Return to flip book view
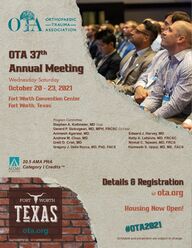
OTA 37thAnnual Meetingota.orgWednesday-SaturdayOctober 20 - 23, 2021#OTA2021Details & Registration@ ota.org20.5 AMA PRA Category I Credits™Fort Worth Convention CenterFort Worth, TexasSchedule and presenters are subject to change.Program CommitteeStephen A. Kottmeier, MD Chair Gerard P. Slobogean, MD, MPH, FRCSC Co-ChairAnimesh Agarwal, MD Edward J. Harvey, MDAndrew M. Choo, MD Kelly A. Lefaivre, MD, FRCSCBrett D. Crist, MD Nirmal C. Tejwani, MD, FRCSGregory J. Della Rocca, MD, PhD, FACS Harmeeth S. Uppal, MD, MS, FACSHousing Now Open!
37th Annual MeetingOctober 20 - 23, 2021Fort Worth, Texas On Demand Gold Registration(Annual Meeting Registration and Annual Meeting On Demand) OTA Member . . . . . . . . . . . . . . . . . . . . . . . $ 550 $ 650 Non-member (Incl. MD, DO, MBBS, etc.) . . . . . . . . $ 1100 $ 1200 Non-member Medical Resident, Fellow, Student . . . . . . . . . . . . . . . . . . . . . . $ 650 $ 750 Non-member Health Care Personnel (incl. NP, PA, AH, PhD, etc.) . . . . . . . . . . . . . . . . . . $ 750 $ 850 Additional Charge for USB . . . . . . . . . . . . . . $ 100 $ 100 Annual Meeting (only) Registration OTA Member . . . . . . . . . . . . . . . . . . . . . . . $ 250 $ 350 Non-member (Incl. MD, DO, MBBS, etc.) . . . . . . . . $ 800 $ 900 Non-member Medical Resident, Fellow, Student . . . . . . . . . . . . . . . . . . . . . . $ 450 $ 550 Non-member Health Care Personnel (incl. NP, PA, AH, PhD, etc.) . . . . . . . . . . . . . . . . . . $ 450 $ 550 Early Bird Registration Until September 30.On/Before 9/30/21After9/30/21On/Before 9/30/21After9/30/21 2Target AudienceThe Orthopaedic Trauma Association (OTA) Annual Meeting is for the benet of orthopaedic trauma surgeons and related allied health care professionals.Meeting Highlights• 26 Breakout sessions including a variety of topics such as pelvic fractures, compartment syndrome, periprosthetic fractures, avoiding burnout, managing lawsuits, dealing with bone loss, open fractures, and many others.• 75 high quality paper presentations, including a session of highlight papers reecting practice-changing research, and over 200 posters • Four main symposia focusing on: - Surgeon Well Being - Practice Changing RCT’s - Racial, Ethnic, and Socioeconomic Disparities in Orthopaedics - IOTA “Tolerate or Re-Operate” Symposium• Industry Symposia showcasing products, demonstrating techniques and/or presenting research offered at three convenient times.Visit ota.org for more details on papers, symposia and breakouts sessions. Border LecturerNoah Galloway“Living with No Excuses” #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org Learning ObjectivesUpon successful completion of this meeting, participants will be able to: üReview the surgical and nonsurgical indications for the included upper extremity fracturesüunderstand that there is a still a roll for nonoperative treatment of fractures and learn when to abandon nonsurgical treatment plansüunderstand the outcomes with nonsurgical and surgical managementPresidents’ Messages“The Courage to Heal: Building Resilience and Transforming Recovery”Heather A. Vallier, MD (Current OTA President)Professor of Orthopaedic SurgeryCase Western Reserve UniversityMetroHealth System – Cleveland, Ohio Michael D. McKee, MD (Immediate Past President)Professor and ChairmanDepartment of Orthopaedic SurgeryUniversity of Arizona College of Medicine – PhoenixBanner – University Medical Center Phoenix
VenueThe Orthopaedic Trauma Association’s 37th Annual Meeting and all pre-meeting courses will be held at the Fort Worth Convention Center and the Resident Comprehensive Fracture Course will be held at the Omni Hotel in Fort Worth, Texas. Visit OTA.org today to register and make hotel reservations. Early Bird Registration: Register by September 30 to save $100 on the Annual Meeting and each Pre-Meeting Registration. Hotel block closes September 26, 2021. Table of ContentsTarget Audience................2Meeting Highlights .............2Objectives ....................2Registration Fees ...............2Donor Appreciation .............3Venue ........................3President’s Welcome ............4Program Chair Welcome .........5Program (Thursday) ...........6 - 8President’s Message ............8Program (Friday) ............9 - 20John Border Lecturer...........14Past President’s Message .......14Program (Saturday) .........20 - 31General Information ............32 Special Events.................33Exhibit Hall Hours..............34The Orthopaedic Trauma Association gratefully acknowledges 2019 Researchand Education Donors. The continued success and increased impact of the Orthopaedic Trauma Association’s research and education effort isdependent upon foundation and industry support.The OTA expresses sincere appreciation to these contributorsfor their generous nancial support.Orthopaedic Trauma Association9400 W Higgins Rd, Suite 305Rosemont, IL 60018Ph: 847.698.1631Email: OTA@ota.orgota.orgotaonline.orgRegister Today at ota.org 32019 & 2020 Research and Education DonorsDIAMOND ($250,000 and above) Platinum ($150,000 - $249,999) Gold ($100,000 - $149,999) SILVER ($75,000 - $99,999)Bronze ($50,000 - $74,999) Copper ($25,000 - $49,999)Sponsor ($5,000 - $24,999) Member ($1,000 - $4,999) Donor level also reects 2019 giving due to the pandemic in 2020
Orthopaedic Trauma Association’s 37th Annual Meeting4 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org President’s WelcomeDear OTA Members and Colleagues,I am hopeful that you have marked your calendar for the OTA’s 2021 Annual Meeting taking place October 20 – 23 in Fort Worth, Texas. I know many of you have already made hotel reservations. Following more than a year of very few chances to meet in person, this year’s meeting will be a very welcome chance to re-engage with colleagues and friends, and take advantage of an outstanding educational program developed by the OTA Annual Meeting Program Committee under the leadership of Stephen Kottmeier MD, Program Committee Chair, and Gerard Slobogean MD, Co-Chair. The 2021 Annual Meeting offers an outstanding array of opportunities to engage in cutting edge orthopaedic trauma education and research, with offerings tailored to every learner. Whether your career in orthopaedic trauma is just beginning, or you are a seasoned practitioner, don’t miss this year’s long awaited reunion of the orthopaedic trauma community!Finally, I want to extend sincere appreciation to the OTA Annual Meeting Program Committee and the many OTA members, presenters, committee members and other volunteers contributing to making this year’s meeting one of the best ever. Hope to see you in Fort Worth! Sincerely,Heather A. Vallier, MDOTA PresidentHeather A. Vallier, MDOTA President
Register Today at ota.org 5October 20 - 23, 2021 • Fort Worth, TexasProgram Chair’s WelcomeStephen A. Kottmeier, MDAnnual Meeting Program ChairDear Colleagues,On behalf of the OTA Program Committee and President Heather Vallier MD, I am pleased to invite you to the 37th Annual Meeting of the Orthopaedic Trauma Association (OTA) to be held in Fort Worth, Texas, from October 20 to 23, 2021. It is our hope and expectation that the present favorable pandemic trajectory will enable us to gather again in October. As a profes-sional medical society, we have remained vibrant over the past year despite not being able to meet in person, but I know our membership and colleagues are looking forward to a long-awaited reunion this forthcoming fall, a time of year cherished for OUR annual meeting. Last year’s virtual meeting was a success, conrmed our resourcefulness as a society, and familiarized us with alternative mechanisms of information delivery. Lessons learned will enable us to supplement our live event with virtual content both live and on demand.In the months leading up to the meeting, the Annual Meeting Committee reviewed over 1,000 scientic abstracts, more than 80 symposia/breakouts, and over 100 technical tricks and innovations. This has culminated in a program that includes the latest cutting-edge, high quality research and state-of-the-art treatment for musculoskeletal injuries. Paper presentations will begin with a “Program Highlights” session, featuring nine original research presentations of the highest quality, many with the potential to be practice-changing. Additionally, there will be many topic-centered paper presentations. Four main symposia will include the evermore important topics of physician wellness and diversity in medicine and our professional society in addi-tion to current surgical procedural “hot topics”. Included within the meeting will be 26 breakout sessions, each with a specic focus to satisfy your interest. There will be over 200 posters in the exhibit hall, and the continuation of a highly regarded novel category entitled Technical Tricks/Innovation in e-poster format.This year we welcome John Border Memorial Lecturer; Iraqi war veteran Noah Galloway who will deliver a talk titled, “Living with no Excuses.”Premeeting events will include:• Inaugural events; Local rst responders session/OTA fellow reception and research event/ OTA Fireside – The Case That I have Learned the Most From: An Evening with Your Colleagues• Orthopaedic Trauma Boot Camp • Orthopaedic Trauma for NPs and PAs• International Trama Care Forum • E/M and Surgical Coding Course• Young Practitioners Forum • Resident Comprehensive Fracture Course• Pelvis and Acetabulum Course • Soft Tissue Coverage Skills CourseThe OTA will continue to monitor any evolving pandemic related issues. The safety of our meeting attendees is a top priority, and we will be working closely with our Fort Worth venue partners to ensure CDC and city/state safety guidelines are in place at the time of the meeting.Your presence and contributions to the meeting are welcomed. The OTA Leadership is looking forward to an academically engaging in person meeting with the social gratications that accompany and nurture it. The collective ambition and mission is to offer a meeting of quality in an environment both safe and collegial. See you in Fort Worth!Sincerely,Stephen A. Kottmeier, MDProgram Chair®NEW!
6 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasPreliminary ProgramThursday, October 21, 2021 1:00 PM - Welcome and Donor Awards 1:20 PM Heather A. Vallier, MD – President Stephen A. Kottmeier, MD – Program Chair 1:20 PM - Local Host Welcome 1:25 PM Cory A. Collinge, MD 1:25 PM - Symposium I: 2:55 PM How Can the OTA Support Your Well-Being? A Panel Discussion and Town Hall on Sustaining Your Career via Advocacy, Leadership and Wellness Moderator: Jeffrey Smith, MD Faculty: Philip R. Wolinsky, MD Heather A. Vallier, MD Anna N. Miller, MD Matthew R. Garner, MD Preston B. Cline, EdD Thomas M. Large, MD Benjamin Caesar, MBBS, MD Learning Objectives • Embody the Wellness Task Force directives from the OTA Board of Directors and the organization’s strategic plan to support our members professional lives. • Recognize and help create opportunities within OTA that foster surgeon wellness / well-being; advocate for these oppor- tunities of career development/support, sustainability, and satisfaction; and combat administrative and organizational burdens that lead to surgeon burnout, moral injury, and disengagement. • Acknowledge the value of your individual input, experiences and ideas on physical, mental, and emotional wellness and share these with the OTA Wellness Task Force openly or through condential feedback and surveys. Description One of the OTA’s new strategic goals is to advocate for orthopaedic trauma surgeons by supporting careers through mentoring, working to improve wellness in physical and mental health, and shaping and inuencing public policy regarding musculoskeletal injury care. In this symposium, we will introduce the Wellness Task Force and the directives from the OTA BOD and Strategic Plan, with the goal of increasing awareness of what the OTA can/should do for your career development and sustainability, and your work-life “wellness.” 2:55 PM - Refreshment Break3:35 PM 3:35 PM - Paper Session I4:45 PM Program HighlightsModerators: Stephen A. Kottmeier, MD Gerard Slobogean, MD, MPH3:35 PM - PAPER 603:41 PM A Randomized Controlled Trial Comparing Operative and Nonoperative Treatment of Humeral Diaphyseal Fractures Stephane Bergeron, MD; Prism Schneider, MD; Allan Liew, MD; Hans J. Kreder, MD, MPH; Gregory Berry, MD3:41 PM - PAPER 613:47 PM Is the Use of Bipolar Hemiarthroplasty Over Monopolar Hemiarthroplasty Justied?APropensityScore-Weighted Analysis of a Multicenter Randomized Controlled Trial Marianne Comeau-Gauthier, MD; SoaBzovsky,MSc; Mohit Bhandari, MD, PhD; Daniel Axelrod, MD; Rudolf W. Poolman, MD, PhD; Frede Frihagen, MD, PhD; Sheila Sprague, PhD; Emil H. Schemitsch, MD; HEALTHInvestigators
Register Today at ota.org 7Thursday, October 21, continued 3:47 PM - PAPER 623:53 PM A Prospective Randomized Controlled Trial Comparing Subcutaneous Enoxaparin & Oral Rivaroxaban for Venous Thromboembolism Prophylaxis in Orthopaedic Trauma Patients Mitchell P. John, MD; Benjamin D. Streufert, MD; Hassan R. Mir, MD, MBA; KatheryneDownes,PhD3:53 PM Discussion3:58 PM - PAPER 634:04 PM Intraoperative Hematoma Block Decreases Postoperative Pain and Narcotic Consumption After Intramedullary Rodding of Femoral Shaft Fractures: A Randomized Control Trial Alex Yue, MD; Nihar S. Shah, MD; RobertMatar,MD;RamseyS.Sabbagh,MS; H. Claude Sagi, MD4:04 PM - PAPER 644:10 PM Periarticular Multimodal Analgesia Decreases Postoperative Pain in Tibial Plateau Fractures: A Double Blind Randomized Controlled Pilot Study Patrick Kellam, MD;GrahamJ.DeKeyser,MD; Lucas S. Marchand, MD; Thomas F. Higgins, MD; DavidL.Rothberg,MD;JustinHaller,MD4:10 PM - PAPER 654:16 PM DenitiveFlapCoverageWithin48Hours ofDenitiveFixationReducesDeep Infection Rate in Open Tibial Shaft Fractures Requiring Flap Coverage Paul Tornetta III, MD; Khalid Al-Hourani, MD; Jeff J. Foote, MD,s MSc; AndrewD.Duckworth,MBCHB,MSc,PhD; TimothyO.White,MD; MichaelKellyMBBS,MD; Michael T. Stoddart, MBBS; Justin J. Koh, MD; Stephen A. Sems, MD; M.TayseerShamaa,MBBS;DebiSorg; Hassan R. Mir, MD, MBA; Benjamin D. Streufert, MD; ClayA.Spitler,MD;BrianMullis,MD; John C. Weinlein, MD; Lisa K. Cannada, MD; EmilyWagstrom,MD;JeraldWestberg,BA; AbigailCortez,MD;PeterC.Krause,MD; Andrew J. Marcantonio, DO; Gillian Soles, MD; Jason Lipof, MD; Ross K. Leighton, MD; Michael J. Bosse, MD; Chad Coles, MD; Jowan G. Penn-Barwell, MB ChB; JosephR.Hsu,MD;AleksiReito,MD,PhD; Heather A. Vallier, MD; Saam Morshed, MD4:16 PM Discussion4:21 PM - PAPER 664:27 PM OperativeversusNon-Operative Treatment of Severely Shortened or Comminuted Clavicle Fractures in Older Adolescent Athletes: Results from a Prospective, Multicenter, Level 2 Cohort Study David D. Spence, MD; Philip L. Wilson, MD; Donald S. Bae, MD; Michael T. Busch, MD; Eric W. Edmonds, MD; HenryB.Ellis,MD; KatelynA.Hergott,MPH; Mininder S. Kocher, MD, MPH; G.YingLi,MD;ElizabethLiotta; JeffreyJ.Nepple,MD; NiravK.Pandya,MD; AndrewT.Pennock,MD; CrystalA.Perkins,MD; Coleen S. Sabatini, MD, MPH; DavidN.Williams,PhD; Samuel C. Willimon, MD; BentonE.Heyworth,MD4:27 PM - PAPER 674:33 PM Risk of Iatrogenic Sciatic Nerve Injury During Posterior Acetabular Fracture Fixation:DoesPatientPositionMatter? Jason Chen, MD; Ishani Sharma, BA; JoshuaEverhart,MD,MPH; RamseyS.Sabbagh,MS; NakulNarendran,BA; Michael T. Archdeacon, MD, FAAOS; H. Claude Sagi, MD; Brian Mullis, MD; Roman Natoli, MD4:33 PM - PAPER684:39 PM The Effect of Anterior Support Screw (AS2) for Unstable Femoral Trochanteric Fractures: A Multicenter Randomized Controlled Trial Takashi Maehara MD, PhD; HiroyukiSuzuki;TomohikoShimizu,MD; TakahiroHamada,MD; Masanori Yorimitsu, MD; Hidefumi Teramoto, MD, PhD; KazushiMihara,DC;TakaoMae,MD; TakashiHayakawa,MD; YasunoriOkamoto,MD;TakeshiDoi; YoshihisaAnraku,MD;JunHara,MD4:39 PM Discussion
OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, Texas8 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org Thursday, October 21, continued 4:45 PM - President’s Message 5:15 PM “The Courage to Heal: Building Resilience and Transforming Recovery” Heather A. Vallier, MD Professor of Orthopaedic Surgery Case Western Reserve University MetroHealth System – Cleveland, OhioIntroduction: Brendan M. Patterson, MD5:15 PM - OTA Business Meeting (Members Only) 6:15 PM concurrent pre-reception in Exhibit Hall 5:15 PM - Happy Hour - Exhibitor Reception 6:15 PM Sponsored by 6:20 PM - Welcome Reception 8:20 PM The Water Gardens Join your colleagues for cocktails and hors d’oeuvres at the Water Gardens.
Register Today at ota.org 9and trauma orthopaedist. Furthermore, we will highlight an increasing fracture pattern -- the interprosthetic fracture, and our view on treatment. Managing Complex Humerus Fractures: From Proximal to Distal Moderator: Andrew M. Choo, MD Faculty: Timothy S. Achor, MD Michael J. Gardner, MD Eben A. Carroll, MD Learning Objectives • Identify fracture patterns and characteristics which can pose unique difculties. • Aid with decision-making, planning, and options for complex humerus fractures. • Demonstrate surgical techniques to successfully manage these injuries. Description This breakout session will present case-based discussions on the management of difcult problems with humerus fractures. Proximal, diaphysial, and distal humerus fractures will be examined with special attention to unique fracture problems, including fracture-dislocations, ballistic injuries, segmental fractures, bone loss, and nonunions/malunions. This breakout focuses on challenging problems seen in humeral fracture management which aren’t common-ly discussed in other forums. The case-based nature allows for extensive audience partici-pation as well.Friday, October 22, 2021 6:30 AM - Concurrent Breakout Sessions 7:30 AM Pelvic and Acetabulum Fractures Moderator: Paul Tornetta III, MD Faculty: David C. Templeman, MD Reza Firoozabadi, MD Michael S. Kain, MD Andrew H. Schmidt, MD Learning Objectives • To understand indications for surgery of pelvic and acetabular fractures • To be exposed to multiple xation and reduction tactics • To understand the controversies in the management of pelvic and acetabular fractures Description This is a case-based review of controversial and complex pelvic and acetabulum fractures. It will focus on the indications for surgery as well as intra-operative reduction and xation tactics. From Fixation to Revision in Periprosthetic and Interprosthetic Hip & Knee Fractures: When, How and Getting it Right Moderator: Frank A. Liporace, MD Faculty: Richard S. Yoon, MD Derek J. Donegan, MD, MBA Mark Gage, MD Learning Objectives • Take away strategies for identifying stable versus loose implants in the periprosthetic (PPFx) THA/TKA Fracture setting. Additionally --- what do I do with an interprosthetic fracture? • Fixation strategies, tips and tricks and avoiding pitfalls for PPFx about the acetabulum, proximal and distal femur. • When and how --- revision strategies for a loose cup, loose femoral stem/compo- nent with and without good bone stock. Description This breakout session will offer a case-based, interactive strategy and update on the xa-tion and revision of periprosthetic THA/TKA fractures. Also, treatment of interprosthetic fractures will also be highlighted for partic-ipants. We all know that periprosthetic hip and knee fractures continue rise and are a clinical concern especially with its morbidity/mortality equaling those of hip fractures -- so providing tips/tricks to efcient and effec-tively treat these is essential to the everyday
10 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasFriday, October 22, continued 6:30 AM - Concurrent Breakout Sessions (cont’d) 7:30 AM The Traumatized Midfoot: Tips and Tricks for Successful Reconstruction Moderator: Harmeeth S. Uppal, MD, MS Faculty: Brad J. Yoo, MD Gregory John Della Rocca, MD, PhD, FAAOS, FACS Stephen K. Benirschke, MD Learning Objectives • The registrant will learn surgical strategies and tips for successful midfoot reconstruction. Additional discussion and case examples will be on both surgical techniques and tips for initial provisional xation as well as techniques for denitive ORIF vs primary fusion. • The registrant will learn tips for successful xation of Chopart fractures and/or dislocation injuries. • The registrant will learn surgical strategies and tips for successful midfoot reconstruction. Additional discussion and case examples will be on both surgical techniques and tips for initial provisional xation as well as techniques for denitive ORIF vs primary fusion. Description Through detailed case based discussion the registrant will further their knowledge on how to manage complex midfoot and Cho-part joint injuries. Focus will be on scrutiniz-ing xrays and discussing surgical technique that highlights tips for obtaining stable mechanical xation. Further discussion will address the proper management of com-plex midfoot injuries where initial denitive xation has failed. Complex foot injuries are commonly managed by orthopaedic trauma surgeons. These injuries if managed poorly can result in outcomes that are devastating to the patient. This symposium will address in detail the surgical techniques and tips to manage these injuries correctly the rst time. Although this symposium was done last year, judging by the large attendance and lengthy discussion with faculty during and after the course, it is apparent that many surgeons feel this topic is important and desire further understanding. We will focus solely on case presentations that highlight in depth surgical techniques and steps needed to achieve successful reconstruction of both primary and failed xation. This is a must have! Challenges in Non-union Treatment - A Case-Based Symposium Moderator: Paul S. Whiting, MD Faculty: J. Spence Reid, MD Gerald J. Lang, MD David Goodspeed, MD Learning Objectives • Understand the mechanical and biological principles of fracture healing. • Learn a systematic approach to non-union workup and pre-operative planning. • Understand treatment principles and techniques for non-unions. Description Faculty will use a case-based approach to illustrate principles and techniques of non-union treatment. Principles of fracture healing (mechanical and biological) and strategies for non-union workup and pre-op-erative planning will also be reviewed. This proposal represents a follow-up to mini-sym-posia we offered at the 2018 and 2019 OTA meetings. Based on feedback from partici-pants at the 2018 symposium, we shortened the didactic portions, leaving additional time for case presentations and discussion with attendees. This was very well received at the 2019 meeting, and we would like to offer this session again following a similar format but providing new cases to illustrate the key concepts/objectives we would like partici-pants to gain from the session.
Register Today at ota.org 119:40 AM - Paper Session II11:06 AM Foot, Ankle, Pilon & Hip and FemurModerators: Gregory Della Rocca, MD, PhD, FACS Lori Reed, MD9:40 AM - PAPER 699:46 AM Prospective Randomized Controlled Trial: EarlyWeightBearingAfterConservative TreatmentofWeberBAnkleFractures Robert C. Stassen, MD; StijnFranssen,MD;ErikDeLoos; BerryMeesters;BertBoonenDMed; Raoul Van Vugt, MD, PhD9:46 AM - PAPER 709:52 AM Does Hindfoot Nailing Decrease Unplanned Return to the OR After GeriatricOpenAnkleFracture? Richard Wawrose, MD; MitchellFourman,MD;BrendanCasey,DO; JoshuaN.Adjei,MD;GeleMoloney,MD; PeterA.Siska,MD;IvanS.Tarkin,MD9:52 AM - PAPER 719:58 AM Fractures and Macroscopic Osteochondral Injuries of the Talar Dome Associated with Pilon Fractures Kevin Tetsworth, MD; Nicholas Green, BS; GregoryBarlow,MD;MiranStubican,MD; Frode Vindenes, MD; Vaida Glatt, PhD9:58 AM - PAPER 7210:04 AM Is the Sinus Tarsi Approach Safer Than the Extended Lateral Approach for Calcaneal Fractures? Thomas M. Seaver, MD;ZacharyZeller,MD; Paul Tornetta III, MD; Andrew J. Marcantonio, DO; Alexander J. Ment, BA; Hassan R. Mir, MD, MBA; Randi Alexander, MPH; MitchellK.Messner,MD;ClayA.Spitler,MD; Erin L. Hofer, MD; Anna N. Miller, MD; Jerald Westberg, BA; Jessica M. Downes, MD; Noah Joseph, MD; Heather A. Vallier, MD; Yu Min Suh, MD; Robert F. Ostrum, MD; BenjaminOllivere,MD,MA,MBBS; AdeelIkram,MBBS,MRCS;BrianMullis,MD; Jorge Figueras, BS; Darin M. Friess, MD; Emelia Sodders, MS; NoelleL.VanRysselberghe,MD; MichaelJ.Gardner,MD;AmandaPawlak,MD; Stephen Kottmeier, MD; Saam Morshed, MD; ZacharyLim,MD;AdenMalik,MD; Lawrence H. Goodnough, MD; EliW.Bunzel,MD;RezaFiroozabadi,MD; PatrickYoon,MD10:04 AM DiscussionFriday, October 22, continued 7:30 AM - Symposium II: 9:00 AM Hot Off The Press: Latest Randomized Controlled Trials That Can Change Your Practice in 2021 Moderator: Niloofar Dehghan, MD, MSc Faculty: Tim Chesser, FRCS Robert V. O’Toole, MD Prism Schneider, MD, PhD Steven F. Shannon, MD Emil H. Schemitsch, MD Gerard Slobogean MD, MPH Learning Objectives • Latest evidence regarding best treatment strategies for ankle syndesmosis (tight- rope vs screws) as well as ail chest injuries (surgery vs non-op) • Latest evidence regarding hip fractures in elderly: is THA better than a hemi, and how long should a cephalomedullary nail be. • Latest evidence on adjuncts to fracture xation: use of vancomycin powder, vitamin D supplementation, and negative pressure wound therapy. Description The aim of this symposium is to highlight practice changing clinical trials presented/published in the last 2 years, and provide clear evidenced based recommendations, for the treatment of common fractures and orthopaedic conditions. There have been multiple recent high-quality studies present-ed and published in the eld of orthopaedic trauma. Unfortunately, many surgeons are unaware of the latest evidence and recom-mendations (weather in the community or academics). This session highlights a number of award winning and practice changing clinical trials. This session is applicable to all orthopaedic surgeons attending the OTA, as well as residents, PAs, and allied health. The topics are relevant to those working at large academic centers as well as smaller com-munity hospitals. The session has a diverse and international faculty. The speakers are experts in the topic they will be presenting, many as the principal investigator of the study discussed. Each speaker will have 7 minutes to speak, and there will be 40 minutes for discussion and audience partici-pation at the end. A similar symposium was presented several years ago which was very successful and well received by the audience. 9:00 AM - Break9:40 AM
12 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasFriday, October 22, continued 10:09 AM - PAPER 7310:15 AM Patients with Hip Fractures Treated with Arthroplasty Demonstrate Prolonged Hypercoagulability and Increased Venous Thromboembolism Risk Daniel You, MD;RobertKorley,MD; RichardE.Buckley,MD; PaulJ.Duffy,MD; RyanMartin,MD;AndreaSoo,PhD,MSc; Prism Schneider, MD, PhD10:15 AM - PAPER 7410:21 AM Who,ifAnyone,MayBenetfromaTotal Hip Arthroplasty After a Displaced FemoralNeckFracture?ASubgroup Analysis of the HEALTH Trial Frede Frihagen, MD, PhD; Marianne Comeau-Gauthier, MD; DanielAxelrod,MD;SoaBzovsky,MSc; Rudolf W. Poolman, MD, PhD; Diane Heels-Ansdell, MSc; Mohit Bhandari, MD, PhD; Sheila Sprague, PhD; Emil H. Schemitsch, MD; HEALTHInvestigators10:21 AM - PAPER 7510:27 AM Surgical Approach and Dislocation Rate Following Hemiarthroplasty in Geriatric Femoral Neck Fracture Patients with Cognitive Impairment: Is There an Association? Miles St. Parsons, MD; Brian J. Page, MD; Joshua Ho-Sung Lee, MD; Joel Dennison, MD; KendallA.PyeHammonds,MPH; KindyleL.Brennan,PhD; Michael L. Brennan, MD; Daniel L. Stahl, MD10:27 AM Discussion10:32 AM - PAPER 7610:38 AM DistalFemurFracturesOccur8Times More Frequently in Short versus Long Cephalomedulary Nails for Intertrochanteric Hip Fractures: A Longitudinal Study Patrick Curtin, MD; Laura Thurber, BA; GregoryIovanel;DanielMandell,MD; Eric F. Swart, MD10:38 AM - PAPER 7710:44 AM RiskFactorsforNon-unionofDistal Femur Fractures Ryan Cone, MD;KyleCichos,BS; YvonneE.Chodaba,MD; AlexanderRoszman,MD; Gerald McGwin, MS, PhD; ClayA.Spitler,MD10:44 AM Discussion10:49 AM - PAPER7810:55 AM Midterm Outcomes After the Surgical Treatment of Atypical Femoral Fractures -Minimum3YearFollowup Kyu-Tae Hwang, PhD; Soo-Young Jeong, MD; Chang-Wug Oh, MD; Joon-Woo Kim, MD, PhD; Oog Jin Shon, MD, PhD; Ji Wan Kim, MD; YounghoCho,MD;KiChulPark10:55 AM - PAPER 7911:01 AM Risk Factors for Early Conversion Total Hip Arthroplasty after Pipkin 4 Femoral Head Fracture KyleCichos,BS;PatrickF.Bergin,MD; ParkerA.White,MD;ElieS.Ghanem,MD; Clay A. Spitler, MD; Gerald McGwin, MS, PhD11:01 AM Discussion
Register Today at ota.org 13 • When and how – strategies for addressing supracondylar nonunions in both the aseptic and infected settings. Description This breakout session will offer a case-based, interactive strategy and update on treatment techniques for supracondylar distal femur fractures with and without articular involve-ment. Treatment of supracondylar nonunions will be also be highlighted for participants. Despite signicant advances in orthopae-dic trauma, the ideal xation strategy and implant construct for supracondylar distal femur fractures remains unknown. There remains a relatively high nonunion rate and a signicant complication prole, specically in the geriatric population. This breakout session provides tips/tricks to efciently and effectively treat these injuries essential to all orthopaedic surgeons. Diversity and Inclusion in Orthopaedic Trauma Moderator: Joseph R. Hsu, MD Faculty: Anna N. Miller, MD Hassan R. Mir, MD, MBA Paul B. Gladden, MD Heather A. Vallier, MD Learning Objectives • Dene the problem of lack of diversity among orthopaedic trauma surgeons. • Discuss impact of improving diversity in the subspecialty on surgeons as well as patients. • Identify practical solutions to execute this in own practice. Description Orthopaedic surgery has lagged behind other medical specialties in the recruitment and promotion of underrepresented minori-ties to include women; orthopaedic trauma has done even worse than many Orthopae-dic Subspecialties in recruiting and promot-ing diverse surgeons. Data suggests that increased diversity in physicians decreases disparities in care. This panel will dene the problem, describe opportunities to improve both quality of care for patients and for surgeons and other team members, and provide practical and actionable solutions to execute this in our own divisions, depart-ments, and specialty. As a specialty, Ortho-paedic Surgery has a diversity problem and that problem is even worse in orthopaedic trauma. It is critical to have open and honest discussion about the impact on surgeons as well as patient care, as well as to discuss ways to improve diversity among orthopaedic trauma surgeons.Friday, October 22, continued 10:00 AM - Concurrent Breakout Sessions11:00 AM Navigating Work and Life Stressors as an Orthopaedic Traumatologist Moderator: Matthew R. Garner, MD Faculty: Derek J. Donegan, MD, MBA Milton L. Routt, MD Milton T. M. Little, MD Jonah Hebert-Davies, MD Learning Objectives • An improved understanding of stressors and challenges that Orthopaedic Trauma surgeons face through discussion and personal experiences of faculty. • Statistics surrounding physician suicide. • Tools and resources available for those experiencing stress, loss, or mental challenges. Description This session will focus discussing stressors that occur in a provider’s life, both at work and at home. The faculty will use personal experiences to promote an open discussion of these stressors in hopes of starting a pro-cess of destigmatization. Participants will be encouraged to continue these conversations at their home institution with the goal of improving communication around topics that are often avoided. Provider mental health is routinely overlooked, a fact that has become more apparent with the recent, unexpected loss of colleagues. It is important that OTA members understand that their struggles are rarely unique and that many of us share sim-ilar experiences. Further, it is essential that we promote discussion and awareness of these stressors while avoiding internalization. Treatment of Supracondylar Femur Fractures: Plating, Nailing and Nonunions Moderator: Frank A. Liporace, MD Faculty: Michael A. Maceroli, MD Richard S. Yoon, MD John P. Ketz, MD Marcus F. Sciadini, MD Learning Objectives • Provide operative tips and techniques for treating supracondylar distal femur fractures with both locked plating and intramedullary strategies. • Focus on the geriatric supracondylar femur fracture and the advent of the nail-plate combination technique to allow early weight-bearing and prevent complications.
14 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasFriday, October 22, continued 10:00 AM - Concurrent Breakout Sessions (cont’d) 11:00 AM Bringing Your Idea to Market- The Innovation Dream Moderator: Edward J. Harvey, MD Faculty: Charles Allan Thomas A. Russell, MD Ross K. Leighton, MD Dominique Rouleau, MD Learning Objectives • Learn how to get research translated to a commercial product • Recognize the advantages of corporate partnership to with get an idea noticed or facilitate research goals • Experience some of the pearls and pitfalls other people have been through on their entrepreneurial journeys Description We will outline how new ideas can either be incorporated into your research or clini-cal streams as well as identifying what is a commercial possibility and how to fund it. Almost every surgeon has had a good idea that they thought would be a great product. Our panel has journeyed down the road of development and even commercialization and can bring that knowledge to the viewer. 11:06 AM - John Border Lecture 11:51 AM “Living with No Excuses” Noah Galloway Noah is a military veteran who served in Iraq and was severely injured in combat. Through personal transfor-mation, he shares his struggles and triumphs to help motivate and inspire others to live their best life.11:51 AM - Immediate Past 12:21 PM President’s Message “Orthopaedics in 2021: A View from Both Sides of the 49th Parallel” Michael D. McKee, MD Professor and Chairman, Department of Orthopaedic SurgeryUniversity of Arizona College of Medicine–Phoenix BannerUniversity Medical Center PhoenixIntroduction: Emil H. Schemitsch, MD12:21 PM - Lunch in Exhibit Hall1:21 PM New Member Luncheon Kathy Cramer Women in Trauma Luncheon12:34 PM - Lunch Poster & Video Tours1:14 PM Knee/Tibia – Robert V. O’Toole, MD General Interest – Conor P. Kleweno, MD Video Tours – James A. Blair, Jr., MD
Register Today at ota.org 15Friday, October 22, continued 1:21 PM - Paper Session III2:30 PM Geriatric Fractures and PedsModerators: Edward J. Harvey, MD Dominique Rouleau, MD1:21 PM - PAPER801:27 PM Hip Fracture with Elevated Troponin: Harbinger of Mortality or Need for AcceleratedSurgery? JocelynWu,BA;NathanN.O’Hara,MHA; NicholasRolle;FlaviaK.Borges,PhD; P.J.Devereaux,MD; Gerard Slobogean MD, MPH1:27 PM - PAPER811:33 PM Risk of Conversion to Total Hip Arthroplasty Following Hemiarthroplasty for Hip Fracture Kanu M. Okike MD, MPH; KathrynE.Royse,MPH,MSPH,PhD; DavidW.Zeltser,MD; GurpreetSingh,MD;LizPaxton,PhD,MA1:33 PM - PAPER821:39 PM Persistent Opioid Usage Following Hip FractureSurgeryinOpioid-Naive Older Patients Kanu M. Okike, MD, MPH; Richard N. Chang, MPH; Priscilla H. Chan, MS; LizPaxton,PhD,MA; Heather A. Prentice, PhD1:39 PM Discussion1:44 PM - PAPER831:50 PM The Results: NIHR Feasibility RCT: Acetabular Fractures in Older Patients Intervention Trial (AceFIT: ISRCTN16739011) Andrew D. Carrothers, MD; Joseph Alsousou, MD; Daud Chou, MBBS, MSc; JaikirtyRawal,MA,MBBS; JosephM.Queally,MD; Peter Hull, MBCHB1:50 PM - PAPER841:56 PM Outcomes for Geriatric Proximal Humerus Fractures: A Matched Comparison of Nonoperative Management and Reverse Shoulder Arthroplasty StevenSamborski,MD;Brittany Haws, MD; StevenKarnyski,MD;KyleT.Judd,MD; CatherineA.Humphrey,MD,MBA; GillianSoles,MD;JohnT.Gorczyca,MD; IlyaVoloshin,MD;GreggT.Nicandri,MD; JohnP.Ketz,MD1:56 PM - PAPER852:02 PM Intravenous Tranexamic Acid Given at Femoral Fragility Fracture Surgery Reduces Blood Transfusion Requirements Four-fold Matilda Powell-Bowns, MBCHB, MEd, MRCS; RhysK.Olley,MBCHB; Conor McCann, MBCHB; James R. Balfour; Caitlin M. Brennan MBCHB, MRCS; Jasmine Peh, MBCHB; AndrewD.Duckworth,MBCHB,MSc,PhD; Chloe Scott, FRCS2:02 PM Discussion2:07 PM - PAPER862:13 PM Long-legversusShort-legCast Immobilization for Displaced Distal Tibial Physeal Fractures Christopher D. Souder, MD; James Spearman, MD; Lori A. Thornton, MS, RN, FNP-C; Jessica Treiber, MPH, PA-C; AinsleyK.Bloomer,BA,BS; Brian P. Scannell, MD; Christine A. Ho, MD2:13 PM - PAPER872:19 PM Non-OperativeversusOperative TreatmentofZ-TypeComminutedClavicle Fractures in Adolescents: A Prospective Sub-StratiedCohortAnalysis Coleen S. Sabatini, MD, MPH; Eric W. Edmonds, MD; ElizabethS.Liotta,MBBS; KatelynA.Hergott,MPH; Donald S. Bae, MD; Michael T. Busch, MD; HenryB.Ellis,MD; Mininder S. Kocher, MD, MPH; G.YingLi,MD;JeffreyJ.Nepple,MD; NiravK.Pandya,MD;AndrewT.Pennock,MD; CrystalA.Perkins,MD; DavidD.Spence,MD; DavidN.Williams,PhD; Samuel C. Willimon, MD; Philip L. Wilson, MD; BentonE.Heyworth,MD
16 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasFriday, October 22, continued 2:19 PM - PAPER882:25 PM Changes in Superior Displacement, Angulation, and Shortening in the Early Phase of Healing for Completely Displaced Midshaft Clavicle Fractures in Adolescents: Results from a Prospective, Multicenter Study AndrewT.Pennock,MD; Benton E. Heyworth, MD; TraceyBastrom,MA;DonaldS.Bae,MD; Michael T. Busch, MD; Eric W. Edmonds, MD; HenryB.Ellis,MD; Mininder S. Kocher, MD, MPH; G.YingLi,MD;ElizabethLiotta; NiravK.Pandya,MD; CrystalA.Perkins,MD; Coleen S. Sabatini, MD, MPH; DavidD.Spence,MD; Samuel C. Willimon, MD; DavidN.Williams,PhD; PhilipL.Wilson,MD;JeffreyJ.Nepple,MD2:25 PM - Discussion2:30 PM 1:50 PM - Concurrent Breakout Sessions 2:50 PM Current Strategies and Techniques for Operative Fixation of Complex Ankle Fractures and Fractures of the Tibial Plafond Moderator: Frank A. Liporace, MD Faculty: Richard S. Yoon, MD Mark Gage, MD Marcus F. Sciadini, MD Jason W. Nascone, MD Learning Objectives • Getting the diagnosis right --- don’t miss a higher level injury, not every ankle fracture is a bi- or trimalleolar ankle fracture! • Deciding, how and when, to use approaches (anterior/posterior) and current update on the latest xation strategies (i.e.minifragment, intramedullary nails for bula/tibia) • Salvage (fusions, frames, amputations) --- when to say enough is enough! Description The goal of this breakout session is to provide operative management strategies to avoid complications and achieve desired outcomes. Presentations will be case-based and include everything from the simple to complex fractures. Strategies will focus on the latest decision-making and xation op-tions to maximize outcomes. Higher energy ankle/pilon fractures still offer a challenging clinical scenario to the orthopaedic trauma-tologist/general orthopaedist. Minimizing complications are based on appropriate planning and xation execution --- this case-based breakout will provide the necessary education in this important trauma topic essential to OTA attendees.
Register Today at ota.org 17Friday, October 22, continued 1:50 PM - Concurrent Breakout Sessions (cont’d) 2:50 PM High Energy Proximal Femur Fractures: Avoiding Mistakes to Optimize Success Moderator: Marschall B. Berkes, MD Faculty: Timothy S. Achor, MD Christopher McAndrew, MD Milton T.M. Little, MD Learning Objectives • Understand pearls and pitfalls of intramedullary nailing of proximal femur femur fractures • Appreciate ideal indications for plate xation of proximal femur fractures • Recognize surgical tactics to treat femoral neck fractures and possible associated postoperative complications Description High energy proximal femur fractures can be challenging injuries to manage. This break-out session will utilize case presentations to demonstrate common intra-operative pitfalls and errors that frequently lead to postop-erative failure. Techniques and indications will be demonstrated to optomize success though the use of intramedullary nails, plate xation and femoral neck xation. Surgically managed high energy proximal femur fractures are plagued by high rates of postoperative malalignment and associated nonunion. This breakout session will seek to clarify proper indications for plate and nail xation and demonstrate specic reproduc-ible intraoperative techniques for success-ful application of these devices. Technical pearls for femoral neck xation will also be discussed. State of the Art for Operative Management of Femoral Head Fractures Moderator: Brett D. Crist, MD Faculty: Kyle Schweser, MD John C. Hagedorn, MD Learning Objectives • List the indications for ORIF versus excision of femoral head fractures. • Recognize the indications and benets for the anterior surgical approach versus surgical hip dislocation for femoral head fracture ORIF and addressing associated injuries. • List technical tricks and reconstructive options for femoral head fractures. Description Femoral head fractures are rare. Understand-ing surgical exposure options and tech-niques for ORIF and addressing associated injuries. Learn technical tricks and recon-structive options including cartilage trans-plant techniques. Femoral head fractures are rare and often not discussed frequently. Recognizing the associated injuries and how to address them may be the difference in preserving the patient’s hip. Understanding the reconstructive options for patients are also important. Olecranon and Proximal Ulna Fractures and Fracture-Dislocations: Not So Easy! Moderator: Utku Kandemir, MD Faculty: Milan K. Sen, MD Bertrand Perey Michael D. McKee, MD Learning Objectives • Recognize of injury patterns of olecranon and proximal ulna fractures • Understand treatment options and indications for each injury pattern • Learn how to avoid problems and pitfalls Description Injuries of olecranon and proximal ulna include a wide spectrum of injuries. Detailed understanding of injury patterns and pit-falls in management of critical to minimize problems and complications. There is a knowledge gap of understanding the injuries of olecranon and proximal ulna that leads to inadequate initial management and not uncommonly results in less than optimal results.2:30 PM - Paper Session IV3:27 PM Pelvis and AcetabulumModerators: Kelly A. Lefaivre, MD Peter Bates, MD2:30 PM - PAPER892:36 PM Is External Beam Radiation Therapy Really Associated with Low Rates of Heterotopic OssicationAfterAcetabularSurgery? Adam Boissonneault, MD; Gerard Slobogean, MD, MPH; ElizabethHarkin,MD; JayeshGupta,BS;NathanN.O’Hara,MHA; RobertV.O’Toole,MD
18 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasFriday, October 22, continued 2:36 PM - PAPER 902:42 PM Delayed Fixation of Acetabular Fractures inPolytraumaPatientsWithandWithout Concomitant Lower Extremity Fractures SignicantlyIncreasestheOddsof Complications Lauren Nowak, PhD, MSc; DavidSanders,MD; Abdel-RahmanLawendy,FRCS; Christopher Del Balso, MSc, MBBS; Emil H. Schemitsch, MD2:42 PM - PAPER 912:48 PM Administration of Venous Thromboembolism Chemoprophylaxis Within12HoursofPelvicandAcetabular Surgery Has No Effect on Estimated Blood Loss, Perioperative Change in Hemoglobin, or Need for Transfusion Lukas Keil, MD; Sean A. Flannigan, BS; Robert F. Ostrum, MD; Jesse C. Hahn, MD2:48 PM Discussion2:53 PM - PAPER 922:59 PM Results of Emergency Department Stress of Lateral Compression Type 1 Fracture Correlate with Validated Instability Scoring System Graham J. Dekeyser;PatrickKellam,MD; Thomas F. Higgins, MD; Justin Haller, MD; Lucas S. Marchand, MD; DavidL.Rothberg,MD2:59 PM - PAPER 933:05 PM Contralateral Lateral Stress Radiographs (LSR) to Evaluate Stability of Minimally Displaced Lateral Compression Type 1 Pelvic Ring Injuries Are Equivalent to Ipsilateral LSR Joshua A. Parry, MD; Michael M. Hadeed, MD; AustinHeare,MD;StephenStacey,MD; CyrilMauffrey,MD,MRCS3:05 PM Discussion3:10 PM - PAPER 943:16 PM Percutaneous Posterior Pelvic Stabilization for Spinopelvic Dissociation: A20-YearSeriesofDisplacedand Nondisplaced Fracture Patterns Justin P. Moo Young, MD; JonathanSavakus,MD;DanielE.Pereira,BA; JeffreyHills,MD; ByronF.Stephens,MD; Phillip Mitchell, MD3:16 PM - PAPER 953:22 PM A Comparison of Open versus Percutaneous Approaches to Spinopelvic Dissociation: Presentation, Complications and Outcome Justin P. Moo Young, MD; JonathanSavakus,MD;DanielE.Pereira,BA; JeffreyHills,MD; ByronF.Stephens,MD; Phillip Mitchell, MD3:22 PM Discussion3:27 PM - Break3:57 PM
Friday, October 22, continued 3:57 PM - Paper Session V5:23 PM General Interest and Post-Traumatic General InterestModerators: Andrew M. Choo, MD Stephen Warner, MD, PhD3:57 PM - PAPER 964:03 PM Agricultural Trauma causing Open Fractures: Is Antibiotic Coverage Against AnaerobicOrganismsIndicated? Malynda Wynn, MD;KyleK.Kesler,MD; Michael J. Robertson, MD; Robert T. Higginbotham, BA; John Morellato, MBBS; J. Lawrence Marsh, MD; Matthew Hogue, MD4:03 PM - PAPER 974:09 PM Does Cumulative Topical Antibiotic Powder Use Increase the Risk of Nephrotoxicity? Robert V. O’Toole, MD; NathanN.O’Hara,MHA;JessicaCarullo,BS; Manjari Joshi; Sheila Sprague, PhD; Gerard Slobogean, MD, MPH4:09 PM - PAPER984:15 PM WhatIsMostImportanttoPatientsWhen Pursuing Limb Salvage Following a Limb-ThreateningInjury? Alison L. Wong MD, MS; CynthiaShannon,BS,BSN; AbdulaiBangura,BS;LilyMundy,MD; NathanN.O’Hara,MHA; RaymondA.Pensy,MD4:15 PM Discussion4:20 PM - PAPER 994:26 PM Effects of the Trauma Collaborative Care Intervention: 12 Month Results from a Prospective Multicenter Cluster Clinical Trial Stephen Wegener, PhD; TCCS METRC Investigators4:26 PM - PAPER 1004:32 PM OrthopaedicSurgeryI-PASSIntervention Leads to Sustained Improvement in Quality of Patient Handoffs Derek S. Stenquist, MD; Caleb Yeung, MD; Laura Rossi, PhD, RN; Antonia F. Chen, MD, MBA; Mitchel B. Harris, MD4:32 PM - PAPER 1014:38 PM How Many Sites Should an Orthopaedic Trauma Prospective Multicenter Trial Have?AMarginalAnalysisofCompleted Trials Lauren Allen, MA;RobertV.O’Toole,MD; Michael J. Bosse, MD; WilliamT.Obremskey,MD,MPH; Kristin Archer, PhD; Lisa K. Cannada, MD; Jaimie T. Shores, MD; Renan C. Castillo, MD; METRCInvestigators4:38 PM Discussion4:43 PM - PAPER 1024:49 PM Transfusion After Harvesting Bone Graft with RIA: Practice Changes Reduced Transfusion Rate by More than Half Lucas S. Marchand, MD; PatrickKellam,MD; GrahamJ.DeKeyser,MD;JustinHaller,MD; DavidL.Rothberg,MD; Thomas F. Higgins, MD4:49 PM - PAPER 1034:55 PM Primary Closure of External Fixator Pin Sites Does not Increase the Incidence of Surgical Site Infection JefferyShroff,MD;StevenKarnyski,MD; BrittanyHaws,MD;James D. Brodell, BA; SandeepSoin,MD;KyleT.Judd,MD; Gillian Soles, MD; CatherineA.Humphrey,MD,MBA; JohnT.GorczycaMD;JohnP.Ketz,MD4:55 PM - PAPER 1045:01 PM Intimate Partner Violence During Recovery from an Orthopaedic Injury: An Observational Cohort Study Kim Madden, PhD; Sheila Sprague, PhD; Brad Petrisor, MD; Prism Schneider, MD, PhD; Ydo Kleinlugtenbelt, MD, PhD; ElisaA.M.Hackenberg,MD; MariaVillar,MD,PhD;JeremyHall,MD,MEd; SoaBzovsky,MSc;LehanaThabane,PhD; Mohit Bhandari, MD, PhD; PRAISE-2Investigators5:01 PM Discussion5:06 PM - PAPER 1055:12 PM EfcacyofaMultimodalAnalgesic Protocol at Reducing Opioid Use After Orthopaedic Trauma Brooke Herndon, PharmD; EmilySlade,PhD;SvetlaSlavova,PhD; FeitongLei,MPH;ZhengyanHuang,PhD; Shannon Johnson, BSN, RN; PaulE.Matuszewski,MD; Eric S. Moghadamian, MD; DouglasOyler,PharmDRegister Today at ota.org 19
20 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasFriday, October 22, continued 5:12 PM - PAPER 1065:18 PM EarlyPainSelf-EfcacyPredictsChronic PainandPain-RelatedDisability24 Months After Lower Extremity Fracture Josh Van Wyngaarden, DPT, PT; Brian Noehren, PT, PhD; Kristin Archer, PhD; LucyC.Bowers,BS; PaulE.Matuszewski,MD5:18 PM Discussion5:23 PM 5:30 PM - Suds N’ Science Poster & Video Tours6:10 PM Hip/Femur – Kyle J. Jeray, MD Foot & Ankle – Anna N. Miller, MD Video Tours – Joseph Hoegler, MDSaturday, October 23, 2021 6:30 AM - Concurrent Breakout Sessions7:30 AM Gray Zone Pelvis’: What Do I Do? Moderator: Jason W. Nascone, MD Faculty: Milton L. Routt, MD Adam J. Starr, MD Robert V. O’Toole, MD H. Claude Sagi, MD Learning Objectives • The learner will understand the denition of “Gray Zone” pelvic ring injury and potential concerns that may lead to operative intervention • The learner will understand and become familiarized with the components that various experienced pelvic surgeons use in making the decision between operative and non-operative management • The learner will understand the drivers of poor outcome with pelvic ring disruption and the treating surgeon’s impact on these drivers. Description Case based panel discussion centered on decision making in pelvic ring management. Cases will present diagnostic challenges with regard to operative VS non operative management. Emphasis will be on how and why ‘pelvic experts’ decide on a treatment modality, when is non operative manage-ment appropriate and components of this decision making. Many questions are unanswered with regard to which patients benet from operative intervention of pelvic fractures; in particular those with minimal displacement. Much of the current litera-ture relies on expert opinion although more and more literature is showing acceptible outcomes with non operative management. This session will aim to provide an in depth discussions to how various ‘experts’ make the decision and what factors come into play when deciding operative VS non operative management.
Register Today at ota.org 21 Shoulder Girdle Injuries: Optimizing Decision Making and Surgical Management Moderator: Emil H. Schemitsch, MD Faculty: Michael D. McKee, MD Niloofar Dehghan, MD, MSc Jeremy Hall, MD, MEd Aaron Nauth, MD Peter A. Cole, MD Learning Objectives • How to determine which clavicle fractures and shoulder girdle injuries need surgery • How to optimize xation of shoulder girdle injuries when surgery is indicated • How to manage complications following shoulder girdle surgery Description A primary goal of the symposium will be to achieve consensus opinions on many current issues and controversies regarding the treat-ment of shoulder girdle injuries. The sym-posium will allow registrants to determine which injuries need surgery, optimize xation when surgery is indicated and manage com-plications. There is increasing interest in the management of shoulder girdle injuries. The controversy around indications for operative intervention remains higher than that seen with other fractures and there remains sig-nicant room for improvement in the care of these injuries. Lower Extremity Deformity--How to Evaluate, When to Plate, When to Nail, When to Frame, and When to Give Up Moderator: Brett D. Crist, MD Faculty: Mitchell Bernstein, MD Mark A. Lee, MD Mauricio Kfuri, MD, PhD Rahul Vaidya, MD Learning Objectives • Correctly evaluate lower extremity deformity clinically and radiographically. • Choose the appropriate technique for the location of the deformity through preoperative planning and patient evaluation. • Utilize the appropriate techniques for deformity correction. Description Lower extremity deformity evaluation is important to understand for orthopaedic surgeons managing fractures and for pa-tients seeking arthroplasty--we all see these patients. Choosing the technique that will lead to the most successful outcome is Saturday, October 23, continued 6:30 AM - Concurrent Breakout Sessions (cont’d) 7:30 AM Displaced Intra-Articular Calcaneus Fracture Management from “Soup to Nuts”: When, How, and Getting it Right Moderator: John P. Ketz, MD Faculty: Michael A. Maceroli, MD Roy W. Sanders, MD Mark Gage, MD Learning Objectives • Present a detailed review of surgical technique for both the sinus tarsi and extensile lateral approaches. • Provide an easily reproducible method for deciding the best surgical approach based on timing, patient and fracture characteristics. • Special focus on open, intra-articular calcaneus fractures from soft tissue management and initial xation to denitive surgery. Description Displaced intra-articular calcaneus fractures remain difcult to effectively treat and tend to spur intense debate regarding timing and approaches. The goal of this breakout ses-sion is to provide an overview of calcaneus fracture management, focusing specically on the key techniques that will maximize outcomes. Talks will be case-based and will highlight specic factors that will demystify decisions related to the best surgical ap-proach. Displaced intra-articular calcaneus fractures are complex problems with a very limited margin for error in both technique and decision-making. Errors in management of these fractures can result in signicant dis-ability. Current controversy exists between the sinus tarsi or extensile lateral approach and is a hot topic of debate. The goal of this breakout session is to establish which frac-tures may benet from one approach versus another as well as presenting technical tricks on reduction and xation with a goal of improving outcomes. Treatment strategies for dealing with open fractures will also be discussed as well as having a case based audience participation.
22 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasSaturday, October 23, continued 6:30 AM - Concurrent Breakout Sessions (cont’d) 7:30 AM challenging. Participants will learn how to evaluate and choose the techniques that will most likely lead to success. Thorough deformity evaluation is often underutilized in orthopaedic trauma. We all see patients with nonunions/malunions/bone loss/leg length discrepancy that present for acute fracture management, delayed management, or in preparation for arthroplasty. We will give the participants the knowledge and tools to cor-rectly evaluate and manage these patients. Dying Controversies in Orthopaedic Trauma… Or Are They? Moderator: Milton T.M. Little, MD Faculty: Marschall B. Berkes, MD Carol Lin, MD, MA Geoffrey Marecek, MD John A. Scolaro, MD Learning Objectives • Discuss literature surrounding paradigm shifts in controversial orthopaedic treatment strategies. • Appreciate the evolution of surgical approaches, techniques, treatment strategies and their impact on outcomes. • Recognize the risks and benets associated with these changing treatment strategies. Description The evolution of orthopaedic trauma is de-pendent on evaluating scientic evidence, rening surgical techniques, and working to improve patient outcomes. While this has led to many advancements in patient care, some historical non-operative treatment techniques have persisted despite their mid-dling success. This breakout examines some fractures commonly treated non-operatively and discusses the shortcomings of non-op-erative treatment and the paradigm shift of the management of these injuries. The breakout will provide a forum to discuss evi-dence to challenge persisting historical sup-port for non-operative treatment of common orthopaedic injuries. Non-operative treat-ment of humeral shaft fractures continues to be touted as the gold standard despite non-union rates that range as high as 17-20%. Non-operative treatment of extra-articular scapula fractures continues despite advanc-es in surgical techniques which can limit approach morbidity and pain associated with malunions. Flail chest continues to lead to prolonged intubation in polytraumatized patients despite growing familiarity with rib plating techniques. Fixation of associated bula fractures with plafond fractures may provide indirect plafond reduction and increased lateral column stability, but the bula is still ignored by many surgeons. Lastly, despite evidence posterior malleolus xation improves syndesmotic reduction and stability, the size of the posterior malleolus is often considered the most determining factor posterior malleolus xation.7:30 AM - Symposium III: 9:00 AM How Can We Fix Racial, Ethnic, and Socioeconomic Healthcare Disparities in Orthopaedics and Do these Disparities Exist in Orthopaedic Trauma? An Introduction and Review from the OTA Diversity Committee Moderator: Gilbert R. Ortega MD, MPH Faculty: Toni M. McLaurin, MD Nirmal C. Tejwani, MD Emily S. Benson, MD Lisa K. Cannada, MD Milton T.M. Little, MD Learning Objectives • Dene the problem of racial, ethnic, and socioeconomic healthcare disparities in orthopaedics and orthopaedic trauma • Review the goals, mission, and community projects of the OTA Diversity committee • Discuss effective solutions for orthopaedic trauma surgeons, healthcare systems, and communities regarding healthcare disparities
Register Today at ota.org 23Saturday, October 23, continued 7:30 AM - Symposium III: (cont’d) 9:00 AM Description Several studies have demonstrated racial, ethnic, and socioeconomic disparities in healthcare and orthopaedics. Despite evi-dence to show disparities in orthopaedics, 91% of surveyed orthopaedic surgeons do not believe that differences in race/ethnicity can adversely affect orthopaedic care1. The OTA’s Diversity committee was created in 2020 with several goals to help improve diversity within the OTA while address-ing ways to improve disparities within our orthopaedic trauma patient population and communities. The OTA diversity committee will dene the problems, discuss effective solutions, and offer insight on how ortho-paedic trauma surgeons can play a role in solving these healthcare disparities. When healthcare disparities exist and such a large percentage of orthopaedic surgeons do not recognize or acknowledge how disparities can adversely affect orthopaedic care, patients and communities suffer. The OTA diversity committee plans to not only review and discuss the issues, but also, offer solutions that will help orthopaedic trauma surgeons, healthcare systems, and communi-ties. 1Adelani MA, O’Connor MI. Perspectives of orthopedic surgeons on racial/ethnic disparities in care. J Racial Ethn Health Disparities. 2017;4(4):758-62. 9:00 AM - Break9:30 AM9:30 AM - Paper Session VI10:39 AM Tibia/Knee and Tibial PlateauModerators: Brett D. Crist, MD Animesh Agarwal, MD9:30 AM - PAPER 1079:36 AM Outcomes of Intramedullary Nailing Versus External Fixation in the Treatment of Open Tibial Fractures: Three to Five YearFollow-upStudyofaRandomized Clinical Trial Abigail Cortez, MD;MayurUrva,BS; BillyT.Haonga,MD; ClaireDonnelley,BS; ErickaVonKaeppler,BS; HeatherRoberts,MD;DavidShearer,MD; Saam Morshed, MD9:36 AM - PAPER1089:42 AM Gentamicin-coatedNailisEffective Fracture-relatedInfectionProphylaxisin Open Tibial Fractures Alvaro Zamorano, MD; Pierluca Zecchetto; Carlos Felipe Albarrán, MD; AndrésSebastiánAlbertoOyarzúnMartínez,MD; Luis Bahamonde, MD9:42 AM - PAPER 1099:48 AM HowLongCanDebridementWaitinType IIIBOpenTibiaFractures? Jeff J. Foote, MD, MSc; Paul Tornetta III, MD; Khalid Al-Hourani, MD; AleksiReito,MD,PhD;MichaelJ.Bosse,MD; Ross K. Leighton, MD; Chad Coles, MD; Jamal Al-Asiri, MD; DavidJ.Stockton,MD,MSc; XavierL.Grifn,MBBS,MSc; Stephen A. Sems MD; Heather A. Vallier, MD; HassanRiazMir,MD,MBA; ClayA.Spitler,MD;BrianMullis,MD; LisaK.Cannada,MD;EmilyWagstrom,MD; Jerald Westberg, BA; Saam Morshed, MD; Peter C. Krause, MD; Andrew J. Marcantonio, DO; Gillian Soles, MD9:48 AM Discussion9:53 AM - PAPER 1109:59 AM Pace of Recovery of Physical Function After Tibial Plateau Fractures Patrick Kellam, MD; GrahamJ.DeKeyser,MD; Thomas F. Higgins, MD; DavidL.Rothberg,MD; Justin Haller, MD; Lucas S. Marchand, MD
24 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasSaturday, October 23, continued 9:59 AM - PAPER 11110:05 AM An International Comparison of Acute Versus Staged Fixation of Bicondylar Tibial Plateau Fractures Lazaro Mesa, MD; NicholasBirkett,MBCHB,MSc; Reuben C. Lufrano, MD; Rutba Chatta; Melihah Hassan; Paul J. Hannon; JoshuaMizels,BA;DavidEnsor,MBBS; DavidT.Watson,MD;Anjan R. Shah, MD; Benjamin Maxson, DO; AnthonyF.Infante,DO;DavidDonohue,MD; PeterBates,MBBS;KatheryneDownes,PhD; Pramod Achan, MB, FRCS; RoyW.Sanders,MD,FAAOS; IshvinderS.Grewal,MBBS,BSc; Hassan R. Mir, MD, MBA10:05 AM - PAPER 11210:11 AM PreppingintheEx-xtoFacilitateStaged ORIF of Bicondylar Tibial Plateau Fractures Does Not Increase Infection Rates Derek S. Stenquist, MD; Caleb Yeung, MD; Theodore Guild, MD; MichaelJ.Weaver,MD; Mitchel B. Harris, MD; ArvindG.VonKeudell,MD10:11 AM Discussion10:16 AM - PAPER 11310:22 AM Rates of Early Revision Surgery in OperativelyTreatedPatellaFractures- ARetrospectiveReviewof286Cases Rohit Gopinath, BS; Jonathan Howatt, MD; Allan Liew, MD; Geoffrey P. Wilkin, MD10:22 AM - PAPER 11410:28 AM Fasciotomies in Bicondylar Tibial Plateau Fractures Do Not Have Increased Rates ofInfectionorNon-Union Kyla Huebner, MD, MSc, PhD; DerekS.Stenquist,MD; MichaelJ.Weaver,MD; ArvindG.VonKeudell,MD10:28 AM - PAPER 11510:34 AM Tibial Plateau Fractures in the Elderly Have Clinical Outcomes Similar to those inYoungerPatients Meghan Carey Derken, BA; CodyR.Perskin,BA;PhilippLeucht,MD; SanjitR.Konda,MD;AbhishekGanta,MD; Kenneth A. Egol, MD10:34 AM - Discussion10:39 AM 10:15 AM - Concurrent Breakout Sessions11:15 AM The Treatment of Peri-prosthetic Fractures in 2021: A Comprehensive Evidence-based Approach! Moderator: Emil H. Schemitsch, MD Faculty: Aaron Nauth, MD Adam A. Sassoon, MD Michael J. Gardner, MD Andrew H. Schmidt, MD Learning Objectives • How to accurately classify peri-prosthetic fractures and the common pitfalls of classication. • How to optimize the periprosthetic xation construct to allow early weight-bearing. • The role of revision arthroplasty in managing peri-prosthetic fractures about a THA and TKA. Description A primary goal of the symposium will be to achieve consensus opinions on many current issues and controversies regarding the treatment of peri-prosthetic fractures. The symposium will allow registrants to optimize surgical decision making and xation and manage complications following these difcult injuries. Peri-prosthetic fractures are increasing in frequency and complexity as the number of patients with a joint replace-ment, and their activity levels post-surgery, steadily rise. The failure rate of operative intervention remains higher than that seen with other fractures and there remains signicant room for improvement in the care of these injuries.
Register Today at ota.org 25Saturday, October 23, continued 10:15 AM - Concurrent Breakout Sessions (cont’d) 11:15 AM Combined Pelvic Ring and Acetabulum Fractures: What I’ve Learned and What I Wish I Would Have Known Back Then Moderator: Marcus F. Sciadini, MD Faculty: Michael A. Maceroli, MD Jason W. Nascone, MD Conor P. Kleweno, MD Brent T. Wise, MD Learning Objectives • Provide a comprehensive review of combined pelvic ring and acetabulum fractures from initial temporization to order of operation and denitive xation. • Discuss the different challenges faced when treating acetabular fractures complicated by both subtle and complex posterior pelvic ring injuries. • Highlight cases that helped shape the “learning curve” and how this has changed our practice. Description The goal of this breakout session is to provide treatment strategies for combined pelvic ring and acetabulum fractures. Presen-tations will be case-based and will compre-hensively review management from initial temporization to strategies for denitive reconstruction. Strategies will focus on the latest decision-making and xation options to maximize outcomes. Combined pelvic ring and acetabulum fractures are extremely difcult and rare injuries that present unique challenges. Due the their relative infrequen-cy, “ring-tabs” have not been a focus of discussion at national meetings or in peer- reviewed literature. That, combined with a steep learning curve, makes treating these injuries all the more difcult. The aim of this breakout session is to provide comprehen-sive strategies for initial management, surgi-cal planning and denitive xation through case-based lectures. Furthermore, the cases shown will highlight the key steps in those that went well and, more importantly, those that left room for improvement. Rotation, Rotation, Rotation: Why is it Important and How To Get it Right in Lower Extremity IM Nailing Moderator: James C. Krieg, MD Faculty: Patrick C. Schottel, MD Michael Blankstein, MD Mark R. Brinker, MD Ida L. Gitajn, MD Learning Objectives • The learner will understand the clinical signicance of femoral and tibial malrotation after IM nailing. • The audience will know the most common methods to intraoperatively assess femoral and tibial rotation as well as how to avoid common pitfalls. • The attendee will be able to perform the appropriate diagnostic work-up and deformity correction of rotational malunion cases. Description Diaphyseal femur and tibia fractures com-monly occur in the setting of high energy trauma. Reamed, statically locked intramed-ullary nail xation is widely accepted as the standard of care in most cases. However, high rates of malrotation have been reported resulting in unacceptable clinical outcomes. The purpose of this session is to review lower extremity diaphyseal malrota-tion following IM nailing with an emphasis on intraoperative prevention and malunion deformity correction. The incidence of femo-ral and tibial malrotation following IM nailing is unacceptably high. A review of the most accurate and reliable methods for assessing intraoperative femur and tibia rotation would benet the attendee to ensure that the most appropriate techniques are being used. Additionally, a discussion of deformity plan-ning and execution is important as the topic is not commonly discussed. This Breakout would serve as an excellent forum to review common pitfalls and how to maximize patient outcomes in regard to restoring lower extremity rotation.
#OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org 26OTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasSaturday, October 23, continued 10:15 AM - Concurrent Breakout Sessions (cont’d) 11:15 AM Tips and Tricks for Getting the Metaphysis Right With Different Implants! Moderator: Benjamin Ollivere, MD, MA Faculty: Paul Tornetta III, MD Reza Firoozabadi, MD J. Tracy Watson, MD Learning Objectives • Management strategies for complex metadiaphyseal injuries • Understand different approaches to metadiaphyseal injuries current controversies • Understand how to optimise outcomes in complex metadiaphyseal injuries Description Metaphyseal malalignment is among the most common complication in periarticular injuries. This symposium will cover the tech-nical aspects of contemporary techniques in-cluding ‘extreme nailing’, adjunctive plating, nail-plate constructs and circular frame use. Cases will be used for a discussion of the decision making for complex metaphyseal injuries. Malalignment is common in peri-articular injury (5%-25%). These problems can be caused by bad decision making or by technical issues. This session will cover the underlying decision making processes in the key areas of metadiaphyseal trauma to be discussed and understood. The case illustrated discussion session will cover tips and tricks supported by a principles based approach to complex injuries. There have been no similar sessions at the OTA for the past 4 years.10:39 AM - Paper Session VII11:42 AM Post Traumatic ReconstructionModerators: Nirmal C. Tejwani, MD Daniel N. Segina, MD10:39 AM - PAPER 11610:45 AM 10-YearIncidenceandPossiblePredictors of Conversion to TKA Following Operative Fixation of Distal Femur Fractures: Analysisof6086Patients Zachary Telgheder, MD;JasonStrelzow,MD; JenniferLewis;KatheryneDownes,PhD; HassanRiazMir,MD,MBA10:45 AM - PAPER 11710:51 AM Lower Complications in Acute THA for Intertrochanteric Femur Fractures than Delayed Conversion THA After Failed Operative Fixation Luke Myhre, MD;PatrickKellam,MD; LucasAnderson,MD;JeremyGililland,MD; Justin Haller, MD; Lucas S. Marchand, MD10:51 AM - PAPER11810:57 AM Outcomes and Survivorship of Vascularized Fibular Grafting for Post-TraumaticOsteonecrosisofthe Femoral Head Keith Whitlock, MD;EliseoDiPrinzio,MD; DanielJ.Lorenzana,MD;RachelHein,MD; Daniel J. Cunningham, MD; MarcJ.Richard,MD;MarkGage,MD; JamesR.Urbaniak,MD10:57 AM Discussion11:02 AM - PAPER 11911:08 AM Induced Membrane Technique is Effective for Both Metaphyseal and Diaphyseal Fractures with Acute Bone Loss Lillia Steffenson, MD; Stephen Wallace, MD; AlexanderRoszman,MD;ClayA.Spitler,MD; Michael Githens, MD; Justin Haller, MD
Saturday, October 23, continued 11:08 AM - PAPER 12011:14 AM Risk Factors and Characteristics of Recalcitrant Osteomyelitis Following Appropriate Initial Surgical and Antibiotic Treatment Nihar S. Shah, MD; Arun Kanhere, BS, MSc; RamseyS.Sabbagh,MS; JohnBonamer;AustinFranklin; MatthewD.Doyle; MatthewFrederickson,BS; Drew T. Sanders, MD; H. Claude Sagi, MD11:14 AM - PAPER 12111:20 AM The Effect of Free versus Local Flaps on Time to Union In Open Tibia Fractures Nicole Zelenski, MD; Jennifer Tangtiphaiboontana, MD; AnthonyJ.Archua;DogaKuruoglu,MD; MariaYan,MD;SamydS.Bustos,MD; StevenL.Moran,MD11:20 AM Discussion11:25 AM - PAPER 12211:31 AM Percutaneous Strain Reduction Screws Are a Cost Effective and Reproducible MethodtoTreatLongBoneNon-Union Matthew Bence, MA, MB; Alpesh Kothari, MD, MSc; AndrewRiddick,MBBS; WillEardley,MBCHB,MD; RobertC.Handley;AlexTrompeter11:31 AM - PAPER 12311:37 AM Orthoplastic Treatment of Open Lower Limb Fractures Improves Outcome: A12-YearReview Estelle M. D’Cunha, MBCHB; John M. McMaster, DMed, MBCHB; Jowan G. Penn-Barwell, MB, ChB; Charles A. Fries, ChB, MA, MB, MSc11:37 AM - Discussion11:42 AM 11:42 AM - Lunch12:42 PM11:57 AM - Lunch Poster & Video Tours12:37 PM Upper Extremity – Michael J. Gardner, MD International – Ida Leah Gitajn, MDRegister Today at ota.org 2712:42 PM - Symposium IV: 2:12 PM Tolerate or Re-Operate: What to Do the Day Aer? Moderator: Hans-Christoph Pape, MD Faculty: Miguel A. Triana, MD Francisco C. Rodríguez, MD, PhD Yoram A. Weil, MD Bertil Bouillon, MD, PhD Michael Verhofstad, MD, PhD Guy Putzeys, MD Learning Objectives • To understand principal criteria to evaluate the results of specic fracture treatments, arguments for and against revision surgery, and differences that may exist in different countries’ practices • To outline principles of revision surgery and likely outcomes in individual patients with specic fractures • To highlight surgical approaches and tips and tricks for successful revision surgery Description Surgeons constantly need to decide whether fracture reduction and xation is satisfactory. This symposium seeks to dene what is acceptable post-xation and approaches to managing challenging problems, taking into account specic fractures, patient factors, and available resources. Decision-making on acceptable reduction are common decisions faced by orthopaedic traumatolo-gists worldwide. Ultimately, these decisions are governed by multiple factors.
www.Arthrex.com© 2021 Arthrex, Inc. All rights reserved. evAD1-000392-en-US_AArthrex Trauma…Innovative Solutions for Fractures, Soft Tissue and Wound HealingNew!Humeral Plating SystemNew!Trochanteric Nail System New!New!Patella SuturePlate™ with KreuLock™ Locking Compression ScrewsPilon Fusion SystemVisit us at Booth #309 to Learn More About Our Expanded Trauma Portfolio
Register Today at ota.org 29 Rehab to Optimize Outcomes: Getting Our Patients Back on their Feet Moderator: Daniel J. Stinner, MD, LTC Faculty: William T. Obremskey, MD, MPH Joseph R. Hsu, MD Kristin Archer, PhD Learning Objectives • The audience will understand the typical norms for time to weight bearing follow- ing injuries to the lower extremity. They will also learn about current data where these norms have been challenged to optimize outcome. • The audience will understand the impact that psychosocial factors have on outcome. They will also be instructed on methods to identify patients at higher risk for poor outcome and methods for intervening early to optimize outcome. • The audience will learn about various bracing options that can improve outcome (pain and function) in patients following foot and ankle trauma. They will also learn about several adjunct treatment therapies and the data to support or discount their use. Description This breakout will use evidence to challenge the current standards of rehabilitation following extremity trauma and will provide guidance on incorporating it into clinical practice. From recommendations on early weight bearing to bracing and blood ow restrictive training, this breakout will pro-vide evidence-based tips on rehabilitation to help optimize the outcomes of patients following extremity trauma. Little emphasis is placed on our patients after they leave the operating room and we know that not all patients are created equally. This breakout will 1) help the orthopaedic surgeon identify patients who may be at risk for a worse out-come and 2) provide them with the tools to optimize their recovery well after they have left the operating room. Axial Plane Deformity - How to Avoid It and Correct It Moderator: Geoffrey Marecek, MD Faculty: Milton T.M. Little, MD Mitchell Bernstein, MD Ashley Levack, MD Learning Objectives • Dene axial plane deformity • Use strategies to avoid creating axial plane deformity • Evaluate and correct axial plane defortmitySaturday, October 23, continued 2:12 PM - Concurrent Breakout Sessions3:12 PM From Knee to Ankle: Tips and Strategies for Managing Tibial Sha Fractures in Proximal, Middle, and Distal Thirds Moderator: Michael A. Maceroli, MD Faculty: Cory A. Collinge, MD Sandeep Soin, MD John P. Ketz, MD Roberto C. Hernandez-Irizarry, MD Learning Objectives • Take away strategies for reduction and xation of extra-articular tibia fractures with specic focus on anatomic regions and the unique challenges each presents. • Addressing the combined tibia shaft fracture with intra-articular involvement while maximizing quality of reduction and minimizing soft tissue disruption. • What to do When it Doesn’t Work --- strategies for managing tibial nonunions and bone loss with and without concomitant infection. Description The goal of this breakout session is to pro-vide an in-depth look at tibia fracture man-agement separated by “anatomic thirds”, highlighting specic challenges and tech-niques for each. Presentations will be case-based (with literature support) and include everything from surgical planning to implant selection to reduction techniques. Strate-gies will focus on the latest decision-making and xation options to maximize outcomes. Tibia fractures remain one of the most common injuries treated in tertiary referral and community trauma centers alike. Most educational items discuss “tibia fractures” as a whole despite sometimes stark differences in treatment strategy depending on fracture location and morphology. This breakout session will aim to unpack tibia fractures into anatomic regions, allowing for a more de-tailed discussed of the specic skills required to achieve reduction and promote healing in each location. In addition, a special focus will placed on tibial shaft fractures with con-comitant intra-articular components as well as those with diaphyseal bone loss.
#OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org 30 Saturday, October 23, continued 2:12 PM - Concurrent Breakout Sessions3:12 PM Description Axial plane deformity is fairly common after fracture. This symposium will highlight strategies to avoid malrotation and short-ening. We will discuss how to evaluate and treat patients with deformity. Axial plane deformity is a common source of litigation. New evidence suggests that neither length nor rotation are symmetric. Newer treatment modalities make correction of small deformi-ties feasible. Contaminated Open Fractures: Getting It Right and What to Do If It Goes Wrong Moderator: Benjamin Ollivere, MD, MA Faculty: Paul Tornetta III, MD William M. Ricci, MD J. Tracy Watson, MD Learning Objectives • Management strategies for open-articular fractures. • Dealing with post-operative infection. • Reconstruction options in segmental defects. Description The contaminated open fracture is the most devastating of orthopaedic injuries. Man-agement issues to be addressed include all aspects of management of contaminated open fractures and management of initial soft tissue and contaminated bone manage-ment, secondary infection and strategies for management of joint and diaphyseal bone loss including transport and lengthening nails. The contaminated open fracture pres-ents to every area of orthopaedic practice. There have been improvements in standards of care, reconstructive options and expected outcomes. This session will cover the under-lying decision making processes in the key areas of contaminated open fracture man-agement to be discussed and understood. The case illustrated discussion session will cover tips and tricks supported by a princi-ples based approach to complex injuries. There have been no similar sessions at the OTA for the past 3 years.2:12 PM - Paper Session VIII3:39 PM Upper Extremity & Wrist and HandModerators: Harmeeth S. Uppal, MD, MS John A. Scolaro, MD, MA2:12 PM - PAPER 1242:18 PM SpinintheAbstractsofMeta-analyses and Systematic Reviews: Midshaft Clavicle Fractures Matthew Gulbrandsen, MD; R.CaseyRice,MD;TrevorGulbrandsen,MD; Joseph Liu, MD2:18 PM - PAPER 1252:24 PM Acute Plate Fixation of Displaced Midshaft Clavicle Fractures Is not Associated with Earlier Return of Normal ShoulderFunctionWhenUnionIs Achieved Jamie A. Nicholson, MBCHB, MRCSED; Nicholas D. Clement, MRCS Ed; Andrew D. Clelland; Deborah J. MacDonald, BA; Hamish R.W. Simpson, ChB, Dmed; Christopher M. Robinson, MD2:24 PM - PAPER 1262:30 PM Multicenter, Prospective, Observational TrialofNon-OperativeversusOperative TreatmentforHigh-EnergyMidshaft Clavicle Fractures Kyle J. Jeray, MD; Brian Mullis, MD; JoshuaEverhart,MD,MPH; JohnS.Broderick,MD; Stephanie L. Tanner MS; Southeastern Fracture Consortium2:30 PM DiscussionOTA 37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, Texas
Register Today at ota.org 313:16 PM Discussion3:21 PM - PAPER 1333:27 PM ORIF of Multifragmentary Fractures of theRadialHeadDoesNotLeadtoWorse Outcomes Compared to Arthroplasty Phillip McKegg, MS; Genaro Deleon, MS; NathanN.O’Hara,MHA;QasimGhulam,MS; ZacharyD.Hannan,BS; RobertV.O’Toole,MD; Christopher Langhammer, MD; Lucas S. Marchand, MD; Gerard Slobogean, MD, MPH; RaymondA.Pensy,MD; W. Andrew Eglseder, MD3:27 PM - PAPER 1343:33 PM Percutaneous Fixation of Acute Scaphoid WaistFractures:Long-term Patient-reportedFunctionalOutcomes andSatisfactionataMeanof11Years Following Surgery Paul Stirling BSc(Hons), MBChB (Hons); RyanD.Broll;SamuelMolyneux,MSc; ChristopherW.Oliver,MD,MBBS; Margaret M. McQueen, MD; Andrew D. Duckworth, MBCHB, MSc, PhD3:33 PM - Discussion3:39 PM AdjournSaturday, October 23, continued 2:35 PM - PAPER 1272:41 PM Not All Proximal Humerus Fractures Do WellWithoutSurgery:AnteriorTranslation Predicts the Need for Surgery Amir Shahien, MD; Paul Tornetta III, MD; BrianMullis,MD;EliveF.Likine,MD; GillianSoles,MD;StevenSamborski,MD; ClayA.Spitler,MD; Siddhant K. Mehta, MD, PhD; ScottP.Ryan,MD;TarynE.Leroy,MD2:41 PM - PAPER1282:47 PM Long-TermOutcomesofSecondary Implant Removal and Arthrolysis in Patients with a Painful Stiff Shoulder After Open Reduction and Locking Plate Fixation for a Proximal Humeral Fracture Navnit S. Makaram, MBCHB, MRCS; Christopher M. Robinson, MD2:47 PM - PAPER 1292:53 PM No Change in Outcome between One and FiveYearsafterRepairofDisplaced Proximal Humerus Fracture Sanjit R. Konda, MD; Rachel Ranson, MS; ConnorP.Littleeld,BA;RachelRoller; Kenneth A. Egol, MD2:53 PM Discussion2:58 PM - PAPER 1303:04 PM Surgical Treatment of Dorsally Displaced Distal Radius Fractures with a Volar Locking Plate versus Conventional PercutaneousMethods:MinimumTen-Year Follow-UpofaRandomisedControlled Trial Sandeep R. Deshmukh, MBCHB; Ben Marson; Reuben Ogollah PhD; TimDavis;AlexiaKarantana,PhD3:04 PM - PAPER 1313:10 PM Delayed Fixation of Distal Radius FracturesPastThreeWeeksAfterInitial Failed Closed Reduction Increases the Odds of Reoperation Lauren Nowak, PhD, MSc; MelanieMacnevin;Joel-AmirMoktar,MD; Emil H. Schemitsch, MD3:10 PM - PAPER 1323:16 PM TheTrajectoryofLong-TermRecovery Following ORIF for Distal Radius Fractures Gabriel Larose, MD; HenryM.Broekhuyse,MD;PierreGuy,MD; PeterJ.O’Brien,MD; DarrenRoffey,PhD; KellyAnnLefaivre,MD,MS
32 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org Mission StatementThe mission of the Orthopaedic Trauma Association (OTA) is to promote excellence in care for the injured patient, through provision of scientic forums and support of musculoskeletal research and education of Orthopaedic Surgeons and the public.Vision StatementThe OTA will be the authoritative source for the optimum treatment and prevention of musculoskeletal injury, will effectively communicate this information to the orthopaedic and medical community and will seek to inuence health care policy that affect care and prevention of injury.Value StatementThe OTA is adaptable, forward thinking and scally responsible and is composed of a diverse worldwide membership who provide care and improve the knowledge base for the treatment of injured patients. OTA members provide worldwide leadership through education, research and patient advocacy.37th Annual MeetingOctober 20 - 23, 2021 • Fort Worth, TexasGeneral InformationAccreditation and CME Credit The Orthopaedic Trauma Association is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.The Orthopaedic Trauma Association designates this liveactivity for a maximum of 20.5 AMAPRACategory1Credits™.Physicians should claim only the credit commensurate with the extent of their participation in the activity.CME Mission StatementThe mission of the Orthopaedic Trauma Association is to promote excellence in care for the injured patient, through provision of scientic forums and support of musculoskeletal research and education of orthopaedic surgeons and the public. We will plan, manage and evaluate evidence-based educational activities that enhance participant competence, performance and patient outcomes employing needs assessment data and identied professional education gaps. CME activities will consist of carefully planned programs based on adult learning principles, including live CME activities and enduring materials. It is expected that participants in these CME activities integrate what they learn into their practice to improve their competence and performance in areas of patient care, patient safety and professional practice.techniques and/or presenting research offered at three convenient times. DisclaimerThe material presented at the 37th Annual Meeting has been made available by the Orthopaedic Trauma Associa-tion for educational purposes only. The material is not intended to represent the only, nor necessarily best, methodor procedure appropriate for the medical situations discussed, but rather is intended to present an approach, view, statement or opinion of the faculty which may be helpful to others who face similar situations.OTA disclaims any and all liability for injury or other dam-ages resulting to any individual attending this event and for all claims which may arise out of the use of the techniques demonstrated therein by such individuals, whether these claims shall be asserted by physician or any other person.
Register Today at ota.org 33Register Today at ota.org 37th Annual MeetingGeneral Information and Special EventsPhilosophyIn order to promote transparency and condence in the educational programs and in the decisions of the Orthopaedic Trauma Association (hereinafter referred to as “OTA”), the OTA Board of Directors has adopted this mandatory disclosure policy.The actions and expressions of OTA Members and Others providing education of the highest quality or in shaping OTA policy must be as free of outside inuence as pos-sible, and any relevant potentially conicting interests or commercial relationships must be disclosed. Because the OTA depends upon voluntary service by Members to conduct its educational programs and achieve its organiza-tional goals, this disclosure policy has been designed to be realistic and workable.The OTA does not view the existence of these interests or relationships as necessarily implying bias or decreasing the value of your participation in the OTA.FDA StatementAll drugs and medical devices used in the United States are administered in accordance with the Food and Drug Administration (FDA) Regulations. These regulations vary depending on the risks associated with the drug or medical device, the similarity of the drug or medical device to products already on the market, and the quality and scope of clinical data available.Some drugs or medical devices described or demonstrated in OTA educational materials or programs have not been cleared by the FDA or have been cleared by the FDA for specic uses only. The FDA has stated that it is the respon-sibility of the physician to determine the FDA clearance status of each drug or device s/he wishes to use in clinical practice. AppWatch your email for release of the OTA Annual Meeting app. Special EventsTai Chi ClassWednesday, October 205:00 PM - 6:00 PM Vinyasa Yoga ClassFriday, October 226:00 PM - 7:00 PM Meditation ClassWednesday - Friday, October 20 - 227:00 AM - 7:30 AMWellness RoomWednesday - Friday, October 20 - 227:30 AM - 4:00 PM The wellness room will serve as a quiet room during the meeting. We request that this space be a technology-free quiet zone. Attendees can use this space to briey disconnect.Tour de Bone Bike EventThe ofcial 2021 Tour de Bone has been postponed due to low bike inventory. We look forward to 2022. sponsored by
34 #OTA2021 | @otatrauma | @otatrauma | Register Today at ota.org Exhibit Hall HoursThursday, October 212:30 PM - 5:00 PM 5:15 PM - 6:15 PM – Exhibitors’ ReceptionIndustry Session Opportunities OfferedWednesday, October 20 6:30 PM - 8:00 PM Thursday, October 21 11:15 AM - 12:45 PM Friday, October 22 6:30 PM - 8:00 PMVisit the OTA website for a complete listing of Industry Sessions.Friday, October 229:00 AM - 5:00 PMSaturday, October 239:00 AM - 12:45 PM
Resident ComprehensiveFracture Courseota.orgWednesday-FridayOctober 20 - 22, 2021#OTA2021Omni Hotel • Fort Worth, TexasProgram Chairs Seth R. Yarboro, MDHolly Pilson, MDRegister Today @ ota.orgAnnouncing the Release of theNew OTA Core Curriculum Lectures!New OTA Core Curriculum Lectures!• Over 100 Lectures from OTA Faculty • All Revised Content from Previous Versions • Great Educational Resource! • Project Directors: Lisa K. Cannada, MD Kyle J. Jeray, MD Samir Mehta, MDVisit ota.org/education/core-curriculum-lectures@ota.org
Please refer to the instructions for use for a complete list of indications, contraindications, warnings and precautions.© DePuy Synthes 2021. All rights reserved. 183817-210721 DSUSJOIN OUR INDUSTRY SESSIONSThursday, October 21, 2021 | 11:15 am – 12:45 pm Expanding Fixation Options for Periprosthetic FracturesLocation: 121CImproving Stability in Femur and Tibia Fractures with the Advanced Nailing SystemLocation: 121DEnhancing Plate-to-Bone Conformity by Mapping Clavicle Morphology and Its Relation to Patient HeightLocation: 121E