Return to flip book view
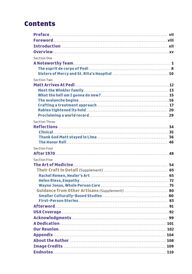
Message ContentsPreface ..................................................................... viiForeword ...................................................................viiiIntroduction .............................................................. xiiOverview ....................................................................xvSection OneA Noteworthy Team ......................................................... 1The esprit de corps of Pedi ................................................ 8Sisters of Mercy and St. Rita’s Hospital .................................10Section TwoMatt Arrives At Pedi ....................................................... 12Meet the Winkler family .................................................. 13What the hell am I gonna do now? ........................................15The avalanche begins .....................................................16Crafting a treatment approach .......................................... 17Rabies tightened its hold ............................................... 20Proclaiming a world record ...............................................29Section ThreeReflections .................................................................34Clinical .................................................................... 35Thank God Matt stayed in Lima ......................................... 36The Honor Roll ........................................................... 46Section FourAfter 1970 ................................................................. 48Section FiveThe Art of Medicine ....................................................... 54Their Craft in Detail (Supplement) ..................................... 65Rachel Remen, Healer’s Art ............................................. 65Helen Riess, Empathy ....................................................72Wayne Jonas, Whole Person Care ........................................75Guidance from Other Artisans (Supplement) ......................... 80Smaller Culturally-Based Studies ...................................... 80First-Person Stories .................................................... 83Afterword ................................................................... 91USA Coverage ...............................................................92 Acknowledgments ........................................................ 99A Dedication .............................................................. 101 Our Reunion............................................................... 102 Appendix .................................................................. 104About the Author ........................................................ 108Image Credits ............................................................ 109 Endnotes .................................................................. 110
viiPrefaceThe Relentless Pursuit of Healing and DiscoveryHeroism in medicine is embodied in the relentless pursuit o healing and discovery, where the stakes are often life and death. Health professionals exhibit quiet bravery as they confront uncertainty with resolve, driven by a deep commitment to their patients. he most successful profes-sionals have an insatiable curiosity expressed in the desire to uncover new treatments, understand complex diseases, and push the medical boundaries. his curiosity is balanced with an incredible compassion for others. his story reflects a healthcare team that embraced that balance as they worked tirelessly to save one life, that o a six-year-old boy, suering from rabies.I felt honored to listen to the original healthcare team share the recounting o this story and to know this eort occurred at St. Rita’s hospital—a place I serve each day with pride. Our current reality is built on the shoulders o those curious, compassionate teams. I hope that our teams one day will be a similar inspiration for future generations o healthcare professionals.—Matthew T. Owens, M.D., Chief Clinical Ocer Mercy Health – St. Rita’s Medical Center“Healthprofessionalsexhibit quietbravery asthey confrontuncer tainty.”—Matt Owens
viiiForewordFor many, virtues such as love for family, hope for good health, and faith in a higher power change little over fifty years. However, simultaneously, within the daily activities o our lives, change is the rule and not the exception, especially within healthcare. Health professionals work on the edge o chaos, filled with the flux o emerging symptoms and emotions and one tiny step away from total disaster or life-changing discovery.Amidst this steady pace o change, we have a constant desire to gain knowledge and improve healthcare. Occasionally along this journey, we intentionally disrupt and challenge the status quo, which is beneficial for us and our patients. Also, these dynamics occur across transdisciplinary healthcare teams that are willing to support one another and collaborate.What is a transdisciplinary team? Perhaps saying what it is not might be easier. he old saying, “Too many cooks spoil the broth,” means when too many people are involved in a task, a poor outcome will result.Transdisciplinary teams are the opposite. A wonderful broth depends on those willing to share their culinary knowledge. Imagine i each cook had a specialty: one supplies ingredients, one seasons the broth, and one watches the broth, so it doesn’t boil over or burn. hile each cook excels in their craft, everyone understands the materials and skills they bring to the stove and, even more important, how they plan to use them. ithout this collaboration, we could end up with noodle-less, overly spicy, burned chicken noodle soup! Hello trash…we’re going out for dinner!Yet, vulnerable, sick patients can’t go out for dinner; they depend on the healthcare team to get the recipe right, every time. A transdisci-plinary team blends their knowledge, warranting a new 21st Century adage, “Many humble cooks nourish the broth.” Clinicians that share their diverse experiences and expertise with each other deliver innovative and exceptional patient care. I have worked in amazing teams like this. hey empowered nurses and other clinicians Confidence and Collaboration: Catalysts for Change
ixFACING THE IMPOSSIBLE and caregivers to speak up and advocate for themselves and their patients. Interestingly, listening to others requires us to leave our judging egos at the door. Setting aside your pride and judgment, involves self- awareness o your own limitations, strengths, and biases. his requires us to take an inward journey—to reflect on our experiences, ponder our values and beliefs, and appreciate others. As you gain skills in listening to yoursel, you can attentively listen to others. he understanding o other disciplines and expanded self-awareness is positive for all, regard-less o which side o the bed you occupy.Transdisciplinary team members, just like our chicken soup cooks, need each other, regardless o role or experience. No role in patient care is more important than another; it truly takes a village… and a healthy work environment! ThenIn the 1970s, healthcare hierarchy was alive and well—physicians on the top, nurses and multiple other disciplines in the middle, and nursing aides at the bottom. Rarely did the three layers collaborate on a level playing field. Moreover, those below the top tier received little acknowl-edgement about their contributions. However, the healthcare team and administration at St. Rita’s Hospital in Lima, Ohio, heroically removed the disciplinary barriers from their practice and saved a child’s life while also accelerating innovative ideas in rabies acute care.This poignant recollection o real-life events provides a chronological narrative o their collaborative work that illustrates the eectiveness o cooperative learning and a passionate common goal. Did the St. Rita’s healthcare team realize their well-organized eort would disrupt rabies care? I don’t know. However, I am certain the team members relied on each other in ways they never had before. hey supported one another as dynamic decision-makers, compassionate care-givers, and innovators o transdisciplinary collaborative care. I worked alongside several o these nurses later in their careers. None o these women ever told me this story. Perhaps there was no story to tell, but simply part o who they were.
xMARY F. WEISNow many years later, when I heard about this unprecedented accomplishment, I was not surprised. hese nurses were confident, compassionate, and caring professionals, willing to voice their concerns for the betterment o patients. As a colleague, they inspired me and countless other nurses. I didn’t realize it at the time, but now on reflection, long before the recent concepts o transdisciplinary teams, they set a professional nursing standard o practice—teamwork was the foundation o excel-lence and informed patient care.NowIn the last fifty years, healthcare education has changed significantly. Today, in addition to standard skills such as starting intravenous lines and placing urinary catheters, we require nursing students to become proficient in leadership, interprofessional communication, and cultural competence. Nurses lead on bedside care, often supported by the entire healthcare team. However, the lingering hierarchical culture o health-care continues to complicate and challenge collaboration. e can take cues from the St. Rita’s team who faced similar issues. Confidence is the first hierarchy-busting-behavior the St. Rita’s team modeled. hey gathered confidence through the support o one another through positive constructive feedback, regardless o discipline or role. The Lima team created a culture o mutual learning, so the exchange o ideas and suggestions was robust.Confidence doesn’t come easily to most novice nurses and some seasoned nurses. Receiving feedback often conjures feelings o failure and giving feedback may oend someone or, worse, may create reper-cussions or hurt feelings. Leaving our judging egos at the door builds a culture o listening, mutual support, and confidence in one another. e can do the same today. I we want great chicken noodle soup, confidence is one key ingredient to bring to the stove.Collaboration is the other hierarchy-busting-behavior. The St. Rita’s team recognized and melded knowledge and expertise, expanding their capacity, rather than remaining limited within narrow norms o tasks and roles. Today the prevailing expertise has expanded exponentially, with new treatments and nursing specialties as well as the increase in mid-level providers, such as nurse practitioners and physician assistants. As baby boomers age, older and sicker patients necessitate even larger healthcare teams. ith so many clinicians involved in the patients’
xiFACING THE IMPOSSIBLE care, interprofessional communication is a necessity and a challenge. As educators, mentors, and colleagues, we can be mindful and model Lima’s collaboration style. hey built a collective vision, designed a simple communication plan, and expressed a willingness to learn from each other. Learning to work in collaborative teams today will build profes-sional integrity, save countless lives, and change our healthcare system.Even with an increase in cooks, we still want gourmet chicken soup, don’t we?In my forty years o working in healthcare, I have concluded that, like so many things in life, healthcare evolves in a cyclical fashion. Lucky for us, learning does as well. I’ve experienced the full range o team cultures. Many times, I left work feeling disrespected and isolated from others in various disciplines and amongst my fellow nurses. My ability to care for patients dimin-ished, as did my confidence. Other times my confidence rose, when a team worked well together and provided excellent patient care and outcomes.American healthcare is a dynamic and adaptive system. rue, changing healthcare can be overwhelming and uncomfortable. However, with self-reflection and collaboration, we gain confidence within ourselves and amidst a team, enabling us to work near the edge o chaos, save lives, build careers, discover life-changing healthcare innovations, and make a real dierence.Let’s keep our eyes on the prize. Delivering and receiving great health-care is like home-made chicken noodle soup, it nourishes everyone’s body, mind, and soul! —Ann Deerhake, D.N.P., R.N., C.N.L., C.N.E., C.C.R.N.Clinical Assistant Professor of Practice, The Ohio State University, College of Nursing
xiiOne day I pulled out a suitcase from my parents’ guest bedroom closet. I discovered newspapers, magazines, and journal articles featuring stories about Matthew Winkler’s recovery from rabies in 1970—the first documented human survival. Friends from all over the United States had mailed my parents copies o these stories. In short order, the yellow newsprint fanned across the bedroom floor. I gathered the Time, Newsweek, Redbook, Readers Digest magazines and walked downstairs to the kitchen table. “Hey Dad, what do you want to do with these?” I asked. “I don’t know,” he said. hen, he oered a bit o a reflection. “Those stories are fine—nice feature writing and news accounts. But my memory is filled with the emotion and remark-able teamwork during the acute ten days o Matthew Winkler’s recovery. No one ever wrote about that part o the story. It’s a shame.” A pediatri-cian, om Weis led the eort to save Matt during those acute days.“What do you mean?” I asked. His voice tremored and tears slid over his checks. I listened for an hour. “Oh, I see what you mean.”Tom was correct. After nine interviews, I understood his tears. hese memories were powerful, and the skills used by the treatment team were noteworthy for the next generation. No, a set o transcribed interviews would not do. So, I wrote the story I heard from participants and exchanged drafts with everyone. By September 2022, we were done. Everyone involved in this remarkable story wanted to see one another, so a reunion was in order. he Winkler family and clinicians gathered at noon on Sunday, September 5, 2022. e marveled at simply seeing each other—fifty-two years had passed. Like spokes in a bicycle wheel, everyone traveled from all directions inward to Lima, since everyone lived many miles outside o town. he warm temperature enabled us to sit outside, in a decorated carport that looked more like a picnic shelter, with hanging flowers, folding chairs, and card tables. e shared hugs and memories. e spoke for two hours, non-stop. Lunch didn’t begin until 2 p.m. hrough the years, admittedly everyone had wondered about the other. he afternoon was filled with goosebumps, tears, marvel, joy, relie, gratitude, and contentment. Introduction
xiiiFACING THE IMPOSSIBLE As we busted into eating cookies, we armed that the oral history should have an additional section—they all felt the skills they used to help Matt were timeless. However, reading the oral history set in the 1970s could easily be dismissed for the simple reason that the relevant technology and research are vastly dierent today. rue. But these clinicians worked in medicine for many decades after caring for Matt. hey’d seen the rise o technology and research. hey respect-fully disagreed. On Monday, September 6, 2022, we presented the oral history to young doctors over their lunch hour at St. Rita’s graduate education program. In a panel format, om Weis, Mike Hattwick, and Sally Dailey shared their memories. However, that was one day, one hour, and one auditorium filled with hungry doctors. hat was a small audience. On Tuesday, phase two o this project began. Our challenge: Gather reflections from the Lima team about the art o medicine and find contemporary physicians who blend the art o medicine with the science that improves healing through evidence-based research and training. The skills that make up the art o medicine can be learned through mentorship and training. o enhance learning, the Lima team wanted to oer both the oral history and other contemporary resources for clinicians and patients alike. The Art o Medicine sections are the culmination o this research and features three such national physicians, Rachel Remen, Helen Riess, and Wayne Jonas as well as reflections from Lima clinicians and a sampler o brie essays. — M. F.W.
xvThe story begins with the remembrances o the ten long days o acute care that the pediatric team provided to Matthew Winkler. Their memories detail a blend o clinical strategies (the science o medi-cine), the personal interactions, and unwavering eort that the family, the clinicians, and the hospital administration drew on to enhance healing (the art o medicine). No question, Matthew Winkler recovered because everyone involved oered every ounce o their knowledge and spirit, non-stop for ten days.Their memories reveal that a very adept team received Matt. ith twenty years o experience, Jean Meyerhoer, the charge nurse, led the pediatric floor and built a team filled with mutual respect. om Weis, the Lima pediatrician, and Mike Hattwick, the internist from the Centers for Disease Control and Prevention, shared a common frame-work, which they described as “treat the whole person,” a central motto at Georgetown University School o Medicine. In hindsight, this deeply informed their approach to Matt’s care. In fact, this perspective bound everyone involved, from the senior administration to nursing aides. “Our sole purpose: caring for a very ill boy and his family. e were used to challenges and very supportive o each other. e just moved ahead. e certainly didn’t think this is gonna be the first person to survive rabies,” said Sally Dailey, a nurse on the pediatric team. Ten long days. The oral history o this remarkable medical accomplishment revealed a whole other realm o care that, to this writer, is almost more noteworthy and carries a deeper legacy and lesson o historical record—the art o medicine. The Reflections section shares the Lima team’s art-of-medicine skills, including humility that enables mutual learning and agility, caring for the whole person, self-reflection through prayer or meditation, being at ease with the unknown, empathy, and constant communication. Participants’ descriptions revealed that, at every stage o Matt’s acute care, family members, clinicians, and administrators used these skills. From the nursing perspective, Rita Deerhake and Kay Wellman, both with long clinical and administrative leaderships roles at St. Rita’s, also share their reflections and analysis. An OverviewTheirmemoriesreveal thata veryadept teamreceivedMatt.
xviMARY F. WEISThe After 1970 section oers a bit about several subsequent cases, most notably Jeanna Giese’s survival in 2004, which was led by pedia-trician Rodney Willoughby at Children’s Hospital o Wisconsin in Milwaukee. Giese was the first unvaccinated rabies survivor. illoughby had contacted Tom for counsel and shares some common skills. He developed the “Milwaukee protocol.” The Medical College o Wisconsin hosts a website to disseminate the protocol information and gathers ongoing case summaries. The Art o Medicine section features three well-designed, road-tested frameworks currently applied nationwide and created by physi-cians who’ve researched and witnessed the positive eects o blending the human spirit or humanity with science: Rachel Remen’s The Healer’s Art, Helen Riess’s The Empathy Eect, ayne Jonas’s How Healing Works. The three frameworks are briefly introduced in this section and described in greater detail in the next segment. All three frameworks are accessible to everyone.For readers that want to further explore the art o medicine, please read the Supplemental Reader section. his section features a few more stories, some research, and reflections that compliment Remen’s, Riess’s, and Jonas’s frameworks. he art o medicine skills are best understood through story, conversation, and reflection. ith this in mind, the oral history and featured stories are a resource. Grab a colleague, a mentor, a classmate, a family member, or friend and share how these stories inform your professional or personal life. Most often, these skills are narrowly explored in the moments o conversation between a clinician and patient. However, as the oral history reveals, they can reside amongst members o an entire team, departments, and at an institutional level. Under the right circum-stances, when groups create a common culture, clinical care shifts to become more creative and precise.After the Remen, Riess, and Jonas stories, this Supplemental Reader features Hanna Ihlebaek’s research, which delves into patient care conversations between nurses during a shift change, and Jonathan Ilegen’s research, which features moments o uncertainty by novice and experienced emergency room physicians and how they manage patient safety and quality o care.Then enjoy three, first-person essays that convey beautiful, tender, goosebump moments illustrating the power o this skill between a clini-cian and a patient—by nurse practitioner Jennifer Bradley and physicians Jean Brutus and Gina Siddiqui.
xviiI anyone enjoys memoirs, physician and anthropologist Arthur Kleinman recently wrote about caring for his wife with early dementia. The title o the book says it all, The Soul of Care, A Moral Education of a Husband and a Doctor. Another book to consider is The Telltale Hearts, A Public Health Doctor, his Patients, and the Power of Story by Dean-David Schillinger. He shares vivid personal experiences o how he gained the skill o deeply listening to patients. He had many hurdles. As a primary care physician working in San Francisco General Hospital caring for the city’s most marginalized, he quickly understood that he needed to listen to his patients’ lived experiences. He had a dual role as a physician and as a sociologist. He oers a life-time o learning moments as he describes how he approached this dual role in his clinical practice and later in his career in public health research and advocacy. The Appendices features a website link to the 1972 Case Summary by Hattwick, et. al. in the Annals of Internal Medicine, the CDC’s summary o rabies in the United States, and further resources for The Healer’s Art, E.M.P.A.T.H.Y., and How Healing Works.FACING THE IMPOSSIBLE
91With the skills o humility, self-reflection, and empathy, we bring the fullness o our own spirit and intention to one another. As we sit three feet apart from each other in a clinical setting, we engage in a conversa-tion that includes both scientific knowledge and love. A clinician skilled in the art o medicine witnesses the beauty o the person’s smile, their ease/calmness, fear/tears, or a small accomplish-ment/joy. his is the tenderness o caring and sharing our common humanity. I sense many clinicians have experienced the beauty when a patient and a clinician come together in a mutual place o learning and healing, and the subsequent joy when the patient feels better, maybe not cured, but better. And the ultimate delight is the mutual joy o caring for one another. I agree with Mike Hattwick, it feels magical.— M. F.W.AfterwordFinally: The mutual joy of caring feels magical
Press Conference (left to right): Thomas T. Weis M.D., pediatrician; John Ackerman M.D., chief of the Bureau of Preventive Medicine Ohio Department of Health; C. John Stechschulte M.D., attending pediatrician; and Robert S. Oyer M.D., Allen County health commissioner, December 21, 1970.
104Appendix1. “Recovery from Rabies, A Case Report,” June 1972by Michael A Hattwick M.D., homas T. eis, M.D., C. John Stechschulte, M.D., George Baer, D.V.M., and Michael B. Gregg M.D. published in the Annals of Internal Medicine, 76, no. 6 (June 1972): 931-942. The publisher American College o Physicians has provided a web page link to those interested in reading the full report. hank you. https://www.acpjournals.org/stoken/default+domain/0003-4819-76-6-931full?redirect Uri=/doi/10.7326/0003-4819-76-6-9312. Rabies TodayRabies is a fatal but preventable viral disease. It can be spread to people and pets through the bites and scratches o an infected animal. Rabies primarily aects the central nervous system, leading to severe brain disease and death i medical care is not received before symptoms start. Immediate medical attention following suspected rabies exposure is critical. Medical care following a rabies exposure is called post-exposure prophylaxis or PEP. PEP includes wound care, a dose o human rabies immune globulin (HRIG), and a series o four or five rabies vaccines, which must be administered as soon as possible after exposure. his care is vital to prevent the disease from developing. It is nearly 100 percent eective i administered promptly. Each year, 60,000 Americans receive PEP after a potential rabies exposure. The disease is rare in humans in the United States, with only one to three cases reported each year. Still, rabies poses a serious public health threat, because o its high death rate in people. It is also present in many wildlife species, nearly three in four Americans live in a community where raccoons, skunks, or foxes carry rabies.In the United States, more than 90 percent o reported cases o rabies in animals occur in wild-life. Contact with infected bats is the leading cause o human rabies deaths in this country; at least seven out o ten Americans who die from rabies in the U.S. were infected by bats. he animals most often found with rabies in the U.S. include bats, raccoons, skunks, and foxes.Worldwide: Dogs cause 99 percent o human rabies deaths outside the United States and every year, rabies kills 70,000 people worldwide.PREVENTIONRabies prevention eorts by veterinary, wildlife management, and public health professionals mean that human cases o rabies in the U.S. are rare. eterinarians vaccinate over forty million cats and dogs each year, and these vaccinations significantly reduce the risk o you or your pets getting rabies. Each year, wildlife management professionals distribute oral vaccines to wildlife, through baits, to control rabies at its source, especially in areas where rabies in wild animals is common.
105FACING THE IMPOSSIBLE The best way you can prevent rabies is by: • Making sure your pets are up-to-date on their rabies vaccines;• Keeping wildlife wild by staying away from wildlife for both human and animal safety;• Calling animal control to remove stray animals from your neighborhood;• Washing bites or scratches immediately with soap and water; and• Seeking medical care shortly after potential exposures.IF BITTENWhat kind o animal did you come in contact with?Any mammal can get rabies. ou should consult a healthcare provider after a bite from any animal. It could be safe to delay rabies-related care, called postexposure prophylaxis, while waiting for the results o a test or observation period. However, i the bite is severe, especially near the head, or i it’s from high-risk animals like bats, raccoons, skunks, or foxes, post-exposure prophylaxis should begin right away.Source: reprinted from United States Center for Disease Control and Prevention, https://www.cdc.gov/rabies/about/index.html, May 2024.3. The Healer’s Art resources, Rachel Naomi Remen, M.D. Training: Remen Institute for Study o Health and Illness (RISHI), right State University Boonshoft School o Medicine, Dayton, Ohio, Healer’s Art Overview: https://rishiprograms.org/healers-art/Books: Rachel Noami Remen M.D., Kitchen Table Wisdom, Stories that Heal, New York, Riverhead Books, 1996 and 2006 and My Grandfather’s Blessings, Stories of Strength, Refuge, and Belonging, New York: Riverhead Books, 2000.Research: Jaiswal, C., Anderson, K. & Haesler, E. “A Self-Report o the Healer’s Art by Junior Doctors: Does the Course Have a Lasting Influence on Personal Experience o Humanism, Self-Nurturing Skills and Medical Counterculture?” BMC Medical Education, 19, 443, (published November 29, 2019). https://doi.org/10.1186/s12909-019-1877-3 4. Empathy resources, Helen Riess, M.D. Training: Empathetics, Inc., for a range o available courses, https://www.empathetics.comBook: Helen Riess, M.D., The Empathy Eect, Seven Neuroscience-based Keys for Transforming the Way We Live, Love, ork and Connect Across Dierences, Boulder, CO: Sounds True, Inc, 2018.Research: Helen Riess, M.D., “The Science o Empathy,” Journal of Patient Experience, ol 4(2) (2017): 74-77. Helen Riess, M.D. and Gordon Kraft-Todd, “E.M.P.A.T.H.Y: a Tool to Enhance Nonverbal Communication Between Clinicians and their Patients,” Academic Medicine, ol 89(8) (August 2014): 1108-1112.
106MARY F. WEISMassachusetts General Hospital, Empathy and Relational Science Program, https://www. massgeneral.org/psychiatry/research/empathy-and-relational-science-program“Empathetics Evidence-Based Solutions for Healthcare’s Multiple Crisis; Empathy Improves Member and Employee Experience, Reduces Burnout and Resignation.” White paper. 2024. Boston: Empathetics Inc. 5. Whole Person Care resources, Wayne Jonas, M.D. Training: Continuing Medical Education Course (CME)Clinician as a Healer in Primary Care, Introducing Whole Person Care into Your Practice, a continuing medical education course, 2024, no charge. ufts University School o Medicine Oce o Continuing Education (TUMC OCE), phone 617-636-6579, https://healingworksfoundation.org/clinician-as-healer-in-primary-care/Podcast about CME Course: Dr. Lauri Medina, Whole Person Health and New CME Course, How Healing Works Podcast with Wayne Jonas M.D., June 27, 2024. Apple: https://podcasts.apple.com/us/podcast/how-healing-works-with-dr-wayne-jonas/id1687537976?i=1000618438427 Vimeo: https://vimeo.com/828070275?share=copyBooks: Wayne Jonas, M.D. How Healing Works, Get Well and Stay Well, Using Your Hidden Power to Heal, California: Lorena Jones Books, 2018. Jonas has co-authored Healing and Cancer, A Guide to Whole Person Care with Alyssa McManamon, M.D, Rodin Books, 2024.Website: Healing Works Foundation: https://healingworksfoundation.orgResearch: Elena Rosenbaum, Andrea E. Gordon, Jake Cresta, Allen F. Shaughnessy and Wayne B. Jonas, “Innovations in Primary Care, Implementing Whole Person Primary Care,” The Annals of Family Medicine, ol 21(2), (March 2023):188. DOI: 10.3122/jabfm.2023.230007R1Podcast: Wayne Jonas, How Healing Works podcast. he programming began May 04, 2023. Healing Works Foundation. https://podcasts.apple.com/us/podcast/how-healing-works-with-dr-wayne-jonas/id1687537976?i=1000612668249INTEGRATIVE HEALTH LEARNING COLLABORATIVEThe Integrative Health Learning Collaborative sought to better manage chronic disease by addressing social and behavioral determinants o health to improve the delivery o whole-person care and make integrative health routine and regular in primary care.103 Seventeen clinics partici-pated in the learning collaborative. hey received training in integrative health, the support o expert faculty, and access to integrative health tools and resources as they worked to make inte-grative health routine and regular in primary care. The clinics were mostly family medicine residencies, federally qualified health centers, and other clinics and health systems. Participating clinics targeted dierent patient populations for their integrative health work, including patients with specific diagnoses (e.g., chronic pain,
107FACING THE IMPOSSIBLE diabetes, hypertension, obesity, anxiety/depression, or multiple chronic conditions), patients new to or interested in integrative health, and all patients.The Family Medicine Education Consortium and the Samueli Integrative Health Programs sponsored the learning collaborative from October 2020 to September 2021, with a grant from The Samueli Foundation. Participants:• BronxCare Health System Department o Family Medicine, Bronx, New York• Central Michigan University, Mount Pleasant, Michigan• Cleveland Clinic Family Medicine Residency, Cleveland, Ohio• Codman Square Health Center, Dorchester, Massachusetts• Greater Lawrence Family Health Center and Residency, Lawrence, Massachusetts• Hunterdon Family Medicine, Flemington, New Jersey• Jamaica Hospital Medical Center, Queens, New York• MetroHealth Medical Center Department o Family Medicine, Cleveland, Ohio• Middlesex Family Medicine Residency, Middletown, Connecticut• Oak Street Health, Philadelphia, Pennsylvania• Phelps Family Medicine Residency Program, Sleepy Hollow, New York• People’s Community Clinic, Austin, exas• St. Louis VA Hospital, St. Louis, Missouri • Susan Samueli Integrative Health Institute at UC Irvine, Irvine, California• University o Cincinnati Department o Internal Medicine and Pediatrics, Cincinnati, Ohio• University o New Mexico Family Medicine, Albuquerque, New Mexico• William Jenkins Medical Center and Family Medicine Residency, Berkeley, CaliforniaINTEGRATIVE ONCOLOGY LEADERSHIP COLLABORATIVE Jonas and McManamon organized a network o oncology leaders from around the world to adapt HOPE tools and resources originally applied in primary care for use in oncology practices and systems, April 2021 to December 2022.104 Participants:105 • Ann B. Barshinger Cancer Institute, Lancaster General Health, Penn Med-Pennsylvania• Davido Center, Rabin Medical Center, Clalit Health, Israel• DeCesaris Center, Anne Arundle Medical Center, Luminis Health, Maryland • James M. Stockman Cancer Institute, Fredrick Health, Maryland• John Hopkins Medicine, Maryland• Karuna Precision Wellness Center, Indiana• Life with Cancer, Inova Schar Cancer Institute, irginia• Mayo Clinic Jacksonville, Florida• Memorial Sloan Kettering Center, New York• Sentara Integrative Therapy Clinic-Sentara Health, irginia• Sidney Kimmel Cancer Center-Jeerson Health, Pennsylvania• University o California at Irvine, California• University o Calgary, Canada