinal cord after spaceflight and recovery Neurochem Res 31 411 415 81 Nagatomo F Ishihara A Ohira Y 2009 Effects of hindlimb unloading at early postnatal growth on cell body size in spinal motoneurons innervating soleus muscle of rats Int J Dev Neurosci 27 21 26 82 Ishihara A Nagatomo F Fujino H Kondo H Ohira Y 2013 Decreased succinate dehydrogenase activity of gamma and alpha motoneurons in mouse spinal cords following 13 weeks of exposure to microgravity Neurochem Res 38 2160 2167 83 Takemura A Roy RR Yoshihara I Ishihara A 2017 Unloadinginduced atrophy and decreased oxidative capacity of the soleus muscle in rats are reversed by pre and postconditioning with mild hyperbaric oxygen Physiol Rep 5 e13353 13 The Journal of Physiological Sciences 2019 69 573 580 84 Adler CH 2005 Nonmotor complications in Parkinson s disease Mov Disord 20 Suppl 11 S23 S29 85 Dauer W Przedborski S 2003 Parkinson s disease mechanisms and models Neuron 39 889 909 86 Kusuda Y Takemura A Nakano M Ishihara A 2018 Mild hyperbaric oxygen inhibits the decrease of dopaminergic neurons in the substantia nigra of mice with MPTP induced Parkinson s disease Neurosci Res 132 58 62 87 Mud G M kel J Di Liberto V Tselykh TV Olivieri M Piepponen P Eriksson O M lki A Bonomo A Kairisalo M Aguirre JA Korhonen L Belluardo N Lindholm D 2012 Transgenic expression and activation of PGC 1 protect dopaminergic neurons in the MPTP mouse model of Parkinson s disease Cell Mol Life Sci 69 1153 1165 88 Wu Z Puigserver P Andersson U Zhang C Adelmant G Mootha V Troy A Cinti S Lowell B Scarpulla RC Spiegelman BM 1999 Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC 1 Cell 98 115 124 89 Liang H Ward WF 2006 PGC 1 a key regulator of energy metabolism Adv Physiol Educ 30 145 151 90 Zadoev SA Evdokimov VV Rumiantsev VB Osmolovski EO 2001 Hyperbaric oxygenation in the treatment of patients with chronic congestive prostatitis and lower fertility Urologiia 1 27 30 91 Leverment J Turner R Bowman M Cooke CJ 2004 Report of the use of hyperbaric oxygen therapy HBO2 in an unusual case of secondary infertility Undersea Hyperb Med 31 245 250 92 Van Voorhis BJ Greensmith JE Dokras A Sparks AE Simmons ST Syrop CH 2005 Hyperbaric oxygen and ovarian follicular stimulation for in vitro fertilization a pilot study Fertil Steril 83 226 228 93 Mitrovi A Nikoli B Dragojevi S 2006 Hyperbaric oxygenation as a possible therapy of choice for infertility treatment Bosn J Basic Med Sci 6 21 24 94 Mitrovi A Brki P Jovanovi T 2011 The effects of hyperbaric oxygen treatment on vigility of spermatozoids preliminary report Acta Physiol Hung 98 85 90 95 Metelev AY Bogdanov AB Ivkinl EV Mitrokhin AA Vodneva MM Veliev EL 2015 Hyperbaric oxygen therapy in the treatment of male infertility associated with increased sperm DNA fragmentation and reactive oxygen species in semen Urologiia 5 74 76 96 Yoshikawa F Netsu Y Shimizu T Ishihara A 2019 Mild hyperbaric oxygen improves the outcome of infertility treatment J Reprod Med accepted Publisher s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations