Return to flip book view
JournalVOLUME 103 2024 ISSUE 2WWW.INDENTAL.ORGThe JOURNAL of the INDIANA DENTAL ASSOCIATIONCHALLENGES OF ACADEMIC LIFE IN DENTAL SCHOOLS PAGE 20COMBATTING COMPASSION FATIGUE PAGE 43STATE OF DENTAL LICENSURE 2024 PAGE 36Dental School in 2024 | PAGE 12IDA Message
The Journal is owned and published by the Indiana Dental Association, a constituent of the American Dental Association.The editors and publisher are not responsible for the views, opinions, theories, and criticisms expressed in these pages, except when otherwise decided by resolution of the Indiana Dental Association. The Journal is published four times a year and is mailed quarterly. Periodicals postage pending at Indianapolis, Indiana, and additional mailing oces.ManuscriptsScientic and research articles, editorials, communications, and news should be addressed to the Editor: 550 W. North Street, Suite 300, Indianapolis, IN 46202 or send via email to kathy@indental.org.AdvertisingAll business matters, including requests for rates and classieds, should be addressed to Kathy Walden at kathy@indental.org or 800-562-5646. A media kit with all deadlines and ad specs is available at the IDA website at www.indental.org/adverts/add.Copyright 2024, the Indiana Dental Association. All rights reserved.Journal IDAPersonnelOfficers of the Indiana Dental AssociationDr. Lisa Conard, PresidentDr. Rebecca De La Rosa, President-ElectDr. Lorraine Celis, Vice PresidentDr. Will Hine, Vice President-ElectDr. Jenny Neese, Speaker of the HouseSubmissions Review BoardDr. Rebecca De La Rosa, AvonDr. Caroline Derrow, AuburnDr. Steve Ellinwood, Fort WayneDr. Karen Ellis, Co-EditorDr. Sarah Herd, Co-Editor Dr. Joseph Platt, Vice Speaker of the HouseDr. Nia Bigby, TreasurerDrs. Karen Ellis and Sarah Herd, Journal IDA EditorsDr. Thomas R. Blake, Immediate Past PresidentMr. Douglas M. Bush, Executive Director, SecretaryDr. Jerey A. Platt, IndianapolisDr. Kyle Ratli, IndianapolisDr. Elizabeth Simpson, IndianapolisKathy Walden, Managing Editor
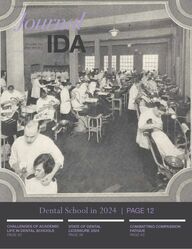
4 Editor’s Message Dr. Karen Ellis 6 IDA President’s Message Dr. Lisa Conard 8 Immediate Past President’s Message Dr. Tom Blake 10 Executive Director’s Message Mr. Doug BushCover Story 12 Finding My Calling: My Journey to Academia Dr. Elizabeth Simpson 14 A Day in the Life: IUSD Students in Their Own Words Dr. Elizabeth Simpson 20 Challenges of Academic Life in Dental Schools: A Faculty Perspective on Connecting All the Pieces to Succeed Dr. Priya Thomas, Dr. Monica Gibson, Dr. Chandni Batra, Dr. Hawra AlQallaf, Dr. Neetha Santosh, Dr. Celine Cornelius, Dr. Halide Namli, Dr. Vanchit John 24 The State of Dental Curricula: Are We Preparing Students for Today’s Practice and Academic Life? Dr. Chandni Batra, Dr. Celine Cornelius, Dr. Monica Gibson, Dr. Hawra AlQallaf, Dr. Priya Thomas, Dr. Halide Namli, Dr. Neetha Santosh, Dr. Vanchit John 30 Mental Health: A Review of Dental Schools and their Mental Health Initiatives for Dental Students Dr. Monica Gibson, Dr. Celine Cornelius, Dr. Neetha Santosh, Dr. Hawra AlQallaf, Dr. Chandni Batra, Dr. Halide Namli, Dr. Priya Thomas, Dr. Vanchit John 36 State of Licensure 2024 Dr. Jill Burns 38 Dental School from the International Student’s Perspective Dr. Elizabeth Simpson News & Features 43 Combatting Compassion Fatigue as a Dental Professional Dr. Catherine MurphyClinical Focus 46 Diagnostic Challenge: Spring 2024 Dr. Angela Ritchie, Dr. Neetha Santosh Member Zone 50 In Memoriam 51 Classieds 52 New Members 53 Out of the OperatoryCONTENTS Issue 02 2024124346COVER PHOTO:General operatory of the Indiana Dental College, 1924. Reprinted with permission from Indiana University School of Dentistry.
4 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2I was not the child that had to be coaxed or promised special treats to go to the dentist. The hygienist did not have to chase me around the room to get me in to the dental chair. I remember liking going to the dentist. The routine was pretty standard: go to dentist, get treated like a princess and walk away with a toy. But the day I had my lling done (an amalgam placed on the occlusal surface of tooth #14) was especially memorable. I remember that now there were TWO people making a fuss all over me. I remember the movement of the hands and arms over my mouth in a uid movement similar to a maestro conducting a symphony. But what made the visit as vivid then as it is to this day was the mirror that was placed on the overhead light. I was xated being able to watch what was going on. I don’t remember being scared. I just remember fascination about what was going on in the mirror: I could feel my body becoming very still and my eyes growing wide, the bare hands, the back and forth passing of instruments, my mouth open with what seemed like cotton rolls everywhere, the whir of the drill and the plugging of whatever it was in my tooth. My amalgam is still there. It is super tiny. And the whole event probably lasted no more than 10 minutes. But in that moment I felt like time was standing still. That mirror was pivotal in fostering my CURIOSITY. I entered dental school with curiosity and a desire to learn. The four years at Indiana University School of Dentistry were dicult to say the least. As Charles Dickens would open A Tale of Two Cities, “It was the best of times, it was the worst of times, it was the age of wisdom, it was the age of foolishness, it was the epoch of incredulity, it was the season of Light, it was the season of Darkness, it was the spring of hope, it was the winter of despair.” The highs and lows I experienced while a student felt very similar to that. I did not come from a family of dentists and the learning curve was great. I was in SBO5 until 11:30 most nights working on my hand skills. The hazing culture was strong and fear was an absolute motivator. I think I cried nearly every day my second year of dental school and remember being encouraged by upper classmen that “next year will be better.” That wasn’t true. And it wasn’t true for my senior year either. But, I did feel buoyed by the support of my classmates who became Dr. Karen Ellis, Journal IDA co-editorEDITOR'S MESSAGE Pivotal MomentsIT WAS 1980. The year was signicant for many reasons. Mount St. Helens Volcano erupted in Washington State, killing 57 people and causing an estimated 3 billion in damage. The U.S. Hockey team beat the heavily favored Soviet Union 4-3 at Lake Placid, NY in one of the biggest upsets in Olympic history. That same year, President Jimmy Carter announced the U.S. would boycott the summer Olympics in Moscow, Soviet Union in protest of the Soviet war in Afghanistan. Pac-Man was released becoming one of the best-selling video games of all time. The Rubik’s Cube was introduced. Blondie released the hit song “Call Me,” which would become the 1980 Billboard Song of the Year. And, it was a national obsession for millions of viewers as they tuned in to watch the television series “Dallas” to learn “Who Shot J.R.?” For me, the year was signicant because that was the year that I had my rst (and only) cavity lled.ABOUT THE AUTHORDr. Karen Ellis is co-editor of the Journal IDA along with Dr. Sarah Herd. Dr. Ellis is a general dentist for the Marion County Public Health Department and can be reached at ellis_karen@yahoo.com.like family and by family who became patients. I always say that even though some of the worst times of my life occurred while a student, so did the best. And, things began to “click.” I learned that the world wasn’t run by geniuses alone but also by those that refused to quit. I refused to quit. I was grateful for the hard times because they made me a better dentist. I knew I wasn’t going to let anything stop me from becoming a dentist. Those years at IUSD were instrumental in shaping my grit and RESILIENCE.
5VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationBolstered with curiosity and my new found resilience, I moved to St. Louis, Missouri for my General Practice Residency at Washington University School of Medicine. I was now in an environment that was in complete contrast to IUSD. My attending dentists were mentors and actually invested in who I was as a dentist and person. They wanted to see me succeed. The rotations through emergency medicine, anesthesiology, oral surgery and pediatric dentistry were challenging, inspiring and collaborative. My favorite experiences though were working side by side with an attending dentist in the operating room with general anesthetic cases for adult patients with developmental disabilities that prevented them from being seen in our oces. Not only were we doing a service that improved the lives of whom we were treating, but that time one on one with an expert to ask questions, be asked questions and work in partnership have always been the highlights of my professional career. No one had an ego in the OR and the goal was always the same—to give the absolute best care to those who needed us most. The patients may not have realized the benet to what we were doing, and they certainly didn’t know that all of the margins were sealed on a Class II restoration, but I always saw the look of gratitude in the eyes of a parent or loved one when we met with them in recovery. It was then that I knew I wanted to help those that could not help themselves or who needed extra assistance with getting dental care. This began my career in public health dentistry. I also thought of always doing my best even when no one was watching. Those patients under general anesthetic were at their most prone. I appreciated that I was working with those that understood “good enough” was NEVER good enough or acceptable. Even in dicult environments or challenging situations, I learned the importance of INTEGRITY. Always do your best.I have been in dentistry for 25 years now, and I am continually shaped by events and experiences that I learn and grow from. I have been a member of organized dentistry for 23 of those 25 years and that has been one of the best decisions I have made. I initially joined to make new friends and because I wanted to have a sense of belonging. In the beginning, I was thinking about what I could “get” from being a member of organized dentistry and not how I could “give.” I was reluctant to get more involved but I was encouraged to join the IDDS Foundation and also the IDA Dental Education and Practice Council. There is great importance in what the tripartite does for its members, the profession and the community. And a funny thing happened, the more I began to serve and give the more I got back in forms of connection and love. Thanks to organized dentistry, I have been able to engage in SERVICE for the greater good and what it means to be a servant leader. As I wrap up my tenure as Co-Editor of the IDA Journal, I wanted to share some of the moments in my life that made me the dentist I am today. What experiences have you had that have shaped your beliefs and made you the professional you are? I would love to hear them. I personally want to thank you for allowing me to share parts of my life in this format and also to SERVE you. It has truly been a privilege.
6 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2Thank you for electing me to be the president of the Indiana Dental Association for the next year. The mission of the IDA is to support dentists, to promote professionalism, and to improve oral health. My goal as President is to continue the mission of the IDA by representing the goals and concerns of the membership to fulll this mission. The leaders before me have modeled this mission well. I would like to recognize the members who have attended the meeting with strollers in tow! These members and their families have made accommodations to remain actively involved while raising their families. This is a testimony to our changing landscape. I commend you for the eort to make this happen and am so excited to see this.A little bit about me. I have been a member of organized dentistry since August of 1983 as an ASDA member when I began dental school at The University of Louisville. I remain an active member in Kentucky, Florida and here in Indiana. But my real engagement started several years ago when I was asked by Dr. Sue Germain to consider applying for the IDA AIR Leadership Program in the 3rd year cohort. The AIR acronym stands for Acceptance, Inclusion and Respect. This program teaches skills needed for leadership. Several of my classmates as well as many other graduates are in this room today. At the completion of that two-year program, I was encouraged by Dr. Dave Holwager to run for trustee of my component, the Ben Hur Dental Society. I did. And I was elected. Then during my time as Ben Hur president, I was encouraged by so many of our members to continue in leadership at the IDA committee level. Once involved for several years and with continued support from many leaders in this organization, I was encouraged by Dr. Tom Blake to go through the line oces for the IDA. The reason I am telling you this story is to ask you to seek out potential leaders in your component dental society. Encourage them like I was encouraged. And when you are on the receiving end of that invitation to get involved… step up and lead. Take advantage of the opportunity to be a leader. Sometimes others see leadership potential in you, even before you see it yourself. Embrace it and take the opportunity to lead.I have a vested interest in leadership, as I have served on the IDA Leadership Committee for several years, most recently as chair. During my time as chair, we encountered a milestone. Several years ago, this House adopted a new committee and subcommittee structure that included three two year term limits. This year, for the rst time, many longtime volunteers termed out of their committee positions. Several of them were committee chairs. We saw the number of vacant slots and began the plan to ll them. We issued a call to current leaders, especially trustees, component presidents and component executive directors to help us and they came through. If you look at the Leadership Committee’s annual report in your House Manual, you will see that almost all of the volunteer positions have been lled. Thank you all who submitted names for committee member prospects. Thank you to those of you who said “yes” and stepped up. We are in good shape.One of our Strategic Plan goals is to make ecient use of volunteers. Thus, rst, we are going to make volunteer recruitment an Dr. Lisa Conard, 2024-25 IDA PresidentPRESIDENT'S MESSAGE Inaugural Address of Dr. Lisa Conard, 2024-25 IDA PresidentON MAY 18, at the 2024 Second House of Delegates, Dr. Lisa Conard became the 2024-25 IDA President. A general dentist in Lebanon and adjunct professor in Cariology and Operative Dentistry at IUSD, Dr. Conard gave the following address to those in attendance.
7VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Associationongoing process. While we usually know in advance when our IDA volunteer opportunities are going to happen, we often nd out about ADA leadership opportunities with very little notice. We want to be prepared by having a pipeline of prospective leaders on standby. The IDA sta is in the process of a revamp of the IDA website. It will include a volunteer site where any member can review upcoming opportunities and express an interest in getting involved as a committee or subcommittee member or consultant. If you have diculty nding this option, please email myself and Andrea New, IDA’s director of volunteer engagement, so that we can get you involved.Attending continuing education meetings usually ignites enthusiasm from presentations in materials, technology, practice management, etc. Those of us who attend the House of Delegates are also intrigued and often inspired by the issues brought before this House, as well as in private discussions and concerns that are shared in casual conversations. My hope is that those of you that have had ideas and thoughts will apply for positions on committees by going to the IDA website and signing up to be committee members so that we can tap your skills and thoughts. Second, we want to equip volunteers with the skills they need to be successful. When Dr. Tom Blake surveyed committee chairs last year, one of the things they asked for was additional training. Again, as an AIR graduate, I know how important training is to help you build your skills and condence as a leader. We are going to have a leadership workshop this year that will provide committee chairs and trustees with guidelines and outlines to help them eectively run meetings. We are going to help them develop clear expectations and an understanding of the purpose of each position. I believe in clear outlines of these positions to encourage people to volunteer knowing the expectations and feeling that they have support to accomplish the goals. Andrea New is going help me develop ocer and committee “manuals” to assist with record keeping and to help leader transitions go smoothly. We will hold a trustee and committee chair (along with their sta member) leadership session, complete with templates for meeting agendas, minutes and nancial recording. This formalization will help with record keeping so that information is easily available for future reference. Having this training can help meetings be more organized and productive, thereby respecting volunteer time.Third, we are going to support volunteers by making better use of technology. The IDA has been through a major technology update and the new website will be unveiled before the end of the year. Plus, the ADA will launch its new association management system this summer. Each of these upgrades will assist chairs and their committees with organization and eciency. These are all exciting opportunities to continue with our existing foundation while laying a new foundation engaging the creative minds of our new committee members who will produce an even more vibrant association. We have recently made great strides legislatively and our relationship with the school is strong. With the recent emphasis of mental health wellbeing, we are addressing having assistance for our members overall health with great strides and initiatives through our newly formed Be Well Subcommittee. Two years ago the need for mental health assistance is our profession became much more apparent to us. IDA leaders formed a subcommittee and entitled it Be Well. This committee is providing resources for health, lling in between stress and addiction. Our Be Well subcommittee is making great strides, holding multiple sessions at this MDA that were highly attended. We are serving the needs of our members. Thank you to all who serve on this subcommittee.During the next year we’re going to have to closely examine our nances and make sure we make the best possible use of every dues dollar. We will examine every IDA program. This examination will allow us to determine which programs that are successful and benecial to our membership, and programs that are not. I have begun to put together a task force that will evaluate our budget line item by line item considering expenditures and value to our overall association. We will ask each committee chair for information to assist with gathering this information. It will be compiled by August 1 so that we can present ndings at the leadership training and the September Board meeting.While we face these changes, I see opportunity. In 2026, Indiana will be hosting the ADA Annual Session – SmileCon for the rst time ever. This October we hope to help elect our own Chad Leighty as President-Elect of the American Dental Association. If elected this fall, Chad will complete his year as ADA president right here in Indiana at the 2026 SmileCon. We are looking forward to that!During the past three years as I’ve moved through the chairs of leadership, I have learned a lot but undoubtedly, I have much still to learn. I ask that you please do not hesitate to share information that you may have that could help as well as sharing your concerns. I want to hear from members as I believe that your leadership is here to serve you. Thank you so much. We are stronger together.
8 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2PAST PRESIDENT’S MESSAGE A Year in the Life of an IDA President… A Look in the Rearview MirrorI AM SURE that by the time that many of you read this that I will have become the Immediate Past President after the Midwest Dental Assembly which was held in French Lick. This has certainly been a time of personal reection and has given me time to look retrospectively at my almost 43-year career (which I have cherished…MOST of the time).I believe that there are so many transitions in our lives and nishing my year as YOUR IDA President is just one more milestone to celebrate. But I am getting ahead of myself. While I have always been a member of Isaac Knapp since graduation, I have not always been involved as a leader in organized dentistry. Knowing that 18 years y by so quickly, I spent my rst 15 years involved in my kids’ schools. I, like so many dentists in my era, have not worked with patients on Fridays unless it was volunteering at Fort Wayne’s Matthew 25 charity clinic or doing some other volunteer work. Going into schools on Fridays to help was simply a joy for me to be around all of those young eager minds and I loved planning activities with the school administration to make education an enjoyable experience for the students. Of course, 12 years of pre-college education is over before you know it and then my sons headed to college. It was at this transition that I had promised my own dentist and mentor, Dr. Gerry Kaufman that I would become involved in Isaac Knapp, which I did for several years on the board and eventually went through the chairs to president in 2011-12. Unfortunately for me, Dr. Kaufman passed before I assumed the oce. I am sure that he knew, however. I have been more than blessed to be a member of such a vibrant local component. I am glad that many senior members of IKDDS saw the leader in me back when I rst started out my organized dentistry career. That mentorship and encouragement along the way helped me to erase some of the PTSD from dental school. (I’m sure we can all relate.) My time leading Isaac Knapp was very rewarding even though during my presidential year I did not have an Executive Director to do the things that Jamee Lock does for Isaac Knapp now. As I reected back to my beginnings, I realized how important it was to have relationships with same-aged peers and started our Young Dentist Committee which has provided most all of the ocers of Isaac Knapp in the last several years. I am a sucker for the younger dentist. I continue this mission to this day serving as the group’s mentor. My desire for these young clinicians is for them to love our profession at the twilight of their careers as much as I do. I understand that each person has his or her own personal journey in the work/life balance arena and MUCH has changed in the last four decades. It has ALWAYS been my goal to assist students and young graduates in our eld. I hope in some respect that I have been of assistance along the way. This by itself would be a wonderful legacy to leave our profession.Of course, in my later years of my practice life, a monumental transition for me was “coming out” at such an advanced age. It wasn’t easy by any stretch of the imagination and I was worried that I would lose the respect of friends, family and colleagues, but one of my foundational words in my leadership language has always been transparency. How could I truly be transparent if I was living non-transparently in this aspect of my life. Coming to meetings at rst was dicult but I was determined to give my best in serving as both an Alternate Delegate and the Delegate to the Annual IDA Meeting (now MDA). To my delight/relief my friends rallied around me as I was still the same Tom Blake…now just living my truth. It was an absolutely amazing time of my life. I am guessing that people still saw the leadership qualities in me and respected my leadership style as many encouraged me along the way. I had always been the Treasurer Dr. Tom BlakeABOUT THE AUTHORDr. Tom Blake is a dentist in Fort Wayne and the 2023-2024 IDA president. He can be reached at tblake5591@aol.com.
9VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Associationof EVERY organization that I was a part of whether it was the PTA, Athletic Boosters or our neighborhood pool board. Numbers are “my thing.” I served as a member of the IDA Finance Committee for many years and when it was known that Dr. Dan Fridh was going to step down as Treasurer, I was encouraged by friends (especially Dr. Steve Ellinwood) to apply for the position and lo and behold, I served in that position for four years…yet ANOTHER transition. It was NEVER on my radar screen to become the President of the IDA and since it is usually a trustee who moves in to go through the chairs, I really didn’t even think about it at all and then something happened. Some of the younger members of the IDA encouraged me to run (among them my good friends Drs. Matt Kolkman, Caroline Derrow, Mandy Miller and Megan Keck). I really had to think about it for a couple of weeks and honestly didn’t know what the process was to run. So, I called Doug Bush. I know that it was a shock to him to be entering the race in February right before the unknown shut down of the world from COVID. So many thoughts raced through my head. Can I do this? Do I have the time? Do I have all the knowledge I need? Will my lifestyle be something that will determine the results? On and on…I nally decided that indeed I would give it a shot AND it was a contested election. I tried to tell myself at the time that no matter how the results ended up that I would be ne, but then I REALLY wanted to win. I felt I had a good platform and lots of support from so many delegates and ocers. Fast forward, past three re-votes due to technical errors since the meeting was on Zoom and I WON! Next transition.So here we are four years later and I couldn’t be happier or prouder that I decided to take the call to head our organization. It has been an amazing four years leading up to this honor and I thank each and every one of you for what you have done to make our organization stronger. Whether it be encouragement, advice, or just a kind text or voicemail, you have meant the world to me. So many experiences I would never have had have now been a realization. I have met state presidents from across the U.S. I have learned so much more about advocacy. I actually got to speak at last year’s IUSD graduation with the current ADA President- Elect. I have gotten to see rsthand how respected Indiana is on a national level. I have seen the inuence that Doug Bush has with other executive directors. I have gotten to give so many speeches for so many dierent events that I never would have gotten to had it not been for those who urged me along the way. It truly has been my pleasure and such an honor and so THANK YOU all.We have had an excellent year this year thanks to YOU and your involvement. Our new programming of the monthly FrIDAy with the IUSD students has been so successful and will continue to level the speed bump between school and rst practice experiences. Welcoming our young colleagues is crucial to the vitality of our organization. Our new Ten Under Twenty group has been formed and we are busy incorporating these leaders into the IDA structure. Our Government Aairs Committee led by Director of Government Aairs Shane Springer hit multiple home runs this year with the passage of Assignment of Benets and Network Leasing will be of great benet to all dentists AND patients in the future. (taking eect July 1, 2024) This would not have happened without YOU contacting your legislators. I am proud of what we have done and look forward to a successful future transition.So as I transition to my new job as Immediate Past President, I anticipate future victories for us. Our Executive Committee is strong and has great ideas as the landscape of organized dentistry is going through great changes. We have the right people in place. For better or for worse, you are not getting rid of me quite yet either. As I have transitioned to semi-retired as “Two Day Tom,” I intend to assume any role which may need attention according to our new leadership group. I am here for all of you and for our outstanding organization. We are dynamic, versatile, thoughtful and nimble. We will continue our role as a leading state in the ADA. Thank you again for an amazing opportunity to serve you. I will treasure this experience forever.
10 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2In 1901, Dr. Frederick McKay left his practice on the East Coast and relocated to Colorado Springs, Colorado, where he encountered a dental condition that he could not explain. Many of his patients had brown stains on their teeth. The locals had theories about what caused the condition, none of which Dr. McKay could nd in any dental literature of the day. With the support of the local dental community, they conducted their own study and found that almost 90 percent of local children showed evidence of the odd condition that came to be known as “Colorado Brown Stain.”In 1909, Dr. McKay persuaded renowned dental researcher, Dr. G. V. Black, to visit Colorado Springs to collaborate on the condition. While rst skeptical that a new dental disorder had been discovered, Dr. Black later wrote: “I spent considerable time walking on the streets, noticing the children in their play, attracting their attention and talking with them about their game, etc., for the purpose of studying the general eect of the disorder. I found it prominent in every group of children…. This was much more than a deformity of childhood. If it were only that, it would be of less consequence, but it is a deformity for life.”1Drs. McKay and Black noted that children with the staining showed remarkable resistance to tooth decay. They continued to investigate the condition, with little success before Dr. Black passed away in 1915. Dr. McKay suspected the condition related to the local water supply but could nd no proof until he was called to Oakley, Idaho, in 1923. Local parents there described the same tooth stain he had seen in Colorado Springs. Oakley’s water was supplied by a single spring not far from the town. Dr. McKay persuaded town leaders to abandon the spring for another water source and within a few years, the stains stopped appearing. He felt the water supply was the culprit, but testing didn’t indicate anything out of the ordinary about the water in Colorado Springs or Oakley. In 1931, when the Aluminum Company of America (Aloca) used new, more sensitive photospectrographic testing equipment, they identied an unusually high concentration of naturally occurring uoride. The mystery cause of the mottled brown teeth was nally solved.Dr. H. Trendley Dean, head of dental hygiene, and chemist Dr. Elias Elvove, both of the National Institute of Health (NIH), began searching for a uoride sweet spot… a concentration of uoride that preserved tooth strengthening properties, while eliminating the mottling eect. The rst large scale test of uoride supplementation occurred in 1944 when the city of Grand Rapids, Michigan, voted to add uoride to its public drinking water supply. During the 15-year study, researchers closely monitored the tooth decay rate of 30,000 school aged children. After just 11 years, the caries rate among Grand Rapids chil-dren had dropped by 60 percent. For the rst time, dental disease could be considered highly preventable.Mr. Doug Bush, IDA Executive DirectorEXECUTIVE DIRECTOR'S MESSAGE Fluoride: History and FutureFEW DENTISTS WOULD dispute the benets of uoride in drinking water, but some may not be familiar with the history of community water uoridation and how it came to be. As has been the case with many discoveries, the benets of uoride were found by accident. ABOUT THE AUTHORMr. Doug Bush is serving his 28th year as IDA Executive Director. He can be reached at doug@indental.org. Eighty years have passed since Grand Rapids introduced community water uoridation. As of 2018, the ADA reports that 74 percent of the U.S. population is served by water districts providing optimal uorida-tion.2Of course, community water uoridation has had detractors since it was rst introduced. Some opposition has been political: “Should the gov-ernment be involved in imposing uoride on the public?” That sentiment
11VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Associationfound its way into the cold-war cult classic movie paro-dy, “Dr. Strangelove” (1965). Noting that uoridation was introduced immediately after World War II, General Ripper concludes uoridation was clearly a “post-war Commie conspiracy” to poison drinking water. His logic was hard to refute. “Have you ever seen a Commie drink a glass of wa-ter?” he asks. “Vodka. That’s what they drink. Never water.” Other opponents of uoridation are more serious. The Fluoride Action Network (FAN) declares that their mission is, “…protecting public health by ending water uoridation and other involuntary exposures to uoride.” They pledge to, “Protect public health in communities experiencing high levels of uoride in water due to pollution or natural occur-rence.”3The group is zealous and, in some cases, eective. In fact, a number of Indiana towns have discontinued, or are considered discontinuing, community water uoridation, partially as a result of FAN inuence. According to Jim Powers, manager of the Indiana Depart-ment of Health’s Water Fluoridation Program, the Indiana communities of Goshen, New Castle, Jasonville and Bristol have announced that they are, or are considering, discon-tinuation of community water uoridation. In some cases, decisions are being driven by the cost of replacing or re-pairing aging equipment, but in other instances, decisions are being driven by vocal anti-uoridation activists. NBC News recently reported an increase in the number of communities around the country discontinuing uoridation, based on misleading claims and perceived government oversteps. They speculate a new surge in anti-uoride sen-timent is fueled by pandemic-related distrust of the govern-ment and healthcare authorities. According to Mr. Powers, support from the dental community has historically been critical to keeping community water uoride systems op-erating. Town leaders pay more attention to local dentists than national experts. “I am grateful for any help the IDA and local dentists can provide,” said Mr. Powers. The IDA is currently working with the Indiana Department of Health to craft legislation that would require local commu-nities to notify the Department of Health before discontin-uing uoridation. Too often, the dental community learns about the discontinuation of uoridation after the decision has been made. Even without such a notication require-ment, it is important for local dentists to remain engaged on the community uoridation issue. Meet your mayor and get to know members of your city or town council. Oer yourself as a resource any time they have questions about an oral health issue. Take advantage of excellent resources on oral health and the benets of community water uori-dation, available from the American Dental Association. And don’t forget to talk to your patients.Dr. Donald Chi, a pediatric dentist at Seattle Children’s Hospital, explained that he had to rethink how he talks to parents who are concerned about uoride. He noted the conversation starts not with data, but with empathy.“There’s a lot of disinformation out there that preys on the vulnerability of patients,” said Dr. Chi. “People don’t want information. They just want to talk through it and process it.”4Sources1. National Institute of Dental and Craniofacial Research, “The Story of Fluoridation”. See www.nidcr.nih.gov/health-info/uoride/the-story-of-uoridation2. American Dental Association, “Fluoride Facts” See www.ada.org/resources/community-initiatives/uoride-in-water.3. Fluoride Action Network. See www.uoridealert.org 4. NBC News, “Medical freedom vs. public health: Should uoride be in our drinking water?” See https://www.nbcnews.com/health/health-news/uoride-safe-drinking-water-cities-ban-rcna143605
12 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2COVER STORYFinding My Calling: My Journey to AcademiaI HAVE NEVER been shy about sharing my dental school journey. I share it so often I always assume people know the ins and outs, but I think more often than not a lot of people have no idea how dental school was for me. And knowing how school was for me is key to understanding why I wanted to eventually end up in academia.Dr. Elizabeth SimpsonMy father had been having some health problems leading up to me starting dental school. I attended Tufts University School of Dental Medicine, and two months into starting school he was diagnosed with stage IV renal cell carcinoma and was given four months to live. I ew home to Indianapolis to be with my mom and dad the weekend after we got the diagnosis. I am an only child and my parents and I were very close, so over the course of that weekend, I secretly thought maybe I should leave school or try and transfer to IU to be closer to my family.When I got back to school on Monday, I went to talk to our dean of academic aairs, but on the way to his oce I ran into the dean of the school at that time, Dr. Lonnie Norris, who was the rst African American dean of the dental school. I told him what was going on at home and admitted that I was thinking about leaving school or transferring. He looked me in the eyes and said “No. You will stay here, and we will get you through this.” I felt his sincerity, even with just the few words that he spoke. And so, I stayed, but not without tears. Not without lots of ights home to be with my family at various times. Not without an accidental needle stick from an HIV+ patient and having to take anti-retroviral medications for a month. Not without nishing almost a year late. Not without panic attacks and depression and being prescribed anti-depressants. Not without counseling.Let me tell you, I felt so much support from my friends, faculty and sta that I knew I would nish school. There were times when I felt more from outside inuences that I would nish school than I felt from my own internal motivation. I can’t tell you the number of times I thought, “I hate this place,” school and Boston in general. On top of my dad’s illness, I was the student whose patients consistently didn’t show. I was the one whose procedures would fall through. During my third year, I went to meet with Debbie, the on-campus counselor for the medical and dental school students. I was so embarrassed about having to take medication, but Debbie told me seven out of the top 10 most prescribed medications to the med and dental school students were anti-depressant/anxiety medications. While I was relieved, I was also frustrated because in my mind, that meant that some of my friends must have been taking medications, and no one was saying anything about it to each other. I felt like everyone knew how stressed I was, and they would comfort me, but not share their own struggles. Sometime during those sessions with the counselor, I got the idea that if there was so much unsaid depression and anxiety in the pursuit of the professions that we were so hopeful about, someday I wanted to be a “a dental school counselor” and do for students what I felt like faculty and my counselor did for me. I got the idea, and it never left. I would envision myself in my oce in the dental school, and students coming to me just to talk about what they were going through. And while I would never discount the credentials our counselor had and the help she provided me, I felt that I would be even more of an asset because as a dentist myself, I could relate to what the students were going through. I had walked in their shoes. Thankfully, my father outlived his initial diagnosis by two years. We were lucky that he would go through periods of remission, but ultimately, he lost his battle to cancer three days after I took part II of the NBDE. He passed June 30, and I only had the month of July before summer vacation, so I stayed home with my mom until school started again in the fall. I did y back
13VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Associationto Boston for a couple days that summer. When I got to school, I went straight to one of our operative faculty members, who I am in touch with to this day, and told her the news. She pulled out a chair in her oce, oered me Fiddle Faddle popcorn and we sat and talked.There’s so many more small (but big to me) details of my story that would make this article the length of a novel. But it comes down to I had a bad experience in school and wanted to use my bad experience to pour into other people. I wanted to look out for the people who I thought might be silently struggling. To me, it felt like everyone else was having a grand time in school: having patients who consistently showed, getting their requirements knocked out in a year, meeting their signicant others and getting married. But now, as faculty, talking with students daily, I think there’s a lot of silent suering. I think it’s safe to say most people think that going into academia – particularly clinical full time – is an end-of- career move. We are constantly told we have to keep our hands wet, and while I completely agree, if we continue with that notion, academia will always be an end-of-career move. I think dental schools would benet from more middle career folks who hear the call to academia and accept it. Another reason I wanted to go into academia, and I hope I don’t get “canceled” for this, is I want to help create more dentists like me. I spent the bulk of my years in practice working in Federally Qualied Health Centers serving the underserved. Now that I am at IUSD, I talk to whoever I can, whenever I can, about a career in public health. I would venture to say that dental schools (not just IUSD) are full of clinicians who came from a private practice setting and are able to give plenty of advice about their experience, but very few people do the students have that they can talk to about what a career in public health might look like. The students spend a couple of weeks on their community dentistry rotation, but if there aren’t dentists who worked in centers like that to keep the conversation going, I think the rotation just becomes a fun experience when they got a break from school for a couple weeks. I’ve even talked to students who give wanting to work with the underserved as their motivation to become dentists, only to be swayed by the perceived glamour of private practice. I had a student tell me a couple years ago that one of her classmates said that public health is not “real dentistry.” I have students come talk to me about public health because, as far as they know, they won’t make any money and will live a pauper’s existence. I’ve talked to students who have excellent hand skills and are interested in serving the underserved express hesitation about it because they are told they are “too good” to work in public health. We all realize the importance of having dentists who will serve the underserved, but we don’t have enough people talking positively and from their own experiences to the students about it. So, I am there to talk about it. People often cite the nancial compensation as why they can’t aord to be in academia full time. I would like to gently push back at that and tell you that you can make it work – if you want to. For me, it was worth the pay cut. I did have to sit down and look at my nancials and yes, I had to give up some things, but it was worth it. People always say nd a job you love, and it won’t feel like work. I always thought that was poppycock – until I got to IUSD. The clincher for me came last year. I had recently become one of the clinic directors, and I was chatting with a fourth year student. She said, “being a clinic director is kind of like being a dental school counselor,” and I knew I was where I am supposed to be. I asked my friend and colleagues, Dr. Natalie Lorenzano, who is a full time visiting clinical assistant professor, why she chose a career in academia. “Going into dental academia was more of a calling than a choice. I felt the pull early in dental school that I would want to come back to be a tangible tool to our students and future dentists. It’s important to me to continue to lift up this profession and make sure we are sending competent, holistic and kind people into the eld of dentistry.”Some of you may never hear the call. That’s okay. But some of you may, and you may have it sooner than you think. Don’t feel like you have to have a story fraught with tragedy and frustration like mine to be in academia. Maybe you are one of the people who loved school. I would say come to the school and help create the experiences that made you love it as well. There’s space and need for all of us. About the AuthorDr. Elizabeth Simpson is a Clinical Assistant Professor at IUSD and a clinic director in the Comprehensive Care Clinic. She also serves as chair of the American Dental Association’s Council on Advocacy for Access and Prevention and is an ADA delegate for the Indianapolis District Dental Society.
14 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2A Day in the Life: IUSD Students in Their Own WordsI HAVE BEEN fortunate that in my two years at IUSD, I have gotten to know some wonderful students. I think anyone who works at the school will tell you, getting to know the students is the best part of the job. I asked several students if they would share either a quick outline of a day in their lives or the best and worst parts of dental school in their opinions. I hope that in reading these anecdotes, you will reminisce about your own dental school experience and maybe even become inspired to start working at the school! COVER STORYDr. Elizabeth SimpsonNina Bakshi, D4A day in my life at Indiana University School of Dentistry always starts with saying “hello!” to my fellow classmates, faculty and sta working at the school. After nding where in clinic I will be working, I prepare for my patient to arrive for my morning appointment. One thing I love about learning dentistry alongside all my peers is being able to always cheer on my friends who are also seeing patients at the same time. Watching a friend prepare for a crown delivery in the operatory down the aisle is so exciting! Even though I may be busy with my own patients, I always love that I am somehow a part of my classmates’ initial learning experiences in the eld. After taking lunch, I will return to clinic for my afternoon appointment or work on some of my cases in the laboratory. Working in the laboratory is not my favorite thing to do in dental school, especially for the classes with laboratory components I am taking. I much rather prefer seeing patients and being around people. However, I understand that this is a step in the learning process—and I am grateful for all I have learned! Being a D3 student can be very demanding, but also very rewarding at the same time. Being able to apply all your studying and pre-clinical laboratory work to actual clinical cases makes all the tough times worth it.Dustin Broyles, D4A typical day in the life of a third-year dental student is a rigorous and demanding experience that combines theoretical learning with practical clinical applications. The day begins with lectures covering advanced topics such as prosthodontics, surgical periodontics, and oral surgery. After the morning classes, we transition to the clinic where we engage in hands-on patient care under the supervision of faculty. This involves diagnosing and treating a variety of dental conditions, performing dental procedures, and honing our skills in patient communication and care. The day concludes with studying and preparing for the next day’s clinical responsibilities, creating a well-rounded and immersive educational experience for aspiring dental professionals. Personally, my favorite part of the day is the hands-on clinical experience that we get. Working with real patients allows me to apply the theoretical
15VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationJordyn Caffray, 2024 graduateMy days during my fourth year tend to vary drastically, but most commonly involve an exciting and educational next step in both a patient’s treatment plan and in my experience at IUSD. During our 3rd year, we have a lot of comprehensive oral exams in order to introduce ourselves to our patients and create holistic treatment plans. While this consumed a majority of my third year, it helped me really understand what comprehensive treatment plans looked like and how dierent doctors had dierent philosophies, when it came to treatment planning. As fourth year rolled around, I started picking up speed and saw myself performing comprehensive exams in half the time it used to take me during my D3 year. As I got faster and more condent, the more cases I was able to take on and more experiences I was able to have. Going into my D4 year, I was able to nally start on some denitive restorations and prostheses, after many months of taking my patients out of the disease control phase. My fourth year diered a lot from my third year, and I was excited to start working on bigger projects like dentures, RPDs, bridges, root canals, and implant crowns. With bigger projects and cases came more responsibility and more “after hours” lab work, but I was excited to start the journey which would eventually help me graduate in May.It’s hard to choose a specic “day” that would represent what my life is like normally because every day is extremely dierent, but I would say most days usually involve seeing two to three patients, depending on if there is “evening clinic” and if the patient doesn’t “no-show” their appointment. Normally one to three appointments per week are dedicated to dierent mandatory “rotations” throughout the specialty clinics like oral surgery clinic, pediatric clinic, screening (new patient intake clinic), or emergency clinic. When we are not in rotations, we are able to see our own patients of record in the Fritts Clinic. Depending on what procedure needs to be completed that day, you and your patient will be assigned a certain chair on a certain oor of the Fritts Clinic. And depending on how soon after you need to get your patient back for their next appointment, sometimes chairs are booked for two to three weeks, so it’s extremely important that I stay on top of my scheduling to ll my appointment slots and nish my patient’s care in a timely manner. Another option we have during the week is to do lab work during one of our appointment slots. I normally reserve these for when patients no-show their appointment or if the clinic chairs are full and I can’t book any patients during that time slot. These lab days are super important because most steps for our prosthodontic experiences need to be checked by prosthodontic faculty/calibrated faculty at least two days before the next appointment with the patient. Preliminary casts, custom trays, master casts, wax rims, wax-try-in arches, dies, RPD frameworks, etc. all need to be checked at least two days before the patient is back for their next visit, so staying organized is extremely important and utilizing the lab work days is helpful for when you have to nd the specic faculty who can “check o” each step that needs to be completed. After my appointments are done for the day, depending on if I have any lab work to complete for school, I’ll normally go home, workout, discuss dierent highs and lows from our day with my roommates (who are also D4 dental students), go over patient cases for the next day, cook dinner, and go to bed. If I do have lab work or if I need to practice for our national board knowledge gained in lectures and provides a sense of accomplishment when I successfully complete procedures. Moreover, the patient interactions hone my communication skills and emphasize the human aspect to practicing dentistry. On the other hand, the sheer volume of information can be overwhelming at times, but I recognize the necessity of balancing academics with clinical practice in order to become a well-rounded dental professional. Overall, the third year of dental school is a rollercoaster of challenges and triumphs, which will help shape me into a more condent and competent dental practitioner.
16 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2COVER STORYexams, then I’ll stay at school until 8 or 9:00, when our labs close for the night.This past year has been challenging, fullling, frustrating, and educational, but it has sculpted me into the provider I am today. Even though we aren’t in classes anymore, like during D1 and D2 years, we still have plenty to focus on and stress about like lab work, national boards, applying to residencies, nding jobs, and guring out what life is going to look like after graduation. These past four years have own by and I’m so grateful for my time at IUSD.Hadi Hachem, 2024 graduateFrom the day I got an acceptance email to a normal Tuesday in dental school, I wake up everyday feeling blessed that this is what I get to do for the rest of my life (besides nals). One of my favorite things about dental school has been the clinic aspect where I get to learn in a hands-on manner and build relationships with faculty and patients I work with. However, if I had to pick a downside to dental school it would be the lack of continuity of care in the clinic. I understand that it’s dicult for schools to be able to set up the same doctor with a student to complete a long case such as denture, but it can be strenuous to both the patient and faculty when dierence of opinions can intervene with the process and elongate it. This does, however, allow me to look forward to when I am able to manage patient cases on my own in the near future.
17VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationJose Herrera, 2024 graduateWe mostly see patients all day as we are nishing up requirements. At IU, we are able to schedule for two patients per day, with limited evening clinic where we may see up to three. On certain days, we begin with rounds with our clinical director around 8:00 a.m. Here, we go through case studies and present our clinical patient cases for round table discussions. We then see our rst patients around 9:00. Depending on the procedure, we are usually out by 11:30 where we have roughly an hour to an hour and a half lunch period. During this time, on most days we have speakers come to present and they provide lunches for the students. In the afternoon, we are back in clinic seeing our patients! As a D4, there are a lot of competencies and national board exams to be studying or practicing in lab for. On our down time, such as when a patient cancels, we are in the lab practicing on our dentiforms. This is also a time period where we are all seeking jobs, interviewing, applying for residencies, etc. Despite not having many didactic classes, D4 year denitely keeps us busy! The best part of D4 year is the autonomy that we are given. As long as we are seeing our patients and keeping up with requirements and attendance, we are able to freely schedule when we want to! Another great thing about this year is that we aren’t sitting in lectures anymore. On the ip side, the worse part about D4 year is the busy work. By busy work, I mean the random competencies that we have, case presentations, both written and clinical boards, residency applications and interviews, etc. It denitely becomes stressful despite not having didactic exams anymore! With all that being said, this year has truly prepared me for the everyday life of a dentist, and I am excited for graduation! Tasneem Nada, D2My day starts around 7:45 a.m. I wake up, get ready for school and am usually out the door by 8:30 a.m. I also get in my morning prayer before leaving for school. In a perfect world I would wake up earlier to have breakfast, but usually all I can manage is running out the door with a granola bar and a cup of coee. The morning is lled with lectures from 9-12. From 12-1 we have our lunch break, which I usually spend in the campus center with my childhood best friends who are in school on other IU campuses in Indy. 1:00-4:30 is usually spent in lab or lecture, where we work on our given lab projects for the day. Throughout this time, I will leave for a few minutes to pray my afternoon prayer and get in a snack in an attempt to lessen my hangryness. I usually get home around 4:30-5:00, which is when my sister will come over and we will cook together. My sister is in undergrad at IUPUI, which is pretty convenient for us to spend some time together. We eat dinner and I always spend some time facetiming my parents, talking about our days together. I nish up the night by getting in an hour or two of studying, or if it is an exam week, I will usually spend the rest of the night studying. I try to do something enjoyable before going to bed, something like watch a movie or TV show to stay sane. I then get ready for bed and get ready to do it all again tomorrow!
18 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2COVER STORYDarius Warner, D3Mondays encapsulate the essence of our entire week, commencing at 8 a.m. with Dr. Michelle Kirkup’s discourse on xed prosthodontics, concluding at 10 a.m. We then descend to preclinical lab from 10 a.m. to noon, where we meticulously hone our crown prepping skills for upcoming projects and practical examinations. 12 p.m. to 1 p.m. oers a breather or an opportunity for enrichment through club meetings and lunch and learn sessions. Post-lunch unfolds a systematic approach to dentistry from 1 p.m. to 3 p.m. in Systems Approach to Biomedical Sciences II (SABS), featuring various esteemed professors. Our day reaches its end, as we immerse ourselves in Clinical Application of Cariology and Operative Dentistry I with Drs. Laura and Willis. Our academic day then concludes at 4 p.m., where we are tasked with the choice of studying for our classes or focusing on our preclinical skills. Often our days really end at 9 p.m.—sometimes later for others. The best thing about dental school is getting the opportunity to learn so many dierent skills that will help to later serve the community we work in. The worst thing about dental school would have to be the early start time. This Monday mosaic mirrors the rhythm and substance of our week—a blend of knowledge, skill renement, and camaraderie to which we thank God for the weekends to come!
19VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Association
20 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2Challenges of Academic Life in Dental Schools: A Faculty Perspective on Connecting All the Pieces to SucceedIN THEIR RECENTLY published article, Burns et al.,1 writing in Oceanography, state that academic science is becoming increasingly recognized for fostering a toxic workplace culture. They list reasons including the presence of a hierarchical academic structure, intense competition among faculty, excessive workload expectations, and lack of adequate nancial compensation model. How does this translate to dental schools?The desire to train and practice dentistry often begins early in the life of a future dentist. When listening to applicants who wish to enroll in dental school and subsequently pursue a career in dentistry, a commonly stated line is ‘I was inspired by my dentist, who I used to go to for treatment when I was younger.’ However, the desire to join the dental faculty on a full-time basis is now a more nuanced and challenging option. The focus of this article is to assess the challenges faced by faculty in dental schools and look at the challenges facing them in their roles as educators.The Number of Dental SchoolsIn 1950, there were 42 dental schools in the U.S., with 60 percent of them being aliated with private universities. The number of schools increased to 60 by 1978. In the mid-1970s, the applicant pool started to decline and by 1989, six of the dental schools were closed. However, by 2013, the number schools increased to 64. Currently, in 2023, there are 72 dental schools in the U.S. and 10 in Canada. The number of applicants to dental schools has shown a signicant increase over the years. In 2007-2008, there were 13,742 applicants to dental school in 56 dental schools.2 Based on recent data, there are approximately 11,000 applicants per year seeking admission to dental schools. According to the American Dental Education Association (ADEA), the average dental school acceptance rate in the US is 53.5 percent.2The Number of Faculty in Dental SchoolsWanchek et al.3 reported in 2017 that a total of 12,926 faculty members who were employed at some point during the 2015–16 academic year at 63 schools participated in their survey. This number was broken down into 5,061 full-time faculty members, 5,814 part-time faculty members, and 2,051 volunteer faculty members. Forty-seven schools that reported had at least one vacant budgeted or lost position. While it is not new, it is worth repeating that dental education is facing a faculty workforce shortage. This has become more acute in the post COVID 19 pandemic phase that we currently occupy. Ramications for the future includes signicant impediments to institutional growth and innovation. Dr. Priya ThomasDr. Monica GibsonDr. Chandni BatraDr. Hawra AlQallafCOVER STORYDr. Neetha SantoshDr. Celine CorneliusDr. Halide NamliDr. Vanchit John
21VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationIn 2006, ADEA started a program titled, ‘Academic Dental Careers Fellowship Program’ (ADCFP).4 The goal of the program was to engage faculty members by providing them with tools to help them teach and mentor dental students and allied dental students. Additionally, the intent was to help faculty develop their academic careers plans with the goal of being successful as academics. Faculty members were also provided with tools to mentor dental students interested in academic life as a future career. Additionally, in 2006,5 110 faculty members at 10 dierent dental schools were interviewed by dental students who were participating as ADCFP fellows. Sixty-nine (63 percent of the total) of these interviews were reviewed and analyzed. Positively inuencing factors on the quality of the academic work environment and career satisfaction included mentorship and student interaction, opportunities for scholarship, job diversity, intellectual challenge, satisfaction with the nature of academic work, lifestyle/family compatibility, exibility, lifelong learning, professional duty and lab responsibility. Negative factors identied were bureaucracy/administrative burdens and barriers, time commitment, nancial frustration, political frustration, lack of mentorship, required research emphasis, lack of teaching skills development, student engagement, isolation, and funding uncertainty.In 2007, Haden et al.6 reported on the ‘quality of dental faculty work life.’ The study was designed to evaluate faculty perceptions and recommendations related to their work environment, job satisfaction and dissatisfaction, and professional development needs. They had a total 1,748 responses from 49 U.S. dental schools. The total number of respondents constituted 17 percent of all U.S. dental school faculty. Data analysis showed that most faculty members reported being very satised to satised with their dental school overall and with their department as a place to work. However, tenured associate professors reported the highest level of dissatisfaction. In 2011, John et al.7 reported the need for dental schools to develop creative solutions to help recruit, develop, and mentor faculty members. Encouraging dental students to consider academic careers through a ‘grow our own’ plan was discussed among other ideas to help with recruitment and retention of dental faculty. Murdoch-Kinch et al.8 in 2017, in their climate study for faculty, sta and students looked at humanistic environment, learning environment, diversity and inclusion, microaggressions and bullying, and activities and space at the University of Michigan School of Dentistry. Findings indicated that the majority (76 percent faculty, 67 percent sta, 80 percent students) agreed that the environment fostered learning and personal growth and that a humanistic environment was important (97 percent faculty, 95 percent sta, 94 percent students). However, microaggressions or bullying was reported by all groups surveyed. Recommendations made from the ndings included working on cultural sensitivity training, adding courses for interpersonal skills, leadership, and team-building eorts, addressing microaggressions and bullying, creating opportunities for collaboration and increasing diversity of faculty, sta and students.In the ADEA Climate Study9 conducted in 2022, a total of 66 schools (58 U.S. and eight Canadian) participated with responses recorded for faculty, sta, administrators, and students. Sixty-four percent of the participants reported that they agreed or strongly agreed that they were satised with the climate at their dental school. Experiences varied depending upon the participant’s location, role, and social identity group.Based on a brief review of the literature along with feedback from the authors of this article, dental faculty have faced several challenges for many years. Faculty responses to dierent questionnaires over the years have indicated an overall satisfaction with their work and their views on academic life in dental schools. However, the feedback
22 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2responses have also indicated several negatives as well. Dental education has become a more complex enterprise. The rising cost of dental education, increased expectations of students along with increased expectations from faculty combined with more challenging faculty to student ratios has taken its toll on faculty, especially the full-time faculty. Effects of the COVID-19 Pandemic on Dental Faculty The global pandemic brought with it signicant changes to life as we know it. Dental education and dental practices had to make changes to continue to provide a safe learning environment for their students and quality care for their patients. Several studies reported on the eects of the pandemic on dental students and sta. However, very few studies have reported on the eects of the pandemic on dental faculty. Smith et al.10 reported on their ndings from dental school faculty from four U.S. dental schools. They self-reported burnout, loneliness and resilience during a one-month period in 2020. Social isolation, new or increased home care responsibilities, and/or nancial hardship along with cancellation of socialization with colleagues at holiday, retirement and welcome celebrations contributed to rates of burnout and loneliness that were higher than the public at large. This added exponentially to the pre-pandemic reported burnout triggers that included academic administrative responsibilities, pursuit of grants and funding, and research. Smith et al.9 also reported that the older respondents, were less likely to report burnout symptoms. These ndings don’t auger well if they are more generalizable as there is currently and is going to be future an increase in retirements of more experienced and seasoned faculty members nationwide. The ndings from the study also indicated, that faculty living alone scored three times higher on the loneliness scale than the group mean. Loneliness was dened as a gap—between the interaction we want to have with others and the interaction we get. As the “graying” of the dental faculty continues, dental schools need to increase their focus on faculty along with providing them with options and support for health and wellness. Arnett et al.,11 in their 2022 study on the Impact of COVID-19 on dental hygiene educators, reported that personal and work-related burnout was signicantly higher for administrator/program directors and full-time faculty compared to part-time didactic and clinical faculty. Emotional exhaustion from personal burnout was positively related to work-related and burnout working with students. Other factors included work-life imbalances, a lack of support, and a shift to hybrid/online learning. Based on the dearth of studies relating to the eects of the pandemic especially in the current post pandemic phase, more work is needed in understanding faculty perceptions of academic life. Ramications going forward will be more critical as there are more dental schools in 2023-2024 compared to prior decades. This combined with increased enrollment of students, will increase the challenges for faculty and their decision to choose a career as a dental educator. Where We Are in 2024As the cost of dental education has increased exponentially, it has become more challenging for young dentists to consider a full-time career in dental education. Graduating dentists usually have a substantial debt load that they need to deal with while trying to establish their careers. Remuneration of the faculty combined with tight budgets of dental schools has made a full-time academic career a distant choice for most dentists. For schools, nding qualied educators who are willing to teach while taking on COVER STORY
23VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Associationthe complexities of becoming full-time educators has become a big challenge. The process of becoming a dental educator is a slow and deliberate journey. Learning to teach requires training. There are many learning options provided by the American Dental Educators Association (ADEA). However, nding time to attend these training sessions combined with the costs of travel and lodging often in locations away from one’s home base means nancial challenges are always going to be present. Finally, with the increase in the dierent and new forms of available technology, faculty must train and retrain to keep up with all these innovations. This is not always exciting to the older faculty, who may choose not to retrain or are not comfortable learning more about new technological options. This can increase tension among faculty and administrators leading to discontent. Learning to become a dental educator while keeping up with new forms of technology, along with dealing with the stresses of working with students and their expectations has increased the challenges that academicians face today. In reviewing the literature, the problems faced by full-time academics is not new. The challenges have persisted through the decades and have become more urgent in 2024. Opening more dental schools, increasing student enrollment in existing dental schools while dealing with the ramications of the pandemic on educators has made of the issue of faculty recruitment and retention more challenging. Dental administrators and other decision makers will need to have a blueprint going forward in 2024 and beyond to ensure that dental students get the best education possible, patients get the best treatment options for their care, while faculty and sta issues are addressed as eectively as they can be. Perhaps dental education is at the crossroads again. In 2024, the need to nd solutions to get the beyond the crossroads is going to be paramount.References1. Burns JHR, Kapono CA, Pascoe KH, Kane HH. Spotlight-The Culture of Science in Academia Is Overdue for Change. Oceanography, 2024, Vol 36 (4).2. Wancheck T, Cook BJ, Valachovic R. U.S. Dental School Applicants and Enrollees, 2016 Entering Class. J Dent Educ, Vol 81 (11) 2017, 1373-1382.3. Wancheck T, Cook BJ, Slapar F, Valachovic RW. Dental Schools Vacant Budgeted Faculty Positions, Academic Year 2015-16 J Dent Educ, 2017, Vol 81 (8), 1033-1043.4. ADEA Academic Dental Careers Fellowship Program (ADEA, ADCFP) https://www.adea.org/dentalfellow/ 5. Roger JM, Wehmeyer MH, Matthews S et al.. Reections on Academic Careers by Current Dental School Faculty. J Dent Educ, 2008, Volume 72, (4), 448-457.6. Haden NK, Hendricson W, Ranney RR et al.. The Quality of Dental Faculty Work-Life: Report on the 2007 Dental School Faculty Work Environment Survey. J Dent Educ, 2008, Vol 72(5), 514-531.7. John V, Papageorge M, Jahangiri L et al.. Recruitment, Development, and Retention of Dental Faculty in a Changing Environment. J Dent Educ, 2011, Vol 75(1), 82-89.8. Murdoch-Kinch CA, Du RE, Ramaswamy V et al.. Climate Study of the Learning Environment for Faculty, Sta, and Students at a U.S. Dental School: Foundation for Culture Change. J Dent Educ, 2017, Vol 81 (10), 1153-1163.9. ADEA Climate Study- https://www.adea.org/climatestudy/ 10. Smith CS, Kennedy E, Quick K et al.. Dental faculty well-being amid COVID-19 in fall 2020: A multi-site measure of burnout, loneliness, and resilience. J Dent Educ, 2022, Vol 86(4), 406-415.11. Arnett MC, Ramaswamy V, Exan MD, Rulli D. J Dent Educ, 2022, Vol86(7), 781-791.See page 35 for author information
24 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2The State of Dental Curricula: Are We Preparing Students for Today’s Practice and Academic Life?DENTAL EDUCATION APPEARS to have arrived at another crossroads. The challenges laid out in the 1995 publication, Dental Education at the Crossroads,1 persists with the addition of many more in 2024. The challenge of attracting high caliber educators has become more intense over the past several decades. This has been magnied by economics, namely the high cost of dental education, leaving graduates with high debt. This has signicantly reduced the number of candidates applying for full-time faculty positions. The lucrative, albeit stressful nature of dental practice has seen fewer and fewer graduates considering a full-time career in dental education.Additionally, the greying of dental educators and subsequent retirement of the more seasoned faculty that is taking place, is putting considerable stress on the younger dental faculty due to a signicant increase in the demands on their time setting the stage for academic burnout. The global pandemic that was COVID-19 and the subsequent challenges that were faced by dental school globally, has put another crimp in the quality of full-time faculty life. Doing more with less, is not an ideal situation in dental education which is a very hands-on task. This article looks at dental curricula and the challenges faced in implementing a contemporary curriculum in dental schools. A Brief Look at the History of Curricular DevelopmentA curriculum has been dened as the subjects comprising a course of study in a school or college. While the origins of dental education may lie in the works of the ancient Middle Eastern and Asian writers who recorded explanations, descriptions, and advice, about oral health problems, formal or institutional dental education began in the United States in 1840 when the state of Maryland chartered the Baltimore College of Dental Surgery. The nineteenth century saw debate on locating dental schools and dental education within a medical school or in independent schools. Between 1865 and 1870, ve new dental schools were founded. By 1884, 12 additional schools had been founded: Nine university-based programs and three freestanding schools. During the 1880s and 1890s, several freestanding for-prot schools were founded in the United States. The state of Illinois led the way, where between 1883 and 1902, 28 dental schools were started. By 1900, there were 57 dental schools in the country. However, as noted by William J Gies, “Some of the dental schools of this period were busy diploma mills, which were created under the sanction of indierent state laws, conducted with the collusion of unworthy dentists, and protected by unfaithful practitioners in posts of public responsibility, freely sold the degree of Doctor of Dental Surgery at home and abroad, and led to the disgrace of the profession and to the dishonor of dental education. Many of the dental schools that were chartered since 1884 have been completely worthless.”1 Abraham Flexner’s 1910 study of medical education was a landmark event. The Flexner report2 still helps guide medical—and dental—school curricula all these years later. In 1926, the Gies Report3 on Dental Education was published, which was a seminal event for the history of formal dental education in the U.S. Dr. Chandni BatraDr. Celine CorneliusDr. Monica GibsonDr. Hawra AlQallafCOVER STORYDr. Priya ThomasDr. Halide NamliDr. Neetha SantoshDr. Vanchit John
25VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationThis report concluded:31. That dentistry be an independent division of health services.2. Teaching and research in dental school should be of a very high standard as should be the status of dental educators.3. The preparatory education needed prior to dental school should be equivalent to that of physicians.4. The curriculum for dental students should require intensive training for a career as a general practitioner.5. Specialization should require an optional year following the completion of the formal dental curriculum. So, where do we stand in 2024?The Dental CurriculumThe mission of dental education and dental schools is rst to develop future practitioners. These goals can be broadly stated as being focused on (1) educating dental students to serve their patients and communities in which they live and work and (2) to help prepare students in becoming lifelong learners. Dental education is focused on being scientically based, clinically relevant, medically informed, and socially responsible. To this list, we now add, technologically advanced. (Figure 1)The ChallengesIt is often stated that it is easier to move a cemetery than it is to change a curriculum. Much of this is a result of human nature, namely, it is dicult for us as humans to change and to embrace change because change is not easy. However, as was evidenced during the global pandemic, dental educators had to go from a traditional classroom and lab-based education to an almost completely virtual form of education in a very short period. It took a lot of bold thinking and planning in warp speed to make this change happen, suggesting that change is possible but requires clear and precise leadership to help achieve the desired outcome. In looking at the criticisms of dental curricula,1 we can group them into ve broad area of concern. These include:1. A weak linking of basic science concepts and methods, which are usually taught in Year 1 and Year 2 of the dental curriculum, to the students’ clinical education and experience, which is traditionally focused in Year 3 and Year 4. 2. The curriculum is often slow to adapt to current and emerging dental science and practice. 3. Implementing comprehensive patient care in dental schools has its limitations due to physically structures of dental schools and their clinical facilities and the often-recognized siloed nature of dental education. 4. Aspirational but weak linkages between dentistry and medicine.5. The dental curriculum, which is recognized as being overcrowded, makes it hard for students to learn concepts, while developing critical thinking skills in preparation for lifelong learning.Rebalancing an Overcrowded CurriculumAs scientic knowledge has increased exponentially over the last century, dental curricula have become overcrowded as more has been added to every hour spent in dental school as a student. Peter Densen in his monograph stated, ‘It is estimated that the doubling time of medical knowledge in 1950 was 50 years; in 1980, 7 years; and in 2010, 3.5 years. In 2020 it is projected to be 0.2 years—just 73 days. Students who began medical school in the autumn of 2010 will experience approximately three doublings in knowledge by the time they complete the minimum length of training (7 years) needed to practice medicine. Students who graduate in 2020 will experience four doublings in knowledge. What was learned in the rst three years of medical school will be just 6 percent of what is known at the end of the decade from 2010 to 2020. Knowledge is expanding faster than our ability to assimilate and apply it eectively, and this is as true in education and patient care as it is in research. Fundamental change has become an imperative.’4 Dental curricula face similar struggles as dental educators try and incorporate more into the curriculum as they try and keep up with all the new knowledge that is presenting itself daily. Figure 1: A snapshot of the various learning modules in a dental curriculum
26 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2In trying to make curricular change, challenges revolve around the cost and the feasibility of obtaining data, that help (1) identify courses that have overlapping material; (2) correlating the emphases in clinical education with that of contemporary dental practice; and (3) documenting the eectiveness of newer educational strategies. This brings us back to shortages of faculty trained to participate in new teaching methods while incorporating new technologies available for patient care.Curriculum at the Indiana University School of DentistryThe Indiana University School of Dentistry was among earliest dental schools established in the nation, when it began as the Indiana Dental College in 1879. Having been acquired by Indiana University in 1925, it has maintained its reputation as being among the better dental schools in the country. The school has experienced curricular changes and challenges across the years just as every other dental school in the country. Finding place in the curriculum to make introductions of new courses, upgrading existing courses while trying to decompress the curriculum has met with varying degrees of success. Additionally, with most of the faculty multi-tasking, nding change leaders is not an easy task. In the publication, Dental Education at the Crossroads: Challenges and Change,1 several key indicators of oral health status were reviewed, oral health goals outlined, while the implications for education were discussed and major curriculum concerns were highlighted. In reviewing the suggestions made for change, almost 30 years ago, many of the suggestions continue to be valid areas for review in 2024. Recommendations from Dental Education at the Crossroads1 as Applicable to Education at IUSDThe following recommendations were made with an emphasis on curricular reform and clinical experience in ecient practice settings:1 A. To stimulate progress toward curriculum goals, the committee recommends that dental schools set explicit targets, procedures, and timetables for modernizing courses, eliminating marginally useful and redundant course content, and reducing excessive course loads. This has been and continues to be a focus at IUSD.COVER STORYi. Designing an integrated basic and clinical science curriculum providing clinically relevant education in the basic sciences and scientically based education in clinical care. The curriculum and assessment committee at IUSD has worked hard at making this recommendation a reality. Integration of biomedical and clinical sciences has been emphasized over the past ve years and more allowing for better integration of the pre-clinical and clinical learning experiences. ii. Incorporating all educational activities with a focus on outcomes and an emphasis on the relevance of scientic knowledge and thinking to clinical choices. IUSD has been more focused on evidence-based education while stepping away from the “expert focused learning” to research and data-based learning and application of treatment choices.iii. A shift of more curriculum hours from lectures to seminars and other active learning strategies that develop critical thinking and problem-solving skills. Faculty at IUSD now use ‘case-based learning’ incorporating learning the fundamental skills of developing a diagnosis, a prognosis and treatment planning and then when shifted to the clinical setting, performing treatment. Critical thinking and problem-solving skills are being implemented and modied on a regular basis.iv. Complement clinic hours with scheduled time for discussion of specic diagnosis, planning, and treatment-completion issues that arise in clinic sessions. Dierent learning modules that incorporate group learning strategies with content experts, integration of biomedical and clinical learning in one module along with grand rounds and formal emergency drills have introduced welcome change to the curriculum.
27VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationB. To prepare students and faculty for an environment that will demand increasing eciency, accountability, and evidence of eectiveness, a change in the traditional discipline based clinical set up in dental schools to a more a comprehensive clinic model was recommended.i. Developing a patient-centered, comprehensive care clinical facility. This has been incorporated in the IUSD clinics since the early 1990’s. However, changes in the clinical structure through a new clinical building, pandemic related issues as they refer to faculty availability has made more change necessary as students see their patients in the clinics. ii. Teamwork and cost-eective use of well-trained allied dental personnel are stressed. This has been stressed at dental schools in general. At IUSD, we work closely with the allied programs and their faculty and seek their expertise especially in Periodontology. However, as an outcome of the global pandemic, availability of faculty, sta and other support personnel has made this outcome more challenging. iii. Evaluations of practice patterns and of the outcomes to improve both the quality and the eciency of such care. Regular interactions through student feedback, patient feedback, sta and faculty feedback allow for a dynamic state of clinical care where change can be incorporated in a rapid manner.iv. General dentists serve as role models in the appropriate treatment and referral of patients needing advanced therapies. This is the overall model of education at most dental schools including IUSD. However, specialists are also present on the pre-doctoral clinic oor either daily or on a consultation-based interaction. So where do we go from here?The Future of Dental Education and Dental CurriculaIn assessing the history of dentistry from its very early origins to where we are in 2024, there have been seismic changes to how dentistry and dental education have advanced over the many millennia. However, to stay contemporary and keep either alongside with or abreast of all the changes happening with technological advancements and treatment options today, dental schools and the dental curricula must: 1. Continue to maintain a symbiotic relationship with technological advancements. Training students in the use of virtual reality simulations, digital imaging, 3D printing, and digital tools like intraoral scanners is now mandatory. These dierent technological advancements enhance diagnostic capabilities, treatment planning, and patient management. Accordingly, recruiting faculty with expertise in the use of the dierent technological options will be critical. This will require a change in the compensation structure for future faculty hires.2. Integrated curricular instruction as opposed to individual discipline teaching to prepare students for the integrated national board dental examination. 3. Transitioning to a more patient-centered approach, while focusing on holistic care of the patient. Personalized treatment plans that oer compassionate care for patients while making sure that dental students acquire these skills is very important. 4. Continued development of an interprofessional education model, with dental students learning with their contemporaries from other healthcare elds, in medicine, nursing, and pharmacy. There have been several schools including IUSD, working on such models of education. A deeper dive into the collaborative inter-professional model will serve the profession well. Dental schools must nd ways to adapt their curricula to embrace this form of education more comprehensively going forward.5. Emphasizing evidence-based dental education and practice should continue to be emphasized. Developing critical thinking skills of the students through specically designed learning modules must be a focus.6. Emphasizing preventive care while promoting oral health should take center stage. Dental education must highlight oral hygiene practices, while also increasing the footprint on the role of diet and nutrition, along with lifestyle changes needed for our patients. Accordingly, a well-dened patient education module to be used in the dental clinics should be made available to dental students. 7. Dental education should continue to focus on ethical and professional conduct. Using case studies from the American College of Dentists could help with ready made modules in this area. Continued on page 28
28 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 28. Fostering a culture of curiosity and lifelong learning should be created in all dental schools. This requires a faculty body that is enthusiastic about the profession while also being skilled at teaching and while enhancing their commitment to dental education for the future. 9. Finally, establishing an emphasis on mental health of the students, sta and faculty in dental schools is very important. The global pandemic has highlighted the need for more support being oered in dental schools to address mental health of all its personnel. This should continue to be a focus in 2024 and beyond.In conclusion, dentistry and dental education has come a long way. Technological advances continue to push the envelope forward making it hard for dental schools and dental curricula to stay contemporary. There are many challenges present and these have been highlighted. However, it is critical that dental schools and their curricula keep up with all the changes taking place in science and medicine and in clinical practice. Training the dentists of the future, will require a group eort from dental educators, the alumni, and the practicing dental community. It will be important that dental schools continue to work closely with COVER STORYorganized dentistry, keep up with advances in dental and medical research while also seeking funding from industry to make sure that dental curricula stay contemporary and dental students of the present and the future are best prepared to ourish in the profession of dentistry. References1. Dental Education at the Crossroads: Challenges and Change. Institute of Medicine (US) Committee on the Future of Dental Education; Field MJ, editor. Washington (DC): National Academies Press (US); 1995.2. Stahnisch FW, Verhoef M. The Flexner Report of 1910 and Its Impact on Complementary and Alternative Medicine and Psychiatry in North America in the 20th Century. Evid Based Complement Alternat Med. 2012; 2012: 647896.3. Gies WJ. Dental Education in the United States and Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. 1926.4. Densen P. Challenges and opportunities facing medical education. TRANSACTIONS OF THE AMERICAN CLINICAL AND CLIMATOLOGICAL ASSOCIATION, VOL. 122, 2011, 48-58.See page 35 for author information
29VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Association
30 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2COVER STORYMental Health: A Review of Dental Schools and their Mental Health Initiatives for Dental StudentsABSTRACT: This article provides an insight into the mental health initiatives within dental schools, aiming to understand the current landscape, challenges, and innovations in promoting the mental well-being of dental students. Recognizing the unique stressors associated with dental education, the article explores various strategies employed by dental schools to support the mental health of their students. Additionally, this article discusses the importance of fostering a positive learning environment and the role of mental health initiatives in enhancing overall student success.IntroductionStress has been dened as the biological reaction to any adverse internal or external stimuli.1 Stress is handled dierently by dierent groups of people. Many recent studies have reported on a worrying trend in the mental health challenges faced by dental students and practicing dentists. The increase in stress in the profession, the high prevalence of anxiety among dental students and the impact of the COVID-19 pandemic on mental health of students have all highlighted the necessity of addressing mental well-being in the dental community.2 Several factors that contribute to the mental health challenges among the dental students including the pressure to excel academically, emotional, and physical fatigue, mounting educational loans and the innate stress of patient care.3 The fact that there is an ethical and legal obligation to be physically and mentally t to practice adds an additional layer of accountability for oral health professionals.4 A multi-faceted approach is recommended to address the mental health challenges in the dental profession which should include education and awareness of the issues faced by the students, the provision of resources on stress management, resilience and seeking help when needed.5 This issue has worsened with several new challenges being faced by dental schools in a post COVID-19 environment. These include:Lack of Support: There has been a signicant reduction in the academic dental workforce reducing the sta to student ratio and the faculty to student ratio that helps provide support in these situations. This reduced support is not isolated to only a few dental schools but felt across the country. Changing learning environments: Students have had to adapt to changing curriculum designs including an online or hybrid learning environments that can be isolating to some students. Post COVID-19 Fatigue: Educational institutions across U.S. are facing faculty and student fatigue in a post COVID-19 environment despite active measures taken to improve the engagement at both levels.However, many educational institutions have implemented measures like accessibility to mental health support services and policies to reduce the stigma surrounding mental health issues to address this predicament and to create a supportive and understanding environment. Poor mental health and wellbeing can signicantly aect the dental students’ decision-making abilities and educational performance that can have a long-lasting impact on patient care during their educational journey and beyond. This can also negatively impact workforce sustainability. To combat these complex issues and to reduce the mental health burden during Dr. Monica Gibson Dr. Celine CorneliusDr. Neetha SantoshDr. Hawra AlQallafDr. Chandni BatraDr. Halide NamliDr. Priya ThomasDr. Vanchit John
31VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Associationdental education, all dental schools are heavily invested in strategies to minimize mental health issues among their students. These eorts are categorized into three levels: primary prevention, secondary prevention, and tertiary prevention.6 A denition for each intervention/prevention level is listed in Figure 1. Each level in turn places separate but related responsibilities on both the individual and the environment they operate in. Primary Prevention StrategiesPrimary prevention strategies are often the strongest method for cultural change. A shift from punitive grading to an evaluation system that allows for growth in the dental students’ education journey is timely. Eective and daily evaluations that allow students to realize their deciencies and allow for course correction instead of only high stakes end of term examinations are great strategies towards primary prevention of mental health issues. A punitive approach to an error versus a learning from our experience and problem-based learning strategies allow dental students to move from defensive behaviors to potentially behavior that encourage learning and growth. Secondary Prevention StrategiesSecondary preventive strategies are great adjuncts to the primary change strategies but cannot be the sole method to tackle mental health and stress related issues. Some of these include faculty training and sta education to recognize the signs of stress and provide a supportive learning environment to the students. Integrating wellness and mindfulness components in the educational curriculum helps students develop habits that promote mental and emotional well-being. Dental schools are also implementing stress management programs that focus on building resilience, time management, and eective coping mechanisms to navigate the pressures of dental education. Tertiary Prevention StrategiesThese include various counseling services, emotional support and coping strategies for students facing mental health challenges. Dental schools are also establishing peer support networks, creating a sense of community among students, and encouraging open communication about mental health. Although secondary and tertiary level strategies have a signicant role to play in the prevention and management of mental health issues, they cannot be used as sole strategies in this complex problem. Primary methods to reduce stress in dental education remains the key initiative that should be utilized in dental schools. An Evolving Process—Steps to ConsiderSome key steps to consider regarding the mental health of dental students include: Academic pressure and clinical demands: As already stated, dental school involves a rigorous curriculum with a signicant amount of coursework, exams, and clinical requirements. Academic pressure can be intense, leading to stress and anxiety. Teaching students eective time management strategies along with coaching to develop better study habits and organization skills can help students cope with academic demands. Faculty mentors and guides who have been through the process before are an invaluable resource. However, faculty development sessions to select the best qualied faculty to serve as guides must be strategically planned. Making sure that students are aware of all available resources in dental schools while encouraging them to seek guidance from mentors or faculty can help alleviate some of the stress.Balancing Personal and Academic Life and Stress Management—A Focus on Self Care: Maintaining a healthy work-life balance is a fundamental requirement to lead a healthy lifestyle. However, arriving at a healthy work-life Figure 1: Levels of intervention for prevention of mental health and wellbeing issues. Adapted from Cooper C L, Cartwright S. An intervention strategy for workplace stress. J Psychosom Res 1997; 43: 7-16.
32 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2balance can be a challenge. Finding time for self-care, relaxation, and maintaining social connections is crucial for overall well-being. This was disrupted signicantly during the pandemic. Self-care includes getting enough sleep, eating well, and engaging in activities that bring joy and relaxation. Setting realistic expectations and understanding that it’s okay to ask for help are crucial components of self-care. Developing eective stress management techniques, such as exercise, mindfulness, and relaxation exercises, can help mitigate the impact of stress on mental health.Identifying signs of Mental Health issues and Seeking Support: The stigma of seeking help because of mental health issues continues to be prevalent in modern society. However, becoming aware of signs of mental health issues, such as anxiety or depression, is crucial. Early identication and seeking appropriate help can prevent more serious problems from developing. It’s important for dental students to be aware of the support systems available to them. This may include counseling services provided by the school, peer support groups, or seeking assistance from mental health professionals. Establishing a network of friends and mentors within the dental school community can provide valuable emotional support. Initiatives at the Indiana University School of DentistrySome notable examples of the strategies developed and being developed at the Indiana University School of Dentistry (IUSD) include:IUSD’s Oce of Academic Aairs and Education, and Oce of Student Aairs: At IUSD, students present to the oce of student aairs with all types of issues/concerns including, academic challenges, nancial struggles, personal/relationship struggles, medical diagnosis, life balancing issues, feelings of failure, impostor syndrome, depression, anxiety, learning challenges and more. Faculty and sta in these oces, as noted above, play a crucial role in providing support for students. These oce professionals guide students and address academic concerns and help address their concerns and seek appropriate referrals for them. Regular check-ins help students stay on track and make informed decisions about their academic success. These oces have an early alert system that identies students who may be struggling academically. This allows for timely intervention, with course directors providing additional assistance and resources. IUSD also has a system in place to provide academic accommodations to students who need extended time and a quiet room to take examinations. These initiatives are designed to assist students dealing with anxiety in taking exams in a calm and supportive environment. Moreover, peer mentoring and study guide programs implemented help to facilitate mentoring newcomers by experienced upperclassmen. Peer mentors oer guidance on academic matters, share study tips, and provide a supportive connection for navigating the academic environment. Additionally, the Oce of Clinical Aairs works with clinic directors to identify third- and fourth-year students who are struggling with mental health issues and directs them to the Oce of Student Aairs to provide them with the available resources. It has been observed that the number of students experiencing mental health issues over the past few years has increased signicantly. A concerted eort has been made to identify and provide early intervention to students in need.The Oce of Diversity, Equity, Inclusion, and Belonging spearheads the fostering of a humanistic, inclusive, and interprofessional learning environment that in turn promotes the overall mental health and well-being of the students. Through its initiatives, the oce actively promotes an environment where students from various backgrounds feel valued, respected, and supported in their academic pursuits. This commitment to diversity and inclusion extends beyond mere representation, aiming to create a sense of belonging for every student. The interprofessional learning environment fostered by the oce encourages collaboration and understanding among students from COVER STORY
33VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Associationdierent cultural backgrounds. This collaborative approach not only enhances the academic experience but also contributes to a supportive community that values the unique perspectives each student brings. The oce’s recent initiative involves providing comprehensive information about the various holidays celebrated by diverse religions and nationalities. Additionally, IUSD also has a plethora of local chapters of national dental student organizations such as American Student Dental Association, American Association for Women Dentists (AAWD), American Dental Education Association, and a variety of student specic organizations such as Christian Dental Association and Global Service-Learning Group. These student organizations provide a sense of community and peer support. Being part of a group with shared experiences creates a network where students can openly discuss challenges, share coping strategies, and provide emotional support to one another. Additionally, they oer mentorship programs where upperclassmen and women or experienced dental professionals guide newer students. These mentoring relationships can serve as valuable sources of advice, encouragement, and understanding, contributing positively to mental well-being. These local chapters often conduct talks focused on mental health awareness, stress management, and overall well-being along with many other fun-lled programs. Hosting social events and recreational activities such as Saturday Strolls organized by AAWD can help dental students relax and bond outside the academic setting. These encouraging social interactions contribute to a supportive and enjoyable atmosphere, positively impacting mental health.In tandem with these organized activities, the Student Wellness Coalition at IUSD arranges a weekly yoga session, fostering a dedicated space for students to engage in physical activity and enhance exibility. This initiative not only supports physical well-being but also serves as a valuable outlet for stress relief, contributing to improved mental health and the cultivation of a sense of community and support among students. Additionally, a National Board-Certied Health/Wellness Coach leads a Monday Mindfulness session each week. This session, which is open to faculty, sta, and students, aims to instill a more mindful and balanced environment by incorporating mind-body tools for relaxation, focus, and renewal. Furthermore, there is a monthly program where therapy dogs visit the IUSD library. Interaction with a therapy dog creates a non-judgmental safe space that provides emotional support, mental break, and mood enhancement.Collectively, these eorts underscore a commitment to addressing various dimensions of well-being, encompassing physical health, mental resilience, and the cultivation of a supportive community at IUSD.Providing Accommodations The term “accommodations” is used to describe an alteration of environment, curriculum format, or equipment that allows an individual with a disability to gain access to content and/or complete assigned tasks. An accommodation is an adjustment and/or aid provided to enable a student with a disability to have access to education equivalent with their peers. The purpose is to ensure that all students have an equal opportunity for success. They allow students with disabilities to pursue a regular course of study. Since accommodations do not alter what is being taught, instructors should be able to implement the same grading scale for students with disabilities as they do for students without disabilities. Some of the accommodations provided at IUSD for students who have been tested and assessed to need accommodations include, extended testing time, quiet testing locations, help through the role of tutors as well as working with the oce of adaptive services on campus to provide and implement the recommended accommodations for the students that need them. Initiatives at the Dental College of Georgia, Augusta University Eorts are being made at the Dental College of Georgia (DCG), Augusta University, to actively address the mental health challenges faced by students, faculty, and sta. Administrative bodies like the oce of Student Aairs and Academic Aairs are proactively involved in guiding students through their academic journey with timely interventions to identify and address mental health issues at an early stage. This helps foster a supportive and inclusive environment in a high-stress setting. The DCG also oers academic accommodations, such as extended time and quiet rooms for examination for students that seek the service, and this allowance helps create a conducive environment for academic success. Despite the academic support, the DCG recognizes the importance of well-being by celebrating occasions like the world mental health day with stress-relieving activities like music, massages and therapy dogs which contributes to destigmatizing mental health issues. Community
34 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2activities like book clubs, kayaking, golf tournaments, marathons, annual Friendsgiving, and gatherings for various multicultural events are facilitated by organizations like the Augusta University chapters of AAWD, ASDA, Dental Multicultural Association, SNDA and Christian Medical & Dental Associations. These events contribute to building a sense of fellowship and fostering social connections. This approach recognizes the importance of both academic and non-academic factors in the well-being of students and sta. By implementing these programs and activities, educational institutions across the country are not only addressing the immediate mental health needs but also contributes to the creation of a positive and supportive culture. It’s crucial to continue these eorts, periodically evaluate their eectiveness and explore new ways to enhance the mental health and well-being of the students. By encouraging a culture that supports mental health and providing accessible resources, the oral health community can contribute to the overall well-being of its members, enhance job satisfaction, and improve the quality of patient care. It is an ongoing process that requires collaboration, awareness, and a commitment to the holistic health of everyone in the profession. Recommendations In discussion with the front-line support personnel that work with dental students who present with challenges, the following recommendations are made to help foster better learning and life experiences for dental students while in dental school. The recommendations include:• Review of the existing dental curricula while ndings ways to decompress these curricula, working closely with the oce of student aairs.• Building a culture in dental schools where students are encouraged to ask for help and are supported when they do. Being mindful that high achieving students have often not asked for assistance in their previous academic pursuits and often feel ashamed and intimi-dated to begin to ask for help at the professional school level.• Allow students multiple ways to demonstrate their knowledge. Semester nal exams week can be bet-ter structured and broken up and scheduled over the course of one to two weeks instead of all the exams being scheduled in one week as they are high stakes exams.COVER STORY• Be transparent with students regarding class/clinic expectations. Make sure students fully understand the requirements and the risks if they do not meet the requirements.• Provide outreach and support as soon as a student shows signs of academic challenges.• Finally, work to foster a truly collaborative approach that involves input from students, faculty, and sta. Conclusion As the landscape of mental health awareness evolves, dental schools must continue to adapt and rene their initiatives oered to dental students. Several strong strides have been made in innovative approaches including creative use of technology, partnerships with mental health organizations, and novel curriculum designs that prioritize student well-being. In conclusion, dental schools play a crucial role in fostering and supporting the mental health of their students. By implementing comprehensive mental health initiatives, addressing challenges, and embracing innovative approaches, dental education can become a model for promoting holistic well-being withing the healthcare profession. This article encourages the ongoing dialogue and collaboration among all the personnel in dental schools to ensure that mental health remains a priority in dental education now and in the future. References1. Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull. 2004 May;130(3):355-91. doi: 10.1037/0033-2909.130.3.355. PMID: 15122924.2. Loch, Carolina, et al. “COVID‐19 and dental clinical practice: Students and clinical sta perceptions of health risks and educational impact.” Journal of Dental Education 85.1 (2021): 44-52.3. Elani HW, Allison PJ, Kumar RA, Mancini L, Lambrou A, Bedos C. A systematic review of stress in dental students. J Dent Educ. 2014 Feb;78(2):226-42. PMID: 24489030.4. “Mental Health and Well-being for Oral Health Professionals and Dental Students.” www.fdiworlddental.org, 1 Sept. 2023, www.fdiworlddental.org/mental-health-and-well-being-oral-health-professionals-and-dental-students.5. Plessas, Anastasios, et al. “Using the Mental Health Wellness Framework in dental practice.” Bdj Team 9.10 (2022): 10-12.6. Cooper CL, Cartwright S. An intervention strategy for workplace stress. J Psychosom Res. 1997 Jul;43(1):7-16. doi: 10.1016/s0022-3999(96)00392-3. PMID: 9263926.
35VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationAbout the AuthorsDr. Priya M. Thomas is the Vice Chair and Director of Comprehensive Care and Predoctoral Clinics in the Department of Biomedical Sciences and Comprehensive Care at Indiana University School of Dentistry. Dr. Chandni Batra is a Clinical Assistant Professor in the Department of Periodontology at Indiana University School of Dentistry.Monica Gibson is the Graduate Program Director in the Department of Periodontology at the Indiana University School of Dentistry.Dr. Vanchit John is Chairperson of the Department of Periodontology at the Indiana University School of Dentistry.Dr. Neetha Santosh is a Clinical Assistant Professor in the Department of Oral Pathology, Medicine and Radiology at Indiana University School of Dentistry. Dr. Halide Namli Kilic is a clinical assistant professor in the Department of Periodontology at Indiana University School of Dentistry.Dr. Hawra AlQallaf is a clinical assistant professor in the Department of Periodontology at Indiana University School of DentistryDr. Celine Joyce Cornelius Timothius is an Assistant Professor in the Department of Periodontics at the Dental College of Georgia, Augusta University.
36 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2State of Licensure 2024Dr. Jill BurnsI was an Indiana State Board of Dentistry (ISBD) member during those last state-directed exam years, and one of the rst Hoosiers to be an examiner for the Northeast Regional Board (NERB) exam. It was quite a transition, and there were lots of opinions about the change. A certain segment thought that we were letting the state of dentistry go down the drain in Indiana by being a part of NERB. Another group welcomed the change and of course, there were those who were ambivalent and were just happy not to have to do it all again. ISBD administered an exam in Indiana from the years of 1879-2007. Dr Phinius Hunt, who had a practice on the Circle in downtown Indianapolis, recruited a group of dentists to test dentists coming into the state in 1879. That same year, he and several dentists, including Dr. John Johnston, founded the Indiana Dental College. At the time there were many itinerant dentists moving through the state, and some of them were quacks. By founding a licensure exam, Dr. Hunt and colleagues sought to protect the citizens of Indiana. In 2006, Dr. Roger Murphy and I, representing the ISDB, traveled around the country looking at dierent regional exams for one that might t with Indiana ideals of excellent dentistry. At all the exams, the examiners were calibrated, the criteria the same across the exam for everyone, and the best part, they were double blind. We were geographically in the middle of the NERB region, respected their exam and in 2007, became a member state. NERB decided to make the licensure exam a separate entity from the main group and built the development organization, American Board of Dental Examiners (ADEX), in 2004-2005. In 2015, NERB became The Commission on Dental Competen-cy Assessments (CDCA). Other regional exams decided to start administering the ADEX exam and have joined with CDCA. Western Regional Examining Board (WREB) joined in 2021, and The Council of Interstate Testing Agencies (CITA) joined in 2022. At this point, 48 of the states accept the ADEX exam for licensure, and the ADEX test is given all over the US, Canada, and Jamaica. Indiana has made signicant contributions to the examining community since 2007. We provide a large group of examiners to administer exams all over the country and several of our own have been ocers on the Board. Dr. Harvey Weingarten is a past chair of CDCA and Dr. Jim Jansen has served as treasurer.The dental licensure exam has changed a lot since that time. When I sat for the Indiana exam in 1984, there were six parts. We had to set denture teeth, prepared and fabricated a crown on a dentiform, scale a quadrant of periodontally diseased teeth, perform amalgam and gold foil restorations, performed an endodontic access opening, an oral pathology exam, and a jurisprudence exam. Now with the ADEX exam, the candidates perform four to ve parts for the exam. There is a didactic exam, an endodontic section, a crown and bridge section, a restorative section where they complete two restorations, and an optional periodontal section. All the clinical work is done on a manikin. The teeth used for the exams are crazy authentic. It still blows my mind that these teeth are so realistic. The candidate also must pass a jurisprudence exam on the Indiana Dental Practice Act. EACH DENTIST IN the state of Indiana has a dental licensure board story. Mine was that a classmate was pregnant, and I spent more time worrying about and checking in on her, than I did on my own exam. Fortunately, both of us passed. Also, my mom picked up all of my patients to make sure that they got to the exam. This was back in the Dark Ages when Indiana had its own exam. A lot has changed since then.COVER STORY
37VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationAt this time in Indiana, a dentist can gain licensure either by initial licensure or by endorsement. Initial licensure requires graduation from an accredited dental school within the U.S., a successful passing of a region-al examination (ADEX), Central Regional Dental Testing Service Examination (CRDTS) and Southern Regional Testing Agency (SRTA) with no more than three failed examinations in the past and passing of the Indiana jurisprudence exam. A seasoned dentist may gain licensure by endorsement. Requirements for endorsement include licensure in an-other state or province of Canada like Indiana’s require-ments, has practiced dentistry two out of the previous three years, performed 20 hours of continuous educa-tion in the past two years, and passed the jurisprudence examination.The Indiana State Board of Dentistry works hard on maintaining the highest standards for our profession in Indiana. They have meetings every two months but work hard in between these meetings on other matters important to dentists in Indiana. The current members of the Board are Dr. Robert Findlay (Board Chair), Dr. Richard Nowakowski, Dr. Annette Williamson, Board Liaison, Dr. Matthew Kolkman, Twyla Rader, L.D.H., Dr. Roger Sheline, Dr. Jerey Snoddy, Dr. Edward Sam-mons, Dr Barbara (Crunchy) Wells, Tammera Glickman, Consumer Member. They meet at the Government Cen-ter South in downtown Indianapolis, and the meetings are open to the public. If you have never attended one, I highly recommend it. They are fascinating. We all take great care of our patients and treat them with skill and compassion working within the connes of the law. We review the law every two years to remind us of this. It is the singular charge of the Dental Practice Act and the watchdog ISBD to protect the citizens of Indiana. And that will always be the number one concern. And as you can see, over time, the state of licensure has been ev-er-evolving, yet keeping a focus on patient care. A lot may have changed since you achieved your license. Stay tuned, there are always more changes on the way. About the AuthorDr. Jill Burns is a dentist in Richmond and the 2022-2023 IDA president. She has also served as the president of the Indiana State Board of Dentistry.
38 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2COVER STORYDr. Elizabeth SimpsonSo welcome everyone. My rst question for each of you is tell me how you got here today to IUSD. Anushri Singh Rajapuri I am a D3 student at IUSD, Class of 2025. I’ve had ve years’ history now with IU. I moved to the U.S. in 2018 for a master’s in health informatics. I graduated once from dentistry back home and I come from a family of dentists. I worked with my mom at her practice for two years. I wanted to explore more what’s there out in the world regarding healthcare, so I picked up a master’s in health informatics. I was a lot into research, and once I graduated in 2020, I got a job with Regenstrief [Institute] in partnership with IU School of Dentistry. I worked there for about two years, and I realized how much I love dentistry and how much I wanted to get back to it. I loved how it was being practiced at IU with the standard of care. I took my boards in 2021. I applied in 2022 for the cycle of 2023, and here I am. Harvi Subhash PatelMy story with dentistry in general and with IU is more like, things that don’t go your way can sometimes be a wonderful stroke of luck, and that is how it has been for me. I completed my dentistry in India in October 2020 and then my plan was to apply to all the dental schools here possible. But before that I had to give my NBD part 1, part 2. Back then, INBD part 2 had not yet started, so I took those exams. I am here on an F-1 visa. So what that means was when I came here for my exams, I was on visitor’s visa and you can give your exams on visitor’s visa. So after my graduation in India, I studied for a couple months and I was here in U.S. for three and a half months. By the time I took my English prociency exam and the results came out, it was just one day left before the IU deadline closed, so by the time I got my results, only 30 minutes remaining on the deadline of IU application and so I hit submit. I thought, this is the rst school and I’m applying 30 minutes before the deadline is closing. There’s no way I’m getting into it. But then luckily, I got in and yes, now here I am, Class of 2024. Dental School from the International Student’s PerspectiveMANY OF US probably take for granted the ease of mobility and benets that come with U.S. citizenship. Dental school is challenging enough for every student, but when you add the pressures of visa applications, work limitations and even restrictions on graduate school attendance, the international dental student experience can be overwhelming. Earlier this spring I interviewed two IUSD students from India, to hear their insights on studying in the U.S. and their future careers in dentistry.Dr. Elizabeth SimpsonHarvi Subhash Patel Anushri Singh Rajapuri
39VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationDr. SimpsonSo second question, in an ideal world, what would you like to do after graduation? HarviIn an ideal world, I think I would like to nd a mentor that I really want to work with who’s also outside practicing. Dr. SimpsonSo when I say ideal world, if you didn’t have the visa issue, what would you want to do? HarviI think I’d apply to a couple of private practices, especially the faculty who’s over here and who also have their clinics open if they have any openings. If they have friends who have openings, that would be my most ideal. Anushri Ideally, I would like to apply for residency in an ideal world. And in my ideal world, I get into a residency program as soon as I graduate, so without any visa issue, yes, I would love to study more. Like Harvi said, I would want to learn from any of the amazing doctors at IU, learn from them in their private practices. Probably I would reach out to a left-handed dentist, because I am a left-handed dentist too! Dr. Simpson Because there are certain residencies you can’t even do, such as oral surgery, correct?Anushri So that is correct. I am limited in my residency choic-es, especially for hospital-based residency programs like pediatrics and oral surgery. These are the two main hospital-based programs that I cannot even apply. The IU School of Dentistry Pediatric Dentistry website has it on their page that if you are an international applicant with a DDS degree or a DMD degree from the United States, you cannot apply. It’s very discouraging.Dr. SimpsonSo even if you got your DDS from the U.S. and you’re an international student, you still can’t apply?Anushri Yes, and my question is to everyone out there why, if our medical counterparts can nish their medicine and they’re allowed to do residency in a hospital-based sys-tem. They’re here. They’re serving their community within the United States and they’re doing really well. And yeah, they do have a contract where they have to work in a rural setting and not in an urban setting. But why hasn’t dentistry reached there yet when our medical counterparts are there, they’re doing their residency. And why is it so dicult for us to even approach the matter? Give us a chance, put us in an exam. If we do not do well on an on a scale with every-one, then I understand. But why take away that chance is my question. Yes, it’s disheartening. Dr. SimpsonSo that leads into my next question. So with having to get the visa, what is the reality of what will happen after gradu-ation for both of you? HarviSo after graduation, two things can happen. One, we have a one-year OPT, Optional Practical Training. With that OPT status, I don’t really need a work visa, but the catch is every year in March is when you can apply for a work visa. So every year, you have one shot to apply. That means my opportunity at applying for an H-1B when I’m graduating in May 2024 would be once in March 2025, but there are some companies or some practices who are willing to at least le for our H-1B before we graduate. So they have to le in March 2023. So then even with my one year of OPT, if my work visa doesn’t get paid in March 2024, I still have a shot in March 2025. Now with the work visa, it is lottery based. So if I want to work for a corporate practice or if I want to work for a private dentist, whenever they le, it is lottery based. Dr. SimpsonSo with the OPT, if you get that in 2025, you’d have to apply all over again, or you’d have that and like in 2025 that ends and you still have to get the visa?Continued on page 40
40 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2Anushri Let me answer this question because I’ve done this before. I graduated with my master’s in 2020 and I was able to work at the school for two years without any sponsorship or any employment visa. To make this easy, let’s just break it out into two parts. Once you graduate, you have two options. One, you take an OPT, that is your work authori-zation for one year, during which you can work in the eld you specialize in, so I cannot go work in any other company apart from dentistry. So even when I graduated with my master’s in health informatics, I had to work in that eld only. I couldn’t go to any computer science or any other eld that I wanted. So that’s one thing that you can do and once your OPT expires, you have no valid status to be in this country. So you have to go back home. Dr. SimpsonI thought you just applied again and then apply again. But no, you’re just done? Anushri The reason after my master’s I could stay for more than a year is because I was part of a STEM program in the United States that gives the STEM students three years of an OPT. But dentistry does not fall in this STEM program, so we get only one year to graduate. We all are here to stay and to work and to provide for the community. Some students want to go back after a year, but with my long-term goals, I do not. So my second option is to nd an employer who would then, during my period of an OPT, ap-ply for an H-1B visa. That is a work visa that, once granted, gives you stability to stay in the United States for a mini-mum of three years and can be renewed for up to six years. Dr. SimpsonSo basically it can only be renewed once, because then at that point it’s six years?Anushri You are right. It’s a very complicated process. But for someone who’s been through this and who has a commu-nity that’s gone through this system, it’s very simple. An ap-plication process for an H-1B right now is $10 for the lottery system. It’s just $10 for a private practice owner to apply and if the number does get picked, then the entire process would be around $800-$1,000 to get a H-1 approved. So your lottery gets picked, then your H-1 gets approved. That is how the system works. Being in the six-year period, I found an awesome employer. Dr. Simpson employs me. Dr. SimpsonAbsolutely. Anushri It’s on the record now. I found you. You’ve gone through the process with me. We’ve worked through it. I got my H-1 approved, and the next step would be apply for an I-140 or a green card process. Dr. SimpsonAnd that’s after six years, though?Anushri No, that’s as an employer. You can apply any given point, so that’s like an alternative branch that an employer can do from day one. But it is not a status. It is not an OPT card. It is not an H-1 status that allows us to stay in the U.S. It is a separate entity of its own that, when it gets approved, then we would get a status. But based on that application, we cannot stay in the U.S. So we’re talking about three sepa-rate branches. We can go on talking about this forever, because that’s how the process is. But Harvi and I are trying to just generate awareness of how simple the process is. Because yes, we are asking employers to invest time, en-ergy and money from your own private practices, but then you are nding someone who’s going to owe you every-thing because you put in that eort for that person. You’ve made the quality of their life much better. And imagine the amount of work we would give back to the community. We would be there. Honestly, that’s what we are here for, pro-viding care and we all believe in it. Dr. SimpsonWhat kinds of things have you seen people do to be able to stay in the States? Have you seen people marry somebody so they can stay? COVER STORY
41VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationHarviSo other ways of staying are continuing your education. So just stay in school. So then and even when you’re staying in school, if you choose something that is a part of STEM program, then you still have multiple shots, like at least three shots at the end of that. And then you try and you try, but yes, you stay in school. Anushri Yes, I cannot think of anything else apart from staying in school or getting married to someone, but honestly, I’ve only seen that in movies. I have never witnessed anyone marrying in my circle, and I’ve been here for ve years now. I’ve never seen anyone do that just to stay here. But even staying as a student, it’s so much money, and most of us don’t have cosigners here. I don’t have a cosign-er here. I’m getting private loans. I think both of our parents are putting their hard-earned money into our education, and that’s a big sacrice and commitment from their end that I cannot put them through this indenitely. And that brings me back to the question about residency in hospital-based programs where students are getting paid for their work. Most residency programs that are hospital based get paid. And again, that’s my question. Why are we not allowed to even apply for a program?One other option is working for a nonprot. You still need a work visa. They still need to le for your work visa, but that is a dierent kind of work visa that doesn’t go through the lottery. Dr. SimpsonSo would community health centers count for that?Anushri Yes, so community health centers would count. But when I have my work visa with a nonprot, that is not transferable. So if I want to still work with you as a private practice own-er, as an associate, I need to keep ling. You need to keep ling for me every year so that the private clinic work visa gets approved. Dr. SimpsonSo then my question would be as somebody who worked in community health centers, it sounds like you have a real-ly heavy emphasis on private practice. Why do you not look more into working in a health center?HarviMy Eskenazi rotation got me more thinking about it. The problem that I had with the community clinic was that there were very limited procedures. They were doing just llings and extractions right out of dental school, that is the period where if I learn 10 things, I’m going to practice those 10 things for a longer period of time. Dr. SimpsonAnd so I get that. But I think it’s sort of a situation where it’s like, well, if you’re desperate, maybe you need to put that on the back burner. And not every health center is limited. Anushri I agree with both of you. Yes, if I am desperate to stay here and pay my parents back on the student loans, I will do that. But again, we’re trying to bring awareness. When we get an option to study from someone great and meet my goals, and think about the kind of services I would like to give. Dr. SimpsonWhat you guys brought up is sort of a feeling all students have. I had been out maybe a year or two, and I went to complain to one of my mentors thinking I should be doing more procedures. And she actually shut me down and was like, no, you’re a new dentist. You need to focus on ve things. To this day I don’t remember what the ve things were, but they were very basic things. And she was like, you have to stop looking at what your friends are doing. Next year, or in ve years, you’re not going to be at the end of your career. And our eld changes so often. I think there is still some value in working on talking to patients, getting better at restorations, getting better extractions and doing all those things and building on it. I tell that to everybody. Continued on page 42
42 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2Anushri I completely agree with you, Dr. Simpson. I worked with my mom who worked for almost 30 years in Saudi Arabia be-fore we moved back to India so she schooled me the same way. She said, get your basics right, your hand work has to get good, you know. Dr. SimpsonSo I’m trying to be like devil’s advocate and think of what people would say to push back at this, like well, they should have thought of that before they decided to come here. And so what would you kindly say back to them? COVER STORYAnushri The most basic answer, America is a land of opportunities and we are here just trying to make the best of our oppor-tunity provided to us by our parents, by our teacher. To everybody, our current sta, our current mentors at the school at IU because honestly, this kind of pushback I’ve not experienced at our school. Everyone has been so supportive.I’m hoping and I’m being optimistic about the fact that we do not nd this kind of pushback outside our school outside the boundaries of Indiana because this school is very diverse. It represents number of people working from a number of stages of life. And I’m kind of optimistic about this just because how the school’s environment is.
43VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationNEWS & FEATURES Combatting Compassion Fatigue as a Dental ProfessionalDr. Catherine MurphyWhat is Compassion Fatigue?Compassion fatigue is a form of burnout that arises from the continuous exposure to the suering and trauma of others. In dentistry, we witness patients, and often team members, in pain, distress, and/or fear on a regular basis. Over time, the constant exposure to these emotional stressors can lead to a gradual erosion of empathy, leaving dental professionals feeling emotionally drained and disconnected. Signs and SymptomsRecognizing the signs and symptoms of compassion fatigue is crucial for early intervention. Dental professionals experienc-ing compassion fatigue may exhibit but can vary:• Emotional exhaustion: Feeling overwhelmed, drained, and emotionally depleted.• Decreased empathy: Diculty connecting with patients on an emotional level or feeling indierent towards their struggles.• Irritability and cynicism: Increased irritability, negativity, and cynicism towards patients and colleagues.• Physical symptoms: Fatigue, headaches, muscle tension, and sleep disturbances.• Decreased satisfaction: Loss of enjoyment in patient interactions and decreased satisfaction with one’s work.Causes of Compassion Fatigue in DentistrySeveral factors contribute to the development of compassion fatigue among dental professionals:• Patient suering: Constant exposure to patients’ pain, anxiety, and dental trauma can take a toll on dentists’ emotional well-being.DENTISTRY DEMANDS EMPATHY, compassion and dedication from its practitioners. Dentists often nd themselves immersed in the daily challenges of alleviating pain, restoring smiles, and improving oral health. However, amidst the pursuit of serving patients, there lies a silent struggle known as compassion fatigue. The world renowned traumatologist, Charles Figley, who referred to compassion fatigue as “the cost of caring,” dened it as “the deep physical, emotional, and spiritual exhaustion that can result from working day to day in an intense caregiving environment.” This phenomenon can profoundly impact dental professionals, aecting their well-being and the quality of care they provide.
44 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2NEWS & FEATURES • Team members struggles: Constant exposure to the concerns of our co-workers can amplify the emotional bur-den we carry. As dental professionals, we often form close bonds with our colleagues, and witnessing their struggles and challenges can take a toll on our emotional well-being.• High workload: Long hours, tight schedules, and the pressure to meet patient demands contribute to stress and burnout.• Emotional investment: Dentists often invest emotionally in their patients’ and team members’ well-being, which can lead to emotional exhaustion over time.• Perceived lack of support: Limited support from col-leagues, supervisors, or the healthcare system can exacer-bate feelings of isolation and burnout.• Personal factors: Pre-existing mental health issues, perfectionism, and a lack of work-life balance can increase susceptibility to compassion fatigue.Impact on Patient CareCompassion fatigue not only aects the well-being of dental professionals but also compromises the quality of patient care. Dentists experiencing compassion fatigue may struggle to communicate eectively with patients, exhibit decreased clinical performance, and make errors in judgment. Moreover, patients can sense when their dentist is emotionally distant or disengaged, which can negatively impact the therapeutic relationship and patient satisfaction.Preventing and Managing Compassion FatiguePreventing and managing compassion fatigue re-quires a multifaceted approach that addresses both individual and organizational factors:• Self-care: Prioritize activities that promote well-ness and wellbeing such as regular exercise, journaling, mindful eating, quality sleep, meditation, breathwork and leisure time. Daily self care should be sustainable, thus activities that require signicant time and/or nances should be viewed as adjuncts, not your “go to” routines. If you’re looking to get started or want ideas, please join in the free self-care revolution I co-created with Bre Grzych, an acupuncturist and licensed massage therapist, on our Facebook Group: Take 3 For Me.• Boundaries: Set boundaries to maintain a healthy work-life balance and prevent emotional overload. The word “No” can be a complete sentence. • Peer support: Seek support from colleagues, mentors, or support groups to share experiences and coping strate-gies. • Continuing education: Stay updated on stress man-agement techniques, mindfulness practices, and resil-ience-building strategies.• Organizational Support: Organizational support is paramount in addressing compassion fatigue. Advocating for policies that prioritize employee well-being, provide resources for mental health support, and foster a cul-ture of empathy and compassion within dental practices is essential. Personally, I am immensely grateful for the Northwest Component’s Membership Assistance Program (MAP), Encompass. The availability of counselors for chat sessions without prior appointments has been immensely benecial to me. Recently, I noticed a shift in my attitude during my com-mute, as I found myself feeling sour and reluctant to engage with patients—a departure from my natural dispo-sition. However, through one of these counseling sessions, I realized that I was carrying emotional baggage that wasn’t rightfully mine. With just a few simple questions during my commute session, I was able to untangle myself from these burdens and approach each new day with renewed positivity.
45VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationIt’s worth noting that similar support services are also ac-cessible to those utilizing the IDA Insurance Program. Furthermore, the acknowledgment of support on a national scale is reassuring. The American Dental Association (ADA) is committed to meeting the needs of its members. In response to voiced concerns, the ADA has taken proactive steps by hosting the Inaugural Wellness Summit last year, establishing the 2nd Cohort of Wellness Ambassadors, creating a dedicated Resource Page, organizing continu-ing education (CE) events, and implementing various other initiatives aimed at promoting well-being within the dental community. About the AuthorDr. Catherine Murphy takes a holistic approach to her orthodontics practice in Grith. She was inducted into the American College of Dentists and was also selected as an American Dental Association Wellness Ambassador. Dr. Murphy also speaks nationwide on holistic orthodontics, myofunctional therapy and wellness.ConclusionCompassion fatigue is a pervasive issue in our profession that can have profound consequences for both dental pro-fessionals and our patients. By raising awareness, recog-nizing the signs and symptoms, and implementing preven-tive measures, the dental community can work together to mitigate the impact of compassion fatigue and foster a culture of resilience, empathy, and well-being. Are you rec-ognizing the signs of this within yourself or another? Please review the resources on the IDA’s Be Well webpage, ADA website or simply reach out to me. I’ll help connect you. Scan the codes below to access helpful resources:ADA Council on Dental Practice Wellness ResourcesADA Wellness ResourcesTake 3 for Me: drcatherinemurphy.comIDA Be Well Committee and Resources
46 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2Diagnostic Challenge: Spring 2024THE CHALLENGE: A 65-year-old male presents to the Indiana University School of Dentistry (IUSD) with a chief concern of “I want to get my crown xed.” Medical history is noncontributory. Social history is signicant for heavy cigar smoking. Extraoral exam is unremarkable. Intraoral exam revealed a white plaque with a rough surface texture and partial sharply demarcated borders located on the left mandibular retromolar pad and extending to create a ring around the gingival collar of tooth #18 (Figure 1). The lesion was initially detected over one year ago in which he was referred to an outside oral surgeon for evaluation. The patient does not recall a biopsy being performed but recalls being informed the lesion was benign. He was then referred to IUSD Oral Surgery clinic for a diagnostic biopsy. Histologic examination reveals a soft tissue specimen composed of surface stratied squamous epithelium and supporting brous connective tissue. The surface of the specimen is markedly verrucous in architecture and covered by a thick layer of orthokeratin subjacent to which is a prominent granular layer. The spinous cell layer exhibits atypical cytological and morphologic features including increased nuclear/cytoplasmic ratio, nuclear hyperchromatism, loss of intercellular orientation and irregular, focally bulb shaped rete pegs (Figure 2). Occasional high level mitotic gures are also noted. Can you make the diagnosis?A. Squamous cell carcinomaB. Benign alveolar ridge keratosisC. Oral lichen planusD. Oral hairy leukoplakiaE. Dysplastic leukoplakia The Diagnosis: E. Dysplastic leukoplakia Oral white lesions are commonly encountered in dental practice and have a variety of potential causes including developmental, frictional, infectious, and neoplastic. Leukoplakia is a precancerous, nonremovable condition manifesting as a white patch or plaque on the mucous membranes of the oral cavity. It is one of several oral potentially malignant disorders (OPMD). Of all OPMDs, including erythroplakia, leukoplakia is the most common. Clinically, leukoplakias can be divided into two broad categories based on their surface and morphologic features: homogenous and nonhomogeneous. Homogenous leukoplakias typically present as a thin, at white plaque with sharply demarcated borders. Nonhomogeneous leukoplakias present with either erythroplakic or verrucous areas.1 Leukoplakia can aect any site in the oral cavity, but the more common sites include the lateral border of the tongue and oor of mouth, buccal mucosa, hard and soft palate, and gingival mucosa. Oral leukoplakia may be localized to one site or may present as a diuse process. Proliferative verrucous leukoplakia (PVL) is rare but aggressive form of leukoplakia. It is seen more frequently in women with no tobacco history. PVL starts initially as a white plaque that evolves over time to large lesions with verrucous or rough surfaces. It is common for PVL to aect multiple sites of the oral cavity with the gingiva being the most common site of involvement.2Dr. Angela RitchieDr. Neetha Santosh CLINICAL FOCUS
47VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationFigure 1: White plaque of the left retromolar pad. Leukoplakia is strictly a clinical term. Denitive diagnosis is determined by histopathologic examination. A biopsy of oral leukoplakia can show hyperkeratosis, epithelial hyperplasia, epithelial dysplasia, or squamous cell carcinoma. Oral epithelial dysplasia or squamous cell carcinoma is noted in 39-53 percent of cases of leukoplakia. Generally, nonhomogeneous leukoplakias are associated with a higher risk of dysplasia or oral cancer. PVL is the most aggressive form of leukoplakia with a malignant transformation rate of 70 to 100 percent.1 In considering the site of biopsy in large white lesions, sampling multiple sites is generally recommended to avoid sampling error. Management strategies for leukoplakia should initially be aimed at mitigating risk factors, such as counseling for tobacco and alcohol cessation. Early detection and intervention of premalignant lesions is of utmost importance. Regular clinical examinations and biopsy is essential for the detection and diagnosis of OPMD. Comprehensive intraoral and extraoral exams are recommended at all patient visits, including recall appointments and emergency visits.2 For lesions exhibiting dysplasia, interventions range from complete surgical excision to less invasive alternatives like laser ablation. Treatment of mild epithelial dysplasia may include careful long-term follow-up or surgical intervention depending on the lesion’s characteristics, location, and patient-specic considerations. Lesions that show moderate or severe epithelial dysplasia should be managed with complete surgical excision. Surgical removal with a scalpel is recommended to prevent cautery artifact on histopathologic examination. Despite interventional therapy, including laser ablation, PVL has a recurrence rate of up to 85 percent.2 Differential DiagnosisA primary diagnostic concern for a nonremovable white plaque is invariably squamous cell carcinoma (SCC). We also included benign alveolar ridge keratosis given the location. Other white lesions that may present with a similar clinical appearance include oral lichen planus. Given the rough surface texture, oral hairy leukoplakia was the last lesion included in the dierential diagnosis. Squamous cell carcinoma (SCC)SCC accounts for more than 90 percent of malignancies aecting the oral cavity, making it a signicant community concern. Data from the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) program estimate there will be 54,540 new cases of oral and oropharyngeal cancer in the USA in 2023 with 11,580 deaths.3 75 percent to 80 percent of oral cavity SCC cases can be attributed to cigarette smoking, other forms of tobacco use, and the synergistic eects of excessive alcohol consumption.4 These typically manifest in older men on the ventral and lateral surfaces of the tongue and the oor of the mouth with a lower frequency in the other parts of the oral mucosa (descending order) such as gingiva, buccal mucosa, labial mucosa, and hard palate. The remaining 20 percent to 25 percent of oral cavity SCC occur in individuals without discernible risk factors on the lateral tongue in young adults or on the gingiva in older women. Remarkably, SCC aecting the oropharyngeal areas such as the base of the tongue, tonsils, and soft palate has been on the rise alarmingly in younger men and is predominantly linked to human papillomavirus infection. Clinically, SCC can present as an exophytic mass with an irregular granular surface, an endophytic chronic ulceration, or more subtly even as an erythroplakia or leukoplakia.5 Histopathologic features include an epithelial malignancy arising from the dysplastic surface epithelium that invades the underlying brous connective tissue as islands and cords of malignant squamous epithelial cells. Given the long Continued on page 48
48 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2history of cigar smoking in our patient, it was prudent to include SCC in the dierential diagnosis.Benign alveolar ridge keratosis (BARK)Benign alveolar ridge keratosis is a relatively common, non-neoplastic oral condition characterized by the presence of a white or whitish-yellow patch or plaque with a slightly warty surface located predominantly on the alveolar ridges or retromolar pads. These lesions are usually asymptomatic and may be unifocal or bilateral. BARK is considered a reactive condition often arising in response to chronic irritation or trauma. Diagnosis is supported by histopathologic examination which generally shows marked hyperorthokeratosis and acanthosis with elongated, slender, tapered rete ridges.6 Treatment typically involves removing the source of irritation, if identied, and monitoring the lesion for any changes. Due to its benign nature, BARK does not generally require aggressive treatment unless it undergoes signicant changes in appearance or symptomatology, at which point further evaluation would be warranted. BARK was included in the dierential diagnosis for this patient given the location of the lesion on the retromolar pad. Oral lichen planusLichen planus is a common dermatological condition that frequently aects the oral mucosa. It is an autoimmune condition, although the specic target antigen remains unidentied. Lichen planus primarily aects middle-aged adults, with rare occurrences in children. Women are predominantly aected, outnumbering men by a ratio of 3 to 2 in most reported cases. Oral lichen planus (OLP) typically presents bilaterally, and the common intraoral locations include buccal mucosa, labial mucosa, ventral and dorsal tongue, and gingiva. Reticular lichen planus appears as white reticulations/striations or papules that are not usually painful. However, erosive lichen planus presents as erythematous and painful erosions and ulcerations on the oral mucosa. When it occurs on the gingiva, it is clinically referred to as desquamative gingivitis. The diagnosis of OLP is usually done through hematoxylin and eosin studies (H&E) of a biopsy sample and often direct immunouorescence (DIF) studies are required to obtain a denitive diagnosis. The histopathological characteristics of OLP are distinctive however, other conditions such as the initial stages of proliferative verrucous leukoplakia, lichenoid drug reactions, lichenoid amalgam reactions, lichenoid foreign body gingivitis, oral graft-versus-host disease, lupus erythematosus, chronic ulcerative stomatitis, and oral mucosal cinnamon reactions can also exhibit a similar histopathological pattern. Hence clinicians should consider a clinical pathologic correlation before the standard management with oral topical corticosteroids is started and patients require continued follow-up to monitor any clinical changes.7Oral hairy leukoplakiaOral hairy leukoplakia (OHL) is an EBV-related pathology that occurs in immunocompromised individuals, most commonly in HIV/AIDS patients and patients with a history of organ transplants. Healthy patients especially older adults may also manifest OHL due to the alteration of immune functions due to aging. Though OHL has leukoplakia in its term, this lesion has no evidence of premalignant dysplasia or malignancy. It clinically manifests as bilateral painless white vertical streaks on the lateral border of the tongue. Histopathologically OHL exhibits hyperplastic, hyperkeratinized oral epithelium with balloon cells that show nuclear positivity for Epstein-Barr virus-encoded RNA CLINICAL FOCUSFigure 2: High-power photomicrograph showing focally moderate epithelial dysplasia (hematoxylin and eosin stain, x10 magnication).
49VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationAbout the AuthorsDr. Angela Ritchie is an assistant clinical professor in the department of oral pathology, medicine and radiology and is director of laboratory services for the Oral Pathology Group at Indiana University School of Dentistry. Dr. Neetha Santosh is a Clinical Assistant Professor in the Department of Oral Pathology, Medicine and Radiology at Indiana University School of Dentistry. She completed an oral and maxillofacial pathology residency at The Ohio State University College of Dentistry. Dr. Santosh is also a fellow of the American Academy of Oral and Maxillofacial Pathology and a Diplomate of the American Board of Oral and Maxillofacial Pathology.with in situ hybridization study. Treatment is not typically required. However, modication of antiretroviral therapy or steroid therapy may resolve the lesions. Since OHL could be the rst sign of an HIV infection, patients should be tested if there are chances for any HIV exposure.8ConclusionWith this diagnostic challenge, we reiterate the importance of comprehensive oral examinations. The emphasis on preventive measures, early detection, and timely intervention underscores the dental professional’s pivotal role in the multidisciplinary approach to managing oral potentially malignant disorders, including leukoplakia, and mitigating its progression to oral squamous cell carcinoma. References1. Villa A, Woo SB. Leukoplakia – A Diagnostic and Management Algorithm. J Oral Maxillofac Surg 2017; 75:723-734. 2. Wetzel SL, Wollenberg J. Oral Potentially Malignant Disorders. Dent Clin N Am 2020; 64:25-373. Seigel RL, Miller KD, Wagle NS, Jemal A. Cancer Statistics, 2023. CA Cancer J Clin 2023; 73:17-48.4. Speight PM, Farthing PM, Bouquot JE: The pathology of oral cancer and precancer. Curr Diag Pathol 1997; 3:165-176.5. Lubek JE, Clayman L: An update on squamous carcinoma of the oral cavity, oropharynx, and maxillary sinus. Oral Maxillofacial Surg Clin N Am 2012; 24:307-316.6. Natarajan E, Woo SB: Benign alveolar ridge keratosis (oral lichen simplex chronicus): A distinct clinicopathologic entity. J Am Acad Dermatol 58:151, 2008. 7. Cheng YL, Alan Gould A, Kurago Z, Fantasia J, Muller S. Diagnosis of oral lichen planus: a position paper of the American Academy of Oral and Maxillofacial Pathology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016; 122:332-54.8. Greenspan J.S., Greenspan D., Webster-Cyriaque J. Hairy leukoplakia; lessons learned: 30-plus years. Oral Dis 2016; 22:120-127.
50 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2MEMBER ZONEIN MEMORIAMDR. C. RICHARD ALTENHOF of Valparaiso and a member of the North-west Indiana Dental Society passed away March 18, 2024. Dr. Altenhof graduated from Loyola University of Chicago in 1970.DR. RICHARD P. BOWLING of Indianapolis and a member of the Indianapolis District Dental Society passed away February 27, 2024. Dr. Bowling graduated from Indiana University School of Dentistry in 1962.DR. NORRIS BRANSON of Evansville passed away February 1, 2024. Dr. Branson graduated from the University of Louisville School of Dentistry in 1963.DR. JAME FALL of Marion and a member of the North Central Dental Society passed away June 10, 2023. Dr. Fall graduated from Indiana University School of Dentistry in 1950.DR. DONALD FORSEE of Floyds Knobs and a member of the Southeastern Indiana Dental Society passed away March 2, 2024. Dr. Forsee graduated from Indiana University School of Dentistry in 1979.DR. JULIAN E. GRAY of Trafalgar and a member of the Indianapolis District Dental Society passed away June 4, 2024. Dr. Gray graduated from Indiana University School of Dentistry in 1986.DR. JAMES E. HULETT of Hammond and a member of the Northwest Indiana Dental Society passed away February 6, 2023. Dr. Hulett graduated from Chicago College of Dental Surgery in 1952.DR. W. K. MANCHETTE of Evansville and a member of the First District Dental Society passed away April 11, 2024. Dr. Manchette graduated from St. Louis University in 1950.DR. MARK R. MONTGOMERY, formerly of Kokomo, passed away May 16, 2024. Dr. Montgomery graduated from the Indiana University School of Dentistry in 1982.DR. TED M. REESE of Indianapolis and a member of the Indianapolis District Dental Society passed away May 8, 2024. Dr. Reese graduated from Indiana University School of Dentistry in 1984. DR. THOMAS D. VANOSDOL, formerly of Warsaw and a member of the North Central Dental Society, passed away March 17, 2024. Dr. VanOsdol graduated from Indiana University School of Dentistry in 1964.
51VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental AssociationClassifiedsINTRAORAL X-RAY SENSOR REPAIR/SALESWe repair broken sensors. Save thousands in replacement costs. Specializing in Kodak/Carestream, major brands. We buy/sell sen-sors. American SensorTech 919-229-0483 www.repairsensor.comEQUIPMENT REPAIRDENTIST-TERRE HAUTEWe are seeking an Associate Dentist to join our growing team. Take care of your community while participating in activities to promote a positive image of the company! Requirements include DDS/DMD from a dental education program, current, valid license to practice dentistry, compassion and a strong desire to provide dental care to both children and adults. careers.benevis.com/careers-home/jobs/3942?lang=en-usASSOCIATE DENTIST-DYER Part-time or full-time associate position available in a growing family practice in Dyer, Indiana. We are an established family-owned practice with over 40 years of experience. We nd ourselves in need of another dentist due to growth and the approaching retirement of the owner. In-quiries and resumes may be directed to Mari Carrasco, Oce Manager, Email: mc.petersonfamilydental@gmail.com.PART TIME DENTIST NEEDED FOR EXTRACTIONS Busy practice on 86th and Michigan Road in Indianapolis is looking for a part time dentist to help with extractions. Must be able to do surgical and wisdom teeth extractions. Prefer Mondays or Wednesdays or any Monday of the month. Call 317-748-4603.DENTIST-BROAD RIPPLE INDIANAPOLISAre you a talented dentist with a passion for providing excellent care? Do you have at least two years of experience and a desire to work in a brand new, state-of-the-art oce? If so, SoBro Dental in the thriving Broad Ripple area of Indianapolis is looking for you! Competitive com-pensation, CE opportunities, professional development support and more. Submit resume and cover letter to SoBrodental@gmail.com.TRAVELING DENTIST We are seeking a highly skilled and compassionate Traveling Dentist. If you are a new college graduate or experienced Dentist, this opportuni-ty is for you! Being a Traveling Dentist with Aria Care Partners provides you the opportunity to deliver unmatched patient care to residents in skilled nursing facilities. You will be responsible for assessing dental health, addressing dental concerns, developing and discussing the treatment plan, performing limited procedures, and oral cancer screen-ings. Competitive pay, exible schedule, drive time + clinic time is all compensated. https://boards.greenhouse.io/ariacarepartnersEMPLOYMENT OPPORTUNITIESMEMBER ZONEGENERAL DENTIST-TOPEKA, INGeneral dentist needed for growing community practice that treats the underserved Amish community in Topeka IN. Full or Part time positions available. Competitive compensation based on experience with signif-icant signing bonus. Join our experienced, high functioning team that values a positive work climate. Passion for pediatrics preferred but not necessary. Generous FT benets include but are not limited to health insurance, disability, professional liability, 401K, PTO, vision, and paid holidays. Check out our mission at www.thecommunitydentalclinic.orgASSOCIATE DENTIST OPPORTUNITYJoin Our Team as a Caring Part-Time General Dentist at Rector Family Dental in Muncie. We’re excited to invite an enthusiastic General Dentist to join us on a part-time basis. Your three days a week will be lled with meaningful interactions, where you’ll create positive dental experiences that children will carry with them into adulthood. Our well-equipped facility and supportive team ensure that you can focus on delivering exceptional care. Full clinical autonomy, work side by side with owner doctor, competitive compensation packaged based on pro-duction, PTO, Medical/Dental/Vision/401k. Email Je.Dreels@D4C.com.EMPLOYMENT OPPORTUNITIESPRACTICES AVAILABLEDENTIST PRACTICE OPPORTUNITY-VEVAY2,800 sq. ft. building attached to the Switzerland County Medical Build-ing, owned by Switzerland County Commissioners. Numerous operato-ries with room to expand. Aordable lease available to full-time dentist. Building includes other medical oces. Just 60 miles from Louisville and Cincinnati. Email coadmin@switzerland.in.gov.GENERAL PRACTICE FOR SALE IN PLYMOUTHSpectacular Dental Practice Opportunity in Plymouth, Indiana! 6 opera-tories with space for expansion, strong fee-for-service environment, free from PPO constraints. 2023 collections exceeded $1.1 Million, reecting the practice’s strong performance and potential for growth. For more information, contact Stephen at 919-723-8061 or stephen@encom-pass-ihc.com. www.encompass-ihc.comHIGHLY PROFITABLE PRACTICE FOR SALE IN JASPER COUNTYLong established 80% FFS/20% PPO Practice in a small downtown setting. This EXCEPTIONAL practice is a “MUST SEE” with 2,300 sq ft., 5 Op’s, digital and paper patient records, digital X-ray, and more. This beautiful practice is located in a free standing well-maintained building with ample parking in a downtown setting. Real estate is available, if de-sired. Team has been there for many years! Call 847-242-1203.
52 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2New MembersBEN HUR DENTAL SOCIETYDr. Molly-Emma Jones (IU 2023)EAST CENTRAL DENTAL SOCIETYDr. Amber Reid (IU 2007)Dr. Teresa Watkins (IU 2000)FIRST DISTRICT DENTAL SOCIETYDr. William Fowler (IU 1983)Dr. Dana Morris (Univ of Louisville 2006)Dr. Lauren Watson (Univ of Louisville 2008)INDIANAPOLIS DISTRICT DENTAL SOCIETYDr. Hawra AlQallaf (IU 2018)Dr. Chandni Batra (IU 2020)Dr. Marcus Bigot (Marquette Univ 2020)Dr. Helen Bishara (Tufts Univ 2006)Dr. Manpreet Kaur Dhanjal (Univ of CO 2023)Dr. Nichole Downing (IU 2023)Dr. Brian Fraiz (IU 2017)Dr. Trent Kirkwood (IU 2018)Dr. Ben Mohrman (IU 2005)Dr. Halide Namli Kilic (IU 2009)Dr. Inessa Ostrovsky (IU 2001)Dr. Alexandria Schwei (IU 2015)Dr. Caitlin Shannon (IU 2020)Dr. Milan Sheth (IU 2016)Dr. Deborah Simmers (E Carolina Univ 2021)Dr. Kevin Toole (IU 2007)MEMBER ZONEISAAC KNAPP DISTRICT DENTAL SOCIETYDr. Colin Brannagan (Univ of Detroit-Mercy 2023)Dr. Julie Fullenkamp (IU 2018)Dr. Forrest Fullenkamp (IU 2019)Dr. Uday Sekhar Reddy Mareddy (Rutgers, Univ of NJ 2021)NORTH CENTRAL DENTAL SOCIETYDr. Linda Burns (IU 1995)Dr. Steven Hodges (IU 1992)Dr. Amber Leer (IU 2009)Dr. Jennifer Roig (IU 1997)NORTHWEST INDIANA DENTAL SOCIETYDr. Gerald Childs (IU 2020)Dr. Susan Foundos-Biegel (Univ of IL-Chicago 1987)Dr. Stephanie Joly (Univ of IL -Chicago 2008)Dr. Christopher McGue (Univ of IL-Chicago 2020)Dr. Vivienne Zhang (NY Univ 2013)
53VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Association MANY DENTISTS FIND physical activity such as walking, running and yoga to be a great way to unwind from the emotional stress and physical strain of work, but Dr. Rob Holland, an orthodontist in Indianapolis and Carmel, takes a less conventional approach to his time out of the operatory. Since 2019 he’s found fun, relaxation and even love through salsa dancing.Dr. Holland began salsa dancing in 2019. He always enjoyed music and played piano and trumpet from childhood until his rst year in college, but he never did much dancing and instead focused mainly on boxing and wrestling for exercise. After deciding that both were becoming too rough on the body, he decided to take lessons at Latin Expressions Dance Company in downtown Indianapolis as a way to have fun and make friends. Latin Expressions teaches beginning through advanced courses and even has a competitive team, so Dr. Holland found the studio to be a great place to meet people at all levels of skill.After taking a break from the dancing during COVID, he returned to the studio again in 2023. He met his ancée, Tasha, at Latin Expressions and even proposed to her on the dance oor there. Their wedding is scheduled for August. Dr. Holland and Tasha dance together once a week but often practice separately. Tasha has branched out and joined one of the teams that does choreography and competitive dancing. For Dr. Holland and many others at Latin Expressions, salsa dancing is an ideal blend of physical activity, creative expression and socialization. “I like that it’s a partner dance. Since it’s a partner dance, you go and socialize and everyone dances together,” he said. “We’ve made a lot of friends with other single people and couples.” Dr. Holland also nds the music of salsa dancing inspiring. “I just like Latin music, the rhythms and the percussion. It’s lively and fun to dance to. I like watching ballroom, but it’s a little rigid and formal. The Latin dancing is more loose and fun.”Dr. Holland encourages his fellow members in IDDS to join in on the fun. “I keep telling them, ‘You should go. You don’t need any experience. You can go and learn with your group and make good friends.’”Learn more about Latin Expressions Dance Company at www.latinexp.com. Finding Fun, Fitness, Friends and Love on the Salsa Dance FloorOrthodontist Dr. Rob Holland and his ancée, Tasha, met while salsa dancing. See page 54 for more photos.OUT OF THE OPERATORY
54 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2OUT OF THE OPERATORY Top: Dr. Holland and his ancée, Tasha, in action on the dance oor.Middle left: Dr. Holland proposed to Tasha at the salsa dancing studio earlier this year.Middle right: Dr. Holland and some of his fellow salsa dancers.Bottom: A typical class at Latin Expressions Dance Company.
55VOLUME 103 · 2024 · ISSUE 2 | Journal of the Indiana Dental Association
56 Journal of the Indiana Dental Association | VOLUME 103 · 2024 · ISSUE 2